approved
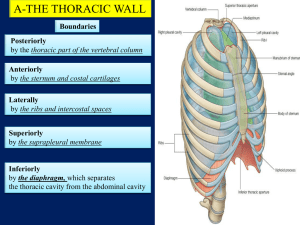
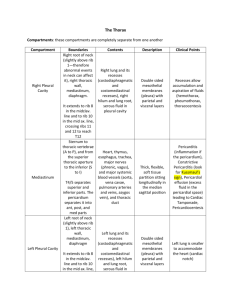
advertisement

Ministry of Health of Ukraine BUKOVINIAN STATE MEDICAL UNIVERSITY “APPROVED” on methodical meeting of the Department of Anatomy, Topographical anatomy and Operative Surgery “………”…………………….2008 р. (Protocol №……….) The chief of department professor ……………………….……Yu.T.Achtemiichuk “………”…………………….2008 р. METHODICAL GUIDELINES for the 3d-year foreign students of English-spoken groups of the Medical Faculty (speciality “General medicine”) for independent work during the preparation to practical studies THE THEME OF STUDIES “Topographical anatomy and operative surgery of the thoracic wall and pectoral gland” MODULE I Topographical Anatomy and Operative Surgery of the Head, Neck, Thorax and Abdomen Semantic module “Topographical Anatomy and Operative Surgery of the Thorax” Chernivtsi – 2008 1. Actuality of theme: The topographical anatomy and operative surgery of the thorax are very importance, because without the knowledge about peculiarities and variants of structure, form, location and mutual location of their anatomical structures, their agespecific it is impossible to diagnose in a proper time and correctly and to prescribe a necessary treatment to the patient. Surgeons usually pay much attention to the topographo-anatomic basis of surgical operations on the thorax. 2. Duration of studies: 2 working hours. 3. Objectives (concrete purposes): To know the definition of regions of the thorax. To know classification of surgical operations on the thorax. To know the topographical anatomy and operative surgery of the thoracic wall and organs of the thoracic cavity. 4. Basic knowledges, abilities, skills, that necessary for the study themes (interdisciplinary integration): The names of previous disciplines 1. Normal anatomy 2. Physiology 3. Biophysics The got skills To describe the structure and function of the different organs of the human body, to determine projectors and landmarks of the anatomical structures. To understand the basic physical principles of using medical equipment and instruments. 5. Advices to the student. 5.1. Table of contents of the theme: The thorax (or chest) is the region of the body between the neck and the abdomen. The framework of the walls of the thorax (thoracic cage) is formed posteriorly by the thoracic part of the vertebral column; anteriorly by the sternum and costal cartilages; laterally by the ribs and intercostal spaces; superiorly by the suprapleural membrane; and inferiorly by the diaphragm, which separates the thoracic cavity from the abdominal cavity. The thorax is an irregularly shaped cylinder with a narrow opening (superior thoracic aperture) superiorly and a relatively large opening (inferior thoracic aperture) inferiorly. The superior thoracic aperture is open, allowing continuity with the neck; the inferior thoracic aperture is closed by the diaphragm. The thoracic cage protects the lungs and heart and affords attachment for the muscles of the thorax, upper extremity, abdomen, and back. Structure of the Thoracic Wall The thoracic wall is covered on the outside by skin and by muscles attaching the shoulder girdle to the trunk. It is lined with parietal pleura. As physicians you will be examining the chest to detect evidence of disease. Your examination will consist of inspection, palpation, percussion, and auscultation. Inspection shows the configuration of the chest, the range of respiratory movement, and any inequalities on the two sides. The type and rate of respiration will also be noted. Palpation will enable the physician to confirm the impressions gained by inspection, especially of the respiratory movements of the chest wall. Abnormal protuberances or recession of part of the chest wall will be noted. Abnormal pulsations will also be felt and tender areas detected. Percussion is a sharp tapping of the chest wall with the fingers. This produces vibrations that extend through the tissues of the thorax. Air-containing organs such as the lungs produce a resonant note; conversely, a more solid viscus such as the heart produces a dull note. With practice, it is possible to distinguish the lungs from the heart or the liver by percussion. Auscultation enables the physician to listen to the breath sounds as the air enters and leaves the respiratory passages. Should the alveoli or bronchi be diseased and filled with fluid, the nature of the breath sounds will be altered. The rate and rhythm of the heart can be confirmed by auscultation, and the various sounds produced by the heart and its valves during the different phases of the cardiac cycle can be heard. It may be possible to detect friction sounds produced by the rubbing together of diseased layers of pleura or pericardium. To make these examinations, a physician must be familiar with the normal structure of the thorax and must have a mental image of the normal position of the lungs and heart in relation to identifiable surface landmarks. Furthermore, it is essential that a physician be able to relate any abnormal findings to easily identifiable bony landmarks so that he or she can accurately record and communicate them to colleagues. Since the thoracic wall actively participates in the movements of respiration, many bony landmarks change their levels with each phase of respiration. In practice, to simplify matters, the levels given are those usually found at about midway between full inspiration and full expiration. The Landmarks and the Projections of the Thoracic Wall Anterior Chest Wall The suprasternal notch is the superior margin of the manubrium sterni and is easily felt between the prominent medial ends of the clavicles in the midline. It lies opposite the lower border of the body of the second thoracic vertebra. The sternal angle (angle of Louis) is the angle made between the manubrium and body of the sternum. It lies opposite the intervertebral disc between the 4th and 5th thoracic vertebrae. The xiphisternal joint is the joint between the xiphoid process of the sternum and the body of the sternum. It lies opposite the body of the 9th thoracic vertebra. The xiphoid process, lies in the depression where the converging costal margins form the infrasternal angle. The xiphoid projects over the left lobe of the liver into the epigastric region of the abdomen. The subcostal, or infrasternal, angle is situated at the inferior end of the sternum, between the sternal attachments of the 7th costal cartilages. The costal margin is the lower boundary of the thorax and is formed by the cartilages of the th th 7 , 8 , 9th, and 10th ribs and the ends of the eleventh and twelfth cartilages. The lowest part of the costal margin is formed by the 10th rib and lies at the level of the 3rd lumbar vertebra. The clavicle is subcutaneous throughout its entire length and can be easily palpated. It articulates at its lateral extremity with the acromion process of the scapula. Ribs There are 12 pairs of ribs, all of which are attached posteriorly to the thoracic vertebrae. The upper 7 pairs are attached anteriorly to the sternum by their costal cartilages. The 8-10th pairs of ribs are attached anteriorly to each other and to the 7th rib by means of their costal cartilages and small synovial joints. The 11th and 12th pairs have no anterior attachment and are referred to as floating ribs. A typical rib is a long, twisted, flat bone having a rounded, smooth superior border and a sharp, thin inferior border. The inferior border overhangs and forms the costal groove, which accommodates the intercostal vessels and nerve. The first rib lies deep to the clavicle and cannot be palpated. The lateral surfaces of the remaining ribs can be felt by pressing the fingers upward into the axilla and drawing them downward over the lateral surface of the chest wall. The 12th rib can be used to identify a particular rib by counting from below. However, in some individuals, the 12th rib is very short and difficult to feel. For this reason an alternative method may be used to identify ribs by first palpating the sternal angle and the second costal cartilage. Nipple In the male it usually lies in the fourth intercostal space about 4 inches (10 cm) from the midline. In the female its position is not constant. Diaphragm The central tendon of the diaphragm lies directly behind the xiphisternal joint. In the midrespiratory position the summit of the right dome of the diaphragm arches upward as far as the upper border of the fifth rib in the midclavicular line, but the left dome only reaches as far as the lower border of the fifth rib. Apex Beat of the Heart The apex of the heart is formed by the lower portion of the left ventricle. The apex beat is caused by the apex of the heart being thrust forward against the thoracic wall as the heart contracts. The apex beat is normally found in the 5th left intercostal space 9 cm from the midline. Should you have difficulty in finding the apex beat, have the patient lean