Butterwick Hospice Care
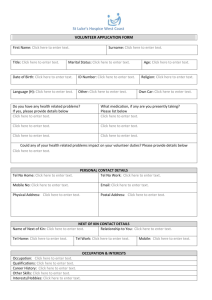
advertisement

Butterwick Hospice Care Butterwick Adult Hospice Stockton on Tees Quality Account 2013-2014 Butterwick Hospice Middlefield Road Stockton on Tees TS19 8XN Registered Charity 1044816 Our Mission Statement and Philosophy Why we are here We aim to improve the quality of life for those who have a progressive life limiting illness and those close to them and to offer positive support for every challenge they may encounter during their illness and to see death as part of life’s journey. In particular we will: Provide supportive and specialist palliative care for adults with progressive life limiting conditions Ensure each person receives care in a homely environment whilst maintaining privacy, dignity and choice. Provide holistic centred care by responding to and respecting the patient and those close to them by meeting their individual, physical, social, cultural, educational, spiritual and emotional needs throughout the illness and bereavement. Acknowledge and respect the way those close to the patient care for them and endeavour to continue their chosen pattern of care. Work together in developing an environment based on support and mutual respect. Maintain the high quality of the service through ongoing reflection, evaluation and education. Communicate effectively and efficiently both within the Hospice and with external agencies, to ensure continuity of care and promote service development. Part 1: Chief Executive’s Statement It gives me great pleasure to present the second Quality Account for the Butterwick Adult Hospice, Stockton on Tees. The Hospice is an integral part of Butterwick Hospice Care (registered charity 1044816) which provides services from three separate Hospices in the North East of England. All of the Hospices’ services are provided totally without charge to our patients and their carers. The day to day management of the Butterwick Adult Hospice, Stockton on Tees clinical services is under the leadership of Mrs Carole Harrison who is designated the Registered Manager in the Hospice’s registration with the Care Quality Commission. The Butterwick Hospice endeavours to provide an excellence in evidence based palliative care for all patients regardless of age or diagnosis; to be a centre of expertise and a specialist resource within the community as a whole. The needs of patients and their carers are paramount to the Charity’s existence and are the root and focus of all we do. Quality is at the core of the Charity’s strategic and operational priorities. An independent impartial assessment of the quality of care provided was obtained when the Care Quality Commission performed a routine unannounced inspection of the Hospice on 28th August 2013. Their Report showed that the Hospice was meeting all of the required standards. A copy of their full Report is available at : www.cqc.org.uk/directory/1-113000508. During the last year we have worked effectively in partnership with the Hartlepool & Stockton on Tees Clinical Commissioning Group and other partners for the benefit of the community we freely serve. In the year the Hospice has achieved the Commissioning for Quality and Innovation (CQUIN) outcomes detailed in the 2013/14 Contract with NHS Tees. The Charity only achieves its key objectives because of the professional skills, commitment and enthusiasm of our staff and volunteers I am responsible for the preparation of this report and its contents. To the best of my knowledge, the information reported within this Quality Account is accurate and a fair representation of the quality of healthcare provided by our Hospice. Graham Leggatt-Chidgey Chief Executive May 2014. Part 2: Priorities for improvement and statements of assurance from the board (in regulations) 1. IMPROVEMENT Within the Organisation, quality is fundamental to improvement and accountability. The Board of Trustees continues to support and promote the ongoing development and improvement of services to ensure that the care and support provided evolves to meet patient and carer needs. The priorities for quality improvement for 2014/15 are set out below. These priorities have been identified in conjunction with patients, carers, staff and stakeholders. The priorities we have selected will impact directly on each of the three priority domains: Patient safety Clinical effectiveness Patient experience Part 2 Priorities for improvement 2014-2015 and Statements of assurance from the Board (in regulations) Section 2.1 Priorities for improvement 2014-15. Patient Safety Priority One Formalise regular education sessions for clinical staff as part of the Palliative Care Consultant sessions at the Hospice. How was this identified as a priority? Following the successful appointment of a Palliative Care Consultant at our neighbouring Trust and the formalising of the three consultant sessions to the hospice, we were keen to ensure that the three sessions were used as effectively as possible to benefit patients and staff. As we were developing services within the adult hospice which included caring for patients with more complex palliative care needs and undertaking additional procedures, we believed it was important to use one of these sessions for the education of staff which would ultimately benefit patients. How will Priority One be achieved? Fortnightly education sessions lasting one hour take place between 2-3pm either within the sitting room area on the in-patient unit or in the education room, depending on the subject and if any resources are required. This time slot is when the morning and afternoon shift are both on duty, thereby enabling more staff to benefit from the sessions. The topics covered are influenced by experience on the unit where a case review may be discussed or a topic identified by staff to meet specific interest or need. Staff are also encouraged to participate in these sessions which may include facilitating a group discussing an article they have read or an issue that is very relevant to the palliative care national or local agenda. How will progress be monitored and reported? Attendance at sessions is recorded in the hospice’s training book and entered onto the training database. All sessions are evaluated and the evaluations are sent to the Quality and Practice Development nurse. Participation by staff e.g. by leading a session will be discussed in staff’s annual Individual Development Review (IDR) and encouraged as part of staff development. These sessions will help staff develop skills and confidence in relation to complex management of patient symptoms, help them cope with difficult situations and challenges through case reviews and offer opportunities for staff to develop skills in facilitating groups and presenting. We expect to notice changes in individual staff in regards to their coping strategies and confidence and this will be monitored by the Clinical Lead within the area of practice. 2b Clinical Effectiveness Priority Two Introduction of a Breathlessness Support Programme How was this identified as a priority? In response to an invitation for non –recurrent funding applications, a neighbouring hospice proposed a programme for patients with heart failure and Chronic Obstructive Pulmonary Disease. As this proposal was discussed further with the CCG, the programme developed into a support programme for patients with long term and progressive pulmonary conditions. The CCG were keen to provide equality of service over the whole of Tees and Hartlepool and therefore Butterwick Hospice were asked if they could provide an equivalent service in the Stockton area. In their 2010 publication relating to the management of Chronic Obstructive Pulmonary Disease in adults in primary and secondary care, the National Institute for Health and Clinical Excellence stated an estimated 3 million people have COPD in the UK and recognised that these patients require support from various members of the multidisciplinary team. (NICE. June 2010). Whilst this is a significant number of patients we must also acknowledge that breathlessness can be related to other cardiac and pulmonary conditions. This programme is to therefore help meet the needs of these patients by establishing a support service for patients who have symptoms of breathlessness related to a progressive non-cancer diagnosis e.g. COPD, Emphysema, pulmonary fibrosis and by doing so, also provide a support network for their carers. The vision of the Clinical Commissioners for Hartlepool and Stockton-On-Tees is to improve health care by involving service users, carers, staff, providers, partners and the public to develop services and reduce health inequalities by working in partnership to transform services. The Joint Health and Wellbeing Strategy for Stockton-On-Tees 2012-2018, recognises the need to “Enhance the quality of life for people with Long Term Conditions” and to “increase primary and community services to support care closer to home and enable independent living”. (JSNA 2012) The programme embraces the challenges of health care provision and aims to work within local strategy requirements to provide safe, high quality, cost effective care. Many patients experience increased breathlessness for various reasons throughout their illness progression. These symptoms are extremely distressing for the patient and also traumatic for the carer involved in supporting the patient. Patients are often cared for by members of their own family who may not have any experience in health care. Carers often state that the worst thing is not being able to do anything to help the patient when these exacerbations occur. This can often lead to patients or carers contacting emergency services and patients being admitted to hospital who could perhaps have remained at home given the appropriate support. The programme therefore focuses on helping patients recognise and identify the triggers which contribute to their exacerbations of breathlessness, develop coping strategies and selfmanagement skills to enable them to cope at these times. The overall aim is to reduce the patient’s dependency on out of hour’s community resources as well as reducing the number of inappropriate admissions to the acute sector. How will priority two be achieved? A key objective of the programme is to work alongside other care providers in primary and secondary care to support patients and their carer’s in the self-management of ongoing symptoms throughout their disease progression. In order to provide equitable care across the commissioning locality, referral criteria are identical across the Hartlepool and Tees area and the aims and objectives of the programme are mirrored across both Butterwick and Hartlepool Hospice. Referral criteria were agreed and a specific referral form formulated. A series of joint meetings have taken place with our neighbouring hospice as well as several meetings between staff at Butterwick Hospice, Community Matron and Respiratory Specialist Nurse. Core objectives of the programme are to: Provide an integrated support service working in collaboration with primary and secondary care. Provide patients with self-management tools. Increase social inclusion and peer support. Deliver an innovative high quality service. Signposting to other appropriate services. The programme consists of: 1 2 2 1 day per week of specialist day services for 6 weeks. individual and 2 group counselling / psychotherapy sessions. complementary therapy sessions complementary therapy session for patient’s main carer. In addition during the 6 week programme patients will experience and have access to: Weekly relaxation session Weekly Tai Chi session Access to diversional activities such as creative writing One to one advice and support from nursing staff during weekly sessions Benefits advice Bespoke support for smoking cessation and medicine management where applicable to patients Carers will have access to tuition in providing hand or foot massage The majority of patients will be identified and referred to the service by the Respiratory Specialist Nurses at University Hospital of North Tees (UHNT) and the Community Matrons who will be able to identify patients who could benefit from this programme and who may already have had hospital admissions for anxiety related breathlessness or may have the potential to do so. Following the structured 6 week period the patients will be referred back to the original referrer. Non –recurrent funding from the CCG has enabled this 12 month pilot programme to take place and will be evaluated in regards to continuing funding after the 12 month pilot. How will progress be monitored and reported? The service will be audited/evaluated quarterly using recognised audit tools to identify patient and carer benefits and any areas for improvement. i.e. Key Performance Indicators determined by the clinical commissioners. Patient/Carer feedback in the form of a questionnaire. (MYCAW, Family & Friends Test) Referrer feedback questionnaire. The findings of audit and evaluations will be used to drive the service forward throughout the programme. Quarterly reports will be sent to the CCG in addition to patient and carer evaluation feedback following each 6 week programme. 