ssep anatomy handout - Neuroconnectllc.com
advertisement
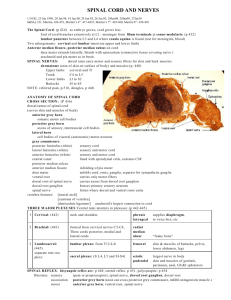
SSEP ANATOMY HANDOUT Action potential- electrical response of the nerve, that causes 1) depolarization of cell by a stimulus, 2) release of chemical transmitter substance, 3) release of Ca+ to enter axon terminal, 4) Ca+ opens synaptic vesicles that release neurotransmitter substances (inhib & excit) 5) if excitatory, Na+ rushes into cell, resting membrane goes from –80 to +10, and 6) as Na+ permeability decreases K+ leaves the cell. Active Transport Pump (ATP) (also known as sodium pump and Na+/K+ pump) – forces ions in and out of cell to make cell go from action back to resting. ATP (adenosine triphosphate) is the neurotransmitter substance that energizes the pump. Anions- negatively charged ions (ions that have gained an electron). They are attracted to the positively charged anode. Anterior horn cell- large nerve cell in the anterior horn of the spinal cord. The axon of the cell is an efferent (away) fiber innervating a muscle. Anterolateral system – carries information about pain and temperature Association area- located in the posterior area of the parietal lobe and is necessary for correlation of cutaneus sensation, enabling recognition of familiar objects by touch Axon- is a single fiber, surrounded by a myelin sheath extending from the neuron, it sends impulses away from the soma to other neurons Baroreceptors- detect changes in blood pressure and govern blood flow Cations- positively charged ions (ions that have lost an electron). They are attracted to the negatively charged cathode. Cauda equina- (Latin for horse’s tail)- extension/bundle of the spinal nerve roots that form a tail like projection at the bottom of the vertebral column. The spinal cord ends at L2. The cauda equina contains the nerve roots of L3- L5, S1-S5 and the coccygeal. Cell body (also called soma & perikaryon)- is the main part of a cell and contains cytoplasm, a nucleus and organelles Chemoreceptors- detect changes in chemicals such as oxygen, detect tension in blood and assist in respiration. Cutaneous- relating to the skin Dendrites- are tapering branches from the soma. Their main function is reception of nerve impulses which they carry toward the cell body 1 Depolarization- to stimulate the cell in some form. Upon excitation, the cell undergoes permeability and allows Na+ to enter the cell and K+ to leave the cell. Effector- peripheral tissue that receives nerve impulses and reacts by contraction (muscle) or secretion (gland) Epineurium- is a connective tissue (sheath) that surrounds the peripheral nerve trunk. Within the sheath, are bundles of nerve fibers surrounded again by another sheath called the perineurium. Between the individual nerve fibers is another connective tissue called the endoneurium. EPSP- excitatory post synaptic potential- depolarizes the cell, making it more likely to fire, less negative, increases permeability to Na+ and makes the membrane potential fall Fascicles- a peripheral nerve is composed of individual axons wrapped in a myelin sheath, these individual fibers are arranged in bundles called fascicles Fasciculus (nucleus) cuneatus- is part of the dorsal or posterior columns. It contains input from the upper half of the body with fibers from the lower (thoracic) segments more lateral than the higher (cervical) ones Fasciculus (nucleus) gracilis- is part of the dorsal or posterior columns. It contains input from the lower half of the body with fibers that arise from the lumbrosacral region.(more medial segments) Ganglia- term used to designate a group of nerve cells lying outside the CNS or a mass of nerve cell bodies located in the PNS Glial cells- act primarily as support for neurons, they comprise ½ the volume of the brain and the spinal cord. There are four kinds of glial cells astrocytes (provide support, nutrition & insulate), oligodendrocytes (formation and maintenance of myelin), microglia (defend against infection & injury) and ependyma. There are 60-70 axons served by one oligodendrocyte. The glial cells in the PNS are called schwann cells. Only one axon is served by a schwann cell. Innervate- the supply of nerve fibers functionally connected with a part Intervertebral foramina of the vertebral column- the 31 pairs of spinal nerves enter and leave the spinal cord through this. (foramina is a hole or opening) Ion- an electrically charged atom or group of atoms that have gained or lost electrons 2 IPSP- inhibitory post synaptic potential- This hyperpolarizes the cell, making it less likely to fire, makes it more negative, increases the membrane permeability for Cl- and stabilizes the membrane. This can happen following an action potential. Lemnisci (Latin for ribbon) - a bundle of sensory nerve fibers ascending from sensory nuclei in the spinal cord to the thalamus. They can be lateral (exterior) or medial (interior). Lissavers tract- is a bundle of fibers that ascends from the dorsal root of the spinal cord. Myelin- is an insulating material that surrounds the axon. It is a milky, white, slippery chemical that greatly increases the speed of impulses spreading along the axon. Nerve tracts- bundles of nerve fibers in the CNS Neuron- is