MOVEMENT DISORDERS

CHAPTER II
MOVEMENT DISORDERS
THE MOTOR CONTROL SYSTEMS
& THEIR DYSFUNCTION
Motor Control Systems:
1.
Pyramidal system: ( U.M.N
.)
2.
Extrapyramidal system
Rubrospinal Tract
Reticulospinal Tract
Vestibulospinal Tract
Tectospinal Tract
3.
Cerebellum
Pyramidal Dysfunction:
Paralysis: Plegia or paresis, improved by physiotherapy
Spasticity: Hypertonia of clasp-knife type
Hyperreflexia ± clonus
Babinski’s sign
Flexor spasms
Treatment of Spasticity:
Drugs Useful for Spasticity
Drug
Dantrolene sodium
( Dantrium )
Dosage
25 mg qd, slowly increased to 100 mg qd over 1 month
Main Uses
Wheelchair-bound paraplegic, spasticity of cerebral origin
Major side effects
Generalized weakness, nausea diarrhea, drowsiness, hepatotoxicity
Baclofen
( Lioresal )
10 mg qd, slowly increased to 30-100 mg qd in divided
Spinal cord lesions, flexor spasms, increased tone to
Nausea, drowsiness, depression, dyspepsia
Diazepam
( Valium ) doses
6 mg qd, slowly increased to 60 mg qd in divided doses passive movement
Spinal cord lesions, flexor spasms, increased tone to
Sedation, ataxia passive movement
Other drugs:
Tizanidine ( Sirdalud ), up to 36 mg / day
Clonidine ( Catapres )
Phenytoin ( Epanutin ), 300 mg + Chlorpromazine ( Largactil ), 300mg/day
Vigbatrin ( Sabril )
57
Other Treatments of Spacticity:
Intrathecal alcohol or phenol may → incontinence.
Botulinum toxin ( Botox ) in cerebral palsy, adductor spasm, M.S. & stroke
Peripheral nerve blockade is tried ê local anesthetic, if successful; a permanent nerve block is produced ê alcohol or 5% phenol injection.
Selective posterior rhizotomy for spasticity of cerebral palsy.
Physiotherapy: Postural adjustments, topical cooling, close splinting, & range-of-motion exercises
Transcutaneous electrical nerve stimulation ( TENS )
Cerebellar, dorsal column, & other forms of electrical brain stimulation
Orthopedic procedures
Cerebellar Dysfunction:
Clinically:
Intention tremor
Dysmetria
Dysdiadochokinesia
Hypotonia
Treatment:
Treatment of the underlying cause
Physiotherapy
Orthopedic correction of scoliosis
Destruction of the ventrolateral thalamus may alleviate cerebellar intention tremor & rubral (cerebellar outflow) tremor (have features of parkinsonian tremor & cerebellar tremor)
Medications:
Physostigmine, 8 mg / day
5- Hydroxytryptophan, 10 mg/kg/day alleviates dysarthria & postural disequilibrium
Basal Ganglia Dysfunction:
Produces movement disorders in the form of:
Akinesia or bradykinesia e.g. Parkinson’s disease & Parkinsonism
Hyperkinesia or dyskinesia e.g. Huntington’s chorea
Dystonias & tics
Drug-induced extrapyamidal syndromes:
Medications
Neuroleptics:
Phenothiazines:
Thioxanthines:
Butyrophenones:
Diphenylbutylpiperidines:
Drugs
Chlorpromazine ( Largactil )
Thioridazine ( Melleril )
Perphenazine ( Trilafon )
Trifluoperazine ( Stelazine )
Fluphenazine ( Moditen )
Chlorprothixene( Taractan )
Haloperidol ( Haldol, Safinace )
Pimozide ( Orap )
Relative severity
++ (moderate)
+ (mild)
+++ (severe)
+++ (severe)
+++ (severe)
++ (moderate)
+++ (severe)
+++ (severe)
58
Antinauseants:
Catecholamine analogues & depleting drugs:
Long-term therapy with Ldopa
Prochlorperazine ( Compazine
Metoclopraminde ( Plasil )
Domperidone ( Motilium )
Methyldopa ( Aldomet )
Tetrabenazine ( Nitoman )
Reserpine ( Serpasil )
)
Levodopa/Carbidopa ( Sinemet )
The abnormal movements produced include the following:
Acute idiosyncratic dyskinesia & dystonia
1.
Dyskinesia e.g. chorea, athetosis, ballismus
2.
Dystonia e.g. oculogyric crisis & dystonia of neck, trunk & proximal limb muscles
Treated by:
Benztropine ( Cogentin ), 1mg IM or IV, or Biperidin ( Akineton ), &/or
Diphenhydramine ( Benadryl ), 50mg IV, followed by oral medication for 48 hrs &
Stopping the offending drug
Parkinsonism :
Dose-related, occur between two days & 4 wks after starting therapy, may persist for many months
Treated by:
The antipsychotic drug dosage, or
Adding anticholinergic medcation:
Benztropine ( Cogentin ), 0.5-4mg bid, or
Biperidin ( Akineton ), 1-2mg tid, or
Trihexyphenidyl HCl ( Artane ), 1-5mg tid
Akathisia (Restlessness): Dose - related
Treated by:
Withdrawing the offending drug
Anticholinergics is only partially effective,
Benzodiazepines, Clonidine & Amantadine are effective
Tardive (late) dyskinesias : e.g. orobuccal dyskinesia
Usually occur > 1 yr after continuous neuroleptic medication
More in elderly, especially women
May include: facial & limb chorea, athetosis, dystonia & akathisia
Treatment: a.
Tetrabenazine ( Nitoman ) depletes central biogenic monoamine stores
(25mg tab.), ½ tab.,
slowly to 200mg day. b.
Reserpine ( Serpasil ) depletes central biogenic monoamine stores
0.25mg PO daily &
slowly to 2-4 mg/day. c.
Other drugs:
Baclofen ( Lioresal ), Valproic acid ( Depakine ),
Amantadine ( Mantadix, Adamine ),
Clonidine ( Catapres )
Carbidopa/Levodopa ( Sinemet )
59
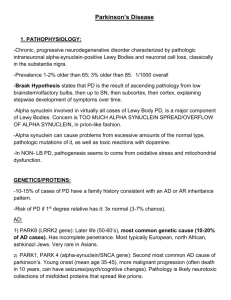
PARKINSON’S DISEASE
Organization of the basal ganglia:
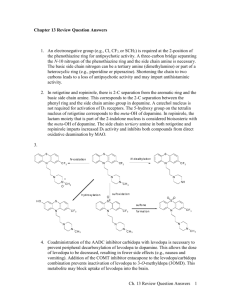
Fig. 1 Classic model of the organization of the basal ganglia in:
A. Normal; B. Parkinsonism; C. Levodopa – induced dyskinesia
GPe = globus pallidus pars externa
PPN = pedunculopontine nucleus
GPi = globus pallidus pars interna
SNc = substantia nigra pars compacta
SNc = substantia nigra pars reticularis
VL = venteralis lateralis
STN = subthalamic nucleus
STN & GPi are upregulated in PD, leading to increased inhibition of brain stem & thalamocortical neurons with the development of parkinsonian motor features
In contrast, dyskinesia is believed to be related to decreased firing in the STN & GPi, with reduced inhibition of thalamus & motor cortical regions
Pathophysiology of Parkinson’s disease
Three major changes have been identified in the “substantia nigra” of parkinsonian pts at autopsy:
1.
Evidence of oxidative stress & depletion of reduced glutathione
2.
High levels of total iron with reduced ferritin buffering
3.
Mitochondrial complex I deficiency
I.
The oxidative stress hypothesis:
Because aerobic cells use molecular oxygen as the terminal electron acceptor in oxidative phosphorylation , they must be capable of dealing with the side effects of oxygen & its reactive derivatives e.g.: a) Superoxide anion radical b) H
2
O
2 c) Hydroxy radicles
60
Superoxide is reduced to H
2
O
2
, O
2
& water by enzymes e.g. suproxide dismutase , catalase & glutathione peroxidase or by interaction with transitional metals (Cu, Fe) → hydroxyl radicals → apoptosis .
In addition to reduction by enzymes , free radicals are opposed or destroyed by several defense mechanisms which include: a) Antioxidant molecules e.g. glutathione b) Scavengers e.g. vit.E & ascorbate which react directly with free radicals to prohibit their damaging effects c) The post-oncogene bel-2 (located on mitochondrial membrane) which blocks apoptosis by ↓ generation of the reactive oxygen species
The brain is vulnerable to oxidative stress as neuronal membranes are rich in radicalssuspected unsaturated fatty acid
The brain's antioxidant defenses are weak with low levels of glutathione , almost no catalase , & low concentration of glutathione peroxidase & vit.E
The brain's relatively high oxygen consumption & susceptibility to physiologic disequilibrium → oxidative stress → free radical damage
The substantia nigra (which is rich in dopamine ) could undergo both MAO-mediated enzymatic oxidation & auto-oxidation to neuromelanin , H
2
O
2
→ free radicals in its neurons
Normally lipid permeation can be inhibited by vit.E
or by the enzyme glutathione peroxidase which removes H
2
O
2
& lipid peroxides
Glutathione is transformed to oxidized glutathione disulfide by H
2
O
2
in conjunction with glutathione peroxidase
Reduced glutathione is regenerated by the action of glutathione reductase
Only 1 % of total glutathione are normally present in the brain, but levels ↑ with oxidant stress
Peroxide mediated changes in glutathione could arise from levodopa therapy
Levodopa → quinones → irreversible addition products with glutathione → its permanent removal from further participation in cellular defense mechanisms
Levodopa therapy may contribute to the observed change in brain glutathione/glutathione oxidized disulfide
In neurodegenerative diseases , neurons die by apoptosis (= programmed cell death) which can be induced by: a) Glutathione depletion b) Chronic inhibition of superoxide dismutase c)
β–amyloid fragments d) Dopamine e) Ischemia
II.
Altered iron metabolism hypothesis:
Neurodegeneration → defective iron uptake & storage
Iron can facilitate decompensation of lipid peroxides & formation of hydroxyl radicals
The free ionic form of iron (if not used by enzymes as a cofactor ), is largely bound to the storage & transport proteins, ferritin & transferritin , or to low molecular weight chelators e.g. ATP , ADP & citrate
Transferritins are the main iron-binding proteins in body fluids
The neuromelanin in dopaminergic nigro-striatal neuron has binding sites for ferric iron , thus can serve as a buffer for free iron
Iron is involved in many progressive neurodegenerative diseases e.g. PD, MSA, TSP &
AD. It is markedly increased in such diseases
61
The direct contribution of iron to the progression of neurodegeneration is evidenced by:
1.
Parkinson-like behavior responses & ipsilateral ↓ in dopamine has been induced by unilateral injection of iron into the substantia nigra of rats
2.