2c Patient Experience Priority Three Establish a service user advisory group How was this identified as a priority? We are aware that patient or service user groups have been established in the acute sector for some time and also that other hospices have successfully created groups of carers/service users which have been very beneficial in providing a patient/user perspective on services provided, new services being developed and information being provided to people using the services. Nationally it is seen as good practice to involve patients or carers in these discussions and many organisations have a patient or carer representative attending multi-disciplinary meetings. We have discussed the value of having our own service user group in several clinical meetings but were aware of the difficulties in finding suitable representatives due to the nature of the service where patients may be too poorly to contribute or may have a short life expectancy and would be difficult to establish continuity for the group. Following our stakeholder questionnaire last year, valuable comments were received in regards to what the professionals thought would be beneficial for their patients, both in regards to types of services provided, activities offered within the Day Care setting and whether the taboo surrounding hospice care prevented many patients attending and benefitting from the services offered by the Hospice. We have developed new services over the last few months which have required patient leaflets as well as information for professionals to be designed and developed and believe that a specific service user group would be particularly beneficial when developing these; especially regarding the language and terminology we so often use and take understanding for granted. We therefore decided that in order to benefit from the direct views of the people actually using our services or we would make this one of our priorities for 2014/15. How will priority three be achieved? We will consult with other hospices who have successfully established a similar group. We will also formulate and agree terms of reference for the group in order that the group will have a clear purpose and aims. As part of our patient/user satisfaction surveys we will ask for interested parties to express their interest. In September we plan to hold an open event for the public which will enable people to have a tour, view the facilities, learn about the services available and during this event we will have information available about the service user group and enable them to express interest in joining this representative group. How will progress be monitored and reported? The recruitment of suitable representatives will be a key achievement. The group will meet with and feedback to the Director of Clinical Services at regular intervals. Key projects which the group should be involved in and any leaflets which require to be formulated will be identified at the monthly meeting of Clinical Managers which are minuted. Group members will be asked to evaluate the group’s activities in respect of the objectives laid out in the Terms of Reference annually. Section 2.2 Review of services During 2013/14 the Butterwick Adult Hospice at Stockton on Tees provided three key services: To provide a 24 hour, 7 days a week in-patient service. To provide a day hospice service four days each week (Tuesday to Friday). To provide nursing, medical care, counselling, advice, complementary therapies and bereavement support to patients, their carers and relatives. The Butterwick Adult Hospice at Stockton on Tees has reviewed all the data available to us on the quality of care in all of the above services. The income generated by the NHS services reviewed in 2013/14 represents 100% of the total income generated from the provision of NHS services by the Butterwick Adult Hospice, Stockton on Tees for 2013/2014. The income generated from the NHS represents approximately 28% of the overall patient care costs incurred by the Hospice. Section 2.3 Participation in Clinical Audits, National Confidential Enquiries During 2013/14 no national clinical audits and no national confidential enquiries covered NHS services relating to palliative care. During that period Butterwick Adult Hospice, Stockton on Tees, participated in no national clinical audits and 0% national confidential enquiries of the national clinical audits and national confidential enquires. The Butterwick Adult Hospice, Stockton on Tees only provides palliative care therefore were ineligible to participate. The following mandatory statements are therefore not applicable to Butterwick Adult Hospice Stockton on Tees: “The national clinical audits and national confidential enquiries that [name of provider] was eligible to participate in during [reporting period] are as follows: [insert list].” “The national clinical audits and national confidential enquiries that [name of provider] participated in during [reporting period] are as follows: [insert list].” “The national clinical audits and national confidential enquiries that [name of provider] participated in, and for which data collection was completed during [reporting period], are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. [Insert list and percentages].” “The reports of [number] national clinical audits were reviewed by the provider in [reporting period] and [name of provider] intends to take the following actions to improve the quality of healthcare provided [description of actions].” Following attendance at a Help the Hospice’s Quality and Audit event during 2013/14, we decided to participate in the National Hospice in-patient safety benchmarking pilot. The audit focuses on patient falls, pressure ulcers and medication incidents. Following the gathering of data from approximately 100 hospices we expect to receive the first report from Help the Hospices in the next few weeks. Local Clinical Audit and Service Improvement Butterwick Adult Hospice undertakes a series of audits in accordance with Butterwick Hospice Care’s comprehensive annual audit programme. The audit programme includes nationally validated audits from Help the Hospices where available, internally designed audits and external infection control audits in line with the Service Level Agreement with our local NHS Trust. Some examples of these audits, undertaken in the Adult Hospice during 2013/14, are included in this report on the following pages. Record Keeping Audit Introduction Record Keeping is integral to nursing care. It is essential that good standards of record keeping are established and maintained. The audit tool is to be used for auditing standards of record keeping across all sites and services offered by Butterwick Hospice Care. It is divided into generic and service specific sections. Part A is generic and to be completed for all services. The other sections contain criteria which are specific to individual services and the relevant section is to be completed in addition to the generic section. The form can audit details of up to 8 patient records. The number of records auditing will be appropriate to the service. Criteria The assessment is made using the entries recorded in the last 3 months or on last admission if this is longer than 3 months. Results 6 sets of notes were audited covering 27 criteria. Out of the 6 sets of notes 19 of the criteria were met and 3 were almost met. This leaves 5 of the criteria not met. The following points were identified: UNMET CRITERIA All set of notes had entries that had not been timed. All entries must be timed as this is the proof that the entries are chronological. All sets of notes some of the entries did not include the designation of the person making the entry. All entries must include the designation of the person making the entry. Not all of the sheets had the patients Palcare number recorded on each sheet. This was evident in all 6 sets of notes. The palcare number must be recorded on each separate sheet. Not all of the staff had signed the sample signature sheet. Any clinical member of staff making an entry in the patient’s notes must complete the sample signature sheet. ALMOST MET CRITERIA Any alterations to the text should be scored out with a single line, dated and signed. Most staff do score out alterations and initial the change, but we must sign and date any alterations in order to meet the criteria fully One set of notes did not have the patient’s preferred name documented. It is important that this information is recorded. One of Sample signature sheets did not have the patients palcare number recorded BUTTERWICK HOSPICE CARE RECORD KEEPING AUDIT TOOL This audit tool is to be used for auditing standards of record keeping across all sites and services offered by Butterwick Hospice Care. It is divided into generic and service specific sections. Part A is generic and to be completed for all services. The other sections contain criteria which are specific to individual services and the relevant section is to be completed in addition to the generic section. This form can audit details of up to 8 patient records. The number of records auditing will be appropriate to the service. It may be necessary therefore to use two sheets in areas where a greater number of patients use the service. Please enter PAL number of the record being audited where indicated and tick yes or no under the relevant column. When scoring the criteria use entries made in the last 3 months or on last admission if this is longer than 3 months. * Criteria 6 & 7:- NMC guidelines (July 2009) state that printed name and designation need only be stated after the first entry. However, within Butterwick Hospice Care, if the patient record consists of separate sheets it is recommended that the printed name and designation should be entered after the first entry on each separate sheet and this is the standard to be assessed. Dept/Service In-Patient Unit Date of audit Person(s) completing