SIRS and Septic Shock
advertisement

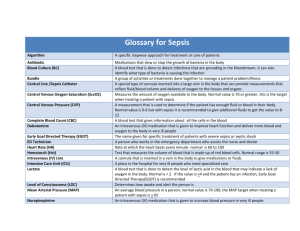
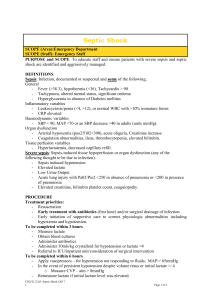
Resident Version SIRS and Septic Shock created by Dr. Dana Davis Objectives: 1. Define and differentiate bacteremia and the clinical spectrum of SIRS, sepsis, severe sepsis, and septic shock. 2. Identify typical choices for empirical antibiotics for patients with sepsis. 3. Identify patient groups with increased risk for the development of sepsis, increased morbidity or mortality, or uncommon etiologic organisms. 4. Describe the indications, contraindications and side effects of therapeutic agents including fluids, vasopressors, antibiotics, steroids, and activated protein C in the treatment of sepsis. References: 1. Lorente JA, et al, Time course of hemostatic abnormalities in sepsis and its relation to outcome., Chest, 1993, May, 103(1536-42) 2. McGill, Endothelial cells: role in infection and inflammation. World J Surg - 01FEB-1998; 22(2): 171-8 3. Levi M, Disseminated intravascular coagulation. N Engl J Med - 19-AUG-1999; 341(8): 586-92 (antibiotics) 4. Bernard GR . Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med - 8-MAR-2001; 344(10): 699-709 5. O’Brien JM. New approaches to the treatment of sepsis. Clinics in Chest Medicine. Volume 24 • Number 4 • December 2003 6. The International Sepsis Forum. Guidelines for the management of severe sepsis and septic shock. Intensive Care Med 2001;27(Suppl. 1):S1–134. 7. Simon D, Trenholme G. Antibiotic selection for patients with septic shock. Crit Care Clin. 2000;16:215–230. 8. Annane D, Sebille V, Charpentier C, Bollaert PE, Francois B, Korach JM, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 2002;288(7):862-71. 9. Briegel J , Forst H , Haller M , et al: Stress doses of hydrocortisone reverse hyperdynamic septic shock : A prospective, randomized, double-blind, single-center study . Crit Care Med 1999 ; 27 : 723–732 10. 14th European Congress of Clinical Microbiology and Infectious Diseases, May 1–4, 2004 11. Kumar A, Roberts D, Wood KE, et al. Delays in antimicrobial therapy for sepsis. Crit Care Med. 2004;32:A11. 12. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 2004; 32:85. CASE History: 33 y/o F presents with Fever, non-productive cough, sore throat and head ache. URI sxs X 5 days. Came in b/c feeling tired and a little SOB. Not eating or drinking much. . 2 kids at home both of whom have had recent URI/sore throat about 2 weeks ago. PMH MVA spleenectomy at age 9 Immunization status unknown No medications G2 P2 NKDA ROS Neg. except as reported in HPI T 35.8 P 98 R 20 (PaCO2 will be 30) BP 100/56, O2 sat 91% RA A&O X 4. Skin is dry. HEENT – pharynx injected. Neck supple. No adenopathy CV – no murmurs Lungs – L posterior crackles Abdomen – benign Skin – no rash Lymph – no adenopathy Normal genital/rectal exams No muscle or joint swelling. WBC 24.5 (85 PMN - automated(15 Bands, 70 Segs), 5 lymphs, 10 monos), H/H 13.6/40, Plt 166 K Chem 10 Na 148, K 4.6, Cl 105, Bicarb 24, BUN 22, Cr 1.2 , Ca 9.4, PO4 5, Mg 2.0 CXR – Possible LLL pneumonia Hospital course: Patient admitted to the hospital with suspected pneumonia in an asplenic patient. Initial blood cultures were taken, as were sputum and urine cultures. Antibiotics were ordered in the Emergency Room, but were delayed for approximately 2 hours. Initially she was started on cefotaxime and doxycycline. She was started on IV fluids, bolused with lL of NS and infused with 1/2 NS at 150 cc per hour. At the time that the antibiotics were being administered it was noted that her pulse was now 110 to 124 and her blood pressure was 98/46. The patient was complaining of worsening headache and photophobia. The remainder of her vitals were unchanged. Suspecting meningitis a CT was performed which was normal. An LP was performed. Gram stain showed Gram positive diplococci. WBC count was 1500 with 200 RBC. Glucose 44 and protein 88. At that time a call from the lab was received that the patient was noted to have Gram + diplococci on her peripheral blood smear. Vancomycin was added to her antibiotics and she was switched from cefotaxime to ceftriaxone and was given a single dose of dexamethasone. Two hours later the patient began to complain of bilateral leg numbness and weakness. She was noted to have diminished strength in both lower extremities, as well as decreased pinprick sensation and reduced sphincter tone. The exam was also significant for a pulse of 138, BP of 86/42, she appeared mottled with multiple bruises where she had been stuck for lab draws and IVs, and she was oriented to person only. Repeat labs were ordered: Chem 10 – Na 144, K – 4.9, Cl – 98, Bicarb – 20, BUN – 32, Cr – 