File
advertisement
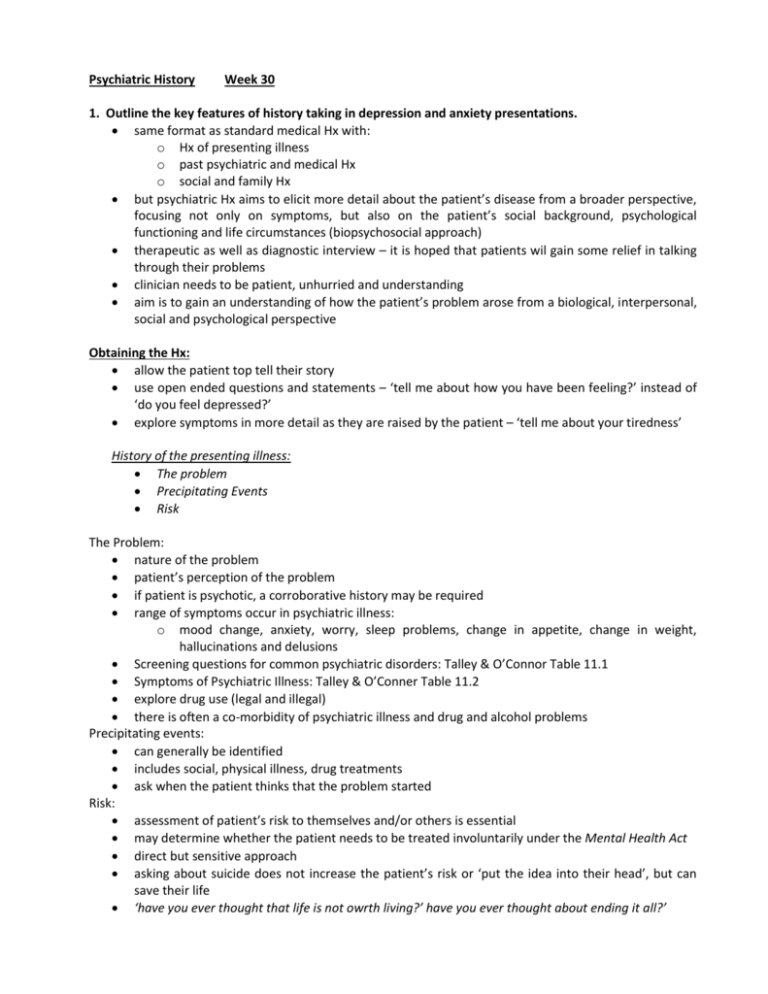
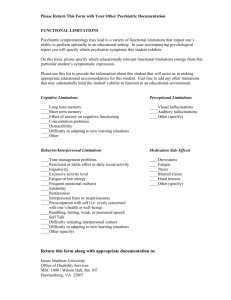
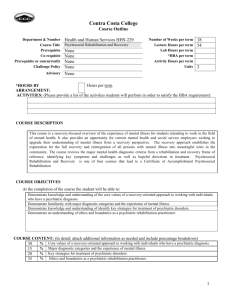
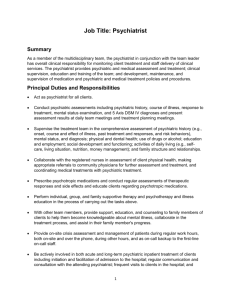
Psychiatric History Week 30 1. Outline the key features of history taking in depression and anxiety presentations. same format as standard medical Hx with: o Hx of presenting illness o past psychiatric and medical Hx o social and family Hx but psychiatric Hx aims to elicit more detail about the patient’s disease from a broader perspective, focusing not only on symptoms, but also on the patient’s social background, psychological functioning and life circumstances (biopsychosocial approach) therapeutic as well as diagnostic interview – it is hoped that patients wil gain some relief in talking through their problems clinician needs to be patient, unhurried and understanding aim is to gain an understanding of how the patient’s problem arose from a biological, interpersonal, social and psychological perspective Obtaining the Hx: allow the patient top tell their story use open ended questions and statements – ‘tell me about how you have been feeling?’ instead of ‘do you feel depressed?’ explore symptoms in more detail as they are raised by the patient – ‘tell me about your tiredness’ History of the presenting illness: The problem Precipitating Events Risk The Problem: nature of the problem patient’s perception of the problem if patient is psychotic, a corroborative history may be required range of symptoms occur in psychiatric illness: o mood change, anxiety, worry, sleep problems, change in appetite, change in weight, hallucinations and delusions Screening questions for common psychiatric disorders: Talley & O’Connor Table 11.1 Symptoms of Psychiatric Illness: Talley & O’Conner Table 11.2 explore drug use (legal and illegal) there is often a co-morbidity of psychiatric illness and drug and alcohol problems Precipitating events: can generally be identified includes social, physical illness, drug treatments ask when the patient thinks that the problem started Risk: assessment of patient’s risk to themselves and/or others is essential may determine whether the patient needs to be treated involuntarily under the Mental Health Act direct but sensitive approach asking about suicide does not increase the patient’s risk or ‘put the idea into their head’, but can save their life ‘have you ever thought that life is not owrth living?’ have you ever thought about ending it all?’ Past History: Family Hx Social and personal Hx Premorbid Hx assess past medical and psychiatric Hx, diagnoses and treatment past suicide attempts Family Hx: familial compnonent to psychiatric disorders explore whether anone in the family has had a mental illness treatment for psycholical problems (incl. drug and alcohol abuse) draw a family tree try and explore family situation that patient grew up in, nature of household, experiences as a child Social and Personal Hx: explore work Hx and support networks living circumstances coping and adapting ability Pre-morbid personality: ask patient to describe themselves, have they noticed a change? explore personality traits Delirium: direct physiological consequence of a general medical condition (substance intoxication or withdrawal, use of medication, exposure to a toxin or a combination of these) characterized by: o confusion o clouding of consciousness may be accompanied by; o poor memory o disorientation o inattention o agitation o emotional upset o hallucinations, visions, illusions, suspiciousness o disturbed sleep Screening questions: what day is it today? how long have you been here? what is the name of the place we are in? do you remember my name? Need to do a MMSE Dementia: chronic brain syndrome generalized impairment of intellect, memory and personality with no impairment of consciousness characterized by: o loss of memory (esp short term) o loss of orientation o deterioration in social functioning and behaviour and emotional control (may be easily upset, tearful or irritable) screening questions as for delirium need to perform a MMSE 2. Outline the components of the mental state history and examination. Mental state exam is part of the total process of assessing the patient and is not something that is done at the end of the history while taking the Hx, make observations about: o patterns of speech o attitude o way of interacting o unsusual behaviours o thought patterns o emotional state General description: o appearance o behaviour o attitude Mood and affect: o appropriateness o speech o perceptual disturbances thought, form and content sensorium and cognition o alertness and level of consciousness o orientation to time, place and person o short term memory o long terme memory o concentration o general knowledge judgment and insight more formal assessment with scoring system out of 30 (see Talley and O’Connor table 11.5) MMSE