Family Medicine Junior Clerkship Syllabus 2014-2015
advertisement

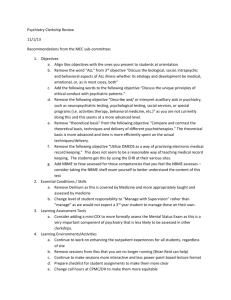
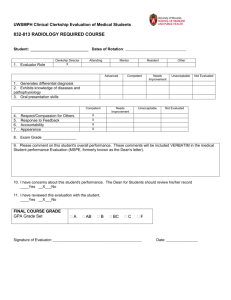
FAMILY MEDICINE THIRD YEAR CLERKSHIP COLLEGE OF MEDICINE DEPARTMENT OF UNIVERSITY OF ARKANSAS FOR MEDICAL SCIENCE 2014 – 2015 http://familymedicine.uams.edu/medical-student-education-program. Welcome to the UAMS Family Medicine Clerkship. We sincerely hope that you will enjoy learning and practicing new skills during your time with Family Medicine. This syllabus should provide you with the information you need to be successful during this clerkship. The clerkship will be delivered in a decentralized fashion, with training sites in Springdale, Fort Smith, Jonesboro, Little Rock, Magnolia, Pine Bluff, Texarkana, and the Northwest Campus. If there is any additional information or help that you need throughout the month, please contact either our Clerkship Coordinator, Kathy Carlson, at carlsonkathleenl@uams.edu or 501-686-6564 or your site coordinator (see table on page 5). You should have received details about each clerkship site as a separate attachment, but if you are unable to find that document, please go to department website. Family medicine is the specialty which provides continuing, comprehensive health care for the individual and family. It is a specialty that integrates the biological, clinical and behavioral sciences. The scope of family medicine encompasses different genders, ages, organ systems and disease entities. The clerkship will focus on the outpatient management of medical problems commonly encountered by family physicians. The student educational experience incorporates the philosophy that each patient is a unique individual who has the right to dignity, respect and the pursuit of a healthy, fulfilling life. Our statewide faculty is committed to providing you with an educational experience which will be valuable, regardless of your field of future practice. Website information For academic year 2014-2015, the Family Medicine Junior Clerkship syllabus will be available online at the UAMS website: http://familymedicine.uams.edu/medical-student-education-program. Since we will be making online updates, students are encouraged to check it periodically. If students have difficulty using the website or have questions prior to their rotation they may contact the clerkship coordinator at the address above. 2 TABLE OF CONTENTS Family Medicine Clerkship Dates Clerkship Directory 2013-2014 NW Longitudinal Information Clerkship Policies Attendance Policy Vacation Work Hour Rules Participation in Invasive Procedures Notification of Grades Student Responsibilities Faculty Responsibilities Family Medicine Clerkship Goals and Objectives Resources Grades and Evaluations Overview Minimum Passing Standards Grade Appeal Process Student at Risk of Failure Clinical Performance NBME information and example questions fmCases Evidence-Based Medicine Module Nutrition and Cardiovascular Disease module Requirement Checklist Healthcare Reform Video Interactive Video Lectures Conferences Course and Preceptor evaluations Course Evaluation Faculty Evaluation Appendix A Evidence-Based Medicine Module Overview, Student Responsibility, Principles Duke University Website link Common Study Designs Tips for reviewing articles Review of Statistical significance Critical Review Forms Grading sheet for the module Worksheet 4 5 6 7 7 7 7 7 8 8 9 - 12 13 14 - 23 14 14 15 15 15, 19 - 21 15, 18 – 19 16 - 17 16 16, 18 16 16 17 17 22 – 23 22 23 24 – 36 24 25 25 – 27 28 – 30 30 – 32 32 – 34 35 35 – 36 3 2013-2014 Family Medicine Clerkship Dates Rotation #1: July 8 – August 1, 2014 Orientation/Pre NBME: Tuesday, July 8 Mid-Rotation Evaluation: see site calendar Post fmCases exam: Friday, July 25 NBME: Friday, August 1 Rotation #2: August 4 – August 29, 2014 Orientation/Pre NBME: Monday, August 4 Mid-Rotation Evaluation: see site calendar Post fmCases exam: Friday, August 22 NBME Final Exam/Friday, August 29 Rotation #3: September 1 – September 26 Holidays: Thanksgiving: Thursday, November 27 and Friday, November 28 Winter Break: December 22 - January 4 Rotation #7: January 5 – January 30, 2015 Orientation/Pre NBME: Monday, January 5 Mid-Rotation Evaluation: see site calendar Post fmCases exam: Friday, January 23 NBME Final Exam: Friday, January 30 Holiday: Martin Luther King Day, Monday, January 19 – see site calendar for work schedule Rotation #8: February 2 – February 27 Holiday: September 1 Orientation/Pre NBME: Tuesday, September 2 Mid-Rotation Evaluation: see site calendar Post fmCases exam: Friday, September 19 NBME Final Exam: Friday, September 26 Orientation/Pre NBME: Monday, February 2 Mid-Rotation Evaluation: see site calendar Post fmCases exam: Friday, February 20 NBME Final Exam: Friday, February 27 Holiday: President Day, Monday, February 16 – see site calendar for work schedule Rotation #4: September 29 – October 24 Rotation #9: March 2 – March 27 Orientation/Pre NBME: Monday, September 29 Mid-Rotation Evaluation: see site calendar Post fmCases exam: Friday, October 17 NBME Final Exam: Friday, October 24 Rotation #5: October 27 – November 21 Orientation/Pre NBME: Monday, October 27 Mid-Rotation Evaluation: See Site calendar Post fmCases exam: Friday, November 14 NBME Final Exam: Friday, November 21 Holiday: Veterans Day, Tuesday, November 11 – see site calendar for work schedule Rotation #6: November 24 – December 19 Orientation/Pre NBME: Monday, November 24 Mid-Rotation Evaluation: see site calendar Post fmCases exam: Friday, December 12 NBME Final Exam: Friday, December 19 Orientation/Pre NBME: Monday, March 2 Mid-Rotation Evaluation: see site calendar Post fmCases exam: Friday, March 30 NBME Final Exam: Friday, March 27 Spring Break: March 30 – April 3 Rotation #10: April 6 – May 1 Orientation/Pre NBME: Monday, April 6 Mid-Rotation Evaluation: see site calendar Post fmCases exam: Friday April 24 NBME Final Exam: Friday, May 1 Rotation #11: May 4 – May 29 Orientation/Pre NBME: Monday, May 4 Mid-Rotation Evaluation: see site calendar Post fmCases exam: Friday, May 22 NBME Final Exam: Friday, May 29 Holiday: Memorial Day, Monday, May 25 – see site calendar for work schedule Rotation #12: June 1 – June 26 Orientation/Pre NBME: Monday, June 1 Mid-Rotation Evaluation: see site calendar Post fmCases exam: Friday, June 19 NBME Final Exam: Friday, June 26 4 FAMILY MEDICINE/CLERKSHIP – Directory of Campuses and Sites Overall Clerkship Coordinator Overall Clerkship Director UAMS Central Office Executive Director Director for Education Kathy Carlson Arlo Kahn, MD 501-686-6564 501-686-6564 Mark Mengel, MD, MPH 501-686-5798 501-686-6557 or 1-800-482-9612 Tricia Edstrom Clerkship Sites: DFPM Little Rock Site Overall Clerkship Director Clerkship Site Coordinator Arlo Kahn, MD Kathy Carlson 501-686-6564 501-686-6564 Scott Laffoon, MD Cheryl Broadaway Robin Mouzy 870-972-9603 870-336-7941 870-931-9137 870-930-2911 ex 271 Block Rotation Site Director Michael Macechko, MD Longitudinal Site Director Linda McGhee, MD 479-750-6585 or 1-800-292-2541 479-521-0263 Clerkship Site Coordinator Janice Huddleston Longitudinal Site Coordinator Morgan Hogue UAMS Northeast - Jonesboro Clerkship Site Director Clerkship Site Coordinator UAMS Northwest - Springdale 479-521-0263 479-466-9847 479-713-8303 UAMS South - Magnolia Clerkship Site Director Clerkship Site Coordinator Elisabeth Avramescu, MD Jana Terry 870-234-7676 870-234-7676 ext 1215 870-866-3005 cell Herb Fendley, MD Cynthia Turner 870-541-6010 870-541-3179 870-541-6010 or 800-395-6011 Kyle Diaz, MD Debbie Birmingham Lusk 870-779-6021 870-779-6063 Bryan Clardy, MD Allexcia Rankin 479-424-3193 479-424-3175 or 479-785-2431 UAMS South Central – Pine Bluff Clerkship Site Director Clerkship Site Coordinator UAMS Southwest - Texarkana Clerkship Site Director Clerkship Site Coordinator UAMS West – Fort Smith Clerkship Site Director Clerkship Site Coordinator Northwest Campus Longitudinal Program CLERKSHIP DIRECTOR Arlo Kahn, M.D. UAMS Main Campus 4301 W. Markham Little Rock, AR 72205 Office: 501-686-6564 SITE DIRECTOR Linda McGhee, M.D. Office: UAMS Regional Program Center 1125 North College Fayetteville, AR Office #: 479-521-0265 NW Contact Morgan Hogue Office: UAMS Northwest Campus College of Medicine Office #: 479-713-8303 Cell: 479-409-9039 Email: mahogue2@uams.edu The Goals and Objectives used with the longitudinal students are the same as with the traditional block students. Please see the section on UAMS Northwest for site specific information. 