- Keele Research Repository
advertisement
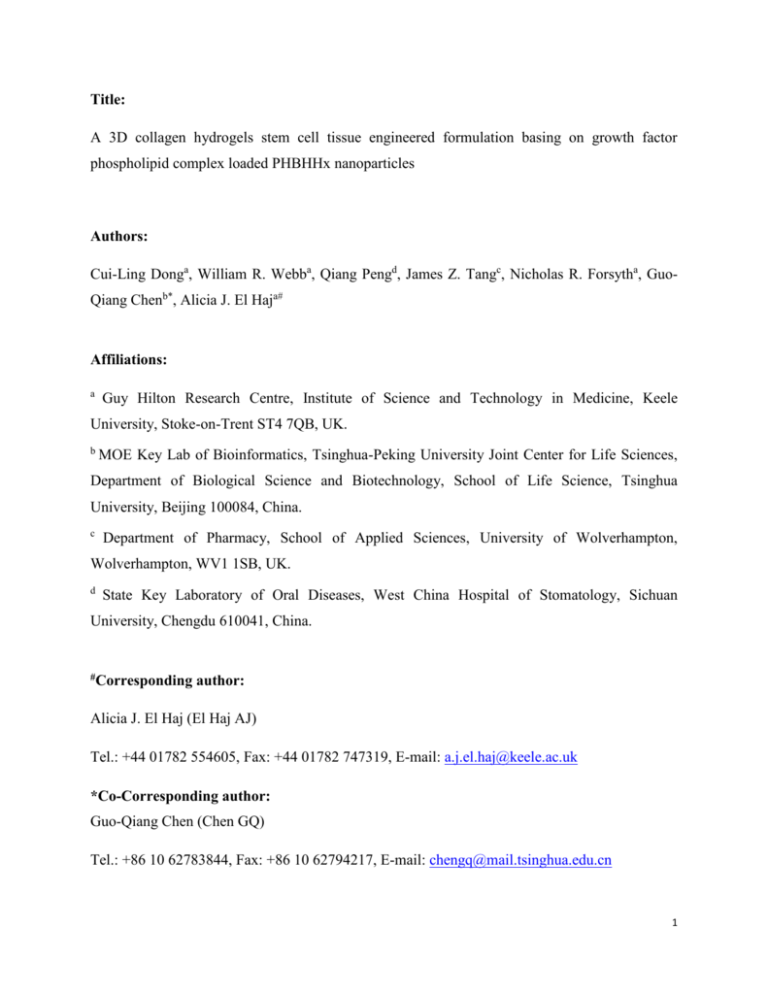
Title: A 3D collagen hydrogels stem cell tissue engineered formulation basing on growth factor phospholipid complex loaded PHBHHx nanoparticles Authors: Cui-Ling Donga, William R. Webba, Qiang Pengd, James Z. Tangc, Nicholas R. Forsytha, GuoQiang Chenb*, Alicia J. El Haja# Affiliations: a Guy Hilton Research Centre, Institute of Science and Technology in Medicine, Keele University, Stoke-on-Trent ST4 7QB, UK. b MOE Key Lab of Bioinformatics, Tsinghua-Peking University Joint Center for Life Sciences, Department of Biological Science and Biotechnology, School of Life Science, Tsinghua University, Beijing 100084, China. c Department of Pharmacy, School of Applied Sciences, University of Wolverhampton, Wolverhampton, WV1 1SB, UK. d State Key Laboratory of Oral Diseases, West China Hospital of Stomatology, Sichuan University, Chengdu 610041, China. #Corresponding author: Alicia J. El Haj (El Haj AJ) Tel.: +44 01782 554605, Fax: +44 01782 747319, E-mail: a.j.el.haj@keele.ac.uk *Co-Corresponding author: Guo-Qiang Chen (Chen GQ) Tel.: +86 10 62783844, Fax: +86 10 62794217, E-mail: chengq@mail.tsinghua.edu.cn 1 Abstract: This study aimed to design a growth factor loaded copolyester of 3-hydroxybutyrate and 3-hydroxyhexanoate (PHBHHx) nanoparticles containing 3D collagen matrix to achieve growth factor sustained release for long-term stimulation of human mesenchymal stem cells (hMSCs) proliferation/differentiation for tissue engineer application. Platelet derived growth factor-BB (PDGF-BB), which is known to enhance hMSCs proliferation in human serum, was selected as a model growth factor, and biodegradable copolyester of PHBHHx was chosen to be the sustained release vehicle. PDGF-BB phospholipid complex encapsulated PHBHHx nanoparticles were fabricated, and their effect on hMSCs proliferation was investigated via assays of CCK-8 and live-dead staining to cells inoculated in 2D tissue culture plates and 3D collagen gel scaffolds, respectively. The resulting spherical PHBHHx nanoparticles were stable in terms of their mean particle size, polydispersity index and zeta potential before and after lyophilization. In vitro study revealed a sustained release of PDGF-BB with a low burst release. Furthermore, sustain released PDGF-BB was revealed to significantly promote hMSCs proliferation in both cell monolayer and cell seeded 3D collagen scaffolds inoculated in serumfree media. Therefore, the 3D collagen matrices with locally sustained release growth factor nanoparticles hold promise to be used for stem cell tissue engineering. Key words: PHBHHx; Nanoparticles; Platelet derived growth factor-BB; Mesenchymal stem cell; Collagen hydrogel 2 INTRODUCTION Bone marrow mesenchymal stem cells (MSCs) are considered to be one of the most promising cell types in the field of tissue engineering 1. MSCs have been shown to differentiate into a number of cell types such as osteoblasts, chondrocytes, adipocytes, as well as muscle cells 2-4 , and it is known that culture conditions and growth factors are essential factors for the control of their differentiation and proliferation 5,6 . Growth factors have been shown to be powerful regulators with biological function, and their presence in MSCs is highly regulated in both time and spatial cues 7,8 . However, the rapid inactivation and extremely short plasma half-life of the growth factors prevent their sustained effect 9. It is therefore essential to develop a carrier system to maintain growth factors at an effective concentration for a longer period, which potentially can direct MSCs differentiation spatially in a 3D environment 10-11. Among the possible strategies to achieve sufficient bioavailability of growth factors, nanoparticle carriers made from biodegradable polymers represent an exciting approach to improve the transport of growth factors and its subsequent initiation of a cellular response 12-14 . Compared with other colloidal carriers, such as