Ultrasound Physics and Instrumentation
advertisement

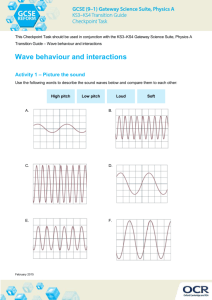
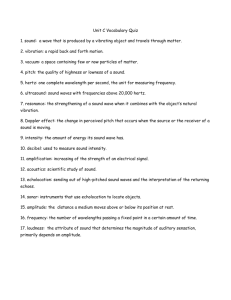
Ultrasound Physics and Instrumentation A. Sound wave propagation. Sound Wave is energy transported through a medium in a mechanical cyclic wave form. 1. Electromagnetic wave: e.g. radio wave, light wave…does not require medium for transmission and is measured in wavelength (distance between 2 adjacent vibrations). 2. Mechanical wave: e.g. sound wave…is transmitted through a medium such as air, water, solid and is measured in frequency (vibrations per second) or Hertz(Hz = 1 vibration/second). We live in a world full of various forms of energy wave forms, some are visible or audible while others can not be perceived by our senses. These wave forms or vibrations form a spectrum of varying frequencies. Light vibrations range from 370 trillion (1 trillion = 1,000,000,000,000) to 750 trillion Hz. However, when referring to light, wavelength is used as the measuring unit instead of frequency). The spectrum of visible light ranges from wavelength of 780 nanometer (1 Nanometer = 1 billionth of a meter) to 380 nm. Ultra-violet, X-ray and gamma rays have progressively shorter wavelengths while infra-red and radio microwave have progressively longer wavelengths. The sound spectrum, on the other hand, ranges from 20 to 20,000 Hertz (Hz). Ultrasound is in the range higher than 20,000 Hz. Medical ultrasound is in the Range of 2 to 7 megahertz (MHz or 1,000,000 Hz). 3. Some useful terms: Attenuation: weakening of sound as it propagates through a medium. Causes: absorption, reflection and scattering. Decibels(dB): units used to relatively quantify intensity of sound for comparison purposes. Frequency: cycle (vibration) per second expressed in Hertz (1 Hz = 1 vibration/second) Intensity: Power(energy/time)/area = Watts/area Incidence: Direction of sound wave travel to the boundary between 2 media, e.g. perpendicular, oblique angle. Impedance: = density of medium times propagation speed. 1 2 Inverse square law: intensity of sound varies inversely with the square of the distance from the source. Speed of propagation: depends on the medium. The more solid (high elasticity or stiffness) medium allows faster speed. Decreasing speeds in solids, water, air. Boundary (interface between media) behavior: a, reflection: bouncing back from the boundary. specular reflection: when the boundary is smooth and flat. scattering: when the boundary is rough and uneven. b, refraction: crossing the boundary with change in direction. c, transmission: going through the boundary. B. Transducer function. Transducer converts one form of energy to another. Ultrasound transducer converts sound wave energy to electric energy and vice versa. Piezoelectric element: material that is capable to convert pressure and electricity. such as ceramic, quartz etc. 1. Composition of an ‘US Probe’: a, piezoelectric element (crystal) in linear, curved(sector), and phased array. b, damping or matching material: to improve transmission. 2. Operating frequency: The higher the operating frequency, the thinner the transducer element, the greater the attenuation (or the lesser the depth penetration). 3. Beam focusing: focusing electronically to improve resolution at various depths. 4. Coupling medium: Gel used to eliminate air at transducer-skin interface to maximize ultrasound transmission. 5. Types of transducer: a, external: linear array (flat top, curved top, pointed top), sector (convex, phased, vector). b, internal(endo-): rectal, vaginal, esophageal, vascular, etc. 3 6. Penetration: depth of images obtained is directly related to: a, attenuation by the medium. b, power of the beam. c, frequency (Hz). inverse relationship. C. Time-gain compensation (TGC slope). To provide a more uniform image by ‘compensating’ the weaker signals from deeper (further from the transducer) tissue as a result of longer time and greater attenuation D. Resolution. 1. Detail: degree of separation of structure echoes or signals a, axial resolution: along the beam direction. b, lateral resolution: perpendicular to the beam direction. Increased frequency means increased resolution but decreased penetration. Useful US frequency is 2 – 15 mHz. 2. Contrast: improves with: a, greater gray scale (US signal strength or signal strength vs B-W scale). b, color display. 3. Temporal: improves with higher frame rate. E. Artifacts. Types: 1, false(erroneous) signals or images. 2, missing signals or structures. 3, wrong locations. 4, incorrect sizes. Causes: 1, section thickness. Ultrasound beam is 3-D while the displayed image is 2-D. 2, acoustic speckles. Interference effects of scattered sound beams and echoes from various tissues and directions of the ultrasound beam. 3, reverberations. Repeated echoes occur between the transducer and a strong reflector. ‘mirror image’ is a form of reverberation artifact and formed with a strong reflector within a tissue. 4. refraction. Laterally misplaces or mis-shapens a structure when a beam is refracted in the tissue. e.g. observed depth of object in water. 5, speed error. Axially misplaces a structure when the speed of US beam is miscalculated. 4 6, shadowing. Decrease or loss of US signal behind a strongly reflecting or attenuating structure, or from the edge of a refracting structure. 7, enhancement. Increase in echo signals behind a poorly attenuating structure. 8. grating lobes. False duplicated and miscalculated images created by side beams in directions different from the primary beam. F. Proficiency in imaging technique. 1. Patient interaction: professional but friendly. courteous and respectful, esp. in regard to privacy issue. informative re the procedure, but not the diagnosis. 2. Proper instrument settings, probes and gel. correct transducer frequency (mHz) and type adjust field size, near & far gain settings, contrast, gain and TGC slope. 3. Scanning technique. a, Patient position: supine, prone and lateral , to provide shortest distance to the anatomical structure of interest. b, Image: in traditional sagittal and transverse (axial) planes. Also oblique, coronal and angled planes, if necessary. c, Identify anatomical structures and landmarks. D, Know the pathology (the abnormal findings). G. Safety. There is no known risk associated with diagnostic ultrasound since first used in the 70’s. However prudence dictates a conservative and judicious usage because the possibility of adverse bio-effects from even a low level, delayed harm of the US energy transfer can not be absolutely denied. Therefore one needs to minimize the use, exposure time and intensity of the diagnostic ultrasound without sacrificing the proper gathering of diagnostic information.