6 Clerkship Policies: Please follow the UAMS Student Manual policies for all topics on this page. http://com.uamsonline.com/files/2012/05/STDMAN-webversiondecember-2013.pdf Attendance Policy: Family Medicine Clerkship: Attendance is required throughout the entire 4 week rotation. Page 107 Note: While third year medical students do not have personal or sick days, we do recognize illness or personal emergencies may occur. Absentee Policy for the Junior Year page 107 Vacation Policy: page 112 All Junior Medical students receive Christmas Break (December 20 – January 4, 2015) and Spring Break (March 30 – April 5, 2015) and all College of Medicine holidays as noted in the College of Medicine Academic Schedule. Work Hour Rules page 108 Student Participation in Invasive Procedures page 10 Notification of Grades page 34 7 Student Responsibilities 1. Participate in patient care at the assigned clinical facilities. 2. Develop a knowledge base and understanding of problems common to Family Medicine through exposure to these problems in clinical care. 3. Complete all didactic assignments. 4. Attend Family Medicine conferences, seminars, and other educational activities. Follow the College of Medicine Attendance Policies. 5. Complete all student evaluation forms. Faculty Responsibilities 1. Communicate with students about the clerkship program and be available when questions or problems arise concerning course content or curriculum. 2. Meet with students periodically to discuss the strengths and weaknesses of the clerkship to date and to ensure that students have a meaningful learning experience. 3. Provide timely submission of written evaluations to the Dean’s office. Final grades will be assigned at the end of each rotation. 8 Family Medicine Clerkship Goals and Objectives A variety of activities are planned in order to reach the goals and objectives below. The assessment for each objective describes how students will be evaluated. Goal #1: Medical Knowledge: The student will learn the diagnosis and management of common problems in Family Medicine. Learning Objectives: At a level appropriate for a third year medical student, the student will: 1.1. See a variety of patients from specific categories of diseases and document each encounter on their O2 requirement checklist. 1.2. Will demonstrate knowledge of diagnosis and management of acute and chronic health problems by scoring above a required minimum on fmCase exam and final NBME test. Assessment: 1. Students will have seen the required number of patients from each category that is listed on the O2 requirement checklist. 2. Scores on the fmCases exam and final NBME test must be sufficient to receive a passing grade for the rotation. 3. Fund of knowledge is evaluated as a routine part of the clinical evaluation by preceptors. Goal #2: Patient Care: The student will demonstrate a basic level of competency in gathering patient information, with an emphasis on problem-specific history taking, physical examination and problem solving skills required to adequately assess and manage problems commonly encountered in Family Medicine. Learning Objectives: At a level appropriate for a third year medical student, the student will: 2.1 Obtain a problem-specific history, review past medical history and conduct an appropriately focused physical examination based on the patient’s reported complaint. 2.2 The students will be able to present history and physical exam finding with written documentation as well as in verbal presentations during encounters in the outpatient clinic. 2.3 Exhibit an appreciation for comprehensive, coordinated, culturally competent and continuous care for individuals and their families through participation in direct clinical care with patients of all age groups. 2.4 Investigate patient barriers to chronic disease management and overall health. Assessment: 1. Patient care is evaluated by each preceptor as a routine part of the clinical evaluation. 2. Each student will be directly observed at least once by clinical faculty as they perform a history and physical examination. 9 Goal #3: Interpersonal and Communication Skills: The student will establish effective and ethically sound relationships with patients, faculty and staff that facilitate the provision of quality health care. Learning Objectives: At a level appropriate for a third year medical student, the student will: 3.1 Provide concise and accurate presentations to faculty and resident preceptors. 3.2 Communicate effectively and demonstrate caring, respectful and culturally sensitive behaviors when interacting with patients and their families. 3.3 Communicate effectively with members of the inter-professional team including nurses, physicians, office staff and consultants to provide patient-focused care. Assessment: 1. Interpersonal and communication skills are evaluated by each preceptor as a routine part of the clinical evaluation. 2. Each student will be directly observed at least once by clinical faculty as they perform a history and physical examination. 3. Preceptors and clinical faculty will evaluate students as to their interpersonal relationships with peers. Goal #4: Population Health and Preventive Medicine: The student will apply principles of wellness and health promotion in the provision of patient care. Learning Objectives: At a level appropriate for a third year medical student, the student will: 4.1 Demonstrate familiarity with appropriate resources for health promotion and disease prevention during discussions with clinical preceptors. 4.2 Examine the role of fitness, nutrition, and smoking cessation in health promotion. 4.3 Counsel patients about the effect of harmful personal behaviors and habits and appropriate health maintenance strategies. 4.5 Recommend appropriate immunizations based on age and risk factors. Assessment: 1. Adequate performance on the Nutrition and Cardiovascular Disease On-Line Module. 2. Adequate performance of the fmCases related to population health and preventive medicine. 3. Counseling skills are evaluated as a routine part of the clinical evaluation by preceptors. 10 Goal #5: Practice –Based and System-Based Healthcare: The student will be introduced to aspects of the organization and management of a family medicine clinic. Learning Objectives: At a level appropriate for a third year medical student, the student will: 5.1 Observe and discuss cost effective healthcare and resource allocation affecting the practice of family medicine. 