Critical Appraisal Topics Outline
advertisement
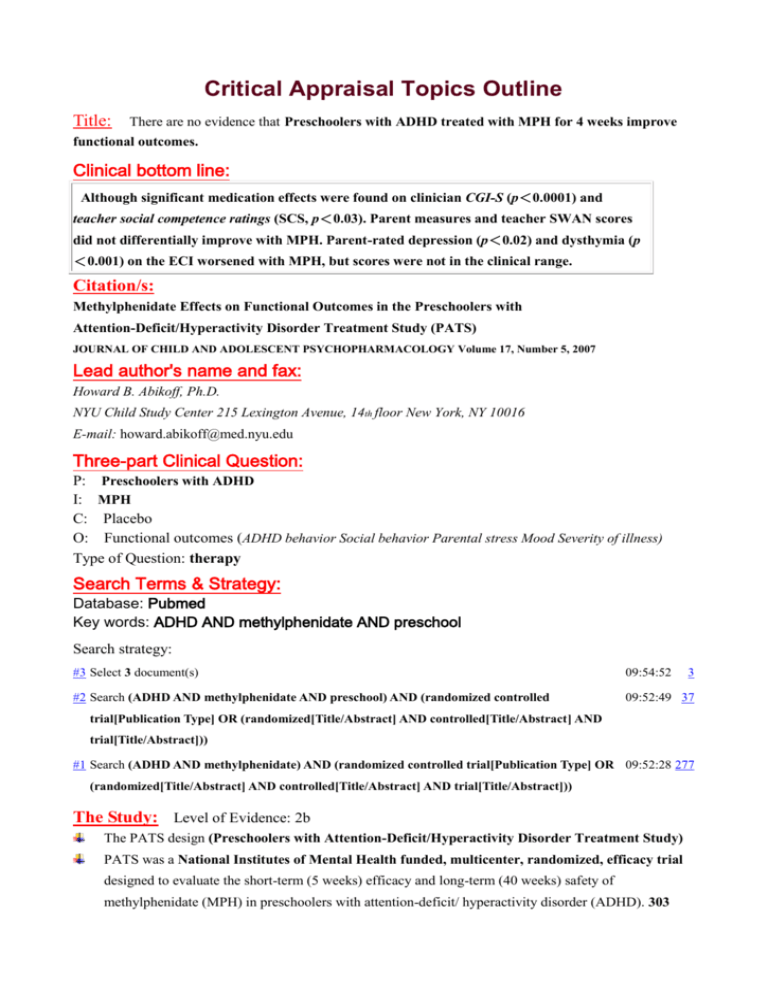
Critical Appraisal Topics Outline Title: There are no evidence that Preschoolers with ADHD treated with MPH for 4 weeks improve functional outcomes. Clinical bottom line: Although significant medication effects were found on clinician CGI-S (p<0.0001) and teacher social competence ratings (SCS, p<0.03). Parent measures and teacher SWAN scores did not differentially improve with MPH. Parent-rated depression (p<0.02) and dysthymia (p <0.001) on the ECI worsened with MPH, but scores were not in the clinical range. Citation/s: Methylphenidate Effects on Functional Outcomes in the Preschoolers with Attention-Deficit/Hyperactivity Disorder Treatment Study (PATS) JOURNAL OF CHILD AND ADOLESCENT PSYCHOPHARMACOLOGY Volume 17, Number 5, 2007 Lead author's name and fax: Howard B. Abikoff, Ph.D. NYU Child Study Center 215 Lexington Avenue, 14th floor New York, NY 10016 E-mail: howard.abikoff@med.nyu.edu Three-part Clinical Question: P: Preschoolers with ADHD I: MPH C: Placebo O: Functional outcomes (ADHD behavior Social behavior Parental stress Mood Severity of illness) Type of Question: therapy Search Terms & Strategy: Database: Pubmed Key words: ADHD AND methylphenidate AND preschool Search strategy: #3 Select 3 document(s) 09:54:52 3 #2 Search (ADHD AND methylphenidate AND preschool) AND (randomized controlled 09:52:49 37 trial[Publication Type] OR (randomized[Title/Abstract] AND controlled[Title/Abstract] AND trial[Title/Abstract])) #1 Search (ADHD AND methylphenidate) AND (randomized controlled trial[Publication Type] OR 09:52:28 277 (randomized[Title/Abstract] AND controlled[Title/Abstract] AND trial[Title/Abstract])) The Study: Level of Evidence: 2b The PATS design (Preschoolers with Attention-Deficit/Hyperactivity Disorder Treatment Study) PATS was a National Institutes of Mental Health funded, multicenter, randomized, efficacy trial designed to evaluate the short-term (5 weeks) efficacy and long-term (40 weeks) safety of methylphenidate (MPH) in preschoolers with attention-deficit/ hyperactivity disorder (ADHD). 303 subjects ages 3 to 5.5 years old who met criteria for a primary DSM-IV diagnosis of ADHD entered the trial. Subjects participated in an 8-phase, 70-week trial that included screening, parent training, baseline, open-label safety lead-in, double-blind crossover titration, double-blind parallel efficacy, open-label maintenance, and double-blind discontinuation. Double-blind, parallel design study phase 114 children went on to participate in the between-subjects, randomized, 4-week, double-blind, parallel design study phase of the PATS trial, where in they were randomized to either their best dose of MPH or PL. (61 were randomized to MPH and 53 to PL.) Assessments of functional outcomes. ADHD behavior parent and teacher versions of the Strengths and Weaknesses of ADHD-Symptoms and Normal Behaviors (SWAN) Social behavior Social Competence Scale (SCS), Social Skills Rating System (SSRS) Parental stress Parenting Stress Index (PSI) Mood Early Childhood Inventory (ECI) Severity of illness Clinical Global Impression-Severity (CGI-S) The Evidence: Of the 114 children who entered the 4-week parallel-design phase, 36 (32%) dropped out. Behavioral deterioration, (45% vs 15% PL vs MPH) drop out rate the power to