A dysrhythmia is defined as an abnormality in the rate or rhythm
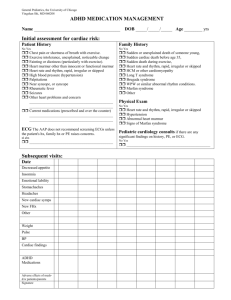
advertisement

A dysrhythmia is defined as an abnormality in the rate or rhythm (regularity) of the heart beat or both. Because of their ability to lower cardiac output, dysrhythmias are associates with a high degree of morbidity and mortality. NORMAL CARDIAC ELECTROPHYSIOLOGY Myocardial cells possess the properties of: a. excitability: ability to respond to an electrical stimulus, an electrical impulse b. automaticity: ability to spontaneously initiate an electrical impulse (property of pace maker cells in the SA node, AV node, and Purkinje fibers ONLY). c. conductivity: ability to conduct or transmit an impulse from cell to cell. d. contractility: ability to respond to an electrical impulse by contracting Refractory period: throughout most of repolarization, cardiac muscle cells do not respond to any stimuli. The property of refractoriness of myocardium prevents uncontrolled, rapid cardiac contractions which would prove fatal without immediate intervention. Cardiac cycle consists of diastole (relaxation; 2/3 of heart cycle) followed by systole (contraction; 1/3 of heart cycle). HEART’S ACTION POTENTIAL Action potential is the process of depolarization (contraction) and repolarization (relaxation) Electrical activity before mechanical contraction Stimulated cell depolarized When an electrical impulse Resting polarized cell – inside of stimulates a resting muscle cell, cell is more negatively charged inside of cell is converted from (-) to (+), causing depolarization. than outside. Depolarized cells then contract. Recovered cell repolarized Repolarization = electrical recovery; returns cell’s charge to negative. Cell relaxes – returning to polarized resting state until another impulse starts the cycle. SUMMARY: electrical activity depolarization contraction/systole repolarization/dystole TREATING DYSRHYTHMIAS Assess/evaluate patient for serious signs or symptoms of dysrhythmia, e.g. rapid HR > 150 bmp Hemodynamically unstable patient with serious signs: CARDIOVERT FIRST. What constitutes a hemodynamically unstable patient? Chest pain, dyspnea, level of consciousness, hypotension, shock, HR, MI, acute pulmonary edema PSVT (PAROXYSMAL SUPRAVENTRICULAR TACHYCARDIA) ECG: stable narrow QRS complex Vagal maneuvers > Adenosine > Cardiovert ATRIAL FIBRILATION Normal cardiac function <48h 1. Control rate: beta blockers; calcium channel blockers (Verapamil/Diltiazem); Digoxin 2. Control rhythm: electrical cardiovert or pharm cardiovert (Amiodarone, Ilbutilide; Dofetilide) 3. Control clot: anticoagulant therapy (Heparin) Normal cardiac function >48h 1. Control rate: beta blockers; calcium channel blockers (verapamil/diltiazem); digoxin 2. Control clot: anticoagulant therapy (Heparin) 3. Control rhythm: delayed for fear of dislodging clot Impaired cardiac function <48h 1. Control rate: Amiodarone, Diltiazem, Digoxin (no beta blockers) 2. Control rhythm: electrical cardiovert or pharm cardiovert (Amiodarone) 3. Control clot: anticoagulant therapy (Heparin) “What did I say? If someone is in HF and A-fib, the drug of choice is Amiodarone.” Impaired cardiac function >48h 1. Control rate: Amiodarone, Diltiazem, Digoxin (no beta blockers) 2. Control clot: anticoagulant therapy (Heparin) for 4 weeks 3. Control rhythm: delayed three weeks for fear of dislodging clot PVC (PREMATURE VENTRICULAR CONTRACTIONS) Acute therapy with beta blockers (Esmolol), Amiodarone or Lidocaine. V-TACH Hemodynamically stable: Cardiovert or Amiodarone/Lidocaine or Procainamide or Sotalol Hemodynamically unstable: Cardiovert V-FIB Assess; check rhythm 1 shock CPR; 5-2 minute cycles Check rhythm 1 shock CPR Vasopressors: vasopressin or epinephrine check rhythm 1 shock CPR Antiarrhythmics: Amiodarone/Lidocaine check rhythm 1 shock CPR ASYSTOLE 1. Confirm asystole in more than one lead 2. Transcutaneous pacing 3. Epinephrine first, then Atropine BRADYCARDIA 1. Atropine 2. Transcutaneous pacing 3. Dopamine, Epinephrine LECTURE When do you treat for dysrhythmia? When you see signs of CO. You will be responsible AV blocks, AV when impulses are excessively delayed or totally blocked in the AV node or junction (junction involves the Bundle of His before it divides). Sinus tachycardia = HR>100 – way above 100 – but the rhythm will be regular. Why? Because it originates from the SA node. Your SA node is your pacemaker, so the disturbance is really in rate. When you have automaticity of the SA node you have sinus tachycardia