Getting Better in Fife
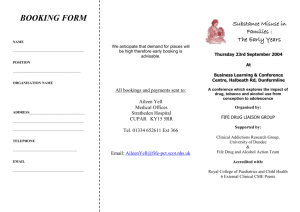
advertisement

Getting Better in Fife 2012-2017 Version 12.10 (12/09/2012) 1 Getting Better in Fife Contents 1. CHIEF EXECUTIVES’ FOREWORD ................................................................ 3 2. NHS FIFE’S STRATEGIC OVERVIEW ............................................................ 4 2.1 Context ............................................................................................................. 4 2.2 The Position in NHS Fife .................................................................................. 5 2.3 Working in Partnership ..................................................................................... 7 2.4 Responding to the Coming Challenges ............................................................ 8 2.5 Moving toward 2020 – NHS Fife’s Vision ......................................................... 9 2.6 Maximising NHS Fife’s Estate .......................................................................... 9 3 MOVING FORWARD – GETTING BETTER IN FIFE ....................................... 9 3.1 What are we trying to accomplish? ................................................................. 10 3.2 Delivering Getting Better in Fife; A Programme of Improvement Projects ...... 11 3.3 Improving Flow and Emergency Access- the Right care in the Right Place at the Right Time ................................................................................................ 12 3.4 Improving Elective Flow –Care where it counts, care when it counts ............. 14 3.6 Safe and Accessible Mental Health Services ................................................. 18 3.7 Safe and Effective Medicines Management ................................................... 21 3.8 Examples of improvement projects and tests of change ................................ 23 4 IMPROVEMENT APPROACHES .................................................................. 23 4.1 Quality Improvement Methodology ................................................................. 23 4.2 Programme Management Office .................................................................... 25 5 HOW WILL WE KNOW WHEN CHANGE IS AN IMPROVEMENT ............... 25 5.1 Measures for Improvement............................................................................. 25 6 ALIGNING RESOURCES TO SUPPORT THE PRIORITIES ......................... 26 6.1 Building Capacity and Capability for Sustainable and Effective Quality Improvement .................................................................................................. 26 6.2 Quality Improvement Hub ............................................................................... 26 7 WHAT DOES THIS MEAN FOR THOSE WE CARE FOR AND OUR STAFF?.......................................................................................................... 27 Appendix 1 ............................................................................................................... 29 2 Getting Better in Fife CHIEF EXECUTIVES’ FOREWORD 1. In 2002 Fife Health Board embarked upon an ambitious programme of service redesign across all the strands of healthcare in Fife. This plan became known as “Right for Fife” and anticipated many of the issues which have caused all healthcare systems to review how services can be provided. The success of “Right for Fife” has put NHS Fife in a good position to move forward. Much of “Right for Fife” was structural and has resulted in improved in-patient facilities for patients at St Andrews, Adamson, Stratheden, Lynebank, Randolph Wemyss and Victoria Hospitals, and new community facilities for example in Anstruther and Dunfermline and across Fife in respect of dental access centres. Importantly, it also encompassed new models of care and patient pathways resulting in reduced lengths of stay, reduced waiting times and reduced numbers of hospital attendances through developments of increased “one stop” clinics and services provided on an ambulatory, or day case, basis. So, ten years on we have achieved much, but there is still more to do. My goals over the next five years are to: Recognise the need for continuous improvement and to enable staff to redesign services they provide while continuing to provide safe and effective care in a changing environment. Build on the good work of “Right for Fife”, ensure we finish what we started and further improve clinical care. I want NHS Fife to be a place where: Staff are able and encouraged to make changes to reflect patient needs in their area and to ensure care is person centred. The culture is that we are always looking at how we can do things better. The culture that patients feel safe, valued and well looked after. Staff feel able to raise issues and suggest improvements. People are prepared to make changes and to think about the “how to” and not the “why not”. This plan – Getting Better in Fife – sets out the processes to make this happen and the priority areas in which we will invest time and resources to make it happen. We will also continue to provide the wide range of services to the people of Fife and meet our performance targets This plan is not an end product – it is the start of a process which will evolve over time. John Wilson Chief Executive, NHS Fife 3 Getting Better in Fife 2. NHS FIFE’S STRATEGIC OVERVIEW 2.1 Context NHS Fife works with and on behalf of the citizens of Fife to improve their health and healthcare. The Scottish Government set out the national framework for improving Scotland’s health and healthcare in its Quality Strategy1 which sets out NHSScotland’s vision to be a world leader in healthcare quality, described through 3 quality ambitions: effective, person centred and safe. These ambitions are articulated through the 6 Quality Outcomes that NHSScotland is striving towards: Everyone gets the best start in life, and is able to live a longer, healthier life; People are able to live at home or in the community; Healthcare is safe for every person, every time; Everyone has a positive experience of healthcare; Staff feel supported and engaged; The best use is made of available resources. The Quality Strategy builds on Better Health, Better Care2 and, together with subsequent supporting publications; they provide the overall strategic context. Since 2002, NHS Fife Board has been delivering an ambitious programme of development and modernisation designed to improve the range and quality of healthcare services and to improve the quality of the premises from which services are provided the implementation in Fife of the Quality Strategy and of Better Health, Better Care. Within the national framework, NHS Fife has prime responsibility for the protection and improvement of its population’s health and for the delivery of frontline healthcare services. It does this through services it provides itself, through primary care contractors, through joint working with other agencies and NHS Boards and through public participation and patient focus. Services are provided in people’s own homes and from a range of locations and premises across NHS Fife. All NHS Boards work together for the benefit of the people of Scotland; NHS Fife works principally with NHS Lothian and NHS Tayside to provide specialist and other healthcare to the people of Fife. Because social and economic participation is vital to good health and economic growth, NHS Fife also works closely with its Community Planning Partners - Fife Council, Fife Constabulary, the Further Education Colleges located in Fife and the voluntary sector, all of whom come together as part of the Fife Community Planning Partnership. 