↑ Brain iron can → oxidative stress (interaction with peroxide → hydroxyl radical)
→ free radical – induced neurodegeneration
3.
In the presence of excess free iron , the antioxidant neuromelanin releases free iron to participate with peroxide in the formation of free radicals
III.
Mitochondrial injury hypothesis:
Mitochondrial dysfunction in PD was deduced from understandin of MPTP
(methylphenyltetrahydropyridine) mechanism of action
After conversion by monoamine oxidase type B (MAO-B) the neurotoxin's product , methylphenylpyridinium ion (MPP+), is actively taken up into dopaminergic neurons & concentrated into mitochondria , where it inhibits complex I (NADH CoQ
1
) reductase ,
(the first enzyme of the respiratory chain) → ↓ in ATP synthesis → death of the dopamine – containing neurons
Selective deficiency of complex I activity is confined to the substatia nigra particularly the pars compacta
Platelet complex I activity is significantly lower in PD pts
Glutathione could be the link between the pathogenetic hypotheses of neurodegeneration in PD: oxidative stress & mitochondrial injury
Approximately 10 % of glutathione is compartmized within mitochondria which also contain the complete enzymatic system, for detoxification of hydroperoxides
Glutathione is involved in maintaining intramitochondrial protein thiols in a reduced state
Thiols are essential to many organelles' functions , e.g. selective membrane permeability
& Ca homeostasis
↑ Production of peroxide within mitochondria → depletion of glutathione , oxidation of protein thiols & impairment of mitochondrial function
Glutathione synthesis requires ATP & so a deficient mitochondrial activity → impairment of the cellular turnover of glutathione → ↑ susceptibility of dopaminergic neurons of the substantia nigra to oxidative damage
A cascade of events involving both oxygen radicals & mitochondrial metabolism contribute to cell injury
The Genetics & Pathogenesis of Parkinson’s Disease
The identification of three genes and several additional loci associated with inherited forms of levodopa-responsive PD has confirmed that this is not a single disorder. Yet, analyses the structure & and function of these gene products point to the critical role of of protein aggregation in dopaminergic neurons of the substantia nigra as the common mechanism leading to neurodegeneration in all known forms of this disease. The three specific genes identified to date —
α
-synuclein, Parkin, & and ubiquitin C terminal hydrolase L1
— are either closely involved in the proper functioning of the ubiquitin-proteasome pathway or are degraded by this protein-clearing machinery of cells. Knowledge transmitted PD also has clear implications for nonfamilial forms of the disease . Lewy bodies , even in sporadic PD gained from genetically
, contain these three gene products, particularly abundant amounts of fibrillar α -synuclein . Increased aggregation of α -synuclein by oxidative stress , as well as oxidant-induced proteasomal dysfunction , link genetic & and potential environmental factors in the onset & and progression of the disease. The biochemical & and molecular cascades
62
elucidated from genetic studies in PD can provide novel targets for curative therapies
(Neurology 2002;58: 179-185).
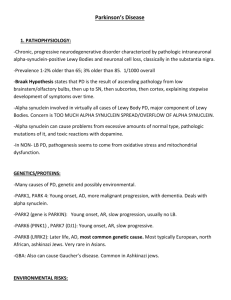
Fig. 2 Proposed pathogenetic cascades leading to neuronal death in PD. The accumulation of insoluble and /or toxic intermediates appears to be a central factor in these processes regardless of the specific gene mutation or potential environmental factor.
Genes responsible for dopa-responsive parkinsonism:
Gene Locus
α -Synuclein 4q21-q23
Parkin
UCH-L1
6q25.2-q27
4q14-15.1
? (PARK3) 2p13
? (PARK4) 4p15
? (PARK6) 1p35-p36
? (PARK7) 1p35-36
Inheritance
Autosomal dominant
Autosomal recessive
Autosomal dominant
Autosomal dominant
Autosomal dominant
Autosomal recessive
Autosomal recessive
Phenotype slightly early onset
Juvenile onset
Typical PD
Typical PD
PD/essential tremor
Early onset
Early onset
Lewy bodies
+
-
?
+
+
?
?
SCA3
SCA2
14q32.1 Apparent autosomal dominant Apparent typical PD
12q23-q23.1 Apparent autosomal dominant PD/ataxia/supranuclear gaze palsy
?
?
Besides α -Synuclein, Parkin, and UCH-L1, four additional loci are linked to inherited PD.
The actual genes in these loci responsible for PD are still unknown. The association of triplet repeat expansions in the supranuclear ataxia SCA3 and SCA2 genes with clinical parkinsonism also has been described. The pathology or molecular events that link the latter mutations to death of nigral neurons are currently unknown.
63
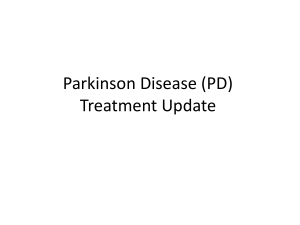
Fig. 3 Dopamine-induced apoptotic cascade. Dopamine either synthesized by a cell or tansported across the plasma membrane generates ractive oxygen species (ROS).
Establishing the Diagnosis & Differential Diagnosis
Manifestations of Parkinson’s Disease
Cardinal manifestations
1.
Rest tremor
2.
Rigidity
3.
Akinesia / bradykinesia
4.
Postural instability
Secondary manifestations
1.
Cognitive / Neuropsychiatric
Anxiety
Bradyphrenia
Dementia
Depression
Sleep disturbance
2.
Cranial nerve / Facial
Blurred vision (impaired upgaze, blepharospasm)
Dysarthria
Dysphagia
Glabellar reflex (Myerson’s sign)
Mask facies
Olfactory dysfunction
Sialorrhea
3.
Musculoskeletal
Compression neuropathies
Dystonia
Hand & foot deformities
64
Kyphoscoliosis
Peripheral edema
4.
Autonomic
(including gastrointestinal & genitourinary symptoms)
Constipation
Light-headedness (orthostatic hypotension)
Increased sweating
Sexual dysfunction (impotence, loss of libido)
Urinary dysfunction (frequency, hesitancy or urgency)
5.
Sensory
Cramps
Pain
Paresthesias
6.
Skin
Seborrhea
Classification of Parkinsonism
I.
Primary (idiopathic)
Parkinson’s disease
II.
Secondary (symptomatic)
Drug-induced (phenothiazines, butyrophenones, metoclopramide, reserpine, alphamethyldopa)
Infectious (postencephalitic, syphilis)
Metabolic (hepatocerebral degeneration, hypoxia, parathyroid dysfunction)
Structural (brain tumor, hydrocephalus, trauma)
Toxic (CO, carbon disulphide, cyanide, manganese, MPTP)
Vascular
III.
Parkinsonism-plus syndromes
Cortical-basal ganglionic degeneration
Hemiparkinsonism-hemiatrophy
Dementia syndromes
Alzheimer’s disease
Diffuse Lewy body disease
Multiple-system atrophy (MSA)
Parkinsonism-amyotrophy
Shy-Drager syndrome
Sporadic olivopontocerebellar degeneration
Striatonigral degeneration
Parkinsonism-dementia-ALS complex of Guam (Lytico-Bodig)
Progressive supranuclear palsy (PSP)
IV.
Hereditary degenerative diseases
Autosomal-dominant cerebellar ataxias (includes Machado-Joseph disease )
Hallervorden-Spatz disease (HS)
Huntington’s disease (HD)
65
Mitochondriopathies
Neuroacanthocytosis
Wilson’s disease (WD)
Signs of Akinesia in Parkinson’s Disease
General
Delayed motor initiation
Slowed voluntary movements ( bradykinesia )
Diminution in voluntary movements ( hypokinesia )
Rapid fatigue with repetitive movements
Difficulty executing sequential actions
Inability to perform simultaneous actions
Decreased dexterity
Freezing
Specific
Mask facies ( hypomimia )
Decreased blink
Hypometric saccades
Hypophonia
Dysarthria
Sialorrhea
Micrographia
Dysdiadochokinesia
Difficulty rising from a chair
Shuffling gait, short steps
Decreased arm swing
Hohen & Yahr Staging Scale
It is useful to monitor the progression of PD
It divides pts into 5 different stages of severity:
1.
Unilateral disease only
2.
Bilateral disease, with or without axial involvement
3.
Mild to moderate bilateral disease, with first signs of deteriorating balance
4.
Severe disease requiring considerable assistance
5.
Confinement to wheelchair or bed unless aided
Atypical Features in Parkinsonism
Early or Predominant Feature o Young onset o Minimal or absent tremor o o o o
Atypical tremor
Postural instability
Ataxia
Pyramidal signs
Juvenile PD, HS, WD
Disease
SND, PSP, SDS
Vascular parkinsonism
Hydrocephalic parkinsonism
CBGD, OPCD
PSP, MSA (all forms)
Vascular parkinsonism
Hydrocephalic parkinsonism
MSA (particularly OPCD)
MSA (particularly SND), CBGD
Vascular or hydrocephalic parkinsonism
66
o Neuropathy o
Marked motor asymmetry
MSA (particularly parkinsonism-amyotrophy)
Hemiparkinsonism-hemiatrophy, CBGD o
Symmetrical onset o
Myoclonus o
Dementia o
Focal cortical signs o
Alien limb sign o
Oculomotor deficits o
Dysautonomia
SND, Vascular or hydrocephalic parkinsonism
CBGD, CJD
LBD, AD, CJD, MID, PSP
CBGD
CBGD
PSP, OPCA, CBGD
MSA (particularly SDS)
AD, Alzheimer’s disease; CBGD. Cortical-basal ganglionic degeneration; CJD, Creutzfeldt-
Jakob disease; HS, Hallervorden-Spatz disease; LBD, diffuse Lewy body disease; MID, multi-infarct dementia; MSA, multiple-system atrophy; OPCD, olivopontocerebellar degeneration; PSP, progressive supranuclear palsy; SDS, Shy-Drager syndrome; SND, striatonigral degeneration; WD, Wilson’s disease.
Therapeutic Protocol of PD:
Non Pharmacologic :
Education, Support, Exercise, Nutrition
Pharmacologic Therapies :
Neuroprotection : Selegiline (Jumex)
Anticholinergics
Amantadine
Dopamine Agonists
Levodopa / carbidopa
COMT inhibitors
Surgery:
Fetal Nigral Transplantation
Stereotaxic Surgery:
Ventrolateral Thalamotomy
Pallidotomy
Deep Brain Stimulation ( DBS )
Subthalamic Nucleus ( STN ) Stimulation.