forward in the sitting position. In the female with pendulous breasts, the examining fingers should gently raise the left breast from below as the intercostal spaces are palpated. Axillary Folds The anterior fold is formed by the lower border of the pectoralis major muscle. This can be made to stand out by asking the patient to press a hand hard against the hip. The posterior fold is formed by the tendon Trachea The trachea extends from the lower border of the cricoid cartilage (opposite the body of the sixth cervical vertebra) in the neck to the level of the sternal angle in the thorax. It commences in the midline and ends just to the right of the midline by dividing into the right and left principal bronchi. At the root of the neck it may be palpated in the midline in the suprasternal notch. Lungs The apex of the lung projects into the neck. It can be mapped out on the anterior surface of the body by drawing a curved line, convex upward, from the sternoclavicular joint to a point 2.5 cm above the junction of the medial and intermediate thirds of the clavicle. The anterior border of the right lung begins behind the sternoclavicular joint and runs downward almost reaching the midline behind the sternal angle. It then continues downward until it reaches the xiphisternal joint. The anterior border of the left lung has a similar course, but at the level of the fourth costal cartilage it deviates laterally and extends for a variable distance beyond the lateral margin of the sternum to form the cardiac notch. This notch is produced by the heart displacing the lung to the left. The anterior border then turns sharply downward to the level of the xiphisternal joint. The lower border of the lung in midinspiration follows a curving line, which crosses the sixth rib in the midclavicular line and the eighth rib in the midaxillary line, and reaches the tenth rib adjacent to the vertebral column posteriorly. It is important to understand that the level of the inferior border of the lung changes during inspiration and expiration. The posterior border of the lung extends downward from the spinous process of the seventh cervical vertebra to the level of the tenth thoracic vertebra and lies about 4 cm from the midline. The oblique fissure of the lung can be indicated on the surface by a line drawn from the root of the spine of the scapula obliquely downward, laterally and anteriorly, following the course of the sixth rib to the sixth costochondral junction. In the left lung the upper lobe lies above and anterior to this line; the lower lobe lies below and posterior to it. In the right lung is an additional fissure, the horizontal fissure, which may be represented by a line drawn horizontally along the fourth costal cartilage to meet the oblique fissure in the midaxillary line. Above the horizontal fissure lies the upper lobe and below it lies the middle lobe; below and posterior to the oblique fissure lies the lower lobe. Pleura The boundaries of the pleural sac can be marked out as lines on the surface of the body. The lines, which indicate the limits of the parietal pleura where it lies close to the body surface, are referred to as the lines of pleural reflection. The cervical pleura bulges upward into the neck and has a surface marking identical to that of the apex of the lung. A curved line may be drawn, convex upward, from the sternoclavicular joint to a point 2.5 cm above the junction of the medial and intermediate thirds of the clavicle. The anterior border of the right pleura runs down behind the sternoclavicular joint, almost reaching the midline behind the sternal angle. It then continues downward until it reaches the xiphisternal joint. The anterior border of the left pleura has a similar course, but at the level of the fourth costal cartilage it deviates laterally and extends to the lateral margin of the sternum to form the cardiac notch. Note that the pleural cardiac notch is not as large as the cardiac notch of the lung. It then turns sharply downward to the xiphisternal joint. The lower border of the pleura on both sides follows a curved line, which crosses the 8th rib in the midclavicular line and the 10th rib in the midaxillary line, and reaches the 12th rib adjacent to the vertebral column, that is, at the lateral border of the erector spinae muscle. Note that the lower margins of the lungs cross the 6th, 8th, and 10th ribs at the midclavicular lines, the midaxillary lines, and the sides of the vertebral column, respectively, and the lower margins of the pleura cross, at the same points, respectively, the 8th, 10th, and 12th ribs. The distance between the two borders corresponds to the costodiaphragmatic recess. Heart For practical purposes the heart may be considered to have both an apex and four borders. The apex, formed by the left ventricle, corresponds to the apex beat and is found in the fifth left intercostal space 9 cm from the midline. The superior border, formed by the roots of the great blood vessels, extends from a point on the 2nd left costal cartilage (remember sternal angle) 1.5 cm from the edge of the sternum to a point on the third right costal cartilage 1.5 cm from the edge of the sternum. The right border, formed by the right atrium, extends from a point on the third right costal cartilage 1.5 cm from the edge of the sternum downward to a point on the 6th right costal cartilage 1.5 cm from the edge of the sternum. The left border, formed by the left ventricle, extends from a point on the 2nd left costal cartilage 1.5 cm from the edge of the sternum to the apex beat of the heart. The inferior border, formed by the right ventricle and the apical part of the left ventricle, extends from the 6th right costal cartilage 1.5 cm from the sternum to the apex beat. Thoracic Blood Vessels The arch of the aorta and the roots of the brachiocephalic and left common carotid arteries lie behind the manubrium sterni. The superior vena cava and the terminal parts of the right and left brachiocephalic veins also lie behind the manubrium sterni. The internal thoracic vessels run vertically downward, posterior to the costal cartilages, 1.5 cm lateral to the edge of the sternum, as far as the 6th intercostal space. The intercostal vessels and nerve ("vein, artery, nerve" – VAN - is the order from above downward) are situated immediately below their corresponding ribs. Posterior Chest Wall The spinous processes of the thoracic vertebrae can be palpated in the midline posteriorly. The first spinous process to be felt is that of the 7th cervical vertebrae (vertebra prominens). Below this level are the overlapping spines of the thoracic vertebrae. The spines of C1-6 vertebrae are covered by a large ligament, the ligamentum nuchae. It should be noted that the tip of a spinous process of a thoracic vertebra lies posterior to the body of the next vertebra below. The scapula (shoulder blade) is flat and triangular in shape and is located on the upper part of the posterior surface of the thorax. The superior angle lies opposite the spine of the 2nd thoracic vertebra. The spine of the scapula is subcutaneous, and the root of the spine lies on a level with the spine of the 3rd thoracic vertebra. The inferior angle lies on a level with the spine of the 7th thoracic vertebra. The Thoracic Apertures The bony thorax has two apertures or openings. The superior thoracic aperture is often referred to as the thoracic inlet, and the inferior thoracic aperture is sometimes called the thoracic outlet. The Superior Thoracic Aperture The head, neck, and limbs communicate with the thoracic cavity through the thoracic inlet or superior thoracic aperture. Through this relatively small, kidney-shaped opening (about 5 cm anteroposteriorly and 11 cm transversely) pass structures entering and leaving the thorax, such as the trachea (windpipe), esophagus (gullet), and the great arteries and veins that supply and drain the head, neck, and upper limbs. This aperture is limited by the body of the first thoracic vertebra posteriorly, the first pair of ribs and their costal cartilages anterolaterally, and the superior end of the manubrium of the sternum anteriorly. As the margin of the aperture slopes inferoanteriorly, the apex of each lung and its covering of pleura (pleural cupula) project superiorly through the lateral parts of the thoracic inlet. The Inferior Thoracic Aperture At the thoracic outlet or inferior thoracic aperture, the thoracic cavity is separated from the abdominal cavity by the musculotendinous thoracic diaphragm. Most structures that pass from the thorax to the abdomen, or vice versa, go through openings in the diaphragm (e.g., the inferior vena cava, aorta, and esophagus). The thoracic outlet is uneven and is much larger than the superior thoracic aperture. The inferior thoracic aperture, which slopes inferoposteriorly, is limited by the 12th thoracic vertebra posteriorly, the 12th pair of ribs and costal margins anterolaterally, and the xiphisternal joint anteriorly. On