Nutrition Study Guide
advertisement

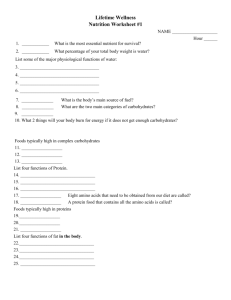
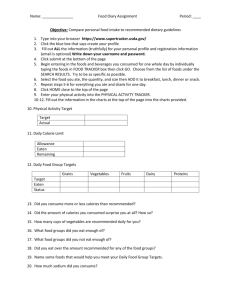
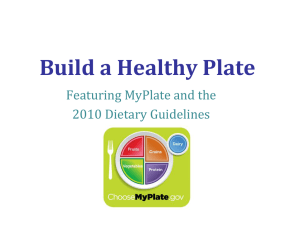
Nutrition Study Guide Essential Nutrients A nutrient provides nourishment and affects metabolic and nutritive process. Nutrients include: Carbohydrates Proteins Lipids Vitamins Minerals Water Carbohydrates = Source of energy; 4 kcals/gram _____________________: mainly from plant foods Fiber: soluble or nonsoluble Soluble: delays GI transit time (helps diarrhea) Nonsoluble: accelerates transit time (helps constipation) Proteins Types: Amino Acids = Essential proteins: cannot be manufactured in body so required in daily diet. Sources: meats, poultry, fish, eggs, dairy products Vegetarians must eat corn/bean combo to achieve essential protein Lipids (Fats) Saturated fats: animal product; solid @ room temp; should be limited in diet Ex: butter, meat fat Unsaturated fats: plant product; liquid @ room temp; Ex: Olive oil, canola oil Cholesterol: in foods and also produced by body; synthesized in the liver Lipids are stored as adipose tissue AHA recommends limiting fats to __________________ of total calories and saturated fat to 10% Vitamins Vitamins: cannot be manufactured by body and are required for metabolic processes (except for Vit K) Water soluble: body cannot store, must be in diet: Vit C: citrus fruits, broccoli, greens Vit B complex: meats, green leafy veggies Pregnancy: folic acid (B9) to prevent neuro tube defects Fat soluble: body can store for long periods Vit A,D,E,K Therefore should not take more than recommended amt. Vitamin levels are highest in fresh foods consumed ASAP after harvest Minerals Macrominerals: > 100 mg required daily Calcium, phosphorous, sodium, potassium, magnesium, chloride, sulfur Microminerals: < 100 mg required daily Zinc, iron, etc. Role: balance pH of body and promote ______________________________________ Water Roles of water: transportation of nutrients and waste products, providing structure to large molecules, participation in metabolic reactions, serving as a solvent, lubricant and cushion, regulating body temperature and maintaining blood volume. Infants have the greatest percentage of total body weight as water; older adults have the least. Both are most vulnerable to water deprivation. Illness can create a increased need for fluids (ex: fever) or a need to ingest less fluids (ex: cardiac or renal disease) ___________________________is protective and alerts a person to the need for fluids Know these processes Digestion Absorption (primarily in small intestine) Metabolism BMR: energy needs of a person at rest If diet exceeds energy needs = gain weight If diet does not meet energy needs = lose weight Anabolism: producing substances via nutrient synthesis Catabolism: Breakdown of body tissues for energy Energy = Calories 1 g carb = 4 calories 1 g protein = 4 calories 1 g fat = 9 calories 1 g alcohol = 7 calories Think for dieting: what types of food can you eat in great quantities but have less calories? Do you know how many calories you should consume based on your height and optimal weight? New 2010 Food Guide MyPlate Specific goals of the revisions are: Balancing Calories Enjoy your food, but eat less. Avoid oversized portions. Foods to Increase Make half your plate fruits and vegetables. Make at least half your grains whole grains. Switch to fat-free or low-fat (1%) milk. Foods to Reduce Compare sodium in foods like soup, bread, and frozen meals ― and choose the foods with lower numbers. Drink water instead of sugary drinks. New MyPlate Recommendations Some Healthy People 2010 Goals Increase healthier food access Child care centers and school, retail access Increase awareness in healthcare/worksites BMI measurements at appts, work incentive programs Decrease obesity Children and adults Decrease food insecurity Household and child hunger Educate about food consumption MyPlate Decrease iron deficiency Young children and pregnant females Vegetarians Plant based diet Vegans are susceptible to vitamin B12 and protein deficiency; must supplement diet with B12 and carefully choose foods to ensure ingestion of essential amino acids (for example: bean/corn combo meal) Other Common deficiencies Iron deficiency -> anemia Diet sources of iron: meat, spinach, kidney beans Calcium deficiency -> osteoporosis Premenopausal women: 1000 mg/day Ca recommended Postmenopausal women: 1500 mg/day Ca recommended Men variable Food sources: dairy products, greens, broccoli Nursing Assessment Screening: see Mini-Nutritional Assessment (MNA) tool for older adults. A score of 17 or less indicates protein-energy malnutrition If you find a patient at risk for nutritional problems, a more in-depth assessment by a Registered Dietician should be done May do Diet History & Medication History to determine if interactions exist (meds affect appetite, disturb taste, interfere with nutrient absorption) Patients at Risk for Malnutrition Involuntary gain or loss of > 10% usual body weight within 6 months > 5% usual body weight in 1 month Current weight _____________________ under or over ideal body weight Presence of chronic disease or increased metabolic requirements Inadequate nutrient intake Altered diets or diet schedules Inability to ingest or absorb