Tissue Viability Guidance for Reporting and Safeguarding Version 6
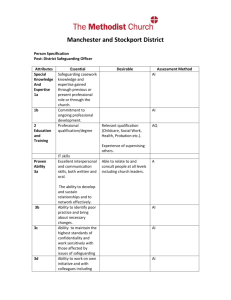
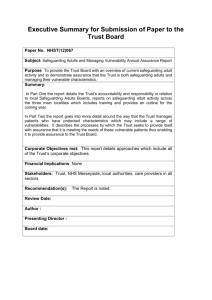
advertisement

Tissue Viability Guidance for Reporting and Safeguarding Version 6.1 FINAL 16th June 2011 June 2011 Page | 1 Acknowledgements West Midlands Strategic Health Authority wishes to thank the following organisations/groups for their assistance in compiling this guidance: NHS Staffordshire NHS Stoke on Trent West Midlands Regional Tissue Viability Advisory Group (TAGS) Heart of Birmingham NHS FT Tissue Viability Team Bradford PCT Solihull Care Trust Staffordshire and Stoke-on-Trent Adult Safeguarding Partnership University Hospital Coventry and Warwick Tissue Viability Team West Midlands Regional ‘Your Skin Matters’ High Impact Action Working Group Further information For further information please contact: Contact: Manjeet Garcha. Interim Head of Patient Safety, NHS West Midlands Michelle Mello. Modernising Nursing Careers Lead, NHS West Midlands Telephone: 0121 695 2561/0121 695 2300 Email: manjeetk.garcha@westmidlands.nhs.uk michelle.mello@westmidlands.nhs.uk Page | 2 Contents 1.0 Introduction - Purpose 2.0 Background Page Number 4 4 3.0 Definitions of a Pressure Ulcer 5-7 Definitions of Avoidable and Unavoidable Pressure Ulcers 4.0 Reporting Guidance - Pressure Ulcer Reporting Chart - Definition of timescales for Hospital and Primary Care Acquired Pressure Ulcers - Assurance 5.0 Pressure Ulcer Reporting Flowchart 6.0 Safeguarding 7 8-9 10 11-14 -Pressure Ulcer Safeguarding Triggers Pathway 1 15 -Pressure Ulcer Safeguarding Triggers Pathway 2 16 -Safeguarding Referral Pathway for Pressure Ulcers 17 7.0 References Appendix 1 Page | 3 18 Appendices Page Number NHS West Midlands High Impact Action Your Skin Matters Recommended Route Cause Analysis (RCA) Investigation Report (Template) 19-34 Serious Incident Reporting Introduction Experience of reporting and managing pressure ulcer related serious incidents (SI’s) has indicated the need for additional guidance, support and clarification of the criteria to be used when evaluating pressure ulcer related serious incidents. This guidance has been designed to offer further guidance for safeguarding, reporting and investigating tissue viability related pressure ulcers and should be used in conjunction with the previously published National Framework for Reporting Serious Incidents (2010) and NHS West Midlands Serious Incident Reporting Policy (2010). 1.0 Purpose The purpose of this guidance is to: a) Ensure management of SI’s related to pressure ulcers conform to the processes and procedures set out for managing all SI’s b) There is a consistent approach to evaluating Pressure Ulcers related SI’s c) Early reports of pressure ulcer reporting SI’s are sufficient to decide on appropriate escalation, notification and communication to interested parties including Safeguarding d) Appropriate action is taken to prevent damage to patients, staff and the reputation of the NHS e) All aspects of the SI are fully explored and ‘lessons learned’ are identified and communicated; and f) Appropriate corrective action is taken to prevent/reduce the number of incidents occurring. 2.0 Background In November 2009 Dame Christine Beasley, Chief Nursing Officer for England, launched the High Impact Action for Nursing and Midwifery’. This document identified 8 key examples of high quality and cost effective care that potentially would make a transformational difference in the NHS. The reduction target for reducing pressure ulcers is now a major work stream in Safety Express, CQUINs including CNO’s High Impact Actions. The target reduction was set at 80% for hospital acquired pressure ulcers and 30% for community acquired by 2014 as identified in the Nurse Sensitive Outcome Indicators (2010). Pressure ulcers of grade 3 and 4 are to be reported as a serious incident on the Strategic Executive Information System (STEIS) and to clarify the process; the following reporting guidance has been developed. Page | 4 3.0 3.1 Definition of a Pressure Ulcer A localized area of damaged tissue as a result of pressure in combination with other variables of which there are 4 grades; these are described in detail on pages 5 and 6. Grade 1: Non-blanchable erythema Description: Intact skin with non-blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its colour may differ from the surrounding area. The area may be painful, firm, soft, warmer or cooler as compared to adjacent tissue. Grade 1 may be difficult to detect in individuals with dark skin tones. Progression of pressure ulcer Grade 1 Non-blanchable erythema (redness) of intact