Silva, AT., Chung, MC., Castro, LF., Guido, RV. and Ferreira, EI.
advertisement
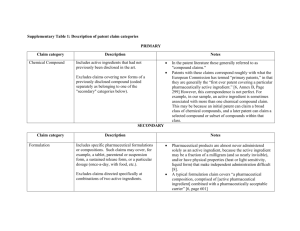
PHARMACOLOGY AND TOXICOLOGY OF PRO DRUG AND SOFT DRUG Chukewar A. B.1, Modi C. M. 1, Sudhir kale1, Mody S.K. 1 and Patel H. B.1 1 Department of Pharmacology and Toxicology, College of Veterinary Science and Animal Husbandry, Sardarkrushinagar Dantiwada Agricultural University, Sardarkrushinagar, Gujarat, India-385 506 ABSTRACT: Nowadays, we try to design new drugs that heal sick people having the best acceptance. These drugs must be efficient and selective on their site of action and metabolized to non toxic products. Both prodrug and soft drugs should have good distributive properties to enhance their quality. Prodrug- pharmacological inactive compound converted into active drug in vivo. According to The International Union of Pure and Applied Chemistry (IUPAC), the term of prodrug is defined as “Any compound that undergoes biotransformation before exhibiting its pharmacological effects” (IUPAC 1998). To overcome toxicity and limitation in cancer chemotherapy different therapies developed to treat cancer. New techniques are developed like gene-directed enzyme prodrug therapy (GDEPT) or virus-directed enzyme prodrug therapy (VDEPT) and Antibody Directed Enzyme Prodrug Therapy (ADEPT) used to treat solid tumor by introducing suicide genes and by using combination of antibody, enzyme and prodrug to treat solid tumor. Lectin-directed enzyme-activated prodrug therapy (LEAPT) is a bipartite drug-delivery system used to reduced tumor. According to IUPAC definition, Soft drug “is a compound that is degraded in vivo to predictable nontoxic and inactive metabolites, after having achieved its therapeutic role”. Soft drugs used for identification of drugs toxicity, determination of drug pathway, identification of pharmacophore and modification of the parent molecule, introduced by Nicholas Bodar in1977. A number of already marketed drugs, such as esmolol, remifentanil, or loteprednol etabonate, resulted from the successful application of such design principles. Both, the prodrugs and the soft drugs are used to overcome several undesirable properties in order to achieve the best clinical drug application. Drug discovery and prodrug and soft drugs development appear 1 to be complementary for the generation of target specific medicines now and in the future. Key word: Pro drugs, Soft drugs, Pharmacology. INTRODUCTION Prodrugs can be defined as “pharmacologically inert chemical derivatives that can be converted in vivo to the active drug molecules, enzymatically or nonenzymatically, to exert a therapeutic effect”. Ideally, the prodrug should be converted to the original drug as soon as the goal is achieved, followed by the subsequent rapid elimination of the released derivatizing group. According to The International Union of Pure and Applied Chemistry (IUPAC), the term of prodrug is defined as “Any compound that undergoes biotransformation before exhibiting its pharmacological effects. Prodrugs can thus be viewed as drugs containing specialized non-toxic protective groups used in a transient manner to alter or to eliminate undesirable properties in the parent molecule” (IUPAC, 1998). Traditional prodrugs are classified in two main groups, 1) Prodrugs that convert polar groups on active molecules into cleavable and apolar fragments. 2) A second group that add solubility to the active moiety. Prodrugs are converted in vivo by two way metabolism, it is enzyme dependant and chemical methods not depend on enzyme, it consist of hydrolysis of drugs, decarboxylation, not patient dependant, stability or storage issues. HISTORY The term "prodrug" or "proagent" was first introduced by Albert to signify pharmacologically inactive chemical derivatives that could be used to alter the usefulness and/or to decrease associated toxicity (Albert, 1958), Since Albert discussed the concept of prodrugs in the late 1950s, such compounds have also been called "latentiated drugs," "bioreversible derivatives," and "congeners," but "prodrug" is now the most commonly accepted term (Roche, 1977). The prodrug approach gained attention as a technique for improving drug therapy in the early 1970s. Numerous prodrugs have been designed and developed since then to overcome pharmaceutical and pharmacokinetic barriers in clinical drug application, such 2 as low oral drug absorption, lack of site specificity, chemical instability, toxicity, and poor patient acceptance (bad taste, odor, pain at injection site, etc.) (Han, H.K. and Amidon, G.L. 2000). Prodrugs are used to improve patient acceptability, alter and improve absorption, biodistribution, metabolism, elimination. Stella and Himmelstein suggested that at least 3 factors should be optimized for the site-specific delivery of drugs by using the prodrug approach. 