its way to the upper limb, the subclavian artery crosses the first rib, producing a distinct groove. This artery may be compressed where it passes over this rib, producing vascular symptoms, e.g., pallor, coldness, and cyanosis (blue color) of the hands. Less frequently, nerve pressure symptoms (numbness and tingling) in the digits result from pressure on the inferior trunk of the brachial plexus. These conditions have been described under several different terms (e.g., the thoracic inlet syndrome), depending on what the author thought was the cause of the symptoms. Usually the condition is called the neurovascular compression syndrome. The designation thoracic inlet syndrome has also been used to describe the signs and symptoms resulting from multiple enlarged lymph nodes that constrict the superior thoracic aperture or thoracic inlet. These nodes usually enlarge as the result of infiltration of them by malignant cells from a lymphosarcoma, a lymphatic tumor. As a result, blood does not drain normally from the head, neck, and upper limbs and they become congested with blood and appear swollen. Anatomic and physiologic changes in the thorax with aging Certain anatomic and physiologic changes take place in the thorax with advancing years: • The rib cage becomes more rigid and loses its elasticity as the result of calcification and even ossification of the costal cartilages; this also alters their usual radiographic appearance. • The stooped posture (kyphosis), so often seen in the old because of degeneration of the intervertebral discs, decreases the chest capacity. • Disuse atrophy of the thoracic and abdominal muscles can result in poor respiratory movements. • Degeneration of the elastic tissue in the lungs and bronchi results in impairment of the movement of expiration. These changes, when severe, diminish the efficiency of respiratory movements and impair the ability of the individual to withstand respiratory disease. Coordinate System of the Thoracic wall The horizontal and the vertical imaginary lines are used to describe surface locations on the anterior and posterior chest walls. Horizontal Lines of Orientation These lines correspond to the ribs and intercostal spaces. Vertical Lines of Orientation Midsternal line: Lies in the median plane over the sternum. Sternal line: Runs vertically downward over the edge of sternum. Parasternal line: Lies between the sternal line and midclavicular line. Midclavicular line: Runs vertically downward from the midpoint of the clavicle. Anterior axillary line: Runs vertically downward from the anterior axillary fold. Midaxillary line: Runs vertically downward from a point situated midway between the anterior and posterior axillary folds. Posterior axillary line: Runs vertically downward from the posterior axillary fold. Scapular line: Runs vertically downward on the posterior wall of the thorax, passing through the inferior angle of the scapula. Paravertebral line: Lies between the scapular line and vertebral line. Vertebral line: Lies vertically over the transverse processes of the thoracic vertebrae. Posterior sagittal line: Lies in the median plane over the spinous processes of the thoracic vertebrae. The regions of the thorax There are 5 regions of the anterior chest wall and 5 regions of the posterior chest wall. The lateral boundaries between them are the left and right midaxillary lines. The regions of the anterior chest wall are: - sternal region (unpaired) - anterosuperior region (left and right) - anteroinferior region (left and right) The regions of the anterior chest wall are: - vertebral region (unpaired) - scapular region (left and right) - subscapular region (left and right) Layers of the Thoracic Wall Conventionally there are three layers of the thoracic wall: - Superficial layer (skin; subcutaneous fatty tissue with the superficial blood vessels and nerves; superficial fascia with the mammary glands); - Medium layer (investing, or pectoral, fascia; muscles); - Deep layer (bones of the thoracic cage; intercostal spaces; internal thoracic vessels; transverses thoracic muscles; visceral, or endothoracic, fascia; parietal pleura). Superficial layer of the thoracic wall The skin of the anterior thoracic areas is thin and mobile, but behind it is thicken. The superficial fascia is composed of loose connective tissue. The hypodermis contains a variable amount of fat, sweat glands, blood and lymphatic vessels and nerves. Some blood vessels and nerves are forms the neurovascular fascicles, which provide the blood supply of the superficial soft tissues: - lateral thoracic artery and veins, long thoracic nerve; - superior thoracic artery and veins, supraclavicular nerves; - thoracoacromial artery and veins, lateral pectoral nerve; cutaneous branches from the intercostal nerves and vessels. Mammary gland The mammary (lactiferous) gland is a modified sweat gland; this explains why it has no special capsule or sheath. It lies in the superficial fascia, anterior to the thorax. The deep aspect of the breast is separated from the pectoral muscles by the deep fascia. Between the breast and deep fascia, there is an area of loose connective tissue that contains little fat. This zone, referred to as the retromammary space (bursa), allows the breast to move freely on the deep fascia covering the pectoralis major muscle. Although easily separated from the deep fascia, the mammary gland is firmly attached to the skin of the breast by suspensory ligaments (Cooper's ligaments). These fibrous bands, which support the breast, run between the skin and the deep fascia. The rounded contour and most of the bulk of the breasts are produced by fat lobules, except during pregnancy and lactation when the mammary glands enlarge. The shape of the breast varies considerably in different persons and races and in the same person at different ages. During puberty the lactiferous ducts undergo branching and there is an increased deposition of fat. As a result, progressive enlargement of the breasts occurs. In some women the breasts enlarge slightly during their menstrual cycles owing to the increase in gonadotropic hormones. During pregnancy the breasts enlarge greatly owing to the formation of new glandular tissue. The milk-secreting cells, referred to as alveoli, are arranged in grapelike clusters or lobules. Although the mammary glands are prepared for secretion by midpregnancy, milk is not secreted until after delivery of the fetus and placenta. Colostrum, a creamy white to yellowish premilk fluid, may be expressed from the nipples during the last trimester of pregnancy. Near term, colostrum often leaks from the nipples. In multiparous women (those who have borne several children), the breasts may become large and pendulous. In elderly women the breasts are small and wrinkled owing to the decrease in adipose and glandular tissue. Although breasts vary markedly in size, their roughly circular bases are fairly constant and have the following limits in well-developed females: vertically from the second to sixth ribs and laterally from the edge of the sternum to the midaxillary line. Two-thirds of the breast rest on the pectoralis major muscle; one-third covers the serratus anterior muscle. Its inferior border overlaps the superior part of the rectus sheath. The skin of the breasts around the nipples is called areolae. The lactiferous ducts give rise to buds that form 15 to 20 lobules of glandular tissue, which constitute the mammary gland. Each lobule is drained by a lactiferous duct, which opens on the nipple. These ducts extend from the nipple in a manner similar to spokes of a wheel. Deep to the areola, each duct has a dilated portion called the lactiferous sinus, in which milk accumulates during lactation. Accessory breasts (polymastia) or nipples (polythelia) may occur superior or inferior to the normal breasts. Usually supernumerary breasts consist of a nipple and areola that may be mistaken for a mole or nevus (birthmark). They may appear anywhere along a line extending from the axilla to the groin; this is the location of the embryonic mammary ridge. A transient increase in the size of the breasts of boys commonly occurs during puberty; however, in some boys with the Klinefelter syndrome (over 50%), the breasts enlarge during puberty and usually increase slowly in size over a period of years. Enlargement of the breasts (gynecomastia) is often the presenting symptom in young men with this syndrome, who usually have an XXY sex chromosome complex. The areolae contain numerous sebaceous glands, which enlarge during pregnancy and secrete an oily substance that provides a protective lubricant for the areola and nipple. The areolae, variable in size, are pink in white nulliparous women (those who have not borne children). There is no fat beneath the areolae. During the first pregnancy the areolae of white women change permanently to brown; the depth of colour depends on the woman's complexion. The nipples are conical or cylindrical prominences