1 2 The Scottish Government. The Healthcare Quality Strategy for NHS Scotland; Edinburgh 2010 The Scottish Government. Better Health, Better Care; Action Plan; Edinburgh 2007 4 Getting Better in Fife Fife’s Community Plan and Single Outcome Agreement demonstrate how the Partnership will contribute towards delivering the Scottish Government’s National Outcomes in order that: We tackle the significant inequalities in Scottish society; Our children have the best start in life and are ready to succeed; We improve the life chances for children, young people and families at risk; We live longer, healthier lives; Our public services are high quality, continually improving, efficient and responsive to local people’s needs; We reduce the local and global environmental impact of our consumption and production; and Our people are able to maintain their independence as they get older and are able to access support when they need it. 2.2 The Position in NHS Fife Since 2002, NHS Fife has significantly changed the way it contributes to the health and healthcare of the population. Over the decade we have transformed a very large part of the way NHS care is provided. The paragraphs which follow offer some key headlines from a much longer story. In terms of health improvement and primary prevention we are for example: Strengthening the ability of General Practice o By supporting chronic disease management, developing and strengthening our community and public health nursing, podiatry, speech and language, physiotherapy and occupational therapy services, increasing direct access to diagnostic services and through investment in modern premises, including the refurbishment of Rosyth and Kirkcaldy Health centres, the redevelopment of Cupar Health Centre and the development of Skeith and Linburn Health Centres. Strengthening the ability of General Dental, Ophthalmic and Pharmaceutical Services o Through investment in premises- 10 new dental services centres, by further improving links to specialist care (e.g. the eye care project) and in the introduction of a range of pharmacy based services including the roll out of the new community pharmacy contract, and a range of local services based on need. For example, we have a network of palliative care community pharmacies, ‘Just in Case’ boxes to meet the anticipatory medication needs for patients at the end stages of life. Implementing and sustaining a range of health improvement programmes o Including smoking cessation, alcohol brief interventions and weight management, mental health – facilities, therapies, earlier diagnosis and interventions for dementia and better collaboration across services. 5 Getting Better in Fife In terms of helping to meet the needs of the most vulnerable members of our community we have strengthened some services and redesigned others. Examples include: Children We have centralised inpatient paediatric services within Victoria Hospital, increased service provision for the care of children in the community, redesigned services and health improvement work in the monitoring and delivery of the child healthy weight programme and developed an integrated care pathway for vulnerable under 2 year olds. We have further developed and are delivering an integrated model of care across council and health – pathways and implementation of ‘Getting it right for every child’ across the Fife partnership. NHS Fife is one of the first Boards to implement the Family Nurse Partnership (FNP). FNP is evidence based, preventative programme offered to young mothers having their first baby. It begins in early pregnancy and is orientated to the future health and well-being of the child. It is a nurse-led, intensive, home visiting programme and supports universal services in supporting teenage families. FNP is a licensed programme with structured inputs and well tested theories and methodologies. Creating the right environment to deliver the FNP is important and challenging. The aims are achieved by maintaining fidelity to the programme license which is essential if the benefits identified in the research are to be realised. These benefits of this are: O Improving the outcome of pregnancy by supporting women to improve their prenatal health; O Improving child health and development by supporting parents to provide more competent care of their children in the first 2 years of life; O Improving families’ economic self-sufficiency by supporting parents to develop a vision of the future, accomplish goals by planning timing of pregnancies and staying in school/finding work. People with Learning Disabilities NHS Fife participates in a national accreditation programme to ensure staff are highly trained in this speciality area and additional investment has been made in Community Based Care with additional specialists in post to deliver the care and enable the development of the Learning Disabilities Unit and the Regional Learning Disabilities unit at Lynebank. In terms of improving care, we are for example: Strengthening the workforce by o Training and developing highly specialised clinicians e.g. Advanced Nurse Practitioners, Specialist Nurses and other Allied Health Professionals 6 Getting Better in Fife o Using Redesign, Organisational Learning and Development resources, In-house and external training programmes and organisation-wide implementation of the electronic Knowledge and Skills Framework to provide our workforce with the skills required to deliver 21st century healthcare Moving to new ways of delivering care for example by o Implementing the Scottish Patient Safety Programme methodology including the use of care bundles, use of Day Surgery where possible and appropriate, shorter waits for investigation and treatment, one stop clinics, state of the art facilities, increasing use of IT e.g. electronic prescribing, telehealth, telecare and video conferencing including Telepresence, electronic patient referral processes and ordering of investigations Redeveloping premises including o 2.3 The new wing at the Victoria Hospital, the Learning Disabilities Assessment and Treatment Unit based at Lynebank Hospital, two new mental health wards at Stratheden hospital, the new community hospital in St Andrews and redevelopment of Adamson Hospital and Randolph Wemyss. Working in Partnership Community Planning is a process which helps public agencies to work together with the community to plan and deliver better services which make a real difference to people's lives. NHS Fife is a major contributor in this work in Fife. Partners identify the priorities for joint working and align/pool resources around projects where they identify an advantage in doing so. The breaking down of barriers between organisations and the requirement to achieve more with the resources available should foster innovation and new ways of working in partnerships. Single Outcome Agreements are an important part of this drive towards better outcomes. They are agreements between the Scottish Government and Community Planning Partnerships which set out how each will work towards improving outcomes for the local people in a way that reflects local circumstances and priorities. The Fife Partnership is responsible for community planning in Fife and is made up of representatives from local agencies. Fife’s Health and Wellbeing Alliance comprises NHS Fife, Fife Council and Fife’s Voluntary sector and works to reduce health inequalities and improve health and wellbeing for the people of Fife. The Fife Health and Social Care Partnership (FHSCP) is a partnership between NHS Fife and Fife Council and its Social Work and Health Committee. The partnership works closely together to plan and integrate the care provided for the people of Fife. This closer joint working enables more