1. The prodrug must be readily transported to the site of action, and uptake to the site must be rapid and essentially perfusion rate limited. 2. Once at the site, the prodrug must be selectively cleaved to the active drug relative to its conversion at other sites. 3. Once selectively generated at the site of action, the active drug must be somewhat retained by the tissue (Stella et al., 1982). The prodrug is able to overcome one or more of the barriers to drug delivery more efficiently than the parent drug. These barriers include physicochemical properties and pharmacokinetic properties (Friend, D.R. and Chang, G.W. 1984). Physicochemical properties of prodrugs: It includes Poor aqueous solubility, It Prevents the drug from being administered in form of injectables, it gives rise to dissolution rate-limited and variable oral bioavailability, low lipophilicity it limits the design of lipid-based formulations and chemical instability, it prevents the drug from being incorporated into adequate dosage forms. Pharmacokinetic properties: Incomplete absorption across biological membranes in gastrointestinal mucosa and blood-brain barrier, unfavourable metabolism and low and variable bioavailability due to extensive first-pass metabolism. Types of Prodrugs: There are two types of prodrugs Carrier-linked prodrugs and Bioprecursor prodrugs. Carrier-linked prodrug in which active drug linked to metabolically cleaved carrier group, carrier-linked prodrug are of three types, bipartate prodrug: one carrier attached to drug, tripartate prodrug: carrier attached to linker attached to drug, mutual prodrug: two usually synergistic drugs attached to each other (one acts as carrier for the other). 3 Bioprecursor prodrug: compound has no carrier but requires one or more steps of metabolic activation (oxidation, reduction etc.) Carrier-linked prodrugs are the drugs that are attached through a metabolically labile chemical linkage to another molecule designated as the “promoiety”.The “promoiety” alters the physical properites of the drug to increase water or fat solubility or provide site-directed delivery. Advantages of carrier-linked prodrugs are increased absorption, Injection site pain relief, elimination of unpleasant taste, decreased toxicity, decreased metabolic inactivation, increased chemical stability and prolonged or shortened action. Examples of Carrier-Linked Prodrug includes Alcohols as carboxylic acid or phosphate esters affects water solubility Also effects stability of prodrug, fast or slow unmasking. Use succinate ester for fast hydrolysis, in stomach acid for fast hydrolysis, use electron-releasing group, in blood or nonacidic tissues for fast hydrolysis, for slow ester hydrolysis, use poor substrates for esterases or phosphatases, for rapid ester hydrolysis, use good substrates for esterases or phosphatases. Amines can be turned into amide, N-Mannich base, or imine prodrugs Increase lipid solubility by lowering the pKa of amine nitrogen. Amides released by plasma amidases (good substrates: phenyl carbamates or peptides) example: water-soluble benzocaine prodrug, benzocaine is a topical anesthetic, N-Mannich base example: prodrug of the decongestant phenylpropanolamine hydrochloride, Imine example: progabide, blood-brain barrier-crossing prodrug of the anticonvulsant neurotransmitter GABA. Sulfonamides are acylated like amines, and hydrolyzed by plasma amidases, but are acidic and become water-soluble salts Example: The anti-inflammatory drug and COX-2 inhibitor valdecoxib (poor water solubility) is converted into parecoxib sodium aldehydes and ketones are converted into various acetal, thioacetal, or hydrolysable heterocycles as prodrugs. Phosphatase-activated drugs like procorticosteroid prednisolone phosphate and proantitumor drug etopside phosphate. Nonenzymatic activation of procorticosteroid methylprednisolone sodium succinate to unstable in solution, Better absorption and distribution Skin penetration very lipophilic, skin esterase-activated drugs flucinolone acetonide and flucinonide, prodrugs for treatment of inflammation and 4 itching Cornea penetration and dipivefrin is a prodrug for the antiglaucoma drug epinephrine. Tripartate Prodrugs of a bipartate prodrug is too labile or too stable, use a tripartate prodrug that puts a linker between the carrier and the drug. Enzyme-specific loss of linker causes spontaneous release of drug. Mutual Prodrugs commonly used for metastatic carcinoma of the prostate, promoiety also a drug. Prodrug is selectively taken up into estrogen receptor positive cells then urethane linkage is hydroylzed and formation of 17-alphaestradiol slow prostate cell growth. Sultamicillin a tripartate mutual prodrug of the b-lactam antibiotic ampicillin and the b-lactamase inactivator penicillanic acid sulfone. Bioprecursors prodrugs that are metabolized into a new compound that may be active or further metabolized to an active metabolite. The