that are located in the center of the areolae. There is no fat in the nipples. In nulliparous women they are usually located at the level of the fourth intercostal spaces. However, the position of the nipple varies considerably and therefore cannot be used as a guide to the fourth intercostal space. The tip of the nipple is fissured and contains the openings of the lactiferous ducts. The nipples are composed mostly of circularly arranged smooth muscle fibers that compress the lactiferous ducts and erect the nipples when they contract. Arterial Supply of the Breast. There is an abundant blood supply to the breast. The arteries are mainly from the internal thoracic artery via its perforating branches, which pierce the 2nd to 4th intercostal spaces. The breast also receives several branches from the axillary artery, mainly from its lateral thoracic and thoracoacromial branches and lateral and anterior cutaneous branches from the intercostal arteries (in the 3rd to 5th intercostal spaces). Venous Drainage of the Breast. Veins from the breast drain into the axillary, internal thoracic, lateral thoracic, and intercostal veins. The chief venous drainage is to the axillary vein. Lymphatic Drainage of the Breast. Most lymph passes from the mammary gland along interlobular lymphatic vessels to a subareolar plexus. From here and other parts of the breast, most lymph vessels follow the veins of the breast to the axilla. Most of the lymphatic drainage (about 75%) is to the axillary lymph nodes, mainly the pectoral groupof nodes. They are located along the inferior border of the triangular pectoralis minor muscle, which lies deep to the pectoralis major. From the deep surface of the breast, the lymphatics pass through the pectoralis major muscle and drain into the apical group of axillary lymph nodes. Lymph from the medial part of the breast drains into the parasternal lymph nodes, which are located within the thorax along the internal thoracic vessels. Lymph from the skin of the breast may pass to the abdominal wall and the opposite breast. Innervation of the Breast. The breast is supplied by lateral and anterior cutaneous branches of the 2nd to 6th intercostal nerves. These nerves include both sensory and sympathetic fibers, which supply the skin, smooth muscle of the areolae and nipples, blood vessels, and mammary glands. The breasts are usually equal in size, but if one is larger and more inferior, it is usually the right one. The superolateral quadrant of the breast contains a large amount of glandular tissue and is where most breast cancers develop. This tissue may extend superior to the clavicle and/or inferiorly into the epigastrium. Similarly, glandular tissue from one breast may cross the median plane. The vascularity of the breasts begins to increase early in pregnancy. The increased blood supply dilates the vessels, often making them visible. The connections of the intercostal veins with the vertebral venous plexuses provide a route for spread of cancer cells from the breast to the vertebrae and then to the skull and brain. When carcinoma or CA of the breast invades the retromammary space and attaches to or invades the deep fascia covering the pectoralis major muscle, contraction of this muscle causes the breast to move superiorly. This is a clinical sign of advanced malignant disease of the breast. The lymphatic and venous drainage of the breasts is of highest importance in the spread of CA of the breast (breast cancer), one of the two most common types of cancer in women. Cancer cells are carried from the breast by lymph vessels to lymph nodes, chiefly those in the axilla . The cells lodge in these nodes where they produce nests of tumor cells called metastases (G. meta, beyond + stasis, a placing). As there is free communication between lymph nodes inferior and superior to the clavicle and between the axillary and cervical (neck) lymph nodes, metastases from the breast may develop in the supraclavicular lymph nodes, the opposite breast, or in the abdomen. The axillary lymph nodes are the most common site of metastases from CA of the breast. Enlargement of these nodes in a woman therefore suggests the possibility of breast cancer. Cancerous nodes tend to be hard, but they are not usually tender. The absence of enlarged axillary lymph nodes is no guarantee that metastasis from a breast cancer has not occurred. Often there is dimpling and a thickening of the skin over the site of a CA of the breast, giving it the appearance of an orange peel; this skin change is called “orange skin”. Interference with the lymphatic drainage of the breast produces the leathery thickening, whereas dimpling of the skin is mainly caused by infiltration of cancer cells along the suspensory ligaments. This invasion shortens the ligaments and causes the skin to invaginate (dimple). Subareolar CA may cause inversion of the nipple by the same mechanism. Methods of Examination of the Breast Mammography (radiographic examination of the breast) is one of the radiographic techniques used to detect breast masses. Mammographs are also used by surgeons to guide them during the removal of breast tumors, cysts, and abscesses. Breast tumors emit more heat than normal breast tissue, consequently thermography is used as a method of measuring and recording heat radiation emitted by the breast. It is sometimes used in conjunction with mammography. Computerized tomography (CT) is also combined with mammography for detection of breast cancer. Before CT scans are taken, an iodide-contrast material is given intravenously to the patient. Breast cancer cells have an unusual affinity for iodide and so become recognizable. Medium layer of the thoracic wall The investing, or pectoral, fascia is thin but is usually dense and loosely attached to the superficial fascia. It forms an envelope, deep to the superficial fascia, which is adherent to the underlying muscles and constitutes their covering, called epimysium. The pectoral fascia can be separated only by sharp dissection because the epimysium sends septa into the muscles. This fascia covers the muscles up to their attachment to bone (e.g., the sternum and ribs) and is itself attached to the periosteum of bones. The part of investing fascia between the clavicle and the upper edge of pectoralis minor muscle is named clavipectoral, or coracoclavicular, fascia. Muscles of the Thorax Many muscles are attached to the ribs, such as the anterolateral muscles of the abdomen and some back muscles. The pectoral muscles, covering the anterior thoracic wall, usually act on the upper limbs, but the pectoralis major can also function as an accessory muscle of respiration to expand the thoracic cavity when inspiration is deep and forceful. In addition, the serratus anterior muscle, which protrudes the scapula, runs around the anterolateral surface of the thorax from the scapula. It is also an accessory muscle of respiration. The accessory muscles of respiration (pectoralis major and serratus anterior) are often used by patients with respiratory problems or heart failure when they struggle to breathe. They hold onto a table to fix their pectoral girdles (clavicles and scapulae) so these muscles can act on their attachments to the ribs. Deep layer of the Thorax Intercostal spaces The spaces between the ribs are called intercostal spaces. Each space contains three muscles of respiration: the external intercostal, the internal intercostal, and the innermost intercostal muscle. The innermost intercostal muscle is lined internally by the endothoracic fascia, which is lined internally by the parietal pleura. The intercostal nerves and blood vessels run between the intermediate and deepest layers of muscles. They are arranged in the following order from above downward: intercostal vein, intercostal artery, and intercostal nerve (i.e., VAN). Intercostal arteries and veins Each intercostal space contains a large single posterior intercostal artery and two small anterior intercostal arteries. The posterior intercostal arteries of the first two spaces are branches from the superior intercostal artery, a branch of the costocervical trunk of the subclavian artery. The posterior intercostal arteries of the lower nine spaces are branches of the descending thoracic aorta. The anterior intercostal arteries of the first six spaces are branches of the internal thoracic artery. The anterior intercostal arteries of the lower spaces are branches of the musculophrenic artery, one of the terminal branches of the internal thoracic artery. Each intercostal artery gives off branches to the muscles, skin, and parietal pleura. In the region of the breast in the female, the branches to the superficial structures are particularly large. The corresponding posterior intercostal veins drain backward into the azygos or hemiazygos veins, and the anterior intercostal veins drain forward into the internal thoracic and musculophrenic veins. Intercostal nerves The intercostal nerves are the anterior rami