effective and efficient use of partnership resources, maximises opportunities and facilitates the delivery of higher quality and more 7 Getting Better in Fife responsive services. The FHSCP Service Delivery Plan3 sets out how the joint service will deliver health and social care for: Older people People with learning disabilities or autism spectrum disorder People with and affected by mental ill health People with physical disabilities or sensory impairments People with and affected by drug and alcohol dependency The processes of continual improvement in our services are ongoing. Working with Council partners and using the Older People’s Change Fund – a government initiative – we are changing the approach to the care of older people. Residential care, whether in a care home or a hospital, is becoming the last resort rather than the first choice. A wide range of re-ablement rehabilitation services will enable people to stay healthier and stay at home longer, and the developing “virtual ward” approach will mean even when actually ill, many people will be able to stay at home. In May 2012, the Cabinet Secretary for Health, Wellbeing and Cities, Nicola Sturgeon, launched a consultation document outlining proposals to integrate adult health and social care across Scotland. The aim is to improve care for patients by overcoming some of the 'disconnects' between different parts of public sector services including primary care, social work, community health and some acute hospital services. While it is recognised that progress has been made across Scotland, more needs to be done in partnership to meet the future needs of the population. The specific proposals outlined in the consultation are to establish a health and social care partnership which will take a joint local responsibility for the delivery of adult health an social care in each Council area. We have made significant progress across Fife with the existing partnership arrangements. We have been at the forefront of many significant service improvements and have led innovation across services for older people, mental health services and in the development of community based service for people with a learning disability. We believe the development of a health and social care partnership in Fife, working as part of a whole system, will help us take that joint working a step forward to ensure that we provide seamless care for the people of Fife. 2.4 Responding to the Coming Challenges While services have changed and continue to change, the challenges facing the NHS continue to grow. As a society, we are getting older, with more people living longer and fewer people in the workforce. Lifestyle diseases such as obesity are generating new healthcare demands and advancing technology, including new drugs, means the NHS can do more to help more people. The NHS can only reconcile that growing need with the reality of contained resources by doing more with less. Our investment programme, in new community facilities as well as new hospitals, has put us in a strong position already but we need to do more. 3 Health and Social Care Partnership Service Delivery Plan 2012 - 2015 8 Getting Better in Fife By looking to nationally recognised evidence and best practice we must work to provide harm free care and identify unwarranted (wasteful or harmful) variation and waste in the system. We must challenge out dated traditional ways of organising and delivering services and redesign them to provide an up-to-date and highly efficient and safer health service. We must identify productive opportunities and use them. Our vision for 2020 is that everyone is able to live longer healthier lives at home, or in a homely setting. We will have a healthcare system where we have integrated health and social care, a focus on prevention, anticipation and supported self management. Primary Care has a key role in helping the healthcare system as a whole make improvements. When hospital treatment is required, and cannot be provided in a community setting, day case treatment will be the norm. Whatever the setting, care will be provided to the highest standards of quality and safety, with the person at the centre of all decisions. There will be a focus on ensuring that people get back into their home or community environment as soon as appropriate, with minimal risk of re-admission. 2.5 Moving toward 2020 – NHS Fife’s Vision The narrative above gives an indication of some of the challenges that lie ahead. Funding increases will be lower and demands for services higher. NHS Fife recognises the opportunities this offers. We will need to scrutinise all areas of service to ensure they are efficient, perform to the highest standards and deliver the best possible care. We share the national ambition for achieving world leading quality in healthcare services and are committed to realising it. 2.6 Maximising NHS Fife’s Estate The major infrastructure changes in NHS Fife have largely taken place already, but we will continue to improve the healthcare environments and deliver the necessary equipment and technology systems to enable the highest possible clinical care provision to our patients. Our Property and Asset Management Strategy, (PAMS) will target the areas of improvement over the next five years and beyond. The work undertaken as part of this improvement plan will guide the decisions and priorities for our capital investments. 3 MOVING FORWARD – GETTING BETTER IN FIFE Getting Better in Fife is the name for our healthcare improvement plan for the next five years. It describes our priority areas for improvement in the delivery of clinical services. It underpins our strategic objectives. 9 Getting Better in Fife 3.1 What are we trying to accomplish? The aim of Getting Better in Fife is to improve the patient experience through reducing harm, waste and unwarranted variation. Getting Better in Fife describes our five areas of strategic priority relating to the healthcare services we provide. Some of these services are delivered in partnership and others by NHS Fife alone. NHS Fife also has a responsibility to improve the health of the population. This responsibility is driven by related strategies and action plans developed in partnership with local council and primary care colleagues who have a significant contribution in improving the quality of services4. So the focus of Getting Better in Fife is the systematic improvement of the clinical services delivered to our local population across the whole healthcare system. Getting Better in Fife builds upon the improvements that were the subject of Right for Fife and describes our next areas of focus. Here are some examples of what we believe a quality service looks like for our staff and patients. These are real examples that already exist and we want everyone engaged with us to have experiences of this quality. 4 Colin’s Story Evelyn’s story Colin was in our Intensive Therapy Unit (ITU) for extended period of stay. Shortly after admission he was given the ‘ITU look’ (clean shaven, short haired), listened to whatever radio choice the nursing staff made and his family were only allowed to visit at specific times. He was receiving good quality clinical care but as he became able to articulate his desires it was obvious we weren’t meeting his personal needs. Colin didn’t like to be woken early, wanted to keep his facial hair and his head hair long and preferred to have peace and quiet rather than music. The clinical team made these changes and, as well as seeing Colin cheer up, they also noticed an improvement in his response to and compliance with the clinical care.” Evelyn is an experienced staff member working in occupational therapy. By working in radically different way with one client, she discovered moments of great satisfaction for her and for the client. Her client lived at home but required lots of support and had effectively become house-bound. By enquiring what this person really wanted she discovered that cups of tea and chat were as, if not more, important as the clinical care as this kept her client feeling more in touch with the outside world. Secondly, her client really wanted to visit the local shops. Working with partners in other teams and organisations, they enabled the client to visit the local supermarket. This experience was really positive for her client. Delivering Quality in Primary care National Action Plan, Scottish Government August 2010. 