DRP Assessment
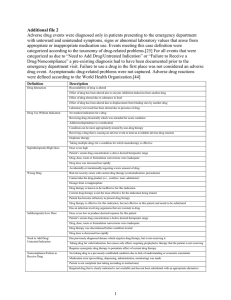
advertisement

Patient Assessment- Process to Identify Drug-Related Problems (DRPs) 1. Gather Information: Before starting to work through the process of identifying DRPs it is important to: o Observe the patient’s presentation (i.e. physical appearance, emotional state) o Gather relevant patient information Create a Patient Database o Data can be obtained from various sources including the patient, medical record, family members (with permission), other healthcare workers (pharmacist, nurse, physician, etc..), Netcare (laboratory findings) o Critical components of the database include a Medical History and Medication History Medical History Review medical record and interview the patient Medication History Review medical record, Netcare/PIN, interview the patient/caregivers, contact community pharmacy 2. Identify Drug-related Problems: Categories of Drug-Related Problems (DRPs): Assessment Indication Efficacy Safety Adherence Type of DRP Unnecessary Drug Additional Drug Therapy Required Ineffective Drug- incorrect drug or drug product Dose too Low (correct drug, wrong dose) Adverse Drug Reaction Dose too High (toxicity) Drug Interaction Nonadherence (not taking enough drug) Overadherence (taking too much drug) Evaluate the following parameters: INDICATION Review Medical History o Consider medical condition/problems, patient signs/symptoms, abnormal laboratory findings Medication History Patient preferences and goals of therapy o Does the patient even want drug therapy? Non-drug measures Is the problem caused by a drug? (review current and past drugs) Inquire Is drug therapy indicated? If drug therapy is not indicated, can it be discontinued? If drug therapy is indicated: o Has drug therapy been initiated? o Is there an indication for each of the drugs listed? o Are there any medical problems that require drug therapy, but are not being currently treated? Why? o Are there non-drug measures that can be considered? Is drug therapy appropriate? o Consider patient preference/ needs, drug efficacy, drug safety, adherence and cost o If not, why? (i.e. contraindication, adverse effect, non-adherence) EFFICACY Review Goals of Therapy for each medical problem Efficacy Monitoring Parameters for drug therapy o Consider drug efficacy, subjective/objective parameters; timeframe anticipated to achieve the desired outcome. Inquire Is drug therapy effective for each indication? o Consider goals of therapy and efficacy monitoring parameters. If drug therapy is not effective, why? o Consider additional therapies, non-adherence, low dose/dosing frequency/titration, interaction, onset of action, malabsorption, formulation ADHERENCE Review Medication History Medical History Inquire Is the patient able to take drug therapy as prescribed? If unable to adhere to therapy, why? o Adverse effect, incorrect dosage form/frequency, directions not understood, cost/drug access, patient preference, ability to self-medicate (i.e. age, dexterity, vision, swallowing, memory) SAFETY Review - Safety Monitoring Parameters for drug therapy Signs & symptoms experienced by the patient Abnormal laboratory data Drug interactions (drug-drug, drug-disease, drug-food) Inquire Is the patient experiencing adverse effects that could be caused by drug therapy? o Consider safety monitoring parameters o Consider causality, timeframe, type of reaction [i.e. dose-related, hypersensitivity] Is the drug dose too high? o Consider weight, organ function, age, drug kinetics/therapeutic index, duration of therapy Can the adverse effect be managed? o Consider dose decrease, patient education, timeframe, need for additional drug therapy, nonpharmacologic intervention o If the drug is discontinued, is there another appropriate therapy instead? Are there any significant drug interactions? o Consider drug-drug, drug-food, drug-disease interactions Can the drug interaction be managed? o Consider onset/offset, dosage adjustment, spacing apart, food effect, drug substitution, increased monitoring, therapeutic drug monitoring (TDM) Draft Document- Pharmacy Patient Care Working Group Jan 2011


![Quality assurance in diagnostic radiology [Article in German] Hodler](http://s3.studylib.net/store/data/005827956_1-c129ff60612d01b6464fc1bb8f2734f1-300x300.png)