5.2 Discuss billing and coding with preceptors during patient visits in the outpatient clinic. Assessment: 1. Adequate completion of the on-line Health reform module. 2. Cost effectiveness, billing, and coding are discussed and assessed with preceptors during patient care. Student understanding is assessed as part of the routine clinical evaluation. 3. The performance of the student as part of the healthcare team is reported as part of the clinical evaluation. Goal #6: Professionalism: The student will demonstrate a commitment to excellence and ongoing professional development and will be provided feedback concerning his/her performance during the clerkship. Learning Objectives: At a level appropriate for a third year medical student, the student will: 6.1 Actively seek and act upon feedback and constructive criticism about performance, application of medical knowledge and interpersonal interactions with staff from faculty and staff. 6.2 Demonstrate a commitment to ethical principles pertaining to the provision of clinical care, confidentiality of patient information and informed consent. 6.3 Demonstrate interest and eagerness to learn through review of medical literature and use of information technology. 6.4 Attend all required activities and complete all assignments in a timely manner. 6.5 Display proper dress, grooming, punctuality, honesty and respect for patients and all members of the healthcare team. Assessment: 1. Attendance, dress and punctuality are closely monitored by the site coordinator. 2. Eagerness to learn through review of medical literature and use of information technology is assessed by the site director as part of the Evidence-Based Medicine Module. 3. Commitment to ethical principles and response to feedback is assessed as a routine part of the clinical evaluation and during the mid-clerkship and wrap-up sessions with site directors. 11 Goal#7: Medical Informatics: The student will effectively and efficiently use scientific studies to manage information and optimize patient care. Learning Objectives: At an appropriate level for a third year medical students, the student will: 7.1 Identify a clinical problem or question pertinent to the specialty of family medicine, conduct a literature search, critique the quality of the information gathered and discuss the article and the conclusions drawn. 7.2 Demonstrate the utility of the electronic medical record in quality patient care including a review of active problem list, flow sheet data and past medical history. Assessment: 1. Objective 7.1 is assessed by the adequate performance on the Evidence-Based Medicine module. 2. Use of EMR and guidelines for clinical care are assessed as a routine part of the clinical evaluation by preceptors. 12 Resources Students should ask the Clerkship Coordinator at their assigned sites for information on access to designated computers. There should be computers available at the clinic or library of each site where students can access the internet and the UAMS website. There is no required textbook for this course. We encourage you to use UpToDate http://www.uptodate.com as you care for patients on this rotation and to use the other resources listed here as references and study guides for the NBME exam. Blueprints: Family Medicine – Will be provided Case Files: Family Medicine – Will be provided AAFP Thumb Drive-will be provided AAFP Website http://www.aafp.org/home.html USPSTF A-Z Topic Guide http://www.uspreventiveservicestaskforce.org/uspstopics.htm Prevention, Detection, Evaluation & Treatment of Hypertension: The JNC 7 Report http://www.nhlbi.nih.gov/guidelines/hypertension/phycard.pdf 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults Report from the Panel Members Appointed to the Eighth Joint National Committee (JNC 8) http://jama.jamanetwork.com/article.aspx?articleid=1791497&resultClick=3 Prevention, Detection, Evaluation & Treatment of High Blood Cholesterol: National Cholesterol Education Program High Blood Cholesterol Desk Reference http://www.nhlbi.nih.gov/guidelines/cholesterol/atglance.pdf http://circ.ahajournals.org/content/129/25_suppl_2/S1.full 13 Grades and Evaluations The Department of Family Medicine will issue the grade “A”, “B”, or “C”, as defined in the UAMS College of Medicine’s grading policy. Under highly unusual circumstances the department may issue the grade of “I” when work is incomplete at the end of the clerkship or academic year. The minimum passing standard for the Junior Year Family Medicine Clerkship will be met by attaining at least 50% of all possible points. The final grade for the clerkship will be calculated from the following components: Clinical Performance Evaluations NBME Final Subject Exam fmCases Exam 55% 30% 15% Additional requirements in order for grades to be released include satisfactory completion of the following activities: Nutrition and CVD Project Patient Log Viewing of Healthcare Reform Video Interactive Video Seminars Site-specific Conference Attendance Evidence-Based Medicine Project Grading Example: Clerkship student Athena receives 250 out of a possible 300 points on her clinical performance (from 5 preceptor evaluations); a raw score of 74 on her NBME final subject exam (62 percentile rank for the national norm); and a 14 out of a possible 15 points on her fmCases exam. Her grade is calculated as follows: Clinical Performance: 250/300=83.33%; NBME national percentile: 62% fmCases Exam: 14/15=93.33%; Total Points: 83.33 x 0.55= 46 points 62.00 x 0.30= 19 points 93.33 x 0.15= 14 points 46 +19+14= 79 points 14 78-100 points = 60-77 points = 50-59 points= A B C In this example, Athena would receive an “A” for the course. Grade Appeal Process: A student may appeal their clinical performance scores in the following order: 1. Clerkship Site Director 2. Course Director 3. Promotion Committee Board Students at Risk of Failure All Students will receive a mid-rotation evaluation approximately two weeks into the rotation. If a student is identified as performing unsatisfactorily in the Clerkship, he/she will be informed and a written improvement plan will be developed. Every effort will be made on the part of the instructor to assist the student in improving his/her performance. Requirement and Evaluation Details: A) Clinical Performance Clinical performance evaluations will be requested from each clinical instructor (faculty or resident) who has had an adequate opportunity to work with the student in the clinic or in another significant capacity. The final clinical performance score will be based on the average of ratings from clinical instructors. A copy of the evaluation form used is on page 19 - 21. Clinical performance constitutes 55% of the final grade for the clerkship. B) NBME Subject Exam This web-based exam is required by the College of Medicine. We recognize that the comprehensive nature of Family Medicine makes this exam particularly challenging. (Please see NBME distribution of question topics below on page18. To aid in preparation, Case Files Family Medicine and Blueprints in Family Medicine books are loaned to the student at orientation. These books must be returned at the final NBME session to receive a grade. The NBME Subject Exam constitutes 30% of the final grade for the clerkship. 