1.6, PO4 – 2.2, Mg – 1.7 CBC - WBC 12.5 (15 Bands, 55 Segs, 5 metamyelocytes, 12 Monos, 13 Lymphs), H/H – 11/33, Plt - 70 PT – 28 (INR 9.2), PTT – 65 LFTs – AST 108, ALT 114, Alk. Phos 88, Total Bili. 5.2, Direct Bili. 1.1, Albumin 3.6, Total Protein 8.6 MRI of L / S spine showed hematoma present in lumbar spinal cord. The patient was transferred to the MICU and dopamine was instituted. Shortly after transfer the patient became hypoxic and required mechanical ventilation. A repeat CXR showed diffuse “white out” consistent with severe ARDS. The following day the patient developed unrelenting seizures. Once the seizures were controlled with lorazepam and fosphenytoin a repeat CT scan was done which showed intracerebral hemorrhage. The patient also had bilateral dilated pupils and lacked brainstem reflexes. After discussions with her family life support was withdrawn and the patient died shortly thereafter. Autopsy was performed. The blood cultures and spinal fluid grew out pneumococcus which was sensitive to ceftriaxone. The official cause of death was determined to be pneumococcal sepsis resulting in coagulopathy and subsequent intracerebral hemorrhage Discuss management of this patient including use of fluids, antibiotics, pressors, steroids as well as significance of results from lab/diagnostic tests. Outline for discussion Definitions: 1)Bacteremia – presence of viable bacteria in circulating blood 2)SIRS - is a widespread inflammatory response to a variety of severe clinical insults. This syndrome is clinically recognized by the presence of two or more of the following: Temperature >38ºC or <36ºC Heart rate >90 beats/min Respiratory rate >20 breaths/min or PaCO2 <32 mmHg WBC >12,000 cells/mm3, <4000 cells/mm3, or with >10 percent immature (band) forms Non-infectious causes of SIRS Trauma / burns (34 %) CVA (6%) GI bleeding (5%) Pancreatitis, vaginal delivery, CHF, TTP, malignancies, acute coronary syndrome, thromboembolism, and DKA. SIRS + infection = Sepsis Severe Sepsis Septic Shock 3) Sepsis - This is a systemic inflammatory response to a documented infection. The manifestations of sepsis are the same as those previously defined for SIRS. 4) Severe Sepsis - This is sepsis and SIRS associated with organ dysfunction, hypoperfusion, or hypotension. 5)Septic Shock A subset of people with severe sepsis develop hypotension despite adequate fluid resuscitation, along with the presence of perfusion abnormalities that may include lactic acidosis, oliguria, or an acute alteration in mental status. 6) MODS (multiple organ dysfunction syndrome) This is the presence of altered organ function in a patient who is acutely ill and in whom homeostasis cannot be maintained without intervention. Epidemiology: Patient characteristics which increase risk of sepsis: Extremes of age, compromised immune system, prolonged hospitalization, disruption in natural barriers to bacterial injury, malignancies. Microorganisms: Prior to the introduction of antibiotics in clinical practice, gram-positive bacteria were the principal organisms causing sepsis. More recently, gram-negative bacteria and fungal infections have become key pathogens causing severe sepsis and septic shock. Pathophysiology: SIRS results from a dysregulated inflammatory response. Activation of the complement system leads to generation of bradykinin and nitric oxide which have been implicated in the induction of hypotension and hyperdynamic shock. Abnormalities of coagulation and fibrinolysis homeostasis in sepsis An imbalance of homeostatic mechanisms lead to subclinical coagulopathy and occasionally disseminated intravascular coagulopathy (DIC) and microvascular thrombosis causing organ dysfunction and death. Activated protein C acts as an antithrombotic in the microvasculature, but is decreased in sepsis. The imbalance among inflammation, coagulation, and fibrinolysis results in widespread coagulopathy and microvascular thrombosis and suppressed fibrinolysis, ultimately leading to multiple organ dysfunction and death. Circulatory pathophysiology of septic shock The predominant hemodynamic feature of septic shock is arterial vasodilation. Peripheral circulation during septic shock An elevation of cardiac output occurs; however, the arterial-mixed venous oxygen difference usually is narrow, and the blood lactate level is elevated. This is a result of maldistribution of blood flow and oxygen delivery/extraction. Diagnostic Tests CBC Chemistry - Na, Cl, HCO3, BUN, Cr, lactate, liver tests Coagulation studies. Blood and Urine cultures, preferably prior to initiation of antibiotics. Chest x-ray Abdominal films, possibly including CT if unable to localize site of