1. Classification Genes that regulate & code for the MHC of human
advertisement
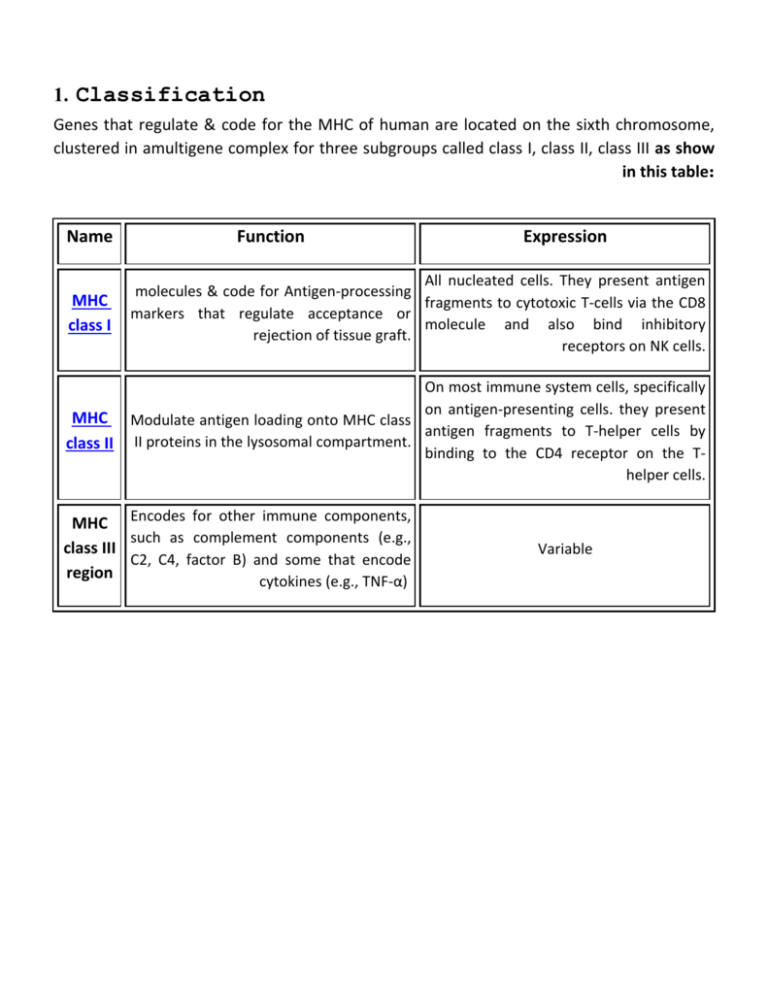
1. Classification Genes that regulate & code for the MHC of human are located on the sixth chromosome, clustered in amultigene complex for three subgroups called class I, class II, class III as show in this table: Name Function Expression MHC class I All nucleated cells. They present antigen molecules & code for Antigen-processing fragments to cytotoxic T-cells via the CD8 markers that regulate acceptance or molecule and also bind inhibitory rejection of tissue graft. receptors on NK cells. MHC class II On most immune system cells, specifically on antigen-presenting cells. they present Modulate antigen loading onto MHC class antigen fragments to T-helper cells by II proteins in the lysosomal compartment. binding to the CD4 receptor on the Thelper cells. MHC Encodes for other immune components, such as complement components (e.g., class III C2, C4, factor B) and some that encode region cytokines (e.g., TNF-α) Variable 2. Responses The MHC proteins act as "signposts" that display fragmented pieces of an antigen on the host cell's surface. These antigens may be self or nonself. If they are nonself, there are two ways by which the foreign protein can be processed and recognized as being "nonself". Phagocytic cells such as macrophages, neutrophils, and monocytes degrade foreign particles that are engulfed during a process known as phagocytosis. Degraded particles are then presented on MHC Class II molecules. On the other hand, if a host cell was infected by a bacterium or virus, or was cancerous, it may have displayed the antigens on its surface with a Class I MHC molecule. In particular, cancerous cells and cells infected by a virus have a tendency to display unusual, nonself antigens on their surface. These nonself antigens, regardless of which type of MHC molecule they are displayed on, will initiate the specific immunity of the host's body. 3. Uses of HLA typing a- Determination of HLA compatibility prior to transplantation. b- Paternity testing. c- Establishing HLA disease associated, 4. Disease associated with HLA antigen have several characteristic a- Of unknown cause& unknown pathophysiology mechanism, with hereditary pattern of distribution but weak penetrance. b- Associated with immunologic abnormalities. c- Have little or no effect on reproduction. Example:For MHC associated disease: Dermititis herpitiformis Insulin-dependent diabetus mellitus Autoimmune chronic active hepatitis. MHC & Disease :1. Certain human diseases occur more frequently among individual who carry particular MHC alleles. These diseases include the susceptibility to certain in factions agents. As well as to a number of auto immune disorders. For exam ankylosing spondylitis whose cause is unknown but another of Caucasian parent with this disease express HLA Balled designated. 2. HLA associated susceptibility to infection disease HLA could be due to an inability of the particular HLA protein to associate effectively with processed Ag. From the pathogen there by limiting the capacity of the individual to mount an immune response against it. 3. Animal populations that reduced MHC polymorphism may predispose a population to infections disease. This accrue because the reduced polymorphism limits the range of Ag to which a population can respond. 4. Although there may be individuals within a species that are unable to respond to a given pathogen because they lack the appropriate MHC alleles. Polymorphism ensures that at least some individuals will be able to respond & that the species as a whole will survives. Antigen, Immunogen : Immunogen : is any agent that is able of inducing an immune response such as M.O or tissue graft; or acquired immune response arise as a result of exposure to foreign stimuli, the compound that evokes the response is referred to either as antigen or immunogen. Antigens : are compounds that are incapable of inducing an immune response& they are capable of binding with the component of the immune system that has been induced specifically against them. Thus all immunogens are antigens but not all antigens need to be immunogens. Required for immunogenecity :Substances must posses the following characteristics to be immunogenic: A) Foreignness : Animals normally don’t respond immunologically to itself, thus for example if a rabbit was injected with its own serum albumin will not mount an immune response. It recognizes the albumin as itself, by contrast if the rabbit serum albumin is injected into guinea pig. The guinea pig recognizes the rabbit serum albumin as foreign & mounts an immune response against it. B) Method of administration : Quantitatively of substances that have no effect when injected intravenously may evoke great Ab response when injected subcutaneously. C) Genetic constitution of the host animal : For example pure poly saccharides are immunogene when injected in to mice or human but not when injected into guinea pigs or rabbits. D) Chemical composition: - large macromolecular proteins are most potent immunogen - polysaccharide & short polypeptides & some synthetic organic polymers are also immunogen but the pure lipids & nucleic acid have not been show to be immunogenic, although Ab that reach with them can be elicited by immunization with nucleoprotein or lipoprotein complex. Therefore this material called Hapten which are substances and called HAPTENS if they fail to stimulate immune-response in their native form due to their low M.WT & their chemical simplicity. These compounds are not immunogenic unless they are conjugated to high M.WT Physiochemically complex carriers. Thus an immune response can evoke thousand of chemical compounds. The hapten simply serves as one of the residues that contribute to the epitope together with amino-acid residues from the carrier. This method has practical importance since it provide simple way of obtaining antibodies directed against any small molecule regardless of its inherent immunogenicity. Therefore the hapten can act as antigen. E) High molecular weight : Immunogenic is that it must have a certain minimal molecular weight. In general, compounds that have M.WT less than 1000 Daltons for example penicillin & progesterone are not immunogenic. Those of M.W between 1000 – 6000 like insulin may or may not be immunogenic & those of M.WT greater than 6000 Daltons, for example albumin tetanus toxins are generally immunogenic. F) Chemical complexity : It’s a certain degree of physiochemical complexity such a polymer of lysine which is of M.W 3000D are seldom good immunogenic, similarly a photopolymer of poly – - D – glutamic acid (the capsular material of Bacillus antharacis of M.W 5000D is not immunogenic); the absence of immunogenecity is because of these compounds, although they are of high M.W are not sufficiently chemically complex. In general, an increase in the chemical complexity of compounds results in increase of the immunogenecity. G) Degradability: The substance must be susceptible to partial enzymatic degradation that takes place during antigen processing by presenting cells such as macrophages. Substances which are resistant to enzymatic degradation are not immunogenic. Antigenic determinant (epitop) :- These structures are referred to as antigenic determinant or epitopes & represent exposed active area of the molecule with which an antibody can combine & can be found by immunoglobulin proteins, therefore called B-cell epitopes but T-cell epitopes are recognized by T – lymphocytes only often being processed & presented in association with a MHC protein on the surface on an (APC). There are many characteristic for epitopes which are : 1. Conformational & linear epitop: Conformational epitop linear 2. Immunodominance: large Ag usually contains numerous epitopes, for example one epitope may evoke Ab quantities & with high binding affinity; than do other available epitop such appeared epitope is said to be immunodominant. Cross – reaction : Identical epitope may be found on a number of different antigenic molecules. As a result Antibodies directed against one antigen may be found to react unexpectedly with antigen from apparently unrelated source. Major classes of antigens : Most materials that serve as antigens fall into the following chemical categories: 1. 2. 3. 4. Proteins & poly peptides (enzymes, albumin, antibodies, hormones, exotoxins). Glycoproteins (blood cell markers). Nucleoproteins (DNA complexed to proteins but pure DNA is not). Polysaccharides (certain bacterial capsule & lipopolysaccharide). Definition of antigenic specification : In general Antigens may be classified into two major types: 1. Exogenous Ags : are those that are presented to the host from the exterior in the form of micro – organisms, pollen, drugs or pollutant. 