Neuroprotection in PD
Possible mechanisms for obtaining neuroprotection:
Antioxidant agents
Free radical scavengers (vitamin E, glutathione, spin-trap agents)
Glutathione
Iron chelators
Agents that block glutamate-mediated toxicity
Excitatory amino acid antagonists
Glutamate-release inhibitors (e.g., Riluzole)
Glutamate reuptake enhancers
Nitric oxide synthesis inhibitors
Poly (ADP-ribose) polymerase inhibitors
Calcium channel blockers
Mitochondrial bioenergetics
Creatine
67
Co-enzyme Q1O
Ginkgo biloba
Nicotinamide
Caraitine
Anti-inflammatory agents
Nonsteroidal anti-inflammatory agents (e.g., COX-2 inhibitors)
Steroids
Estrogens
Trophic factors
GDNF
Immunophillins
Transplant strategies
Human fetal nigral transplantation
Porcine fetal nigral transplantation
Anti-apoptotic agents
Desmethylselegiline, TCH-346
Caspase inhibitors
Agents that maintain closure of mitochondrial pore (e.g., cyclosporine)
Agents that prevent protein accumulation & aggregation
Initiating therapy for Parkinson’s disease
The goals of treatment for younger pts (<60 years) with PD are control of impairing symptoms, sparing of levodopa to minimize long-term complications, & consideration of neuroprotection .
The primary initial medication choices for pts<50 years include selegiline , amantadine ,
& anticholinergic agents .
Patients in their fifties may require a dopamine agonist in addition to or instead of selegiline to achieve adequate symptom control.
If the desired response is still not achieved, sustained-release carpidopa-levodopa should be added, followed by adjunctive amantadine or anticholinergic therapy
For older patients (60 years & over) , improvement of functional impairment is the primary goal.
A special concern is to avoid inducing or exacerbating cognitive impairment.
Sustained-release carbidopa-levodopa is considered first-line treatment for these patients.
Inadequate response can be handled by a trial of immediate-release carbidopa-levodopa
& then addition of a dopamine agonist when maximum levodopa doses are reached.
Anticholinergic agents , amantadine , & selegiline should be avoided because of their
CNS effects.
68
PD
Selegiline
<50yrs
Amantadine
Anticholinergic
Agents
<60yrs
Selegiline
50-59yrs
Dopamine
Agonists
>60yrs
Sustained release
Carbidopa/
Levodopa
Switch to
Immediate release
Carbidopa/
Levodopa
Add
Sustaine release
Carbidopa/
Levodopa
Add
Dopamine
Agonist
Add
Amantadine,
Anticholinergic
Agents
Decrease
Dopamine
Agonist
Dose
Switch
Dopamine
Agonist
Add
Clozapine
Levodopa Neurotoxicity:
Levodopa therapy remains the major form of treatment for the symptoms of Parkinson’s disease (PD)
Its use may hasten the progression of nigral cell degeneration
Levodopa generates reactive oxygen species
Oxidative stress is a component of the degenerative process that occurs in PD
Autoxidation of levodopa causes oxidative stress, leading to neuronal destruction by necrosis or apoptosis
If the nigrostriatal tract is already damaged; levodopa treatment can produce further cell destruction associated with oxidative processes.
No clinical evidence to suggest that levodopa has adverse effects on dopamine cells in normal humans or on the viability of remaining dopaminergic cells in patients with PD
Adjuncts to levodopa therapy (Dopamine agonists)
The classical role of dopamine agonists in Parkinson’s disease (PD) therapy is adjunctive treatment to levodopa once “wearing-off” fluctuations or more malignant types of “on-off” swings have developed.
Dopamine agonists reduce the frequency, severity, & duration of “off” periods while allowing the levodopa dose to be reduced.
Interest is growing in the role of dopamine agonists as primary monotherapy in PD.
Studies of early monotherapy have shown that, even with sustained treatment, druginduced dyskinesias rarely develop.
Continuous dopaminergic stimulation via subcutaneous dopamine agonist infusions is being investigated as a way to control levodopa-associated peak-dose dyskinesias.
Early combined treatment with levodopa has been suggested as effective while avoiding long-term complications.
69
Despite the entry of several new dopamine agonists into clinical practice, the ideal agonist, with long duration of action & efficacy equal to that of levodopa, is still lacking.
Parkinson's Disease
DA Treatment
Reduced
Dopamine
Turnover
Reduced formation of
Free
Radicles
Reduced
Levodopa intake
Direct Stimulation of Post-synaptic
Receptors
Continueous
Stimulation of receptors
Reduced
Degeneration of pre-synaptic neurons
Protect against fluctuating levels of
Dopamine in the striatum
Neuroprotection Prevent striatal post-synaptic alteration
Mechanism of action of dopaminergic agents in Parkinson’s disease
As the substantia nigra degenerates in (PD) the nigrostriatal pathway is disrupted, reducing striatal dopamine & producing PD symptoms.
Although dopamine does not readily cross the blood-brain barrier, its precursor, levodopa, does.
Levodopa is absorbed in the small bowel & is rapidly catabolized by aromatic-L-aminoacid decarboxylase (AADC) & catechol-O-methyltransferase (COMT).
Because gastric AADC & COMT degrade levodopa, the drug is given with inhibitors of
AADC (carbidopa or benserazide), & inhibitors of COMT.
Although the exact site of decarboxylation of exogenous levodopa to dopamine in the brain is unknown, most striatal AADC is located in nigrostriatal dopaminergic nerve terminals.
70
Newly synthesized dopamine is stored in the terminals & then released, stimulating postsynaptic dopamine receptors & mediating the antiparkinsonian action of levodopa.
Dopamine agonists act directly on postsynaptic dopamine receptors, thus obviating the need for metabolic conversion, storage, & release.
Extending levodopa action (COMT inhibition)
Degradation of levodopa in the periphery is known to be associated with motor fluctuations & dyskinesia in Parkinson’s disease (PD) patients.
The enzyme catechol-O-methyltransferase (COMT) is responsible for much of this degradation. Therefore, inhibiting COMT activity is one method of extending the action of levodopa.
The new nitrocatechol-type COMT inhibitors entacapone, nitecapone, & tolcapone inhibit COMT in the periphery.
Tolcapone also inhibit COMT activity centrally.
COMT inhibitors increase patient’s duration of response to levodopa & reduce response fluctuations.
Administration may prolong levodopa-induced dyskinesia, but peak-dose dyskinesia does not appear to increase.
To reduce dyskinesia, the total daily dose of levodopa can be reduced.
Medications for Parkinson’s disease
Dopamine precursors
Levodopa in combination with a dopa decarboxylaes inhibitor ( Sinemet, Sinemet CR ).
Dopamine receptor agonists
Bromocriptine ( Parlodel )
Pergolide ( Permax )
Pramipexole ( Mirapex ).
Ropinirole ( Requip )
Cabergoline ( Dostinex, Cabaser )
Lisuride ( Dopergin )
Monoamine oxidase (MAO) B inhibitors
Selegiline ( Jumex, deprenyl, Eldepryl ).
Amantadine
( Symmetrel, Amantine, Adamine )
Catechol-o-methyltransferase inhibitors
Tolcapone ( Tasmar )
Entacapone ( Comtan )
Anticholinergics
Trihexyphenidyl ( Artane )
Benztropine ( Cogentin )
Biperiden ( Akineton )
Orphenadrine ( Disipal )
Procyclidine ( Kemadrin )
Treatment of PD
Diet & lifestyle
Levodopa is absorbed in the gut by an energy-dependent carrier protein that also transports large neutral aminoacids.
With high-protein meals, levodopa absorption could be delayed.
71
Protein-restricted diets may diminish motor fluctuations in some patients.
7-g protein redistribution diet, which is a low-protein diet (with protein given at the last meal or divided up into two meals).
5:1 carbohydrate-to protein diet → nutritionally adequate meals & improves fluctuations.
Carbohydrates enhance insulin secretion &
neutral amino acids without restricting proteins in the diet.
A protein restriction diet may be helpful in the treatment of fluctuations.
Vitamin B6 intake in patients with PD (it is a cofactor in the metabolism of levodopa by dopa decarboxylase). With the use of a dopa decarboxylase inhibitor (Carbidopa), this restriction is no longer necessary.
Drug Treatment
Dopamine agonists
They stimulate postsynaptic receptors in the striatum.
Bromocriptine (Parlodel), 2.5-mg & 5-mg tablets.
(1.25 mg/d é gradually up to 15 to 30 mg/d divided in three to five doses).
Pergolide (Permax), 0.05-mg, 0.25-mg, & 1.0-mg tablets.
(0.05 mg/d é gradually up to 3mg/d divided in three doses).
Pramipexole (Mirapex), 0.125-mg, 0.25-mg, 0.5-mg, 1.0-mg, & 1.5-mg tablets.
(0.125mg tid, é gradually up to 1.5 to 4.5 mg divided into three doses).
Ropinirole (Requip), 0.25-mg, 0.5-mhg, 1.0-mg, 2.0-mg, & 5.0-mg tablets.
(0.25mg tid, é gradually up to 8mg three times a day).
Cabergoline ( Dostinex, Cabaser )
(0.25 mg qd, ↑ up to 0.5 – 5 mg/d )
Lisuride ( Dopergin )
(0.2 mg qd, ↑ up to 1 – 2 mg/d)
Side effects:
Dyskinesia, hallucinations, confusion, orthostatic hypotension, nausea, & sleep disturbance.
Catechol-O-methyl transferase (COMT) inhibitors
Tolcapone (Tasmar), is a selective, reversible, primarily peripheral COMT inhibitor.
Initiate dose at 100mg tid for patients with dyskinesia, the levodopa dose should be ↓ by
20-30% to avoid or minimize worsening.
The dose can be increased to 200 mg tid if necessary.
Entacapone (Comtan), is a new COMT inhibitor significantly decreasing the off-time & lower Levodopa requirements.
One 200mg tablet is given with each dose of Levodopa.
Side effects:
Dyskinesia which can be treated with ↓ Levodopa dose.
Late side effects are diarrhea, nausea, orthostatic hypotension, confusion, hallucinations
& ↑ liver enzyme levels (diarrhea & liver enzyme changes are lesser with Entacapone).
Sinemet CR
This controlled-release form of levodopa increases its half-life
This drug is frequently used in combination with standard carbidopa/levodopa
Dosage: Available as 25/100 mg & 50/200 mg.
To convert from standard carbidopa/levodopa to Sinemet CR, evaluate the number of hours “on” per dose of the standard drug & multiply by two. For patients with dyskinesia, increase the total daily dose by 20%.
72
Side effects:
Dyskinesia (sometimes worse in the evenings), dystonia, nausea, orthostatic hypotension, confusion, hallucinations, & sleep disturbance.
Amantadine (Adamine)
This is an antiviral agent used in the treatment of the flu.
Dosage:
Initial therapy with 100 mg/d & increase by the same amount to a twice-or three-times-aday dose.
Side effects:
Primarily anticholinergic-type side effects, including dry mouth, nose, & throat; blurred vision; nausea; light-headedness; constipation; sleep disturbance; memory difficulties; confusion; psychosis; pedal edema; & a skin rash; livido reticularis.
Monoamine oxidase B inhibitors
Selegiline ( Jumex ) is the only drug in its class available for the treatment of PD.