submicron emulsions and liposomes, biodegradable polymeric nanoparticles offer a higher stability when they are in contact with biological fluids 15,16. The polymeric nature of nanoparticle also protects the growth factors from adverse external conditions and controls their release during the polymer degradation process 17. Poly-3-hydroxybutyrate-co-3-hydroxyhexanoate (PHBHHx), including its other members of polyhydroxyalkanoates (PHA) biopolyester family, has been extensively studied as a tissue engineering biomaterial and considered to be a very promising biomaterial due to its total biodegradability, non-toxic, non-immunogenic degradation products and better elastic properties 18-23 . PHBHHx was ever used as a biodegradable nanoparticle carrier for sustained release of hydrophobic drugs due to its hydrophobic ester backbone and alkane side chain 24,25 . However, most growth factors are hydrophilic proteins and this poses a significant challenge to encapsulating not hydrophobic protein into hydrophobic PHBHHx nanoparticles efficiently. In a previous study, Peng et al 26 and his group developed an attractive way to improve the liposolubility of water-soluble protein with a higher entrapment efficiency by formation of a drug phospholipid complex, which is consistent with the results reported by Cui et al 12. 3 Thermo-sensitive collagen hydrogel is a free-flowing liquid under room temperature and can form a non-free-flowing gel at 37oC 27 . Based on its solution to gel transition property and favorable biological characteristics (i.e., biocompatibility, biodegradability), the thermo-sensitive hydrogel has been widely studied as a 3D tissue engineer scaffold. Herein, we propose to prepare the growth factor phospholipid complex loaded PHBHHx nanoparticles to achieve growth factor sustained release for long-term stimulation of hMSCs proliferation/differentiation in 3D collagen hydrogel cell culture systems. A growth factor, platelet derived growth factor-BB (PDGF-BB), which has previously been demonstrated to maintain undifferentiated proliferation of mesenchymal stem cells 28 , was used as a model growth factor due to its ease of analysis and ready availability. PDGF-BB phospholipid complex loaded PHBHHx nanoparticles (PDGF NPs) were fabricated, then co-embedded in collagen hydrogel with hMSCs. The sustained release PDGF-BB from PDGF NPs was evaluated and its effect on human MSCs proliferation was investigated via assays of Cell Counting Kit-8 (CCK-8) and live-dead staining to cells inoculated on 2D tissue culture plate and 3D collagen gel scaffold, respectively. MATERIALS AND METHODS Materials PHBHHx [Poly(R-3-hydroxybutyrate-co-12 mol% R-3-hydroxyhexanoate)] was supplied by Lukang Group (Shandong, China). Recombinant human PDGF-BB was purchased from Peprotech (NJ, USA). Human PDGF-BB quantikine ELISA kit was bought from R&D systems (UK). DMEM containing high glucose, L-glutamine, non-essential amino acids (NEAA), and phosphate buffered saline (PBS), were purchased from Lonza (Switzerland). Rat tail collagen type I was provided by BD Biosciences (UK). Cell Counting Kit-8 (CCK-8) was supplied by Dojindo (Japan). Live-dead cell double staining kit, l-α-phosphatidylcholine, poloxamer 188 (F68), sodium deoxycholate, acetic acid, dimethyl sulfoxide (DMSO) and chloroform were purchased from Sigma Aldrich (SL, USA). All other chemical reagents were analytical grade or better (Sigma Aldrich, USA). Fabrication of PHBHHx nanoparticles 4 PHBHHx nanoparticles were prepared based on a method reported previously 26 with some modifications. PDGF-BB and l-α-phosphatidylcholine were co-dissolved in DMSO containing 1.25% glacial acetic acid under magnetic stirring at 30°C, then freeze-dried overnight to obtain PDGF-BB phospholipid complex (PDGF-PLC). PHBHHx and PDGF-PLC were dissolved or dispersed in chloroform at a weight ratio of 80:1. Subsequently, an aqueous solution containing 0.5% F68 and 0.5% sodium deoxycholate was added to the organic solution with a volume ratio of 20:1, and