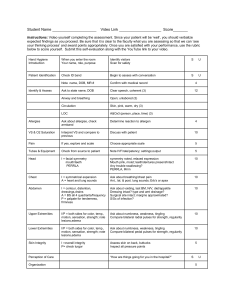
Document
advertisement

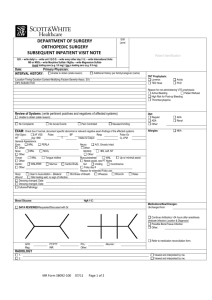
Student Nurse Assessment Sheet Pt. Initials_______________________________ VS: T_______P______R________ B/P R_______ L______ Pain Location_____ Scale 1-10_____ Onset_____ Duration______ Characteristics___________ Aggravating factors____________________ Relieving factors_______________________ Normal Assessment__________________________________Client Assessment_______ Y N Neuro/ Motor: Client is awake, alert Oriented to person, place and time Responds to voice and follows commands Equal, symmetrical strength all extremities Ambulates ad lib Speech clear and understandable Memory intact Behavior appropriate PERRLA Cardiovascular: Apical heart rate regular, rate 60-100 Palpable peripheral pulses all extremities Capillary refill within 3 seconds Extremities warm to touch No numbness or tingling Normal skin color No edema noted No calf tenderness No chest pain Pulmonary: Respirations regular, rate 12-20 No dyspnea at rest or on exertion Breath sounds clear No cough, no sputum Pulse ox >93% on room air Gastrointestinal: Abdomen flat, non-tender Positive bowel sounds all quadrants No nausea/vomiting, tolerates diet Oral mucosa intact Soft, formed, brown, regular bowel movements Genitourinary: Voids independently, no pain or frequency Bladder is not distended after urination Urine is clear, yellow to amber color Skin: Warm, dry and intact Good skin turgor No redness, swelling or breakdown IV access: Type_____ Location___________ No redness, drainage, swelling, pain Flushes easily Dressing intact Surgical dressing or wound assessment: Dressing dry and intact Sutures, staples, steri-strips intact No redness, tenderness, increased warmth Wound edges well approximated No drainage present Decubitus ulcer assessment: Stage_____ Size in cm: L____ W____ D_____ Appearance of wound base_______ Appearance of wound edges______ Drainage__________ Odor_______ Pain_______ Treatment____________________ Y N