skin. Discolouration of skin, warmth, oedema, induration or hardness may also be used as indicators, particularly on individuals with darker skin Grade 2: Partial thickness Description: Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled or serosanginous filled blister. Presents as a shiny or dry shallow ulcer without slough or bruising (indicating deep tissue injury). This grade should not be used to describe skin tears, tape burns, incontinence associated dermatitis, maceration or excoriation. Page | 5 Progression of pressure ulcer Grade 2 Partial thickness skin loss involving epidermis, dermis or both The ulcer is superficial and presents clinically as an abrasion or blister Grade 3: Full thickness skin loss Description: Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle is not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling. The depth of a grade 3 pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have (adipose) subcutaneous tissue and grade 3 ulcers can be shallow. In contrast, areas of significant adiposity can develop extremely deep grade 3 pressure ulcers. Bone or tendon is not visible or directly palpable. Progression of pressure ulcer Grade 3 Full thickness skin loss involving damage to or necrosis of subcutaneous tissue that may extend down to, but not through the underlying fascia. Grade 4: Full thickness tissue loss Description: Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present. Often includes undermining and tunneling. The depth of a grade 4 pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have (adipose) subcutaneous tissue and these ulcers can be shallow. Grade 4 ulcers can extend into muscle and/or supporting structures (e.g. fascia, tendon or joint capsule) making Page | 6 Osteomyelitis or osteoitis likely to occur. Exposed bone/muscle is visible or directly palpable EPUAP (2009). Progression of pressure ulcer Grade 4 Extensive destruction, tissue necrosis, or damage to muscle, bone, or supporting structures with or without full thickness skin loss. pressure ulcers 3.2 Defining avoidable and unavoidable In the absence of definitions in the UK, the Department of Health has used two definitions from The Wound, Ostomy and Continence Nurses Society of the US and created one modified definition for use in the UK: Avoidable Pressure Ulcer: “Avoidable means that the person receiving care developed a pressure ulcer and the provider of care did not do one of the following; evaluate the person’s clinical condition and pressure ulcer risk factors; plan and implement interventions that are consistent with the persons need and goals, and recognised standards of practice; monitor and evaluate the impact of the interventions; or revise the interventions as appropriate.” Unavoidable Pressure Ulcer: “Unavoidable” means that the person receiving care developed a pressure ulcer even though the provider of the care had evaluated the person’s clinical condition and pressure ulcer risk factors; planned and implemented interventions that are consistent with the persons needs and goals; and recognised standards of practice; monitored and evaluated the impact of the interventions; and revised the approaches as appropriate; or the individual person refused to adhere to prevention strategies in spite of education of the consequences of nonadherence”. Guidance: In determining whether the pressure ulcer is avoidable; commissioners, regulators or others could request to see evidence demonstrating the actions outlined in the “avoidable” definition are demonstrated. Page | 7 4.0 Reporting Guidance The guidance chart for reporting pressure ulcers can be found in figure 1 and a flowchart capturing the timescales for reporting and investigating can be found in figure 2 Figure 1 STAGE Reporting organisation Pressure Ulcer Serious Incident Reporting Chart ACTION Hospital acquired grade 3 and 4 pressure ulcers should be reported on STEIS by the acute Trust. Primary care acquired pressure ulcers should be reported on STEIS by the community provider organisation and performance managed by commissioners via the Care Quality Review process. Primary care acquired pressure ulcers in commissioned independent providers should be reported on STEIS by the commissioning organisation, this includes care commissioned in nursing or residential care homes. Incident found in patients own homes where there is no input from any health services, these should be reported to the commissioner and internal analysis undertaken of any significant trends. These do not need to be reported on STEIS. Safeguarding All Grade 3&4 Pressure Ulcer Incidents should first be assessed for evidence of neglect or abuse and if this