15 C) fmCases. This project is to be completed by the 3rd Thursday of the rotation. A 15- item multiple choice test will be given on the third Friday of the rotation and will cover information in the required fmCases cases. Please see page 17 18 for instructions. This exam constitutes 15% of the final grade for the clerkship. D) Evidence Based Medicine Project: (EBM) This project teaches students the skills of critical appraisal of the literature. The student will work through the process of developing a clinical question, performing an on-line journal search, choosing a journal article, appraising the article, and presenting findings to the site director. Please see Appendix A on page 24 -36 for background and instructions on how to complete the EBM project. The EBM project is pass/fail. Final grades will not be released until this requirement is completed. E) Nutrition and CVD Project . This project is to be completed by the 2nd Friday of the rotation. The student will be provided with a booklet to record risks for coronary heart disease for 10 patients and a detailed nutrition and CVD risk assessment on 1 patient seen during the clerkship. This information will be used to complete the on-line module in Blackboard. Please turn in the booklet to your site coordinator prior to leaving the site. Please see page 18 for instructions. This project is pass/fail. Final grades will not be released until this requirement is completed. F) Requirement Checklist The recording of patient encounters will be accessed through the Oasis (O2) software. The student will be required to record all of the patients seen, where seen, student’s level of involvement with the patient, key diagnoses addressed at the visit, and the preceptor (faculty or resident).The site director will review the checklist at the mid-clerkship evaluation and sign off at the end of the clerkship. The requirement checklist will also have a place to document when a faculty member observes student performance of a history and physical. This observation will be either in person or by digital recording. Completion of the log is pass/fail. Final grades will not be released until the log is completed. G) Healthcare Reform Video. Please view this video within the first ten (10) days of the clerkship. The student will be required to view the presentation by Dr. Joe Thompson on Health care reform and the potential impact that it will have on the practice of medicine in the future. It can be found in Blackboard. 16 This project is pass/fail. Final grades will not be released until this requirement is completed. H) Interactive Video Seminars The topics of Diabetes, Hypertension and Hyperlipidemia will be presented by 3 PharmD professors located at the UAMS Regional program centers. The presentations will be on the 2nd, 3rd, and 4th Tuesday’s of the rotation. They are currently schedule from 1:30 – 2:30 pm with a 30 minute question and answer session following the presentations. Check with the site coordinator for the location of the presentations. An evaluation will be sent from O2. I) Conferences Students are required to attend conferences at their respective sites. The Site Director or Coordinator will describe these on the first day of the rotation. fmCases fmCases is a series of interactive virtual patient cases that are designed to build clinical competency, fill educational gaps, and teach the core values and attitudes of family medicine through an evidence-based and patient-centered approach to patient care. The on-line virtual patient cases are at www.medu.org. Each student will be required to register at the Med-U website using the students UAMS e-mail address. Student will be expected to work through each case assigned and have the weekly cases completed during the assigned week. At the web site, scroll to the bottom to see: Click on the fmCases button. Click on the Sign in button. On the next screen click on the gray Register button, Follow the instructions on the screen that comes up. Once registered, you will then have access to the fmCases. Over the first 3 weeks of the clerkship, students will complete the following cases: #1. 45-year-old female annual exam – Mrs. Payne #2. 55-year-old male annual exam – Mr. Reynolds #6. 57-year-old female presents for diabetes care visit – Ms. Sanchez #8. 54-year-old male with elevated blood pressure – Mr. Martin #10. 45-year-old male presenting with low back pain – Mr. Payne 17 #20. 28-year-old female with abdominal pain – Ms. Bell #35. (CLIPP #2) Infant well child (2, 6 and 9 months) - Asia #40. (SIMPLE # 16)45-year-old man who is overweight – Mr. James Nutrition and Cardiovascular Disease Module To help you understand the role of nutrition in Cardiovascular Disease including prevention, you will be responsible for completing the Cardiovascular Disease and Nutrition Assessment booklet and online module and discussing it with your site director or their designee towards the end of your rotation. NBME Distribution of Question Topics Distribution Across Age Groups Childhood 5%–15% Adolescence 5%–10% Adulthood 65%–75% Geriatric 10%–15% General Principles 10%–15% Infancy and childhood (normal growth and development) Adolescence (sexuality, separation from parents/autonomy; puberty) Senescence (normal physical and mental changes associated with aging) Medical Ethics and Jurisprudence Applied Biostatistics and Clinical Epidemiology Patient Safety Organ Systems Immunologic Disorders 1%–5% Diseases of the Blood and Blood-forming Organs 1%–5% Mental Disorders 5%–10% Diseases of the Nervous System and Special Senses 5%–10% Cardiovascular Disorders 10%–15% Diseases of the Respiratory System 10%–15% 18 Nutritional and Digestive Disorders 10%–15% Gynecologic Disorders 5%–10% Renal, Urinary, and Male Reproductive System 5%–10% Disorders of Pregnancy, Childbirth, and the Puerperium 1%–5% Disorders of the Skin and Subcutaneous Tissues 1%–5% Diseases of the Musculoskeletal System and Connective Tissue 5%–10% Endocrine and Metabolic Disorders 5%–10% Physician Task Promoting Health and Health Maintenance Understanding Mechanisms of Disease 15%–20% 5%–10% Establishing a Diagnosis 30%–35% Applying Principles of Management 25%–30% Clinical Performance Evaluation Form in O2 1. Patient Care: History taking, physical exam, and presentation skills Generally incomplete; frequently disorganized without pertinent information; lacks confidence (6) Generally complete, but needs direction in the organization of pertinent information. Major exam finding missed. (7) Generally complete with good organization. Usually includes all important information. Clearly prepared and confident. (8) Complete and thorough. Well organized. All important information consistently included. Reliable, selection of facts highlights understanding. (9) Outstanding history taking and exam. Superior organization and always includes important information. (10) Not Observed 2. Medical Knowledge: Overall fund of knowledge and ability to apply to patient care Limit knowledge of disease, pathophysiology, diagnosis, and treatment. No application to patient care. (6) Inconsistent knowledge of disease, pathophysiology, diagnosis, and treatment. Poor application to patient care. (7) 19 Appropriate fund of knowledge for level of training. Can sometimes apply to basic patient care principles. (8) Very good knowledge base. Consistently applies basic science to medical pathophysiology. (9) Superior knowledge of disease, pathophysiology, diagnosis, and treatment. Frequently applies knowledge to complex patient care scenarios. (10) Not Observed 3. Practice-Based Learning: Use of experiences and feedback as well as evidence