10 Getting Better in Fife 3.2 Delivering Getting Better in Fife; A Programme of Improvement Projects In order to meet the aim of Improving the patient experience through reducing harm, waste and unwarranted variation, five strategic priority areas have been identified. These areas have been developed by integrating and analysing current programmes of work across the whole system, reviewing quality and efficiency data and responding to national strategic drivers. The priorities within Getting Better in Fife are: Improving Flow and Emergency Access Improving Elective Flow Reshaping Older People’s Services ( Including Integrating Health and Social Care ) Safe and Accessible Mental Health Services Safe and Effective Medicines Management Discussions with staff and public representatives have endorsed the choice of these priority areas and the detail of activities under each heading will be reviewed and updated on an ongoing basis. 11 Getting Better in Fife 3.3 Improving Flow and Emergency Access- the Right care in the Right Place at the Right Time Jean was admitted to our hospital in January 2012 with a recurrence of a chronic respiratory condition. She was experiencing shortness of breath and could no longer walk around her garden. Jean was cared for in the respiratory ward for 2 weeks but 2 days before she was due to be discharged, she was transferred to a ward which did not specialise in caring for patients with respiratory conditions (boarded) as her bed in the respiratory ward was required for a more acutely unwell patient. Jean’s family were really concerned when they came for evening visiting and discovered she was not on the ward they expected. Although Jean described receiving excellent care in the new ward, the nurses were new to her and she did not see the physiotherapist every day as she had done in the respiratory ward. Jean became increasingly anxious that the staff were not familiar with her or her condition. Jean then experienced a recurrence of her shortness of breath which was attributed to anxiety around the move between wards. This resulted in Jean spending an extra 2 days in hospital. Although she did make a good recovery, she found the experience very difficult. Jean says “I do still remember what happened and although all the staff in the new ward were very nice, I found it frustrating and worrying that they didn’t seem to know what I needed’. What are our aims? To ensure that patients accessing emergency care receive the Right Care in the Right Place at the Right Time through: Meeting the 4 hour emergency access standard which aims for 98% of patients who attend the Emergency Department having their needs met within four hours of arrival. This will involve being admitted, discharged or transferred from the department. Ensuring that patients who require specialty review in the Emergency Department are referred to and assessed by that specialty within a clinically appropriate time scale Improving the efficiency of the patient journey (Flow) to ensure that patients who are admitted urgently and who require to stay in hospital do not have to 12 Getting Better in Fife stay longer than necessary and get access to the appropriate service in the appropriate place at the appropriate time. Collaborative working across the health and social care system to deliver an optimum length of stay for patients with complex care needs Why will this improve the patient experience and reduce harm, waste and variation? Prompt access to emergency care-initiation of appropriate treatment and reduction in unnecessary moves between wards will help us reduce length of stay and improve the outcomes and experience of our patients. Transfers late at night for non clinical reasons leads to staff spending increased time identifying and following up patients. Moves between wards can also lead to unnecessary variation in treatment and lengths of stay in hospital and contribute to the disorientation of frail elderly patients. Extended length of stay in hospital for non clinical reasons, e.g. patients with complex discharge planning needs and patients being discharged later in the day, can negatively impact on the care of new patients through delays in admission, assessment and initiation of treatment. 13 Getting Better in Fife 3.4 Improving Elective Flow –Care where it counts, care when it counts Mr Simpson was referred by his GP to see a specialist. He had an initial consultation and was sent for tests. He was told that he required more specialised tests and had to wait 8 weeks to have these carried out. During this time Mr Simpson had to take time off work and was concerned about the financial impact of this. He struggled to cope with the impact of his physical condition which had an impact on his mental health. He asked, “Why was I treated as an illness rather than a person, with no thought or consideration given to my personal or professional life?” What is our aim? To deliver patient centred care and enable people to maintain their contribution to society, through prompt assessment, diagnosis, and intervention. By ensuring that 90% of patients who are referred have their assessment, diagnosis and treatment within 18 weeks from referral. 95% of patients who are referred with a suspicion of cancer receive assessment, diagnosis and treatment (if required) within 62 days from referral. 95% of patient diagnosed with cancer receive their treatment within 31 days from the decision to treat This program will maximise the use of technology and make effective use of all resources on all sites. This will reduce unnecessary hospital visits, reduce unwarranted variation and will deliver a person centred, timely, high quality planned care service This programme will also contribute to the delivery of the following objectives: Meet the 18 weeks referral to treatment guarantee Meet the 12 week treatment time guarantee for patients requiring inpatient and day case treatment Meet the 6 week waiting time target for key diagnostic tests Meet the 12 week waiting time target for outpatients 14 Getting Better in Fife Meet the 62 day and 31 day cancer targets Improve the early detection of Lung, Colorectal and Breast cancers Why will this improve the patient experience and reduce harm, waste and variation? This programme has identified examples of where waste, variation and harm has occurred across the whole of the patients pathway from referral, through consultation and diagnosis, to preparation and planning for treatment to the period after intervention. If waste, harm and variation is reduced this would improve the quality of experience for patients and bring significant efficiency benefits to NHS Fife. Examples of benefit include: Providing GPs with direct access to diagnostic tests improves the patient experience and reduces the number of visits and steps in a patients pathway A reduction in Did Not Attend (DNA) and cancellation of appointments and theatre slots ensures effective use of expensive resources and an improved experience for patients through quicker access to clinical care. Ensuring demand and capacity for services are appropriately balanced and managed reduces the need for additional clinics and theatre sessions and reduces the need for expensive waiting list initiatives. Increased use of day surgery means patients do not need to stay in hospital longer than is necessary and it improves their outcomes. Maximising the use of available resources and facilities at Queen Margaret Hospital, in particular day surgery capacity, will allow increased and appropriate use of resources across sites. Early detection of cancer facilitates earlier treatment and improves the chance of better outcomes and experience for patients. When they are required, ensuring timely access to services improves the experience for patients. 