but the rhythm is regular. It’s still considered a dysrhythmia. In most cases if you have a sinus tachycardia you look for the underlying cause and treat it. Possible causes could be hyperthyroidism, anemia, hypoxia. Somehow there is an in sympathetic effect and a in parasympathetic effect. Many things can cause it, including the bodies own compensatory mechanisms to counterbalance CO – remember that early on HR will CO but overtime it will CO. So when you have S&S of CO you may need drugs that are gong to slow the HR. What drugs can slow the SA node? Digoxin, beta blockers, and calcium channel blockers i.e. Verapamil and Diltiazem – not Nifedipene. They will all slow the SA node and then slow conduction through the AV node. And that will slow the HR. Those three drugs act as SA node blockade and AV node blockade. Digoxin, Beta blockers, and Calcium channel blockers. Sinus bradycardia = HR <60 but the rhythm will be regular b/c it comes from the sinus node. If your rate is so slow it is going to lead to CO and BP leading to tissue perfusion. Identify the cause and treat the cause. In some circumstances you may need a pacemaker to deliver the electrical impulse to which the myocardial cells will react and contract. With bradycardia sometimes a pacemaker will be used; that’s one way to treat a bradycardia. However, what drugs can we use? Atropine. Atropine is a vagolytic (causing inhibition of the vagus nerve), anti-cholinergic, antiparasympathetic that will stimulate the SA node and stimulate conduction through the AV node. It is a major drug given for bradycardia. Remember, bradycardia ends in a, a for Atropine. Amiodarone shows beta blocker-like and calcium channel blocker-like actions on the SA and AV nodes, increases the refractory, and slows conduction of the cardiac action potential. Used for V-tach, V-fib Slows nerve impulses in the heart by acting directly on the heart tissues Side/Adverse Effects: lung problems, liver problems, and new or worsening irregular heartbeats. Drug of choice for life-threatening ventricular dysrhythmias. Adenosine Decreased AV nodal conduction Indications: Supraventricular tachycardias. Since adenosine is only available as an IV solution, and because of its short half life (a matter of seconds) it is only used for acute therapy. Sometimes when people have PSVT healthcare providers can do vagotonic maneuvers to slow the HR by vagal (vagal = parasympathetic) impulses to the heart: carotic sinus massage, valsalva maneuver, gagging, vomiting, coughing, ice bag to face, pressure to eyeballs. PSVT Supraventricular because the foci is above the ventricles. Treatment focus: treat unstable patients urgently. There’s a rule, if the patient is hemodynamically unstable, cardiovert first to covert dysrhythmia to normal sinus rhythm. If HR >150bpm with serious S&S such as chest pain, dyspnea, level of consciousness, hypotension, shock, HR, MI, acute pulmonary edema you don’t have time for drugs. You want to convert the rhythm as soon as possible to normal sinus rhythm. It’s synchronous when you terminate a dysrhythmia with a QRS complex. What we’re going to do if we’re not hemodynamically unstable then we’re going to use AV nodal blocking agents. These ectopic foci that are firing these impulses are not in the SA node, so we’re not talking about SA nodal blocking agents now, we’re talking about these atrial impulses that are going to go down the AV node to the ventricles and we don’t want all those impulses to get down there because it’s your ventricular rate that determines CO, so we want to block a lot of those impulses and prevent those impulses from getting out of control and sending patient into cardiac arrest. We’re talking about foci that are no longer in the SA node. Your impulses from the atria will go down to your ventricles, so we use an AV nodal blocking agent. In this situation what they do to the SA node is meaningless. The drug of chose in PSVT is Adenosine. What are other AV nodal blocking agents? The calcium channel blockers, beta blockers, and digoxin. They work on both the SA and AV node. Normal EF means you’re not in heart failure. When you are in heart failure Adenosine and then Amiadoarone because we said even in heart failure a-fib we want Amiodarone. Diltiazem has less of an effect on myocardium then Veramapil does, so Diltiazem is safer in someone who has HF. And of course you see your Digitioxin. If things are going to cause delay through the AV node, in general you know there is the potential adverse effect of hypotension and