is substantiated then reported to the trust safeguarding lead for further investigation. (The person (s) undertaking the initial assessment must have undertake appropriate Safeguarding training). Should signs of neglect be identified using locally agreed or regional tissue viability criteria, the Trust must report this to the Local Safeguarding Board and the Care Quality Commission (CQC). Reporting Timeframe Root Cause Analysis Page | 8 All incidents should be reported on STEIS within 2 working days in line with the SHA’s policy for the ‘Reporting & Management of Serious Incidents’ 2010. The Root Cause Analysis (RCA) should be completed within 21 working days following notification of the incident. This is in line with current local agreed CQUINs and the SHA High Impact Action Group for ‘Your Skin Matters’. STEIS Closure On completion of the RCA, the lessons learnt and actions planned and completed must all be summarised on STEIS; the Trust can then request closure from the SHA, including any actions arising from referral to the Local Safeguarding Adults Board. The commissioning PCT should also assure compliance with action plans via the normal Quality Review Group Meetings. Page | 9 4.1 Definition of timescales for Hospital and Primary Care Acquired Pressure Ulcers For patients admitted or transferred to a healthcare setting without any obvious signs or symptoms of skin damage, the development of a stage 3 or 4 pressure ulcer within 72 hours of admission to that institution is likely to be related to pre-existing damage incurred prior to admission or transfer of care. For any pressure area damage arising after 72 hours thereafter, the most likely cause will be related to care within the healthcare setting the patient is in, this must be regarded as a new event. All professionals must ensure that pressure ulcer details are stated in any clinical correspondence e.g. discharge or admission letter, should clearly identify relevant information in respect to the initial source of occurrence 4.2 Assurance It is the responsibility of the Commissioner to ensure that all grade 3 and 4 pressure ulcers are reported on STEIS and investigated. In addition, the trust must ensure that the incidence and progress is analysed and reported internally through the organisation’s governance reporting framework and ultimately to the Trust Board. Page | 10 5.0 Pressure Ulcer Reporting Flowchart Figure 2: Flow Chart showing timescales for reporting and investigating Incident Pre 72 hrs Community Post 72 hrs Hospital Report on STEIS and refer to trust Safe Guarding Lead within 2 working days (Assess for suspected neglect) Yes No Report to Local Safe Guarding Board And CQC Investigate and complete RCA with 21 working days Page | 11 6.0 Safeguarding 6.1 Introduction This guidance has been written to provide a framework for decision making in relation to establishing the need for raising a safeguarding referral in the event of tissue damage occurring. 6.2 What is safeguarding? Safeguarding is defined within the Staffordshire and Stoke on Trent Inter-agency adult protection procedures (2010) as “All work which enables an adult who is or may be eligible for community care services to retain independence, wellbeing and choice and to access their human right to live a life that is free from abuse and neglect” This includes people in need of health care services. 6.3 Who is a vulnerable adult? Vulnerable adult is a term used to describe a person who is aged 18 or over, who is, or may be in need of community care services, by reason of mental or other disability, age or illness and who is, or may be unable to take care of him or herself or take steps to protect him or herself from significant harm or exploitation. (DOH, 2000) 6.4 What is Neglect or Acts of Omission? The withholding, either deliberately or unintentionally, of help or support necessary to carry out daily living tasks. This includes ignoring medical and physical care needs or failing to provide access to health, social or educational support, the withholding of medication, nutrition and heating. Pressure ulcers are cited twice in Staffordshire and Stoke-on-Trent Policy Inter Agency Adult Protection Procedures (2010); 1. Physical abuse: section 6 Under possible indicators of physical Abuse: “Ulcers, pressure sores and left in wet clothing” 2. Neglect and acts of omission: section 6 Under possible indicators of neglect “Inadequate physical care both of the person and the environment” Page | 12 6.5 What is a pressure ulcer? A localized area of damaged tissue as a result of pressure in combination with other variables of which there are 4 grades as described in section 2.1. Notification Required 6.6 Primary/Secondary Care A clinical incident form should be completed for all grade 2, 3 and 4 pressure ulcers in line with the National Institute for Health and Clinical Excellence (NICE, 2005) and all grade 3 & 4 pressure ulcers must be reported as an SI as per the SHA SI Reporting Policy 2010. 