audit 16/10/2013 Lesley Blakemore. Quality & Practice Development Nurse PART A GENERIC (To be completed for all record keeping audits) Pal No. of record 20130174 20130191 Criteria Yes No Yes No A1 All entries are in black ink √ √ A2 All entries are dated √ √ A3 All entries are timed X X A4 All entries use the 24 hour clock or √ √ clearly state am or pm A5 All entries are signed with full √ √ signature (where space allows) or initials (where space is restricted). A6 Name of person making entry is X X printed next to the signature. (* see 20130051 Yes No √ √ X √ 20130096 Yes No √ √ X √ 20130218 Yes No √ √ X √ 20130195 Yes No √ √ X √ √ √ √ √ X X X X Yes No TOTALS Yes No YES NO 6 0 6 0 0 6 6 0 6 0 0 6 Pal No. of record Criteria note above) A7 The designation of person making the entry is stated after the signature. (*see note above) A8 Patients name is on all documentation sheets. A9 Patient’s PAL number is stated on all documentation sheets. A10 All entries are legible. A11 All alterations are scored out with a single line, dated and signed. A12 There are no gaps between entries. A13 All entries are in chronological order. A14 Irrelevant, speculative, offensive or subjective statements are not used. A15 Highlighter pen is not used. A16 An up-to-date sample list of signature and initials with staff name and designation is included in the patient’s records. A17 Sample signature list states the name and PAL no. of the patient to which the sheet refers. A18 Patient’s preferred name is documented. A19 A risk assessment is identified in the patient’s care plan where indicated. A20 Where a risk assessment is identified, this is completed and contained in the patient 20130174 Yes No 20130191 Yes No X √ X √ X √ 20130051 Yes No 20130096 Yes No X √ X 20130218 Yes No X √ X 20130195 Yes No X √ X X √ X X Yes No TOTALS Yes No YES NO 0 6 6 0 0 6 √ √ √ √ √ √ √ √ √ √ 6 5 0 1 √ √ √ √ √ √ √ √ √ √ √ √ 6 6 0 0 √ √ √ √ √ √ 6 0 √ √ √ √ √ √ 6 0 0 6 X X X X X X X √ X √ √ √ √ 5 1 √ X √ √ √ √ 5 1 √ √ √ √ √ √ 6 0 √ √ √ √ √ √ 6 0 Pal No. of record 20130174 Criteria Yes No documentation. A21 All entries are signed or √ countersigned by a qualified practitioner. A22 Where abbreviations are used, there √ is a sheet explaining what these mean. B1 B2 B3 B4 B5 B6 Is an ‘active decisions’ sheet completed? Have ALL sections of the in-patient information sheet been completed and signed? Has the Braden Scale been completed and reviewed as directed. Have ALL sections of the patient profile been completed? Have ALL sections of the PAL care form been completed and evidence of details being checked? Catheter care. If applicable: Has the overnight drainage bag been changed in accordance with best practice. 20130051 Yes No 20130096 Yes No 20130218 Yes No 20130195 Yes No √ √ √ √ √ 6 0 √ √ √ √ √ 6 0 √ √ √ √ √ √ 6 0 √ √ √ √ √ √ 6 0 √ √ √ √ √ √ 6 0 √ √ √ √ √ √ 6 0 √ √ √ √ √ √ 6 0 n/a n/a n/a n/a n/a n/a 0 0 RESULTS: TOTAL COMPLIANCE A-GENERIC B-IN-PATIENT UNIT C-CHILDREN’S UNIT COLLATED BY: TOTALS Yes No YES NO 20130191 Yes No PERCENTAGE 75% 100% N/A LESLEY BLAKEMORE Quality and Practice Development Nurse. SIGNATURE: Lesley Blakemore Yes No COMMENTS AND ACTION PLAN FOLLOWING A RECORD KEEPING AUDIT This form is to be completed following each record keeping audit. Please give comments where appropriate where criteria are not fully met and complete action section to show how your department aims to increase the level of achievement for the specific criteria. Please send a copy of your results to the Quality and Practice Development Nurse for monitoring purposes and collation into the organisation’s audit log. Dept/Service Completed by: Signature Criteria No. A3 A6 A7 A9 A11 A16 In-Patient Unit Lesley Blakemore Comments 6 sets of notes had entries that did not indicate the time they had been written. 6 sets of notes did not have the name of the person making the entry. 6 sets of notes did not have the designation of the person making the entry. 6 sets of notes did not have the pal care number on all of the sheets Not all alterations were signed and dated. All alterations were crossed out legibly and initialled but not signed and dated as required. Not all of the staff signed the sample signature sheet. Date of audit to which this sheet relates. 16/10/13 Name and Lesley Blakemore Designation Quality & Practice Development Action Plan By whom By when A memo will be circulated to remind all staff that any entries must be timed. This criteria will be discussed at the documentation group. A sample signature sheet is used within the notes. A memo will be circulated to remind all staff that they must include their designation when making any entry into the notes A memo will be circulated to remind all staff that each of the sheets must have the patients palcare number recorded. A memo will be circulated reminding staff of the correct process for alterations Lesley Blakemore Lesley Blakemore 25th October 2013 A memo will circulated to remind all clinical staff of the need to complete the sample signature sheet. Lesley Blakemore 25th October 2013 25th October 2013 25th October 2013 Lesley Blakemore 25th October 2013 Lesley Blakemore 25th October 2013 Lesley Blakemore Criteria No. A17 A18 Comments 1 set of notes did not have the patients Palcare number recorded on the sample signature sheet. 1 set of notes did not have the patients preferred name documented. Action Plan A memo will be circulated to remind all staff that the patients Palcare number must be recorded on the sample signature. A memo will be circulated to remind all staff that the patients preferred name must be recorded. By whom By when 25th October 2013 Lesley Blakemore 25th October 2013 Lesley Blakemore BUTTERWICK HOSPICE CARE MEDICINE KARDEX AUDIT TOOL This audit tool is to be used for auditing the standards of medication prescribing and completion of Medicine Kardex within the In- Patient Unit. The tool is based around Sub Topic 4 of the Help the Hospices National General Medicines Audit tool and tailored around the medicine kardex used by the organisation. This form can audit up to 6 kardex’s. The number of kardex’s audited will be appropriate to the number of patients in the unit at the time of the audit. TITLE OF AUDIT. MEDICINE KARDEX Audit undertaken by:- Name and Designation Lesley Blakemore Dept/Site to which the audit relates IN-PATIENT UNIT Date of audit 16/10/13 SIGNATURE: Quality & Practice Development Nurse Number of Kardex’s 6 Pal care No of audited. Kardex Criteria: 1 Patient information. 1.1 The name of the patient? 1.2 Date of birth of the patient? 1.3 Hospice number of the patient? 1.4 Information on any known allergies or hypersensitivities? Criteria: 2 Regular medicines prescribed have the following 2.1 Name of medicine using the generic or brand name as appropriate? 2.2 Dose of medicine? 20130174 20130191 20130096 2013051 20130218 20130195 TOTALS Yes Yes No Yes No Yes No Yes No No √ √ Yes No YES NO n/a 6 6 4 6 0 0 2 0 0 0 0 0 √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ 6 0 0 √ √ √ √ √ √ 6 0 0 X X 2.3 2.4 2.5 2.6 2.7 Date of prescribing? Weight of patient where the dosage of medication was related to weight? Route of administration of medicine? Frequency for administering each dose? Time for administering each dose? Number of Kardex’s audited. 2.8 2.9 6 Pal care No of Kardex √ n/a √ n/a √ n/a √ n/a √ n/a √ n/a 6 0 0 0 0 6 √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ 6 6 6 0 0 0 0 0 0 20130174 20130191 20130096 2013051 20130218 20130195 TOTALS Yes √ √ Yes √ √ No Yes √ √ No Yes √ √ No Yes √ √ No No Yes √ √ No YES NO n/a 6 0 0 6 0 0 2.1 3.2 3.3 Signature of prescriber? Information on any known allergies or hypersensitivities? Any special requirements/instructions? As required (PRN)/ Variable doses prescribed have the following: Name of medicine Dose of medicine Route of administration of medicine 3.4 3.5 Signature of prescriber Date of prescribing √ √ √ √ √ √ √ √ √ √ √ √ 6 6 0 0 0 0 3.6 Frequency/Instructions √ √ √ √ √ √ 6 0 0 Criteria: 4 Each prescription is: Written clearly (handwritten or preferably computer generated)? Indelible (handwritten or preferably computer generated)? Entries for replaced prescriptions are deleted clearly, preferably as a strikethrough to avoid duplication of medication. √ √ √ √ √ √ 6 0 0 √ √ √ √ √ √ 6 0 0 √ √ √ √ √ √ 6 0 0 2.10 Criteria: 3 4.1 4.2 4.3 √ √ √ √ √ √ 6 0 0 √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ 6 6 6 0 0 0 0 0 0 RESULTS: TOTAL COMPLIANCE CRITERIA 1 CRITERIA 2 CRITERIA 3 CRITERIA 4 COLLATED BY: PERCENTAGE 91% 100% 100% 100% LESLEY BLAKEMORE Quality and Practice Development Nurse. SIGNATURE: Lesley Blakemore PATIENT SATISFACTION SURVEY 2013/14 Which Service was used % 100 80 60 40 79 20 21 0 0 0 0 Day hospice Bishop Auckland Outreach at Sedgefield Outreach at Stanhope 0 0 In patient unit stockton Day hospice stockton Outreach at Barnard Home Care Durham Castle Dales Impressions very satisfactory Satsified somewhat satisfied very dissatisfied Not Applicable 100 80 60 40 82 91 87 92 85 84 94 92 78 3 00 4 4 00 4 Overall impression of the hospice 13 0 0 9 Staff Attitude 6 00 9 Patient information 6 0 010 Regular handwashing or using hand gel by staff 3 00 5 Explanation of facilities 4 00 5 The cleanliness of the hospice 5 00 8 The hospice facilities Reception area and greeting 8 0 010 0 Did you feel safe 20 Were you offered Complementary Therapy? 100 80 60 95 40 20 1 4 No No answer 0 Yes How beneficial did you find this? 100 80 60 40 67 20 14 0 0 19 Satisfied Somewhat Satisfied Very Dissatisfied Not applicable 0 Very Satisfactory How well did we communicate information to you? Very Satisfactory Satisfied Somewhat Satisfied Very Dissatisfied Not applicable 100 80 60 75 66 57 51 9 0 0 25 11 0 1 11 1 0 30 Communication with you carers/family 6 0 0 23 Involvement in decisions making Before you arrived 0 13 0 0 13 Explaining you treatments 19 1 0 19 37 During you stay 20 71 61 On your first visit 40 Catering how well did you rate it? Very Satisfactory Satisfied Somewhat Satisfied Very Dissatisfied Not applicable 100 80 60 78 82 82 85 90 85 40 20 13 1 0 8 15 1 0 1 13 0 0 5 8 1 0 6 9 0 0 6 8 0 0 3 0 The quality of Menu variety Presentation the food and choice Prompt service Correct orders Overall impression of catering services Our Nurses were they professional and understanding? Very Satisfactory Satisfied Somewhat Satisfied Very Dissatisfied Not applicable 100 80 60 92 87 77 75 40 53 44 20 4 0 0 19 3 0 0 23 3 0 0 1 0 0 6 76 11 1 0 0 11 0 0 13 0 Were you treated with respect? When you Was your privacy requested pain and diginity relief was it timely? maintained? Were your Did you feel Overall impression questions supported with any of the nursing care answered to your emotional issues? satisfaction? How satisfied were you with other team members? Very Satisfactory Satisfied Somewhat Satisfied Very Dissatisfied Not applicable 100 80 92 60 85 81 40 54 53 20 38 5 0 0 14 6 0 0 9 5 1 1 44 52 43 1 0 0 6 4 0 0 4 0 0 Doctors Family support team 0 Catering staff Complementary Therapist Chaplain Day Hospice Volunteers 100 80 60 40 58 20 65 56 43 37 71 65 59 34 30 29 28 5 0 0 1 0 0 4 1 0 6 0 0 8 0 0 0 0 0 Housekeeping In-patient volunteers Maintenance Team Physiotherapists Reception team Volunteer drivers 0 Additional patients or carer comments from survey in regards to their experiences IPU If you would like to mention any particular members of staff or volunteers who you feel have provided an especially good service, please do so below. “Think everyone were excellent and provided a good service.” “All very good” Butterwick Hospice strives to provide the best of care