fluid _ electrolyte - Glory Cubed Productions
advertisement

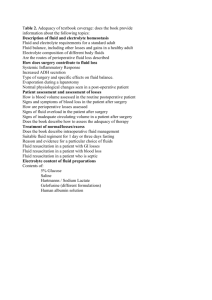
CONTENT - BODY FLUIDS AND ELECTROLYTES - FLUID AND ELECTROLYTE MOVEMENTS & BALANCE - ACID-BASE BALANCE - DISTURBANCES - ASSESSING, DIAGNOSING, PLANNING - IMPLEMENTING TO MEET NEEDS - I & O KEY TERMS - ACID - ACIDOSIS - ACTIVE TRANSPORT - ALKALOSIS - ANION - BASE - BUFFER - CATION - COLLIOD OSMOTIC PRESSURE - DIFFUSION - ELECTROLYTE - FILTRATION - HYDROSTATIC PRESSURE - IONONCOTIC PRESSURE - OSMOLARITY - OSMOSIS - PH - SOLUTE - SOLVENT OBJECTIVES - Discuss the function, distribution, movement and regulation of fluids and electrolytes in the body - Describe the regulation of acid-base balances in the body, including the roles of buffers, the lungs and the kidneys - Compare the third space syndrome and edema - Define key terms used with fluid and electrolyte disorders - TOTAL VOLUME OF FLUID AND TOTAL AMOUNTS OF ELECTROLYTES IN BODY NORMALLY REMAINS CONSTANT - FLUID BALANCE AND ELECTROLYTE BALANCE ARE INTERDEPENDENT INTAKE MUST EQUAL OUTPUT TO REMAIN IN BALANCE Homeostasis - Stability of the internal processes of the body; state of physiologic balance in the presence of constantly changing conditions (at the cellular level) - Concentration of oxygen, carbon dioxide, available nutrients & wastes, normal body temperature - Normal volume, composition, distribution, and pH of body fluids BODY FLUIDS - THE AVERAGE ADULT has approx. 40L of H2O compromising 60% of THE BODY WEIGHT - 25 L. INTRACELLULAR (ICF) - 15 L. EXTRACELLULAR (ECF) FUNCTIONS - TRANSPORT - FACILITATES CELLULAR METABOLISM - SOLVENT FOR ELECTROLYTES AND NON-ELECTROLYTES - MAINTAIN BODY TEMPERATURE - AIDS DIGESTION/ELIMINATION - ACTS AS TISSUE LUBRICANT BODY FLUID COMPARTMENTS - INTRACELLULAR COMPARTMENTS (ICF) - EXTRACELLULAR COMPARTMENTS (ECF) EXTRACELLULAR FLUID 1. INTERSTITIAL FLUID 10-12L. 2. PLASMA 3 L. 3. SMALL FLUID COMPARTMENTS 1 L. (e.g. fluids, aqueous humor, serous, synovial, lymphatic) 4. GI TRACT 1 L. for all organs BALANCE - FLUID BALANCE MAINTAINED PRIMARILY BY MECHANISMS THAT ADJUST OUTPUT TO INTAKE - SECONDARILY BY MECHANISMS THAT ADJUST INTAKE TO OUTPUT ALSO MAINTAINED BY A PHYSICAL MECHANISM OF WATER BETWEEN FLUID COMPARTMENTS (OSMOSIS) VARIATIONS IN FLUID CONTENT DEPENDENT UPON: 1. AGE - infant - more body fluid & ECF (more prone to FVDs) 2. LEAN BODY MASS - fat cells contain little lean tissue is rich in water 3. SEX - females - more body fat - All body fluids are related and mix well with each other - Plasma becomes interstitial fluid as it filters across the capillary wall - Interstitial fluid can return to the capillary by osmosis or enter lymphatic channels becoming lymph RISK FACTORS AGE Very old Very Young CHRONIC DISEASES Ca CARDIOVASCULAR DISEASES (CHF) ENDOCRINE DISEASE such as: Cushing’s Disease and Diabetes Mellitus MALNUTRITION COPD RENAL DISEASE CHANGES IN LOC TRAUMA CRUSH INJURIES HEAD INJURIES BURNS THERAPIES DIURETICS STEROIDS IV THERAPY TPN GI LOSSES GASTROENTERITIS NASOGASTRIC SUCTIONING FISTULAS VARIATIONS IN FLUID CONTENT Risk Factors for Fluid, Electrolyte, and Acid-Base Imbalances AGE VERY YOUNG VERY OLD Third-Spacing - The accumulation and sequestration of trapped extracellular fluid in an actual or potential body space as a result of disease or injury. (unavailable for normal physiologic processes) Peritoneal, pericardial, pleural, joint cavities, bowel, abdomen, soft tissues Causes organ malfunction Interstitial and Intercellular fluid are in osmotic equilibrium across the cell membranes, regulated by the Na+ concentration of interstitial fluid and the K+ concentration of the ICF. PRINCIPLE - OVERHYDRATION IS AN EXCESS OF WATER IN THE ECF COMPARTMENT WITH A NORMAL AMOUNT OF SOLUTE OR DEFICIENT AMOUNT OF SOLUTE Many different terms - Overhydration, Water excess, Hypervolemia FLUID EXCESS IN VASCULAR SYSTEM 1. Weight gain and edema 2. Fluid congestion in lungs 3. Dyspnea 4. Cough 