of the first 11 thoracic spinal nerves. The anterior ramus of the 12th thoracic nerve lies in the abdomen and runs forward in the abdominal wall as the subcostal nerve. Each intercostal nerve enters an intercostal space between the parietal pleura and the posterior intercostal membrane. It then runs forward inferiorly to the intercostal vessels in the subcostal groove of the corresponding rib, between the innermost intercostal and internal intercostal muscle. The first six nerves are distributed within their intercostal spaces. The seventh to ninth intercostal nerves leave the anterior ends of their intercostal spaces by passing deep to the costal cartilages, to enter the anterior abdominal wall. In the case of the 10th and 11th nerves, since the corresponding ribs are floating, these nerves pass directly into the abdominal wall. Branches of the intercostal nerves • Rami communicantes connect the intercostal nerve to a ganglion of the sympathetic trunk. The gray ramus joins the nerve medial to the point at which the white ramus leaves it. • A collateral branch, which runs forward inferiorly to the main nerve on the upper border of the rib below. • A lateral cutaneous branch, which reaches the skin on the side of the chest. It divides into an anterior and a posterior branch. • An anterior cutaneous branch, which is the terminal portion of the main trunk, reaches the skin near the midline. It divides into a medial and a lateral branch. • Numerous muscular branches are given off by the main nerve and its collateral branch. • Pleural sensory branches to the parietal pleura. • Peritoneal sensory branches to the parietal peritoneum (seventh to eleventh intercostal nerves only). The first intercostal nerve is joined to the brachial plexus by a large branch that is equivalent to the lateral cutaneous branch of typical intercostal nerves. The remainder of the first intercostal nerve is small, and there is no anterior cutaneous branch. The second intercostal nerve is joined to the medial cutaneous nerve of the arm by a branch, called the intercostobrachial nerve, that is equivalent to the lateral cutaneous branch of other nerves. The second intercostal nerve therefore supplies the skin of the armpit and the upper medial side of the arm. In coronary artery disease, pain is referred along this nerve to the medial side of the arm. With the exceptions noted, the first six intercostal nerves therefore supply (a) the skin and the parietal pleura covering the outer and inner surfaces of each intercostal space, respectively, and (b) the intercostal muscles of each intercostal space and the levatores costarum and serratus posterior muscles. In addition, the seventh to the eleventh intercostal nerves supply (a) the skin and the parietal peritoneum covering the outer and inner surfaces of the abdominal wall, respectively, and (b) the anterior abdominal muscles, which include the external oblique, internal oblique, transversus abdominis, and rectus abdominis muscles. The Dermatomes Through the cutaneous branches of the dorsal and ventral rami, each spinal nerve supplies a continuous strip of skin, which extends from the posterior midline to the anterior midline. These strips of skin are called dermatomes. This term is derived from Greek and means skin slices. The thoracic and abdominal dermatomes are arranged in a segmental fashion because the thoracoabdominal nerves arise from segments of the spinal cord. There is considerable overlapping of contiguous or closely related dermatomes; i.e., each segmental nerve overlaps the territories of its neighbours. The first two intercostal nerves (Tl and T2) supply the upper limbs in addition to supplying the thoracic wall. Also note that the inferior five intercostal nerves (T7 to T11) supply the abdominal wall, as well as the thoracic wall. Bones of the thoracic wall The osteocartilaginous thoracic cage is formed by part of the vertebral column (12 thoracic vertebrae and intervertebral discs); 12 pairs of ribs and costal cartilages, and the sternum. The ribs and costal cartilages form the largest part of the thoracic cage. The Thoracic Vertebrae Thoracic vertebrae are unique in that they have facets on their bodies and transverse processes for articulation with the ribs (T11 and T12 are exceptions). Two demifacets are located laterally on the bodies of T2 to T9. The superior demifacet articulates with the head of its own rib and the inferior demifacet articulates with the head of the rib inferior to it. The costal facets of other vertebrae vary somewhat. T1 has a single costal facet for the head of the first rib and a small demifacet for the cranial part of the second rib. T10 has only one costal facet which is partly on its body and partly on its pedicle. T11 and T12 have only a single costal facet on their pedicles. The Spinous Processes. These bony projections from the vertebral arches of T5 to T8 are nearly vertical and overlap the vertebrae like roof shingles. This arrangement covers the small intervals between the laminae of adjacent vertebrae, thereby preventing sharp objects such as a knife from penetrating the vertebral canal and injuring the spinal cord. The spinous processes of Tl , T2, T11 and T12 are horizontal, and those of T3, T4, T9 and T10 slope inferiorly. The Ribs The first seven (and sometimes the eighth) pairs of ribs are called true or vertebrosternal ribs because they are connected to the sternum by their costal cartilages. The 8th to 12th pairs of ribs are false or vertebrochondral ribs. Each of the 8th to 10th ribs is connected by its costal cartilage to the cartilage of the rib superior to it. The 11th and 12th pairs of false ribs are often called vertebral or floating ribs because they are unattached anteriorly. They end in the muscles of the anterior abdominal wall. Although these ribs are free, they are not floating; they articulate with the body of their own vertebra. The 3rd to 9th ribs are typical. However, typical ribs vary slightly in length and other characteristics. The 1st, 2nd, and 10th to 12th pairs of ribs are atypical. The 1st rib is the broadest and most curved of all the ribs. It is also the shortest of the true ribs. The first rib is clinically important because so many structures cross or attach to it. It is flat and has a prominent scalene tubercle on the internal border of its superior surface for the attachment of the scalenus anterior muscle. The subclavian vein crosses the first rib anterior to the scalene tubercle and subclavian artery. The inferior trunk of the brachial plexus, a network of nerves on their way to the upper limb, passes posterior to it. A distinct groove is formed by the subclavian vessels and brachial plexus on the superior surface of the first rib. This rib articulates with the body of the first thoracic vertebra. The prominent tubercle of the first rib articulates with the transverse process of this vertebra. The 2nd rib has a curvature similar to the first rib, but it is thinner, much less curved, and is about twice as long as the first rib. It can easily be distinguished from the first rib by the presence of a broad, rough eminence, which is the tuberosity for the serratus anterior muscle. The 10th Rib is usually articulates with T10 vertebra only. The 11th and 12th ribs are short, especially the 12th pair. They are capped with a small costal cartilage, have a single facet on their heads, and have no neck or tubercle. The 11th rib has an illdefined angle and a shallow costal groove. The 12th rib has neither of these features and may be shorter than the first rib. Although there are usually 12 pairs of ribs, the number may be increased by the development of cervical ribs or lumbar ribs, or the number may be decreased by failure of the 12th pair to form (agenesis). Persons with trisomy 21 (Down syndrome) may have only 11 pairs of ribs. It is extremely rare to find an additional rib or pair of ribs in both the cervical and lumbar regions of the same person. Lumbar ribs are more common than cervical ribs, but they are usually quite small. The 12th rib may be absent on one side and shortened on the other side. Lumbar ribs have clinical significance in that they may confuse the identification of vertebral levels in radiographs and other images. A cervical rib (i.e., a rib arising from the anterior tubercle of the transverse process of the seventh cervical vertebra) occurs in about 0.5% of persons. It may have a free anterior end, may be connected to the first rib by a fibrous band, or may articulate with the first rib. The importance of a cervical rib is that it can cause pressure on the lower trunk of the brachial plexus in some patients, producing pain down the medial side of the forearm and hand and wasting of the small muscles of the hand. It can also exert pressure on the overlying subclavian artery and interfere with the circulation of the upper limb. Variations in the sternocostal junctions are not uncommon. The first seven costal cartilages nearly always join