followed by sonication in an ice-water bath to form a stable o/w emulsion. A homogeneous fresh nanoparticles suspension was obtained after chloroform evaporation. Before storage, 10% maltose was dissolved in nanoparticles suspension. The mixture was frozen at 80°C overnight followed by lyophilization for 48 h. Blank NPs and BSA NPs were prepared as controls using the same protocol. Physicochemical characterization of PHBHHx nanoparticles The mean particle size, distribution and zeta potential of the resulted PHBHHx nanoparticle suspension were studied using a Zetasizer 3000 HSA (Malvern Instruments Ltd., U.K.) at 25°C. The particle size was evaluated based on the intensity distribution, which was evaluated by polydispersity index (PDI). After re-dispersion in distilled water, the lyophilized PHBHHx nanoparticle suspension was measured via the same parameters as fresh nanoparticles. The morphology of PHBHHx nanoparticles was observed using a Scanning Electron Microscope (Hitachi S4500) (Japan) at an accelerating voltage of 5 kV. One drop of the resulted PDGF NPs suspension was placed on a glass surface. After an air drying process, the sample was coated with gold using an Ion Sputter. Encapsulation efficiency of PHBHHx nanoparticles Briefly, 0.5 ml the resulted PDGF NPs suspension was mixed with 0.5 ml 0.05 M NaOH. The mixture was stirred for 24 h at room temperature so that the PHBHHx nanoparticles could be degraded by alkaline hydrolysis. The resultant sample was analyzed by ELISA kit after proper dilution. As a result the total added amount of PDGF-BB (Wt) was obtained. Meanwhile, another 0.5 ml PDGF NPs suspension was taken, and mixed with 0.5 ml dH2O. The sample was also analyzed by ELISA kit after proper dilution. As such the amount of non-encapsulated PDGF-BB (Wn) was obtained. Therefore, the encapsulation efficiency could be calculated according to the following equation: 5 EE = (Wt - Wn) / Wt × 100% In vitro release kinetic of PDGF-BB from PDGF NPs PDGF-BB release profile was measured using the dialysis tube (Spectrum Labs) with 100 kDa molecular weight cut off, which keeps PDGF NPs in and allows the released PDGF-BB out of the tube. After 1 ml PDGF NPs suspension was transferred into a dialysis tube, the sample loaded dialysis tube was soaked in 6 ml dH2O at room temperature under magnetic stirring. At predetermined time intervals the dH2O outside the dialysis tube was withdrawn completely and replaced with 6 ml fresh dH2O. The collected samples were diluted into 10 ml then stored at 80°C for ELISA kit analysis. Optimization of PDGF-BB concentration for hMSCs proliferation Primary human mesenchymal stem cells (Lonza) were employed to investigate optimal PDGF-BB concentration to promote hMSCs proliferation in vitro. hMSCs (passage 3-5) were plated in 96-well plates with a cell density of 4×103 cells per well, and cultured for 24 h on a full serum medium (DMEM supplemented with 5% fetal bovine serum, 1% L-glutamine and 1% NEAA). Then followed by 24 h culture in serum free medium (DMEM supplemented with 1% L-glutamine and 1% NEAA). PDGF-BB was supplemented at final concentrations of 0, 5, 10, and 25 ng/ml, respectively, with 1% NEAA and 1% L-glutamine in DMEM media. At multiple time points, cell proliferation was evaluated using the CCK-8 assay. Effect of sustained released PDGF-BB on hMSCs proliferation in 2D cell culture system hMSCs were seeded in 6-well plates at the density of 5×104 cells per well, and cultured for 2 days with a full serum medium to reach about 50% confluence. Then followed by 24 h culture in serum free medium. hMSCs were incubated in sterile PDGF NPs contained serum-free media. Cell viability was measured using CCK-8 kit after culturing for 2 and 4 days, respectively. Cells cultured in BSA NPs, blank NPs and no NPs contained media were used as controls. Effect of sustained released PDGF-BB on hMSCs proliferation in cell seeded 3D collagen hydrogels hMSCs were seeded in T75 flasks, then cultured for 3 days with the full serum