15 Getting Better in Fife 3.5 Reshaping Older People’s Services (Including: Integrating Health and Social Care) Mrs Smith a 90 year old lady was admitted on three occasions from a Nursing Home to our Acute Hospitals between the December and January 2012. She was admitted initially with respiratory symptoms (she is known to have a chronic chest complaint) and was subsequently diagnosed and treated for a chest infection. On the third admission to hospital Mrs Smith was accommodated in four different wards. She spent four days in the Admissions Unit, a further four days in the Respiratory Ward, six days in an orthopaedic ward as there were not enough beds available in her speciality and a final move to a rehabilitation ward where she stayed for a further 20 days. During the time Mrs Smith spent in hospital there were issues with continuity of care. Had Mrs Smith had access to treatment in the nursing home from the outset, her admissions may have been prevented. What is our aim? To meet the needs of the older population now and in the coming years, all Health and Social Care Services should have a primary aim of maintaining and supporting independent living and maintaining quality of life. The resources of local people and communities will be at the centre of social care provision. Within the context of Getting Better in Fife we aim: To ensure that older people with complex needs are well supported by all parts of the care system. To develop care settings, with partners that will help older people to remain at home; or in a homely setting; and developing community capacity to enable older people and their communities to develop local systems of self-care. To reduce the length of stay for older people in hospital, and avoid any unnecessary transfers in care. To reduce falls-related admissions to hospital in the over 65s by 20% through the implementation of integrated falls and fracture care pathways. 16 Getting Better in Fife To build relationships with the voluntary sector and private providers to develop community capacity models, and new models of care. Develop and invest in support for Carers And in particular to: Develop a new Integrated Assessment and Community Support Service (ICASS) which provides hospital at home, intermediate care and home re-ablement services that are responsive to need and will prevent admission to hospital as well as supporting early discharge. Review the community bed resource, in line with our intention to move to more care at home and agree a plan of reduced inpatient based care and treatment. Why will this improve the patient experience and reduce harm, waste and variation? Hospitals have generally been viewed as the source of expert care and the public have become accustomed to receiving inpatient care as the first option when faced with a crisis or emergency. Hospitals do not always provide the most appropriate environment in which to provide care that is not of a specialist nature. This is particularly so for elderly frail patients and other vulnerable groups. Importantly patients have also expressed the preference to remain in their own homes and to be treated there if possible. Smooth transition for patients between health and social care sectors in Fife will reduce the opportunity for duplication and improve the patient experience A patient safety approach to developing a “transfer bundle” will improve communication, and ensure transfers in care are undertaken efficiently and without harm. The ICASS model currently being implemented across Fife plans to deliver a fully integrated service for frail older people who would have otherwise been admitted to hospital for common conditions. The re-ablement and Home Care Change Programme will enable patients to maintain their skills and independence for longer periods. Developing the use of technology for example using mobile telecare devices can support people beyond the confines of their own home allowing them to remain in the community. Building on our programme of falls and fracture prevention has significant potential to improve the patient experience and reduce harm waste and variation A focus on modernising current day services and day hospital models will promote independence and re-ablement, and avoid unnecessary admissions to institutionalised based care. 17 Getting Better in Fife 3.6 Safe and Accessible Mental Health Services Tracey is a 28 year old woman who experiences episodes of depression and thoughts of self-harm and who has required short episodes of inpatient care in the past few years. She dislikes being in the ward setting stating that she feels unsafe, that there is a lack of staff engagement with her, and that there is little meaningful activity throughout the day. As a result, she does not think the experience is therapeutic and she struggles to achieve the intended improvement in her health. . What is our aim? To improve the mental health of the people of Fife and deliver prompt, safe and effective treatment for those with mental illness. We will focus on a range of work designed to support the key themes and areas of change identified in the recently published Mental Health Strategy for Scotland and on specific areas of work identified locally as essential for the effective, efficient and sustainable delivery of current and future services. Within the context of Getting Better in Fife we will aim to: Continue the improvements made in ensuring faster access to specialist services for children and young people with mental health problems. Improve the care and treatment options for those with common mental health problems. Work in conjunction with Social Work and other partners to develop the range of community care settings and options available for those with a severe and enduring mental illness, and so reduce the reliance on hospital care. Support initiatives to improve the physical health of those with a mental illness and ensure consistent and effective standards of physical healthcare and treatment in psychiatric settings. Ensure that inpatient care and treatment is person-centred, safe and effective, and delivered in therapeutic environments appropriate to the patients’ needs. Reduce the length of stay in admission wards and maintain the significant reduction in readmissions through the development and redesign of community services when opportunities arise and through the effective crisis response. Continue the development and delivery of services which ensure early diagnosis, treatment and support for those with dementia. 