Pillar: Transparency
advertisement
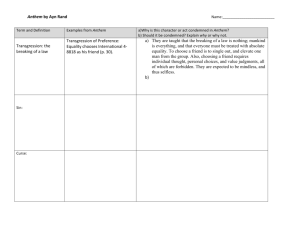
The Leapfrog Group 2007 Health Plan Users Group Scorecard ANTHEM NATIONAL ACCOUNTS RESPONSES PART 2 OF 2 April 30, 2007 Anthem National Accounts (referred to herein as “Anthem”) represents fourteen Blue Cross and/or Blue Shield plans, all under the same parent company, in the following states: California, Colorado, Connecticut, Georgia, Indiana, Kentucky, Maine, Missouri, Nevada, New Hampshire, New York, Ohio, Virginia, and Wisconsin. The Anthem National Accounts business unit serves members of the Blue Cross licensee for California; the Blue Cross and Blue Shield licensee for Colorado, Connecticut, Georgia, Indiana, Kentucky, Maine, Missouri (excluding 30 counties in the Kansas City area), Nevada, New Hampshire, New York (as Blue Cross Blue Shield in 10 New York City metropolitan counties and as Blue Cross or Blue Cross Blue Shield in selected upstate counties only), Ohio, Virginia (excluding the Northern Virginia suburbs of Washington, D.C.) and Wisconsin. Anthem Blue Cross and Blue Shield is the trade name for the following: In Connecticut: Anthem Health Plans, Inc. In Colorado, Rocky Mountain Hospital and Medical Service, Inc. In Indiana: Anthem Insurance Companies, Inc. In Kentucky: Anthem Health Plans of Kentucky. In Maine: Anthem Health Plans of Maine, Inc. In Nevada: Rocky Mountain Hospital and Medical Service, Inc. In New Hampshire: Anthem Health Plans of New Hampshire, Inc. In Ohio: Community Insurance Company. In Virginia: Anthem Health Plans of Virginia, Inc. In Missouri: RightCHOICE® Managed Care, Inc. (RIT), Healthy Alliance® Life Insurance Company (HALIC), and HMO Missouri, Inc. RIT and certain affiliates administer non-HMO benefits underwritten by HALIC and HMO benefits underwritten by HMO Missouri, Inc. Life and disability products are underwritten by Anthem Life Insurance Company (ALIC). RIT and certain affiliates only provide administrative services for self-funded plans and do not underwrite benefits. In Wisconsin: Blue Cross Blue Shield of Wisconsin ("BCBSWi") underwrites or administers the PPO and indemnity policies; Compcare Health Services Insurance Corporation ("Compcare") underwrites or administers the HMO policies; and Compcare and BCBSWi collectively underwrite or administer the POS policies. Independent licensees of the Blue Cross and Blue Shield Association. ® Registered Marks Blue Cross and Blue Shield Association. 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 2nd Pillar: Standardized Measurement and Practices No. 2007 Goal Fully Met 4 Evaluate hospitals based on standard efficiency and/or cost measures and link such performance data to information on provider quality measures for which adequate denominator volumes exist. Best practice: Efficiency measures should meet Leapfrog/BTE efficiency measure guidelines available at http://www.regence.com/research/ Efficiency is defined as the cost and quantity of services (i.e., total resources used) for the episode of care. For additional information, see "Measuring Provider Efficiency Version 1.0" available at http://www.regence.com/research/docs/measuringPr oviderEfficiency.pdf The plan meets all of the following criteria: i. The plan collects and publicly publishes hospital data for efficiency and/or cost measures for its entire book of business, across all geographic areas, and links such data with data on quality measures at the hospital level. ii. The plan evaluates efficiency and/or cost measures for hospitals that account for at least 75% of the plan’s acute care hospital admissions or payments in each market. iii. The plan communicates provider performance on efficiency measures to hospitals in the markets at least annually and offers outlier hospitals an opportunity to discuss results. Partially Met Not Met The plan meets all of the following criteria: i. The plan commits to evaluate hospital data based on efficiency and/or cost measures for its entire book of business, across at least 10 metropolitan areas and to link such data with data on quality measures at the hospital level in 2007. ii. The plan commits to evaluate efficiency and/or cost measures for hospitals that account for at least 75% of the plan’s acute care hospital admissions or payments in the market in 2007. iii. The plan commits to communicate provider performance on efficiency measures to hospitals in the market at least annually and offer outlier hospitals an opportunity to discuss results. The plan utilizes hospital cost and efficiency measurement: methodological approaches at http://www.pbgh.org/programs/documents/PBGHHo spEfficiencyMeas_01-2006_22p.pdf Anthem Care Comparison is a proprietary tool that displays total cost estimates for an episode of care using Anthem’s contracted rates for 39 medical procedures (inpatient and outpatient), diagnostic tests, and common office visits. The information is at the facility level. Currently, data for the Dayton, OH market is available to approximately 2 million members, but planning is underway to expand the pilot to Cincinnati, OH; Columbus, OH; Indianapolis, IN; Louisville, KY; and Lexington, KY in 2007. In addition to expanding to additional geographic areas, planned future enhancements include tying in quality metrics. This pilot is being highlighted as a “best practice” and model for other Blue plans by the Blue Cross and Blue Shield Association. See the “Anthem Care Comparison Screens” document for screen prints. Consumer-directed health plan members have access to quality and cost information about specific providers and facilities through the online provider directory. Members can view provider- and hospital-specific quality information, such as NCQA designations, disciplinary actions, and safety ratings (Leapfrog metrics). They can also view cost estimates (discounted and undiscounted) for 8-10 high-volume services for the given specialty. Planned future enhancements include expanding the features to other product lines. See “Lumenos Provider Finder Screens” for screen prints. Anthem offers members across all books of business a suite of online decision-support tools administered by Subimo (WebMD), including Healthcare AdvisorSM. Through that tool, members have the ability to view quality information, as well as estimated treatment costs for specific services, tests, physician visits, and medications. For example, members can select from a number of common inpatient procedures, and then enter their age group, gender, and zip code to view the total estimated cost before insurance benefits for the procedure. The typical estimated cost ranges for the procedure at an innetwork facility and at an out-of-network facility are provided. Typical costs are calculated from the average fees for each type of service at the average 3 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 2nd Pillar: Standardized Measurement and Practices No. 2007 Goal Fully Met Partially Met Not Met rates