medium, followed by 24 h culture in serum free medium. After the trypsinizing treatment, hMSCs suspension in DMEM media, sterile 10×DMEM, sterile concentrated PDGF NPs suspension, 6 sterile 1 M NaOH, and rat tail collagen, were combined according to the BD Biosciences (UK) manufacturer’s instructions in ice bath to produce a final concentration of 2×105 cells/ml in 0.5 mg/ml collagen gel. After mixing homogeneously by pipetting, a volume of approximately 400 µl was dispensed into 6-well plates. After incubation in 37oC for 30 min, the collagen scaffold was covered with serum-free DMEM media, and incubated in 37oC incubator. Cell viability was measured using CCK-8 kit after culturing 2 and 4 days, respectively. In addition, the overall cell morphology was monitored via a live-dead cell double staining kit using Nikon Eclipse T1 microscope fluorescence microscope (Japan) at day 2 and 4. Collagen scaffolds fabricated with BSA NPs, blank NPs and no NPs were used as controls. Statistical analysis All data was expressed as the mean ± standard deviation (SD). Statistical analysis was carried out using the unpaired Student’s t-test (Microsoft, Seattle, USA). P < 0.05 was considered to be statistically significant and P<0.01 highly significant. RESULTS Characterization of PHBHHx nanoparticles before and after lyophilization The properties of PHBHHx nanoparticles before and after lyophilization were studied and compared with their mean particle sizes, PDI, zeta potentials and encapsulation efficiencies (Table 1). Among the three types of PHBHHx nanoparticles, mean particle size and PDI slightly fluctuated, while PDGF NPs and BSA NPs had significantly higher zeta potential than that of the blank NPs. In addition, the lyophilized PHBHHx nanoparticles could be dispersed in distilled water and quickly re-formed to become a homogeneous nanoparticle suspension. Compared with fresh nanoparticles, lyophilized nanoparticles became slightly larger having a higher PDI value and lower zeta potential. Importantly, the lyophilization process did not lead to a significant change in encapsulation efficiency of PDGF NPs where a slight, but non-significant decrease from 82.97% to 74.63% was observed. These results indicated that the lyophilization process did not lead to a big change on properties of PHBHHx nanoparticles. Meanwhile, the PHBHHx nanoparticles, observed via SEM, were mostly spherical in shape and well distributed in size (Fig. 1). 7 In vitro release kinetic of PDGF-BB from PDGF NPs Figure 2 showed the in vitro release profile of PDGF-BB from PDGF NPs obtained using a dynamic dialysis method. Over the 72 h course, the cumulative amounts of released PDGF-BB were almost 25%. Nearly 20% of encapsulated PDGF-BB was released during the initial 24 h, and about 5% release was observed in the late 48 h. Overall, a sustained release of PDGF-BB was achieved, and the optimal PDGF-BB concentration range could be achieved by varying of the amount of PDGF NPs in the further cell culture studies. Optimization of PDGF-BB concentration for hMSCs proliferation To determine the optimal working concentration range of PDGF-BB for hMSCs proliferation, viability of cells grown in four different concentrations (0, 5, 10 and 25 ng/ml) of PDGF-BB media was studied after 2, 4 and 6 days incubation, respectively (Fig. 3). In all cases, cells cultured in PDGF-BB media displayed improved viability when compared to the control group of cells cultured without PDGF-BB. Among three different concentrations, activities of cells cultured with 5 ng/ml and 10 ng/ml PDGF-BB were much better compared with 25 ng/ml PDGF-BB group (Fig. 3). These results suggested that the presence of PDGF-BB promoted hMSCs proliferation and 5-10 ng/ml had the most significant positive effect, while too high concentration (25 ng/ml) or negative control (0 ng/ml) was not inductive for hMSCs proliferation. Effect of sustained released PDGF-BB on hMSCs proliferation in 2D cell culture system Cell proliferation in monolayer 2D cell culture