to patients and carers. Is there anything the hospice could have done better to improve or enhance the care you received? “No” “No, all care has been second to none, excellent!” Please provide any further comments or suggestions concerning your visit or stay at the hospice. “Would perhaps be nice - I would find it helpful to have a small shelf close to hand basin to put toothpaste etc on.” Day Care Stockton If you would like to mention any particular members of staff or volunteers who you feel have provided an especially good service, please do so below. “All staff and volunteers could not have provided better service.” “XXXXX the volunteer driver is really caring and gives me confidence in the ambulance” “Aromatherapist XXXX is always helpful and gives us excellent attention” “XXXX nurse” “XXX and XXX exceptional people” Butterwick Hospice strives to provide the best of care to patients and carers. Is there anything the hospice could have done better to improve or enhance the care you received? “Fully Satisfied.” Please provide any further comments or suggestions concerning your visit or stay at the hospice. “We, as a family have been very happy with xxxx’s care and cannot fault anything. Thank you” “Everyone concerned with my care has been most helpful and caring. Every visit is thoroughly enjoyable and beneficial.” “Haven’t been coming long enough to pass comment on staff individually” “I live for a Wednesday, absolutely love my visits.” Research The number of patients receiving NHS services provided by or sub contracted by the Butterwick Adult Hospice Stockton on Tees in 2013-2014 that were recruited during that period to participate in research approved by a research ethics committee was: none. Butterwick Hospice Care’s current policy is that we do not undertake primary research within the hospice. Section 2.4 Use of the CQUIN payment framework A proportion of Butterwick Adult Hospice’s income in 2013/14 was conditional on achieving quality improvement and innovation goals agreed between Butterwick Hospice Stockton and NHS Tees, through the Commissioning for Quality and Innovation payment framework.” “Further details of the agreed goals 2013/14 and for the following 12 month period are available electronically at [N/A]” Section 2.5 What others say about us Statements from the CQC Butterwick Adult Hospice, Stockton on Tees is required to register with the Care Quality Commission and its current registration status is: Diagnostic and screening procedures Treatment of disease, disorder or injury Transport services, triage and medical advice provided remotely Butterwick Adult Hospice, Stockton on Tees has the following conditions on registration:Conditions:‘The Registered Provider must ensure that the above regulated activities are managed by an individual who is registered as a manager in respect of this location.’ “The Care Quality Commission has not taken enforcement action against Butterwick Adult Hospice, Stockton on Tees during 2013/14. Butterwick Adult Hospice, Stockton on Tees has not participated in any special reviews or investigations by the CQC during the reporting period. The Butterwick Hospice is subject to periodic reviews by the Care Quality Commission and its last review was July 2013 The Butterwick Hospice was fully compliant and rated as low risk following assessment by the Care Quality Commission. We have included some comments from our last inspection below. Selection of comments from the last CQC compliance assessment:We saw that staff were attentive and treated patients with dignity and respect. Staff responded quickly when patients called for help. We saw that staff communicated well with people and explanations of care were given in a way that could be easily understood. One patient said, "The doctors are brilliant, they fully explained things in a way we understood." "Privacy and dignity are well respected and I feel safe and secure." One person who had been admitted for symptom control said, "Within two days of being here they had my pain under control." Another person said, "They explained the number of ways to manage my pain, I was consulted and agreed the treatment plan." They said that for the first time in a long time they had woken up pain free. The environment was calm and relaxed. One patient said, "It is so peaceful." They also described the staff as, "Absolutely fabulous staff, they are so compassionate and understanding." "Nothing is ever a problem, they are so reassuring." The two patients we spoke with and relatives commented that the hospice was always clean. One patient said, "The cleaners are in a couple of times a day." Another patient said, "It is immaculate." Within the hospice there was also the involvement of various disciplines in providing people with treatment, therapy and care. This included the involvement of complimentary therapists and physiotherapists. The patients we spoke with confirmed that other professionals were involved in their care. Both patients said that during their admission to the hospice they had been visited by their Macmillan nurse, district nurse or social worker. The full compliance report can be viewed at www.cqc.org.uk . Stakeholder survey 2013/14 A key objective of the Hospice Business Plan for 2013/14 was to survey our stakeholders regarding the adult services currently offered by the Hospice in Stockton, particularly those who refer, or could, refer patients to us. The aim being to identify if our services effectively meet the needs of their patients, explore some ideas for how we could develop or change services to benefit more patients and enable us to make the most effective use of our resources including the Hospice’s expertise. Although the response rate was low (16%) we received some interesting results and valuable feedback across a range of stakeholders including a good representation of GP’s. Several of the findings have now been incorporated into the business plan for 2014/15 and several of the actions contained in the report have now been completed. A copy of the full report can be found below. The Views of Stakeholders into the services provided by Butterwick Hospice Stockton Results of the October 2013 stakeholder questionnaire Carole Harrison Director of Clinical Services Butterwick Hospice Care February 2014 Contents Page Introduction 2 Section 1: Questionnaire and Sample 3 Section 2: Responses Knowledge of current services 3 Individual referral trends and reason for referrals 4 Views on Day Care services 4-6 o Current service and model 4-5 o Potential changes 6 o Accessing Day Care services 5 Views on additional services/opportunities 5-6 In-patient services 6-7 o Views on potential opportunities 6-7 o Blood Transfusion at the hospice 7 Community Services 7-8 Telephone advice 8 Outpatient services 8 Support to nursing and residential homes 9 Open day events 9-10 Additional ideas and comments from respondent 10 Section 3: Recommended Actions Section 4: Opportunities for service development 11 11 11 References Introduction The provision of palliative and end of life care has faced many challenges in recent years and continues to do so. It is therefore essential that hospices are able to anticipate and meet the changing and growing needs of the community they serve. (Help the Hospices Commission 2013). A key objective of the Butterwick Hospice Business Plan for 2013/14 was to find out the views of our stakeholders into the services currently offered by Butterwick Hospice at Stockton and to identify whether our services were meeting the needs of their patients, explore some ideas for how we could benefit more patients and to maximise the use of resources and hospice expertise. Section 1: Questionnaire and Sample It was important to us that we were to gain valuable and meaningful information which would play a significant role in helping us shape our services for the future, therefore the questionnaire was designed to enable us to gain qualitative and quantitative data. We wished to be able to identify the designation or area of work of respondents so that we could evaluate responses and target any areas for development more appropriately. There were also several key aspects of our services and potential future services for which we wished to gain stakeholder views; therefore the questionnaire was structured with the following themes: Knowledge of current services Individual referral trends and reason for referrals Views on Day Care services o Current service and model o Potential changes o Accessing Day Care services Views on additional services/opportunities In-patient services o Views on potential opportunities o Blood Transfusion at the hospice Community Services Telephone advice Outpatient services Support to nursing and residential homes Open day events Additional ideas and comments from respondent A sample of the questionnaire is available on request. Sample A total of 230 questionnaires were sent out to stakeholders working in the following sectors/specialities: General Practitioners in referral area Palliative Care Consultants and Consultant Oncologists Ward Managers from referring wards at University Hospital North Tees (UHNT) and James Cook University Hospital Macmillan Team Palliative Care Team, UHNT Community Nursing Team Social Worker Specialist Nurses and Matrons, acute sector 36 completed questionnaires were returned. (16%) The range of respondents can be seen in the table below. Position/Job Title of Respondents GP 14 (39%) Macmillan Nurse/ Specialist Nurse 8 (22%) Ward manager/Sister 2 (5%) Consultant 3 (8%) Psychologist 1 (3%) Macmillan Technician 1 (3%) Occupational Therapist 2 (5%) Anonymous 2 (5%) Social Services 1 (3%) Ward Matron 1 (3%) Physiotherapist 1 (3%) Section 2: Responses It can be seen from the above chart that although the response rate was only 16%, the respondents were from a wide area of sectors and professions. We were particularly pleased with the response rate from GP’s but the lack of response from the Community Nursing Team was disappointing as we receive many referrals from District Nurses and would have liked to have incorporated more of their views in this survey. We do believe however that one of the anonymous responses received was from the Community Team. The responses and specific comments relating to each question are outlined below mirroring the questionnaire layout. All comments from respondents are written as stated in the questionnaire responses. Question 1 Are you fully aware of all the services Butterwick Hospice currently offers? Yes 25 (69%) No 7 (19%) Think so 1 (3%) Not sure 1 (3%) Most of them 1 (3%) No answer 1 (3%) Question 2 Have you ever referred patients to Butterwick Hospice? Yes 33 (92%) If yes, was this for: Day Care Family Support and Bereavement 18 (50%) Complementary Therapy No 25 (69%) Symptom control 11 (30%) Other :- please state:- 3 (8%) In- patient 28 (78%) 26 (72%) Respite 18 (50%) Psychological Support 22 (61%) End of life 1 (3%) If ‘No’ was this because:You were not aware of the services offered by Butterwick Hospice 2 (5%) Patient did not wish to go to hospice 2 (5%) Times/Days not suitable You felt the patient ‘was not ready for hospice care yet’ 1 (3%) The services provided did not meet your patient’s needs (if you tick this box please give details below) Other (please state reason below) [we] Cope at home with hospice, palliative specialist and Macmillan advice We are a specialised practice and have very few patients with life limiting illnesses (Aware of services) – not all of them Day Care Services Question 3 Do you think the ‘traditional’ day care model such as