6.7 The Health & Social Care Act Outcome 20 (Notification of other incidents) in the CQC Guidance about Compliance - Essential Standards of Quality and Safety states: The registered person (this now includes NHS, Adult Social Care & Independent Health) must notify CQC of: "The development after admission of a pressure sore of grade 3 or above that develops after the person has started to use the service (European Pressure Ulcer Advisory Panel Grading)." Outcome 20 relates to Regulation 18 of the Care Quality Commission (registration) Regulations 2009 6.8 Safeguarding adult referral in relation to Tissue viability Potential indicators for a safeguarding referral: Development of a Grade 3/4 EPUAP pressure ulcer Rapid onset/deterioration of tissue damage Unexplained weight loss/dehydration Unexplained bruising or injuries of any sort Poor physical condition i.e. failure to attend to physical needs such as toileting, dressing and washing Poor continence management Burns Leaving a resident unattended for an extended length of time This is not an exhaustive list and there may be other areas of tissue viability that would trigger a safeguarding referral. (See local Safeguarding Adults Policy). Page | 13 6.9 Reasonable measures that should be taken to prevent tissue damage: Implementation of, or increase in repositioning regime with clear documentation Evidence of a 24 hour approach to repositioning at regular intervals appropriate to each individual Regular skin inspection and clear documentation to include continence management and protection of skin with barrier creams and/or emollients Appropriate plan of care which is updated accordingly and addresses the cause of the pressure damage. Care Homes: Monthly risk assessment acknowledging changes in need Primary care: Three monthly risk assessment or as clinical condition changes acknowledging changes in need Secondary care: Risk assessment within 6 hours of admission and daily risk assessment thereafter Appropriate equipment with supporting documentation Nutritional assessment and involvement of necessary professionals Wound assessment and evaluation to include photographs and regular wound measurements Appropriate dressing selection with a treatment chart Pain assessment and liaison with the GP Documented evidence of offering care to non concordant residents Absence of any of the above may indicate a safeguarding referral but would be considered on an individual basis. 6.10 Factors that may influence the safeguarding referral decision In some cases pressure ulcer development may be inevitable for example; Palliative diagnosis End of life care Non concordance of patient with recommended treatment and interventions Multiple co-morbidities Change in condition History of development Capacity and mental health issues( these are patients that may not co-operate with treatment or prevention interventions due to capacity or mental health problems i.e. taking off wound care dressings or declining to be repositioned) This is not an exhaustive list, medical conditions along with other professionals opinions needs to be taken into account. Reasonable measures still need to be carried out regardless of diagnosis. Failure to do so may still result in a safeguarding referral Page | 14 6.11 Consideration of Capacity If a person lacks capacity to make a decision in relation to the care or treatment of the pressure ulcer a decision must be taken to act in the best interests of the patient utilizing the Mental Capacity Act 2005. The two diagrams (pages 13 and page 14) indicate the pathway for individuals who are receiving professional support i.e. in a care home, hospital, from a domiciliary care provider, a nursing agency and those individuals who are not receiving any professional care and are looked after by an unpaid carer, family or friend. Page | 15 Pressure Ulcers – Safeguarding Triggers- Pathway 1 To determine if the identification of a pressure ulcer on an individual receiving professional support (in a care home, hospital or from domiciliary care of nursing agency care) should result in a safeguarding referral the following triggers should be considered. IF IN DOUBT senior manager Initiate Safeguarding Adults Procedures Discuss with Record decision and reasons for decision. Possibly NOT Safeguarding at this stage Possibly Safeguarding Definitely