18 Getting Better in Fife Maintain prompt access to services for those with alcohol and drug problems and, in collaboration with partner agencies, ensure the provision of effective interventions and support. Provide appropriate inpatient and community services for those with forensic mental health needs. Improve the provision of psychiatric liaison services to the general hospitals and review other areas of unmet and emerging need. Why will this improve the patient experience and reduce harm, waste and variation? The following are examples of some key programmes of work which demonstrate anticipated improvements in the patient experience and the reduction of waste, harm and variation: Early intervention for children and young people with mental health problems and developmental disorders is essential to build resilience and prevent problems in later life. We will continue the significant improvements made in pursuit of the CAMHS Waiting Time HEAT Target through service redesign with specific focus on areas with high demand. Improving the access to a range of ‘talking therapies’ for people with common mental health problems is a key element of developing better care and treatment options. We will work towards achieving the Psychological Therapies HEAT Target by focusing on the referral, assessment and treatment arrangements across mental health and psychology services, and the identification of service gaps and the additional training necessary to improve capacity and capability. This will lead to the more efficient use of existing resources and the development of the required skills to provide matched therapies for people requiring a psychological intervention, so reducing waiting times and preventing unnecessary treatments or deteriorating health. The Rehabilitation Redesign Programme is a collaborative project with Social Work designed to develop and provide community care options for people with severe and enduring mental illness currently resident in Stratheden hospital. The programme will ensure patients have the opportunity to maximise their own potential and, with the proper type and level of support, be able to live in a community setting appropriate to their own needs. The physical health of people with mental health problems is a priority for the Scottish Government. Through the development of core care pathways, clinical practice protocols and the skills development of staff we will improve the quality and consistency of physical healthcare and the management of common medical conditions in psychiatric settings. In both hospital and community settings we will support people to make better lifestyle choices and so improve their quality of life and general health. 19 Getting Better in Fife The Scottish Patient Safety Programme-Mental Health alongside Releasing Time to Care and the AHP Realising Potential strategy are key programmes aimed at improving person-centred, safe and effective care and treatment for people with mental health problems, and supporting a recovery based approach. The initial focus on adult acute inpatient care will improve the patient experience by increasing staff engagement with patients and reducing the occurrence of incidents, accidents and adverse events, so reducing the possibility of harm being experienced by individuals in receipt of care from mental health services. The provision of therapeutic facilities and environments which offer privacy and maintain dignity is an essential aspect of good patient care. We will continue to seek improvements in the quality of the mental health estate with the initial focus on developing a proposal for the re-provision of the Intensive Psychiatric Care Unit. Prompt access to specialist services for those with alcohol and drug problems is vital in reducing harm to individuals and their families. We will maintain the delivery of services in line with the Drug and Alcohol Waiting Time and the Alcohol Brief Interventions HEAT Targets in collaboration with partner agencies to improve the treatment options for people, reduce harm and ensure equity of access across Fife. We will develop and provide a Forensic Low Secure inpatient unit on the Stratheden hospital site. This development will ensure NHS Fife better meets its responsibilities for the care and supervision of patients with forensic mental health needs. It will enable Fife patients to be cared for in a local facility, improving the patient experience and service efficiency, and will eliminate the need to purchase services from outside Fife and so realise expenditure savings. 20 Getting Better in Fife 3.7 Safe and Effective Medicines Management Mary’s Story Mary, who is 75 years old and lives in her own home, has a number of chronic health problems and is taking multiple medications. A community pharmacist carried out a review of the number of medications Mary was taking. At the time she was on: 1. A water tablet for high blood pressure 2. An anti-depressant for her low mood 3. An anti-inflammatory painkiller for osteoarthritis 4. Treatment for osteoporosis which the lady was having difficulty swallowing and remembering to take regularly. Mary had a reduced kidney function and a low sodium level. The pharmacist recommended to the GP that Mary should stop her water tablet as this could be causing her low sodium and could increase her risk of having an epileptic seizure. Mary was changed onto another medication for her blood pressure and her sodium level subsequently improved and her blood pressure was well controlled. The pharmacist also recommended that Mary should have her anti-inflammatory painkiller stopped due to her poor kidney function and an alternative paracetamol based painkiller prescribed instead. Furthermore, the combination of the anti-inflammatory with her anti-depressant put her at risk of having a bleed from her stomach or intestines. Mary’s pain control was improved as a result of this change and her risk of having a bleed was significantly reduced. Mary’s osteoporosis treatment was reviewed by the pharmacist who noted that it could also cause problems due to Mary’s reduced kidney function and discussed it with the consultant who had initiated it. An alternative preparation was started which was better tolerated and more suitable for her kidney function. Mary’s community pharmacist was contacted to arrange support to help Mary with compliance of her medication, thus reducing her risk of osteoporosis and hip fracture in the future. What is our aim? Our aim is to ensure that the use of medicines within NHS Fife is safe, clinically effective and cost effective 21 Getting Better in Fife Why will this improve the patient experience and reduce harm, waste and variation? Medicines can make a major contribution to people’s health and healthcare through a variety of mechanisms including curing illness, controlling symptoms and preventing or containing disease. Next to staff, medicines represent the largest area of NHS expenditure. There is evidence that patients experience side effects and other adverse effects from medicines, that resources could be used more efficiently in relation to medicines management and that there is significant variation in the way certain medicines are used by both clinicians and patients. Harm will be reduced by: preventing or minimising side effects and adverse events and the associated problems for patients such as morbidity and increased or prolonged admissions to hospital. improving communication between healthcare professionals in relation to the use of medicines for individual patients particularly when patients are admitted to or discharged from hospital or when their prescribed medicines are changed Waste will be reduced by working with patients and clinicians to: improve compliance with prescribed medicines ensuring that patients derive maximum benefit from their treatments and that there is no unnecessary expenditure on medicines that are unlikely to be effective or which are not being taken. ensure that medicines on repeat prescription are ordered in appropriate quantities and only when needed ensure that when there is a choice of treatments the most cost effective options is prescribed Variation will be reduced by: seeking to identify and explain variations in the way that clinicians prescribe and patients take medicines. promoting use of the Fife Formulary which provides guidance on the best options in terms of both clinical and cost effectiveness. promoting management plans for people on multiple medications to control multiple long terms conditions which are in line with best clinical practice. Medicines and in particular how they are used and how much they cost are the most obvious manifestations of this workstream looking at medicines management but key to effective and efficient use are the underpinning systems and processes. The success of this workstream is dependent on the engagement and leadership of pharmacists working with other clinical colleagues to look at and optimise the flows and processes associated with all aspects of the use of medicines and related products. In parallel with the initiatives outlined above work is also underway to look at how pharmacists can work most effectively with each other and with other clinicians. 