detect treatment differences was decreased because of the reduced sample size available for analysis. Effect (p<0.03; ES=0.39) was found in teacher ratings on the SCS, with preschoolers treated with medication improving in their social competence scores, Clinicians’ global ratings of severity on the CGI-S at posttreatment were significantly lower for children in the MPH group compared to those on PL (p<0.0001; ES=0.73). Children in the MPH group had significantly higher mood scores on the parent rated ECI Major Depressive Disorder (p<0.02) and Dysthymic scales (p<0.001). an increase in mood symptoms from pre- to posttreatment with MPH in contrast to a decrease over time with PL Comments: Medication effects varied as a function of informant and outcome measure. MPH resulted in a significant increase in scores on the Major Depressive Disorder and Dysthymic Disorder scales on the ECI compared to PL, the scores were not in the clinical range. 情緒障礙會和 學齡兒童一致在使用MPH 6到10個月左右會減輕和改善 (Wigal et al. 2006), (Hechtman et al. 2004). The MPH doses in the double-blind parallel group study phase were relatively low (M=14.22 ± 8.1 mg/day), PATS maintenance phase (Vitiello et al., this issue), (M=19.98 ± 9.56 mg/day) was associated with improvements in children’s social skills as rated by parents. Improved parent–child interactions, decreased negative parenting practices often occur with MPH treatment but not been shown to increase positive parenting practices or positive changes in parent functioning, such as improved mood and ability to complete tasks (Stein et al. 1996; Hechtman et al. 2004; Chronis et al. 2003). The power to detect treatment differences was decreased because of the reduced sample size available for analysis. Greenhill et al. 2006 : children withdrawn from the study had an increase in ADHD symptoms. 所 有個案都服用過MPH, 家長可能會因為吃PL無效而退出對照組(?). Gordon et al. 2006 : the association of ADHD symptom severity and degree of functional impairment has been reported to be relatively small. Poor concordance rates for parent and teacher ratings of ADHD symptoms in the PATS sample has been reported by Murray et al. (this issue). The variability of children’s behaviors across situations (McDermott et al. 2005).家長較長的時間看到個案沒有療效,導致家長對於效果的評值較低(?). Missing data, especially from teachers, precluded analyses of teacher ratings on the SSRS and ECI. 老 師比家長對於社交功能及服藥之後的行為或情緒有更多機會觀察,缺乏老師資料可能影響效果的呈現. 4 weeks is typically sufficient to detect improvements in ADHD symptoms, a longer treatment period may be needed for functional changes to occur. Intensive behavioral treatment in combination with medication. Preschoolers with ADHD treated with MPH for 4 weeks show some improvements in functioning, although not as extensive as those found in their elementary school-aged counterparts. Systematic, randomized controlled trials are needed to address this issue. Reference: 1. Rationale, design, and methods of the Preschool ADHD Treatment Study (PATS).J Am Acad Child Adolesc Psychiatry. 2006 Nov;45(11):1275-83. 2. (Study design) Efficacy and safety of immediate-release methylphenidate treatment for preschoolers with ADHD.J Am Acad Child Adolesc Psychiatry. 2006 Nov;45(11):1284-93. Erratum in: J Am Acad Child Adolesc Psychiatry. 2007 Jan;46(1):141. Level of Evidence: 2b Appraised by: 張庭綱 Kill or Update By: Date: 2008/04/10 2008/12/30 Email: