Parts of the Nervous System
advertisement

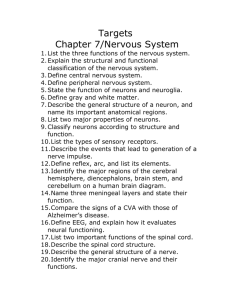
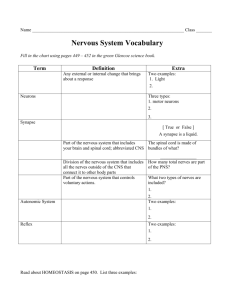
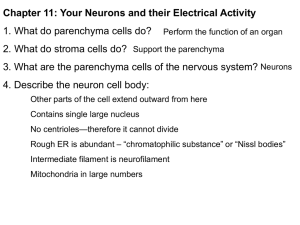
Neuroscience and Mental Health · S Tran Session 1: Neurological Disorders and their Main Causes Learning Objectives Define the following terms used to describe the Nervous System and explain how they interact with each other: Central Nervous System Peripheral Nervous System Autonomic nervous System Somatic Nervous System List the major causes of neurological disorders and give examples. State the difference in the regenerative capacity of injured axons between the CNS and PNS. Describe the main components of a standard neurological examination. Outline the main electrophysiological and imaging techniques used in neurological diagnosis, noting the main advantages and disadvantages. Parts of the Nervous System Central Nervous System = Brain + Spinal Cord o ‘Housekeeping’ Functions. – Processing sensory + motor information o Supports higher functions: perceptions, cognition, emotion & memory. Peripheral Nervous System = Peripheral nerves + Ganglia o Provides sensory & motor innervations to the body Autonomic Nervous System = parts of the CNS + PNS. o Controls visceral function & homeostasis e.g. peristalsis & bladder release o Internal organs, blood vessels, glands, eye structures, genitalia. Somatic Nervous System o Controls motor and sensory function for body wall Causes of Neurological Disorders: A. Trauma o Spinal Cord Injury Can cause paralysis B. Cerebrovascular Accident o Cerbrovascular Infarct / Stroke Degeneration of neural tissue as no backup energy reserves like muscle C. Neoplasia o Meningioma Pressure is an issue Normally metastasis, If primary then it’s normally connective tissue or glial D. Infection o Bacterial Meningitis E. Metabolic Disorders o Diabetic Neuropathy e.g. Hypoglyceamia Can result in comas In peripheral nerves Injury tingling sensation pg. 1 Neuroscience and Mental Health · S Tran F. Genetic Defects o Huntington’s Disease Degeneration of caudate and putamen nuclei Basal gangular are for movement o Down’s syndrome G. Environmental o Heavy Metal encepholopathies e.g. Lead Poisioning o Alcohol fetal alcohol syndrome o o ? Mobile Phones Recreation Drugs etc H. Immunological o Multiple Sclerosis Degeneration of neurones Differences in regeneration capacity of the NS No replacement of neurones No axonal regeneration of CNS High energy requirement – Low Energy Reserves Little space inside the cranial cavity In PNS, Regeneration may be functionally compromised In CNS, regeneration is limited in distance therefore not viable Investigations Neurological Examination 1. Level of consciousness o Glasgow Coma Scale 2. Speech o Talking to patient 3. Mental state and cognitive function o Simple general knowledge/mathematical questions 4. Sensory function o Pain, temperature, pressure and position tested 5. Motor function o Twichage, feet touch, evaluation of strength of muscle groups 6. Cranial nerve function o Eyelid strength, facial movement, gag reflex, smell, taste, hearing Electrophysiology: EEG: Electroencephalography measures the electrical potentials measured at scalp of underlying neurones Epilepsy & Coma. EMG: Electromyography examines integrity of muscles e.g. motor neurone disease NCS: Nerve Conduction Studies examines integrity of peripherphal nerves & lower motor neurones Imaging CT: Computerised Tomography uses x-ray sources. Shows hard tissue. Can’t be used too often. Cheap and Quick. MRI: Magnetic Resonance Imaging is based on the behaviour of hydrogen protons to a externally applied magnetic field. Use for soft tissue differentiation. Time consuming. Can be used to give a functioning image: Functional MRI. Angiography demonstrates cerebral vessels radiographically after a contrast medium injection. Neuronal Dysfunction and Death Neuronal Dysfunction = Epilepsy (abnormal synchronous firing) Neuronal Death = Parkinson’s disease pg. 2 Neuroscience and Mental Health · S Tran Session 2: Cells of the NS Learning Objectives Draw and label a diagram of a typical neuron, identifying soma, dendrites, axon and terminals. Define the role of each cellular component in the specialised function of the neuron. Outline the organisation and functions of intracellular transport in the neuron. Define the functional subtypes of neurons and list the ways in which they are organised collectively in the nervous system. Describe the organisation of synapses. Name the main classes of neuroglia and explain their functions in the nervous system. Structure of a Neuron Axon – Long extension of a neuron that carries nerve impulses away from the body of the cell. Axon Terminals - The hair-like ends of the axon Cell Body/Soma - The cell body of the neuron; it contains the nucleus Dendrites - The branching structure of a neuron that receives messages on the Soma. Myelin Sheath - The fatty substance that surrounds and protects some nerve fibers Node of Ranvier – Gaps in the myelin sheath, allows salutatory conduction to occur Nucleus - Organelle in the cell body of the neuron that contains the genetic material of the cell Schwann's Cells - Cells that produce myelin - they are located within the myelin sheath. pg. 3 Neuroscience and Mental Health · S Tran Function of parts of the Neuron The neuron is the basic structural and functional unit of the nervous system, it is the information processing unit, responsible for the generation and conduction of the electrical signals Neurons communicate with one another via chemicals released at the synapse. (neurotransmitters) Neurons are supported by neuroglia, comprising of several different cell types. (NB. Neuroglia outnumber neurons by approx. 9:1) A. Cell Body (Soma) Metabolic centre of the cell Large nucleus with prominent nucleolus due to large amounts of mRNA Abundant rough ER – protein synthesis Well developed Golgi Large number of mitochondria – for the generation of electric impulse Numerous lysosomes Highly organised cytoskeleton – because they can be quite long cells Highly organised metabolically active cell. B. Dendrites. Major area of reception of incoming information Spread from the cell body and branch frequently Greatly increase the surface area of the neuron. Dendritic spines receive majority of synapses (spines = protrusions on the dendrites) Large pyramidal neurons may have as many as 30,000/40,000 spines C. Axon. Conducts impulses away from the cell body Emerges as the axon hillock Action potential generated at hillock Usually only one axon per cell but can branch extensively Microtubules and neurofilaments are prominent Myelinated or unmyelinated Axon membrane exposed only at nodes of Ranvier. D. Terminals. Close to the target the axon forms a number of terminal branches (terminal arbor). Specialised structures called synaptic terminals. Boutons or varicosities E. Neuronal cytoskeleton. In the human adult axons range in length from micrometers to up to a meter Highly organised cytoskeleton is required Neurofilaments play a critical role in determining axon calibre Microtubules are very abundant in the nervous system pg. 4 Neuroscience and Mental Health · S Tran Intracellular Transport in a Neuron Axonal transport is the process by which the neuron replenishes components of the axon and the nerve terminal. Axonal membrane is constantly being replaced by new components arriving from the cell body as are the macromolecular components of the nerve terminal needed for synaptic transmission. Anterograde transport - transport of materials needed for neurotransmission and survival away from cell body. A. Fast Anterograde a. synaptic vesicles, transmitters, mitochondria b. 400mm/day c. uses microtubular network and requires oxidative metabolism d. uses specific molecular motors B. Slow Anterograde a. delivery of cytoskeletal and cytoplasmic constituents (via bulk cytoplasmic flow of cytoplasmic constituents Retrograde transport - The process by which material returns from the terminals to the cell body either for degradation or recycle. a. transport rate approx. 200mm/day b. transport of substance from extracellular space c. trophic growth factors, neurotropic viruses d. uses different molecular motors e. Particles are driven along microtubules by a microtubule-associated ATPase – dynein f. The composition of the material is similar to that of the anterograde fast component and is packaged in large membrane-bound organelles Morphological subtypes of neurons A. Pseudounipolar Neurons Dorsal root ganglia sensory neurons have two fused processes and both axonal in structure. DRG neurons give rise to no dendrites and receive no synapses single axon acts as a continuous cable carrying action potentials from the peripheral receptor organ to the central terminal in the spinal cord without passing through the cell body found in the spinal cord ganglia B. Bipolar neurons Cerebral cortex, retina. Bipolar neurons of the retina have one dendritic process and an axon coming off the cell body pg. 5 Neuroscience and Mental Health · S Tran C. Golgi type I multipolar neurons D. Highly branched dendritic trees Cells whose axons extend long distances Pyramidal cells of the cerebral cortex All of the cortical output is mediated through pyramidal neurons which are the major excitatory neurons Pyramidal cells can be subdivided into numerous classes based on morphology, laminar location and connectivity Purkinje cells of the cerebellum Anterior horn cells of the spinal cord Golgi type II multipolar neurons – highly branched dendritic trees Cells with short axons terminating quite close to the cell body of origin. Stellate cells of the cerebral cortex and cerebellum Spiny stellate cells represent the other major excitatory input to cortical pyramidal cells Small multipolar cells with local dendritic and axonal arborizations use glutamate or aspartate as transmitter. (NB. multipolar, meaning they have more than two cell processes with only one being an axon and the remaining processes being dendrites) Functional subtypes of neurons A. Sensory neurons Commonly pseudounipolar with one major process which divides into two branches, one running to the CNS and one to a sensory receptor. Conduct impulses from sensory receptors to the spinal cord and brain. Dorsal root ganglia neurons. B. Motor neurons Conduct impulses from the brain and spinal cord to effectors - muscles and glands. Generally multipolar with large cell body. Spinal motor neurons. C. Interneurons (vast majority) Neurons whose cell bodies and processes remain within the CNS. Majority of neurons in the CNS. Can be large multipolar neurons or small bipolar local circuit neurons. pg. 6 Neuroscience and Mental Health · S Tran Interneurons are responsible for the modification, coordination, integration, facilitation and inhibition that must occur between sensory input and motor output. Functional Organisation (Groups) of Neurons 1. Nucleus Group of encapsulated neuronal cell bodies within the CNS Usually consist of functionally similar cells o E.g. brain stem nuclei and deep cerebellar nuclei 2. Laminae Layers of neurons of similar type and function o E.g. cerebral cortex and cerebellum 3. Ganglion groups of neuronal cell bodies in the peripheral nervous system and encapsulated to form a ganglion o E.g. dorsal root ganglia and sympathetic ganglia 4. Fibre Tracts Groups or bundles of axons (mixture of myelinated and unmyelinated) in the CNS White matter tracts o e.g. corpus callosum- links the right hemisphere of brain to the left side 5. Nerves Discrete bundles of axons outside the CNS (exceptions) Often mixed sensory/motor Terminal portions of axons form synapses onto other neurons allowing communication through chemical transmitters. There is a diversity of chemical transmitters Neurons receive multiple synaptic inputs. Competing inputs are integrated in the postsynaptic neuron. Synapses Axo-dendritic (on the dendrites) - these are often excitatory Axo-somatic (on the cell body) - these are often inhibitory Axo-axonic (terminating on the axon at either the hillock or the terminal) – ? Modulatory Gray’s type I synapses – vesicles clear and rounded excitatory Gray’s type II synapses- vesicles oval or flattened – inhibitory Neuroglia Support cells of CNS (glia=glue) Important for neuron function. pg. 7 Neuroscience and Mental Health · S Tran A. Astroglia (astrocytes) a. Structure: o Largest population (numberwise) in the CNS o Divided morphologically into: i. Fibrous astrocytes ii. Protoplasmic astrocytes iii. Radial Glia o Intimate association with blood vessesl, ventricle, leptomeninges, neuronal soma, synpases & nodes of Ranvier. o Most prominent cytoplasmic component is numerous intermediate filament bundles o Gap junctions b. Function: i. Scaffold for other cell types ii. Formation of the blood brain barrier & brain-CSF barrier via endfeet. iii. Transporting substances between the circulation and neurons iv. Removal & degeneration of neurotransmitters v. K+ Buffering vi. Release of Neuotrophic factors vii. Repond to injury by dividng, migrating into areas of injury – Scar formation. viii. Glioma Formation B. Oligodendroglia (oligodendrocytes) Myelin forming cells in CNS Interfascicular olgodendroglia – found in axon tracts Sometimes found in association with neuronal cell bodies a. Structure: o Nuclei are small & spherical o Few thin processes o Prominent Golgi o No Intermediate filament b. Function: i. Elaboration & maintainence of myelin sheath ii. One oligodenroglia is capable of producing numerous myelin internodes (~40) iii. Up to 50 myelin lamellae are common pg. 8 Neuroscience and Mental Health · S Tran iv. Dark and light bands seen at EM v. Olgodendroglia are very susceptible to nutritional state, toxins and infection vi. Meylin disease states – diasterous neurological consequence e.g. Multiple Sclerosis, Adenoleucodystrophy C. Microglia Cells a. Structure: o Derived during early development from blood monocytes that invaded the brain. o Dense lysosomes, lipid droplets & residual bodies phagocytosing cells. b. Function: i. Phagocytoses of foreign material ii. Antigen-presenting cells iii. Widespread network throughout the brain iv. Role in tissue modelling v. Synapse stripping. D. Ependymal Cells Epithelial type cells, which line the ventricle & central canal of the cord Apical microvilli & cilia Prominent gap junctions between ependymal cells Not connected by tight junctions. E. Peripheral Glia 1. Schwann Cells Axons of peripheral neurons are eveloped by Schwann Cells Myelin Producing Cells of the PNS 1:1 Relationship with axon Also perform astroglial functions Promotes repair. 2. Satellite Cells Cell bodies of neurons in the spinal ganglia are surrounded by metabolically supportive cells. Perform function of astrocytes in the grey matter of the CNS pg. 9 Neuroscience and Mental Health · S Tran pg. 10 Neuroscience and Mental Health · S Tran Session 3: Resting Potential Learning Objectives Define the following: o Diffusion of an ion o Permeability of a cell membrane o Electrochemical gradient of an ion. Describe how a resting membrane potential can arise from a difference in concentration of an ion across a selectively permeable membrane (use diagrams). Define electrochemical equilibrium for an ion. What is the equilibrium potential for an ion? The Nernst equation is Ex+ = (RT/ZF) ln (Co/Ci). You should know that Ex+ is the equilibrium potential of ion X+, R is the gas constant, T is absolute temperature, Z is the charge on the ion, and F is Faraday’s number 96,500 coulombs of charge/mol of a singly charged ion. Substituting the values of the constants and T= 37oC, and converting to log10, gives (for an ion with charge +1) Ex+ = 61 log (Co/Ci) You need not memorize the Nernst equation, but you are expected to be able to use it (and get the signs right!). For example, given this equation and Co and Ci, you should be able to calculate the equilibrium potential for the ion, or given the equilibrium potential and one of the concentrations, you should be able to calculate the other concentration. What are typical values for the concentration of K+ and for Na+ inside and outside a normal neuron? What is a typical value for the resting potential of a neuron? K+ concentration has a much stronger effect on the resting potential than Na+ concentration does. Explain the basis of this difference. Definitions Flux: number of ions that cross a unit area per unit time Diffusion equilibrium: no net flux Potential (emf) : electrical force between ions that repel like charges and attract opposite charges (Units: mV) Current: movement of ions due to the influence of potential (Units: Amps) Resistance of a material: a measure of how hard it is for current o flow through it (Units: Ohms) Electrochemical equilibrium: concentration gradient is balance by the electrical gradient across the membrane Equilibrium potential Ex+: the electrical potential that prevents diffusion down the ion’s concentration gradient. Resting potential Zero reference point is OUTSIDE the cell Inside the cell is negative compared to ref. All cells have a membrane potential pg. 11 Neuroscience and Mental Health · S Tran Importnat in excitable cells for cell function Membrane separates charges because: o Membrane is selectively permable o Concentration of at least one permanent ion is different on each side The ENa+ is +72 mV whereas EK+ is -90mV Na+ in plasma: 150 mmol/l and outside: 10 mmol/l K+ in plasma: 5 mmoll and outside: 150 mmol/l Graded Potentials Action Potential Occurs in axons Equilibrium potentials for Na+ is +72 mV Equilibrium potentials for K+ is -90 mV 3 1 2 4 5 pg. 12 6 Neuroscience and Mental Health · S Tran 1. Resting Potential a. Voltage gated Na+ Channels and Voltage-gated K channels are closed. b. Na-K pump maintains the resting potential 2. Foot of the Action potential (Exaggerated here) a. Stimulus depolarises the membrane potential (towards positive) 3. Upstroke Phrase a. PNa because the voltage-gated Na channels open quickly i. This starts at the threshold potential ii. Na ions enter the cell down their electrochemical gradient b. PK as voltage-gated K channels start to slowly open i. K ions leave the cell down their electrochemical gradient but fewer than Na ion entering. ii. As upstroke progresses, more and more Voltage-gated K channels open. c. Membrane potential moves towards the Na Equilibrium potential. 4. Repolarisation phase a. b. PNa because voltage-gated Na channels close. Na entry stops. PK as more voltage-gated K channels open & remain open i. K ions leave the cell down their electrochemical gradient c. Membrane potential moves towards the K equilibrium potential d. Absolute refractory period: A new action potential cannot be triggered even with a very strong stimulus (Inactivation gates closed) 5. After-hyperpolarisation phase a. PK is greater at rest because the voltage-gated K channels are still open i. K ions continue to leave the cell ii. Membrane potential moves closer to the K equilibrium potential until the voltage-gated K channels close b. Membrane potential returns to resting potential. c. Relative refractory period: stronger than normal stimulus can trigger an action potential (Inactivation gate is open) pg. 13 Neuroscience and Mental Health · S Tran Regenerative Relationship between PNa and Membrane potential Threshold must be reached before depolarisation. o Positive Feedback Behaviour All or Nothing Reponse: Once threshold is reached, a full sized action potential is produced. Cycle continues until the voltage-gated Na Channels INACTIVE, which means they close and become voltage INsensitive. The membrane remains in a refractory (unresponsive) state until the voltage-gated Na channel recovers from inactivation and becomes voltage-sensitive again. Key Points on Ions Movement Na ions enter the cell, K ions leave Only a very small number