best known example of bioprecursor is acetaminophen, which is an O-deethylated metabolite of phenacetin. Acetaminophen shows superior analgesic activity when compared with phenacetin. The main advantage of acetaminophen over phenacetin is that it does not produce methemoglobinemia and hemolytic anemia (Wermuth, 1984). Examples: sulfasalazine is a prodrug. It is not active in its ingested form. It has to be broken down by bacteria in the colon into two products -- 5-aminosalicylic acid (5ASA) and sulfapyridine before becoming active as a drug. Oseltamivir is an ethyl ester prodrug of Ro 64-0802, a selective inhibitor of influenza virus neuraminidase. Oral administration of oseltamivir delivers the active antiviral Ro 64-0802 to the bloodstream, and thus all sites of influenza infection (lung, nasal mucosa, and middle ear) are accessible (He et al., 1999). Capecitabine (Xeloda®) was developed as a pro-drug of fluorouracil (FU), with the aim of improving tolerability and intratumor drug concentrations through its tumor specific conversion to the active drug. Better stability, propranolol hemisuccinate, blocks first-pass effect, so 8x greater serum levels of the antihyperyensive propranolol achieved. anthranilate and prodrugs of the opioid addiction treatment naltrexone, have 28-45 times greater serum levels than 5 naltrexone itself. Slow and prolonged release use long-chain aliphatic ester prodrugs are injected intramuscularly. Better patient compliance since the patient doesn't have to take the drug as often and there are fewer unpleasant side effects due to serum concentration peaks and valleys, gastrointestinal distress, and high concentration toxicity. Antipsychotic ester prodrugs of haliperidol and fluphenazine are active for a month instead of only a few hours. Lower Toxicity Ester prodrugs of aspirin are hydrolyzed by plasma pseudocholinesteraase, thus avoiding gastric irritation. Better Patient Compliance and where better compliance comes from less frequent drug administration and better drug performance and prodrug of the antibacterial clindamycin doesn’t hurt when injected. The acetyl prodrug of the pediatric antibacterial sulfisoxazole is tasteless. No formulation problems topical fungistatic prodrug triacetin is a solid that is hydrolyzed to the active agent acetic acid by skin esterases. Application of the prodrug approach: To identify suitable derivatives, to improve drug therapy when the physicochemical characteristics of a very interesting lead constitute an impediment to its further development, to improved competitiveness of the drug in the marketplace by the optimization of parameters like bioavailability or pharmacokinetic profile and for development of two or more dosage forms of the drug candidate. Prodrugs are used to improved oral absorption, dermal absorption, ocular absorption, prevention of first-pass metabolism and site-specific drug delivery it may be achieved by site-directed drug delivery or site-specific bioactivation and improvement of drug formulation. Characteristics of a prodrug: The changes in physicochemical properties and the pharmacological profile of the drug are transient, since the well-characterized parent drug molecule is regenerated in vivo. Introduction of a number of chemical transient changes in the drug molecule is possible, thus allowing prodrug derivatives with a broad spectrum of physicochemical properties to be considered. Prodrug formation can be considered as a means to mask temporarily undesirable physicochemical properties of the parent molecule. Ideal Property of Prodrug: 6 It should not have intrinsic pharmacological activity, It should rapidly transform into the active form where desired and metabolic fragment, apart from the active drug should be nontoxic. The design of prodrugs directed selectively to their site of action, should take into account the following basal criteria, the prodrug should be able to reach its site of action, the prodrug should be converted efficiently to the drug at the site of action and the parent active should to some extent be retained at the target site for a sufficient period of time to exert its effect. Prodrug readily transported to the site of action, prodrug is rapidly absorbed at the site, selective and rapid conversion to the active drug, Kidney and Liver are easy targets due to high perfusion and high metabolic rates and drug migrate slowly from site of action to a site of excretion. Advantages of a prodrug: Producing nontoxic nutrient byproducts when they regenerate the active drugs in vivo. There have been extensive studies on gastrointestinal enzymes, which provide necessary information e.g. enzyme distribution, activity, and specificity for prodrug design. Prodrugs are used to improve aqueous or lipid solubility of drugs, to direct the drug to specific site of action, Increase stability of drug, prolonged release: steady low