22 Getting Better in Fife 3.8 Examples of improvement projects and tests of change Appendix 1 outlines in more detail the worsktreams and projects identified to date under each of the five programmes. A number of these are transformational programmes which focus on improving the quality of service to patients and consequently, will not have an explicit financial impact identified. For example the Falls project under the older people’s programme. There are however, a number of projects which are aligned to the strategic efficiency plan, for example prescribing projects. The timescale for delivery will vary with some projects anticipated to deliver within one year and others to take longer to reach maturity. All, however, are expected to return an incremental benefit throughout the life of the project. 4 IMPROVEMENT APPROACHES “Efficiency without quality is unthinkable. Quality without efficiency is unsustainable”. NHS Fife is adopting two overarching approaches to support the delivery of Getting Better in Fife: Quality Improvement Methodology and the Programme Management Office. The combination of these is intended to ensure that we realise the full quality and efficiency benefits and thus achieve the aim of Improving the Patient Experience through reducing harm, waste, and variation. 4.1 Quality Improvement Methodology Improvement is about continually working together to improve the service user’s experience and outcomes. Mostly we know what we should be doing but consistently applying that knowledge can be difficult. When things go wrong it is normally because there has been a problem in applying knowledge. Most problems happen because of the way things are done, not as a result of who is doing them. Systems need to be improved so that problems are less likely to happen. Recognising the need to improve, having the will and ideas is not enough. We need to ensure that we identify changes that will lead to improvement and effectively deliver them in order to achieve and sustain the desired outcomes. There are many change theories and models but experience tells us that choosing a few and using them consistently is more important than which ones are chosen. However, whichever we chose they should be based on a simple formula. Having a clear aim, an understanding of the changes that need to be made and having measurement embedded will allow us to determine if the changes made are leading to the improvements required which will achieve the aim. 23 Getting Better in Fife NHS Fife has chosen to use the Model for Improvement as the framework to guide our improvement work. The Model for Improvement5 is a simple but effective tool for accelerating improvement and can be used alongside the organisations’ existing change models and other improvement tools and techniques. The Model for Improvement provides a framework for developing testing and implementing changes which lead to improvement. It is based on a scientific method and is the framework used by the Scottish Patient Safety Programme. The framework uses three key questions and a process for testing change ideas. The three questions are What are we trying to accomplish? (The aims statement) How will we know if the change is an improvement? What changes can we make that will result in improvement? Testing the ideas is achieved by using repeated Plan, Do, Study Act (PDSA) Cycles Langley GL, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance (2nd edition). San Francisco: Jossey-Bass Publishers; 2009 5 24 Getting Better in Fife The four stages of the PDSA cycle are Plan - the change to be tested or implemented Do- carry out the test or change Study- data before and after the change and reflect on what was learned Act - plan the next change cycle or full implementation 4.2 Programme Management Office The Programme Management Office (PMO) Is responsible for establishing and managing the operational framework and processes for the development, planning and monitoring of service and financial improvement within NHS Fife. It provides both challenge and support to services engaged in change and improvement processes and the mechanism that supports governance and reporting processes. The PMO approach is the process within which quality improvement, efficiency and service development plans are identified, implemented and monitored to deliver realisable benefits. 5 HOW WILL WE KNOW WHEN CHANGE IS AN IMPROVEMENT 5.1 Measures for Improvement Measures for improvement help us to understand the impact of changes made, share successes when things go well and learn when things don't go so well. There are three parts to the process of quality improvement work where measurement is likely to be most important6 : When identifying issues or opportunities for improvement and those which require our attention; When the improvement team is obtaining baseline measurements and During the tests of change and after they have been implemented The measures are tools for learning and demonstrating improvements, not for judgement. Measures for improvement will be identified for all of the Getting Better in Fife projects to demonstrate whether changes result in improvement. The measures will be reported regularly on time series graphs know as ‘run charts' or statistical process control charts (SPC). 6 Solberg L, Mosser G, McDonald S. The three faces of performance measurement: Improvement, accountability and research. Journal on Quality Improvement Vo 23 (3), 135-147 1997. 25 Getting Better in Fife 6 ALIGNING RESOURCES TO SUPPORT THE PRIORITIES There are a number of key supporting processes and services which are critical to the successful delivery of improvements in the priority areas which have been identified. These include information services, e-health services and workforce development. Agreeing the priorities enables these supporting processes and services to prioritise their work plans accordingly. 