charged, and they represent the total cost for the service. The data is provided by third party sources and is not hospital-specific. See “Anthem 2007 HPUG Response Supplement – Screen Prints” document to view sample screen prints. Enhanced inpatient cost information is available to Anthem Blue Cross and Blue Shield members in Virginia through the “Find and Compare Hospitals” tool within Healthcare Advisor. The Virginia hospitals are rated as below average, average, or above average in cost on 23 common inpatient procedures. PPO contract reimbursements are used to calculate the average costs. We do not currently evaluate efficiency and/or cost measures for hospitals that account for at least 75% of acute care hospital admissions or payments in each market. Anthem does not currently communicate provider performance on efficiency measures to hospitals. C:\PPU\External C:\PPU\External Organizations\Leapfrog\Score Organizations\Leapfrog\Score Sheet 2007\ResponseSheet Supplements\Anthem 2007\Response Supplements\Lumenos Care Comparison Screens.ppt Provider Finder Screens.ppt *Please contact Anthem or Leapfrog staff for additional information. 4 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 2nd Pillar: Standardized Measurement and Practices No. 2007 Goal Fully Met 5 Evaluate physicians based on standard efficiency measures and/or cost measures and link such performance data to information on provider quality measures for which adequate denominator volumes exist. Best practice: Efficiency measures should meet Leapfrog/BTE efficiency measure guidelines available at http://www.regence.com/research/ Efficiency is defined as the cost and quantity of services (i.e., total resources used) for the episode of care. For additional information, see "Measuring Provider Efficiency Version 1.0" available at http://www.regence.com/research/docs/measuring ProviderEfficiency.pdf See "Advancing Physician Performance Measurement: Using Administrative Data to Assess Physician Quality and Efficiency" available at http://www.pbgh.org/programs/PhysicianPerforma nce.asp PARTIALLY MET The plan meets all of the following criteria: i. The plan collects and publicly publishes physician data for efficiency measures for its entire book of business, across all geographic areas, and links such data with data on quality measures at the physician or medical group level. ii. The plan evaluates efficiency and quality measures for physicians that account for at least 75% of the plan’s payments to physicians in each market. iii. The plan communicates provider performance on efficiency and quality measures to physicians in the markets at least annually and offers outlier providers an opportunity to discuss results . Partially Met Not Met The plan meets all of the following criteria: i. The plan commits to evaluate physician data based on efficiency measures for its entire book of business, across at least 10 metropolitan markets, and to link such data with data on quality measures at the physician or medical group level. ii. The plan commits to evaluate efficiency and quality measures for physicians that account for at least 75% of the plan’s payments to physicians in the market in 2007. iii. The plan commits to communicate provider performance on efficiency and quality measures with physicians in the market at least annually and to offer outlier provider an opportunity to discuss results. Anthem offers members across all books of business a suite of online decision-support tools administered by Subimo (WebMD), including Healthcare AdvisorSM. Through that tool, members have the ability to view quality information, as well as estimated treatment costs for specific services, tests, physician visits, and medications. For example, members can select from a number of common outpatient procedures, and then enter their age group, gender, and zip code to view the total estimated cost before insurance benefits for the procedure. The typical estimated cost ranges for the procedure at an in-network provider and at an out-of-network provider are provided. Typical costs are calculated from the average fees for each type of service at the average rates charged, and they represent the total cost for the service. The data is provided by third party sources and is not provider-specific. See “Anthem 2007 HPUG Response Supplement – Screen Prints” document to view sample screen prints. Anthem Care Comparison is a proprietary tool that displays total cost estimates for an episode of care using Anthem’s contracted rates for 39 medical 5 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 2nd Pillar: Standardized Measurement and Practices No. 2007 Goal Fully Met Partially Met Not Met procedures (inpatient and outpatient), diagnostic tests, and common office visits. The information is at the facility level. Currently, data for the Dayton, OH market is available to approximately 2 million members, but planning is underway to expand the pilot to Cincinnati, OH; Columbus, OH; Indianapolis, IN; Louisville, KY; and Lexington, KY in 2007. In addition to expanding to additional geographic areas, planned future enhancements include tying in quality metrics. This pilot is being highlighted as a “best practice” and model for other Blue plans by the Blue Cross and Blue Shield Association. See the “Anthem Care Comparison Screens” document for screen prints. Consumer-directed health plan members have access to quality and cost information about specific providers and facilities through the online provider directory. Members can view provider- and hospital-specific quality information, such as NCQA designations, disciplinary actions, and safety ratings (Leapfrog metrics). They can also view cost estimates (discounted and undiscounted) for 8-10 high-volume services for the given specialty. Planned future enhancements include expanding the features to other product lines. See “Lumenos Provider Finder Screens” for screen prints. Our physician pay-for-performance programs in certain California and Missouri markets include cost metrics, in addition to clinical quality metrics, in evaluating physicians. In California, we estimate that at least 75% of Blue Cross of California plan payments to physicians are for physicians evaluated on efficiency and quality. All providers participating in our pay-for-performance programs receive annual performance reports related to the quality and, where in use, efficiency metrics employed in the program. We are available to meet with any provider to discuss options, and, in many cases, actively reach out to underperforming providers. Anthem’s strategy to evaluate physician performance is to utilize metrics endorsed by national quality organizations. Given the availability of such metrics for primary care, and the importance of primary care in the health care delivery system, half of Anthem’s physician pay-for-performance programs are currently targeted at PCPs; the balance are targeted at specific specialty