based medicine for improvement Rarely show initiative in seeking out information, feedback, etc. Infrequently responds to instruction. (6) Seeks out information but only when directed to do so. Difficulty in accepting instruction. (7) Often show initiative in seeking out information. Responsive to instruction and feedback. (8) Shows clear evidence of seeking out additional knowledge. Engages in outside reading and research. Shows great initiative after receiving instruction. (9) Exceptional initiative in seeking out information; uses PDA, web-based, and other resources in daily activities. (10) Not Observed 3. Interpersonal Communication Skills: Based on interactions with faculty, residents, staff, patients, and families Poor team skills. Works in isolation. Does not interact well with medical staff or patients. (6) Difficulty in collaborating with others. Self-centered goals. Basic communication with patients and families only. (7) Ease of communications with all staff. Cooperative and reliable. Good member of team. Mature and dependable. Sensitive to others. Shares pertinent information. (8) Staff and peer relationships are productive and meaningful. Establishes good rapport with other hospital staff, patients, and families. Always a team player. (9) Outstanding interpersonal skills. Appropriately respectful, mature, and cooperative. Superior team member. (10) Not Observed. 4. Professionalism Disruptive behavior. Unreliable. Fails to study, read, or investigate. Does not attend assigned duties or is frequently late. Unprofessional attire. (6) 20 Lacks insight into own deficits and ignores feedback. Assumes responsibility only when stimulated. Frequently late or misses lectures and rounds. Unprepared. Marginal behavior and appearance. (7) Good insight into own deficits & assets. Incorporates feedback. Assumes share of workload, conscientious & reliable. Punctual with good attendance for assigned duties. Generally aware of professional behavior & responsibilities. (8) Almost always prepared & punctual. Identifies sensitive issues & addresses them. Marked improvement on skills addressed with feedback. Proactive in patient responsibilities & takes ownership of patients. Exhibits self-directed investigation & study. (9) Curious and solicits feedback. Exceptional insight into strengths and deficits. Exceptionally hard worker. Unusually mature and professional. Always courteous, well groomed, punctual, and prepared. (10) Not Observed 5. Systems Based Practice: Understanding the health care delivery system on a global and local level Poor knowledge of health care delivery. Lacks interest in learning basic systems issues. (6) Limited knowledge of health care delivery. Can use basic campus systems inconsistently. (7) Appropriate knowledge of health care delivery. Consistently uses local systems for patient care. Desire to learn. (8) Good understanding of health care delivery. Actively seeks out new information for education. Shows application of newly obtained knowledge. (9) Superior knowledge and understanding of health care delivery. Can help others in use of local systems. Able to identify system barriers to patient care. (10) Not Observed 6. General Comments (Use complete, grammatically correct sentences. These comments WILL BE USED in the students' Dean's Letters): 7. Additional comments NOT to be included in Dean's Letters (Include areas needing improvement): 21 Clerkship and Preceptor Evaluations by Students The student will log into the O2 during the last few days of the clerkship rotation to complete the course and preceptor evaluations. These must be completed before grades can be released. Course Evaluation by Students This process is anonymous and the comments are collated and reviewed by the entire faculty at the end of the academic year. This feedback from students informs the faculty about student concerns in order that the clerkship can improve from year to year. We appreciate your honest input, but expect your statements to be made in a professional manner. This evaluation is one of the Dean’s office requirements. Faculty/Resident Evaluation: The purpose of gathering this information is to evaluate the effectiveness of our clinical preceptors. This information will be shared quarterly with preceptors Course Evaluation Items 1. 2. 3. 4. 5. 6. 7. 8. Organization: Clinical experience was well organized, information and procedures were presented in a logical sequence, student assignments and activities were well organized. Clarity: Goals and objectives of the clinical experience were clear, faculty expectations of the students were clear, course content was presented clearly, and questions were answered understandably. Testing: Material on exams was related to material covered during the clinical experience. Participation: Clinical experience provided adequate opportunities for "hands-on" experience and for appropriate student participation in the patient care process of this specialty. Content: Informational content of the clinical experience was current and facilitated student ability to achieve clerkship goals and objectives. Professional Characteristics: Instructor(s) demonstrated qualities that were of use to me (respect for Students, Cultural Awareness, and Respect for Health Professions). Overall: The quality of this course is outstanding. Comments: Please make any comments about this clerkship here. 22 Faculty Evaluation Items 1. The above named faculty/house-staff participated in my learning experiences during this rotation. 2. Organization and Clarity (presents material in an organized fashion, understands students' questions and answers questions clearly, emphasizes important points, summarizes well). 3. Enthusiasm (is enthusiastic about medicine and the teaching of medicine, stimulates student interest, is dynamic and energetic, and enjoys teaching). 4. Knowledge (is knowledgeable in his/her specialty area, discusses recent developments, directs students to appropriate research/literature, demonstrates breadth of knowledge, discusses multiple viewpoints). 5. Rapport (listens attentively to students and residents, is interested in student progress, treats students and residents with respect, is sensitive to needs of others, asks/answers questions and corrects students in a positive manner, is accessible to students and residents). 6. Communication Skills (uses resources and technology effectively, encourages student participation, reinforces students efforts, gears teaching to student level of readiness, uses questions effectively, helps students organize and clarify their thoughts about patient problems, demonstrates clinical procedures and techniques well, communicates effectively, explains well). 7. Clinical Supervision (communicates performance expectations to students and residents, actively guides development of clinical skills, provides specific, appropriate practice opportunities, directly oversees performance frequently) 8. Professional Characteristics (sensitive to moral and ethical practice issues, demonstrates empathy with patients, takes responsibility for actions, has selfconfidence, recognizes limitations, is open-minded and non-judgmental, does not display arrogance) 9. Overall excellence of instructor (based on the responses to items above, the summative evaluation for this preceptor would be.....) 10. Enter any additional comments in the space provided. 