that described above, meets the needs of the majority of your patients? Yes 28 (78%) No 5 (14%) Partly 1 (3%) Think 1 (3%) so If you answered ‘no’ is this because:Patients do not wish to spend a full day (10-3) at the hospice Weekdays are not suitable for patients 2 (5%) 2 (5%) The diversional activities currently offered do not appeal to 4 (11%) your patients Other reasons: Some people find this model of care wonderful and gain a lot of support from it. However, others are more reserved and find contact with strangers is not what they want/how they deal with problems. I have been informed by several patients that use the service, especially men that so much more could be accomplished/achieved. Male patients don’t particularly like what is mentioned above as the activities are more feminine. Introducing male interests would be advised. Younger clients feel they are too young or not ill enough. Some people may like weekend visits. Some younger women may not wish to do the activities suggested and may want to look at pamper sessions. Does not always appeal to teenage and young adult groups, but some patients are initially wary of attending. They are fearful of what to expect. Not everyone is comfortable in group settings – also younger people don’t necessarily feel it is for them. Patients would like to attend the day care services more often than they are open i.e. 2-3 days per week rather than once per week Question 4 Do you think there is a demand for day care services to be offered:In an evening? Yes 14 (39%) No 19 (53%) D/K 2 (5%) At a weekend? Yes 22 (61%) No 9 (25%) D/K 4 (11%) Maybe 1 (3%) Never asked patients about this. Possibly to allow families one off support for events, appointments etc. Where there are younger children, situations may arise where the patient who is unwell is too ill to go out for the day or weekend, therefore the whole family stay at home. This may improve quality of life for carers and children. You need to ask patients Question 5 Do you think some patients would like to access specific services only, rather than attend for a full day care session? Yes 32 (88%) No 1 (3%) N/R 3 (8%) If ‘YES’ please tick which services you believe they would be interested in:Complementary 30 (83%) Relaxation 25 (69%) Therapies Meditation 17 (44%) Clinical support 25 (69%) Breathlessness clinics 22 (61%) Gentle exercise 19 (53%) sessions e.g. Tai Chi or specialist programmes Physiotherapy 24 (67%) Counselling 28 (78%) Bereavement support 29 (80%) Other -Please list 4 (11%) below Comments Did not know about some of the above sessions Clinics with the wider multi-professional team. Drop- in clinics re medical issues i.e. pain, symptom control. Family drop-ins for support. Some of my clients would like to have access to bathing facilities only for full submersion baths. Is this something you do, or would consider? It is offered by some residential homes in Darlington and at Teesside Hospice. Definitely Auricular acupuncture for hot flushes. One of the services may be a way in, but I believe the benefit of social interaction is crucial for the patients I see. Bathing. Question 6 Please answer the following in relation to the above:I would like to/have referred patients to day care but the 21 (58%) patient did not wish to come. I would like to/have referred patients to day care but the 6 (17%) patient’s relative/carer did not want them to come. I believe the hospice is really for patients towards the end of 3 (8%) their life. There is a taboo surrounding hospice care which prevents 18 (50%) patients from coming to the hospice. Other: I don’t always think of the option. Our team members (Macmillan) have referred very suitable patients for day care, however, on many occasions they have waited far too long to be assessed by the Hospice Team, therefore have become too poorly to attend. It would also appear that some patients are favoured over others………which has been the case for whatever reason! I feel patients are not assessed early enough for referral to day care – sometimes they are ‘taken over’ by secondary care; District Nurse and the GP doesn’t see them at this stage. It may be appropriate to somehow target this earlier phase for patient awareness/access. Sometimes access is slow/unavailable at the time wanted. (Re taboo) Yes, but a little less nowadays. Comments for Question 6 cont.. Some people feel that the Hospice is there for end of life only and it is their misunderstanding of what can be offered; sometimes those preconceived ideas put them off - sometimes making it difficult to change that interpretation. Patients/carers are often reluctant to be referred until they accept they are in the final stage of their illness. Staff in the acute sector tend to only refer patients toward the end of their life. Further publicity is required to advise day to day care services to patients who are discharged home being newly diagnosed and referred to Macmillan services. Could we have leaflets on the wards please to show what you offer. Need more advertising/information re services we can access for patients. I have referred patients to day care and they have been deemed not appropriate or access has been an issue. By the time this has been resolved they are too poorly to attend. Also delays when people are off increased. Time delays to make arrangements to attend. Brain and CNS patients may deteriorate unexpectedly between referral and attendance. Many people are not aware of service. Question 7 Do you think there may be a demand for any of the following:a) Service/support for patients newly diagnosed with a life limiting condition? Yes 32 (89%) No 2 (5%) D/K 1 (3%) b) Service/support for patients who have completed their course of treatment and classed as ‘cured’ or in remission? Yes 26 (72%) No 5 (14%) D/K 2 (5%) 7a Fear of stigma would be a consideration. If they can get over the stigma of ‘hospice’ many of my patients are not at the point of accepting this. Perhaps this type of service would needs its own ‘branding’ – how would this sit with specialist nurses. Yes, although this is often covered by CNS - could augment this Survivorship issues as a sub-section of the hospice back to work. This could be provided by an OT, but am not aware of there being one at Butterwick.. 7b 7ab Yes but I am not sure that demand is best met by a hospice [Yes] as long as there is enough capacity In-patient Services Question 8 We currently offer in-patient facilities for patients with life-limiting conditions such as cancer, neurological conditions, end stage heart failure and end stage COPD. Do you think there is a need/demand to offer this facility to patients with other conditions such as:End stage renal disease? Yes 31 (86%) No 1 (3%) D/K 2 (5%) No 1 (3%) D/K 3 (8%) No 7 (19%) D/K 3 (8%) End stage liver disease? Yes 30 (83%) Patients with dementia? Yes 21 (59%) Other: COPD (Re dementia) - Yes but should still have specialist palliative care needs. Comments: Unsure about dementia – what activities would be appropriate. Although we often find that patients with end stage malignant disease that get admitted to hospital, whose preferred place of care may be the hospice, cannot be transferred because of capacity problems. Taking on more malignant conditions will exacerbate this! As cancer is increasing - a great deal is given and offered to cancer patients. There are many other life threatening diseases that deserve equal support as cancer, but don’t receive it – especially dementia. I feel all these groups could be very useful though as a GP we are often not aware of the ‘end stage’ as the patients are often under secondary care. Sorry, I am not sure as I don’t come across these groups of patients regularly enough to answer this question. (Re liver and renal) Yes, but only very rarely in these cases. Can’t comment on the above [all] Yes, but never enough beds to accommodate long waiting list. Dementia may cause challenges and impact on other patients/families – we think dementia patients need specialised place of care for themselves. Question 9 We have now recommenced blood transfusions at the hospice- Is this something you would be interested in for your patients? Yes 30 (83%) No 2 (5%) N/R 3 (8%) N/A 1 (3%) Comments Unsure whether hospital or hospice would be appropriate. (Yes) but would be trust wide decision. UHNT Community Services Question 10 Do you believe there may still be a need for the hospice to provide support in some way to patients and carers in their own home? Yes 32 (89%) No 1 (3%) * N/A 3 (8%) If ‘yes’ would this be:A sitting service during the day? Yes 25 (69%) No 5 (14%) D/K 1 (3%) A sitting service during the night? Yes 27 (75%) No 3 (8%) A rapid response service 24/7 to provide support and help patients remain at home? Yes 32 (89%) No 0 (0%) D/K 3 (8%) Other: Hospice at Home. Specialist palliative knowledge to support D/nurse services. New sitting service during the day. Comments re. Question 10 Re sitting service during the day Potentially my clients are often younger with spouses who work – need finances, and normality, but often give up work to care. Re sitting service during the night ? in addition to any Marie Curie nurses. This would allow family members to continue to work or to care during the day – often 1-2 nights isn’t enough per week to give enough respite. Re 24/7 service In certain situations. This was an excellent service [reference to OOH]. Especially when discharged on a fast track discharge pathway. Telephone advice Question 11 Have you ever phoned Butterwick Hospice for advice? Yes 19 (53%) No 16 (44%) N/R 1 (3%) If ‘yes’ was this helpful? Yes 19 (100%) No 0 (0%) Would you like to see a more formal, ?commissioned help line for health professionals? Yes 20 No 3 (8%) Not 1 (3%) Not 1 (3%) sure necessarily (55%) Comments Used the on-call palliative care physician Didn’t know I could Medical advice which was helpful. [Yes] spoke to medical team. Re formal commissioned help-line- It may be useful for some staff. Outpatient services Question 12 Would you be interested in accessing a Specialist Palliative Care Clinic for your patients? Yes 27 No 3 (8%) N/R 4 (11%) N/A 2 (5%) (75%) Comments Not sure how it would function for patients and symptoms control. Not in my own role, however, this would benefit the CNS. How would this link into MDT, working with the clients current care. Would this be handed over fully to their clinic or would it be for a one off specific situation?