5. Moist rales 6. Puffy eyes 7. Increased central venous pressure 8. Bounding pulse 9. Neck vein engorgement 10. Bulging fontanels 11. Decreased HGB and decreased HCT (hemodilution) 12. Nausea and vomiting PRINCIPLE - DEHYDRATION IS A LOSS OF BODY FLUIDS, PARTICULARLY FROM THE EXTRACELLAR FLUID COMPARTMENTS ELECTROLYTES - SUBSTANCES CAPABLE OF BREAKING INTO ELECTRICALLY CHARGED IONS WHEN DISSOLVED IN A SOLUTION 1. CATION ions that develop a positive charge 2. ANION ions that develop a negative charge MEASUREMENTS OF ELECTROLYTES - MILLIEQUIVALENTS - mEq chemically equal to the activity of 1mg of hydrogen 1 mEq cation = 1 mEq of anion PRINCIPLE - WHEN ELECTROLYTES ARE NOT IN A NORMAL BALANCE, THE PERSON IS IN A STATE OF RISK FOR ALTERATIONS IN HEALTH NON-ELECTROLYTES - If molecules in the body’s chemical components remain intact, they are called nonelectrolytes Examples: Urea and Glucose REGULATION OF ELECTROLYTES - REGULATES WATER DISTRIBUTION, REGULATES ACID-BASE BALANCE, AND MAINTAINS A BALANCED DEGREE OF NEUROMUSCULAR EXCITABILITY SOLVENTS - LIQUIDS THAT HOLD A SUBSTANCE IN SOLUTION SOLUTES - SUBSTANCES THAT ARE DISSOLVED IN A SOLUTION CATIONS - SODIUM - MOST ABUNDANT IN ECF - SODIUM PUMP - pumps Na+ out of ICF - REGULATES CELL SIZE - BASIC FOR COMMUNICATION BETWEEN NERVES AND MUSCLES - HELPS REGULATE ACID-BASE BALANCE REGULATION and LOSSES - Na+ intake regulates Na+ concentration - Sodium is conserved through reabsorption in the kidneys, a process stimulated by aldosterone - Most eliminated by kidneys, small amts. eliminated by feces & perspiration - Normal EC concentration of Na+ concentration is 135 to 145 mEq/L PRINCIPLE - Easily moves between intravascular and interstitial spaces and moves across cell membranes by active transport. FUNCTIONS - Controls and regulates the volume of body fluids - Maintains water balance throughout the body - Primarily regulator of ECF volume FUNCTIONS - Influences ICF volume - Participates in the generation and transmission of nerve impulses - An essential electrolyte in the Na-K pump Sources of Na+ - Na+ is well stored in the human body - Food sources rich in Na+ can be easily remembered by the use of this acronym Prevent More Sodium - Sodium- rich foods can be best categorized as belonging to one of three groups: processed foods, dairy foods, and salty foods The P stands for Processed Foods - often used as a preservative in foods Frozen foods - vegetables, dinners Canned foods - soups, gravies, fruits Boxed pastries - cakes, breads Prepared cereals and breads Processed meats - luncheon, bacon, sausage, and hotdogs The M stands for Moo Foods that are Dairy Products such as: Milk and Cream Cheese Butter Ice Cream The S stands for salty foods. Those that taste salty such as: Potato chips and pretzels Pickles and olives Nuts Bacon Ham Table salt Na+ restriction diets - No added salt diets Na+ restriction for fluid imbalances - CHF - Renal disease Sodium - Where Na+ goes, water goes. - Although Na+ as an electrolyte that influences central nervous system (CNS) function, its primary action is on fluid balance in the body. Thus, when the patient experiences an Na+ imbalance, the nurse must also anticipate an alteration in fluid balance. HYPERNATREMIA HYPER - “too much” or “excess” NA - symbol for sodium EMIA - “serum” or “blood” - is an excess of Na+ concentration in the blood, characterized by a shift of fluid from the cells into extracellular fluid, causing a shrinking of the cells. HYPERNATREMIA Cause: 1. increased concentration of serum Na+ 2. excess loss of body fluids Hallmark feature is DEHYDRATION. - high concentration of serum Na+ pulls fluid from the cells, resulting in cell shrinkage. Classic symptoms of Dehydration: - Hot, dry, flushed skin with poor turgor - Thirst - Dry mucous membranes - Absence of tears (particularly in children) - Soft, sunken eyeballs (fontanels) - Doughy abdomen - Increased body temperature Vascular effects of