types for which national metrics are available. Therefore, Anthem does not generally target physicians for pay-for-performance programs based on the percentage of plan payments they account for in the market. Rather, Anthem’s goal is to engage as many eligible providers as possible into pay-for-performance programs in order to drive positive health outcomes and increased patient safety. Anthem’s enterprise Blue Precision networks are high performance networks composed of cost-efficient specialists identified using an Episode Treatment Group (ETG) methodology to stratify performance. These networks give members the choice of selecting a physician at a lower overall cost to them and to their employer through tiered benefit designs. To view Blue Precision providers, members can visit the Blue Cross and Blue Shield Association website (http://www.bcbs.com/healthtravel/finder.html). The display of Blue Precision specialists in the online provider directories is under development. We are developing quality designations for selected specialists in the Blue Precision network, to be rolled out in 2008. Similar to the approach taken in our pay-forperformance programs, metrics that are endorsed by national quality organizations are being utilized. The leaders in this arena are the National Committee for Quality Assurance (NCQA), the National Quality Forum, (NQF), the Joint Commission for the Accreditation of Healthcare Organizations (JCAHO), the AQA (formerly Ambulatory Care Quality Alliance) and the American Medical Association’s Physician Consortium for Performance Improvement (AMAPCPI). A number of national organizations with an interest in a specific disease or specialty areas have also developed measures. For example the American College of Cardiology (ACC) and the Society of Thoracic Surgeons (STS) have each defined process and outcome measures and have additionally set up disease registries to which data on these metrics are reported for participating physicians. The level of involvement of other specialty societies in developing and promoting quality metrics is variable. In instances where no or limited metrics are available for a given specialty, Anthem is working with the relevant 6 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 2nd Pillar: Standardized Measurement and Practices No. 2007 Goal Fully Met Partially Met Not Met national specialty societies to promote the development of measures or to obtain endorsement of measures proposed. Given the limited metrics that are currently available for specialists, our approach is to roll out the quality component sequentially over several years. C:\PPU\External C:\PPU\External Organizations\Leapfrog\Score Organizations\Leapfrog\Score Sheet 2007\ResponseSheet Supplements\Anthem 2007\Response Supplements\Lumenos Care Comparison Screens.ppt Provider Finder Screens.ppt *Please contact Anthem or Leapfrog staff for additional information. 7 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 3rd Pillar: Incentives and Rewards No. 2007 Goal Exceeded 1 Design and implement a 2007 hospital incentive and reward (I&R) strategy1 based on a standardized set of measures and lessons learned from I&R programs. Best Practice: Incentives and Rewards Best Practices Primer: Lessons Learned from Early Pilots, July 2006 (with support from Robert Wood Johnson Foundation and California Health Care Foundation). Find pdf of report at www.leapfroggroup.org or www.chcf.org For information regarding non-financial incentives, see: http://www.academyhealth.or g/nhcpi/models.pdf In addition to meeting the fully met criteria, the plan: i. calculates return-oninvestment for its I&R program(s) in ten metropolitan markets, and ii. documents statistically significant improvement on at least three quality measures and one efficiency (or cost) performance measure targeted by incentives over two years in at least three metropolitan markets. Plans using steerage strategies for their I&R programs should calculate % achieved savings compared to other plan benefit designs, in lieu of ROI. Fully Met Partially Met Not Met In at least ten metropolitan markets, the plan has either licensed and implemented the Leapfrog Hospital Rewards Program or implemented another hospital I&R program. In at least one metropolitan market, the plan has either licensed and implemented the Leapfrog Hospital Rewards Program or implemented another hospital I&R program. The plan’s I&R program meets all of the following criteria: i. targets network hospitals that account for at least 50% of plan admissions in each market; ii. uses standardized measures of hospital performance; iii. includes non-financial incentives (e.g., published performance ratings) related to hospital performance on targeted measures, and iv. includes financial incentives that annually equate to at least 2% of annual plan payments to I&R-participating hospitals.2 The plan’s I&R program meets all of the following criteria: i. targets network hospitals that account for at least 50% of plan admissions in the market; ii. uses standardized measures of hospital performance; iii. includes non-financial incentives (e.g., published performance ratings) related to hospital performance on targeted measures, and iv. includes financial incentives that annually equate to at least 2% of annual plan payments to I&R-participating hospitals. PARTIALLY MET Anthem uses standardized, nationally endorsed hospital performance metrics across its programs, including metrics endorsed by organizations like the National Quality Forum (NQF), the Hospital Quality Alliance (HQA), the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and “Steerage strategies” using quality-based benefit design products are considered to represent one possible I&R strategy that insurers can employ to address this goal. 2 For quality-based benefit design products, performance relative to the 2% criterion should be evaluated within 24 months of introduction in each market. For all other I&R strategies, performance relative to the 2% criterion should be evaluated within 18 months of introduction in each market. 