/ set of symptom?. Feel CNS does this in community. Nursing/Residential Care Home support Question 13 Do you think there may be a role for Butterwick Hospice to provide support in palliative and/or end of life care to:Clients/residents in Nursing homes? YES 27 (75%) NO 7 (19%) N/R 1 (3%) 6 (17%) N/R 1 (3%) Clients/residents in Residential care? YES 29 (80%) NO If ‘yes’ what kind of support do you think would be beneficial:Support and advice re client/resident’s palliative, end of life care needs? Yes 25 (69%) No 2 (5%) No 2 (5%) Education and support to staff? Yes 27 (75%) Other: Family members. Planning end of life care. Prevention of acute admissions. Comments I find the residential/nursing homes are quite good with palliative patients. ‘Rapid Response’. Not sure, sorry. The hospice would provide a useful source of telephone advice. Patients need not be admitted to the hospice – however, staff can give telephone advice etc. to nursing home staff. Open day events Question 14 Would you be interested in attending an open day event at the hospice in the future? Yes 19 (53%) No 15 (42%) N/R 2 (5%) If ‘Yes’ what would you be interested in? Tour of building and facilities Yes 8 (22%) No 3 (8%) Finding out about the services offered and benefits Yes 16 (44%) No 1 (3%) Meeting and talking to a range of clinical staff Yes 13 (36%) No 2 (5%) Taster sessions such as Complementary Therapies, Tai Chi etc. Yes 9 (25%) No 4 (11%) Other Clinical education. Educational training from clinical staff. Contact and referral system etc. Comments Perhaps just an afternoon (my time is well stretched!). I already know a lot of the services on offer, however would love to meet more of the staff in their own roles/areas. Have already visited – feel able to contact team for further visit should this be needed. No – have previously attended. No – have visited before and also worked as palliative care physician for five years. Hospice at UHNT – referred patient to this service who are on end of life pathway, unfortunately there have been a lack of beds and patients have died on the ward instead of their preferred place of death - hospice. Can patients from the ward be accepted over the weekend and not just Monday-Thursday. There appears to be more capacity at Hartlepool’s hospice than at North Tees. Can this be looked into. Benefits advisor – closure of George Hardwick’s Foundation imminent – massive loss to our trust. [No] – I already work closely with hospice staff and visit the hospice as needed. Question 15 Do you think an open day event would be beneficial for your patients, their carers or the general public? Yes 33 (92%) No 1 (3%) Maybe 2 (5%) Additional comments from respondents If you have any other comments you would like to make in regards to Butterwick Hospice’s current or future services please use the space below. Patients and the general public have an understanding that all those that go to the hospice go there to die. Publicising the many other sides of the hospice and what it has to offer will open up new opportunities for the hospice and patients alike. I have experienced the fabulous care and love the hospice give to those who are dying……….just wonderful and comforting. Re-open event for public/patients:- ‘perhaps a regular monthly one which clients could be encouraged to go to informally. Your ongoing support is invaluable to those who access the service, whilst I have ticked ‘yes’ to many questions, I would not like to think of your support being spread too thinly trying to achieve so much! You do not provide holistic care as there is no element of rehabilitation. You have no other manual handling equipment other than a hoist and therefore you disable individuals who would transfer using a rota-stand etc. You are selective in who you admit – there is still not clear referral criteria which I asked for over a year ago. You are looking at clinics for e.g breathlessness, no doubt you will not employ AHPs, which would benefit the patient/carer. I do think that the hospice can be very selective over which patients they accept and how long different people stay for. I think respite care should be stopped to enable patients that need to be there for symptoms control management. Need to employ own occupational therapist. Physios need to access equipment themselves if they are recommending equipment. Joint working and effective two-way communication works very well with day care, however, I think this can be improved with the inpatient unit by ensuring that we get discharge summaries in a timely manner, or a telephone update if a letter is not available, so we can continue to support the patients and carers effectively – Thank you. Better discharge communication (written) in a timely manner to those staff supporting the patient in the community i.e. medication list would be beneficial to both patients and staff. Section 3: Recommended actions We were extremely pleased with the valuable and wide ranging comments we received from respondents and also grateful for the honesty when writing these. This will enable us to focus our actions on addressing these issues and take appropriate measures to clarify and resolve any areas where our services may not be meeting the needs of patients in the way we would like. The following key recommendations have therefore been formulated from the responses and individual comments. In no particular order, they are: Ensure GP’s are aware of the Specialist Palliative Care Clinic Meet with Macmillan team representatives to discuss and resolve concerns re. access to adult services for their patients and availability of specific moving and handling equipment. Distribute copies of this report to Hospice Managers and key stakeholders. Send copy of this report to Contracts Manager and CCG. Review activities in Day Care and where appropriate introduce activities which are more appealing to men and younger adults. Plan and hold an open event for stakeholders. Plan and hold an open event for the public. Explore offering support/facilities to patients with end stage renal or liver disease. Explore the benefits and feasibility of having a hospice Occupational Therapist. Meet with Community Nurses to discuss their views on current and future services Section 4: Opportunities for service development In addition to enabling us to formulate specific actions, the questionnaire was designed and has enabled us, to identify areas for potential development in the future and we will be taking the opportunity to discuss these with commissioners and relevant personnel. Provision of palliative and supportive care in the community e.g. o Sitting service during the day o Sitting service during the night o Rapid response service 24/7 Support to Nursing and Residential Homes e.g. o Support for clients/residents in nursing homes o Support for clients/residents in residential care o Education and training to support staff working in nursing homes o Education and training to support staff working in residential care Sessional Day Care o Continue to develop sessional services. References Help the Hospices (2013) Future ambitions for hospice care: our mission and our opportunity October 2013. The final report of the Commission into the Future of Hospice Care. Help the Hospices. London. Patient and Carer feedback We receive many thank you cards and letters from patients their families and carers which provides feedback on the quality of service provided by the Hospice. This feedback also forms part of our CQUIN data and samples of the comments received are therefore sent on a regular basis as part of the reporting process. We have included a selection of these comments below:…..her first words on being admitted were that she felt safe and in good hands. This, we believe, is a reflection on all looked after her during her final days. The care, time, kindness and compassion that staff gave ensured ‘K’s’ fear of pain and losing dignity would never be realised. Despite the difficult time we were facing as a family, your approach to her care (and ours) eased the distress for us all. We were able to be together as a family, and were made to feel like, for those final days, the Hospice was our home. You will never know how much that meant to us all. ‘K’ died peacefully, in her sleep, on the morning of 7th January 2014, feeling safe and loved. We are eternally grateful to you all for this - thank you so much. Thank you all so much – you all do a difficult job so extremely well. Best wishes to you all with greatest thanks. Sadly my mum ‘B’ passed away Sunday 1st December. We sadly miss her. We would like to greatly thank all the staff who cared for her whilst in respite care. She was so well looked after. She particularly enjoyed her 80th birthday on day care and we all enjoyed seeing the pictures of her cutting the cake you had made for her. She was so very pleased. To each and every one of you at the Butterwick – no words can express how grateful we are for your time, care and support you all showed ‘J’ and us as a family in ‘J’s’ last days of his life. We feel so privileged to have met each and every one of you from Maria, the nursing staff and all the volunteers. You truly do a wonderful job and go the extra mile. I know ‘J’ was in the best place possible. The Butterwick will hold a special place in our hearts and I feel a great comfort knowing that we will return to the Butterwick. I would like to say a special thank you to Jeanette, Michelle and Millie, who were with ‘J’ and myself when ‘J’ passed away. You all supported ‘J’ and my family until the very end. You are all amazing people, just keep doing what you all do, we truly respect each and every one of you. Words really cannot express my gratitude for the excellent care you gave my dad ‘D’. during the last few weeks of his life. I was so pleased that he was admitted in to the Butterwick rather than a hospital or having to manage at home, and I know he really appreciated all help and treatment you gave him (particularly the Jacuzzi baths). He was a wonderful man and we were very lucky to have him thank you for the making the end of his life as best as it could be. We would like to express our sincere thanks and gratitude for all you did for ’K’ during his recent battle with cancer and sadly his death. The care and support that you offered him and also us was exceptional and the dignity, peace and pain relief you were able to give will always be remembered and appreciated by us. The Butterwick is such a special place, filled with extremely special staff. We are so thankful that there is such a place. We only wish that you could have known ‘K ’as the loving, kind and wonderful man that he was. We just wanted to say a great big thank you for all the care and support you gave us all during ‘J’s’ stay. To have been given the use of the family room gave immense comfort to the whole family which we really appreciated. We apologise for what must have seemed like we were taking over the place (we’re not the quietest of families!). However, you made us feel so welcome. The warmth and generosity of the staff will never be forgotten. Heartfelt thanks. To all staff – day centre – I would like to thank you for all your hard work you do. I don’t know how we as a family would have managed without you all in the five years mam was with you. As mam said you were a life saver for s as a family, knowing mam was getting looked after, and for mam a reason to get up and fight another day. I know she classed you all like her second family as well as good friends, and no doubt she will have left a void in your hearts as she has ours. Keep up the good work, you will be always in our thoughts hearts and prayers. The amazing staff of Butterwick Hospice. Thank you does not go anywhere close to expressing our feelings for the staff who cared for my mum ‘V’. Every single one of you made her feel part of a little family, and became her friends. The gentleness and care you showed her made it much easier for us all to cope with those last few weeks. Your kindness to our family we will never forget, and even thought we were there for a very sad reason, we have taken away many happy memories. As for myself, the support you all gave me in that last week was amazing. I could never thank you enough. You looked after me as well as Mam. Thank you again. Section 2.6 Data quality NHS Number and General Medical Practice Code Validity Butterwick Adult Hospice, Stockton on Tees did not submit records during 2013/14 to the Secondary Uses service for inclusion in the Hospital Episode Statistics which are included in the latest published data. The following mandatory statement is therefore not applicable to Butterwick Adult Hospice Stockton:[Name of provider] will be taking the following actions to improve