drug concentration for long half-life, decrease toxicity: mostly activated at target tissue, so less random tissue damage, better patient compliance. Limitation of Prodrug: Its toxicity which is due to formation of unexpected metabolite from the total drug conjugates, due to inert carrier generated by cleavage of promoiety and drug conjugate which is converted into toxic metabolite. The prodrug might consume a vital cell constituent such as glutathione during its activation stage which causes depletion of prodrug. Drawback of prodrugs: The most serious drawback of prodrugs which do not require an enzymatic release of the the active agent is their inherent lability, which raises stability issues at least in case of liquid dosage forms. 7 Prediction of chemical reactivity through substituent effects is often possible from empirical linear free energy relationships (LFERs). In particular, neutral or alkaline hydrolysis of ester functions are facilitated by low electron density at the carbonyl carbon atom. This situation can be realized by introducing an electronegative substitute in a proper position of an aromatic ring or in an aliphatic chain. There are a number of small pharmaceutical and biotech companies dedicated to using prodrugs for the delivery of older but problematic drugs as well as to developing broad-based prodrug technologies for application to new and future drugs. These volumes represent a comprehensive guide to prodrugs and will guide the reader through the current status of the prodrug concept and its many applications and to highlight its many successes in overcoming formulation and delivery of problematic drugs. The newest therapies: Recently, new therapies have been proposed to overcome this limitation of prodrug therapy. These new approaches are referred to as an antibody-directed enzyme prodrug therapy (ADEPT) and gene-directed enzyme-prodrug therapy (GDEPT). The attempt is to localize prodrug-activating enzymes in specific cancer cells prior to prodrug administration. Appropriately designed drugs have been found to be effective in the treatment of human tumours possessing high levels of an activating enzyme. Cancer chemotherapy encompasses a large number of well-documented and clinically established methods for the treatment of malignant diseases. However, the efficacy of these approaches is often hampered by an insufficient therapeutic index, lack of specificity, and the emergence of drug-resistant cell subpopulations. One approach aimed at enhancing the selectivity of cancer chemotherapy for solid tumors relies on the application of gene therapy technologies. Clinical results were disappointing when it was found that human tumors containing appropriately high levels of the activating enzymes were rare and that the high levels of activating enzymes were not associated with any particular type of tumor. Recently, new therapies have been proposed to overcome this limitation of prodrug therapy (Bagshawe et al., 1993). Tumor cell targeting, ADEPT (Antibody-Directed Enzyme Prodrug Therapy) Tumor-specific antibody covalently linked to a nonhuman or rare enzyme that attaches to 8 the tumor cell, then the unbound conjugate is cleared and the prodrug (not cleaved by human enzymes) is administered. The tumor cell bound to the antibody-enzyme conjugate is killed and all nearby (mostly tumor) cells. GDEPT (Gene-Directed Enzyme Prodrug Therapy or suicide gene therapy) integrates the gene for the prodrug-activating antibody next to tumor-selective promoters. VDEPT (Virus-Directed Enzyme Prodrug Therapy) Retroviral vector needs dividing cells to work (only 6-20% of tumor cells) Possibility of reversion to pathogenic wild-type virus. The rationale behind this approach is that the transport properties of the macromolecular prodrug should be dictated predominantly by the macromolecular transport vector. In the field of cancer, chemotherapy design of such compounds have received considerable interest, since anticancer agents tend to be highly toxic and their effectiveness limited by a very small therapeutic ratio. Macromolecules endowed with intrinsic target receptor affinities (e.g. monoclonal antibodies and hormones) have been evaluated (Singh, et al., 2008). Prodrugs can be designed to target specific enzymes or carriers by considering enzyme-substrate specificity or carrier-substrate specificity in order to overcome various undesirable drug properties. This approach has two alternatives: Toxin gene therapy, in which the genes for toxic products are transected directly into tumor cells; enzymeactivating prodrug therapy, in which the transgenes encode enzymes that activate specific prodrugs to create toxic products. The latter approach, known as gene-directed enzyme prodrug therapy (GDEPT) or virus-directed enzyme prodrug therapy (VDEPT), may be used in isolation, such as the biotherapies. VDEPT using selectively replicating viruses as vectors represents a promising means to target suicide genes specifically to tumor cells (Silva, et al., 2005). The catalytic activity of the expressed protein must be adequate to activate the prodrug under physiological conditions. Because expression of the foreign enzymes will not occur in all cells of a targeted tumor in vivo, a bystander effect (BE) is required, whereby the prodrug is cleaved to an active drug that kills not only the tumor cells in which it is formed, but also neighboring tumor cells that do not express the foreign enzyme (Misiura, et al., 2002). 