2. Endogenous antigens : are those that are found within the individual & include many types of antigens, allogenic antigens (Homologous). Some terms used by immunologist for detection of Ag types: 1. Autologous Antigen is ones own Ag, which under appropriate circumstance includes auto antibody formation, autologous Ag is thus synonymous with auto-self antigen. 2. Heterologous Antigen is merely an antigen different from that used in an immunization, it may or may not reach with the antiserum, depending on its chemical similarity to homologous antigen. 3. Homologous Antigen is simply that antigen used in the production of antiserum. In serology (serologic tests) a heterologous antigen may be used as a negative control for any non specific reaction arising from errors in performing the serologic test or in the preparation of the serologic reactants. 4. Cross reactive Antigen heterophil (Heterogenic) antigens are antigens that exist in unrelated plants or animals but are either identical or so closely related that antibodies to one will cross – react with the other. In many instances, heterophil antigens are polysaccharides. Antigen Nomenclature (T – Cell dependant & independent antigens) : T. dependant Ag : The antigens that require T – cells in order to generate an immune response T. dependant Ag & have this characteristic : 1. T – cells are required for the high level of immunity that follows booster injections of antigen. 2. Only (TD) antigens are able to initiate the booster or memory response. 3. The clonal expansion of Ag specific helper T cell is required for many of the characteristic features of secondary Ab response & that an immunogen must contain at least on T-cell epitope in order to induce functional immunological memory. T – cell – independent (TI) antigen :Antigens that stimulate B-cells without the intervention of T-cells & characteristic : 1. To stimulate an optimal immune response to (TI) antigen, the antigen dose must be selected carefully. Too little antigen will be inadequate & too much will favor the development of immunological tolerance rather than immunity. 2. (TI) antigens are structurally simpler than (TD) antigen (it’s not proteins). Diphtheria toxoid, bovine serum albumin, hemocyaneis…are usually (TD) antigen. 3. (TI) antigens are often composed of a limited number of structural units that are repeated through the molecule. This arrangement limits the variety & complexity of their epitope. 4. Though (TI) antigens are less complex than (TD) antigen, they are often catabolized more slowly in vivo. 5. One striking property of the responses to thymus independent Ags, is that no apparent memory even after repeated exposure & the Ab responses are occur after a relatively long lag period & in all other respects resembles primary humeral response. Comparison of T- cell independent & dependent Ags (TI) ANTIGEN (TD) ANTIGEN 1. required T cells No Yes 2. initiated memory response No Yes High Low Simple, repetitive More complex IgM & IgG3 IgM, IgG, IgG2, IgG3, IgG4, IgA, IgE Limited Varied Slow Fast 3. dose dependency of immune response 4. structure 5. class of antibody formed 6. idiotype of Ab formed 7. metabolism in vivo 8. induction of tolerance 9. Ag processing Easy More difficult May not be required for all Required Antibody & Immunoglobulin The Ab are bifunctional molecules which bind specifically to Ags & also initiate a variety of secondary phenomena such as complement activation or opsonization The 4 – chain Basic unit : 1. Each Ig molecule is made up of 2 different types of polypeptides, the larger of these called heavy (H) chains, but smaller light (L) chains & the Ig molecule contain equal number of heavy & light chain. These chains are held together by non covalent forces & also by covalent interchange disulfide bridges & both the heavy & light polypeptide chains are composed of a number of folded globular domains. Light chains always contain 2 of these domains, whereas heavy chains contain either 4 or 5. 