1 8 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 3rd Pillar: Incentives and Rewards No. 2007 Goal Exceeded Fully Met Partially Met Not Met others. Our hospital pay-for-performance programs include over 500 facilities in twelve states. Most widespread is the Anthem Quality-In-Sights®: Hospital Incentive Program (Q-HIPSM) in six states. Anthem does not generally target hospitals for I&R programs based on volume of admissions. Anthem’s goal is to engage as many eligible providers as possible into pay-for-performance programs to drive positive health outcomes and increased patient safety. In the Virginia, California, Colorado, Indiana, Ohio, Missouri, and Kentucky markets, however, an estimated 50% or more of plan admissions do come from participating hospitals. Anthem Blue Cross and Blue Shield plans in the Indiana, Kentucky, Ohio, and Missouri markets hold annual educational conferences in each state. National quality improvement speakers attend, hospitals share best practices, and Anthem “Successful Practice” award winners are showcased at these conferences. Each year, hospitals are asked to submit abstracts on performance improvement projects they instituted at their facilities. The abstracts are reviewed by Anthem Medical Directors and three hospitals in each state are publicly recognized with awards at the annual educational conference. In addition, displaying performance across the quality metrics included in Anthem Blue Cross and Blue Shield in Virginia’s Quality-In-Sights®: Hospital Incentive Program (Q-HIPSM) for hospitals with ‘above-average’ scores is under development. This data would be displayed within the Anthem.com site and be available to all members and all commercial product lines. As of now, members can view which Virginia hospitals are participating in the program via an indicator displayed in the provider directory on the Anthem.com website. Whether the financial incentives provided under Anthem’s hospital I&R programs annually equate to at least 2% of annual plan payments to those hospitals cannot be evaluated at this time. Many of the programs are very new (2006 or 2007 rollouts) and others vary by individual hospital contracting arrangement. Program incentives are negotiated with the participating hospitals. In aggregate, Anthem paid out approximately $49 million in financial incentives in 2006 to hospitals participating in its pay-for-performance programs enterprise-wide. Anthem is building methodologies to appropriately and consistently calculate return-on-investment for pay-for-performance programs enterprise-wide and to quantify program results. 9 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 3rd Pillar: Incentives and Rewards No. 2007 Goal Exceeded 2 Design and implement an outpatient physician recognition strategy3 based on a standardized set of measures and lessons learned from I&R programs. Best Practice: Incentives and Rewards Best Practices Primer: Lessons Learned from Early Pilots, July 2006 (with support from Robert Wood Johnson Foundation and California Health Care Foundation). Find pdf of report at www.leapfroggroup.org or www.chcf.org In addition to meeting the fully met criteria, the plan meets all of the following criteria: i. calculates return-oninvestment for the I&R program(s) in all ten metropolitan markets, and ii. documents statistically significant improvement on at least three quality measures and one efficiency (or cost) performance measure targeted by incentives in at least three metropolitan markets. Plans using steerage strategies for their I&R programs should calculate % achieved savings compared to other plan benefit designs, in lieu of ROI Fully Met Partially Met In at least ten metropolitan markets, plan has licensed and implemented one or more components of the Bridges to Excellence Program and/or has implemented another physician I&R program. In at least one metropolitan market, the plan has licensed and implemented one or more components of the Bridges to Excellence Program and/or has implemented a physician I&R program. The plan’s I&R program meets all of the following criteria: i. targets network physicians that account for at least 50% of plan physician payments in each market; ii. uses standardized measures of physician performance; iii. includes multiple reinforcing incentives, including non-financial incentives (e.g., published performance ratings) related to targeted physician performance, and iv. includes financial incentives that annually equate to at least 2% of annual plan payments to I&R-participating physicians. 4 Not Met The plan’s physician I&R program meets all of the following criteria: i. targets network physicians that account for at least 50% of plan physician payments in each market; ii. uses standardized measures of physician performance; iii. includes multiple reinforcing incentives, including non-financial incentives (e.g., published performance ratings) related to targeted physician performance, and iv. includes financial incentives that annually equate to at least 2% of annual plan payments to I&R-participating physicians. FULLY MET “Steerage strategies” using quality-based benefit design products are considered to represent one possible I&R strategy that insurers can employ to address this goal. 4 For quality-based benefit design products, performance relative to the 2% criterion should be evaluated within 24 months of introduction in each market. For all other I&R strategies, performance relative to the 2% criterion should be evaluated within 18 months of introduction in each market. 3 10 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 3rd Pillar: Incentives and Rewards No. 2007 Goal Exceeded Fully Met Partially Met Not Met Anthem is building methodologies to appropriately and consistently calculate return-on-investment for pay-for-performance programs enterprise-wide and to quantify program results. Anthem does not generally target physicians for I&R programs based on the percentage of plan payments they account for. Participation in pay-forperformance programs is voluntary and is offered to the physician types being targeted (e.g. primary care physicians, OB/GYNs, cardiologists, etc.) by the program who meet minimum eligibility thresholds, not the entire network. Physicians who are interested in working with Anthem to improve quality as part of a contracting strategy are targeted. Anthem also looks for groups that are interested in working together on an ongoing basis to keep the measures fresh and continually evolve the P4P program. Anthem’s goal is to engage as many eligible providers as possible into pay-for-performance programs to drive positive health outcomes and increased patient safety. Given that half of our physician pay-for-performance programs are targeted at primary care physicians, and most of the others are targeted at specific specialty types, it is difficult to achieve the 50% of plan payments in the market threshold. In the Indiana, Missouri, and Ohio markets, however, it is estimated that this threshold is met. We use standardized, nationally endorsed physician performance metrics across our programs, including those metrics endorsed by organizations like the National Quality Forum (NQF), the AQA (formerly Ambulatory Care Quality Alliance), the National Committee for Quality Assurance (NCQA), and others, in areas for which endorsed measures are available. However, for a number of medical specialties and diseases, there are no nationally endorsed quality metrics. Anthem’s approach to identify metrics for these diseases and specialties is to work directly with national medical specialty societies to promote the development of performance metrics. Performance scorecards for medical groups participating in our pay-for-performance Physician Quality Incentive Program (PQIP) through the