data quality [insert actions]. Butterwick Adult Hospice, Stockton on Tees was not subject to the Payment by Results clinical coding audit during the reporting period by the Audit Commission. Information Governance Toolkit attainment levels Butterwick Adult Hospice, Stockton on Tees was asked to undertake the Information Governance Toolkit during 2013/14. At the time of writing this report this exercise is still being undertaken and therefore the information was not available to complete the statement below. Butterwick Adult Hospice, Stockton on Tees’s Information Governance Assessment Report score overall score for [reporting period] was [percentage] and was graded [insert colour from IGT Grading Scheme]” Part 3 Review of quality performance 2012/13 (provider determination) In our first Quality report last year three developments were chosen from the business plan and Clinical Strategy Action Plan as our focus for quality improvement and these are reviewed below. Development 1: Patient Safety To strengthen the medical and nursing team in order to provide increased specialist palliative and supportive care. State how development was identified In 2010/11 a revised nursing structure was established and successfully implemented in 2011/12 with key posts of a Clinical Lead for Adult Services supported by Clinical Team leaders being introduced. This structure was supported by a Clinical Strategy, the key aim of which is to ensure we continue to meet the current and future needs of patients and their families in regards to palliative, supportive and end of life care needs within a changing health arena. Key objectives in the clinical strategy for 2013/14 was to continue to up-skill the nursing staff in several clinical skills such as cannulation, intravenous drug administration, phlebotomy etc. as well as supporting the Clinical Team Leaders to achieve advanced skills in regards to independent prescribing and clinical assessment skills. All of the qualified staff were trained in the former skills during 2011 and three of our Clinical Team Leaders had completed either independent prescribing or clinical assessment skills course in 2012/13. Alongside the increasing of nursing skills we had been striving to strengthen our medical team for some time but without success. With our previous Hospice physician moving to another post and the Palliative Care Consultant from the local Trust retiring in December 2012 this need became even more relevant. Whilst recruitment took place for Hospice Physicians we used a team of locum GP’s and continued to provide palliative, supportive and end of life care for a wide range of patients. However, in order to ensure safe and appropriate medical care we had to use revised admission criteria which resulted in patients with complex symptom control needs being admitted to other local hospices or the acute trust. How was it achieved? Following the successful recruitment of two Hospice Physicians in early 2013, we began to re-establish specialist palliative and supportive care in June 2013 which enabled us to admit and care for patients with more complex needs nearer to home. This was also supported by the successful recruitment of a Palliative Care Consultant by the University Hospital of North Tees and the formalisation of three consultant sessions to Butterwick Hospice. Although the Palliative Care Consultant does not take on medical responsibility for the hospice patients, she provides specialist advice and support to the Hospice Physician and clinical team via attendance at the weekly MDT meeting, educational sessions and telephone support. Review and evaluation of success of development We have been able to admit and care for patients with more complex needs nearer to home which has been beneficial for patients, carers, referrers and also reduced the impact on neighbouring hospices. Our bed occupancy has increased and is more consistent as we have been able to admit more than one patient per day and the time between referral and admission has reduced resulting in more patients being cared for in the place of their choice. In addition, many patients have been admitted on the day of referral either from home or the acute trust. Due to the skills of the Hospice Physician patients have been able to have specific treatments and procedures in the Hospice such as ascetic drainage and therapeutic IV drug infusion which previously would have required patients to be transferred to and from the acute trust. This is extremely beneficial for patients and also reduces the impact on services and resources within the Acute Trust. Following meetings between the Director of Clinical Services, clinical team and Palliative Care Consultant to discuss and agree the utilisation of the three consultant sessions, a planned programme of bespoke educational sessions for staff has been established which plays a significant part in the education of staff to meet the needs of patients with complex palliative and end of life care needs. The medical staff have also been fully supportive of the nursing staff developing additional skills and mentorship for specific university modules. Due to the knowledge, experience and skills of the current Hospice Physician, the number of advice calls to the Palliative Care consultants has decreased thereby reducing the impact on them from the hospice and enabling them to support staff providing palliative and supportive care to patients in the acute and community trust. Although one of our hospice physicians left the hospice after 6 months to move nearer to her family, we have still been able to achieve the improvements set out above. We have not, however, succeeded in recruiting to the vacancy to date. Development 2 To enable patients to receive blood transfusions and intravenous medication within the hospice. State how development was identified Patients were being transferred from the hospice to the acute trust if they required a blood transfusion or intravenous medication which could be distressing for patients and relatives. We were also aware that some palliative care patients require regular blood transfusions and were being admitted to the acute Trust for this. We believed that the hospice environment would be more appropriate and comfortable for the patients as well as removing the costs associated with these procedures for the acute trust. Blood transfusions and intravenous medication had been conducted at the hospice previously and it was a key objective to re-establish these procedures as part of the hospice’s clinical strategy. How was it achieved? The two new Hospice physicians were confident for these procedures to be reintroduced into the hospice and expressed their support for staff to undertake blood transfusion and the administration of intravenous medication appropriate to patient need and the hospice environment. The competencies of the clinical team in regards to blood transfusion were updated and following liaison with the Blood Transfusion Practitioners at the local hospital, training sessions were provided for staff and key trainers. This was carried out as part of our Service Level Agreement for Blood Transfusion Services with the Trust. All qualified nursing staff had received training in cannulation and administration of intravenous antibiotics during 2012 and the IV policy and procedures were put in place. The hospice physicians undertook training of all staff in the management of anaphylaxis and a bespoke anaphylaxis kit was ordered and put in an appropriate place. The Quality and Practice Development Nurse liaised with the Clinical Lead for Adult Services to ensure the staff undertook all required training and their competencies were assessed prior to the commencement of these procedures. Review and evaluation of success of development Blood Transfusions within the in-patient unit were successfully introduced in the summer of 2013, closely followed by the administration of intravenous medication. Patients are no longer transferred to the acute trust for blood transfusion or for most intravenous medication administration. This has been much less stressful for patients, carers and reduced the impact on resources at the local hospital. We expect the number of patients receiving blood transfusions at the Hospice to increase as 83% of respondents in the stakeholder questionnaire stated they would be interested in patients being able to have blood transfusions at the hospice. Development 3 Patient experience Pre and post Bereavement Support – Direct GP access State how development was identified Pre and post death bereavement support is an essential part of end of life care for the relatives or carers of the patient and their children. Prior to the commencement of the pilot scheme, Butterwick had only provided pre and post bereavement support and family support to relatives and carers of patients known to the Hospice. However, we frequently receive requests from GP’s and multi-disciplinary professionals asking our Family Support Team if they can provide bereavement support to clients not known to us which we had had to decline due to our standard resources being fully utilised by providing support to patients and their families who are or have accessed our services. These requests often include a need for child specific bereavement counselling within the local area. Being able to access services in a timely manner is extremely important and we were aware that often clients currently have to wait up to 6 weeks to access support via their GP. We wished to use the skills and resources at the Hospice to provide a high quality bereavement support service to a wider group of clients, thereby responding to the requests of local GP’s and other professionals. This aim of this development was to enable direct access for GPs to refer patients who were not currently accessing Butterwick Hospice services; therefore adults and children would be able to access the full range of specialist bereavement support services at the Hospice. This development was in accordance with an established, highly successful service offered by our Bishop Auckland Hospice which provides similar specialist services in County Durham and Dales for both adults and children. How was it achieved? We used the skills of our existing family support staff at Butterwick Hospice as well as trained volunteer counsellors. Letters and referral forms were sent to local GPs explaining the services available and posters were designed and produced to be displayed in GP surgeries enabling potential clients to be aware of the services and ask their GP to refer them. The new development was discussed at our weekly clinical meeting attended by representatives of the multi-disciplinary team and external health professionals. Information was also included on the Hospice website. The following services were made available for clients who had not previously been able to access Butterwick’s Family Support Services: Individual counselling for patients pre death. (Coping with a bad prognosis) Preparing to say goodbye etc. Preparation for death with the use of letter writing, memory boxes, family D.V.D messages, funeral plans and wishes of the dying or terminally ill patient etc. Pre death and post death counselling for relatives and friends of the patient. Home visits if the client is not able to come into the hospice. Children’s support. Preparation for the death of a parent or relative by individual play and support sessions for young children with preparation and post procedural play carried out by qualified staff. Young persons counselling pre and