system was analyzed by CCK-8 assay. Primary hMSCs were used to evaluate cell proliferation in various nanoparticles containing media. After 2 days incubation, hMSCs cultured in PDGF NPs containing media showed the strongest increase in cell numbers compared with that in BSA NPs, blank NPs and no NPs ones (Fig. 4). Meanwhile, cells cultured in BSA NPs and blank NPs media were similar in number compared with the group cultured in no NPs contained media. After 4 days incubation, cell number increased significantly in PDGF NPs media, while little increase was observed in control groups (Fig. 4). It became clear that the presence of PDGF NPs in media improved hMSCs proliferation. Effect of sustained released PDGF-BB on hMSCs proliferation in cell seeded 3D collagen hydrogels 8 After 2 and 4 days cultivation in 3D collagen scaffolds containing PDGF NPs, BSA NPs, blank NPs or no NPs, hMSCs were stained using a live-dead fluorescent double staining kit which is able to simultaneously stain viable cells green, and dead cells red. Although cell shapes in hydrogels could not be clearly observed under a fluorescence microscope, more green fluorescence was visible inside the PDGF NPs containing collagen scaffolds than that of BSA NPs, blank NPs and no NPs containing scaffolds, respectively (Fig. 5). In addition, green fluorescence was observed to become more intensive and widely distributed on day 4 compared with that on day 2, especially in the PDGF NPs containing scaffolds. This phenomenon suggests that PDGF NPs sustained release system was more effective in promoting cell proliferation than the controls outlined above. CCK-8 assay was employed to compare hMSCs viability in various nanoparticles containing collagen gels. The highest cell viability was observed in PDGF NPs containing gels, while other groups were similarly lower in viability among BSA NPs, blank NPs and no NPs controls (Fig. 6). These results again demonstrated that sustained released PDGF-BB significantly promoted hMSCs proliferation in serum-free media. DISCUSSION It is a challenge to directly encapsulate hydrophilic protein into hydrophobic PHBHHx vehicle. Among the present encapsulation techniques used, w/o/w method represents a relatively simple and efficient way for entrapment of hydrophilic compounds 20 . Nevertheless, the protein loading capacity of the carriers is reduced significantly due to the rapid migration and loss of drug into the external aqueous phase 20. Improving the liposolubility of hydrophilic protein is an attractive way to enhance their loading efficiency. Previous studies have shown that the lipophilicity of protein was significantly enhanced by the formation of protein phospholipid complex, and it was successfully used to fabricate a controlled release insulin nanoparticles 26,27. Based on this successful study, PDGF-BB was complexed with phospholipid by an anhydrous co-solvent lyophilization procedure, which led to the high encapsulation efficiency of PDGF-BB in the PDGF NPs system (Table 1). To prepare PHBHHx nanoparticles loaded with growth factor, different parameters including polymer concentrations, polymer and drug solvents, as well as preparation 9 temperatures were optimized to obtain nanoparticles with small particle sizes, low PDI value and high zeta potential, which indicated the fine stability of the prepared nanoparticle system (Table 1). Nevertheless, it is well known that the stable system would be destroyed due to oxidation of phospholipid, particle aggregation and/ or bacterial growth if nanoparticles were mainatianed in a suspension for a long time. Hence, lyophilization technique was applied to maintain the longterm stability of the nanoparticle system. As shown in Table 1, nanoparticles before and after lyophilization presented similar quality with a bit change possibly due to partial aggregation among nanoparticles. Generally, there are two distinct release mechanisms of encapsulated proteins from nanoparticles or microspheres. Firstly, the initial minor