the primary cell of both the CNS and the PNS. Its main function is reception and conduction of nerve impulses and the property of excitability. It is incapable of reproducing itself after damage to it’s cell body and nucleus. Neurotransmitters- chemical agents released by a presynaptic cell upon excitation, it crosses the synapse to stimulate or inhibit the postsynaptic cell Excitatory: 1) Acetylcholine (ACTH) at synapses, 2) L-glutamic acid & 3) L-aspartic acid Inhibitory: 1) Gamma-aminobutyric acid (GABA), 2) Glycine & 3) Acetylocholine (ACTH) in superficial cerebral cortex Other: 1) Monoamines a) dopamine b) noradrenaline c) 5-hydroxytrptamine 2) Histamine, 3) ATP (Adenosine Triphosphate), 4) Substance P & 5) Endorphines Nodes of Ranvier- are gaps that interrupt the sheath along the axon. They are sections of myelin around the axon that allow potentials to leap faster from one section to another, it looks like sausage links. Organelles- are responsible for energy metabolism, removal of waste and cell repair Peripheral nervous system (PNS)- Structurally the PNS is composed of the cranial nerves, spinal nerves and their associated ganglia. Their pathways are divided into afferent and efferent. Functionally the PNS can be divided into the somatic nervous system and the autonomic nervous system. It is the relay system of all sensory and motor messages being sent to and from the CNS. 3 Peripheral nerves- bundles of nerve fibers in the PNS Peripheral nerves are classified into groups A, B and C. Group A has 4 sizes of nerve fibers Alpha, Beta, Gamma and Delta. They are all heavily myelinated and range in size from 2 - 20 microns (micrometer) and are as fast as 12 – 120 meters per second. Group B fibers have some myelin and are medium sized at less than 3 microns and 3-15 meters per second. Group C fibers are unmyelinated, the smallest at .3 to 1.3 microns and the slowest moving at .5 to 2 meters per second. Postcentral gyrus (sensory strip/Brodman’s 1, 2 & 3)- the primary somatosensory cortex is located here. It receives sensory information from the corresponding areas of the contralateral body. It is located posterior (behind) to the central gyrus (Rolandic fissure). The secondary somatosensory is located posterior to the posterior central gyrus in the posterior parietal lobe and is labeled Brodman’s area 5 and 7. Posterior or dorsal columns- contain the fasciculus gracilis and cuneatus. It conveys information about touch, pressure, position, joint sense and vibration. The fibers in the dorsal column terminate in the brainstem at the level of the medulla. Precentral gyrus (also called the motor strip)- controls motor function to the corresponding areas of the contralateral body, located in front of the central gyrus Proprioceptors- detect changes in the position of the body Receptors- are special sensory endings. Communication about an individual’s external environment, begin here. They transform stimulus energy into electrochemical energy and establish a common language for all sensory systems. Refractory periods- time of decreased excitability in the wake of an action potential. 1) absolute- cell is incapable of responding to stimulus & 2) relative- action potential can be generated, but conduction velocity is decreased and threshold is increased. Resting membrane potential- The neuron is relatively quiet and maintains a potential difference across its membrane so that the inside is –70 to –80mV with respect to the outside. The inside contains negatively charged protein molecules and high amounts of K+. The outside has high amounts of Na+ and Cl- and low amounts of K+. There is disequilibrium of Na+ and K+ ions across the cell membrane. It is disrupted by synaptic processes. Somatosensory system- is a part of both the CNS and the PNS. It begins in the PNS where receptors code specific information. It conveys information from the musculature and skin areas to the brain. It regards sensations such as touch, pressure, pain, temperature and vibration. All somatosensory information from the body is relayed over dorsal root ganglion neurons. 4 Synapse- is the site of communication between two neurons where information is passed by chemical transmitter substances known as neurotransmitters. There are 3 types of synapses, axo-axonic, axo-somatic and the most common axo-dendritic. Tegmentum roof or covering – dorsal portion of cerebri of midbrain. It contains red nucleus and nuclei and roots of oculomotor nerve. Teledendria- many fine branches at the end of the axon. Threshold- degree of depolarization necessary to elicit the action potential Trapezoid body- (also called the corpus trapezoid) bundle of transverse fibers in the ventral portion of the tegmentum of the pons. F YI The posterior or dorsal root consists of nerve fibers carrying information towards (afferent) the central nervous system. The anterior or ventral root carries signals away (efferent) from the CNS. Lower motor neurons are located in the anterior gray column of the spinal cord. The posterior tibial nerve controls motor function for the plantar flexion of toes and sensory distribution for the plantar aspect of the foot. The initial negative activity appearing at the scalp (16-19msec) from the stimulation of the median nerve is generated by the thalamus. The motor and sensory pathways have a close anatomical relationship. SSEPs are thought to be generated by the posterior columns and the medial leminisci. 