statewide Integrated Healthcare Association (IHA) collaborative in California are available publicly on Blue Cross of California’s website. Members can view and compare results across medical groups. The reported information includes: clinical measures (an aggregate measure of screening, immunization, and chronic disease management measures); service satisfaction; and complaint resolution. See http://www.bluecrossca.com/wps/portal/chpmemberbcc?content_path=shared/noapplication/medcalparticipants/nosecondary/notertiary/pw_a087005.htm &label=Physician/Medical%20Group%20Quality. In addition, BlueCross BlueShield of Georgia plans to review administrative requirements for physician groups participating in the pay-for-performance program there that have the highest scores, in an effort to streamline, simplify, and/or eliminate appropriate requirements (“goldcarding”). The financial incentives provided under Anthem’s physician I&R programs in California are estimated to represent at least 2% of annual plan payments to participating providers. In aggregate, we paid out approximately $96 million in financial incentives in 2006 to physicians participating in our pay-forperformance programs enterprise-wide. Anthem signed an enterprise licensing agreement with Bridges to Excellence (BTE) in September 2006. Anthem plans to continue its existing regional initiative in Georgia, and to expand to additional geographies across the enterprise, likely beginning with Ohio and Kentucky. We will also integrate BTE components into pay-for-performance programs and enhance online provider directories to indicate BTE designations. 11 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT No. 2007 Goal Fully Met Partially Met 3 Support Leapfrog’s Never Events Policy The plan meets both of the following criteria: i. The plan documents support of this Leapfrog goal. ii. The plan actively encourages its contracted hospitals to implement Leapfrog’s Never Events Policy. The plan documents support of Leapfrog’s Hospital Policy (See the Leapfrog Hospital Quality and Safety Survey) The following states required public reporting of Never Events as of February 2007: htww.pstoolbox.org/_docdisp_page.cfm? LID=6BC2AB7D-6F1E-4DF2AD20DAE18001147B Not Met Best practice: HealthPartners (MN) stipulates that contracted hospitals must report Never Events that occur to plan members and that the hospital will not pay for costs associated with Never Events. FULLY MET Anthem is in full support of the Never Events policy. We have finalized boiler plate language related to Never Events for the enterprise hospital agreement templates. See the “Never Events Hospital Agreement_4-5-07” supplemental document. As hospital agreements come up for renewal, we will begin to include this language as part of the standard contract. It is expected that his language will be incorporated into the majority of hospital agreements within the next three years. C:\PPU\External Organizations\Leapfrog\Score Sheet 2007\Response Supplements\Never Events Hospital Agreement_4-5-07.doc 4 Encourage physicians to employ electronic prescribing technology. The plan meets both of the following criteria: i. The plan utilizes incentives to encourage and assist physician practices to employ electronic prescribing technology in at least 10 metropolitan markets. ii. The plan reports that in at least two metropolitan markets, 25 percent or more network physicians are employing electronic prescribing technology The plan utilizes incentives to encourage and assist physician practices to employ electronic prescribing technology in at least 10 metropolitan markets. PARTIALLY MET 12 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT No. 2007 Goal Fully Met Partially Met Not Met Electronic prescribing is a component of several physician pay-for-performance programs. Anthem Blue Cross and Blue Shield plans in Connecticut, Maine, and New Hampshire include e-prescribing in the Technology/Structure section of their program scorecards. Provider groups can earn points by having electronic prescribing installed and in use by the end of the measurement period. Anthem Blue Cross and Blue Shield in Virginia rewards PCPs participating in its statewide pay-for-performance program that have electronic medical records that meet certain criteria, including decision support tools using evidence-based medicine for pharmacy management – this includes electronic prescribing technology. Blue Cross of California’s pay-forperformance program allocates 20% of the overall score for medical groups to information technology measures, which include electronic prescribing. The physician pay-for-performance program in Greater Cincinnati and Dayton, OH evaluates and scores use of electronic medical records. Both components of the EMR metric must be met to receive credit: (1) the system must be able to store prescription information which allows the system to identify allergies and potential drug interactions, and (2) the system must be able to identify patients with chronic diseases and specific disease management requirements (e.g. HgbA1c in diabetics, flu vaccine in asthmatics, etc.). Anthem Blue and Cross Blue Shield in Ohio has begun a pilot e-prescribing initiative with General Motors. It will involve 100 physicians and benefit thousands of patients in Dayton, Ohio. The pilot will equip the participating physicians with computer hardware and software that provide instant access to health plan formularies and patient medical histories. It will allow them to send prescriptions electronically to retail and mail order pharmacies. Specifically, the targeted physicians have been offered free use of software needed for e-prescribing through MedPlus, a subsidiary of Quest Diagnostics, as well as a $1,000 subsidy on the purchase price of a specific computer for use in the pilot. All groups that are also participating in the local Anthem payfor-performance program can also earn financial incentives by adopting and utilizing e-prescribing. The program is still too new to evaluate utilization of e-prescribing by the physicians. We are committed to e-prescribing as a mechanism for reducing medication errors and providing more affordable care. This e-prescribing pilot will be rolled out to additional markets. We will also be conducting studies to evaluate the impact on patient safety from eprescribing (e.g. reductions in drug-drug interactions). See “ePrescribing recruitment letter – Dayton – 7 21 06 All” document for a sample of the letter that went out to physicians introducing the pilot. In comparing results across plans, we caution that criteria (ii) can be evaluated differently by different plans. For example, should a physician that used eprescribing for just one script out of, say, a thousand count as a physician utilizing e-prescribing and be counted towards the 25% target? We announced participation and collaboration with RxHub in February 2007, further demonstrating our support of e-prescribing. Anthem is also a partner in the National E-Prescribing Patient Safety Initiative (NEPSI), a new coalition of technology companies, health care companies, and physician groups that is dedicated to improving patient safety and eliminating medication errors by providing access to free electronic prescribing for every physician in America. Anthem will play a key role in funding this program. *Please contact Anthem or Leapfrog staff for additional information. 