infection, especially if the patient has abdominal complaints. Lumbar puncture if the patient has meningeal signs or altered mental status. Treatment General supportive care: Initial treatment includes support of respiratory and circulatory function, supplemental oxygen, mechanical ventilation, and volume infusion. Hemodynamic support of septic shock Evidence of inadequate tissue perfusion and oxygenation: MAP < 60 mmHg, or a decrease in MAP of greater than 40 mm Hg. Elevated blood lactate. Mixed venous saturation of less than 65%. Evidence of end-organ damage – acute coronary syndrome, renal dysfunction (decrease urine output or increase in creatinine), decreased level of consciousness, elevated transaminases, ileus or malabsorption. The hemodynamic support in septic shock is provided by restoring the adequate circulating blood volume, and, if needed, optimizing the perfusion pressure and cardiac function with vasoactive and inotropic support to improve tissue oxygenation. Intravascular volume resuscitation Up to 10 L in six hours. Frequent (2 to 3/hour) boluses of 10 to 20 ml/kg. Reassess for clinical endpoints frequently Vasopressor supportive therapy When proper fluid resuscitation fails to restore hemodynamic stability and tissue perfusion, initiate therapy with vasopressor agents. Typical agents are: dopamine, norepinephrine, epinephrine, and phenylephrine. Empirical antimicrobial therapy Initiate this therapy early (prior to cultures if obtaining cultures would result in a delay in administering antibiotics) in patients experiencing septic shock as appropriate antibiotic therapy has been shown to have a survival benefit when compared to delayed, inadequate or inappropriate antibiotic therapy, though antibiotics have little effect on the clinical outcome in the first 24 hours Surgery may be required for patients with localized foci of infections (abscesses) or intraabdominal infections. Recombinant human activated protein C A recent publication by the Recombinant Human Activated Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study group demonstrated that the administration of recombinant human activated protein C (drotrecogin-alfa, activated) resulted in lower mortality rates (24.7% versus 30.8%) in the treated group compared to placebo. High-dose glucocorticoids: While theoretical and experimental animal evidence exists for the use of large doses of corticosteroids in those with severe sepsis and septic shock, all randomized human studies (except 1 from 1976) found that corticosteroids did not prevent the development of shock, reverse the shock state, or improve the 14-day mortality rate. However, a study reported in JAMA in 2002 showed that 75% of patients in the study who remained hypotensive despite adequate fluid resuscitation and vasopressor therapy were adrenally insufficient and did benefit from hydrocortisone and fludrocortisone. Stress-dose glucocorticoids: Recent trials demonstrated positive results of stress-dose administration of corticosteroids in patients with severe and refractory shock. Review Question A 71 year old man with a history of hypertension and chronic bronchitis who continues to smoke presents with a complaint of increasing shortness of breath. He has felt feverish and has had an increase in his usual cough, which is now productive of green, blood tinged sputum. His medications prior to admission were an Albuterol inhaler PRN, Atrovent inhaler every six hours, and he had increased his prednisone from his usual 5 mg per day to 40 mg per day this morning because, “That’s what his doctor usually does when he has an exacerbation.” On exam the patient is pale, diaphoretic and appears anxious. Vitals: P 122, BP 92/42, Temp. 38.2, Resp. 24, O2 Sat. 90% on RA. He responds appropriately to questions, but is oriented only to person. He has no retractions and has good air movement. Crackles are heard in the left posterior lung fields. What intervention will have the most immediate impact on this patient’s mortality? A) Initiate empirical antibiotics for community acquired pneumonia with a macrolide and a third generation cephalosporin. B) Obtain sputum and blood cultures prior to initiation of antibiotics. C) Obtain a CXR to affirm the cause of the patient’s symptoms are due to pneumonia rather than an exacerbation of CHF prior to any intervention. D) Bolus with 1 L of NS immediately, then repeat boluses with 250 to 500 cc of crystalloid solution until the patient is clinically volume repleted. E) Administer norepineprhine, initial dose 0.5 mcg/kg/min, titrate to MAP of 60. Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111). 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student