SHOCK
advertisement

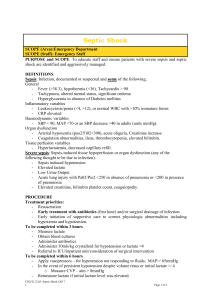
Shock Septic shock Resuscitation fluids SHOCK DEFINITION OF SHOCK Circulatory insufficiency Global hypoperfusion Inadequate tissue oxygenation Inadequate removal of toxic metabolites CLASSIFICATION OF SHOCK Hypovolaemic Inadequate circulating volume Haemorrhagic Trauma, Gastrointestinal (peptic ulcer, oesophageal varices , ca lower bowel, angiodysplasia) Vascular (ruptured AAA) Gynaecological emergencies (ruptured ectopic pregnancy) Loss of extravascular fluid Gastroenteritis, burns Cardiogenic Inadequate cardiac pump action Myocardial infarction Arrhythmias Severe valvular disease, valve rupture Myocarditis/cardiomyopathy Cardiac drugs – antiarrhythmics, beta blockers, Ca channel blockers Cardiac obstruction or compression Pericardial tamponade Pulmonary embolus Atrial myxoma Hypertrophic cardiomyopathy Aortic dissection Distributive Maldistribution of blood flow Anaphylactic Neurogenic Septic shock SEPTIC SHOCK (especially in the elderly) DEFINITION OF SEPTIC SHOCK Criteria proposed by the American College of Chest Physicians and the Society of Critical Care 1991 Sepsis 2 or more of the following ( SIRS ), as a result of infection Temperature >38deg C or < 36 deg C HR > 90 bpm RR> 20, or PaCO2< 32mmHg WCC > 12,000, < 4,000 or > 10 % immature forms Septic shock is present when there is sepsis as defined by the criteria above, as well as Hypotension, usually defined as SBP< 90mmHg, and Evidence of inadequate organ perfusion, such as Altered mental status Decreased urine output Lactic acidosis And failure of the hypotension to respond to at least 1 L of isotonic saline Aetiology Any infection - bacterial, fungal, viral , parasitic- can cause fever and SIRS. G+ve bacteria are the causative organisms in 35 to 40 % of cases, G-ve in 55 to 60 %. The most frequent sites of infection are the lungs, the abdomen and the urinary tract. Factors predisposing to G-ve bacteremia are: Diabetes mellitus Lymphoproliferative disease Cirrhosis of the liver Burns Invasive procedures Indwelling catheters Chemotherapy Factors predisposing to G + bacteremia are: Vascular catheters Indwelling mechanical devices Burns IV drug injection Incidence Not uncommon - exact statistics? USA 2 cases of sepsis per 100 admissions to hospital 55% ICU, 12 % ED, 33 % other inpatient specialty. 5O % of patients with sepsis develop septic shock. Age - mean age is 55 to 60 years Mortality Mortality of septic shock ranges from 20 to 80 %, average about 45 %. The higher statistics apply to the elderly and the immune compromised. Complications of septic shock CNS dysfunction ARDS 18 % Liver failure ARF 50 % DIC 38 % CLINICAL FEATURES Elderly patients are more susceptible to sepsis. They have less physiological reserve to tolerate sepsis and are more likely to have underlying disease. They are also more likely to be on medications such as betablockers and steroids, which will modify their response to the disease and the therapy. HISTORY Nonspecific symptoms - fever, chills, malaise, fatigue, anxiety or confusion. Dizziness or syncope. Sometimes, there may have been a fall or an RTC or other accident. In the elderly there may be no fever. The most consistent feature is altered mental status. This can be subtle. Mild disorientation or confusion is especially common. Unexplained apprehension, anxiety and agitation may be present. The very ill patients may be obtunded or comatose. Hyperventilation with a respiratory alkalosis is a common feature. Some may complain of shortness of breath, or family or friends may observe SOB. Localizing symptoms may be present -chest, abdomen, head and neck, pelvic or genitourinary, or to the musculoskeletal system and soft tissues. EXAMINATION FINDINGS General condition The patient may look unwell. Or may look acutely ill with a toxic appearance. This is not specific but will alert the examiner (or triage nurse). Or the patient may look deceptively "well". Simple observation will tell you if the patient is hyperventilating. Raised respiratory rate ( > 20 Breaths ) and respiratory alkalosis are common. Vital Signs An accurate temperature is essential, using a rectal thermometer if necessary. Temperature may be raised or lower than normal. Look at and feel the skin, the hands and the feet. In the early stages they feel warm. Capillary refill is normal. The heart rate is commonly increased. The blood pressure is low and the pulse pressure will often be increased. However, again if the patient is on BBlockers, then the heart rate may not go up