Hypernatremia - Cause fluids to shift from IC to EC compartments, thereby initially raising BP (pressure in the arteries) and causing tachycardia, and increased UOP. The body then compensates for the fluid shift and loss with oliguria and decreased BP in an effort to retain needed fluid. - Because Na+ influences the transmission of nerve impulses, CNS symptoms may also appear, including irritability, excitability, restlessness, confusion, and convulsions. Clients at Risk and Tx - Diabetes Insipidus - Severe diarrhea - Reduced glomerular filtration (Kidney failure, CHF, Shock) Treatment - Fluid Replacement Therapy HYPONATREMIA HYPO - “too little” or “decreased” NA - symbol for sodium EMIA - “serum” or “blood” - is a less than normal concentration of sodium in the blood. PRINCIPLE CAUSE: 1. excess loss of Na+ 2. excess retention of Na+ Effects of Hyponatremia - a low serum level of sodium, 135 mEq/L or lower. Because Na+ influences The transmission of nerve impulses, decreased Na+ will cause symptoms of headache, abdominal cramps, and muscular weakness. Because of excess fluid accumulations, nausea and vomiting are common symptoms. Clients at Risk: - Through skin from excessive sweating - Burn victims - post-operative wound drainage - hemorrhaging - taking a combination of a low-Na+ diet and potent diuretics - taking an excessive plain water intake - adrenal cortex dysfunction - Addison’s disease - SIADH - syndrome of inappropriate antidiuretic hormone Treatment GOAL - to restore normal sodium levels TREATMENT 1. If excess of fluid with a decrease of Na+ levels, aimed at restricting fluids. 2. If fluid balance is normal with decreased Na+ levels, an isotonic saline solution is given. POTASSIUM - MOST ABUNDANT CATION OF ICF - K+ PUMP BRINGS K+ INTO THE CELL - RESTING POLARIZATION AND REPOLARIZATION OF NERVE AND MUSCLE CELLS DEPENDS ON K+ FUNCTIONS - Chief regulator of cellular enzyme activity and cellular water content - Plays a vital role in such processes as the transmission of electric impulses, particularly in nerve, heart, skeletal, intestinal, and lung tissue; protein and CHO metabolism; and cellular building - Assists in regulation of acid-base balance by cellular exchange with H+ SOURCES AND LOSSES - Intake of 50 to 100 mEq/d maintains balance FOOD SOURCES BANANAS, TOMATOES, PEACHES, KIWI, FIGS, DATES, APRICOTS, LEMONS, ORANGES, PRUNES, MELONS, RAISINS, BROCCOLI. AND POTATOES ALSO MEAT AND DAIRY ( INSTANT COFFEE, AND SALT SUBSTITUTES ) EXCRETED PRIMARILY BY THE KIDNEYS NO EFFECTIVE WAY TO CONSERVE GI secretions contain large amounts Some found in perspiration REGULATION - CONSERVED BY THE NA+ PUMP - KIDNEYS CONSERVE WHEN CELLULAR k+ IS DECREASED ALDOSTERONE SECRETION TRIGGERS EXCRETION IN URINE - NORMAL RANGE FOR SERUM POTASSIUM IS 3.5 TO 5 mEq/L PRINCIPLE - Potassium is an essential electrolyte in the body whose principle function is to irritate (excite). Potassium serves to irritate nerve cells, which ultimately influences muscular function. Both smooth and skeletal muscles, and especially the heart, are dependent upon K+ for proper and regulated contraction and function. - Unlike Na+, it is stored poorly in the body. Imbalances can occur very quickly and requires a daily intake of potassium-rich foods (Fruits) PRINCIPLE WHERE NA+ GOES, K+ DOESN’T Na+ and K+ have an inverse relationship in the human body. Thus when an imbalance of Na+ occurs, the opposite imbalance of K+ occurs. PRINCIPLE - HYPERKALEMIA is an increased SERUM K+ LEVELS characterized by MUSCULAR IRRITABILITY and TENSION. (HYPEREXCITABILITY OF NERVES AND MUSCLES) Greatest priority is on cardiac function, because the heart is overstimulated and may evidence lifethreatening arrhythmias it can cause cardiac ARREST or failure. Over stimulation of GI - N & V, colic, diarrhea, Overstimulation of muscles - cramping, pain, and weakness TREATMENT MUST BE PROMPT - MONITOR SERUM K+ LEVELS CAREFULLY AND OFTEN AND ASSESS