Safeguarding 1. What is the severity (grade) of the pressure ulcer? Grade 2 pressure ulcer or below – care plan required Several grade 2 pressure ulcers/ grade 3 to 4 pressure ulcers- consider question 2 Grade 4 and other issues of significant concern 2. Does the individual have mental capacity and have they been compliant with treatment? Has capacity and declined treatment Does not have capacity or capacity has not been assessedcontinue to question 3 Assessed as NOT having capacity and treatment NOT provided Has a assessment completed? Capacity assessment recorded. capacity been is 3. Full assessment completed and care plan developed in a timely manner and care plan implemented? Documentation and equipment available to demonstrate full assessment completed, care plan developed and implemented. Documentation and equipment NOT fully available to demonstrate full assessment completed, care plan developed or care plan implemented BUT general care regime (e.g. nutrition, hydration) not of concerncontinue to question 4 Little or no documentation available to demonstrate a full assessment has been completed, or care plan implemented AND general care regime (e.g. nutrition, hydration) is of concern. 4. This incident is part of a trend or patternthere have been other similar incidents with this individual or others. Evidence suggests this is an isolated incident. There have been similar incidents Evidence demonstrates this is a pattern or trend. NOT SAFEGUARDING If 2 or more of the above apply - SAFEGUARDING other SAFEGUARDING Always clearly record decision and reasons for decision. Page | 16 Pressure Ulcers – Safeguarding Triggers- Pathway 2 To determine if the identification of a pressure ulcer on an individual with No professional support (i.e. the only support available is from an unpaid carer/ family member) should result in a safeguarding referral the following steps should be considered. IF IN DOUBT senior manger Initiate Safeguarding Adults Procedures Discuss with Record decision and reasons for decision. Possibly NOT Safeguarding at this stage Possibly Safeguarding Definitely Safeguarding 1. What is the severity (grade) of the pressure ulcer? Grade 2 pressure ulcer or below – care plan required Several grade 2 pressure ulcers/ grade 3 to 4 pressure ulcers- consider question 2 Grade 4 and other issues of significant concern 3. Does the individual have mental capacity and have they been compliant with treatment? Has capacity declined treatment Does not have capacity or capacity has not been assessedcontinue to question 3 Assessed as NOT having capacity and treatment NOT provided Has a assessment completed? capacity been Capacity assessment is recorded. 3. Unpaid carer raised concerns and sought support at an appropriate time. Evidence available to show concerns raised and support sought – e.g. from GP, DN, SW. Evidence NOT CLEAR that concerns were raised or support sought in a timely manner. No support sought 4. Full assessment completed and care plan developed in a timely manner and care plan implemented? Evidence available to show unpaid carer cooperated with assessment and has implemented care plan Evidence of partial cooperation or implementation of care plan- some aspects may have been declined e.g. certain equipment. NO cooperation and refusal to implement care plan and or purposeful neglect. 5. This incident is part of a trend or pattern – there have been other similar incidents or other areas of concern Evidence suggests that this is an isolated incident There have been other similar incidents or other areas of concern Evidence demonstrates that this is a pattern or tend. NOT SAFEGUARDING If 2 or more of the above apply Safeguarding SAFEGUARDING and Always clearly record decision and reasons for decision. Page | 17 Safeguarding Referral Pathway for Pressure Ulcers Pressure ulcer: Primary or Secondary Care acquired Grade 1 or grade 2 EPUAP pressure ulcers Grade 3 or Grade 4 EPUAP pressure ulcers Refer to Tissue Viability Service Have reasonable steps been made to prevent/manage pressure ulceration? Have reasonable steps been made to prevent/manage pressure ulceration? See definitions See definitions Yes No Care Homes with nursing: Refer to the Tissue Viability Service if there are management concerns. Refer to Tissue Viability/ District Nurse to address quality issues with training and management advice. Complete Incident Form for Grade 2 pressure ulcers Consideration may be given to a safeguarding referral. Complete Incident Form for Grade 2 pressure ulcers Yes Refer to the Tissue Viability Service and/or Intermediate care /District Nurse for management. Complete Incident Form to Risk