of ions cross the membrane and change the membrane potential The concentration change is extremely small, less than 0.1% Ion pumps are NOT directly involved in ion movement during the action potential only between. pg. 14 Neuroscience and Mental Health · S Tran Conduction Velocity Large diameter, myelinated axons – 120m/s Small diameter, non-myelinated axons – 1 m/s Increases with axon diameter (less resistance to current flow inside the large diameter axon) Is higher in myelinated due to nodes of Ranvier Reduced by axon diameter (regrowth), demyelination (MS, diphtheria), cold, anoxia, compression and drugs (some anaesthetics) Propagation Local current flow depolarizes adjacent region toward threshold Direction of propagation of action potential Active area at peak of action potential Remainder of axon at resting potential Adjacent area at resting potential pg. 15 Neuroscience and Mental Health · S Tran Session 4: Neurotransmitters Learning Objectives Define the essential components required for neurotransmitter release Understand the differences between excitatory and inhibitory transmission Define at least two mechanisms for the termination of neurotransmitter action at the synapse Describe how modulation of the synaptic properties of GABA can be used pharmacologically to treat epilepsy Neurotransmission Restricted to specialised structures – Synapses. ~20nm Types of neurotransmitters: o Amino acids (e.g. glutamate & gamma amino butyric acid (GABA), o Amines (noradrenaline & dopamine o Neuropeptides (opioid peptides) Mediate rapid (μs-ms ) or slower effects (ms-s) Vary in CNS tissue concentrations: mM to nM Neurotransmitter Release 1. Action potential reaches PRE-synaptic terminal & depolarises it. Calcium channels open. 2. Ca2+ ions enter pre-synaptic terminal through their voltage gated channels. Allows neurotransmitter vesicles to fuse with the pre-synaptic membrane & release their content into the synaptic gap. 3. Vesicles then are invaginated back into pre-synaptic terminal & are recycled. 4. Neurotransmitters diffuse across the synapses to the POST-synaptic terminal receptor (Protein/lipid gated channels). This allows inflow of Na+ ions depolarisations occurs (in an excitory synapse) Depolarisation in pre-synaptic Ca2+ channels open Ca2+ ions enters NT vesicles fusion & exocytosis Recyling of Vesicles & Receptor Action Na+ Influx Depolarisation in post synaptic Inactivation occurs by: Enzyme destruction of NT in cleft Re-uptake of NT by PRE-synaptic terminal pg. 16 Neuroscience and Mental Health · S Tran Uptake of NT by glial cells Diffusion out of the cleft Agonists – Enhance/Mimics neurotransmitter’s effects Antagonists – Binds & blocks receptors Synaptic Transmission Quantum: the minimum quantity of transmitter released and detected at the postsynaptic membrane ( = content of a a synaptic vesicle) Quantal hypothesis: Quanta ~ 4000-10,000 molecules of transmitter Synaptic vesicles Small clear (Ach) 200 μs Large dense cored (neuropeptides and proteins) 50 ms Toxins: TETANUS toxin: C. Tenani causes paralysis. Zn2+ dependent endopetidase inhibit transmitter release BOTULNUM toxin: C.notulinum causes falcid paralysis α-LARTROTOXIN black widow spider stimulates transmitter release to depletion. Speed of synaptic potentials at post-synaptic terminal: Fast: Uses ion channels (pentameric complexes) to bring about change in membrane potential e.g. Na+, Ca2+, K+ & Clo CNS: Glutaminergic & GABAergic synapses. NMJ: Acetylcholine (Ach) at nicotinic receptors. Slow: G-protein receptors and second messengers e.g. cAMP, IP3 via amplification cascades. o CNS & PNS: Ach at muscarinic receptors, Dopamine (DA), Noradrenaline (NA), 5hydroxytryptamine (5HT) & neuropeptides e.g. enkephalin. Ion channel linked receptors Rapid activation μ to msec. Diversity and rapid information flow o Nicotinic cholinergic receptors (nAChR) o Glutamate (GLUR) o GABA (GABAR) o Glycine (GlyR) o 5-hydroxytryptamine (5HT3 receptors) pg. 17 Neuroscience and Mental Health · S Tran Excitatory vs Inhibitory Excitatory: Post-synaptic membrane depolarises due to transmitter (e.g. GLUR/glutaminergic) uses Na+ Inhibitory: Post-synaptic membrane hyperpolarises due to transmitter (e.g. GABAergic) uses Cl- Glutamate receptors: AMPA receptors – α-amino-3-hydroxy-5-methyl-isoazole propinoic acid o Majority of FAST excitatory synapses o Rapid onset, offset and desensitisation NMDA receptors – N-methyl-D aspartate o Slow component of excitatory transmission o Serves as coincidence detectors which underlie learning mechanisms GLUR and (Excitatory amino acid transporter) EAAT in glial cells with glutamine synthetase o Glutamate Glutamine Epilepsy One of the commonest neurological conditions 50 million people worldwide Characterised by recurrent seizures due to abnormal neuronal excitability Despite advances in modulating seizure generation and propagation, the disease is disabling 30% are refractory to treatment pg. 18 Neuroscience and Mental Health · S Tran Inhibitory CNS synapses mediated by GABA Glucose TCA cycle α-ketoglutamate glutamate GABA ( Succinate semialdehyde) Cl- ions opening Glutamate GABA via Glutamic acid decarboxylase GAD (B6) GABA Succinate semialdehyde via GABA transaminase GABA-T Research has found drugs targeting GABA synapses have been beneficial for epilepsy. With epilepsy, there is either a decrease in GABA-mediated inhibition or an increase in glumate-mediated excitation, which results in brain seizures This can be treated by enhancement of GABA-mediated inhibition and suppression of glutamate-mediated excitation using glutamate receptor antagonists. Benzodiazepines (such as clonazepam, clobazam and diazepam) enhance GABA action Vigabatrin inhibits GABA transaminase Phenobarbital enhances GABA action and inhibits synaptic excitation pg. 19 Neuroscience and Mental Health · S Tran Session 5: Organisation of CNS Learning Objectives Draw a diagram to explain the relationship between the following major divisions of the CNS: spinal cord, brainstem, cerebellum, diencephalon, cerebral hemispheres. Define the functions of the dorsal and ventral horns of the spinal cord and explain how the dorsal and ventral roots and spinal nerves relate to them. Define the 3 components of the brainstem and state the main functions of the brainstem. Describe the functions of the 2 main structures in the diencephalon. State the functions of the basal ganglia and the cerebellum. Draw on a diagram of the cerebral hemisphere, the cortical lobes and primary cortical areas. Recognise the main structures of the brain in a diagram or MRI. Describe the 3 layers of the meninges and explain