post bereavement Home or school visits if deemed more suitable for the child or young person. Telephone support if distance is a problem Bereavement groups which include a thriving drop in which takes place every Monday 10 till 12.00 for the newly bereaved and 1.30 till 3.30 for those further along in their grief (except for bank holidays) And a monthly evening support group for people who work. We also run 7 week M.O.T (moving on together group) several times a year for people who prefer a more structured approach to loss. Twice Yearly bereavement service’s which serve to unite the bereaved in their loss with an average attendance of 400/500.people Children’s bereavement group fortnightly. As we did not know what the demand would be for the services and wished to ensure we continued to provide a high quality, timely service, the direct access project was rolled out to groups of GPs on a planned basis whilst monitoring the impact on current resources. Review and evaluation of success of development. Between April 2013 and March 2104, 66 clients were referred to the Family Support Team via the direct access scheme. These clients mostly accessed one to one counselling and 12 referrals were children who received specialist child grief work. Evaluation of the service was carried out with clients who had received this and questionnaires were sent to the practices from which referrals had been received. Comments received from clients included: Very much appreciated being able to discuss my problems with such a lovely lady. It was helpful to know that what I felt was normal and there was someone to share it with who understood. Very good at listening, very caring and I was very much at ease talking about things. Would recommend the Family Support Team to other friends The support is fantastic, caring, understanding. Only glad there is places like the Butterwick The service given by the group is second to none Feedback from referrers:36 Questionnaires were distributed to the GP practices who had referred patients to the service and 13 were returned (36%) Unfortunately only 8 of the 13 questionnaires returned were completed which equates to a 22% response. 5 questionnaires returned were not completed and the reason for this is unclear. The questionnaire comprised of 5 key questions and whilst the response is quite low the feedback received is extremely positive. The majority of responses indicated that the GP’s were very satisfied with the service provided and 100% of respondents indicate that they feel the service should continue. The results of the evaluation questionnaires are set out on the next pages :- Question 1. REFERRAL PROCESS How would you evaluate the referral process? Very satisfied 8 (100%) Satisfied 0 Less than satisfied How satisfied were you with the response time from referral to your patient being seen by the Family Support Team? 0 Very satisfied 6 (75%) Satisfied 1 (13%) Less than satisfied 0 Question 2. CHOICE OF SERVICE The Family Support Service aims to provide specialist support to patients facing life limiting illness, including grief and loss counselling before and after a person’s death. How important do you think this is for your patient? How important was it to you that your patient could choose which support they felt suitable for their needs i.e. 1:1 Counselling; MOT work group (seven week structured group sessions for the bereaved); drop-in sessions? Essential 7 (88%) Important 1 (13%) Not Important Essential 0 Important 0 Not important 0 Question 3. LENGTH OF SUPPORT Our support services are not time limited i.e. we will work with a client for as long as necessary e.g. not just 6 sessions How important do you think this is for your patients? Essential 6 (75% Important 1(13%) Not important 0 Question 4. CHILDREN’S SPECIAL SUPPORT We also provide support for children and young people before and after a person’s death, including individual, group, school and home support sessions. Yes 8 (100%) Do you feel this is a service which would be of value to your younger patients NO 0 General Questions How would you rate the service offered by Butterwick’s Family Support Team in comparison with other counselling support services that you may have used prior to the 12 month pilot project? Better than other services Not as good as other services No difference 6 (75%) 0 2 (25%) Please give comments below: I have had feedback from families which is very positive. Good comments regarding prompt service and helpful for teenagers/children. I regularly refer patients for Psychological Counselling via Dr Williams. N/A as I have been in post less than 12 months. Our patients can often experience rapidly deteriorating situations where their needs change automatically and quickly/ The response time from referral to support is excellent and invaluable for our setting. Would you like this service to continue? Response: Definitely! Most Definitely!! Have you received any feedback from your patients in relation to the Family Support Service? If yes please provide comment: As previously mentioned prompt and supportive. They feel it has been invaluable the service you have provided. Patient are “relieved” , “glad”, “pleased” “comforted” by the service. Sensitive, caring and non-judgmental. Quick response very much appreciate. Felt “tailored to needs”. Verbal/very positive. Very positive. They have been able to adjust and accept diagnosis/bereavement. Felt well supported. Response YES 8 (100%) NO 0 Response YES 7 (88%) NO 0 Please add any other comments you may have regarding the service: It would be useful to know of the full services that you provide- maybe a leaflet explaining these. I think it would benefit patients/ carers / family members – allowing them to understand the services and accept support more readily. Valuable service for patients and families in the community who need access quickly to bereavement and counselling in palliative support. We really value the service especially in relation to helping to support young adults who will be bereaved. If the service continued we would be able to plan with families for this necessity in the same way we try to establish “preferred place to die”. We are trying to do this earlier when it is known that treatment for Leukaemia and Lymphoma has not worked. Wonderful service – please let it continue. Please continue and further develop. I didn’t know anything about this service, so something went very wrong. I lead the CCG locally and haven’t heard about this as a commissioner or as a GP provider. In regards to the last comment above, we were surprised and concerned and therefore investigated this and were able to contact the GP directly. A letter and poster had been sent to the GP surgery but unfortunately the GP had not been made aware of the service. 3.2 An explanation of those involved in this quality account The Quality Account was discussed at the Hospices Management Team meeting which is chaired by the Chief Executive and includes clinical and non clinical managers, the Director of Clinical Services and the Director of Finance. The task of writing it was delegated to the Registered Manager with a statement from the Chief Executive. The Quality Account was also discussed at the Senior Clinical Meeting where the quality priorities were agreed. It has also formed part of an Agenda item of the Clinical Strategy and Governance Committee which is a key element of the Charity’s governance structure: the Minutes of which are distributed to the Board of Trustees as will a copy of this Quality Account. Once completed the Quality Account was distributed to Clinical and non clinical Managers for comment and approval. The completed Quality Account was then forwarded to Hartlepool & Stockton on Tees Clinical Commissioning Group and the local Healthwatch team to approve and comment on the quality priorities mentioned in the report. ANNEX: Statements from Commissioning Group and Local Healthwatch Team. 27th June 2014 C Harrison Director of Clinical Services Butterwick Hospice Middlefield Road Stockton-on-Tees TS19 8XN Dear Carole Re: Butterwick Adult Hospice, Stockton, Quality Account 2013/14 review & priorities for 2014/15 I am pleased to provide you with a commissioner narrative as requested for your Quality Account. I would also like to reiterate the continued commitment of NHS Hartlepool and Stockton-on-Tees Clinical Commissioning Group to actively engage in meaningful and productive ways with the Butterwick Hospice and key stakeholders in the prioritisation and development of future Quality Accounts. NHS Hartlepool and Stockton-on-Tees Clinical Commissioning Group (HaST CCG) welcomes the opportunity to comment on your 2013/14 Quality Account. Overall the report is presented in a concise and meaningful way, and it is considered to accurately reflect the Hospices commitment and positive ethos to deliver quality improvements, demonstrating in an open and transparent manner its performance during 2013/14 and the key challenges it has encountered. It would have been a welcome addition, however, to see in the report patient safety information relating to incidents and complaints that have occurred throughout the year and the lessons learned and actions taken to address any themes. In reviewing delivery of the 2013/14 priorities, the CCG specifically acknowledges the challenges associated with strengthening the medical and nursing team and the impact on the service model whilst maintaining a clear focus on achieving positive patient outcomes. In addition, the CCG recognises that there is a need to improve communication between primary care and the Hospice if pilot schemes such as the pre and post bereavement service are to be effective and succeed in the future. The CCG would like, however, to commend the Hospices success in introducing Blood Transfusions within the in-patient unit including the administration of intravenous medication which has resulted in the majority of patients not having to transfer to the acute hospital. In relation to the priorities identified for 2014/15 the CCG is supportive and encouraged by the focused attention on ensuring quality improvement activity links with the CCGs strategic vision to improve health care and quality outcomes for patients. The Introduction of the Breathless Support Programme working with primary and secondary care providers is evident of this. Whilst, the emphasis on clinical educational sessions and introduction of a service user advisory Group positively reflects the Hospices desire to continue to listen and respond to both its own staff and patients through measured and meaningful approaches. NHS Hartlepool and Stockton-on-Tees Clinical Commissioning Group (HASTCCG) look forward to continue to work with Butterwick Hospice in 2014/15 to improve the quality of health care services’ Yours sincerely Ali Wilson Chief Officer cc. Jean Fruend, Executive Nurse Dr Posmyk, Chair ********** Healthwatch Stockton-on-Tees Catalyst House 27 Yarm Road Stockton on Tees TS18 3NJ Tel 01642 688312 healthwatchstockton@pcp.uk.net www.healthwatchstocktonontees.co.uk Click here to enter text. Wednesday 2nd July 2014 Dear Carole Please see below comments from Healthwatch Stockton-on-Tees in response to the recent Quality Account. Healthwatch Stockton-on-Tees welcomes our involvement in the Butterwick Quality Account. In particular, we were encouraged by the service user/ carer involvement development. We would be keen to be more meaningfully engaged in the Quality Account process next year. Yours sincerely Joanne Shaw-Dunn Community Development Worker Healthwatch Stockton-on-Tees