23 Appendix A: EVIDENCE-BASED MEDICINE MODULE Definition of EBM Evidence-based medicine is the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence-based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research. Student Responsibilities: Week 1 – Identify a clinical problem or a question that you’ve encountered in the care of patients at the clinic site. Week 2 – Conduct a literature search on that problem or question and pick an article that you want to present. Beginning, Week 3 – Critique the quality of the information gathered, i.e., are the claims in the article supported by the research, using the Duke University Critical Appraisal Worksheets. Ending, Week 3 – Be prepared to discuss the article reviewed and conclusions drawn from your research with the site director. Students will fill out the Evidence-Based Medicine Clerkship Worksheet (sample given below on page 35 - 36) which will be e-mailed to them or they may use the form below and submit it electronically to Little Rock using the address at the bottom of the form. If you encounter problems with electronic submission, print your completed form and turn it in to the coordinator on the last day of the rotation. Presentation –All students will meet with their site assigned faculty moderator and present their clinical question and an overview of their article. Students will review their Evidence-Based Medicine Clerkship Worksheets. This is a requirement of the clerkship. Four basic principles of EBM 1. Build a good clinical question 2. Conduct an efficient search for the best external evidence (search PubMed, EBSCO, etc.) 3. Critically appraise the literature for validity and relevance 4. Apply what has been learned to clinical practice Four elements of a well-built clinical question (P.I.C.O.) 1. What is the Problem or patient issue? 2. What is the educational Intervention or the exposure to the new/different material? 24 3. Is there a Comparison group or intervention? 4. What is the educational Outcome? Criteria for article selection: 1) All articles should be peer-reviewed and published in a medical/scientific journal. 2) For this exercise, the studies should be limited to experimental designs (Randomized controlled trials), the more scientifically convincing epidemiological/observational studies (Cohort or case control designs), or some combination of any of the 3 designs above (see attached description of the study designs, if necessary). Review articles, meta analyses, and case reports-are not acceptable for this exercise. 3) Keep in mind that many times information from more than one article is necessary to make a good clinical or research-based decision on any particular topic; however, this exercise is only requiring the selection of one article. Included below: a) Review of study types b) Duke University Critical Appraisal Worksheets to help you evaluate the validity of your article. The hyperlinks below are for an optional EBM tutorial and for online versions of the worksheets: http://www.hsl.unc.edu/services/tutorials/ebm/index.htm http://guides.mclibrary.duke.edu/content.php?pid=274373&sid=2262222 c) Evidence-Based Medicine Clerkship Worksheet Background Common Study Designs The descriptions below include the types of studies allowed for article selection for the clerkship (randomized controlled trials, cohort, and case control), plus descriptions for other types of studies (surveys, ecological studies, review articles, meta-analysis, case series) for your information. This summary was provided by Bridget Mosley, MPH. Randomized controlled trials: An experimental study in which the study participants are randomly assigned by a research investigator to a treatment group and followed for the outcome(s) of interest. The goal is usually to evaluate the effects of one or more types of treatments/therapies/medications on a disease or condition. The randomization helps ensure that the treatment alone resulted in the outcomes being observed. These studies are usually the more expensive 25 studies, because they require close monitoring and follow-up procedures. But, they are also the most convincing scientifically. Ethical considerations and expense prevent many research questions from being addressed with this type of study design. Examples: Women’s Health Init.: Rossouw JE et. al. Risk and benefits of hormone replacement therapy in postmenopausal women. JAMA 2002; 288: 321-33. Tashkin DP. et. al. Cyclophosphamide versus placebo in scleroderma lung disease. New Eng J Med. 2006; 354(25):265566. Cohort: An observational study in which a research investigator observes the exposure levels of interest among the study participants, classifies participants into an exposure group based upon a priori criteria, and then follows the participants for the outcome(s) of interest. These types of studies are commonly used when assessing a causal relationship between a detrimental or preventive exposure (especially rare exposures) and a health condition of interest. These studies can be prospective, i.e., the health outcome has not occurred or been identified at the time of study enrollment, or retrospective, i.e., the status of the health outcomes has occurred and been recorded in a data set, but the investigator are only assessing the outcomes after exposure statuses have been determined. A well-designed prospective cohort study can be quite convincing to the scientific community. Examples: Framingham Heart Study: Wilson PWF, et. al. Creactive protein and risk of CVD in men and women. Arch Intern Med. 2005; 165: 2473-8. Polluck BE, et. al. Patient Outcomes after Vestibular Schwannoma Management: Comparison of Microsurgical Resection and Stereotactic Radiosurgery. Neurosurgery. 2006; 59(1): 77-85. Case-control: An observational study in which a research investigator observes and classifies study participants into groups based upon their disease status or health condition, and then retrospectively assesses their exposure levels prior to the disease occurring. These types of studies are commonly used when assessing a causal relationship between a detrimental or preventive exposure and a health condition of interest. For rare diseases, these types of studies are the most common and feasible design to use. Example: National Birth Defects Prevention Study: Cleves MA, et. al. Maternal use of acetaminophen and NSAIDs and ventricular septal defects. Birth Defects Research Part A. 2004; 70(3):107-13 26 Adelow C, et. al. Epilepsy as a risk factor for cancer. J Neurology, Neurosurg & Psych. 