13 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 4th Pillar: Opportunity Rate No. 2007 Goal 1 Calculate and share the plan’s opportunity rate on both an aggregate and employerspecific basis using the Leapfrog methodology. Fully Met Partially Met Not Met The plan meets all of the following criteria: i. The plan calculated and submitted to Medstat the plan’s opportunity rate using the Leapfrog Group methodology https://leapfrog.medstat.com/or/ ii. The plan shares the plan’s current opportunity rate score with employers. iii. The plan shows 10% improvement over the Leapfrog overall opportunity rate reported by the plan in 2005/2006. The plan meets each of the following criteria: i. The plan calculated and submitted to Medstat the plan’s opportunity rate using the Leapfrog Group methodology https://leapfrog.medstat.com/or/ ii. The plan either shares the plan’s current opportunity rate score with employers OR the plan shows 5% improvement over the Leapfrog overall opportunity rate the plan reported in 2005/2006. PARTIALLY MET Anthem has been working very closely with Medstat over the past several weeks to calculate the opportunity rate. We will report our opportunity rate score when it is available. 2007 will serve as our baseline year. 14 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 5th Pillar: External Collaboration No. 2007 Goal 1 Define an implementation strategy to work collaboratively with the 31 Leapfrog Group Regional Roll-Out leads to increase hospital reporting of the Leapfrog hospital survey and increase implementation of the Leapfrog patient safety and quality practices. Fully Met Partially Met Not Met The plan meets all of the following criteria: i. The plan has designated an employee in each of the 31 defined Leapfrog Group Regional Roll-Out (RRO) areas where the plan has covered lives to act as a RRO liaison and coordinate efforts to increase hospital reporting and implementation of the Leapfrog patient safety and quality practices5. ii. The plan has contacted each of the RROs and offered to develop a collaborative strategy designed to increase survey reporting and implementation of leaps. iii. The plan liaison with each RRO actively participates in at least 50% of RRO meetings and calls as requested by the RRO and has submitted the attached tracking sheet to reflect achievement of this metric. The plan meets both of the following criteria: i. The plan has designated an employee in each of the 31 defined Leapfrog Group Regional Roll-Out (RRO) areas where the plan has covered lives to act as a RRO liaison and coordinate efforts to increase hospital reporting and implementation of the patient safety and quality practices. ii. The plan has contacted each of the RROs and offered to develop a collaborative strategy designed to increase survey reporting and implementation of leaps. FULLY MET Fourteen Regional Roll-Outs covering eleven states overlap markets in which Anthem has commercial business. See “RRO_List0207_Anthem Overlap” to see those RROs and their leaders. We have identified individual contacts to actively participate in each of the RROs. Though not formally participating in the RROs to date, Anthem has been involved in local activities to increase Leapfrog survey reporting and implementation of the Leaps. For example, Anthem Blue Cross and Blue Shield in Ohio worked with Barbara Belovich of the Health Action Council, and RRO lead in Northeast Ohio, to send out a letter signed by health plans and employers to all hospitals that have not yet reported to the survey in April 2007. Similarly, Blue Cross of California’s Chief Medical Officer signed a letter coordinated by the Pacific Business Group on Health that was distributed to hospitals encouraging them to participate (see “PBGH CA letter” file). In addition, Dennis Matheis, President of Anthem Blue Cross and Blue Shield in Missouri joined the St. Louis Area Business Health Coalition, for which Louis Probst (the St. Louis RRO lead) is Executive Director, in signing a statement supporting the "cornerstones of value-driven health care" at a March 2, 2007 press conference led by Missouri Gov. Matt Blunt and U.S. Department of Health and Human Services Secretary Mike Leavitt. 5 Scorecard criteria relating to Regional Roll Outs apply only to RRO areas where the plan has covered lives. 15 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 5th Pillar: External Collaboration No. 2007 Goal Fully Met Partially Met Not Met Blue Cross of California also sent out its own letter to hospitals (see “2006_ltr to CA Hospitals” file). Anthem Blue Cross and Blue Shield in Colorado mailed a letter to hospitals (see “2006 CO Letter to Hospitals – Final” file). BlueCross BlueShield of Georgia annually mails a letter to network hospitals encouraging them to participate in the Leapfrog Survey (see “Leapfrog letter06 GA” file). This letter is sent to all participating hospitals in the Atlanta and Savannah areas that have not submitted Leapfrog Survey data. C:\PPU\External C:\PPU\External C:\PPU\External C:\PPU\External Organizations\Leapfrog\Score Organizations\Leapfrog\Score Sheet 2007\Response Organizations\Leapfrog\Score Sheet Supplements\PBGH 2007\Response Organizations\Leapfrog\Score CA Sheet Supplements\2006_ltr letter.pdf 2007\ResponseSheet Supplements\2006 to CA 2007\Response hospitals.doc COSupplements\Leapfrog Letter to Hospitals - Final.doc letter06 GA.doc 2 *Please contact Anthem or Leapfrog staff for additional information. Participate in coordinated hospital The plan participates in at least two of the performance measurement initiatives with following in a coordinated measurement other plans and/or with purchasers. initiative with other plans or with purchasers: i. standardized measures of hospital Best practice: performance, The Wisconsin Collaborative for ii. standardized measures for hospital Healthcare Quality is working to develop incentives, and/or iii. pooling data with other plan(s) to verifiable measures for public reporting. measure and report hospital http://www.wisconsinhealthreports.org/ performance. FULLY MET The plan participates in at least one of the following in a coordinated measurement initiative with other plans or with purchasers: i. standardized measures of hospital performance, ii. standardized measures for hospital incentives, and/or iii. pooling data with other plan(s) to measure and report hospital performance. The California Hospital Assessment and Reporting Taskforce (CHART): Implementation date: 2007; Pools