rapid dissociation of surface-adsorbed proteins; secondly, a sustained release of proteins ruled by thermodynamic equilibrium 29. Many studies have reported that the encapsulated proteins show a significant fast release rate with an initial burst 30,31. One potential reason is the large amount of proteins absorbed on the surface of nanoparticles; another one is the faster degradability of materials. In this study, we have shown that there is a high degree of slow release by diffusion through the nanoparticle skeleton of PDGF-BB from PDGF NPs (Fig. 2). Meanwhile, a small degree of burst release was observed potentially due to the intensive washing process and the very slow degradability of PHBHHx at this relative short period. It is well known that the attachment and spreading of cells can occur in serum containing environment since there are many cell attachment and proliferation factors in serum 32. Therefore, hMSCs were pretreated with serum free medium for 24 h before replacing the PDGF-BB containing media. In order to study the optimal PDGF-BB concentration working for hMSCs proliferation, serum free media was also selected with 0, 5, 10 and 25 ng/ml PDGF-BB, respectively (Fig. 3). In addition, since the PDGF NPs were composed of PDGF-BB, PHBHHx and l-αphosphatidylcholine, blank NPs and BSA NPs were prepared as control groups. Meanwhile, nanoparticles free media or collagen scaffold were also selected as control groups in the cell culture study. As expected, cell viability in PDGF NPs containing environment, tested by CCK-8 assay (Fig. 4 & 6), was better than those in all control groups, demonstrating that released PDGF-BB from PDGF NPs improved hMSCs proliferation. More evidence was obtained by the 10 live-dead cell double staining (Fig. 5). In this study, we have also demonstrated the use of PHBHHx nanoparticles to release growth factor in a 3D cell seeded collagen environment. The remarkable increase in cell number and viability implied the critical role of released PDGF-BB in hMSCs growth and proliferation in tissue engineering approaches. Using this technique, we can begin to spatially regulate cell differentiation within a complex tissue engineered organ. CONCLUSIONS PDGF-BB phospholipid complex loaded biodegradable PHBHHx nanoparticles fabricated by a solvent evaporation method was prepared for sustained release PDGF-BB in collagen hydrogel scaffolds. Meanwhile, BSA phospholipid complex loaded nanoparticles and blank nanoparticles were produced as controls. Physico-chemical characterization showed a small particle size, spherical shape, as well as high cytokines encapsulation efficiency. Lyophilized nanoparticles presented similar properties with the fresh ones. PDGF-BB released from PDGF NPs at a slow rate showed a slight burst release. Significantly, CCK-8 assay indicated a clearly positive effect of sustained release PDGF-BB on hMSCs proliferation regardless of whether the inoculation was in 2D tissue culture plates or in 3D collagen scaffolds. Additional live-dead fluorescent double staining assays further confirmed the CCK-8 results. It was concluded that growth factor phospholipid complex loaded PHBHHx nanoparticles was a convenient and effective approach for the sustained and controlled release of growth factors to stimulate stem cells growth, proliferation and differentiation in 3D collagen hydrogels. Therefore, the PHBHHx nanoparticle collagen hydrogel system is promising to serve as a 3D stem cell tissue engineering formulation. ACKNOWLEDGEMENTS This research was supported by the HYANJI Scaffold Project (European Commission Framework 7 program: SP3 PEOPLE- Grant agreement: PIRSES-GA-2008-230791). 11 References 1. Kern S, Eichler H, Stoeve J, Kluter H, Bieback K. Comparative analysis of mesenchymal stem cells from bone marrow, umbilical cord blood, or adipose tissue. Stem Cells 2006;24:12941301. 2. Sarkar D, Ankrum JA, Teo GSL, Carman CV, Karp JM. Cellular and extracellular programming of cell fate through engineered intracrine-, paracrine-, and endocrine-like mechanisms. Biomaterials 2011;32:3053-3061. 