9 The enzyme-targeted prodrug approach can be broadly used to improve oral drug absorption, as well as site-specific drug delivery. In the case of improving oral drug absorption, gastrointestinal enzymes may be the main targets for prodrug design, and the use of a nutrient moiety as a derivatizing group permits more specific targeting for gastro-intestinal enzymes to improve oral drug absorption (Amidon, et al., 1980). Antibody Directed Enzyme Prodrug Therapy (ADEPT) ADEPT is a two-step treatment for cancer. In the first step, an antibody–enzyme conjugate is administered. The antibody is raised against tumor specific antigens and localizes to the tumor, carrying with it an exogenous enzyme. This is followed by administration of a prodrug, which is activated by the exogenous enzyme at the tumor site (Marais et al., 1996). ADEPT is a new type of cancer treatment that uses drugs called monoclonal antibodies. At the moment, ADEPT is being used only in clinical trials (Biela, et al., 2003). ADEPT procedure Enzymes that activate prodrugs can be directed to human tumor xenografts by conjugating them to tumor-selective monoclonal antibodies an antitumor antibody is conjugated to an enzyme not normally present in extracellular fluid or on cell membranes and then these conjugates are localized in the tumor via intravenous infusion. After allowing for the conjugate to clear from the blood, a prodrug is administered that is normally inert but is activated by the enzyme delivered to the tumor (Bagshawe, et al., 1987). Using different combinations of antibody, enzyme, and prodrug, many classes of human tumor xenograft have been shown to be very sensitive to this procedure, although in most cases they are quite resistant to conventional chemotherapy. Early clinical trials are promising and indicate that ADEPT may become an effective treatment for solid cancers for which tumor-selective antibodies are known (Connor, T.A. and Knox, R.J. 1995). (VDEPT) or more generally gene-directed enzyme prodrug therapy (GDEPT) has shown promising results in laboratory systems. In ADEPT, prodrug activation occurs extracellularly, whereas in GDEPT it occurs intracellularly. Therefore, the choice of enzymes can be different in those 2 approaches. The best enzymes for GDEPT would 10 appear to be monomeric enzymes of bacterial or viral origin with wide substrate specificity (Sharma, et al., 1992). One example is a bacterial nitroreductase that can convert a relatively nontoxic monofunctional alkylating agent into a 10,000 times more cytotoxic difunctional alkylating agent. Because nitroreductases require either NADH or NADPH as an essential reductant, activation of prodrugs can only take place within the cells. Therefore, this enzyme may be a better choice for GDEPT than for ADEPT. In contrast, charged prodrugs that are bifunctional alkylating agents are especially suitable for ADEPT (Haisma, et al., 1992). Because of the charge, they will not enter cells and are nontoxic because the essential target for alkylating agents is intracellular DNA. After extracellular activation of prodrugs in tumor cells, the active drug will be freely diffusible and attain a high intracellular concentration (Connor, T.A. and Knox, R.J. 1995). Thus, alkylating prodrugs activated by β-glucuronidase or carboxypeptidase G2 as glucuronic or glutamic acid derivatives should be excellent for ADEPT (Tsuji, et al., 1996). Gene Directed Enzyme Prodrug Therapy (GDEPT) GDEPT and VDEPT are two-step treatments for solid tumors. In the first step, the gene for a foreign enzyme is delivered and targeted in a variety of ways to the tumor where it is to be expressed. In the second step, a prodrug is administered that is selectively activated to the drug by the foreign enzyme expressed in the tumor. Ideally, the gene for the enzyme should be expressed exclusively in the tumor cells and should reach a concentration sufficient to activate the prodrug for clinical benefit. Gene therapies are techniques for modifying the cellular genome for therapeutic benefit. In cancer gene therapy, both malignant and nonmalignant cells may be suitable targets. The possibility of rendering cancer cells more sensitive to chemotherapeutics or toxins by introducing “suicide genes” was suggested in the late 1980s. GDEPT, a form of suicide gene therapy, aims to maximize the effect of a toxic drug and minimize its systemic effects by generating the drug in situ within the tumor. In the first step in this procedure, the gene for an exogenous enzyme is delivered and expressed in the tumor cells. Subsequently, a prodrug is administered that is converted to the active drug by the foreign enzyme expressed inside or on the surface of tumor cells. This type of site-specific drug delivery has been of particular concern in cancer chemotherapy. 