Management. Complete RCA. No Multi Agency Safeguarding referral for further investigation. Refer to the Tissue Viability Service and/or intermediate Care/ District Nursing for management. Complete Incident Form to Risk Management. Complete RCA. Multi Agency Document for Safeguarding vulnerable adults and Incident Form to be completed Any tissue damage, including bruising or injury needs to be considered on an individual basis. A referral should be made when deemed appropriate following the local Safeguarding Adults Multi Agency Guidelines. For advice contact the Safeguarding Adult lead for your area. Page | 18 7.0 References Department of Health, (2000) No Secrets http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_ 4008486 European Pressure Ulcer Advisory Panel (EPUAP), 2009. pressure ulcer prevention: A quick reference guide http://www.epuap.org/guidelines/Final_Quick_Prevention.pdf Health & Social Care Act, (2008), Department of Health http://www.dh.gov.uk/en/Publicationsandstatistics/Legislation/Actsandbills/HealthandSocialCareBill/in dex.htm High Impact Actions for Nursing and Midwifery. NHS Institute of Innovation and Improvement. 2010 http://www.institute.nhs.uk/building_capability/hia_supporting_info/staying_safe_preventing_falls.html Inter-Agency Adult Protection procedures Staffordshire and Stoke-on-Trent Safeguarding adults Partnership (2010) (Web link to follow) Mental Capacity Act Policy (2009) http://www.dh.gov.uk/en/Publicationsandstatistics/Lettersandcirculars/LocalAuthorityCirculars/DH_09 6868 National institute for Health and Clinical Excellence (NICE). The Prevention and Treatment of Pressure Ulcers. (2005) available from http://www.nice.org.uk/ NPSA, “National Framework for Reporting and Learning from Serious Incidents Requiring Investigation”, 2010 http://www.nrls.npsa.nhs.uk/report-a-patient-safety-incident/patient-safety-direct/serious-incidentreporting-and-learning-framework-sirl/ Nurse Sensitive Outcome Indicators DH 2010 http://www.dh.gov.uk/en/Aboutus/Chiefprofessionalofficers/Chiefnursingofficer/Energiseforexcellence /DH_120765 Reproduced with kind permission from Rebecca Martin- Heart of Birmingham PCT and Solihull Primary Care Foundation Trust. Serious Incidents Reporting Policy and Procedure. NHS West Midlands July 2010 Position Paper: Avoidable and Unavoidable Pressure Ulcers. Wound, Ostomy and Continence Nurses Society (WOCNS) March 2009. Accessed 24/08/2010 http://www.cawc.net/images/uploads/wcc/7-2stevenson.pdf Page | 19 Appendix 1 NHS West Midlands High Impact Action – Your Skin Matters Recommended Route Cause Analysis (RCA) Investigation Report Template Learning through Action To Reduce Primary Care Acquired Grade 3 and 4 Pressure Ulcers (This document is based on the National Patient Safety Agency “Learning through action to reduce infection" and adapted from the West Midlands Regional Tissue Viability Group) 20 Root Cause Analysis (RCA) Investigation Report Learning through action to reduce the number of Primary and Secondary care acquired Grade 3 and 4 Pressure Ulcers Root Cause Analysis Summary Patient name Hospital number/ NHS Number Date of birth Ethnic Origin TVN name and designation Date ulcer verified by TVN Grade and location Root causes identified from a Pressure analysis of contributory factors: Friction Shear Moisture Other Where was the ulcer acquired? Name of Acute Hospital Pts own home Nursing home Residential home Community Hospital Outcome Avoidable/Non Avoidable/unable to determine 21 What controls or barriers could be used to prevent the incident from happening again? Examples of good practice: Lessons learned: Recommendations for change / identified solutions: Clinical areas involved Date of Start of process Date of completion of RCA process Signature Using the above information: Has the pressure ulcer developed whilst under the care of (your organisation) Yes/ No. If yes, continue to complete full RCA documentation. If no, report findings to governance. (Datix report etc) 22 Patient Name Hospital/NHS Number Patient History (Timeline) Current admission date to ……………………………………………. Current ward/Nursing team Grade and location of pressure ulcer Grade: Previous history of pressure ulcers? Yes Location: No Grade and location Other clinical areas involved in admission/ Care Current Diagnosis Relevant medical conditions Status on admission What treatment is the patient receiving? Is the patient on the Care of the Dying Pathway? Date: 23 Previous Care episodes Yes/No /not known Details and Dates 1. Care in nursing / residential home 2. Own home – primary care e.g. District nurse, GP , podiatry 3. Community and social care ( home care, day