2006; 77(6):784-6. Surveys (cross-sectional studies): An observational study in which a research investigator assesses both exposure and disease outcome at the same time and usually with the same measurement tool. Participants usually respond to self-reported survey questions and/or an investigator-led assessment tool on multiple exposure and health condition topics. These studies are commonly used to assess health behaviors and conditions among a large population. Example: Youth Risk Behavior Surveillance System: Eaton DK, et. al. YRBSSUnited States, 2005. MMWR Surv. Summ. 2006; 55(5):1-108 Ecological studies: An observational study in which a research investigator measures disease occurrence within a population and implies a connection with the prevalence of the exposure of interest within that same population. Individual level measurements for both exposure and disease are not conducted, only comparisons of rates/occurrence between populations are conducted. These types of studies are common for some environmental health assessments and evaluation of public health programs. Example: Honein MA et. al. Impact of food fortification on the occurrence of neural tube defects. JAMA. 2001; 283 (23): 2981-6. Review articles: A summary of multiple articles or scientific information on a specific topic into one report. These articles can be quite informative and convenient. Meta-analyses: A quantitative summary of multiple research studies on a specific research hypothesis. There is a whole discipline within statistics that concentrates on complex meta-analyses methods. Caution should be used when evaluating these reports, as some may not appropriately take into consideration the varying degrees of scientific credibility of the studies being assessed. Case series: A descriptive report on a unique event or rare disease occurring in the medical community. Usually these reports only involve a few patients and no statistical comparisons take place. These reports may be helpful to develop new hypotheses or to inform the medical/scientific community of new diseases or treatments. Other clinical trials or experimental studies (not randomized): 27 An experimental study that does not involve randomizing participants into treatment groups. Assignment to a treatment group may be based upon medical evidence, self-selection, or convenience sampling. Other: Some studies use combinations of any of the above. Tips for reviewing Medical/Scientific articles in general: For any type of study, remember to look for: Measurement errors: Measurement errors are possible and are not uncommon in research studies. Understanding those errors and how they may be influencing the observed results helps one better know how to interpret the findings. Some studies are more prone to certain types of errors than others. When reviewing an article one should ask if the tools used to identify the outcomes of interest and the treatment/exposure of interest are misclassifying participants. This becomes a major concern for the study if the misclassification is occurring differentially within the study population, i.e., errors are different across the study groups being compared. Uncontrolled factors: The epidemiological terms for these are confounders and effect modifiers. These are factors that are not the primary topics of interest to the investigator, but could be influencing these results. A classic confounder for many studies is smoking. Smoking may confound an evaluation between alcohol and cancer, because alcohol drinkers are more likely to be smokers than non-drinkers and smoking is linked with higher risk of cancer. There are ways to control for many of these factors, either by the design of the study or by statistical methods. Sample size: Many have heard that studies with a larger number of participants are better than studies with smaller numbers. This is primarily because larger samples, or more units to analyze, provide more statistical power to see differences when making a comparison. Clinical/biological/logistical relevance vs. statistical significance: Given a large enough sample size in a research study, small differences between comparisons groups will reach statistical significance. However, other considerations should be taken into account as to whether the observed difference in the outcomes is relevant to the clinical question being considered. A difference of 2 mm Hg in systolic blood pressure between 2 study groups taking different medications may not have clinical significance given the cost or convenience of one over the other. 28 Representation: Does the study group represent a population that is equivalent to a population that is of interest to you? This may be a concern if one is looking at gender or ethnic-specific populations, or those with certain medical conditions. Tips for reviewing Randomized Controlled Trials: Did the randomization work? o In theory, did the investigator design the study so that randomization of participants could properly occur? o From the results, did randomization truly occur? The study groups being compared should be equivalent on all factors other than the intervention factor (hint: These comparisons are usually reported in the one of the first descriptive/demographic tables in the results.). Was blinding appropriately conducted so that participant/investigator bias was limited? o Single-blind = participants blinded to intervention o Double-blind= participants and investigator measuring outcomes are blinded to the intervention Was the follow-up time period between the intervention and outcome appropriate clinically/biologically for the outcome to occur? If participants were asked to administer the intervention (e.g. take medications, etc.) were measures in place to ensure compliance? Was an “intent to treat” approach used for data analysis, meaning those allocated to a specific group were analyzed in that group no matter if they remained in that group or not? What were effects due to loss-to-follow-up, participant withdraw, etc? We usually think that at least 80% participation at the end of the study is good, but this could be flexible. Were the results convincing? Take into account the biological/clinical significance as well as the statistical significance. Tips for reviewing Cohort Epidemiological Studies: Measurement bias: Measurement errors may occur when the participants are classified by their exposure of interest. Remember that an investigator in these studies does not control how much “exposure” a participant receives, only records what is observed. 29 Was follow-up time period between the potential exposure and outcome appropriate clinically/biologically for the outcome to occur? What were the effects due to loss-to-follow-up, participant withdrawal, etc? Uncontrolled or unidentified factors (confounders) should always be considered in observational studies Tips for reviewing case-control studies: Recall bias: Most case control studies are subject to potential recall bias. Primary exposures of interest in these studies are actually measured after the health outcome has occurred. Thus, a participant diagnosed with a disease may recall or record the events in the exposure time period differently than a control participant who does not have the disease. Sample size: Many times case control studies are conducted on “rare diseases”, thus limited number of study participants. An assessment as to whether the sample size was appropriate to address the hypotheses of interest should be considered. Uncontrolled or unidentified factors (confounders) should always be considered in observational studies. Quick review of statistical significance: Statistical testing is used to assess if the results observed from a research study are considered different between 2 or more comparison groups. The end product from these tests will be either a p-value calculated from a specific statistical test or a ratio (odds, risk, or hazard ratio) with a corresponding confidence interval. P-values: For the non-epidemiologist/statistician, one could think of the p-value as the likelihood that the observed difference between comparison groups occurred by “chance”, i.e., not influenced by the intervention/exposure of interest. A p-value of 0.30 would indicate that there was a 30% likelihood that the observed difference between groups was due to chance. The most common “cut-point” used to decide if a comparison is statistically different or not is a p-value of 0.05. Any statistical test resulting in a p-value less than or equal to 0.05 is considered statistically significant, thus different between the 2 groups. 