the sternum, but in some people, only six cartilages articulate with it. In other people, the eighth costal cartilage, especially on the right, joins the sternum. The 10th rib also "floats" in some people. Internal thoracic artery The internal thoracic artery supplies the anterior wall of the body from the clavicle to the umbilicus. It is a branch of the first part of the subclavian artery in the neck. It descends vertically on the pleura behind the costal cartilages, a fingersbreadth lateral to the sternum, and ends in the sixth intercostal space by dividing into the superior epigastric and musculophrenic arteries. Branches • Two anterior intercostal arteries for the upper six intercostal spaces. • Perforating arteries, which accompany the terminal branches of the corresponding intercostal nerves. • The pericardiacophrenic artery, which accompanies the phrenic nerve and supplies the pericardium. • Mediastinal arteries to the contents of the anterior mediastinum, for example, the thymus. • The superior epigastric artery, which enters the rectus sheath of the anterior abdominal wall and supplies the rectus muscle as far as the umbilicus. • The musculophrenic artery, which runs around the costal margin of the diaphragm and supplies the lower intercostal spaces and the diaphragm. Internal thoracic vein The internal thoracic vein begins as small veins accompanying the internal thoracic artery. The small veins eventually join to form a single vessel, which drains into the brachiocephalic vein on each side. Endothoracic fascia The endothoracic, or visceral, fascia is a thin layer of loose connective tissue that separates the parietal pleura from the thoracic wall. The suprapleural membrane is a thickening of this fascia. Suprapleural membrane The thoracic outlet transmits structures that pass between the thorax and the neck (esophagus, trachea, blood vessels, etc.) and for the most part lie close to the midline. On either side of these structures the outlet is closed by a dense fascial layer called the suprapleural membrane. This tent-shaped fibrous sheet is attached laterally to the medial border of the first rib and costal cartilage. It is attached at its apex to the tip of the transverse process of the 7 th cervical vertebra and medially to the fascia investing the structures passing from the thorax into the neck. It protects the underlying cervical pleura and resists the changes in intrathoracic pressure occurring during respiratory movements. Diaphragm The thorax opens into the abdomen by a wide opening. It is bounded by the xiphisternal joint, the costal margin, and the body of the twelfth thoracic vertebra. It is closed by a musculoaponeurotic septum, the diaphragm, which is pierced by the structures that pass between the thorax and the abdomen. The diaphragm is the primary muscle of respiration. It is dome-shaped and consists of a peripheral muscular part, which arises from the margins of the thoracic opening, and a centrally placed tendon. The origin of the diaphragm can be divided into three parts: • A sternal part consisting of small right and left slips arising from the posterior surface of the xiphoid process. • A costal part consisting of six slips that arise from the deep surfaces of the lower six ribs and their costal cartilages. • A vertebral part arising by means of vertical columns or crura and from the arcuate ligaments. The right crus arises from the sides of the bodies of the first three lumbar vertebrae and the intervertebral discs; the left crus arises from the sides of the bodies of the first two lumbar vertebrae and the intervertebral disc. Lateral to the crura the diaphragm arises from the medial and lateral arcuate ligaments. The medial ligament is the thickened upper margin of the fascia covering the anterior surface of the psoas muscle, and the lateral ligament is the thickened upper margin of the fascia covering the anterior surface of the quadratus lumborum muscle. The medial arcuate ligament extends from the side of the body of the second lumbar vertebra to the tip of the transverse process of the first lumbar vertebra. The lateral arcuate ligament extends from the tip of the transverse process of the first lumbar vertebra to the lower border of the twelfth rib. The fibrous medial borders of the two crura are connected by a median arcuate ligament, which crosses over the anterior surface of the aorta. The diaphragm is inserted into a central tendon, which is shaped like three leaves. The superior surface of the tendon is partially fused with the inferior surface of the fibrous pericardium. Some of the muscle fibers of the right crus pass up to the left and surround the esophageal orifice in a slinglike loop. These fibers appear to act as a sphincter and possibly assist in the prevention of regurgitation of the stomach contents into the thoracic part of the esophagus. Shape of the Diaphragm As seen from in front, the diaphragm curves up into right and left domes. The right dome reaches as high as the upper border of the 5th rib, and the left dome may reach the lower border of the 5th rib. The right dome lies at a higher level probably because of the large size of the right lobe of the liver. The central tendon lies at the level of the xiphisternal joint. The domes support the right and left lungs, whereas the central tendon supports the heart. The levels of the diaphragm vary with the phase of respiration, the posture, and the degree of distention of the abdominal viscera. The diaphragm is lower when a person is sitting or standing; it is higher in the supine position and after a large meal. When seen from the side, the diaphragm has the appearance of an inverted “J”, the long limb extending up from the vertebral column and the short limb extending forward to the xiphoid process. Openings in the Diaphragm The diaphragm has three main openings: 1. The aortic opening, which lies anterior to the body of the 12th thoracic vertebra between the crura. It transmits the aorta, the thoracic duct, and the azygos vein. 2. The esophageal opening, which lies at the level of the 10th thoracic vertebra in a sling of muscle fibers derived from the right crus. It transmits the esophagus, the right and left vagus nerves, the esophageal branches of the left gastric vessels, and the lymphatics from the lower one-third of the esophagus. 3. The caval opening, which lies at the level of the eighth thoracic vertebra in the central tendon. It transmits the inferior vena cava and terminal branches of the right phrenic nerve. Other Openings The greater, lesser, and lowest splanchnic nerves pierce the crura; the sympathetic trunks pass posterior to the medial arcuate ligament on each side; and the superior epigastric vessels pass between the sternal and costal origins of the diaphragm on each side. The left phrenic nerve pierces the left dome to supply the peritoneum on its undersurface, and the neurovascular bundles of the seventh to the eleventh intercostal spaces pass into the anterior abdominal wall between the muscular slips of the costal origin of the diaphragm. Action of the Diaphragm On contraction, the diaphragm pulls down its central tendon and increases the vertical diameter of the thorax. Nerve Supply of the Diaphragm The motor nerve supply on each side is from the phrenic nerve (C3-5) only. The sensory nerve supply to the parietal pleura and peritoneum covering the central surfaces of the diaphragm is from the phrenic nerve. The sensory supply to the periphery of the diaphragm is from the lower six intercostal nerves. Functions of the Diaphragm 1. Muscle of inspiration: The diaphragm is the most important muscle used in inspiration. 2. Muscle of abdominal straining: Its contraction aids that of the muscles of the anterior abdominal wall in raising the intra-abdominal pressure to evacuate the pelvic contents (micturition, defecation, parturition). This mechanism is further aided by the person taking a deep breath and closing the glottis of the larynx. The diaphragm is unable to rise because of the air trapped in the respiratory tract. Now and again, air is allowed to escape, producing a grunting sound. 3. Weight-lifting muscle: By taking a deep breath and fixing the diaphragm as described above, it is possible to raise the intra-abdominal pressure to such an extent that it will help support the vertebral column and prevent flexion. This greatly assists the postvertebral muscles in the lifting of heavy weights. Needless to say, it is important to have adequate sphincteric control of the bladder and anal canal under these circumstances. 