CARDIAC FUNCTION BY EKG Withdrawal of potassium sources (foods, supplements, IV Additives) Administer IV fluids and Diuretics to “flush out” K+ (if good renal function) Administer Kayexalate solution (PO or Rectal) HYPOKALEMIA IS A DECREASE IN SERUM K+ LEVELS CHARACTERIZED BY MUSCULAR WEAKNESS AND FATIGUE. INSUFFICIENT SUPPLY OF K+ TO THE BODY CELLS CAUSES INSUFFICIENT STIMULATION OR IRRITATION TO NERVES AND MUSCLES MUSCULAR WEAKNESS - CARDINAL SIGN INTAKE PROBLEMS Surgical patients with NPO status Patients with pronounced anorexia (ChemoRx) Patients with impaired chewing or swallowing (post-CVA) Patients undergoing gastric suction or surgery LOSS PROBLEMS Patients taking diuretics Patients with severe diarrhea HYPOKALEMIA - levels less than 3.5 mEq/L TREATMENT REPLACEMENT BY FOODS OR SUPPLEMENTS (K-LOR, K-LYTE) IV REPLACEMENT ADDED TO FLUIDS (NEVER BY DIRECT PUSH) VENOUS IRRITATION - EXTRAVASION MONITOR UOP CAREFULLY TO AVOID EXCESS (NO uop) CALCIUM - MOST ABUNDANT IN BODY - MOST IONIZED IN BONE AND TEETH - FORMS SALTS WITH PHOSPHOROUS, CARBONATE, AND FLUORIDE - REQUIRED FOR NERVE AND MUSCLE FUNCTIONS - REQUIRED FOR BLOOD CLOTTING, ACTS AS CO-FACTOR IN THE FORMATION OF PROTHROMBIN ACTIVATOR AND THROMBIN FUNCTION - NECESSARY FOR NERVE IMPULSE TRANSMISSION AND BLOOD CLOTTING - CATALYST FOR MUSCLE CONTRACTION - ESP CARDIAC - NEEDED FOR B12 ABSORPTION - CATALYST FOR CHEMICAL ACTIVITIES - NECESSARY FOR STRONG BONES AND TEETH - ESTABLISHES THICKNESS AND STRENGTH FOR CELL MEMBRANES. SOURCES & LOSSES DAILY REQUIREMENT - 1g. SOURCES milk, cheese, dried beans, (some in meat and vegetables) Stimulated by Vitamin D Leaves bone and teeth to maintain normal blood calcium levels Excreted in urine, feces, bile, digestive secretions, and perspiration REGULATION - WHEN ECF CALCIUM LEVELS DECREASE, THE PARATHYROID GLANDS INCREASE THE SECRETION OF PARATHYROID HORMONE (PTH), WHICH ACTS ON BONES TO INCREASE THE RELEASE OF CALCIUM INTO THE BLOOD, AND ACTS ON THE KIDNEY TUBULES AND THE INTESTINAL MUCOSA TO INCREASE THE REABSORPTION OF CALCIUM FROM THE KIDNEYS AND THE INTESTINE. - A HIGH SERUM PHOSOPHATE CONCENTRATION INCREASES SERUM CONCENTRATION; A LOW SERUM CONCENTRATION DECREASES SERUM CALCIUM - CALCITONIN, A HORMONE SECRETED BY THE THYROID GLAND, HAS AN OPPOSITE EFFECT ON CALCIUM THAN PTU. INCREASES IN CALCITONIN REDUCE SERUM CALCIUM CONCENTATION PRIMARILY BY OPPOSING OSTEOCLAST BONE REABSORPTION MAGNESIUM - MOST IS FOUND WITHIN BODY CELLS - PRESENT IN HEART, NERVE, AND MUSCLE TISSUES - SECOND MOST IMPORTANT CATION IN ICF FUNCTION - CO-FACTOR FOR MANY ENZYMES INVOLVED IN ENERGY METABOLISM - CO-FACTOR FOR METABOLISM OF CHO AND PROTEINS - MAINTAINS NORMAL INTRACELLULAR LEVELS OF POTASSIUM - HELPS MAINTAIN ELECTRICAL ACTIVITY IN NERVOUS MEMBRANES AND MUSCLE MEMBRANES SOURCES AND LOSSES AVERAGE DAILY REQUIREMENT - ADULT = 18 TO 30 mEq/d CHILDREN REQUIRE LARGER AMOUNTS FOUND IN MOST FOODS, esp. VEGETABLES, NUTS, FISH, WHOLE GRAINS, PEAS, AND BEANS REGULATION - ABSORBED BY THE INTESTINES - EXCRETED BY THE KIDNEYS - PLASMA CONCENTRATIONS = 1.3 TO 2.1 mEq/L. ANIONS CHLORIDE - MOST ABUNDANT ANION IN ECF - HELPS BALANCE SODIUM - FOUND IN BLOOD, INTERSTITIAL FLUID, LYMPH, AND small amounts in ICF - MAJOR COMPONENT OF GASTRIC SECRETIONS FUNCTIONS - ACTS WITH NA+ TO MAINTAIN THE OSMOTIC PRESSURE OF THE BLOOD - PLAYS A ROLE IN THE BODY’S ACID-BASE BALANCE - IMPORTANT IN BUFFERING ACTION WHEN O2 AND CO2 EXCHANGE IN RBCs - ESSENTIAL FOR THE PRODUCTION OF HYDROCHLORIC ACID IN GASTRIC JUICES SOURCES AND LOSSES - AVERAGE DAILY REQUIREMENTS UNKNOWN - FOUND IN FOODS HIGH IN NA+, IN DAIRY and MEAT REGULATION - NORMALLY PAIRED WITH NA+, and EXCRETED AND CONSERVED WITH NA+ BY THE KIDNEYS - CHLORIDE DEFICITS LEAD TO POTASSIUM DEFICITS, AND VICE VERSA - NORMAL SERUM CHLORIDE LEVELS RANGE FROM 95 to 105 mEq/L BICARBONATE - MAJOR CHEMICAL BASE BUFFER WITHIN THE BODY - FOUND IN BOTH ECF AND ICF FUNCTION - ESSENTIAL FOR ACID-BASE