Dosage:
Initiate dose at 2.5 to 5 mg/d. The maximal dose is 5 mg bid (breakfast & lunch).
Side effects:
Nausea, orthostatic hypotension, anxiety, palpitations, dyskinesia, insomnia, confusion,
& psychosis.
Anticholinergic agents
They are used in younger PD pts with tremors as a predominant symptom
They include:
Trihexyphenidyl ( Artane )
(0.5 – 1 mg bid, ↑ up to 2 mg tid)
Benztropine ( Cogentin )
(0.5 – 2 mg bid)
Biperiden ( Akineton )
(1 – 2 mg bid – tid)
Orphenadrine ( Disipal )
Procyclidine ( Kemadrin )
Side effects:
Central: memory impairment, confusion & hallucinations
Peripheral: dry mouth, blurred vision, constipation, nausea, urine retention, impaired sweating & tacchycardia.
Contraindications:
Glucoma
Prostatic hypertrophy
Surgical Treatment of PD
Ablative procedures:
Thalamotomy
Subthalamotomy
Stimulation procedures:
Thalamus (VIM nucleus)
GPi
Pallidotomy
STN
73
Restorative procedures:
Fetal human nigral transplantation
Trophic factors (e.g., GDNF)
Fetal porcine nigral transplantation
Relative merits of different surgical procedures for PD:
Procedure
Thalamotomy
Pallidotomy
DBS-thalamus
DBS-Gpi
DBS-STN
Fetal nigral transplantation
Tremor
+++
++
+++
++
+++
++
Rigidity/
Bradykinesia
+/-
++
+/-
+++
+++
++
Dyskinesia
+/-
+++
+/-
+++
+++
++/-
Adverse events*
3
3
2
2
2
1
+ = mild benefit; ++ = moderate benefit; +++ = marked benefit
* For bilateral procedures, 1 = minimal risk; 2 = more pronounced risk; 3 = great risk
Stereotactic pallidotomy
The primary target of this procedure is the posteroventral pallidum.
Unilateral procedures are recommended because bilateral procedures may be associated with an increase in complications, including speech & swallowing disorders, cognitive problems, & worsening gait.
The procedure involves the use of magnetic resonance imaging (MRI) or CT-guided stereotactic placement of a lesioning electrode & thermocoagulation of the target at 70o to 90o over seconds.
High-frequency techniques are applied to avoid lesion placement in the internal capsule
& optic radiation.
Indications of Stereotactic Pallidotomy
It should be saved for those patients with several dyskinesia & off periods uncontrolled by standard pharmacologic therapies, asymmetric or unilateral symptoms, or significant response to levodopa.
Contraindications
Dementia, lack of response to levodopa, atypical parkinsonism, freezing, postural instability, axial symptoms, & major medical problems making surgery an increased risk.
Complications
Cerebral hemorrhage, fatalities, hemiplegia, facial weakness, dysarthria & hypophonia, dysphagia & sialorrhea, & worsening gait. Mental complications include psychosis, confusion, personality change, & memory loss, visual field deficits & hemineglect.
Deep brain stimulation (DBS)
The primary target of this procedure is the ventral intermedius (VIM) nucleus of the thalamus.
This procedure has replaced thalamotomy because of several advantages: reversibility, adaptability, fewer adverse effects, less chance of recurrence of tremor, & less risk.
The procedure involves CT-or MRI-guided stereotactic localization of the VIM.
After a burr hole is placed, the lead is introduced through a guide tube, & electrical stimulation is used to determine the effect on tremor.
57
The patient is awake during the procedure so that tremor can be monitored.
Indications of DBS:
Severe disabling tremor refractory to pharmacologic therapies.
Complications of DBS:
Surgical : intracerebral hemorrhage, subdural hematoma, seizures, no suppression of tremor, nausea, & headache.
Stimulation: transient paresthesias, dysarthria, dysquilibrium, gait difficulty, & ataxic gait.
Glial cell line-derived neurotrophic factor (GDNF)
Intracerebral injection of glial cell line-derived neurotrophic factor (GDNF) in rodents
& nonhuman primates has led to an increase in midbrain levels of dopamine, protection of neurons from neurotoxins, maintenance of injured dopaminergic neurons, & improvement in parkinsonian motor signs & symptoms.
This has led to early clinical trials in humans of intracerebral GDNF injections.
Results are not yet available.
Neural transplantation
Immature (fetal) grafted nigral cells survive, innervate the striatum, & reverse motor abnormalities in rodents & nonhuman primates.
Positron emission tomography (PET) studies done on transplant recipients & autopsy results in isolated patients who died for reasons unrelated to PD demonstrated graft survival & striatal innervation as a result of implanted cells.
Emerging Therapies
Selegiline (Jumex)
New delivery systems for selegiline, including a skin patch & a sublingual form, are under investigations.
Contraindications & complications
Same as oral Selegiline
Rasagiline
A new MAO-B inhibitor
Dosage:
Up to 4mg/d
Apomorphine
A nonergot D2 dopamine agonist, given subcutaneously or intravenously.
It acts quickly, in 5 to 10 minutes, when given subcutaneously.
Its duration of action is about an hour.
Used to rescue patients from intractable “off” periods.
Dosage: The drug is available in solution, 20-mg/2 ml.
The injection is given at onset of the “off” period.
The mean dose for bolus therapy was 2.2 mg / injections/ day.
Side effects: Nausea, dyskinesia, hallucination, skin irritation, & the formation of skin nodules, which disappear over time.
Support in PD
(Patient & Family)
Assess emotional needs
75
Education
Peer support
Group support
Professional counselling
Legal/financial counselling
Occupational counseling (early disease)
Help in the home
Respite care
Exercise in PD
Education
Assess exercise capacity & limitations
Regular, focused exercise
Training
Physical therapy for exercise
Nutrition in PD
Assess risk factors:
Physical factors that interfere with proper nutrition
Psychological factors that interfere with proper nutrition
Interventions:
Home health evaluation & aids
Education
Nutritional counseling
76
Algorithm for Initiating
Treatment in Early PD
Age < 60 years
Prevent disease progression;
Use levodopa-sparing strategies
Supportive care
Age <50 years
Selegiline
(1)
(Jumex)
1. Jumex, Deprenyl.
2. Amantine, Adamine
3. Cogentin,
Akineton,
Parkinol
4. Parlodel, Mirapex, Requip,
Permax, Dostinex, Cabaser
5. Sinemet CR
Define treatment goals by patient age lmprove symptoms/function
Age 50-59 yrs
Amantadine
(2)
Or Anticholinergic
Selegiline inadequate response?
Add dopamine agonist inadequate response?
Add sustained release carbidopa/levodopa
Add amantadine, anticholinergic
6. Sinemet
7. Leponex
Decrease
DA dose
Switch dopamine agonist
Age > 60 years
Maintain cognitive status
(avoid selegiline, amantadine, and anticholinergics); improve symptoms/function
Dopamine
Agonist
(4)
Sustained-release
Carbidopa/levodopa
(5)
Inadequate response?
Switch to immediaterelease
Carbidopa/levodopa (6)
Inadequate response?
Add dopamine agonist
Disabling side effects?
Add clozapine (7)
77
78
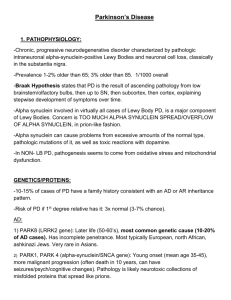
Levodopa metabolism:
3-MT = 3-methoxytyramine; 3-OMD = 3-O-methyldopa; COMT = catechol-Omethyltransferase; DDC = dopa decarboxylase; DOPAC = 3,4,-dihydroxyphenylacetic acid; HVA = 3-methoxy-4-hydroxyphenylacetic acid or homovanillic acid; MAO = monoamine oxidase. Peripherally administered levodopa is metabolized by both DDC and
COMT. DDC and COMT inhibition can be used in conjunction with levodopa to reduce peripheral metabolism and increase brain availability.
Adverse reactions related to dopaminergic agonists
Peripheral
Nausea
Vomiting
Peripheral & central
Orthostatic hypotension
Central
Motor fluctuation
Dyskinesias
Mental changes
79
No response in PD
Trial of increasing doses of levodopa/carbidopa ( Sinemet )
80
Exclude other causes of parkinsonism
Suboptimal peak response in PD
Begin dopaminergic combination therapy:
Add levodopa to dopamine agonist ( Parlodel, or Permax + Sinemet )
Add dopamine agonist to levodopa therapy
Increase dose of levodopa/carbidopa or dopamine agonist
Add COMT inhibitor as adjunct to levodopa ( Comtan + Sinemet )
Add selegiline ( Jumex + Sinemet )
Switch agonists
Surgery
“Wearing off” in PD
Begin dopamenergic combination therapy ( Sinemet + Parlodel/Premax )
Add levodopa to dopamine agonist
Add dopamine agonist to levodopa therapy
Increase frequency &/or dose of levodopa/carbidopa (sustained or immediate release)
( Sinemet CR/Sinemet )
COMT inhibitor ( Comtan )
Substitute or add sustained-release levodopa/carbidopa ( Sinemet CR )
+/- Liquid levodopa/carbidopa
Add selegiline ( Jumex )
S.C. Apomorphine
Surgery
Unpredictable “on” & “off” in PD
Begin dopaminergic combination therapy ( Sinemet + Parlodel/Premax )
Add levodopa to dopamine agonist
Add dopamine agonist to levodopa therapy
COMT inhibitor ( Comtan )
Modify distribution of dietary protein (to be ingested in the evening meal)
S.C. Apomorphine
Surgery
No “on” response in PD
Manipulate time & dose of dopaminergic therapy ( Sinemet )
Add COMT inhibitor ( Comtan )
Avoid dietary protein
Increase G1 transit time by cisapride ( Prepulsid )
81
Freezing (motor blocks) in PD
Choreiform dyskinesias in PD
82
Dystonia in PD
Constipation in PD
Dietary modification: increase fluid, fibre, & bulk
Increase physical activity
Stop anticholinergics (e.g. Cogentin, Akineton )
Stool softeners
Lactulose ( Duphalac )
Cisapride ( Prepulsid )
Enemas
S.C. Apomorphine
Urinary problems (nocturia) in PD
Reduce evening fluid intake
Oxybutynin ( Ditropan, Uripan )
Propanthetine ( Pro – Banthine )
Hyoscyamine
Consider urologic evaluation
Sexual problems (erectile dysfunction) in PD
Review medications
Medical evaluation
Treat depression
Consider urologic evaluation
Alprostadil suppositories ( Caverject = PGE
1
)
Orthostatic hypotension (symptomatic) in PD
Eliminate antihypertensive medications if possible
Behavior modification
Increase salt & fluid intake
Elevate head of bed
83
Fludrocortisone ( Astonin-H )
Midodrine ( Gutron )
Erythropoietin ( Eprex )
Impaired thermoregulation in PD
Increased sweating
Reduce motor fluctuations
blocker for peak-dose sweating e.g. propranolol (Inderal)
Medical evaluation
Pain in PD
Treat parkinsonism
Treat fluctuations/dyskinesia
Treat depression
Evaluate other medical problems
Seborrhoea in PD
Coal tar shampoos
Topical steroids
Blepharitis in PD
Natural tears
Warm compresses
Steroid cream
Eye patch at bedtime
Falls in PD
Postural instability: -review- motor problems
Freezing: -review-motor freezing
Levodopa – induced dyskinesia
Symptomatic orthostatic hypotension: -review- dysautonomias - orthostatic hypotension
Toppling falls: reconsider diagnosis
Associated neurologic deficits: -review- associated neurologic deficits
Medical causes: -review- medical causes
Environmental causes: -review- environmental causes
Associated neurologic deficits as a cause of falls
Evaluate & treat other neurologic deficits
Leg/hip weakness:
Evaluate
Strength exercise
Impaired vision:
Evaluate & treat
Cataract removal
Correct refraction
Vestibular dysfunction:
Evaluate
Consider drug-induced
Ataxia:
84
Evaluate
Consider drug-induced
Spasticity:
Evaluate
Consider antipsychotic – induced
Inattention; confusion:
Evaluate
Consider drug-induced
Dementia:
Evaluate
Behavior modification
Medical causes of falls
Medically evaluate all previously stable patients
Acute illness or worsening of chronic illness: (evaluate & treat)
Arthritis: (symptomatic therapy)
Foot problems: (podiatrist referral)
Poor cardiovascular fitness: (exercise)
Cardiac syncope: (Holter monitoring + cardiology referral)
Parkinsonism or dyskinesia unsatisfactorily controlled by medical therapy
Consider pallidotomy
Consider DBS (Deep Brain Stimulation)/ STN (Subthalamic Nucleus Stimulation)
Consider transplant ( fetal nigral transplantation )
Cognitive impairment in PD
Treat medical problems
Discontinue:
Non-PD medications (e.g. sedatives & anxiolytics )
Anticholinergics (e.g. Cogentin, Akineton, Parkinol )
Tricyclic antidepressants (e.g. Tryptizol, Tofranil, Anafranil )
Amantadine ( Amantine, Adamine )
Selegiline ( Jumex )
Dopamine agonists ( Parlodel )
Reduce:
Levodopa/carbidopa ( Sinemet )
Hallucinations/delirium in PD
Medications-induced
Discontinue:
Anticholinergics (e.g. Akineton, Cogentin )
Amantadine ( Adamine )
Selegiline ( Jumex )
Dopamine agonists ( Parlodel, Permax )
Reduce levodopa/carbidopa ( Sinemet )
Begin low-dose clozapine ( Leponex )
Other medical conditions
Treat
Trial of clozapine ( Leponex )
85
Behavioral impairment in PD
Managing depression in PD:
Is depression exogenous or endogenous?