4. Thoracoabdominal pump: The descent of the diaphragm decreases the intrathoracic pressure and at the same time increases the intra-abdominal pressure. This pressure change compresses the blood in the inferior vena cava and forces it upward into the right atrium of the heart. Lymph within the abdominal lymph vessels is also compressed, and its passage upward within the thoracic duct is aided by the negative intrathoracic pressure. The presence of valves within the thoracic duct prevents backflow. The lymph drainage of the skin of the anterior chest wall passes to the anterior axillary lymph nodes; that from the posterior chest wall passes to the posterior axillary nodes. The lymphatic drainage of the intercostal spaces passes forward to the internal thoracic nodes, situated along the internal thoracic artery, and posteriorly to the posterior intercostal nodes and the paraaortic nodes in the posterior mediastinum. The lymphatic drainage of the breast is described above. The Operations Chest wound Three common pathologic processes may occur in the pleural cavity. If air is introduced into the pleural cavity, a pneumothorax develops and the lung collapses because of its own elastic recoil. The pleural space fills with air, which may further compress the lung. Most patients with a collapsed lung are unlikely to have respiratory impairment. Under certain conditions, air may enter the pleural cavity at such a rate that it shifts and pushes the mediastinum to the opposite side of the chest. This is called tension pneumothorax and is potentially lethal, requiring urgent treatment by insertion of an intercostal tube to remove the air. The commonest causes of pneumothorax are rib fractures and positive pressure ventilation lung damage. The pleural cavity may fill with fluid (a pleural effusion) and this can be associated with many diseases (e.g. lung infection, cancer, abdominal sepsis). It is important to aspirate fluid from these patients to relieve any respiratory impairment and to carry out laboratory tests on the fluid to determine its nature. Severe chest trauma can lead to development of hemopneumothorax. A tube must be inserted to remove the blood and air that has entered the pleural space and prevent respiratory impairment. This man needs treatment to drain either the air or fluid or both. The pleural space can be accessed by passing a needle between the ribs into the pleural cavity. In a normal healthy adult, the pleural space is virtually nonexistent; therefore, any attempt to introduce a needle into this space is unlikely to succeed and the procedure may damage the underlying lung. Before any form of chest tube is inserted, the rib must be well anesthetized by infiltration because its periosteum is extremely sensitive. The intercostal drain should pass directly on top of the rib. Insertion adjacent to the lower part of the rib may damage the artery, vein, and nerve, which lie within the neurovascular bundle. Appropriate sites for insertion of a chest drain are: - in the midaxillary line in the fifth intercostal interspace; - in the midclavicular line in the second intercostal interspace. These positions are determined by palpating the sternal angle, which is the point of articulation of rib II. Counting inferiorly will determine the rib number and simple observation will determine the points of the midaxillary and the midclavicular line. Insertion of any tube or needle below the level of rib V runs an appreciable risk of crossing the pleural recesses and placing the needle or the drain into either the liver or the spleen, depending upon which side the needle is inserted. The operations on mastitis The antemammar (hypodermic) and intramammar (interlobular) mastitis are dissected by radial cut without areola injuring; the retromammar mastitis are drained with the help of arched cut under breast. Mastectomy (excision of a breast) is not as common an operation as it once was. In simple modified radical mastectomy the breast is removed down to the deep fascia. Radical mastectomy is a more extensive surgical operation during which the breast, pectoral muscles, fat, fascia, and all lymph nodes in the axilla and pectoral region are excised. Radical mastectomies are uncommon now. Often only the tumor and surrounding tissues are removed. This surgical operation is called a lumpectomy or a wide local excision. During mastectomy care is taken to preserve the long thoracic nerve. Cutting this nerve results in paralysis of the serratus anterior muscle and a winged scapula. Modified Radical Mastectomy 1 The patient is placed supine on the operating table with the arm extended on an armboard or extension table. The arm is prepped and draped into the operative field, allowing manipulation during surgery. At closure, the ability to adduct the arm may aid the approximation of the skin edges. The tumor is sampled by core-needle or excisional biopsy, or by incisional biopsy if the tumor mass is large. Upon confirmation of malignant histology, a transverse elliptical incision is made because it affords cosmetic advantages and is preferred in the case of subsequent breast reconstruction. The skin incision is made 5 cm above and below the tumor's edges. The nipple and areola are excised. 2 The skin incision is made just deep enough to allow the breast tissue to pout through the wound. Adair clamps are placed on the superior skin edge; the assistant provides steady traction with these clamps while the surgeon applies counterpressure on the breast tissue. Using sharp and blunt dissection techniques, the superior flap is developed from the sternal border medially, to the anterior axillary line laterally, and to the clavicle superiorly. When the dissection is carried out in the appropriate plane, the breast tissue separates easily and relatively bloodlessly from the skin and subcutaneous tissue. No attempt is made to create thin skin flaps. Similarly, the Adair clamps are placed on the inferior skin edge and the lower flap is developed beyond the inferior mammary fold until the rectus and oblique muscles are visible. 3 The superficial pectoral fascia is the deep margin of resection. The pectoralis fascia is in- cised parallel to the sternum. It is grasped with small clamps and sharply dissected from the pectoralis major muscle underlying it. The perforating branches of the internal mammary artery are ligated carefully, because they tend to retract into the substance of the pectoralis muscle. As the dissection proceeds laterally, the fascia is incised parallel to the clavicle and at the inferior margin of the pectoralis major muscle. 4 The pectoral fascia is incised along the lateral border of the pectoralis major, allowing cephalad retraction of this muscle, which exposes the pectoralis minor muscle. The fat between the pectoralis major and minor muscles is dissected bluntly, carrying the specimen laterally toward the remainder of the axillary contents. The nerve innervating the lateral portion of the pectoralis major muscle is present in this plane; an attempt should be made to preserve it. 5 The axillary fascia is then incised at the lateral border of the pectoralis minor muscle. Retraction of this muscle medially exposes the remainder of the axillary contents. The most medial few centimeters of the axillary contents, where the axillary vein enters the chest wall (Level 111 nodes), cannot easily be cleared without the division of the pectoralis minor muscle. However, our past commitment to the complete exenteration of the axilla has not been shown to be as important as the removal of a significant sample of the Level 1 and II nodes. Therefore, in recent years, we have not divided the insertion of the pectoralis minor muscle. 6 The fascia investing the axillary vein is incised. Lymph node bearing tissue along the inferior margin of the axillary vein is dissected inferiorly. Medially, the long thoracic (Bell's) nerve is identified and preserved. The lymph node bearing tissue surrounding it is dissected and included in the specimen. Because of the risk of brachial plexus injury and subsequent lymphedema of the arm, the dissection should not be carried above the axillary vein. 7 While we used to take all of the venous branches and nerves entering the axilla beneath the axillary vein, preserving only the long thoracic and thoracodorsal nerves, we no longer consider this skeletization an important feature of the axillary dissection. The lateral margin of the dissection is the anteromedial border of the latissimus dorsi muscle. 8 The cleared axilla shows the axillary vein superiorly, the pectoral, intercostal, and serratus muscles against the chest wall, and the latissimus dorsi muscle deep and laterally. 