Wound care and Dressings
advertisement
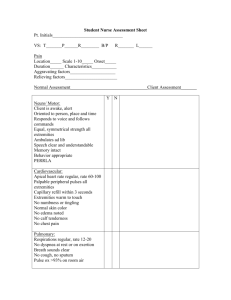
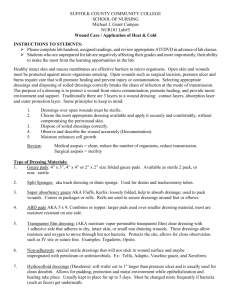
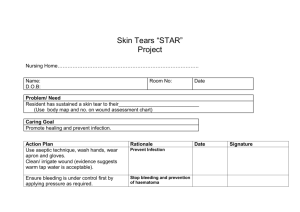
Wound care and Dressings PN 103 • • • • • • • • • Multiple types!!!!! -wounds depth -amount of drainage -location of the wound. -needs a MD/PA/NP order -Follow protocol at your facility -some facilities have pre-written orders depending on the type of lesion. Types of Dressings • Surgical incision• -Clean, well approximated edges, minimal • drainage • • 1. Clean incision with wound cleanser 2. Dry, sterile dressing (DSD) • -Open incision, moderated drainage • • • • • • -packing with normal saline wet to dry dressing -gauze strips -Iodoform, Nu- gauze -Skin prep to surrounding skin -Cover with absorbent dressing -Exudry, ABD-abdominal dressing • Pressure • • • • • and stasis ulcers Wound bed applications -granulating tissue -usually nothing -non-granulating tissue -hydrating gels -Xerophorm/Vaseline gauze • -slough • • • -saline wet to dry -Dakins solution -silvadene crème • -eschar • • • • -debriding ezymes -Dakins solution -large/copious drainage -alginate • -Infected/odiferous wounds• -silver nitrate patches/gels, -anti-fungal gels • Packings• -tunneling/undermined wounds • -Gauze strips• -Iodophorm, Nu-gauze • -pack lightly with Q-tip • -allows granulating tissue to form • Dressings• Thin• -little/no drainage -protection • -transparent (Opsite) • -hydrocolloids (Duoderm, Gentleheel) • -foam (Allevyn, Optifoam), • -gauze (Telfa • Absorbent dressings• -moderate/large amount of wound drainage • -abdominal dressing (ABD), Exudry Tape -paper -clothe (silk, Medipore) -steri-strips -Montgomery straps Wraps -gauze wraps (Kerlex -ace wraps -Coban Etc. -Surgiflex, Band net Allergic reaction to the tape adhesive • -blistering (tape burns) • Avoid tape to fragile, thin skin if possible • Monitoring Wounds • Frequency • • • • • • • • -returning from surgury -wounds appearance changes -Increased odor/purulent drainage -another care setting -each dressing change -Daily-acute care setting -On admission-long-term care facility -once a week there after • Signs of healing• -Decreased size of the wound • -Decreased drainage • - Increased epitheliazation from the edges • to the center of the wound • -scar • Signs of wound deterioration -Increased drainage/odor -Erythema - wound and surrounding skin -Pain -Increased size -Change in wound drainage color • Documentation• • • • • -size -drainage (color, amount) -appearance -surrounding skin -associated pain • Documentation• • • • • -size -drainage (color, amount) -appearance -surrounding skin -associated pain • Wound Evaluation• • -Outcomes based of planning, nursing diagnosis's and goals -if goals are not reached -examine the nursing interventions and strategies, then reassess. -create new goals and modify interventions • Case Study • A patients right heel ulcer is not healing. She is a resident in a long term care facility • How can the care plan be changed to meet the goals of having the right heel ulcer heal with out signs of infection? • • • • • . Float heels when in bed. 2. Change the dressing regime. 3. Padded boots when in bed. 4. Elevate the feet as much as possible 5. Sitting up in the wheelchair with legs elevated only for meals. • 6. Evaluate and measure right heel wound every 3 days x 2 then if healing, evaluate and measure weekly • Therapeutic High Protein Diet • _Components • 1. High protein • -animal proteins • -vegetable proteins (legumes, soy) • -supplements (Ensure, Boost, • Glucerna, Promod) • 2. Vitamin and Mineral Supplements • -leafy green vegetable, citrus fruit • -multivitamin with minerals 3. Fluids/Hydration -1.5-2 liters fluid/day -avoid caffeine drinks -acts as a diuretic -encourage water! • http://www.youtube.com/watch?v=NGocVyrCkC8