their role in protecting the brain. Explain how the major divisions of the brain relate to the cranial fossae in the base of the skull. Explain the relationship between the spinal segments, spinal nerves and vertebrae and state at what level a lumbar puncture can be performed safely. Identify the components of the ventricular system and relate them to the divisions of the CNS. Explain the composition, circulation and functions of CSF. State the average total volume and flow rate of CSF. Define hydrocephalus and outline how it may be treated. Distinguish between an epidural (extradural) and subdural haemorrhage. The Central Nervous System The central nervous system is made up of the brain and the spinal cord. Cerebral Hemispheres Forebrain Diencephalon Brain Midbrain Pons Hindbrain Medulla Cerebellum Spinal Cord: o o Supplies motor, sensory adn autonomic (sympathetic & parasympathic) innervations to the body through spinal nerves Mediates reflexes Brain Stem o o o Consists of the medulla, pons and midbrain Controls vital functions e.g. respiration and consciousness Cranial nerve function pg. 20 Neuroscience and Mental Health · S Tran Cerebellum o Co-ordinates movement Diencephalon o o Thalamus – relay between lower structures and cerebral cortex Hypothalamus – control of homeostasis. Interface between CNS, ANS and endocrine system Cerebal Hemispheres o o Cerebral cortex – involved in all function, Primary areas and association cortex Basal ganglia – control of movement Dorsal and Ventral Horns of spinal cord Grey matter on each side is subdivided into regions called HORNS. The ANTERIOR (VENTRAL) gray horns contain cell bodies of somatic motor neurons and motor nuclei, which provide nerve impulses for contraction of skeletal muscles. The POSTERIOR (DORSAL) gray horns contain somatic and autonomic sensory nuclei. A typical spinal nerve has two connections to the cord: a posterior and anterior root. The posterior & anterior unite to form a spinal nerve at the inter-vetebral foramen. Sensory + motor axons make the spinal nerve a mixed nerve. pg. 21 Neuroscience and Mental Health · S Tran Brainstem Comprised of the midbrain, the pons and medulla. Medulla A continuation of spinal cord that forms the inferior part of the brain. The medulla contains sensory and motor neurones many nuclei – affiliates with 5/12 cranial nerves, the cardiovascular centre and part of the respiratory centre. Pons Pons is a bridge that connects the cerebellum by transverse neurons and is also part of the sensory and motor tracts; it is also involved in the respiratory centre. The pons lie directly superior to the medulla and anterior to the cerebellum Midbrain The midbrain extends from the pons to the diencephalon. The cerebral aqueduct passes through the midbrain connecting the third and fourth ventricle below. Midbrain contains tracts and nuclei, containing neurons for muscle activity, input from proprioceptors. Basal ganglia and the Cerebellum Basal ganglia The basal ganglia receives input from the cerebral cortex and provides output back to motor parts of the cortex Helps with the initiation and termination of movement Helps initiate some cognitive process, such as attention, memory and planning May act with the limbic system to regulate emotional behaviour. Cerebellum The cerebellum is posterior to the medulla and pons and inferior to the posterior portion of the cerebrum. A main function of the cerebellum is to evaluate how well movement initiated by motor cerebrum are carried out. Sends feedback to motor areas of the cerebral cortex to help correct the errors The main brain region that regulates posture and balance. Cortical Lobes: Cortical Areas: pg. 22 Neuroscience and Mental Health · S Tran The Meninges Membrane enclosing the brain and spinal cord- for protection Dura mater – tough membrane attached to bone or forming partitions (dural folds) with venous sinuses in their margins. Archnoid Membrane – thin membrane attached to the underside of the dura, it contains delicate collagen fibres and elastic tissue Pia mater – delicate transparent membrane closely adherent to surface of brain and spinal cord Between arachnoid membrane and pia mater, there is the sub-arachnoid space CSF circulates once around the CNS before being absorbed back into the blood stream. Clinical significance: Cerebro-spinal fluid flows in the subarachnoid space and therefore obstruction by meningitis may cause hydrocephalus or bleeding between layers may cause a type of stroke. The Cranial Fossa Split into anterior fossa, middle fossa & posterior fossa. In the base of the skull, the sphenoid bone and the large hole at the back of the base of the skull called the foramen magnum can be seen o The Frontal Lobe lies in the anterior cranial fossa o The Temporal Lobe lies in the middle cranial fossa o The Cerebellum lies in the posterior cranial fossa o The Pituitary Gland lies directly above the body of the sphenoid bone o The Brain Stem passes through the Foramen Magnum The inferior aspect of the brain and inside base of the skull pg. 23 Neuroscience and Mental Health · S Tran The Vertebrae and Spinal Nerves There are 31 vertebrae in total: o 7 Cervical o 12 Thoracic o 5 Lumbar o 5 Sacral o 2 Coccyx There are also 31 pairs of spinal nerves: o 8 Cervical o 12 Thoracic o 5 Lumbar o 5 Sacral o 1 Coccyx First cervical nerve comes out above C1 and last spinal nerve comes out between the coccyx vertebrae. Big differences in size between the spinal cord and the length of the vertebrae, this is because the spinal cord stops developing but the vertebrae carry on growing in adolescence. Spinal Cord ends at L1/L2, but CSF still flows to the bottom of the spinal column, therefore below L2 is a good place to extract CSF for analysis (Between L4 and L5) Ventricular System Compromises of the spaces between the brain parts, filled with CSF. Function: to hold the brain in its usual position and to protect the brain. Different parts of the ventricular system relates to the divisions of the CNS: o Lateral Ventricle – Cerebral hemispheres o Third Ventricle –Diencephalon o The Aqueduct – Midbrain o Fourth Ventricle – Pons and Medulla. Cebero-spinal Fluid (CSF) Colourless liquid that protects the brain and spinal cord from chemical and physical damage Carries oxygen, glucose and other needed chemicals from the blood to neurons and neuroglia. Provides mechanical protection – it acts as a shock absorber that protects the delicate tissue of the brain and spinal cord from jolts, which would otherwise cause them to the bony wall & vertebral cavities. Buoys the brain; the brain effectively floats in CSF pg. 24 