5 SPINAL CORD TRACTS OUTLINE I. Afferent (sensory/dorsal/posterior) Pathways (tracts/columns/lemnisci/funiculis) (Travels up (ascends) toward the brain) A Spinothalamic Tract (STT) Goes from the spine to the thalamus. 1. Anterior STT (simple touch) a. Nerve endings of peripheral nerve to spinal cord (1st order neuron) b. Spinal cord to thalamus (2nd order neuron) c. Thalamus to somatosensory cortex (3rd order neuron) 2. Lateral STT (pain & temperature) a. 1st order enters SC in dorsal roots & synapses in dorsal horn b. 2nd order crosses SC & ascends to synapse in thalamus c. 3rd order ends in parietal lobe B Dorsal White Columns (DWC) ( Fasciculus Gracilis & Cuneatus (these fibers eventually become the medial lemniscus)) (Impulses from the leg travel in the gracilis. Impulses from the arm travel in the cuneatus) It involves proprioception that goes toward sensory strip. a. 1st order neuron goes from nerve endings to medulla then synapses with either the gracilis or cuneatus b. 2nd order crosses in medulla & ascends to synapse in thalamus c. 3rd order goes from thalamus to somatosensory cortex C Spinocerebellar Tract (SCT) (Proprioception) Goes from the spine to the cerebellum to the motor strip. 1. Anterior/Ventral Spinocerebellar Tract a. 1st order neuron is from nerve endings to spinal cord b. 2nd order goes up SC without crossing to ipsi cerebellum c. 3rd order is from cerebellum to contra somatomotor cortex 2. Posterior/Dorsal Spinocerebellar Tract a. 1st order neuron is from nerve endings to spinal cord b. 2nd order goes up SC without crossing to ipsi cerebellum c. 3rd order is from cerebellum to contra somatomotor cortex The medial lemniscus originates in the posterior column and ascends to the thalamus. It is the major ascending pathway for tactile and proprioceptive information. It is actually an extension of the dorsal white column. Other sensory tracts include the spinoolivary, spinotectal (spine to brainstem) and the spinoreticular tracts. 6 II. Efferent (motor/ventral/anterior) Pathways (tracts/columns/lemnisci) (Travels down (descends) away from the brain) A Corticospinal Tract (CST, Pyramidal Tract) (Voluntary motor impulses) Goes from cortical area of brain to the spine. 1. Ventral/direct 20% of fibers do not cross a. Upper motor neurons (CNS) b. Lower motor neurons (PNS) 2. Lateral/indirect 80% of fibers cross a. Upper motor neurons b. Lower motor neurons B Corticobulbar Tract (CBT) (Same path as CST but takes different route in midbrain. Carries motor impulses to muscles of head & neck via brainstem & cranial nerves not the spinal cord and spinal nerves.) a. Upper motor neurons b. Lower motor neurons The rubrospinal tract is a very small motor tract in humans that originates in the red nucleus and projects to the spinal cord. It is an “alternate route” for signals pertaining to voluntary movement. The reticulospinal tract in another “alternate route” for the same signals as above. It originates in the reticular formation in the pons and travels to the spinal cord. The tectospinal tract is another motor tract. Tectal is the posterior portion of the brainstem. (Anything behind the aqueduct of sylvius is tectal and in front of it is tegmentum.) There are also lateral and medial vestibulospinal tracts. 7 UPPER AND LOWER MOTOR NEURONS In the afferent pathways, we describe specific portions of the pathway or column as 1st, 2nd and 3rd order neurons. In the efferent pathways, we separate specific portions by calling them upper or lower motor neurons. Upper motor neurons (UMN)- are only in the efferent pathway and are completely contained within the CNS. The UMNs are the cell bodies and fibers that make up the pyramidal tract in the CNS. UMNs start in the precentral gyrus (somatomotor cortex) and cross in the medulla at the pyramidal decussation (picture of where pyramidal decussation takes place is on page 7 of your PNS & spinal cord pictorial handout). After leaving the medulla, UMNs go down the spinal cord to the anterior horn cells. Signs of upper motor neuron lesions: 1) 2) 3) 4) 5) spastic paralysis or paresis little or no muscle atrophy positive babinski sign no fasciculations or fibrillations brisk reflexes (hyperactive) Lower motor neurons (LMN)- are also called the final common pathway. Only the very first portion of the LMNs, which is very small, is in the CNS. The entire rest of the LMNs are in the PNS. LMNs begin in the anterior gray horns of the spinal cord, which is in the CNS. After the fibers synapse in the cord, they exit the cord through the ventral roots and are now spinal nerves, which are part of the PNS. The spinal nerves travel out to muscles. The axon of a single LMN branches several times after entering the muscle, so that one neuron supplies as many as 10-300 separate muscle fibers. Signs of lower motor neuron lesions: 1) 2) 3) 4) 5) flaccid paralysis of involved muscles significant muscle atrophy (fasiculations or fibrillations) polio weak or absent reflexes negative babinski sign 8