care) Transfers Has the patient been Transferred between care Settings within the last 12 Months 1. Between wards in a hospital 2. Between Hospitals 3. Between care homes 4. Other Yes/ No If Yes : Dates and Details: Summary of care/status immediately prior to pressure ulcer development Date pressure ulcer found: Grade: Immediate action taken by ward / community staff 24 Did the pressure ulcer deteriorate/improve Was the patient referred to tissue viability? Grade Dates Date referred Date seen Tissue viability recommendations Summary of care/status immediately after pressure ulcer development 25 Assessment Was skin assessment completed within 6 hrs of admission or on admission to caseload? If no state when Condition: Was patient risk assessed within 6 hrs of admission or on admission to caseload? If no state when Score: Was patient risk score reassessed as per trust protocol? Risk Care plan? State dates: Always : Intermittently: Never: Was patient skin condition documented daily or at each visit? Status: Always : Intermittently: Never: Was patient skin assessment documented daily or at each visit? Always : Was a moving and handling assessment completed? Intermittently: Risk Rating; Never: Actions Implemented: Yes No 26 Was a nutritional assessment completed? Yes No High risk Medium Risk Low Risk Actions Implemented: Was a continence assessment completed? Yes No Actions Implemented: Was a Photograph, tracing, clinical incident form Regulation 18, adult safeguarding referral completed? Photograph/tracing Clinical Incident Form/ Req18 Adult Safeguarding Not required 27 Preventative Care Was preventative care planned? Yes /No Details Was preventative care delivered? Was appropriate equipment used? Was repositioning of patient evident? Patient Management Does the patient have any of the following? Yes/No Details Diabetes Skin condition Immobility Vascular disease Incontinence Sensory loss Previous pressure ulcer Malnutrition Organ Failure Anti embolic stockings Prescribed ? Measured? Inotropes (Noradrenaline, metaraminol,high dose adrenaline) History of smoking Epidural 28 Patient Information Is patient information available in clinical area? Yes/No Details Is the patient able to receive pressure ulcer prevention information? Did the patient’s relatives /carers receive information? Is the patient/carer aware of the pressure ulcer? Staff Education Are the staff aware of the pressure ulcer guidelines? Yes/No Are the staff aware of the pressure relieving equipment procedures? Yes/No Are the staff aware of how to access these guidelines? Yes/No Does the ward / team have a link nurse? Yes/No How many link nurse study days has the link nurse attended in the past 12 months? Yes/No What is the percentage of staff that have attended Pressure ulcer prevention training in the last 2 years? Yes/No Details 29 Have the working conditions (administrative, physical, environment, work load, time) had a bearing on the care given to the patient? Details: Have the organisation/strategic (organisational structure, priorities, safety culture, financial restrictions) has an impact on the care given to patient? Details: Local team/ward factors Individual (physical, psychological, social, personality) Details: Team and social (role congruence, leadership, support and cultural factors) Details: Communication (verbal, written, non-verbal) Details: 30 Please tick all that apply Section C – Key issues identified Nutrition Moving and handling Continence issues Lack of skin/risk assessment Preventative care not implemented Issues with resources 31 Please tick all that apply Overall condition of the patient Non-concordance Staff education Other (please specify) 32 Section D – Root causes Please tick all that apply Pressure Shear Friction Moisture Other (please specify) 33 (How will you make the changes?) (What changes need to be made?) Date completed solution (H., L) StartM, date Action and steps Priority Recommendation/ Person responsible for change Key issues/root causes (list) How will this action be monitored? 34 When you have completed this process: Check that each stage has been completed and recorded. Record the details of other key staff that have participated and ensure they receive feedback on the outcomes of this investigation. Name Designation Date Informed Please note that STEIS also needs to be updated with main findings, lessons learnt and closure of this incident needs to be requested from the SHA by emailing ian.baker@westmidlands.nhs.uk This document is based on the National Patient Safety Agency “learning through action to reduce infection” RCA tool and the University Hospital Coventry and Warwick Tissue Viability Team.