BALANCE - BICARBONATE AND CARBONIC ACID CONSTITUTE THE BODY’S PRIMARY BUFFER SYSTEM REGULATION - PART OF BUFFERING SYSTEM REGULATED BY KIDNEYS - READILY AVAILABLE AS A RESULT OF CARBON DIOXIDE - FORMATION DURING METABOLISM - NORMAL LEVELS RANGE = 25 - 29 mEq/L PHOSPHATE - PART OF PHOSPHATE AND BUFFER SYSTEM - FUNCTIONS IN CELLULAR ENERGY METABOLISM: PHOSPHATE + ADP = ATP - COMBINES WITH CALCIUM IN BONE TO CAUSE HARDNESS - INVOLVED IN GENETIC MATERIAL, RNA & DNA FUNCTION - ESSENTIAL FOR ACID-BASE BALANCE - BICARBONATE AND CARBONIC ACID CONSTITUTE THE BODY’S PRIMARY BUFFER SYSTEM SOURCES AND LOSSES - AVERAGE DAILY REQUIREMENTS FOR PHOSPHORUS ARE SIMILAR TO THOSE FOR CALCIUM - FOUND IN MOST FOODS, BUT ESP. BEEF, PORK, and DRIED BEANS AND PEAS - METABOLIZED IN THE SAME MANNER AS CALCIUM REGULATION - PHOSPHATE IS REGULATED BY PTH AND BY ACTIVATED VITAMIN D - CALCIUM AND PHOSPHATE ARE INVERSELY PROPORTIONAL; AN INCREASE IN ONE RESULTS IN A DECREASE IN THE OTHER - NORMAL RANGE 25 - 29 mEq/L OTHER ELECTROLYTES ANION SULFATE ASSOCIATED WITH CELLULAR PROTEIN EXCRETED BY THE KIDNEY LACTIC ACID ORGANIC ACID ANION PROTEIN ANION PLASMA PROTEINS ALBUMIN GLOBULIN FIBRINOGEN ELECTROLYTES FOUND IN TRACE AMOUNTS CHROMIUM = WELL-BALANCED DIETS AVENUES TO ENTER/LEAVE THE BODY - ENTERS GI TRACT (DRINKING & IN FOODS) - FORMED IN THE BODY BY METABOLISM - OXIDATIVE WATER - LEAVES VIA KIDNEYS (URINE), INTESTINES (WITH FECES), AND LUNGS AND SKIN (INSENSIBLE LOSS) MECHANISMS THAT MAINTAIN TOTAL FLUID VOLUME - OSMORECEPTOR SYSTEM, INTERACTION OF THE CIRCULATORY SYSTEM REGULATION OF FLUID - INTAKE: THIRST MECHANISM - VARIOUS OTHER FACTORS THAT MAY ALSO ALTER THE VOLUME OF FLUID LOSS ARE: OSMORECEPTOR SYSTEM - REGULATES WATER OUTPUT VOLUME TO BALANCE FLUID INTAKE VOLUME - MOST IMPORTANT FOR REGULATION OF OUTPUT, BECAUSE OTHER FLUID LOSSES THROUGH THE SKIN, LUNGS, AND GI HAVE NO FEEDBACK MECHANISMS - CELLS IN THE HYPOTHALAMUS SYNTHESIZE ANTI-DIURETIC HORMONE (ADH), WHICH IS STORED IN THE POSTERIOR PITUITARY BEFORE RELEASE INTO THE CIRCULATION - OSMORECEPTORS RESPOND TO DEHYDRATION BY INCREASING THE FREQUENCY OF NERVE IMPULSES TO THE POSTERIOR PITUITARY, RESULTING IN AN INCREASE IN THE AMOUNTS OF ADH RELEASED; THIS INCREASES WATER REABSORPTION IN THE KIDNEY TUBULES AND DECREASES URINARY OUTPUT. - OSMORECEPTORS RESPOND TO OVERHYDRATION BY DECREASING NERVE IMPULSES TO THE POSTERIOR PITUITARY, WHICH DECREASES THE RELEASE OF ADH , RESULTING IN AN INCREASE IN URINARY OUTPUT. INTERACTION OF THE CIRCULATORY SYSTEM - REGULATION OF BLOOD VOLUME (EXTRACELLULAR FLUID VOLUME) - INCREASED FLUID INTAKE INCREASES THE BLOOD VOLUME - INCREASED GLOMERULAR FILTRATION RESULTS IN AN INCREASE IN UOP, AND A DECREASE IN BLOOD VOLUME THIRD SPACE SYNDROME - THE CLIENT WITH A SEVERE THIRD SPACE SYNDROME EXPERIENCES THE EFFECTS OF AN EC FVD. THIS SYNDROME OCCURS WHEN THERE IS A SHIFT OF ECF INTO A BODY SPACE, WHERE IT BECOMES TRAPPED. - THE NET RESULT IS A DEFICIT IN ECF VOLUME. A SMALL BOWEL OBSTRUCTION OR BURN CAN RESULT IN THE SHIFT OF UP TO 5 TO 10 LITERS OUT OF THE ECF SPACES. THE PRECISE AMOUNTS OF THIRD SPACE LOSSES CANNOT BE ACCURATELY MEASURED. REGULATION OF FLUID INTAKE: THIRST MECHANISM - DEHYDRATION OF CELLS IN THE THIRST CENTER OF THE HYPOTHALAMUS GIVES RISE TO THIRST SENSATION. - THIRST SENSATION ARE ALSO INDUCED BY DRYNESS OF THE ORAL MUCOSA. - FLUID INTAKE STRETCHES THE STOMACH AND MOISTENS THE MOUTH AND THROAT: THESE SENSATIONS CANCEL THIRST SENSATION BEFORE THE ACTUAL HYDRATION OF BODY FLUIDS. VARIOUS FACTORS THAT ALSO HELP TO REGULATE: - HYPERVENTILATION - VOMITING - DIARRHEA - CIRCULATORY FAILURE MECHANISMS THAT MAINTAIN ELECTROLYTE CONCENTRATION - Aldosterone feedback mechanism - Parathyroid regulation of calcium ALDOSTERONE FEEDBACK MECHANISM - Adrenal cortex secrets the steroid hormone aldosterone when extracellular fluid sodium concentrations decrease or potassium concentrations increase. - Aldosterone stimulates