2. The light & heavy chains in any single Ig protein are identical but the sequences of these chains vary widely, in both heavy & light chains; this variability is confined largely to the N – terminal domain whereas the sequence of the other domains remains relatively constant. For this reason N – terminal domain in a heavy or light chain is called variable region but the other domains are called constant region. 3. All light chains can be classified into 2 types called (kappa ) & (lambda ) 4. There are 5 (γ – α – μ – δ – ε) different classes of Ig heavy chain which differ in their CH – region sequences & in their physical & biological properties. The γ and α classes are divided into subclasses ( γ1, γ2, γ3, γ4 and α1, α2 ). 5. The Ig are generally natural present in the blood human without previous Ag stimulation but Ab are produced by B cell after antigenic stimulation. Major functional regions of the immunoglobulin in molecule 1. Fab fragment is monovalent with respect to Ag – binding site which contain antigen binding site. 2. Fc region most of the secondary biological property such as (complex activation) is determine by sequence in Fc region & Fc binding site for IgGs that attach via Fc region to the various cell types (Macrophages, neutrophils, mast cells). 3. Hinge region has loose secondary structure that confers flexibility, enabling the 2 arms to move relatively freely with respect to each other (located between the CH1 & CH2 domain). Properties of Ig class : IgG properties 1. The major immunoglobulin & the most abundant Ab produce during secondary H.I.R in the blood. 2. It consists of a monomer. 3. Passes through the placenta. 4. Diffuses readily in to extra vascular spaces. 5. Enhances phagocytosis of microorganism. 6. Activate complement after its reaction with antigen. 7. After attachment to microorganism attracts killer cells.. 8. Macrophages & other cell type express surface receptor that bind the Fc region of IgG molecule. IgM properties 1. 2. 3. 4. 5. 6. 7. 8. 9. The first Ig to appear after immunization & predominant in early P.I.R to most Ag. It is a pentamer (5 units). Does not pass through placenta. Active in phagocytosis (500 – 1000 more than IgG). Activate complement (1000 more activate than IgG). Agglutination particulate Ags (20 than IgG). It has 10 active sites, only 5 are active but all react as hapten. It found as natural Ab against such Ag as the blood group determinant. IgM (usually accompanied by IgD) is the most common Ig express of the B cell. IgA properties 1. 2. 3. 4. 5. 6. 7. The major Ig in extra cellular excretions like milk, tear, mucous, urine, bile. Monomer in serum, dimmer in excretion. Does not pass through placenta Weak in phagocytosis. Activate alternative pathway of complement. Weakly active in agglutination. Protects outside surfaces of body. IgD properties 1. Found mainly on B – lymphocyte & although it found on surface of these cell it is rarely secreted in significant amount. 2. Monomer. 3. It is relatively liable to destroying by heat. 4. Its biological activity is not known. IgE properties 1. 2. 3. 4. 5. 6. 7. 8. Mainly on mast cells, attached to it by Fc.. Monomer. Does not pass through placenta. Not active in phagocytosis. Does not activate complement. Attaches to mast cells & Basophiles. Responsible for defense of body against parasite infection & helminthes. Active in hypersensitivity. When these Ab attach to the surface of mast cell act as Ag receptor, therefore when contact with Ag the mast cell releases inflammatory mediator substance that produce many acute manifestation of allergic disease. Kinetic of the antibody response following immunization : Primary response: The first exposure of an individual to a particular immunogen is referred to as the primary immunization & the measurable response that ensures is called the primary antibody response may be divided into several phases, as follow : 1) Latent or lag phase: after initial injection of antigen, a significant amount of time elapses before antibody is detectable in the serum. The latent period includes the time taken for T & B cells to make contact with the antigen to proliferate & to differentiate. 2) Exponential production phase: during this phase the concentration of Ab in the serum increase exponentially. 3) Study state: during this period production & degradation of Ab are balanced. 