significantly. Later stages, as sepsis progresses, the stroke volume and the cardiac output fall. Signs of poor peripheral perfusion develop - cool skin, cool extremities and delayed capillary refill. Findings depending on focus of infection CNS : altered mental status, neck stiffness Head and neck: sinus swelling or tenderness, lymph glands, tonsillar or peritonsillar abscess. Chest : tachypnoea, cough, phlegm, crackles, dullness to percussion. Heart: murmurs Abdomen and GIT : tenderness, guarding, jaundice, perianal abscess Pelvic and genitourinary tenderness: mass or discharge Skin and Soft tissue - swelling, redness, tenderness, blistering, discharge Musculoskeletal - muscle swelling, fluctuance, tenderness, joint pain and limitation of movement. MANAGEMENT Similar to the trauma “Golden Hour”, management in septic shock must be prompt. Triage : If obtunded and requiring immediate resuscitation and intubation, triaged category 1 and a medical emergency call put out. If presenting with altered mental status, looking unwell, extremities warm, or skin colour not looking good, moderately hypotensive as informed by ambulance, with any other history suggestive of sepsis, Triaged 2 and admitted to resuscitation room. Airway and breathing are assessed immediately. Oxygen. Intubation and ventilation are required. Monitor O2 saturation, respiratory rate, BP, ECG and temperature 12 lead ECG. Two16 gauge intravenous canulae. If immediate peripheral access is unobtainable, an EJ, a subclavian or an IJ line is inserted. Bloods for investigations as below Volume resuscitation is commenced. 500ml boluses of 0.9 % saline, every 5 to 10 minutes, with repeat clinical assessment after each bolus. After 1 to 2 Litres of saline colloid is infused Urinary catheter. A diligent fluid balance chart is commenced. The patient must be monitored for signs of volume overload, such as dyspnoea, pulmonary crackles, and pulmonary oedema on xray. There is relative and absolute intravascular fluid depletion. Causes of fluid depletion include increased microvascular permeability, decreased fluid intake, increased insensible fluid loss, vomiting and diarrhoea, and third spacing of fluids. The choice of fluid remains controversial. Clinical indicators for improved perfusion are improvement in heart rate, blood pressure, mental status, capillary refill, and urine output. Inotropic support The need for inotropes is assessed after 2 to 4 litres of fluid as the majority will require inotropes for hypotension, or if there are signs of fluid overload. Dopamine infusion 5ug/kg/min and increasing to 20 ug/kg/min. Insert an arterial line and commence invasive blood pressure monitoring. If with maximum dopamine therapy the patient remains hypotensive, further inotropes are warranted. Noradrenaline has been shown to be effective for patients failing to respond to fluid and dopamine. The patient requires intensive care support. The patient will need a central line if one has not been placed and will require invasive haemodynamic monitoring. Therefore if it appears that dopamine is not making any significant improvement DCCM assessment is called for early. All of the above measures should have taken less than 1 hour. INVESTIGATIONS Laboratory FBC: WCC may be raised or low, or indicate severe neutropenia. U&E/Cr, Ca, PO4, Mg Glucose ABG Lactate: elevation reflects degree of tissue hypoperfusion and shock. Predictor of mortality. Clotting profile : platelet count falls with DIC. Blood cultures x 2 : Positive 30 % of the time in the febrile elderly, febrile adult patients with elevated WCC or band forms , and the febrile neutropenic patients. Positive 50 % of the time inpatients who have sepsis and end organ dysfunction. Also useful in patients with prosthetic heart valves. Urine MC&S LP if meningitis suspected. See LP guide lines. Appropriate cultures, such as of pus, sputum, joint aspirate. Imaging Chest xray - routine chest Xray has shown clinically occult infiltrates in 3 to 4 % of febrile patients. Ultrasound for biliary tract sepsis. CT scan for intra-abdominal and retroperitoneal abscess. Head CT if increased ICP is suspected. TREATMENT OF INFECTION Empirical antibiotics are given as soon as possible or at the latest within 30 minutes of patient's arrival. They are to be given in the resuscitation room. There is no excuse for delaying antibiotic therapy. The initial therapy depends on the suspected cause – see Antimicrobial Guidelines, Neutorpaenic Sepsis Guidelines. A suitable empirical therapy in a normal adult is gentamicin 5 – 7mg/kg daily