kidney tubules to reabsorb sodium; potassium reabsorption decreases as sodium reabsorption increases; sodium is salvaged while potassium is excreted. - This mechanism helps preserve normal sodium and potassium concentrations in extracellular fluid. Secondary effects of aldosterone Chloride conserved with sodium Water conserved because it is reabsorbed by osmosis as tubules reabsorb salt PARATHYROID REGULATION OF CALCIUM - Parathyroid glands secrete parathormone when extracellular fluid calcium concentration decrease. - Parathormone stimulates the release of calcium from bone calcium reabsorption in the small intestine (vitamin D required), and calcium reabsorption in kidney tubules. - Increased extracellular fluid calcium concentrations result in decreased secretion of parathormone and gradual loss of excess calcium. ACID-BASE BALANCE - Healthy survival depends on the body’s maintaining a state of acid-base balance; more specifically, healthy survival depends on the maintenance of a relative constant, slightly alkaline pH of blood and other fluids. - When the body is in a state of acid-base balance, it maintains a stable hydrogen ion concentration in body fluids; specifically, blood pH remains relatively constant between 7.35 and 7.45. - The body has three devices or mechanisms for maintaining acid-base balance; named in order of the speed with which they act, they are the buffer mechanism, the respiratory mechanism, and the renal or urinary mechanism. - A state of uncompensated acidosis exists if blood pH decreases above 7.35. - A state of uncompensated alkalosis exists if blood increases above 7.45. The pH of body fluids shifts below the ideal of 7.35 to 7.45 for several reasons Glucose, used by almost all body cells, is oxidation; as a result, energy, water, and carbon dioxide are produced; the CO2 combines with the water to produce carbonic acid (H2CO3) Metabolism of sulfur amino acids results in formation of sulfuric acid Metabolism of phospholipids and phosphoproteins results in formation of phosphoric acid. Muscle metabolism under anaerobic conditions produces lactic acid. Rapid weight loss results in extra fat metabolism, producing ketone bodies that include alpha keto acids. The acid produced by the normal mechanisms just mentioned requires neutralization to avoid acidosis, coma and death. BUFFER MECHANISMS FOR MAINTAINING ACID-BASE BALANCE - The buffer mechanism consists of chemicals called buffers, which are present in the blood and other body fluid and which combine with relatively strong acids or bases to convert them to weaker acids or bases; hence, buffers function to prevent marked changes in blood pH levels either acids or bases enter the blood. - A buffer is often referred to as a buffer pair because it consists of not one but two substances: the chief buffer pair in the blood consists of the weak acid, carbonic acid (H2CO3), and its base salts, collectively called base bicarbonate BHCO3); sodium bicarbonate (NaHCO3), is by far the mot abundant base bicarbonate present in blood plasma. - When the body is in a state of acid-base balance, blood contains 27 mEq base bicarbonate per liter and 1.35 mEq carbonic acid per liter; usually this is written as a ratio, referred to as the base bicarbonate/carbonic acid ratio: 27mEq B HCO3 = 20 1.35mEQ H2CO3 = 1 - Whenever the base bicarbonate/carbonate acid ratio of blood equals 20/1, blood pH equals 7.4. - Base bicarbonate buffers nonvolatile acids that are stronger than carbonic acid and a basic salt. Buffering does not prevent blood pH from decreasing, but it does prevent it from decreasing as markedly as it would without buffering. - Buffering removes some NaBicarb from the blood and adds some carbonic acid to it; this necessarily decreases the base bicarbonate/carbonic acid ratio, which in turn necessarily decreases the pH of blood as it flows through capillaries (from it arterial level of about 7.4 to its venous level of