30 If the study is designed appropriately, this would imply that the intervention/ exposure of interest influenced that difference. A resulting p-value greater than 0.05 is considered not statistically different, thus any difference between the groups could be due to chance alone and not attributed to the intervention/exposure of interest. Ratios and confidence intervals: When the rate or odds of a health outcome occurring in one group is divided by the rate or odds of that health outcome occurring in a different group, an investigator will get a ratio number. If these rates or odds are similar between the groups, the ratio will be close to 1 (exactly 1 if the rates are identical). Ratios can be greater than 1, indicating that the intervention group (numerator or top number) had higher risk of the outcome than the comparison group (denominator or bottom number). Or, the ratios can be less than one, indicating a protective effect of the intervention of interest. o Example 1: The odds of smoking among cancer patients may be observed at 15.2%, while the odds of smoking among participants without cancer was observed at 5.7%. The corresponding odds ratio would be 15.2 / 5.7 = 2.7. o Example 2: The rate of neural tube defects among women taking folic acid vitamins periconceptionally was 4 per every 10,000 live birth, while the rate among women not taking a vitamin was 7 per every 10,000 live birth. The risk ratio would be 4 / 7 = 0.57. Confidence intervals (CI) are used to assess statistical significance between groups. The most common used in scientific research is the 95% CI. This can be thought of as equivalent to the 0.05 p-value cutpoint mentioned above. A confidence interval is a calculation of a range of variance (low and high ends) where the ratio measure is included within that range. o If 1.0 is included within that range of the interval, the comparison between the 2 groups is not considered statistically significant. o If 1.0 falls outside that range of the interval (either higher or lower) than the difference between the 2 groups is considered statistically significant and thus may be attributed to the exposure of interest. 31 Above examples: Ratios Smoking among cancer 15.2 / 5.7 = 2.7 patients vs. non-cancer participants 95% confidence interval (1.3, 3.8) statistically significant since 1.0 is not within CI NTDs among folic acid users vs. non-users (0.43, 1.23) not statistically significant since 1.0 is within CI 4 per 10,000 / 7 per 10,000 = 0.57 CRITICAL REVIEW FORM FOR PROGNOSIS STUDY Citation: Users’ Guide: Article: Are the Results Valid? Was the sample of patients representative? Were patients sufficiently homogenous with respect to prognostic risk? Was follow-up complete? Were objective and unbiased outcome criteria used? What are the Results? How likely are the outcomes over time? How precise are the estimates of likelihood? How can I apply the results to patient care? Were the study patients and their management similar to my own? Was the follow-up study long? Can is use the results in managing patients in my practice? From McMaster EBCP Workshop/Duke University Medical Center – 03/18/03, 5/12/09 32 CRITICAL REVIEW FORM FOR DIAGNOSIS STUDY Citation: Users’ Guide: Article: Are the Results Valid? Did the clinicians face diagnostic uncertainty? Was there blind comparison with an independent gold standard? Did the results of the test being evaluated influence the decision to perform the gold standard? What are the Results? What likelihood ratios are associated with the range of possible test results? How can I apply the results to my patient care? Will the reproducibility of the test result and its interpretation be satisfactory in my setting? Are the results applicable to my patient? Will the results change my management? Will patients be better off as a result of the test? Are the benefits worth the potential harms and costs? From McMaster EBCP Workshop/Duke University Medical Center – 03/18/03, 5/12/09 33 CRITICAL REVIEW FORM FOR THERAPY STUDY Citation: Users’ Guide: Article: Are the Results Valid? Did experimental and control groups begin the study with a similar prognosis? Were patients randomized? Was randomization concealed? Were patients analyzed in the groups to which they were randomized? Were patients in the treatment and control groups similar with respect to known prognostic factors? Did experimental and control groups retain a similar prognosis after the study started? Were 5 important groups (patients, caregivers, collectors of outcome data, adjudicators of outcome, data analysts) aware of group allocation? Aside from the experimental intervention, were groups treated equally? Was follow-up complete? What are the Results? How large was the treatment effect? How precise was the treatment effect? How can I apply the results to my patient care? Were the study patients similar to my patient? Were all patient-important outcomes considered? Are the likely benefits worth the potential harms and costs? From McMaster EBCP Workshop/Duke University Medical Center – 03/18/03, 5/12/09Grading for Evidence Based Medicine Module 34 Category Quality of Clinical Question Thoroughness and Effectiveness of Literature Search: Completion of the EBM Worksheet Reflects the 4 elements: 1)population 2)intervention 3)comparison 4)outcome appropriately Student has all elements of thorough and effective literature search: 1) adequate search method 2) explained why the article was chosen 3) study type is appropriate to answer clinical question All parts of the worksheet are complete Evidence-Based Medicine Worksheet: Student Name: ________________________ Block _________ Clerkship site____________________________ E-Mail Address: ________________________________ (If you do not have E-mail, please enter your home address) Describe your initial question: This question was based on: Previous rotation Personal interest Patient seen in FM clinic (outpatient) Patient seen in hospital Describe your final question, including: Patient/Problem, Intervention, Comparison, Outcomes Your final question was based on: Discussion with preceptor or other faculty Research material available on subject Discussion with resident(s) Orientation material Other reasons (please describe): 35 Identify source of your information Title & Author ______________________________________________________ Journal (name, volume #, etc.)_________________________________________ Source: Internet - online OVID - online Medline - Library - utilized research librarian Index Medicus - CD-Rom- hardcopy - Other source not mentioned: _____________________ Describe the following components of your article: Background: Methods: Result: Conclusion: Summarize validity based on the type of question asked & article selected. (choose the type(s) that most apply and summarize below) Treatment article (discuss trial design, patients similar to your biases, significance) Diagnosis article (describe identification of disease & test, comparison w/ gold standard, reasonableness, patients similar to yours) Prognosis article (discuss inception cohort, selection criteria, follow-up, patients similar to yours, where subjects came from) Why does this matter to you or your patient (Usefulness) What is your interpretation of the information? How will the information be applied to your clinical practice? Send back to predocadminoffice@uams.edu 36