data for hospital feedback, benchmarking, consumer rewards and payment rewards. CHART is a voluntary collaboration among hospitals and health plans in California. CHART has defined more than 50 hospital performance indicators that include process and outcome measures in specific clinical areas such as cardiac care, maternity, pneumonia treatment, and intensive care. They also include hospital-wide outcomes in areas such as patient experience, nursing-sensitive measures, and appropriateness of cardiac procedures. The measures are aligned with national initiatives such as the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) and the National Quality Forum (NQF). More than 200 hospitals, representing 70% of all hospital admissions in California, agreed to participate in the voluntary effort. The major health plans working in California [Blue Cross of California, Blue Shield of California, Health Net, and PacifiCare] have agreed to use the data as the basis for quality reporting and have committed to providing some financial support. Government and regulatory agencies are actively supporting the effort, including the California Office of Statewide Health Planning and Development (OSHPD) and JCAHO, as well as the PBGH and CalPERS. Program details can be viewed at http://www.chcf.org/topics/hospitals/index.cfm?itemID=111065. The Colorado Health and Hospital Association (CHA) Performance and Quality Group is a collaborative effort by twelve major health care, business, and governmental organizations. Participants include Colorado Hospitals Quality Managers, Colorado Business Group on Health, Colorado Medical Society, Centers for Medicare and Medicaid Services, Colorado Foundation for Medical Care, COPIC, Business Council on Health Care Competition, Physician Health Partners, Colorado Health Institute, Colorado Association of Health Plans, and the Colorado Department of Public Health and Environment. Anthem Blue Cross and Blue Shield in Colorado is part of this collaborative. This group has selected quality indicators, and encouraged 16 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 5th Pillar: External Collaboration No. 2007 Goal Fully Met Partially Met Not Met Colorado hospitals to voluntarily release these quality indicators to the public. The group has overseen the development and publication of the data. This website provides additional information: http://www.hospitalquality.org/. Care Focused Purchasing (CFP) is a Mercer-led initiative to aggregate claims data from participating health plans (Anthem, Aetna, CIGNA, FiservHealth, Humana, Preferred Care, and Regence BlueShield) and self-insured claims data from participating employers. The data will be housed in a repository and be available to measure quality and efficiency at the provider level. Priorities include: 1) standardized performance measures of quality and efficiency for hospitals and physicians; 2) produce detailed information request to measure quality and efficiency; 3) share provider performance measures; 4) open and accessible information about hospital and physician performance. Blue Health Intelligence (BHI) is another data pooling initiative Anthem is participating in. There are 20 Blues plans participating covering 79+ million members in the Blues system. This will be the deepest data repository available when completed. 17 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 5th Pillar: External Collaboration No. 2007 Goal 3 Participate in coordinated physician performance measurement initiatives with other plans and/or with purchasers. Fully Met The plan participates in at least two of the following in a formally coordinated initiative with other plans/purchasers: i. standardized measures of physician Best practice: performance, Massachusetts Health Quality Partners is ii. standardized measures for physician a broad-based health care coalition to incentives, and/or promote valid, comparable measures to iii. pooling data with other plan(s) to measure drive quality improvement. and report physician performance. www.mhqp.org/default.asp?nav=010000 FULLY MET Partially Met Not Met The plan participates in at least one of the following in a formally coordinated initiative with other plans/purchasers: i. standardized measures of physician performance, ii. standardized measures for physician incentives, and/or iii. pooling data with other plan(s) to measure and report physician performance. California Pay for Performance Program, Integrated Healthcare Association (IHA): Implementation date: 2004; Pools data for physician feedback, benchmarking, consumer reporting and payment rewards. Participants: Integrated Healthcare Association; California Health Plans: Aetna, Blue Cross of California, Blue Shield of California, CIGNA, Health Net, PacifiCare, Western Health Advantage; 225 Physician organizations representing 35,000 California Physicians. Measures include: appropriate long-term medication use for people with asthma, cardiac hyperlipidemia (LDL controlled <130 mg/dL & lipid management), diabetes (A1c test annually, A1c poorly controlled, LDL controlled <130 mg/dL, and nephropathy monitoring), preventive care for children (immunization status), preventive care for women (breast cancer, cervical and Chlamydia screenings), and the appropriate use of antibiotics in children with URI. Improving Performance in Practice (IPIP) Program, Colorado Clinical Guidelines Collaborative. Implementation Date: 2006; Integrates quality improvement and data collection methods into practices; pools data from multiple sources into disease management registry for physician feedback, benchmarking and (in the long-term) consumer reporting. It also prepares physicians to participate in local P4P programs. Participants include (currently have over 50 participants): Colorado Clinical Guidelines Collaborative; Colorado Health Plans: Anthem Blue Cross and Blue Shield in Colorado, Aetna, CIGNA, Colorado Access, Kaiser Permanente, UnitedHealthcare, and other, smaller plans; Medical Groups: Exempla Physician Group, MedSouth, New West Physicians, Physician Health Partners, University Physicians, and others; Medical Societies: Colorado Medical Society, American Academy of Family Physicians, American Academy of Pediatrics, American Cancer Society, and others; Employer participants: Colorado Business Group on Health; Hospital Systems: Exempla, HCA, The Children’s Hospital and University of Colorado Health Sciences Center. Measures include: diabetes (A1c testing & control, eye exam, blood pressure, LDL and LDL control, foot exam, smoking status, etc.) and asthma (medication management, influenza vaccinations, documented action plan, smoking assessment and cessation counseling). Quality Health 1st of Indiana program, Indiana Health Information Exchange (IHIE): Implementation date: 2007; Pools data from multiple payer sources for physician feedback, benchmarking, consumer reporting and payment rewards. Participants: Indiana