Exogenous → Councelling → if not effective → manage as endogenous
Endogenous → Apathetic or Agitated?
Apathetic → SSRIs
→consider ECT
→ if motor symptoms worsened → try TCAs → if not effective
Agitated → prefer TCAs with short plasma half life & little anticholinergic activity
→ if not effective → consider ECT
Managing anxiety & panic attacks in PD:
Are anxiety and panic attacks related to “off” state?
If yes → adjust antiparkinsonian medication → if not effective → try short – acting
Benzodiazepines, Clonazepam or Busparone → if not effective → try TCAs
If no → counselling → if not effective → try short – acting Benzodiazepines,
Clonazepam or Busparone →
If not effective → try TCAs → if not effective → suspect agitated depression
If effective → continue treatment for 3 months, then cautious withdrawal
86
Delirium in PD
Is delirium drug – induced?
If yes → Decrease antiparkinsonian drugs in order of drug’s potential to induce delirium vs its antiparkinsonian efficacy →Decrease or eliminate drugs in the following order:
Anticholinergics; Amantadine; Selegiline; Dopamine agonists; Carbidopa-levodopa
If no → assess if delirium is related to electrolyte imbalance, dehydration, infection:
If yes → treat abnormality
If no → assess if delirium is mild or moderate: o
If mild → treat sleep disturbances with short – acting TCAs with little anticholinergic activity or trazodone →if not effective → treat with atypical neuroleptics e.g. clozapine o
If moderate to marked → treat with atypical neuroleptics e.g. clozapine
Insomnia in PD
Idiopathic: o
Evaluate sleep disorder o Sleep hygiene program o Treat with sedative-hypnotics (e.g. chloral hydrate )
Nocturnal parkinsonian symptoms: o
Add sustained-release carbidopa-levodopa ( Sinemet CR ) or long acting dopamine agonist ( Parlodel )
Dementia
Medication-induced: o
Reduce or stop selegiline ( Jumex ) o Reduce carbidopa-levodopa or dopamine agonist
Depression: o Small doses of TCAs
Medications used in short-term treatment of insomnia
(dose given at bedtime)
Drug
Diphenhydramine ( Amydramine )
Chloral hydrate ( Chloral )
Tricyclic antidepressants ( e.g. Tryptizol )
Dose
25- 75 mg
250-750 mg
10-100 mg
Trazodone ( Trittico )
Temazepam ( Normison )
Diazepam ( Valium )
Clonazepam ( Rivotril )
Zolpidem ( Stilnox )
50-200 mg
15-30 mg
1-5 mg
0.5-1mg
5-10 mg
Excess daytime sleepiness in PD
Depression: -review- neuropsychiatric problems & behavioral impairment
Medications-induced:
Decreased antiparkinsonian medications
Decrease sedating drugs
Dementia
Idiopathic:
Evaluate for primary sleep disorders
Correct night time insomnia
87
Add selegiline ( Jumex )
Add caffeine
Add methylphenedate ( Ritalin )
Nightmares in PD
Medication – induced:
Reduce or discontinue nighttime dose of anti-PD drugs
Reduce or eliminate hypnotics, tricyclic antidepressants ( TCAs )
Dementia
Idiopathic: primary sleep disorder
Restless leg syndrome in PD
Medication-related: [differentiate from akathisia]
Medication–induced: [increase carbidopa-levodopa ( Sinemet ) at nighttime]
Idiopathic:
Evaluate primary disorder
Dopamine agonist ( Parlodel/Permax )
Levodopa/carbidopa ( Sinemet )
Clonazepam ( Rivotril )
Propoxyphene ( Darvon ) or codeine ( Codipront, Codinal )
Causes of excessive daytime sleepiness associated with Parkinson’s disease
1.
Drug-induced: Levodopa, selegiline, anxiolytic, & antidepressant-induced insomnia
2.
Primary sleep disorder: Insomnia, obstructive sleep apnea, restless leg syndrome, periodic limb movements during sleep, REM behavior disorder
3.
Endocrine Dysfunction: Hypothyroidism
4.
Circadian cycle disruption: Dementia, Parkinson’s disease, lack of
Zeitgebers
Motor fluctuations & dyskinesia in Parkinson's disease
Motor fluctuations
Wearing-off effect: Antiparkinsonian effect of levodopa wears off toward the end of the dose in a predictable fashion.
Complicated wearing off: Duration of response of levodopa becomes variable so that the timing of wearing off becomes less predictable.
No-on: A dose of levodopa has no effect.
Delayed-on: A delay in onset of levodopa.
On-off: Response to levodopa varies in an unpredictable manner unrelated to timing of the dose.
88
Dyskinesia
Peak dose dyskinesia: Choreic movements occurring when plasma levodopa levels peak.
Diphasic dyskinesia: Choreic or dystonic movements occurring at the beginning & end of levodopa dose.
Square-wave dyskinesia: Occurring at onset & persisting throughout the beneficial effect.
Early-morning dystonia: Painful dystonic foot posturing on awakening.
Off-period dystonia: Painful foot dystonia occurring as levodopa wears off.
Yo-yoing: Fluctuating abruptly from severe immobility to severe dyskinesia.
Pathogenesis of Levodopa – induced dyskinesias:
Denervation supersensitivity of dopamine receptors is the most plausible mechanism of levodopa – induced dyskinesias
Continuous destruction & denervation of the nigrostriatal pathways in PD pave the way to the appearance of dyskinesias
Levodopa induces changes in the striatum or in the outflow pathways of the basal ganglia motor circuits of pts with PD
It ↑ the activity of adenylcyclase ,
↓ the messenger RNA for proencephalin in the striatum &
↓ the glutamic acid decarboxylase messenger RNA in the internal globus pallidus of animal models of nigrostriatal dopaminergic denervation
These changes may lead to biochemical imbalance which could be involved in the pathogenesis of dyskinesias
Early combination of dopamine agonists with levodopa appears to ↓ the incidence of dyskinesias
Pathophysiology of Levodopa – induced dyskinesias:
Dopamine receptor supersensitivity
Imbalance in striatal outflow pathways resulting from altered dopamine D1 &/or D2 receptor – mediated mechanisms
Pulsatile versus continuous dopamine receptor stimulation by high dose levodopa
Bromocriptin , an agonist of D2 receptor , is less likely to elicit or induce dyskinesias in
PD
It is thus hypothesized that stimulation of the D1 dopamine receptor is responsible for dyskinesias & that a selective D2 agonist would solve the problem
Continuous release levodopa & long acting DA are less likely to induce dyskinesias
High – dose & long – term use of levodopa induce dyskinesia as follows:
The high dose is irrigating the supersensitive receptors directly with high concentrations
→ dyskinesias
The high dose rapidly reaches receptors with no collecting vesicles to collect extra – drug → intermittent or pulsatile stimulation → exaggerated response in the form of dyskinesia
High – dose levodopa ↑ receptor damage by:
Oxidative stress injury to the receptors &
Decreasing the inhibition in the thalamocortical pathway through overdosing GPi
& STN pathway
89
Parkinson’s Disease: Motor Fluctuations
Motor fluctuations represent important late complications of Parkinson's disease treated with Levodopa.
Polytherapy is often the rule in this case with a variety of agents available as adjunctive therapy with Levodopa .
These adjuncts include dopamine agonists (bromocriptine, pergolide, pramipexole, ropinirole), catechol-0-methyl-transferase (COMT) inhibitors (tolcapone), controlledrelease formulations of Levodopa , monoamine oxidase (MAO) B inhibitors (selegiline),
& Amantadine .
For simple wearing off , controlled-release levodopa ( Sinement CR ), COMT inhibitors ,
MAO inhibitors , & dopamine agonists are reasonable options.
For complicated fluctuations, dopamine agonists with limits on levodopa are the first choice, especially when dyskinesia is present.
When dyskinesia is not a factor, COMT inhibitors may be used for dyskinesia specifically, dopamine agonists or addition of amantadine can be helpful.
Surgery should be a treatment of last resort for patients in whom medical therapy fails.