Neuroscience and Mental Health · S Tran Provides an optimal chemical environment for accurate neuronal signalling, as ionic composition changes can seriously disrupt production of action potentials Medium for exchange of nutrients and waste products between the blood and nervous tissue Formed in the choroid plexuses of each lateral ventricle third ventricle (where more CSF is added by choroid plexus on the roof) aqueduct fourth ventricle circulation in subarachnoid space reabsorbed back into the blood through arachnoid villi that project into the dural venous sinuses. Average total volume of CSF is ~ 150 ml Flow rate of CSF is ~ 500ml/day Hydrocephalus Accumulation of excess CSF in the ventricles increased CSF pressure Two main causes: o Communicating-block in the CSF absorption or flow: meningititis, headinjury or subarachnoid haemorrhage o Non-communicating-block caused by aqueduct stenosis, or by a ventricular or paraventricular tumour Relieved by draining excess CSF by implanting a shunt into lateral ventricle to divert into the superior vena cava or abdominal cavity or treated by removing causative agent (ventricular tumour) Symptoms: o Increased Head Circumference o Loss of Upper Gaze in Children o Adults: Headaches, Drowsiness & Blackouts Meningitis Definition: Inflammation of the meninges (covering the brain) Symptoms: Fever, Tiredness, Headache, Irritability. More serious: Confusion, Fits, Photophobia, Severe Headaches & Drowsiness. Viral Meningitis – less severe, but depends on infective agent e.g. enterovirus, EBV. Presents with Headache, Vomiting and Neck Stiffness Bacterial Meningitis – Neisseria Meningtidis, Haemophilus influenza or streptococcus pneumonae. Present with headaches, photophobia and painful eye movement. Sampling of CSF needed to differentiate. Bacterial causes increase in white blood cell count, protein levels and decreased glucose levels because blood vessel permeability increase. Viral – normal glucose levels. Epidural (Extradural) and Subdural Haemorrhage Epidural/Extradural haemorrhage – due to damaged meningeal artery between skull & dura after head trauma Subdural haemorrhage – usually due to a damaged vein between dura and arachnoid membrane Both cause a space-occupying lesion in the confined space of the cranium and hence neurological deficits. pg. 25 Neuroscience and Mental Health · S Tran Distinguishing: Rate of bleeding & onset of symptoms. Epidural is arterial bleeding faster and earlier symptoms. Subdural is venous bleeding slower and slow onset of symptoms. pg. 26 Neuroscience and Mental Health · S Tran anterior posterior pg. 27 Neuroscience and Mental Health · S Tran Session 6: Peripheral Nervous System Learning Objectives Describe the structural and functional components of a normal peripheral nerve. List the factors that affect conduction velocity of peripheral axons. Define the terms: dermatome, myotome, ramus, plexus, and explain their significance with regard to innervation of the body. State the spinal levels which contribute to the nerves of the upper and lower limb. Compare and contrast the effects of injury and disease on peripheral nerve function. Outline the main diagnostic techniques for peripheral nerve disorders. The Peripheral Nervous System Nerves emerging from the brain & spinal cord that innervate peripheral organs. Receptor Dorsal Roots CNS Ventral Root Effector Divided into afferent and efferent o Afferent: Transmit information from receptors into the CNS o Efferent: Transmit information from CNS to the effectors Somatic motor neurons: innervates skeletal muscle Autonomic neurons (pre- & post-ganglionic): Innervates glands &viscera. Cells of a Peripheral Nerve a. Neurons a. Cell bodies (Somata) located in CNS (motor) or periphal ganglia (sensory/autonomic) and their axons/processes project to peripheral targets b. Glial Cells a. Swann Cells wrap around axon, & satellite glial cells found in sensory/autonomic ganglia. c. Connective and vascular tissue components Spinal Nerves 31 pairs of spinal nerves Spinal nerve supply a band of skin & muscle. Have a ventral root (motor) and a dorsal root (sensory) which meet inside the vertebral canal at the level of the dorsal root ganglion Rami branches of the spinal nerves, the different types are: i. Dorsal ramus: innervates skin & muscles on the back ii. Ventral ramus: innervates skin, muscle of chest, limbs and pelvic area. iii. Rami comunicantes: contain axons of pre-ganglionic sympathetic motor neurons (white ramus) and postganglionic sympathetic neurons innervating visceral structures. Connective tissue sheaths: Epineurium o Loose connective tissue surrounding the whole nerve o Strong Collagenous fibres oriented in the long axis of the nerve pg. 28 Neuroscience and Mental Health · S Tran o Carries major blood vessels supplying teh nerve Perineurium o Dense connective tissue surround a fascicle (concentric layers of flttaened fibreoblast-like cells and collagenous fibres) o Diffusion barrier (blood-nerve barrier) which helps preserve the ionic milieu of the axon Endoneurium o Loose connective tissue surrounding individual axons. The larger the diameter, the faster the axonal conduction velocity PN contain a mixture of fibres of different diameters and conduction velocity (CV) Compound action potential recorded from a nerve contains several peaks reflecting different CVs due to diameter and myelination. Myelinated Fibres o Schwann cell membranes wrap around a single axon in a spiral fashion (100 layers) of myelin. Each cell covers only a small segment of the axon (internode) o Node of Ranvier – devoid of myelin o Saltatory conduction – APs jump from one node to the next Unmyelinated Fibres o Several nerve fibres lie within invagination of Schawnn Cells o Axonal diameter (~1 µm) is much less than of myelinated (1.5-2.0 µm) o Continuous conduction: AP causes depolarisation of immediately adjacent membrane. Plexuses C5-T1 (Brachial Plexus) = Upper Limbs L2-S2 (Lumbo-sacral Plexus)= Lower Limbs Ventral rami of the spinal nerves (except T2-T12) form network of nerves called plexuses. Convergence of axons of different spinal nerves to form a peripheral nerve Dermatome 31 pairs of spinal nerves are named according to associated spinal vertebra. Each one innervates the skin and musculature of a circumscribed region of the body. Dermatome: the skin area innervated by a given spinal nerve – Important in establishing the location of a lesion to the spinal cord, dorsal root or peripheral nerve. Each spinal nerve also innervates half of the adjacent dermatome too, so a lesion to a single nerve causes a decrease in sensitivity and not a complete