bradycardia. Even with a beta blockers and calcium channel blockers we said you can have bradycardia and hypotension. Remember Adenosine is the drug of choice for PSVT. ATRIAL FIBRILLATION The most common dysrhythmia in America. Let’s look at the drugs. For less than <48h control the rate. Your calcium channel blocker Diltiazem or Verapamil. Again you see your beta blockers and Digoxin. Control rhythm you can do it with electrical cardio vert of pharmacologic cardiovert; amararodian ibutilide, dopeltilide. What are we trying to do? To prevent all those impulses from getting down there to the ventricles where the problem really is in terms of making them beat to fast CO, and then your going into cardiac arrest. You see with Amiodarone again the bradycardia and hypotension. It can also cause cardiac toxicity and visual problems. The understanding with supraventricular tachycardias – tachycardias above the ventricles -- you don’t want all the impulses to get down to the ventricles. That’s what all these drugs do. But with PSVT the drug of choice is Adenosine. When we think of a-fib we think of clotting and that they’re going to be on an anticoagulant. If they don’t convert them into sinus rhythm and they continue with the a-fib because they can control it with the rate they’re on Coumadin, Warfarin or aspirin. VENTRICULAR TACHYCARDIA With ventricular dysrhythias you don’t see, “control the rate, control the rhythm”. That’s because we have to get rid of the dysrhythmia. Because ventricular rate determines CO, so now we’re talking real serious so we want to terminate the dysrhythmia, restore normal HR and rhythm. PVC Frequency can indicate myocardial irritability. In and of itself PVC is benign, but 6 or more PVC in a row can lead to the lethal dysrhythmias of V-tach or V-fib. These predispose people to lethal dysrhythmias. And if you have a mild cardio infarction the last thing you want to see if a lot of PVCs in a row. Use beta blockers like Esmolol (IV version) in acute care situation. Same drugs for ventricular dysrhythmias in general. Amioadarone, lidocaine, procanamide, and sotalol. If you have stable v-tach your four major drugs are Amiodarone (used for both atrial and ventricular dysrhytmias), lidocaine, procanamide, and sotalol. However, if they are not stable cardiovert first. V FIBRILIATION For all of these dysrythmias the mantra is “treat the patient, not the monitor”. Firs thing you always do in these situations is assess the patient to know if they are stable or not. There is no contractility so there is no pulse so there is no CO so in 4-6 minutes pt. will be brain dead. First action is defibrillation, not CPR. CPR only until defibrillator is available. So then you give a shock. Use CPR (5 cycles of 100 compressions for 2 minutes), check rhythm, continue CPR while defib charges, give shock, resume cpr, when IV is available give vasopressors first (vasopressin or epinephrine). This happens while someone is giving CPR. CHECK RHYTHM after 5 cycles always. Let’s say you maxed out the vasopressin. Next cycle of drugs is Amiodarone (preferred to Lidocaine), and then magnesium. ASYSTOLE There is no electrical or mechanical activity. Transcutaneous pacing but before you do any treatment you always assess the patient. Confirm asystole in more than one lead. Drugs would be epinephrine and atropine. Unless someone had drowned or suffered an electic shock, you usually have died. so it’s important to see if patient has an order for DNR. Consider withholding therapy if greater than 10 minutes of asystole. COMMON CAUSES OF DYSRHYTHMIAS H.ypoxia A.cid-base imbalance T.oxicity E.lectrolyte imbalances S&S OF CARDIAC DYSRHTMIAS All relate to CO. Hypotension, urinary output, dyspneic, cool clammy skin, capillary refill time, diminished peripheral pulses. Anxiety, restlessness, confusion. Chest pain. AV BLOCKS We’re only doing 1st degree AV node 1st degree heart block. Conduction time is prolonged but all impulses are conducted from atria to ventricles. Treatment necessary only if pt has symptomatic bradycardia with CO. Correct with Atropine. PACEMAKERS Single chamber pacemaker, lead is usually going to right ventricle. Infective endocarditis. An invasive procedure such as dental work could lead to infective endocarditis. You will be held responsible for identifying ECG rhythm changes: A-fib, V-tach, V-fib, PVC S3 in an early sign of HF The dysrhtymia commonly associated with HF is atrial fibrillation and the drug of choice for A-Fib would be IV Amiodarone (atrial and ventricular fibrilation)