Patients who are candidates for medial pallidotomy should be fluctuators with severe dyskinesia & “off” periods that have not improved with pharmacologic therapy.
Thalamic deep brain stimulation (DBS) should be used only in patients with tremorpredominant disease & severe intractable tremor that is unresponsive to medication & occurs not only at rest but with posture & action as well.
Surgical therapy should be performed only in centers with surgeons experienced in stereotactic techniques & movement disorder specialists to ensure that the appropriate patients come to surgery & that complications are kept to a minimum.
Dietary adjustment has a limited role in treating advanced Parkinson's disease.
90
SYDENHAM'S CHOREA
(Rheumatic Chorea)
Affects children & adolescents, between 5-15 yrs
A complication of a previous group A hemolytic streptococcal infection
The underlying pathology is probably arteritis
It occurs 2-3 months after an episode of rheumatic fever or polyarthritis in 30% of cases
Onset is acute or insidious
It subsides within few weeks to few months (4-6 months)
It may recur during pregnancy (Chorea Gravidarum), or in ladies taking oral contraceptives
Clinically:
Choreiform movements are irregular brief, jerky, shock-like involuntary movements affecting the face, tongue, extremities & trunk & sometimes unilateral, increased by anxiety & stress, disappear during sleep. They are associated with hypotonia
(Choreic boat-shaped hands) +/- behavioral changes e.g. irritability +/- evidence of cardiac involvement (in 30% of cases). However, the ESR & ASOT are usually normal.
Clinical types:
Hemichorea (Unilateral chorea)
Chorea gravis (severe chorea)
Chorea mollis (Hemiplegic chorea due to severe hypotonia)
Chorea gravidarum (occurring during pregnancy)
Maniacal chorea (associated with severe behavioral abnormalities)
Treatment:
Bed rest
Sedation
Prophylactic antibiotic therapy:
A course of IM Penicillin
Continuous prophylactic oral penicillin daily until about age 20 yrs to prevent streptococcal infection
Halloperidol (Haldol, Safinace), 1.5 mg tid
Reserpine (Serpasil), 0.25 mg qid,
Chlorpromazine (Neurazine), 25 mg tid
Prognosis: is that of the cardiac involvement
91
HUNTINGTON’S DISEASE
Establishing the Diagnosis:
An autosomal dominant, dementing disease, ê relative overactivity of the dopaminergic system
Hypotonia is frequent
Chorea & athetosis may coexist
Childhood onset of Huntington’s chorea may be associated ê parkinsonism
Dysarthria is frequent
Progressive emotional & personality changes & dementia
Depression is common, ê suicide in 5% of cases
D.D. of Huntington’s Disease:
Mercury poisoning
Sydenham’s chorea of acute rheumatic fever & other acute infections (diphtheria, pertussis, rubella, & encephalitis)
Oral contraceptives, & rarely, pregnancy
Thyrotoxicosis
Post-hemiplegic athetosis
Lesch-Nyhan syndrome in childhood
Kernicterus
Senile chorea
Drugs e.g. anticonvulsants, lithium, & antiemetics
Diseases presenting as parkinsonism or choreoathetasis.
Treatment of Huntington’s Disease:
Drug Treatment of Movement Disorders in Huntington’s Disease:
I.
Chorea
Responds to antidopaminergic agents, particularly conventional antipsychotics or typical neuroleptics
They may cause: - Extrapyramidal side effects
- Tardive dyskinesia
Atypical neuroleptics are better tolerated
Drug Treatment
Typical Neuroleptics
Atypical Neuroleptics
Dopamine depletion or receptor blockade is helpful:
Haloperidol (
Chlorpromazine (
Tetrabenazine (
Resepine (
Haldol, Safinace, Serenase
Largactil
Nitoman
Serpasil
)
), 50mg tid
), 1-4mg qid
), 0.5mg qid (in Sydenham’s chorea)
Propranolol ( Inderal
Dantrolene sodium (
), in high dosage, is useful for action tremor
Dantrium ), for chorea + hemiatrophy
92
Typical Neuroleptics:
Drug Receptor affinity Cytochrome
P450
Daily dose range
Haloperidol
( Safinace )
Fluphenazine
High
D2
Low
5.HT2A
H
1
1 ACh
D2
1
5- HT2A
H system
2D6
High
0.5-1
1
2D6 0.5-1
Low
10-15
10
( Modecate )
Thioridazine
( Melleril )
Pimozide
Ach
2
D2
H1
5- HT2A
D2
Ach,
1
2D6 10.25
3A4 1-2
200
10
( Orap )
1-
2 adrenergic receptors; ACh-muscarinic cholinergic receptors; D
2
-D
2 dopamine receptor; H
1
-H
1
histamine receptor; 5-HT2A-2A serotonin receptor.
Atypical Neuroleptics:
Risperidone
(Risperdal)
Receptor affinity Cytochrome p
450
High Low
System
H1
ACH 2D6 5.HT2A
1
D2
Daily dose range
Low
0.5-1
High
6
Clozapine
(Leponex)
5-
HT2A
H1
AC h
1
D2 2D6, 1A2, 3A,
2E1
25-50 150
Olanzapine
(Zyprexa)
ACh
5-
HT2A
H1
D2
1
1A2, 2D6 5 20
Quetiapine H1
1
D2
52D6 25-50 750
(Seroquel) HT2A
1-
1 adrenergic receptors; ACh-muscarinic cholinergic receptors; D
2
-D
2 dopamine receptor; H
1
-H
1
histamine receptor; 5-HT2A-2A serotonin receptor.
II.
Dystonia
Drug Treatment
Trihexyphenidyl ( Artane ), 1-2 mg bid ↑ up to 12-15 mg /d on tid schedule
Baclofen ( Lioresal ), 5 mg bid ↑ up to 60-80 mg /d on tid or qid schedule
Clonazepam ( Rivotril ), 0.25 mg bid ↑ up to 6 mg /d
Botulinum Toxin ( Botox A )
Blepharospasm: 30-50 U
Torticollis: 200 U or more
III.
Myoclonus
( Brief shock-like jerks )
Valproate ( Depakine ), 250 mg tid ↑ gradually to achieve a serum level of 50-100 ug /ml
93
Clonazepam ( Rivotril ), 0.25 mg bid ↑ up to 6 mg /d
IV.
Tics
( Repetitive stereotyped motor or vocal behaviors )
Haloperidol ( Safinace ), 0.5-1 mg /d ↑ up to 10-15 mg /d.
Pimozide ( Orap Forte ), 1-2 mg /d ↑ up to 10 mg /d.
V.
Rigidity & Spasticity
Tizanidine (Sirdalud ), 2 mg at bedtime ↑ every wk to maximum of 12-24 mg /d.
Diazepam ( Valium ), 2 mg tid ↑ up to 10 mg tid-qid
Baclofen ( Lioresal ), 5 mg bid ↑ up to 60-80 mg /d. on tid or qid schedule
VI.
Hypokinesia, Parkinsonism
Levodopa / Carbidopa ( Sinemet ), 100 mg / 25 mg tid
VII.
Seizures
AEDs
Drug Treatment of Psychiatric Symptoms in Huntington’s Disease:
Mood Disorders
Selective Serotonin Reuptake Inhibitors ( SSRIs ): (see the table)
Bupropion ( Wellbutrin ), 75 mg orally / morning to 100 mg / morning , then to 100 mg bid-tid
Venlafaxine ( Effexor ), 37.5 mg / morning with food ↑ to 75 mg / morning up to 225 mg
SR
Nefazodone ( Serzone ), 300 mg /d in divided doses
Mirtazapine ( Remeron ), 15-45 mg at bedtime
Methylphenidate ( Ritalin ), 5 mg / morning ↑ to 5 mg / morning & / noon, then ↑ by 5 mg/3-4 days until response is achieved
Selective serotonin reuptake inhibitors (SSRIs)
Drug Steady state, wk
Cytochrome P450 system
Daily dose range, mg
Low High
4-6
Fluoxetine
( Prozac )
Sertraline
( Lustral )
Paroxetine
( Seroxat )
Citalopram
( Cipram )
Fluvoxamine
( Faverin )
3
3
3
2
2D6
Insignificant
2D6
2C19, 3A4
2C19, 1A2, 3A4
5-20
25-50
10-20
20-40
50-100
60-80
250
40-50
40-60
250-300
94
Anxiety Disorders
Buspirone ( Buspar ), 5 mg / morning ↑ up to 10-60 mg /d
Hydroxyzine ( Atarax ), 25 mg 0.d. – qid
Alprazolam ( Xanax )
Bromazepate ( Lexotanil,Calmepam )
Clorazepate ( Tranxene )
Aggression, Irritability, & Dyscontrol
Propranolol ( Inderal ), < 200 mg /d.
Lithium ( Priadel ), 300-1200 mg /d.
Apathy
Methylphenidate ( Ritalin ), 5 mg / morning ↑ to 5 mg / morning & noon, then ↑ by 5 mg
/ 3-4 days until response is achieved
Psychosis
Risperidone ( Risperdal )
Haloperidol ( Safinace)
Olanzapine ( Zyprexa )
Quetiapine ( Seroquel )
Insomnia
Mirtazapine ( Remeron ), 15-45 mg at bedtime
Trazodone ( Trittico ), 100-600 mg at bedtime
Sexual Disorders
Hypoactive sexual desire
Inhibited orgasm
Paraphilic disorders
Inappropriately heightened sexual activity
Medroxyprogesterone acetate
Leuprolide (
SSRIs
Gonadotropin-RH agonist )
ECT in HD:
It is effective in depression & abnormal movements
It is generally safe
Assistive Devices in HD:
Wheelchairs
Specialized walkers
Adaptive seating & positioning devices
Bed enclosures & padding
Tub seats
Shower rails
Ankle & wrist weights
Weighted utensils
Lidded cups
95
Physical / Speech Therapy & Exercises
Physical & occupational therapies to keep safety & independence
Using assistive devices for performance of A.D.L.