3. Park JS, Yang HN, Woo DG, Jeon SY, Park KH. Chondrogenesis of human mesenchymal stem cells in fibrin constructs evaluated in vitro and in nude mouse and rabbit defects models. Biomaterials 2011;32:1495-1507. 4. Pittenger MF et al. Multilineage potential of adult human mesenchymal stem cells. Science 1999;284:143-147. 5. Bianchi G, Muraglia A, Daga A, Corte G, Cancedda R. Microenvironment and stem properties of bone marrow-derived mesenchymal cells. Wound Repair Regen 2001;9:460-466. 6. Deasy BM, QuPeterson Z, Greenberger JS, Huard J. Mechanisms of muscle stem cell expansion with cytokines. Stem Cells 2002;20:50-60. 7. Molloy T, Wang Y, Murrell G. The roles of growth factors in tendon and ligament healing. Sports Med 2003;33:381-394. 8. Thomopoulos S, Das R, Sakiyama ES, Silva MJ, Charlton N, Gelberman RH. bFGF and PDGF-BB for tendon repair: controlled release and biologic activity by tendon fibroblasts in vitro. Ann Biomed Eng 2010;38:225-234. 9. Chan BP, Fu S, Qin L, Lee K, Rolf CG, Chan K. Effects of basic fibroblast growth factor (bFGF) on early stages of tendon healing: a rat patellar tendon model. Acta Orthop Scand 2000;71:513-518. 10. Tzeng SY, Hung BP, Grayson WL, Green JJ. Cystamine-terminated poly(beta-amino ester)s for siRNA delivery to human mesenchymal stem cells and enhancement of osteogenic differentiation. Biomaterials 2012;33:8142-8151. 11. Park JB, Matsuura M, Han KY, Norderyd O, Lin WL, Genco RJ, Cho MI. Periodontal regeneration in class III furcation defects of beagle dogs using guided tissue regenerative therapy with platelet-derived growth factor. J Periodontol 1995;66:462-477. 12. Cui F, Shi K, Zhang L, Tao A, Kawashima Y. Biodegradable nanoparticles loaded with insulin-phospholipid complex for oral delivery: preparation, in vitro characterization and in vivo evaluation. J Control Rel 2006;114:242-250. 12 13. Zhao J, Mi Y, Feng SS. Targeted co-delivery of docetaxel and siPlkl by herceptin conjugated vitamin E TPGS based immunomicelles. Biomaterials 2013;34:3411-3421. 14. Yamanaka YJ, Leong KW. Engineering strategies to enhance nanoparticle-mediated oral delivery. J Biomater Sci Pplym Ed 2008;19:1549-1570. 15. Hans ML, Lowman AM. Biodegradable nanoparticles for drug delivery and targeting. Curr Opin Solid State Mater 2002;6:319-327. 16. Gan CW, Chien S, Feng SS. Nanomedicine: enhancement of chemotherapeutical efficacy of docetaxel by using a biodegradable nanoparticle formulation. Curr Pharm Des 2010;16:23082320. 17. Moghimi SM. Recent developments in polymeric nanoparticle engineering and their applications in experimental and clinicaloncology. Anticancer Agents Med Chem 2006;6:553-561. 18. Lu XY, Zhang Y, Wang L. Preparation and in vitro drug-release behavior of 5-fluorouracilloaded poly(hydroxybutyrate-co-hydroxyhexanoate) nanoparticles and microparticles. J. Appl. Polym. Sci 2010;116:2944-2950. 19. Wang Y, Bian YZ, Wu Q, Chen GQ. Evaluation of three-dimensional scaffolds prepared from poly(3-hydroxybutyrate-co-3-hydroxyhexanoate) for growth of allogeneic chondrocytes for cartilage repair in rabbits. Biomaterials 2008;29:2858-2868. 20. Williams DF. On the nature of biomaterials. Biomaterials 2009;30:5897-5909. 21. Francis L, Meng DC, Knowles JC, Roy I, Boccaccini AR. Multi-functional P(3HB) microsphere/45S5 Bioglass (R)-based composite scaffolds for bone tissue engineering. Acta Biomaterialia 2010;6:2773-2786. 22. Misra SK, Nazhat SN, Valappil SP, Moshrefi-Torbati M, Wood RJK, Roy I, Boccaccini AR. Fabrication and characterization of biodegradable poly(3-hydroxybutyrate) composite containing bioglass. Biomacromolecules 2007;8:2112-2119. 23. Philip S, Keshavarz T, Roy I. Polyhydroxyalkanoates: biodegradable polymers with a range of applications. J Chem Technol Biotechnol 2007;82:233-247. 24. Kılıçay E, Demirbilek M, Türk M, Güven E, Hazer B, Denkbas EB. Preparation and characterization of poly(3-hydroxybutyrate-co-3-hydroxyhexanoate) (PHBHHx) based nanoparticles for targeted cancer therapy. Eur J Pharm Sci 2011;44:310-320. 