11 Appropriately designed prodrugs have been found to be effective in the treatment of animal tumors possessing high levels of an activating enzyme (Deonarain, 1995). A range of prodrugs causes a dramatic decrease in xenograft tumour volume and many cures are observed in both xenograft models. Tumours that re-grow after initial treatment respond to further administration of the prodrug, indicating that the gene is stable and active in the long term. In vivo models of human hepatocellular carcinoma treated with a single intravenous systemic dose of adenoviral vectors showed tumour-selective replication of adenoviruses and expression of CPG2, not found in normal tissues. Levels of CPG2 greatly exceeded those previously shown to be sufficient to cause regression of the tumours following administration of the prodrug. Thus the adenoviral vectors show great promise for efficacy in GDEPT protocols. (Cancer Research UK Centre for Cancer Therapeutics) Effective tumor destruction with GDEPT depends on the design of the genetherapy vectors, the chemistry of the prodrugs and their toxic metabolites, and the means to deliver one or both components specifically to target cells. Prodrugs for GDEPT must be considerably less cytotoxic than their corresponding active drugs, and must be suitable substrates for the activating enzyme under physiological conditions. In addition, they should be chemically stable under physiological conditions and diffuse readily in the tumor interstitium. They should also have good pharmacological and pharmacokinetic properties, and release an active drug with a good BE. Prodrugs must also be tailored to their site of activation: if activation occurs intracellularly, they must be able to cross the tumor cell membrane. Appropriate combinations of enzymes and prodrugs proposed for ADEPT and GDEPT approaches are: Approach Enzyme ADEPT Carboxypeptidase A Prodrug Drug Methotrexate alanine Methotrexate 12 ADEPT B - Glucuronidase Epirubicin glucoronide GDEPT Thymidine kinase Ganciclovir GDEPT Cytosine deaminase GDEPT Nitroreductase Epirubicin Ganciclovir triphosphate 5-Fluorocytosine 5-Fluorouracil 4-nitrobenzyloxy carbonyl derivative Actinomycin D Tumors have also been targeted with genes encoding prodrug-activating enzymes (Huber, et al., 1994). This approach can use a viral vector (e.g. retroviral or adenoviral) to carry a prodrug-activating enzyme gene into both tumor and normal cells (Misiura et al., 2002). By linking the foreign gene downstream of tumor-specific transcription units, tumor-specific expression of the foreign enzyme gene can be achieved. This approach has been called virus-directed enzyme prodrug therapy. Virus-directed enzyme prodrug therapy: A viral vector encoding an enzyme that can convert an inactive prodrug to a cytotoxic metabolite infects the tumour cell. When the prodrug is administered, expression of the enzyme in the tumour cell leads to production of the cytotoxic metabolite and results in direct tumour cell killing, as well as a bystander effect that kills nontransfected neighboring cells through transfer of toxic metabolites. Lectin-directed enzyme-activated prodrug therapy (LEAPT) Is a bipartite drug-delivery system that exploits endogenous carbohydrate to lectin binding to the localized glycosilated enzyme conjugates to specific, predetermined cell types followed by administration of a prodrug activated by that pre-delivered enzyme at the desired site. LEAPT approach uses two components, the cell-specific delivery of a synthetically glycosylated enzyme and non-mammalian glycosidase enzyme (Robinson et al., 2004). Site selective delivery of a glycosylated rhamnosidase (Rha-cleaving) enzyme by sugar-mediated RME. Delivery of a Rha-capped prodrug that can be cleaved only by the 13 delivered glycosylated rhamnosidase. When these two steps are combined, activation of the prodrug results in site-selective release of the parent drug. Polymer-directed enzyme prodrug therapy (PDEPT) Is a novel two-step antitumor approach that uses a combination of a polymeric prodrug and polymer-enzyme conjugate to generate a cytotoxic drug rapidly and selectively at the tumor site (Satchi et al., 2003). Non-Prodrugs “Hard Drugs” - compounds that contain structural characteristics required for activity but are not susceptible to metabolism. “Soft Drugs” - These are the opposite of prodrugs. These compounds are designed