4) Declining phase: finally the immune response begins to shut down & the concentration of Ab in serum decline rapidly. Secondary response: A second exposure to the same immunogen results in a secondary response. This second exposure may occur after the response to the first immune event has leveled off or has totally subsided (within weeks or even years). The secondary response differs from the primary response in many aspects : 1) The lag phase is considerably shorter. 2) Ab may appear in less than half the time required for the primary response. 3) The production of Ab is much greater & higher concentration of Ab is detectable in the serum. 4) The production of Ab may also continue for a longer period, with persistent levels remaining in several months or even years later. 5) There is a marked change in the type & quality of antibody produced in the secondary response. . 6) The capacity to make a secondary or memory response may persist for a long time (years in human) . CHARACL PRIMARY I. S. SECONDARY I. S. Mainly by non B. cell B lymphocytes increasingly important Relatively high Low 5-10 days Relatively 2-5 days Relatively low Relatively high Mostly IgM Other class IgG, IgA Relatively low Relatively high 7. Mono specific Ab Abundant Rare 8. The periods of reaming of Low period High 1. Ag presentation 2. Ag concentration needed or induce response 3. Ab response lag phase 4. Peak concentration (Ab levels) 5. Classes 6. Ag affinity Ab in the stem at detectible levels Plasma cells & memory cell: Plasma cells are proteins factory, producing about 2000Abs/sec, in their short life time 5 – 7 days. Memory cells are capable of initiating the antibody mediated immune response upon detecting the particular antigen molecule for which they are genetically programmed. They live longer than plasma cells. Memory cells may live for several years or decades & are responsible for the human system rapid secondary Ab response to the same Ag. The Ag – Ab reaction: (A) This reaction has the following feature : a. It’s highly specific. b. The binding of Ag to Ab does not involve covalent bond, but only relatively weak forces (H – bonding, vanderwals forces). c. The entire molecule reacts but not fragments. d. The combination is firm & reversible. e. There should be an optimal proportion between size & number of Ag with that of Ab. (B) The globulins protein in serum: a. Globulin γ β α1 α2 b. Globulin γ β α1 α2 a. Tracing of an electrophoretic separation of normal serum. b. Some type of tracing of serum from a patient with multiple myloma. Albumine (C) Nature of antigen-antibody reactions : 1-Lock and Key Concept : The combining site of an antibody is located in the Fab portion of the molecule and is constructed from the hyper variable regions of the heavy and light chains. X-Ray crystallography studies of antigens and antibodies interacting shows that the antigenic determinant nestles in a cleft formed by the combining site of the antibody. thus, our concept of Ag-Ab reactions is one of a key (i.e. the Ag ) which fits into a lock (i.e. the Ab ). 2-Non-covalent Bonds : The bonds that hold the Ag in the antibody combining site are all non-covalent in nature. These include hydrogen bonds, electrostatic bonds, Van der waals forces and hydrophobic. Multiple bonding between the Ag and the Ab ensures that the Ag will be bound tightly to the Ab. 3-Reversible : Since Ag-Ab reactions occur via non – covalent bond , they are by their nature reversible . (D) Affinity and avidity : 1) Affinity : Antibody affinity is the strength of the reaction between a single antigenic determinant and a single combining site on the antibody . It is the sum of the attractive and repulsive forces operating between the antigenic determinant and the combining site of the antibody. Affinity is the equilibrium constant that describes the Ag-Ab reaction, most antibody have a high affinity for their antigens. 