Speech therapy
Genetic Counseling in HD
DNA testing a) Diagnostic b) Predictive testing of asymptomatic individuals
Psychotherapy in HD
Psychotherapy or supportive or insight-oriented therapy is helpful as an adjunct to drug therapy
Emerging Therapies for HD
Pharmacologic Approaches:
Riluzole ( Rilutek )
N-methyl-D-aspartate ( NMDA ) receptor antagonist
Reduce chorea in HD
Remacemide
NMDA glutamate receptor antagonist
Coenzyme Q
10
↑ Mitochondrial energy production
Acts as an antioxidant
Surgical Approaches:
Striatal transplantation
96
Drugs Commonly Used for Movement Disorders
Drug Availability
Amantadine hydrochloride
( Adamine )
Baclofen ( Lioresal )
Benztropine mesylate ( Cogentin )
Biperiden ( Akineton )
Botulinum toxin (type A) ( Botox )
Bromocriptine mesrlate
( Parlodel )
Chlorpromazine ( Neurazine )
Clonazepam ( Rivotril )
Clonidine ( Catapres )
Dantrolene sodium ( Dantrium )
Deanol acetamidobenzoate
( Deaner )
Diazepam ( Valium )
L- Dopa with bensserazide
( Madopar )
L- Dopa with carbidopa ( Sinemet )
Ethopropazine ( Parsidol )
Haloperidol ( Haldol, Safinace )
Nadolol ( Corgard )
Metoprolol ( Lopressor )
D –Penicillamine ( Artamine )
Pergolide mesylate ( Permax )
Propranolol hydrochloride
( Inderal )
Reserpine ( Serpasil )
Selegiline ( Jumex )
Tetrabenazine ( Nitoman )
Trihexyphenidyl hydrochloride
( Artane )
100-mg capsules
10-mg tablets
0.5-, 1 -, & 2 mg tablets; injectable, 1 mg/ml
2-mg tablets; injectable, 5 mg/ml
100-unit vials
2.5-mg tablets
10-, 25-, & 50-mg tablets
0.5-, 2 mg tablets
0.1-, 0.2-, & 0.3-mg tablets
25-, 50-, & 100-mgcapsules; injectable, 2 mg/vial
25-, 100-, & 250-mg tablets
2-, 5-, & 10-mg tablets; injectable,5 mg/ml
100/25 mg capsules;
200/50 mg capsules
250/25 mg tablets;
Sinemet CR 200/50
10 , 50, & 100 mg tablets
0.5, 1.5, 5 & 10 mg tablets;
injectable, 5 mg/ml
40 , 80 & 120 mg tablets
50 & 100 mg tablets
250 mg capsules
0.25, 0.5,1 mg tablets
10, 40 & 80-mg tablets;
Injectable 1mg/ml
0.1, 0.25 mg tablets;
5-mg tablets
25-mg tablets
2.0 & 5.0 mg tablets;
5-mg sustained –release caps
Frequency of administration bid tid bid tid prn tid tid tid bid bid – qid tid bid – qid tid tid tid or qid tid or qid qid bid qid bid or tid tid or qid qid bid tid tid bid
97
DISEASES PRESENTING WITH
PARKINSONISM & CHOREOATHETOSIS
Wilson’s Disease
An autosomal recessive disorder
Onset between 10 & 40 yrs
Clinically:
1.
Liver cirrhosis → asterixis ê progressive hepatic dysfunction
2.
Neurologic disease:
Children: athetosis or rigidity & dystonia ± myoclonus
Adults: action & intention tremor, dysarthria, & dysphagia
3.
Kayser – Fleischer rings of the cornea ± Renal dysfunction
Diagnosis of Wilson’s disease:
Observing the Kayser-Fleischer ring by slit-lamp examination
Impaired L.F.Ts.
Serum copper & ceruloplasmin levels
Urinary excretion of copper
Liver biopsy reveals cirrhosis &
liver Cu concentration.
CT scan lucencies in the basal ganglia
Treatment of Wilson’s disease:
1.
A low copper diet (< 1.5 mg/day). Avoid shellfish, liver, mushroom, nuts & chocolate
2.
D-Penicillamine ( Artamin ), 250mg tid between meals, continued for life,
dosage during pregnancy. Total drug withdrawal may be fatal.
3.
Zinc sulfate or acetate containing 25 mg of elemental Zn, q4hr between meals & before bed, is useful & harmless. It
copper absorption.
4.
Trietheneteramine dihdrochloride ( Trientine ), 400-800 mg tid before meals, in pts intolerant to penicillamine
5.
Ammonium tetrathiomolybdate is a promising new drug
6.
Treatment of metabolic acidosis in pts ê renal tubular acidosis
7.
Liver transplantation in pts ê liver failure
8.
Symptomatic treatment of the movement disorder
Anticopper Agents for treatment of Wilson's disease:
Drug
Zinc acetate
Trientine
Trade name
Galzin
Syprine
D-penicillamine Cuprimine,
Artamin
Ammonium
Tetrathiomolybdate
None
Advantages Disadvantages
Effective, nontoxic
Effective, moderately fast-acting
Effective, fastacting
-
-
Slow-acting
Moderately toxic Not well studied
Effective, very fast-acting,
Little toxicity
Long list of acute, subacute & chronic toxicities
High frequency of making neurologic presenta-tion worse
Not commercially available
Not studied for maintenance use
98
Zinc ( Gelzin )
50 mg tid ( 1 hr before or after meals
25 mg bid for children < 6 yrs
) for adults
25 mg tid for children 6-16 yrs
Trientine ( Syprine )
250 mg qid 30 min before or 2hrs after meals
Tetrathiomolybdate
20 mg 6 times daily
Penicillamine ( Cuprimine, Artamin )
250 mg qid 30 min before or 2 hrs after meals
Anticopper drugs of choice:
Patient status
Clinical
Presentation
Hepatic
Drugs of choice
Zinc & trientine for4 months, then zinc alone
Initial presentation
Neurologic
Tetrathiomolybdate (with or without zinc) for 8 weeks then zinc alone
If tetrathiomolybdate is unavailable, the second choice is zinc alone
Maintenance phase All Zinc, Second choice is trientine
Presymptomatic
Pregnant
None
All
Zinc
Zinc
Pediatric All Zinc
Therapy for Neurologic Symptoms:
Tremor
Parkinsonism
Limited range of motion
Dystonia
Chorea
All are treated as usual
Therapy for Complications of Hepatic Failure:
Hepatic encephalopathy
Low-protein diet
Lactulose ( Duphalac )
Neomycin
Ascites & Peripheral edema
Salt restriction
Aldactone
Electrolyte management
99
Therapy for Psychiatric Symptoms:
They may precede neurologic symptoms
Difficulty focusing on tasks
Depression
Extremes of emotionality
Bizarre behaviors
Delusions or hallucinations
They respond to anticopper therapy within 1 or 2 yrs
Symptomatic treatment is not different from that of psychiatric problems
Gastrostomy in:
Dysphagia
Bleeding esophageal varices
Surgical Treatment
To reduce the risk of variceal bleeding
Corrective surgery (e.g. tendon lengthening)
Hepatic transplantation for pts with liver failure
Assistive Devices
For dysarthria:
Magnetic boards with letters of the alphabet
Keyboards that will print out the pt‘s messages
For Ambulation: walkers
Physical / Speech Therapy & Exercise
Speech therapy for dysarthria
Physical therapy for maximizing the use of limbs
Occupational therapy
Presymptomatic Patients
Anticopper drug prophylactically e.g. Zinc ( Gelzin )
Pregnant Patients
Continue anticopper therapy during pregnancy e.g. Zinc ( not penicillamine )
Pediatric Patients
Zinc ( Gelzin ), 25 mg bid if < 6 yrs , 25 mg tid if 6-16 yrs
100
Calcification of the Basal Ganglia
& Dentate Nucleus
May occur in the elderly → parkinsonism or choreoathetosis
Causes:
1.
Postsurgical & idiopathic hypoparathyroidism, & pseudo- hypoparathyroidism →
Ca &
phosphorus ( Treated by: Vit. D 50-100.000 unit/day + Ca)
2.
Fahr’s disease (striatopallidodentate pseudo – calcification): Blood chemistries are normal. No treatment is available
3.
Hyperthyroidism rarely cause calcification
4.
Pseudohypoparathyroidism (normocalcemic pseudo-hypoparathyroidism)
Differential Diagnosis of Basal Ganglia Calcification
Disease
Frequency of
Basal ganglia calcification
Hypoparathyroidism
Pseudohypoparathyroidism
Pseudopseudohypoparathyroidism
Uncommon
Half of cases
Rare
Hyperparathyroidism
Fahr disease
Very rare
Always
(required for diagnosis)
PTH, parathyroid hormone
AMP, adenosine monophosphate
Ca
Chemical Data
P PTH
↑
N
N
↓
↓
↓
N or →
↑
N
N
N
↓ or
N
N
↑
↑
Urine cyclic
AMP to
PTH infusion
↑
0
↑
General
Postsurgical effects take
15 yr
Characteristic facies, extremities
& stature
Characteristic facies, extremities
& stature
Chemistries vary with renal impairment
101
HEMIBALLISMUS
Flinging rotatory movements due to hemorrhagic lesions of subthalamus
Treatment:
1.
Initial therapy for acute disability: Reserpine ( Serpasil ) or Tetrabenazine ( Nitoman ) then:
2.
Phenothiazine or Haloperidol ( Safinace )
3.
Ventrolateral thalamotomy for chronic severe cases
IDIOPATHIC DYSKINESIAS & DYSTONIA
Types:
Generalized e.g. dystonia musculorum deformans
Segmental e.g. torticollis, retrocollis, writer’s cramp, blepharospasm, & Meige’s facial dystonia
Treatment:
High – dose ethopazine ( Parsidol ) followed by: diazepam ( Valium ), haloperidol
( Haldol, Safinace ), tetrabenazine ( Nitoman ) & lithium ( Priadel )
Botulinum toxin type A ( Botox ) in segmental dystonia
Closely applied splints
Spinal cord stimulation
DYSTONIA MUSCULORUM DEFORMANS
Hereditary, progressive, more in Jewish
Treatment:
L-dopa
Ventrolateral thalamotomy
Orthoses
SPASMODIC TORTICOLLIS
An idiopathic segmental dystonia, sporadic
Treatment:
1.
Botox A
2.
Sensory & positional feedback therapy
3.
Sectioning the spinal accessory fibres & intradural section of C1 – C3 anterior nerve roots → remission in 1/3 of cases
PAROXYSMAL CHOREOATHETOSIS & DYSTONIA
Familial, sporadic, or acquired
Treatment:
1.
Kinesogenic form of choreathetosis:
Responds to carbamazepine ( Tegretol ) & phenytoin ( Epanutin )
2.
Paroxysmal nonkinesogenic dystonia:
Responds to clonazepam ( Rivotril )
102
Clinical
Rest
Sustained position
Intention
Tremor during sleep
EMG
TICS
Tics are quick, coordinated repetitive movements, in contrast to the irregular & quasi– purposeful jerky movements of chorea .
Tics may be simple or multiple; acute, subacute or chronic
Gilles de la Tourette’s syndrome:
A multiple chronic tic syndrome, occurs between 2 & 13 yrs, more in males.
Clinicaly:
Involuntary grunts, whistles, & cough ± echolalia
Coprolalia (uncontrolled use of offensive language) occurs in 50 %
Other neuropsychiatric disorders e.g. attention deficit hyperactivity disorder ( ADHD )
& obsessive compulsive disorder ( OCD )
Treatment:
Haloperidol ( Haldol, Safinace ), 0.5 mg tid,
up to 8-16 mg qid
Pimozide ( Orap ), 1-2 mg daily,
to 7-16 mg daily
Clonidine ( Catapres ), 0.1 mg/day,
up to 2 mg /day
Tetrabenazine ( Nitoman ), useful in young pts.