9 Meticulous hemostasis is achieved. Two closed suction catheter drains, one under the flaps and one in the axilla, are placed through separate incisions. These drains evacuate any residual blood and lymph from the wound. The wound is closed with interrupted absorbable sutures in the subcutaneous tissues and interrupted #0000 nylon sutures in the skin. The wound must be closed without tension. Should tension be present, the flaps may be further mobilized by freeing the superior flap above the clavicle and dissecting the inferior flap onto the anterior abdominal wall. Once the wound is closed/ a pressure bandage is applied to the chest wall. Thoracostomy This procedure is necessary in patients with tension pneumothorax (air in the pleural cavity under pressure) or to drain fluid (blood or pus) away from the pleural cavity to allow the lung to reexpand. It may also be necessary to withdraw a sample of pleural fluid for microbiologic examination. Anterior Approach With the patient in the supine position, the sternal angle is identified, then the second costal cartilage and the second rib and the second intercostal space are found in the midclavicular line. Lateral Approach With the patient lying on the lateral side, the second intercostal space is identified as above but the anterior axillary line is used. The skin is prepared in the usual way, and a local anesthetic is introduced along the course of the needle above the upper border of the third rib. The thoracostomy needle will pierce the following structures as it passes through the chest wall: (a) skin, (b) superficial fascia (in the anterior approach the pectoral muscles are then penetrated), (c) serratus anterior muscle, (d) external intercostal muscle, (e) internal intercostal muscle, (f) innermost intercostal muscle, (g) endothoracic fascia, and (h) parietal pleura. The needle should be kept close to the upper border of the third rib to avoid injuring the intercostal vessels and nerve in the subcostal groove. Tube Thoracostomy The preferred insertion site for a tube thoracostomy is the 4th or 5th intercostal space at the anterior axillary line. The tube is introduced through a small incision. The neurovascular bundle changes its relationship to the ribs as it passes forward in the intercostal space. In the most posterior part of the space the bundle lies in the middle of the intercostal space. As the bundle passes forward to the rib angle it becomes closely related to the lower border of the rib above and maintains that position as it courses forward. The introduction of a thoracostomy tube or needle through the lower intercostal spaces is possible provided that the presence of the domes of the diaphragm is remembered as they curve upward into the rib cage as far as the fifth rib (higher on the right). Avoid damaging the diaphragm and entering the peritoneal cavity and injuring the liver, spleen, or stomach. Thoracotomy In patients with penetrating chest wounds with uncontrolled intrathoracic hemorrhage, thoracotomy may be a life-saving procedure. After preparing the skin in the usual way, an incision is made over the fourth or fifth intercostal space, extending from the lateral margin of the sternum to the anterior axillary line. Whether a right or left incision will be made will depend on the site of the injury. For access to the heart and aorta, the chest should be entered from the left side. The following tissues will be incised: (a) skin, (b) subcutaneous tissue, (c) serratus anterior and pectoral muscles, (d) external intercostal muscle and anterior intercostal membrane, (e) internal intercostal muscle, (f) innermost intercostal muscle, (g) endothoracic fascia, and (h) parietal pleura. Avoid the internal thoracic artery, which runs vertically downward behind the costal cartilages about a fingers breadth lateral to the margin of the sternum, and the intercostal vessels and nerve, which extend forward in the subcostal groove in the upper part of the intercostal space. Rib excision Rib excision is commonly performed by thoracic surgeons wishing to gain entrance to the thoracic cavity. A longitudinal incision is made through the periosteum on the outer surface of the rib and a segment of the rib is removed. A second longitudinal incision is then made through the bed of the rib, which is the inner covering of periosteum. Following the operation, the rib regenerates from the osteogenetic layer of the periosteum. Intercostal nerve block Area of Anesthesia The skin and the parietal pleura covering the outer and inner surfaces of each intercostal space, respectively; the seventh to eleventh intercostal nerves supply the skin and the parietal peritoneum covering the outer and inner surfaces of the abdominal wall, respectively; therefore, these areas will also be anesthetized. In addition, the periosteum of the adjacent ribs is anesthetized. Indications Repair of lacerations of the thoracic and abdominal walls; relief of pain in rib fractures and to allow pain-free respiratory movements. Procedure To produce analgesia of the anterior and lateral thoracic and abdominal walls, the intercostal nerve should be blocked before the lateral cutaneous branch arises at the midaxillary line. The ribs may be identified by counting down from the second (opposite sternal angle) or up from the twelfth. The needle is directed toward the rib near the lower border, and the tip comes to rest near the subcostal groove, where the local anesthetic is infiltrated around the nerve. Remember that the order of structures lying in the neurovascular bundle from above downward is intercostal vein, artery, and nerve and that these structures are situated between the posterior intercostal membrane of the internal intercostal muscle and the parietal pleura. Furthermore, laterally the nerve lies between the internal intercostal muscle and the innermost intercostal muscle. 5.2. Theoretical questions to studies: 1. 2. 3. 4. 5. 6. 7. 8. 9. The topographical anatomy of the pectoral wall. The regions of the thoracic cage. The layer-by-layer structure of the thoracic wall. Topography of the mammary gland. The blood and nerve supply of the thoracic cage. The topography of diaphragm. The main stages of the tracheostomy. The kinds of thoracotomy. The operations on the mammary gland. 5.3. Materials for self-control: DIRECTIONS: Each question below contains four or five suggested responses. Select the one best response to each question. 1. Knowledge of the lymphatic drainage of the breast is clinically important because of the high incidence of breast tumors. The major pathway of lymphatic drainage from the mammary gland is along lymphatic channels that parallel A subcutaneous venous networks to the contralateral breast and to the abdominal wall B tributaries of the axillary vessels to the axillary nodes C tributaries of the intercostal vessels to the parasternal nodes and posterior mediastinal nodes D tributaries of the internal thoracic (mammary) vessels to the parasternal (internal thoracic) nodes E tributaries of the thoracoacromial vessels to the apical (subclavicular) nodes 2. A patient who has undergone a radical mastectomy with extensive axillary dissection suffers winging of the scapula when the flexed arm is pressed against a fixed object. This indicates injury to which of the following nerves? A Axillary B Long thoracic C Lower subscapular D Supraclavicular E Toracodorsal 3. The second rib or its costal cartilage articulates with all the following structures EXCEPT the A body of the sternum B manubrium C second vertebral body D third vertebral body E transverse process of the second vertebra 4. The “bucket-handlle” movement of the ribs during relaxed expiration involves all the following EXCEPT A decrease of the transverse thoracic diameter B contraction of the internal intercostal muscles C inward rotation of the ribs D movement at the costovertebral joints E untwisting of costal cartilages 5. The “pump-handle” movement (elevation of the sternum) during inspiration involves all the following EXCEPT A increase in the anteroposterior chest diameter B increase in the superior-inferior chest diameter C movement at the costovertebral joints D movement at the sternocostal joints E movement at the sternomanubrial joint 6. Contraction of which of the following muscles contributes to forced inspiration? A External oblique B Internal oblique C Rectus abdominis D Transverse abdomimis E None of the above 7. Gravity assists the inspiratory effort of the diaphragm when a person is A lying prone B lying on the left side C lying on the right side D lying supine sitting 8. All the following correctly describe the phrenic nerve EXCEPT A it is a component of the somatic nervous system B it does not innervate the entire diaphragm C it innervates the diaphragmatic peritoneum D it originates from spinal nerves C3-C5 E it passes through the aortic hiatus 9. All the following statements correctly pertain to the left costodiaphragmatic recess EXCEPT A it accommodates lung tissue during inspiration B it extends below the twelfth rib posteriorly C it is formed by the apposition of diaphragmatic and mediastinal pleura D it is maximal upon forced expiration E it is the most dependent (lowest) part of the pleural cavity when a person is sitting Literature 1. Snell R.S. Clinical Anatomy for medical students. – Lippincott Williams & Wilkins, 2000. – 898 p. 2. Skandalakis J.E., Skandalakis P.N., Skandalakis L.J. Surgical Anatomy and Technique. – Springer, 1995. – 674 p. 3. Netter F.H. Atlas of human anatomy. – Ciba-Geigy Co., 1994. – 514 p. 4. Ellis H. Clinical Anatomy Arevision and applied anatomy for clinical students. – Blackwell publishing, 2006. – 439 p.