2) Avidity : Avidity is a measure of the overall strength of binding of an antigen with many antigenic determinants and multivalent antibodies. Affinity refers to the strength of binding between a single antigenic determinant and an individual antibody combining site whereas avidity refers to the overall strength of binding between multivalent antigens and antibodies. Avidity is influenced by both the valence of the antibody and the valence of the antigen. Avidity is more than the sum of the individual affinities. (E) Monoclonal Antibody production : Clinical immunology :First\\ Immunodeficiency : There are 2 types : (A) Primary imm.def. states : These occur in the human as result of any stage of differentiation in the whole immuno system. Defect in phagocytic cells, complement pathway or B-cell system lead to infection with bacteria which eliminated by opsonization & phagocytosis. T- cell deficiencies are susceptible to viruses & molds which are normally eradicated by (CMT). (B) Secondary immunodeficiency: These may arise as a secondary consequence of malnutrition & lymphoproliferation disorder & some agents such as cytotoxic drugs & viral infection, AIDS. Second\\ Hypersensitivity : Allergy (hypersensitivity) allergy is an altered state of reactively to an antigen or hapten, hypersensitivity means a heightened reactively. The 2 terms are interchangeable on the basis of common usage & the pathological reaction can subsequently elicited by that antigen or by structurally similar substance. Immunological basis of hypersensitivity: 1. Immunization & the formation of antibodies does not uniformly leads to state of 2. 3. 4. 5. resistance or immunity e.g immunization with bovine γ globulin, sheep RBC …..Etc. Allergic or hypersens. Responses are immunologic in origin. The initial stage in their development is an exposure to an antigen (called sensitizing exposure). Sensitization is expressed after immunologic waiting period of 5-10 days. The sensitivity can be demonstrated by injection a second dose of antigen. Classification of hypersensitivity: According to time required for host sensitized. 1. Immediate hypersensitivity. This response appear within a few second or a few minutes after administration of second dose of antigen. This reaction disappear rapidly. It depends on IgE. 2. T- lymphocyte – mediated hypersensitivity delayed hypersensitivity (DH). The response in this type is slow in developing reach its maximum after 24-72 hr after exposure to antigen. Comparison of IgE &T. cell mediated hypersensitive T -cell mediated IgE- mediated Second response. Appear with in few minuts fades with in few hrs (immediate). Develop & rades gradually 24- 72 hrs (delayed). 2. Special target tissue. Usually smooth muscle but organ vary with spec. Generalized tissue involvement May occur. Occurs. Yeas: IgE. None. Vascular. Vascular & relatively a Vascular. 6. Histology of skin reaction. Neutrophils , eosinophils edema , wheal & erythema. Mononuclear some Neutrophils less edema & wheal erythema . 7. Mediators. Histamine, serotonin, kinins. lymphokines . Yes, relatively easy. Yeas, with difficult . 1. Timing of response after. 3. Tissue death. 4. Humoral factors involvement. 5. Type of tissue involved. 8. Immunotherapy. Immunophathologic classification of hypersensitivity according to this system four type of hypersensitivity are included :- 1. Anaphylactic type of reaction is that in which immunoglobulin of the IgE type synthesized by plasma cell become attached to mast cells & basophiles through the in Fc portion. Fab regions protrude from the cell surface & when combined with antigen alter the permeability of these cells pharmacologically active substance such as histamine & serotonine released by the cells affect the smooth muscles primary plasma cell. 2. Cytotoxic allergy: this involves the death of cells bearing Ab attached to antigen , Abs are of IgG & possibly IgM classes react directly with antigen on the surface of tissue cells. Complement participate in this reaction & promot cytolysis or cytotoxic reaction E.g. hemolytic reaction drug, allergies, autoimmune disease & allograff rejection. 3. Immune complex reaction antigen antibody complex form in the soluble or fluid phase of tissue or in blood & then deposit on vessel walls & glomerular membrane to interrupt normal physiological process. This lead to complement become activated & release chemotactic factors. The attracted leucocytes release enzymes possibly other agent that injure local times, E.g. Arthur reaction auto immune reaction, glomerlonephritis. 