food Problems Associated with Poor Nutrition in Older Adults Difficulty chewing & swallowing Lowered glucose tolerance Decreased social interaction/living alone Loss of appetite Loss of senses of smell and taste Limited income Difficulty sleeping at night (too tired to prepare meals) Dysphagia = swallowing dysfunction; many causes Indicators warning of dysphagia Cough; change in voice tone or quality after swallowing; abnormal movements of mouth, tongue or lips; slow, uncoordinated speech Usually do NOT overtly cough when food enters airway; “silent aspiration” is common cause of complications such as pneumonia Dysphagia causes decreased food intake which results in malnutrition Nurses and CNAs are often first to detect dysphagia and can notify health care provider for followup See Aspiration Precautions Physical Exam Look for signs of malnutrition; skin and hair are primary areas that reflect deficiencies. General Appearance: apathetic, easily fatigued Weight: Over or underweight Muscles: flaccid, poor tone, “wasted” appearance Nervous system: irritability, decreased reflexes, burning/tingling of hands/feet, Skin: Rough, dry, flaky, lack of subq fat Nails: brittle, ridged Hair: dry, dull, sparse, brittle Lips: Swollen, red cracks at side, fissures Tongue: swollen, beefy red, smooth Gums: swollen, inflamed, bleed easily Edema and _______________________ BMI: Body Mass Index BMI = weight in kg -----------------(height in meters)² 19-24.9 recommended for good health Under 19= underweight 20-24 = normal 25-29 = overweight 30-39 = obese 40+ = Extreme obesity Assessing: Lab Data Serum proteins (=estimate of protein stores) Albumin (4.0) and Prealbumin (20) Low levels can indicate prolonged protein depletion If protein depletion, then the immune system can be depressed. See WBC differential: lymphocyte count decreased Diagnosing Imbalanced Nutrition: More than Body Requirements Imbalanced Nutrition: Less than Body Requirements Risk for Imbalanced Nutrition Feeding Self Care Deficit Risk for Aspiration Planning Goals: Weight gain or loss of ½ to 1 pound per week is realistic Remember correction of poor dietary patterns is a long term goal Implementation Use tools like MyPlate, Food Diaries, BMIs Educate about food choices, food labels and their meaning Educate about healthy diet and exercise and help integrate changes into client’s lifestyle Must be designed to meet intellectual ability, motivational level, lifestyle, culture and economic status Educate about food safety In Acute Care Recognize stress affects intake Meds can affect intake and utilization of nutrients Symptoms such as pain, nausea, sob have major effect on appetite Food presentation is a factor Promoting a Comfortable Environment to Stimulate Appetite Make sure environment is free of odors and reminders of treatments Provide mouth care Administer analgesics and antiemetics early enough before meals Position patient comfortably Reduce stress via therapeutic communication Assisting Clients with Feeding Assisting clients who are weak & debilitated but protect dignity and involve them If possible, help them feed themselves instead of feeding them Position in chair or high Fowlers position Be sensitive to loss of autonomy, embarrassment Convey unhurried attitude, sit at bedside Ask what order to eat food If visual problems: use clock method or describe food If cannot communicate, offer fluids every 3-4 bites Dysphagia Interventions Thickened liquids Modification of food texture Position upright Replacement of oral feeding with enteral tube feeding Remain upright 30 minutes after meal Special Diets Assisting with special diets NPO: nothing by mouth Clear liquids: you can see through Full liquids: All food and fluids mixed with liquid for thin consistency Regular: all foods, no restrictions Puree: Uniform “pudding like” Mechanically altered: moist, soft textured; forms a bolus Modified per disease process: Diabetic, low salt, low cholesterol Enteral Feedings Given via tube into stomach or intestinal tract; must have functional GI tract Types: NG tube (thru nostril into esophagus) Must have intact cough/gag reflex, adequate gastric emptying, usually short-term PEG/PEJ tube: puncture thru skin into stomach (PEG) or jejunum (PEJ) Continuous or intermittent feeding Must elevate HOB _____________________- to avoid aspiration Parenteral Nutrition Administration of solution containing glucose, amino acids, lipids, minerals, electrolytes and vitamins through central venous catheter into superior vena cava Used when GI tract nonfunctional Hypertonic so only administered into high flow central veins where diluted by blood Goal: maintain anabolic state in clients unable to maintain normal nitrogen balance such as in severe malnutrition, severe burns, metastatic CA, renal/hepatic failure Risks: Infection: ______________________________ Requires frequent monitoring of fluid, electrolytes, glucose Home Care Special Community Nutritional Services: Meals on Wheels, Food Stamps Evaluation Weight gain/loss Improved labs (albumin and prealbumin) Self-reported improved intake If progress does not occur: Were interventions not effective, not realistic, not done by patient or affected by unanticipated factors. Success depends on patients willingness and ability to change behavior patterns