about 7.38). - Anything that decreases the blood’s base bicarbonate/carbonic acid ratio necessarily decreases blood pH and thus tends to produce acidosis; the corollary is also true; anything that increases the base bicarbonate/carbonic acid ratio necessarily increases blood pH and thus tends to produce alkalosis. - Other buffer systems Protein buffer Most plentiful; three fourths of all chemical buffering power lies in the proteins of the body fluids. Provides support to other buffering systems such as bicarbonate buffer and phosphate buffer. Phosphate buffer system One sixth the neutralizing ability of bicarbonate buffer in extracellular fluid. More important in intracellular fluids, where its concentration is considerably higher. Helps to buffer pH of urine in kidney tubules. - Bicarbonate buffer is the most important buffer in human body fluids because it components, base bicarbonate and carbonic acid, are actively and constantly regulated by the action of the respiratory and urinary systems. RESPIRATORY MECHANISM FOR MAINTAINING ACID-BASE BALANCE - Respiratory control acid-base balance by controlling rate of CO2 exhalation from lungs; during normal body metabolism CO2 is produced, which reacts with warm to form carbonic acid, resulting in a decrease in pH (as acidity increases, pH decreases); when the respiratory system blows CO2 out of the body, carbonic acid breaks down into CO2 and water, resulting in an increase in pH (as acidity decreases, pH increases) RENAL MECHANISM FOR MAINTAINING ACID-BASE BALANCE - The renal mechanism is the most effective device the body has for maintaining acid-base balance; unless it operates adequately, acid-base balance cannot be maintained. The renal mechanism for maintaining acid-base balance makes the urine more acidic and the blood more alkaline. - This neutralizes the constant production of acid products from cells; the mechanism consists of two functions performed by the distal renal tubule cells, both of which remove hydrogen ions from blood to urine and in exchange reabsorb sodium ions from tubular urine to blood. CARE OF CLIENTS WITH FLUID AND ELECTROLYTE PROBLEMS ASSESSMENT - Obtain history to identify risk factors affecting fluid and electrolyte status - Monitor vital signs - Evaluate skin turgor, hydration and temperature - Auscultate breath sounds - Weigh client daily - Monitor intake and output - Evaluate changes in behavior and energy level - Review lab tests Urinary specific gravity, Serum pH and serum electrolyte, Hematocrit, Blood urea nitrogen (BUN),Creatinine clearance Analysis/Nursing Diagnosis - Activity intolerance r/t muscle weakness - Decreased cardiac output r/t cardiac dysrrhythmias - Fluid volume deficit r/t: - DIARRHEA - LOSS OF GASTRIC CONTENTS (VOMITING, NASOGASTRIC INTUBATION) - DIAPHORESIS - POLYURIA - Fluid volume excess r/t: ANURIA DECREASED CARDIAC OUTPUT ALTERED REGULATORY MECHANISM TRAPPING OF FLUID IN THE THIRD SPACE; WHERE EXTRACELLULAR FLUID ACCUMULATES AND IS PHYSIOLOGICALLY UNAVAILABLE TO THE BODY - IMPAIRED GAS EXCHANGE R/T EXCESSIVE SECRETIONS RISK FOR INJURY R/T SENSORY AND PERCEPTION ALTERATIONS - ALTERED NUTRITION: LESS THAN BODY REQUIREMENTS R/T: ANOREXIA NAUSEA VOMITING RISK FOR IMPAIRED SKIN INTEGRITY R./T POOR SKIN TURGOR PLANNING/IMPLEMENTATION - MANAGE FLUID AND ELECTROLYTE INTAKE - ADMINISTER IV THERAPY - ADMINISTER PHARMACOLOGICAL AGENTS - MANAGE FLUID AND ELECTROLYTE INTAKE - FLUIDS GIVEN TO CORRECT DEFICITS AND RESTRICTED TO PREVENT EXCESSES - NUTRITIONAL INTAKE CAN BE INCREASED OR RESTRICTED TO CORRECT ELECTROLYTE DISTURBANCES NA+= SALT, DAIRY, MEATS, SOUPS, CANNED FOODS K+ = BANANAS, ORANGES, NUTS, DARK LEAFY GREENS, DRIED FRUITS CA++=MILK, CHEESE, YOGURT ADMINISTER PHARMACOLOGIC AGENTS - DIURETICS (THIAZIDE, POTASSIUM-SPARING, LOOP OR OSMOTIC DIURETICS) - ELECTROLYTE REPLACEMENTS (E.G., POTASSIUM CHLORIDE, CALCIUM GLUCONATE) - POTASSIUM-REMOVING RESIN: SODIUM POLYSTYRENE SULFONATE (KAYEXALATE) EVALUATION/OUTCOMES - MAINTAINS FLUID BALANCE - SERUM ELECTROLYTE LEVELS ARE WITHIN NORMAL LIMITS - VITAL SIGNS ARE WITHIN NORMAL LIMITS INTAKE and OUTPUT - MEASURING AND RECORDING ALL LIQUID INTAKE AND OUTPUT DURING A 24-HOUR PERIOD HELPS COMPLETE THE ASSESSMENT DATABASE FOR FLUID, ELECTROLYTE, AND ACID-BASE BALANCES. - INTAKE INCLUDES ALL LIQUIDS TAKEN BY MOUTH, FLUIDS GIVE THROUGH NASOGASTRIC AND OTHER FEEDING TUBES, LIQUIDS GIVEN AS IVs, AND BLOOD AND ITS COMPONENTS. OUTPUT INCLUDES URINE, DIARRHEA, VOMITUS, GASTRIC SUCTION, AND DRAINAGE FROM POSTSURGICAL TUBES. CASE STUDY REASONING EXERCISES 1.The nurse caring for a patient with dehydration should expect to note which of the following clinical manifestations? a. Hypertension b. Hot, flushed skin c. Bradycardia d. Peripheral edema REASONING EXERCISES 2. Which of the following changes in the laboratory values of a patient receiving fluid replacement for dehydration would indicate to the nurse that therapy has been effective? a. Increase in blood urea nitrogen (BUN) b. Decrease in hematocrit (HCT) c. Increase in creatinine (Cr) d. Decrease in hemogloblin (Hgb) REASONING EXERCISES 3. Which of the following classes of medication is indicated for the management of hyponatremia related to fluid volume excess? a. Loop diuretic b. Broad spectrum antibiotics c. NSAIDS d. Plasma expanders REASONING EXERCISES 4. A patient receiving intravenous fluids at a flow rate of 150cc/h develops a moist cough and dyspnea. Which of the following actions should the nurse take initially? a. Elevate the head of the bed to semi-Fowler’s position. b. Encourage the patient to cough and deep breathe. c. Administer 5 L of oxygen per nasal cannula. d. Decrease the rate of flow of the IV fluids. REASONING EXERCISES 5. A patient is receiving diuretic therapy for fluid volume excess. Which of the following observations would indicate to the nurse that therapy has been effective? a. Increase in BP b. Decrease in body weight c. Increase in CVP d. Decrease in pulse REASONING EXERCISES 6. A patient is placed on a low-sodium diet. Which os the following meals would be appropriate? a. Tuna fish sandwich, potato chips and dip, lettuce salad, glass of iced tea. b. Veal parmesan, broccoli, baked potato, milkshake. c. Breast of chicken, peas, lettuce salad, 1 slice of bread, glass of 2% milk. d. T-bone steak, cauliflower with cheese sauce, green beans, instant chocolate pudding, cup of hot tea. REASONING EXERCISES 7. A newly admitted patient has a serum potassium value of 3.1 mEq/L Which of the following questions would be important for the nurse to ask the patient during the admission history? a. “ Do you have any difficulty sleeping at night?” b. “ Have you had any surgeries in the past?” c. “ Have you developed any new symptoms in the past few days?” d. “ Are you presently taking any medications?” REASONING EXERCISES 8. A nurse is reviewing the laboratory values of a patient newly admitted for CHF. Which of the following should the nurse report to the physician? a. b. c. d. Serum potassium 5.6 mEq/L Serum glucose 110mg/dL Serum creatinine 1.1mg/dL Platelet count 320,000 REASONING EXERCISES 9. A patient in acute CHF is ordered to receive Furosemide (Lasix) 80 mg IV daily. The patient’s morning serum K+ values 3.8 mEq/L. In the light of the serum K+ value, which action should the nurse take? a. Phone the physician to question the medication order. b. Administer the Lasix 80 mg IV as ordered. c. Administer half of the ordered dose (40 mg) d. Withhold the Lasix and notify the physician. REASONING EXERCISES 10. A nurse caring for a patient in renal failure whose potassium level value is 6.4 mEq/L. Which of the following actions would be most beneficial for the nurse to take? a. Maintain the patient’s bed in high Fowler’s position b. Apply oxygen @ 2L/min pnc. c. Attach the patient to 3-Lead continuous cardiac monitoring. d. Place an artificial airway at bedside.