25. Xiong YC, Yao YC, Zhan XY, Chen GQ. Application of Polyhydroxyalkanoates Nanoparticles as Intracellular Sustained Drug-Release Vectors. J Biomater Sci 2010;21:127140. 13 26. Peng Q, Zhang ZR, Gong T, Chen GQ, Sun X. A rapid-acting, long-acting insulin formulation based on a phospholipid complex loaded PHBHHx nanoparticles. Biomaterials 2012;33:1583-1588. 27. Peng Q, Sun X, Gong T, Wu CY, Zhang T, Tan J, Zhang ZR. Injectable and biodegradable thermosensitive hydrogels loaded with PHBHHx nanoparticles for the sustained and controlled release of insulin. Acta Biomaterialis 2013;9:5063-5069. 28. Gharibi B, Ghuman MS, Hughes FJ. Akt- and Erk-mediated regulation of prolideration and differentiation during PDGFRβ-induced MSC self-renewal. J Cell Mol Med 2012;16:27892801. 29. Shen H, Hu X, Yang F, Bei J, Wang S. Cell affinity for bFGF immobilized heparincontaining poly(lactide-co-glycolide) scaffolds. Biomaterials 2011;32:3404-3412. 30. Tabata Y, Hijikata S, Muniruzzaman M, Ikada Y. Neovascularization effect of biodegradable gelatin microspheres incorporating basic fibroblast growth factor. J Biomater Sci Polym Ed 1999;10:79-94. 31. Liu J, Gong T, Wang C, Zhong Z, Zhang Z. Solid lipid nanoparticles loaded with insulin by sodium cholate-phosphatidylcholine-based mixed micelles: preparation and characterization. Int J Pharm 2007;340:153-162. 32. Underwood PA, Bean PA, Mitchell SM, Whitelock JM. Specific affinity depletion of cell adhesion molecules and growth factors from serum. J Immunol Methods 2001;247:217-224. 14 Table 1 Characterization of PHBHHx nanoparticles before and after lyophilization Before lyophilization After lyophilization Sample Size (nm) PDI ZP (mV) EE (%) Blank NPs 114.1±3.9 0.244±0.030 -21±1.1 --- BSA NPs 118.9±5.1 0.243±0.037 -28.4±1.9 --- PDGF NPs 119.0±0.4 0.198±0.019 -34.3±3.3 82.97±1.83 Blank NPs 149.7±1.8 0.307±0.017 -15.6±1.1 --- BSA NPs 141.3±1.5 0.275±0.013 -19.0±2.1 --- PDGF NPs 152.7±0.8 0.216±0.021 -19.8±1.1 74.63±1.18 PHBHHx: poly(3-hydroxybutyrate-co-3-hydroxyhexanoate); Blank NPs: empty nanoparticles; BSA NPs: bovine serum albumin phospholipid complex loaded nanoparticles; PDGF NPs: PDGF-BB phospholipid complex loaded nanoparticles; PDI: polydispersity index; ZP: zeta potential; EE: entrapment efficiency; Values are mean ± s.d.; n=3. 15 Figure 1. SEM image of PHBHHx nanoparticles. Scale bar: 1.00 µm; accelerating voltage: 5kV. 16 Figure 2. In vitro release profile of PDGF-BB phospholipid complex loaded nanoparticles. Each data presented as mean ± s.d.; n=3. 17 Figure 3. Viability of hMSCs cultured in different concentrations (0, 5, 10 & 25ng/ml) of PDGF-BB media using CCK-8 assay. Values are mean ± s.d. *: P < 0.05 and **: P < 0.01 compared with that of 0 ng/ml PDGF-BB media; n=3. 18 Figure 4. hMSCs proliferation study cultured in sustained release 2D cell culture system. Blank NPs: empty nanoparticles; BSA NPs: bovine serum albumin phospholipid complex loaded nanoparticles; PDGF NPs: PDGF-BB phospholipid complex loaded nanoparticles. Values are mean ± s.d. *: P < 0.05 and **: P < 0.01 compared with that of no NPs containing media; §: P < 0.05 and §§: P < 0.01 compared with that of blank NPs containing media; #: P < 0.05 and ##: P < 0.01 compared with that of BSA NPs containing media; n=3. 19 Day4 PDGF NPs BSA NPs Blank NPs No NPs Day2 Green: Live Red: Dead Figure 5. Live-dead cell double staining of hMSCs cultured in sustained release 3D cell culture system. Scale bar: 100 µm. 20 Figure 6. hMSCs proliferation study cultured in sustained release 3D cell culture system. Blank NPs: empty nanoparticles; BSA NPs: bovine serum albumin phospholipid complex loaded nanoparticles; PDGF NPs: PDGF-BB phospholipid complex loaded nanoparticles. Values are mean ± s.d. *: P < 0.05 compared with that of no NPs containing collagen scaffold; §: P < 0.05 compared with that of blank NPs containing collagen scaffold; #: P < 0.05 compared with that of BSA NPs containing collagen scaffold; n=3. 21