Ca channel blockers: nifedipine ( Adalat, Epilat ), flunarizine ( Sibelium ), & verapamil
( Isoptin )
Botulinum toxin A ( Botox )
ADHD may respond to desipramine ( Norpramine ) & clonidine ( Leponex )
OCD may respond to fluoxetine ( Prozac ) & clomipramine ( Anafranil )
TREMOR
Involuntary, regular, & repetitive shaking of a body part around a fixed point
Characteristics of Major Tremor Syndromes:
Parkinsonism
++ pill rolling
+
0
+
Alternating agonist & antagonist contractions 3-7 cps essential tremor also seen
Essential Cerebellar Rubral Asterixis Physiological
0 + + + 0
+
0
++ -
++
+
++
Sway
++
+
++
Irregular
+
+
+
0
0
Agonist &
antagonist contractions
Agonist & antagonist contractions, asynchronous
&overlaping
Mixed pattern
Loss of activity
Alternating agonist & antagonist contractions 8-12 cps
103
Classification:
Action Tremors:
7-12 cps, of low amplitude, may be asymmetric
They include:
Physiologic tremor: - induced by movements requiring extremes of precision or power
by fatigue, anxiety, weakness, hypercapnia, drug withdrawal, hypoglycemia, uremia, cholemia, thyrotoxicosis, heavy metal intoxication, drugs e.g. catecholamines, amphetamine, theophylline, caffeine, lithium, tricyclic antidepressants, antipsychotics, sodium valproate
Familial tremor
Senile tremor in the elderly
Essential tremor if no demonstrable cause
Treatment
1.
Tranquilizers: in anxiety tremors
Diazepam ( Valium ), 6-15 mg daily in divided doses
2.
A single dose of alcohol reduces action tremor for 3-4 hrs!
3.
Beta-adrenergic blockers:
Propranolol ( Inderal ), 40-240 mg daily in divided doses
Metoprolol ( Lopressor , 50 mg bid, ↑ to 100 mg bid (for asthmatics)
Nadolol ( Corgard ), 40-80 mg single daily dose
4.
Primidone ( Mysoline ), 25-500 mg PO in divided doses
5.
Glutethimide, 250-1000 mg daily
6.
Botulinum toxin A ( Botox ) in essential rubral & cerebellar intention tremor of the limbs, but not head tremors:
Orthostatic Tremor:
Unsteadiness while standing but steadiness while walking.
Treated by: clonazepam ( Rivotril ), 0.5-1 mg/day
Asterixis:
The rate of limb flexion & extension is irregular & slow
It arises from temporary loss of tone in the outstretched limb
Occurs in metabolic disorders (renal, pulmonary, hepatic), in Wilson’s disease, & with some drugs e.g. metoclopramide ( Plasil ) & anticonvulsants
Treatment is that of the cause
MYOCLONUS
Rapid, irregular, jerking, shock-like contractions
Treatment:
Treatable causes: toxoplasmosis, neuroblastoma, thalium poisoning, uremia, hepatic encephalopathy, drug intoxications (imipramine, penicillin, L-dopa,
MAOIs, piperazines), & nocturnal myoclonus.
Drugs:
1.
Clonazepam ( Rivotril ), 1.5 mg daily, ↑ over 4 wks up to 7-12 mg daily
2.
Valproic acid ( Depakine ), up to 1600 mg/day is useful in posthypoxic type
3.
Piracetam ( Nootropil ), 18-24 g/day
4.
5-Hydroxytryptophan ( 5-HTP ), 150-1600 mg PO daily divided into 2-4 doses± carbidopa
5.
Tetrabenazine ( Nitoman ) is useful in spinal myoclonus
104
RESTLESS LEGS SYNDROME
Unusual sensations in the muscles & bones of legs, occur at rest, mostly at night, & disappear on movement
It may be seen in pts with chronic renal failure
Also seen in association with periodic movements during sleep → insomnia
Treatment:
1.
Anticonvulsants:
Clonazepam ( Rivotril ), 0.5mg tid
Carbamaazepine ( Tegretol ), 200mg tid
2.
Dopaminergic agents:
L-dopa ( Sinemet ), 10/100mg tid
Bromocriptine ( Parlodel ), 2.5mg tid
3.
Clonidine ( Catapres ), 0.1mg tid
4.
Opioids
Cerebellar Neurotransmitters:
CEREBELLAR ATAXIA
Afferent pathways to cerebellar cortex & deep cerebellar nuclei
Mossy fibers from the pons - ( glutamate, acetylcholine , various neuropeptides)
Climbing fibers from the inferior olives - ( aspartate , corticotropin releasing factor)
(Noradrenergic) fibers from the locus ceruleus
(Serotinergic) fibers from the raphe nuclei
(Histaminergic) fibers from the upper brain stem & hypothalamus
Cerebellar cortical neurons
Purkinje’s cells, basket cells, stellate cells , Lugaro cells, Golgi cells (GABA) (both
GABA-A/ benzodiazepine & GABA-B/ baclofen receptors present)
Granule cells (glutamate) (interacting with n on-NMDA type receptors)
Deep cerebellar nuclei & associated efferent pathways
To brain stem, red nucleus, & thalamus-(glutamate)
To inferior olive- (GABA)
Causes:
I.
Acquired Causes of Cerebellar ataxia
Congenital
Cerebral palsy
Dandy-Walker malformation
Arnold-Chiari malformation
Immune-mediated
Paraneoplastic syndromes ( anti-Yo, anti-Ri, anti-MaTa )
Miller-Fisher variant of Guillain-Barré syndrome
Other postviral syndromes ( varicella, rubeola )
Multipe sclerosis
Infectious
Acute viral syndromes
Creutzfeldt-Jakob disease
Meningitis
Whipple’s disease
Mass lesion-related
Abscess ( bacterial or fungal )
Neoplasm
105
Sarcoid
Paroxysmal
Epilepsy
Febrile illness
Migraine
Supratentorial
Gait disorders of the elderly
Hydrocephalus
Systemic
Endocrine disorder ( hypoparathyroid, hypothyroid )
Gastrointestinal disorders ( celiac disease, other causes of vitamin E malabsorption )
Vasculitis
Toxin-& drug-induced
Mercury, organophosphate insecticides, solvents
Chemotherapy agents, phenytoin
Traumatic
Immediate injury
Delayed injury
Vascular
Stroke
Vascular malformation
II.
Inherited Causes of Cerebellar Ataxia
Autosomal dominant
Triplet repeat diseases
Spinocerebellar ataxia types 1, 2, 3, 6, 7 & 8
Dentatorubral-pallido-luysian atrophy
Point mutations
Episodic ataxia types 1 & 2
Gerstmann-Straussler syndrome – prion protein
Unknown mutation
Spinocerebellar ataxias types 4, 5 & 10
Autosomal recessive
Friedreich’s ataxia -classic, late-onset, or with retained reflexes
Known metabolic abnormalities
Intermittent
Pyruvate syndromes
Aminoacidurias
Hyperammonemias
Progressive
Lysosomal storage diseases
Peroxisomal diseases
Abetalipoproteinemia/ hypobetalipoproteinemia
Tocopherol transfer protein deficiency
Cerebrotendinous xanthomatosis
Ataxia-telangiectasia
Mitochondrial diseases
May be autosomal dominant or maternally transmitted
X-linked
106
Treatment of Cerebellar Ataxia:
Diet & Lifestyle:
Vegetarian diet may predispose to vit. B12 deficiency which could complicate ataxia
Deficiencies of thiamine (B1), Vit.B12, & Vit. E can cause ataxia
Drug Treatment:
Amantadine ( Mantadix , Symmetrel , Amantine )
A tricyclic amine that ↑ release of dopamine & other monoamines ( serotonin & noradrenaline )
Start with 100 mg /d
↑ biweekly to b.i.d. or tid
Children: ½ adult dose (
L-5 HTP start with 50 mg /5 ml syrup )
A precursor of serotonin , may be effective in mild & moderate ataxia
Buspirone ( Buspar )
A serotonin 5-HT1A receptor agonist
Start with 5 mg 0.d.or bid
↑ biweekly by 5 mg to maximum of 20 mg tid
Usually 10-30 mg /d are enough
Acetazolamide ( Diamox, Cidamex )
A brain carbonic anhydrase inhibitor CNS acidosis
Improves episodic ataxia & vertigo
Start with 250-500 mg /d.
↑ up to 1000-4000 mg /d. as tolerated
Benzodiazepines e.g. Clonazepam ( Rivotril )
A GABA-A receptor modulator Can reduce cerebellar tremor
0.5-6 mg /d.
May lead to long-term worsening of balance & incoordination
Baclofen ( Lioresal )
A GABA-B agonist
Improves spasticity, but may worsen ataxia
Choline & Lecithin: ineffective
Physostigmine ( Prostigmine )
A centrally acting acetylcholinesterase inhibitor
Oral & s.c. use may be useful
Isoniazid ( INH )
A GABA transaminase inhibitor
May be useful in kinetic tremor
Can cause an acute cerebellar syndrome
Propranolol ( Inderal )
A beta-blocker
Effective for postural tremor
Primidone ( Mysoline )
A barbiturate AED
Effective for postural tremor, but may worsen ataxia
Carbamazepine ( Tegretol ),
400-600 mg /d.
Improves cerebellar tremor
107
Gabapentin ( Neurontin )
400 mg tid.
Baclofen ( Lioresal ) can improve nystagmus,
Clonazepam ( Rivotril ) but worsen ataxia
Fluoxetine ( Prozac )
An antidepressant
Improves pseudobulbar affect & motor dysfunction
( e.g. dysarthria , dysphagia for liquids )
10-20 mg in the morning
Botulinum Toxin Type A ( Botox A )
Control head nodding & tremor
15-25 U per muscle
Surgical Treatment:
Thalamotomy : control tremor unresponsive to drugs
Thalamic stimulation : is better tolerated
Physical / Speech Therapy, Exercise:
Rehabilitation: safe ambulation & independence in ADL
Assisted exercise, gait training, speech & swallowing training, use of assistive devices, … etc.)
Exercise & biofeedback training
Central vestibular compensation exercises
Other Treatments:
Alternative therapies ( Complementary Medicine ) e.g. acupuncture, chiropractic may be helpful in pain relief
Megavitamin therapy may be harmful:
Excessive vit. B6 intake may → peripheral neuropathy
Excess iron accumulates in neuronal mitochondria in deep cerebellar nuclei in pts with Friedreich ‘ s ataxia gene free radical damage neuronal cell death
Megadose vit .C therapy may → absorption of dietary iron
Emerging Therapies:
Antioxidants e.g. vit.E, coenzyme Q10, idebenone , riluzole ( Rilutek )
N-acetyl-cysteine
A free radical scavenger, Improves speech, coordination & gait
500-1500 mg tid
108