and synthesized as active compounds that readily undergo metabolic inactivation to nontoxic products. Soft drug: According to IUPAC definition, soft drug “is a compound that is degraded in vivo to predictable nontoxic and inactive metabolites, after having achieved its therapeutic role”. It should be an isosteric or isoelectronic analogue of the parent drug. The rational design of soft drugs can be divided into the following steps: I) Identification of drug toxicity problem; ii) Determination of metabolic pathways of drug in the body iii) Identification of pharmacophore in the molecule iv) Modification of the parent molecule in such a way that it shows good therapeutic efficacy at site of action but undergoes metabolism in a controlled and predictable manner to form inactive non toxic moiety when distributed away from this site. Soft drugs are new active therapeutic agents obtained by building into the molecule a detoxification route in addition to activity. Desired activity is generally local and these agents are administered or applied at or near the site of action. Therefore, in most cases they produce pharmacological activity locally but their distribution away from the site results in immediate metabolic deactivation that prevents any kind of toxicity. The aim for designing soft drugs is not to avoid metabolism but to control and direct it. Soft Drugs vs. Hard Drugs: 14 Hard drugs: Ariens’s theoretical, drug design concept of non-metabolizable drugs some strongly lipophobic drugs, such as enalaprilat, lisinopril,cromolyn, and bisphophonates (e.g., alendronate), are not metabolized in vivo, and can be considered as hard drugs (Bodor et al., 2003). Soft Drugs vs. Prodrugs: Prodrugs: pharmacologically inactive compounds that result from transient chemical modifications of biologically active species (Albert, 1958) chemical change is introduced to improve some deficient physicochemical property, such as membrane permeability or water solubility, or to overcome some other problem, such as rapid elimination, bad taste, formulation difficulty, patentability (Bodor et al., 2003). History Nicholas Bodor was the first one who introduced the idea of soft drugs in 1977. According to this concept, soft drugs have been divided into four categories as follows: soft analogues, inactive metabolite-based soft drugs, active metabolite-based soft drugs and pro-soft drug (Friend, D.R. and Chang, G.W. 1984). Soft Analogs: close structural analogues of known active drugs that have a specific metabolically sensitive moiety built into their structure. Inactive Metabolite-Based Soft Drugs: active compounds designed starting from a known (or hypothetical) inactive metabolite of an existing drug. Active Metabolite-Based Soft Drugs: metabolic products of a drug resulting from oxidative conversions at the highest oxidation state that still retains activity. Pro-Soft Drugs: inactive prodrugs of a soft drug (Bodor, 1984). Soft analogues: Soft analogues have a specific metabolically sensitive moiety built into their structure to allow for a facile, one-step controllable deactivation and detoxification after the desired therapeutic role has been achieved. Soft anticholinergics used as antiperspirants or as mydriatic agents (Huang et al., 1998). Inactive metabolites: Soft drugs are active compounds designed starting from a known or hypothetical inactive metabolite of an existing drug by converting this metabolite into an isosteric/isoelectronic analogue of the original drug. Loteprenolol etabonate is structurally similar to other corticosteroids (Rapaka, 1995). 15 Active metabolites: Compounds or metabolic products of a drug that retain the same affinity as the parent drug. Reasonable selection of an active metabolite can lead to a potent drug that will undergo a one-step deactivation process, since it is already at the highest oxidation state. Pro-soft drugs: They are metabolized through enzymatic transformation into the active soft drug (Bodor et al., 2000). Pro-drugs of a soft drug of any of the above classes including endogenous soft molecules. They are converted enzymatically into the active soft drug, which is subsequently enzymatically deactivated. Soft drugs, as any other drug can be the subject of pro- drug design resulting in pro-soft drugs. Pro soft drugs combine the advantages of pro drugs as well as soft drugs. Their design in the form of prodrugs results in targeted drug delivery to the site of action and soft drug properties renders easy, controllable conversion to non-toxic metabolites (Friend, D.R. and Chang, G.W. 1984). Soft Drugs A number of soft drugs are already on the market (e.g., Breviblock™, Ultiva™, Lotemax™, Alrex™) and many are currently being developed (e.g., soft antimicrobials, anticholinergics corticosteroids, β-blockers, analgetics, ACE inhibitors, antiarrhythmics) (Bodor et al., 2000). Conclusion: The prodrug approach