and flucloxacillin 2g IV 6 hourly, If unsure about antibiotic regime or need clearance for use of a controlled antibiotic ring the ID registrar or consultant or the ED consultant. Surgical sepsis. Call the surgical registrar on call early if abscess or other surgical sepsis is suspected. If septic arthritis or other orthopaedic sepsis is suspected, call the orthopaedic registrar. FURTHER CARE Those responding to initial fluids or low dose dopamine may be admitted to a medical ward. Failure to significantly improve within the first hour of treatment indicates a need for DCCM review. Those with severe sepsis and septic shock need referral to DCCM on arrival. PITFALLS Under triaging Failure to initiate adequate fluid therapy Failure to initiate antibiotic therapy Failure to commence inotropes at the appropriate time Failure to admit to DCCM early. Failure to address surgical sepsis REFERENCE: Tintinalli Antimicrobial Guidelines, Auckland Hospital ,1999. Medline RESUSCITATION FLUIDS Controversy in the choice of fluid, the rate and the volume of resuscitation. Recently, the controversy in haemorrhagic shock has been when to give fluid resuscitation. . Comparison between types of fluids available Isotonic Crystalloids Safe, nontoxic, no allergic reaction. No risk of infection. Inexpensive. In large volumes will sufficiently expand the plasma volume. Disadvantages Does not carry oxygen. Large volumes required - 3 x the amount of blood lost, 2 to 4 x the amount of colloid required. Short 1/2 life, only 20 % of infused volume remain in the intravascular space after 2 hours. That implies if 1000 mls are infused only about 200 mls remain in the circulation. Large volumes theoretically associated with more tissue oedema. However, no real documentation that adverse SEs such as pulmonary oedema are any more common with crystalloids than with colloids. Electrolyte abnormalities - hyperchloraemia - may contribute to acidosis. Colloids Haemaccel or Gelofusine. Hetastarch. Dextran 40 and 70 , 5 % and 25 % albumin Result in more rapid resuscitation, as they expand the plasma volume faster and for a longer duration. Associated with anaphylactic reaction. Dextran solutions additionally can cause bleeding and renal failure. More expensive. In a recent meta-analysis (BMJ ) colloid use associated with slightly higher mortality in critically ill patients. Metaanlysis not without flaws. The right choice of fluid till there is any evidence to the contrary is colloids and crystalloids Hypertonic saline Effective volume expander. Smaller infusion volumes, shorter infusion times, less third spacing. Improved haemodynamic, improving cardiac output and contractility Less oedema. Cheap. No infection risk.. Reduces cerebral oedema while raising blood pressure. Improves cerebral oxygenation. Increases tissue perfusion. Particularly good for head injury and burns shock. Results of trial for prehospital use in trauma and haemorrhagic shock ongoing. Some conflicting results. Neg : Increases serum sodium and chloride, osmolarity, can cause metabolic acidosis and hypokalemia. Adverse CNS effects from high sodium load - central pontine demyelination, altered mental status, seizures. Too rapid dehydration of the brain could increase intracerebral bleeding. Blood substitutes Perfluorochemical solutions which can carry a larger amount of dissolved oxygen. Haemoglobin solutions. All experimental. Blood The only fluid that is available to us that will carry oxygen! Indication : If the patient is haemodynamically unstable, or has persistent hypoxia, or has lost significant amount of blood ( 30 % of blood volume ). Best - fully typed and crossmatched, but this takes 45 minutes. Type specific blood can be available in 10 minutes, avoids the majority of incompatibility reactions. In desperate situation, uncrossed O + for men and O - for women. Timing of fluid resuscitation Traditional management of all haemorrhagic shock Two or more large bore IV lines, rapid infusion of large volumes of crystalloid and colloids. Massive units of blood rapidly infused. Resuscitate the patient, then take to theatre Recent studies have shown adverse outcomes with aggressive fluid resuscitation and restoration of blood pressure prior to control of bleeding source, esp. in penetrating torso trauma. Concept : two models : Uncontrolled Haemorrhagic Shock and Controlled haemorrhagic shock Theory of Hypotensive Resuscitation : In UCHS aim for a map of 40 mm Hg or a SBP of 60 to 80 mm Hg - minimal volume resuscitation, Remember : Prevent hypothermia - warm the fluids.