loss. Can point to damaged region of the spinal cord pg. 29 Neuroscience and Mental Health · S Tran Peripheral nerve injury or nerve compression may result in complete sensory and mtoor lsos over the area supplied by the nerve Nerve Dysfunction Nerve Conduction Velocity studies can determine whether a peripheral neuropathy is present and whether it’s demyelinating or axonal. Nerve biopsy of a small peripheral nerve (e.g. sural nerve in the leg) can be used to study the pathogenesis of the disease Injury and Compression to the PNS Medial nerve can be compressed & damaged as it passes a narrow tunnel in the wrist wasting of the thumb muscles (carpal tunnel syndrome) Peripheral nerve injury or nerve compression can result in complete sensory & motor loss over the area supplied by the nerve. Examples are: i. Ulnar nerve: lies near the surface of the elbow & is easily damaged wasting of hand muscles and loss of sensation over the little finger. ii. Sciatic nerve: injured in the buttock by badly placed injections paralysis of the foot % loss of sensation over the front and back of the lower leg and foot. PNS neurons have the capacity to regenerate the axon but severity of the damage affects the functional recovery. Regeneration occurs in these stages: 1. After a crush lesion or complete axotomy, the axons and myelin sheath distal to the jury break up within 48h and macrophages phagocytose the axon & myelin debris – Wallerian Degeneration 2. Cell bodies of the neuron undergo metabolic changes known as chromatolysis 3. Proximal axons needs to make contact with Schwann cells & find their former endoneurial sheaths in the distal part. Failure results in a neuroma (trapped nerves) 4. Regeneration of the axons (2-5mm/day) and will reinnervaste their targets within 1 month to over a year. pg. 30 Neuroscience and Mental Health · S Tran Factors that affect recovery are the severity of damage and the distance of regeneration. Diagram summarising the events occurring during axonal degeneration and regeneration following nerve injury: A. Normal nerve. B. One week after axonal damage. Schwann cells containing myelin debris (‘onion bulbs’) are seen surrounding the degenerated axons. Distally, Schwann cells undergo mitosis forming a scaffold for regeneration. C. Axon sprouts begin to regenerate into the distal stump. D. Schwann cells enfold and begin to remyelinate the regenerating axons. E. Connection with the target organ (e.g. muscle) is re-established. Note the contrast in the response of Schwann cells proximal and distal to the lesion. pg. 31 Neuroscience and Mental Health · S Tran Session 7 & 8: ANS Learning Objectives Describe the sympathetic and parasympathetic pathways and their central/spinal connections. Identify the neurotransmitter substances released at different levels within the autonomic nervous system and describe the principal steps involved in their biosynthesis and metabolism. Describe the influence of the sympathetic and parasympathetic nervous system on the principal systems/organs of the body (e.g. cardiovascular system, lung, gut, exocrine glands) and understand the concept of dual innervation and autonomic tone (giving examples). Give an example of an autonomic reflex and describe the principal pathways involved. Classify the cholinoceptors found within the autonomic nervous system and identify the principal loci of (a) the nicotinic cholinoceptors and (b) the muscarinic cholinoceptors. Note that the nicotinic receptors are ion-gated and the muscarinic receptors are G-protein coupled. Identify the principal loci of adrenoceptors in the autonomic nervous system. Classify these -classes and note that they are G-protein coupled. Describe how autonomic activity can be estimated with physiological and biochemical examples. Describe the main abnormalities in autonomic failure differentiating between localised and generalised disorders. Describe the basic anatomy of ANS innervation in terms of pre-ganglionic neurons, ganglia and post-ganglionic fibres. Contrast the anatomical location of sympathetic and parasympathetic ganglia. Describe the thoracolumbar (sympathetic) and craniosacral (parasympathetic) central origins of the ANS. Understand the terms sympathetic trunk, plexus and subsidiary ganglia. Identify the rich sympathetic plexuses that surround the major organs and blood vessels Understand the pre-ganglionic nature of the thoracic and lumbar splanchnic nerves and their synapses in subsidiary ganglia e.g. coeliac ganglion. Understand the importance of the sacral parasympathetic outflow for innervation of structures within the pelvis e.g. the bladder. Identify which of the cranial nerves contain parasympathetic pre-ganglionic fibres. Fig. A1. PRINCIPAL EFFERENT OUTPUTS FROM THE CENTRAL NERVOUS SYSTEM (CNS) CENTRAL NERVOUS SYSTEM AUTONOMIC NERVOUS SOMATIC NERVOUS SYSTEM NEUROENDOCRINE SYSTEM SYSTEM Exocrine glands Skeletal muscle, Growth, Metabolism, Smooth muscle including the Diaphragm and Reproduction, Development, Cardiac muscle Respiratory muscle Salt & water balance, Metabolism Host defence pg. 32 Host defence Neuroscience and Mental Health · S Tran Autonomic Nervous System One of the principle efferent paths of communication between the CNS and periphery Comprises of two fibres: pre-ganglionic and post ganglionic. Can be split into 2 components, anatomically, functionally and neurochemically different. Fig. A2. THE AUTONOMIC NERVOUS SYSTEM SYMPATHETIC PARASYMPATHETIC “Fight and flight” “Rest and digest” Sympathetic Nervous System Prepares the body for responses to a stressful situation The “Fight or Flight” response Key role in the regulation of a number of body functions including blood pressure, body temperature & metabolism. Arises in the thoracic and lumbar regions. Pre-ganglionic are short whereas post-ganglionic are long. Located in a chain close to the vertebral column (paraventerbral ganglia) and also closer to the target tissue (celiac ganglion) Connection allows for mass activation of the sympathetic system. Also includes modified ganglions to the adrenal medulla, which releases it product directly into the blood stream Parasympathetic Nervous System Controls a number of functions in non-stressful conditions i.e. gasto-intestinal motility and secretion Opposes sympathetic system e.g. on heart rate via bronchiolar diameter Arises in the cranial and sacral region of the spinal cord. pg. 33 Neuroscience and Mental Health · S Tran The pre-ganglionic are long whereas the post-ganglionic are short. Parasympathetic ganglia are therefore located in or very close to the target tissue Neurotransmitters Acetylcholine - Choline ester; a charged molecule with a quaternary ammonium group Noradrenaline & Adrenaline – Catechloamines Parasympathetic system are cholinergic – Ach Sympathetic system the pre-ganglionic fibres are cholinergic – Ach Majority of post-ganglionic fibres of the sympathetic system are (nor)adrenergic – NA Adrenal medulla forms part of the sympathetic system: innervated by pre-ganglionic cholinergic fibres which trigger the release of neurohormones ( 80% adrenaline, 20% noradrenaline) into the blood circulation. Chromaffin Cells Some instances, post-ganglionic sympathetic fibres use acetylcholine. Fast transmission. ACh use nicontinic receptors – ligand gated channels. G-protein coupled recptors are used at effector hence are ‘slower’. o Muscarinic receptors – ACh. o Adrenoceptors (α & β) – NA/Adrenaline. pg. 34 ACETYLCHOLINE ACh = acetylcholine Neuroscience and Mental Health · S Tran Biosynthesis, storage and release of Acetylcholine Acetyl Co A + Choline Choline acetyl transferase ACh + Co A ACh A po ctio te n nt ia l Ca++ ACh 4 Choline + Acetate 1 ACh 2 ACh e ras e t 3 es l in o h lc ety Ac Effector cell Receptor Fig. C5: SYNTHESIS, RELEASE, REUPTAKE AND METABOLISM Biosynthesis, storage andOF release of noradrenaline NORADRENALINE Tyrosine Tyrosine hydroxylase DOPA Tyrosine Metabolites DOPA decarboxylase Dopamine Act ion pot ent ial Dopamine Dopamine b hydroxylase Noradrenaline Monoamine oxidase A (MAO-A) Noradrenaline Uptake 1 Noradrenaline Ca ++ Uptake 2 Noradrenaline Adrenoceptor Degredation (COMT) pg. 35 Neuroscience and Mental Health · S Tran FIG. 6: SYNTHESIS, STORAGE AND RELEASE OF ADRENALINE Biosynthesis, storage and release of Adrenaline Tyrosine Tyrosine hydroxylase DOPA Tyrosine DOPA-decarboxylase Dopamine Dopamine Dopamine b hydroxylase Noradrenaline Adrenal medulla chromaffin cell Ca2+ Noradrenaline Phenylethanolamine methyl transferase Adrenaline Adrenaline Adrenaline Ca2+ Adrenaline capillary pg. 36 Neuroscience and Mental Health · S Tran o o Dual Innervations is where an organ is innervated by the sympathetic and parasympathetic branches Opposing systems result in an overall balanced effect. Heart: Sympathetic o Increase force of contraction of cardiac muscles (inotropic effect) o Increase heart rate (chronotropic effect) o Hence increase cardiac output as CO = HR x SV (stroke volume) Parasympathetic - Vagus o Depresses the heart rate from the myogenic 100bpm to 60-70bpm. Vasoconstriction Sympathetic o Arteries and veins but mainly arterioles o Great influence on total peripheral resistance o Increases cardiac output as CO = mBP/TPR o Increases arterial blood pressure (as CO and TPR increased) o During Exercise, stress and activity, when the sympathetic system is dominant it constricts vessels to non-essential organs: kidneys, GI tract and dilates vessels to the skeletal muscle, cardiac muscle, liver and adipose tissue. Parasympathetic Vasodilution Due to decreased sympathetic tone however: o Increased sympathetic activity to some blood vessels (skeletal muscle) which are cholinergic or adrenergic beta receptors cause vasodilation o Local effect of vasodilator such as CO2 and increased [H+], nitric oxide, histamine o Increased parasympathetic stimulation may cause vasodilation to certain blood vessels to discrete glands/organs (e.g. penis) pg. 37 Neuroscience and Mental Health · S Tran Organ/System Effect of sympathetic Effect of parasympathetic Cardiovascular ↑ Increases cardiac output (ionotropic effect SV and chronotropic effect HR); increased TPR ↓vasodilatation (due to decreased sympathetic tone) ↑ - Slows HR; vasodilatation of certain blood vessels to discrete glands and organs (e.g. penis) Gastrointestinal Decreases motility and tone; stimulates contraction of sphincters; inhibits secretory activity Increases motility and tone; relaxation of sphincters; stimulates secretory activity Eye muscles Relaxes ciliary muscle, lens flattens for distant vision; contracts radial muscle (pupil dilation) Contracts ciliary muscle, lens bulges for near vision; contracts pupillary sphincter (pupil contraction) Bladder ↓ Relaxation of the sphincter vesicae (via hypogastric nerve) Main influence; ↑ contraction of detrussor muscle and relaxation of sphincter vesicae (via pelvic nerve) Lungs Penis ↑ Dilates bronchi and bronchioles (↑ O2 delivery) ↑ penile flaccidity; ejaculation ↑ Erection Autonomic Reflexes When nerve impulses pass over an autonomic reflex arc. These reflexes play a key role in regulating controlled conditions e.g. blood pressure, heart rate, force of ventricular contraction, blood vessel diameter, respiration and digestion or even the diameter of the pupil of the eye Cholinoceptors Nicotinic Cholinoceptors o Ligand gated ion channels Fast o At all autonomic ganglia o Found also in the adrenal medulla Muscarinic Receptors o G-Protein coupled Amplification o Found on effector organs with parasympathetic innervations o Also sweat glands of the sympathetic system Adrenoceptors Found on effector cells of the SYMPATHETIC nervous system o Alpha (α) Radial muscle in eye, salivary glands, sphincter muscles of stomach and bladder o Beta (β) Cardiac muscle, smooth muscle or airways, liver. pg. 38 Neuroscience and Mental Health · S Tran Alpha(α)1 and Beta(β)1 produce excitation, whilst α2 and β2 receptors generally cause inhibition. Another type β3 is only found on brown adipose tissue thermogenesis. Effects of the Autonomic System Mass Sympathetic Discharge Alarm & Stress: o Increased arterial blood pressure o Increased blood flow to active muscle (↓ to other areas e.g splanchnic bed) o Increased blood glucose concentration o Increased Respiration o Increased Awareness Acute Stress Reponse: o Tachycardia o Splanchnic Bed Vasoconstriction o Sweating o Pupil Dilation o Increased Metabolic Rate o Increase Glucose o Increased Mental Awareness Autonomic Failure Systemic: Phaeochromocytoma (PCC) (Mass of the chromaffin cells in the adrenals) Causes excessive release of adrenaline and noradrenaline Symptoms: o Headache o Palpitations o Raised Blood Pressure o Tachycardia o Other Adrenergic Effects Localised: Damage to the spine and loss of autonomic functions below that point. Other Pupil Reactions Miosis (Constrict of eye pupil) Parasympathetic Activation: Pilocarpine Mydriasis (Dilation of eye pupil) Blockage of Parasympathetic: Atropine Enteric System In walls of alimentary tract o Myenteric (Auerbach’s) plexus o Submucous (Meissner’s) plexus Sensory – monitoring mechanical, chemical and hormonal activity of gut Motor – gut motility, secretion, vessel tone Can be overridden by sympathetic and parasympathetic systems pg. 39