4. Delayed type reaction :- the cell mediated hypersensitivity reaction involved antigen sensitize T-cells which respond directly or by the release of lymphokines. E.g. dermatitis & allergies of infections. The delayed appear of an indurate & erythematus reaction which reaches a maximum at 24-48 hrs & is characterize histology by with mononuclear phagocytes & lymphocytes. Type of hypersensitivity reaction Immunoglobuline Ag involved complement Anaphylactic Cytotoxic I gE IgG , possibly other IgG , IgM … Autologous Auto. or Heterologous Heterologous Heterologous Immunocomplex T-cell dep. Non Auto. Or No Yes Yes No Mast cell & basophiles. Red, white blood cell , platelets Host tissue cells Host tissue cells Mast cell product & other Complement dependent cytolysis Complement dependent reaction Lymphpkines Anaphylaxis , hay fever , food allergy Transfusion reaction , Rh disease Arthus reaction serum sickness Allergy of infection , contact dermatitis involved cellular involvement chemical mechanism Examples Third\\ Tumor immunology : 1. Changes on the surface of tumor cells Some tumors express genes which are silent in normal tissue:- - Tumors express weak Ag associated with in oncogenes. Many tumors express normal differentiate Ag specific for that tissue. Tumors may lack class I MHC molecules. Dysregulation of tumor cells frequently causes struct. Abnormalities in surface carbohydrate str. 2. Immune response to tumors 2 Cytotoxic T–cells may provide surveillance & cause tumor cell destruction or apoptosis. NK cell probably play a role in containing tumor growth & melaslases. They can attack MHC class I negative tumor cell because the class I MHC imparts inactivation signal to NK cell. Fourth\\ Autoimmune disease : This disease associated with certain disease which forms a spectrum. At one pole the autoantibodies & the lesion are organ specific with the organ acting as the target for autoimmune attack (e.g. hashimotos thyroiditis). At other pole the autoantibody have wide activity& the lesion relating to deposition of circulating immune complex there for this called non organspecific or systemic autoimmune disease e.g. (SLE). Genetic & environmental influences :- Multif genetic factors increase predisposition to autoimmune disease these include HLA tissue type. Females have higher incidence of autoimmunity than males, perhaps due to hormonal influences. Environmental influences in many disorders: both microbial & non microbial factors. Microbes may initiated auto immune disease by a number of mechanisms, including molecular or by acting as adjuvant or super antigen. Autoimmunity can arise by pass of T- helper tolerance to autoantigens through abnormal modification of the autoantigen by break down & combination with or cross reaction with exogenous antigen can provide new carriers determination which can activate T-cell. B-cell & T-cell can be stimulated directly by superantigen which are a class of bacterial toxin that have the ability to bind both class II molecular & the TCR ß chain outside of the peptide binding groove. Autoimmunity can arise through by pass of regulatory mechanism. The derepression of class II genes could give rise to inappropriate cellular expression of class II so breaking the silence cellular autoantigen & autoreactive T inducer. TH1 & TH2 imbalance may result in overproduction of inflammatory cytokines. Fifth\\ Immunological tolerance : 1. Definition The failure or relative reduction in immune response on reexposure or exposure to certain specific antigen. 2. Tolerance types tolerance may be peripheral which included by soluble antigen , soluble immune complexes , blocking antibodies or it may be central which is attributed to absence of lymphocyte production , absence of Ag receptors & or due to non-production of lymphocyte receptors. Tolerance may be complete or incomplete. 3. Toleragens Antigen which induce tolerance to termed as toleragens. toleragens are of tow types low dose toleragens & height dose toleragens . Soluble Ags are more toleragens than articulate. Ags tolerance occurred in T-cell rapider than in B – cells. 4. Characteristic The I. S. remains specifically to tolerant toward the many self determinant to which it is continually exposed. The tolerance accrue by either B cell (that could be achieved either by eleminating any cell that express an autoreactive Ab or by permining such cell to survive in a functionally & inactive state) or T cell which become tolerance by remove in compination with self MHC.