has been used to overcome various undesirable drug properties and to optimize the clinical drug application. Recent advances in molecular biology provide direct availability of enzymes and carrier proteins, including their molecular and functional characteristics. Thus prodrug design is becoming more elaborate in the development of efficient and selective drug delivery systems. Hence, prodrug design can no longer be considered as just a chemical modification to solve problems associated with drugs. The targeted prodrug approach, which can be combined with gene delivery and controlled expression of enzymes and carrier proteins, is a promising strategy for precise and efficient drug delivery and the enhancement of therapeutic efficacy. Drug discovery and prodrug and soft drugs development appear to be complementary for the generation of target specific medicines now and in the future. 16 References: Albert, A. (1958). Chemical aspects of selective toxicity. Nature.182 :421-423. Amidon, G.L., Leesman, G.D. and Elliott, R.L., (1980). Improving intestinal absorption of water-insoluble compounds: a membrane metabolism strategy. J Pharm Sci. 69:1363-1368. Anon. (1998).IUPAC Pure & Appl. Chem. 70 :1129–1143. Bagshawe, K.D. (1987) Antibody directed enzymes revive anti-cancer prodrugs concept. Br J Cancer. 56 :531-532. Bagshawe, K.D. (1993). Antibody-directed enzyme prodrug therapy (ADEPT). Adv Pharmacol. 24:99-121. Biela, B.H., Khawli, L.A., Hu, P. and Epstein, A.L. (2003) Cancer Biother Radiopharm. 18(3):339-53. Bodor, N. (1984). Adv Drug Res. 13:255. Bodor, N. and Buchwald, P.( 2003). Burger’s Med. Chem., 6th ed., Vol. 2, 533. Bodor, N. and Buchwald, P. (2000). Soft drug design: general principles and recent applications. Med Res Rev. 20: 58-101. Connor, T.A.and Knox, R.J. (1995). Prodrugs in cancer chemotherapy. Stem cells.13:501-511. Deonarain, M.P., Spooner, R.A. and Epenetos, A.A. (1995).Genetic delivery of enzymes for cancer therapy. Gene Ther.2:235-244. Friend, D.R. and Chang, G.W. (1984). A colon-specific drug-delivery system based on drug glycosides and the glycosides of colonic bacteria. J Med Chem. 27: 261–266. 17 Haisma, H.J., Boven, E., van Muijen, M., de Jong, J., van der Vijgh, W.J.and Pinedo, H.M.(1992) A monoclonal antibody-ß-glucuronidase conjugate as activator of the prodrug epirubicin-glucuronide for specific treatment of cancer. Br J Cancer. 66:474-478. Han, H.K. and Amidon, G.L. (2000). Targeted Prodrug Design to Optimize Drug Delivery. AAPS PharmSci. 2 (1): 6. He, G., Massarella, J. and Ward, P. (1999). Clinical pharmacokinetics of the prodrug oseltamivir and its active metabolite Ro 64-0802. Clin Pharmacokinet.. 37(6):471-84. Huang, J.A., Buchwald, P. and Bodor, N.( 1998). Design and evaluation of new soft anticholinergic agents. Drug Dev Res, 43: 117–127. Huber, B.E., Richards, C.A. and Austin, E.A. (1994). Virus-directed enzyme / prodrug therapy (VDEPT): selectively engineering drug sensitivity into tumors. Ann NY Acad Sci. 716:104-114. Marais, R., Spooner, R.A., Light, Y., Martin, J. and Springer, C.J. (1996).Genedirected enzyme prodrug therapy with a mustard prodrug / carboxypeptidase G2 combination. Cancer Res. 56:4735-4742. Misiura, K., Szymanowicz, D., Kusnierczyk, D., Wietrzyk, J. and Opolski, A. (2002). Isophosphoramide mustard analogues as prodrugs for anticancer gene-directed enzyme-prodrug therapy (GDEPT). Acta Bioch Pol, 49: 169–176. Rapaka, R.S., (1995). Membranes and Barriers: Targeted Drug Delivery, NIDA Research Monograph 154: 1–264. Robinson, M.A., Charlton, S.T., Garnier, P., Wang, X.T., Davis, S.S., Perkins, A.C. and Frier, M. (2004). LEAPT: lectin-directed enzyme-activated prodrug therapy. Proc Natl Acad Sci. 101, 14527–14532. Roche, E.B. (1977). Design of Biopharmaceutical Properties through Prodrugs and Analogs. Washington, DC: American Pharmaceutical Association. Satchi-Fainaro, R., Hailu, H., Davies, J.W., Summerford, C. and Duncan, R. (2003). Bioconjug Chem. 14(4):797-804. Sharma, S.K., Bagshawe, K.D., Melton, R.G. and Sherwood, R.F. (1992). Human immune response to monoclonal antibody-enzyme conjugates in ADEPT clinical trial. Cell Biophys.2:109-120. 18 Singh, Y., Palombo, M. and Sinko, P.J. (2008). Recent trends in targeted anticancer prodrug and conjugate design. Curr Med Chem. 15(18):180226. Silva, A.T., Chung, M.C., Castro, L.F., Guido, R.V. and Ferreira, E.I. (2005). Advances in prodrug design. Mini Rev Med Chem. 5(10):893-914. Stella V.J. and Himmelstein KJ.(1982). Critique of prodrugs and site specific delivery. In: Bundgaard H, ed. Optimization of Drug Delivery. Alfred Benzon Symposium 17. Copenhagen, Munksgaard; 134-155. Tsuji, A. and Tamai, I. (1996). Carrier-mediated intestinal transport of drugs. Pharm Res.13:963-77. Wermuth, C.G. (1984). Designing prodrugs and bioprecursors. In: Drug Design: Fact or Fantasy,Ed. Jolles G, Woolridge KRH, Academic Press, London, 47–72. 19