Health Information Exchange; Indiana Health Plans: Anthem Blue Cross and Blue Shield in Indiana, M-Plan, MDwise, Medicare, UnitedHealthcare, and Humana; Medical Groups: Clarian Health Partners, Community Physicians of Indiana, IU Medical Group, Methodist Medical Group, St. Francis Medical Group, St. Vincent Physician Network, The Care Group and American Health Network. Measures include: children’s health (strep testing, URI), women’s health (breast, cervical and 18 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 5th Pillar: External Collaboration No. 2007 Goal Fully Met Partially Met Not Met Chlamydia screenings), diabetes (A1c testing and control, lipid profile and control, nephropathy) and appropriate medications for people with asthma. There is an initiative in Maine run through the Maine Health Management Coalition (MHMC) called Pathways to Excellence (PTE). There are over 40 members, including employers (e.g. Hannaford Bros. and Maine State Employees), doctors, hospitals, and health plans [including Anthem Blue Cross and Blue Shield in Maine, Aetna, CIGNA, and Harvard Pilgrim]. The MHMC does obtain all payer data for their analysis and reporting, but this is not a pay for performance program. This is a reporting and information vehicle as they have listed this information online for consumers to access. Some of the other health plans in the area have rewarded the physicians based on the number of ribbons they receive from PTE, but that is entirely separate from the MHMC. Anthem submits monthly data feeds to the Maine Health Information Center (MHIC) who collects the data for the Maine Health Data Organization (MHDO). The file feeds consist of: eligibility, medical claims and prescription drug claims for fully insured and ASO business across all product lines; and line level detail for medical claims and prescription drugs. Per the state mandate, we submit data for Maine residents that are insured by Anthem. Per a separate agreement, we submit data for the Coalition firms' out of state members. Anthem has worked closely with the MHMC to utilize their technology survey so the physicians, when applicable, would not have to enter two surveys. We receive that data back from the MHMC and feed it into our existing P4P program. However, that is only one component of our existing P4P program and the only piece of information we currently use from the MHMC. More information on the MHMC can be found at: http://www.mhmc.info. Care Focused Purchasing (CFP) is a Mercer-led initiative to aggregate claims data from participating health plans (Anthem, Aetna, CIGNA, FiservHealth, Humana, Preferred Care, and Regence BlueShield) and self-insured claims data from participating employers. The data will be housed in a repository and be available to measure quality and efficiency at the provider level. Priorities include: 1) standardized performance measures of quality and efficiency for hospitals and physicians; 2) produce detailed information request to measure quality and efficiency; 3) share provider performance measures; 4) open and accessible information about hospital and physician performance. 4 Blue Health Intelligence (BHI) is another data pooling initiative Anthem is participating in. There are 20 Blues plans participating covering 79+ million members in the Blues system. This will be the deepest data repository available when completed. Support hospital participation in the IHI’s The plan creates incentives and rewards for The plan creates incentives and rewards for 5 Million Lives campaign to encourage facilities to succeed in the 5M lives Campaign facilities to succeed in the 5 Million lives hospital progress towards patient safety Lives Campaign by doing at least three of the campaign by doing at least two of the following: and quality following: i. publicly recognizing hospitals i. publicly recognizing hospitals participating in IHI 5 Million Lives http://www.ihi.org/IHI/Programs/Campai participating in IHI 5 Million Lives campaign. gn/ campaign. ii. financially rewarding effective ii. financially rewarding effective organization-wide introduction of the organization-wide introduction of the Campaign interventions. Campaign interventions. iii. supporting hospital participation by iii. supporting hospital participation by offering financial assistance for related offering financial assistance for related improvement work or by subsidizing improvement work or by subsidizing facilities to take part in Campaign facilities to take part in Campaign education sessions or meetings. education sessions or meetings. iv. hosting an expert-led learning session 19 of 20 2007 Health Plan Users Group Scorecard – 2-14-07 DRAFT 5th Pillar: External Collaboration No. 2007 Goal Fully Met iv. hosting an expert-led learning session on 5 Million Lives Campaign interventions and on the quality improvement methods known to drive change. Partially Met Not Met on 5 Million Lives Campaign interventions and on the quality improvement methods known to drive change. PARTIALLY MET Anthem’s hospital pay-for-performance programs already allocate points towards implementation of the interventions included in IHI’s 100,000 Lives Campaign (e.g. deployment of rapid response teams). In addition, some of the individual metrics within the new 5 Million Lives Campaign intervention domains are included in existing hospital P4P programs (e.g. ACEI/ARB for LVSD, D2B time for primary PCI, and discharge instructions rate for heart failure). The enterprise Hospital Measures Workgroup is discussing how to pull additional interventions and indicators into P4P programs. Anthem has initiated discussions with hospitals participating in the Quality-In-Sights®: Hospital Incentive Program (Q-HIPSM) in Connecticut, Maine, New Hampshire, Virginia, Georgia, and New York regarding the inclusion of 5M Lives Campaign interventions into the program. Anthem Blue Cross and Blue Shield in Indiana, Ohio, Missouri, and Kentucky are asking network hospitals if they have signed up for the 5M Lives Campaign. Several of the Campaign indicators will be added to the 2007 hospital RFI in those states (e.g. VTE prophylaxis and treatment, infection control guidelines for MRSA, conducting active surveillance cultures on all admitted patients, reducing pressure ulcer occurrence, some SCIP measures, and some of the CHF measures). An article on the 5M Lives Campaign is being included in upcoming plan newsletters to providers across all Anthem plans enterprise-wide, giving information on the Campaign and encouraging hospitals to participate. See “IHI 5M article_Template” document for the template article used by each plan. The Blue Cross and Blue Shield Association gave $5 million to IHI, a significant portion of which came from Anthem, to help get the 5M Lives Campaign off the ground and demonstrate support for the initiative. C:\PPU\External Organizations\Leapfrog\Score Sheet 2007\Response Supplements\IHI 5M article_Template.doc 20 of 20