6.1 Building Capacity and Capability for Sustainable and Effective Quality Improvement Analysis of health care systems that deliver outstanding performance in cost and quality show that their most common characteristic is a systematic approach to capability building for improvement 7 Therefore critical to our success will be the need to ensure we have the Capacity i.e. having the right number and level of people who are actively engaged and able to support quality improvement and the Capability i.e. ensuring our people have the confidence, knowledge and skills to lead the improvement work. 6.2 Quality Improvement Hub Drawing on the extensive global evidence and the work of the National Quality Improvement Hub we are developing a plan to build capability in quality improvement at all levels of the organisation. The development of the NHS Fife Quality Improvement Hub (QI Hub) is a key step towards this systematic approach to developing capability. The hub is both physical - an Improvement Resource Room which can be used by staff working on the improvement projects aligned to the 5 priority areas and virtual because it harnesses staff talents and skills from across NHS Fife to drive sustainable quality improvement. A small number of people work with the QI Hub all or most of their time; many people work with the QI Hub some of their time. The aim is to provide a 'one-stop shop' for quality improvement support in NHS Fife. This support might be provided through for example; initial diagnosis of the need for improvement support, hands on help with running tests of change, improving leadership and working relationships, mapping and redesigning processes or measurement for improvement. Members of the QI Hub have expertise in Model for Improvement, small tests of change, Lean, measurement for improvement, consulting, coaching, enabling better quality conversations using the practices of ‘dialogue’ as well as other skills. 7 Helen Bevan, How can we build skills to transform the healthcare system? Journal of research in Nursing, 15 (2) 139-148, 201o 26 Getting Better in Fife 7 WHAT DOES THIS MEAN FOR THOSE WE CARE FOR AND OUR STAFF? For the people we care for - our commitment is to develop a culture that is person centred, addressing individual needs and focusing on improving the persons experience. We need to learn from experiences so that we understand what works well and what can be improved. For carers - we want to involve them and value and respect the role that they have as an equal partner For members of the public - it means that we will seek involvement from the outset and work harder to engage the right people in meaningful work. For our staff - we want them to feel good about what they do, that they can improve what they do and feel that their contribution is valued whatever their role in the organisation. We want everyone to be involved in making our services work more efficiently for the benefit not only of patients, but also staff themselves. For our partners- we recognise the contribution that our partners in for example primary care, the council and the third sector play in delivering the quality improvements we are striving to achieve. We will endeavour to facilitate constructive and enthusiastic participation and broad representation from all of our partners where appropriate in the programmes of work within Getting Better in Fife. Improvement is not a one - off we need to do it continuously in order to provide safe, high quality, effective care Getting this right will mean that we will have many more examples of improved experience like the ones reported below. The availability of services to support routine, planned treatments in our community hospitals is improving patient experience. This is David’s story “I was overwhelmed when the new community hospital was available to accommodate me for renal dialysis during my stay. This proved to be a successful visit and very much accessible to me (as I am registered blind). This hospital is spacious and is located in an easy to reach position in the town, something that NHS Fife, I believe, would be rightly proud of. The staff were very professional, cheery and indeed helpful, making my holiday even better than I could have imagined. May I congratulate you on all the hospital staff for enabling this holiday to be pleasurable for me. Their dedication was truly evident.” 27 Getting Better in Fife Julie attended A & E at Victoria Hospital recently on a Sunday afternoon with her son. She wrote to tell us about her experience “A&E was extremely busy and the staff were obviously working flat out yet everyone was brilliant. A member of the ambulance crew saw me waiting to give my details and he came over to make sure my son was o.k. We were taken through almost straight away and seen by the triage staff and then the doctor. It is very reassuring when it is your child that is hurt to feel people care. People are often quick to criticise the NHS, well today you did a great job” Sarah became unwell at home with what appeared to be a chest infection. Her GP contacted the Hospital at Home Team who assessed her that day and decided that she needed to have antibiotics through a drip. Sarah was admitted to Ward 7 at QMH (in the ICASS unit) given antibiotics, assessed by the physiotherapy service and the hospital at home nurse. Sarah was able to go home with the Hospital at Home team (supported by one of the nurses) after 2 days on antibiotics and provided with physiotherapy and home care support immediately. John has Alcohol Related Brain Damage (ARBD) and as a result has a complex range of needs and exhibit s behaviour which can place him at severe risk of harm but this does not necessarily justify long term residential or hospital care. The particular nature of his condition and his needs means that normal community health and social work services are unlikely to be able to provide a successful package of care for him. The mental health service developed a small team of nursing staff to provide an ARBD liaison and support resource. The team are able to co-ordinate the various services that may be required to ensure the optimum package of care and to determine the most appropriate care strategies. This has led to a significant improvement in the quality of life for John and others with similar problems. The work of the team has recently been recognised with them securing the top award at the Scottish Mental Health Nursing Forum Awards event. The development of a “one stop shop” in ophthalmology has brought about real improvements in the patient experience. No longer do delays in the process feature and feedback from patients is very positive. Mrs Bruce is typical of elderly patients attending. She has now had both cataracts removed and enjoys an improved quality of life as a result. She described not having to wait and not having to go back and forward to appointments as a real benefit. 28 Getting Better in Fife Appendix 1 Programme Improving Flow and Emergency Access Work stream Front Door Projects/tests of change Acute Admissions and Speciality Flow Community Flow Implementation of GP ‘hot line’ to senior A&E Doctor with a proposal to provide ‘hotline’ to NHS 24 and SAS Fast track process for patients with minor injuries to decrease overall length of stay in A&E Redirection of patients, who do not require the services that A&E provide, to alternative care providers Focus on achieving 50% of discharge activity before midday Reducing variation in daily discharge numbers Elimination of boarding Reintroduction of discharge lounge Nurse facilitated discharge Improved access to specialty beds Predicted Date of Discharge Increased number of patients who retain their existing care package following an admission to hospital Reduction in waiting time for patients who require a new social work care package Increased number of patient transfers to community hospitals and community teams at the 29 Getting Better in Fife Improving Elective Flow Inpatient/Day case Outpatients and diagnostics Detect Cancer Early weekend and on public holidays Increased number of patients with a Predicated Date of Discharge (PDD) in Community Hospitals Standardisation of nursing documentation across acute and community Increased number of patients discharged before midday in Community Hospitals Optimising waiting list management orthopaedics – in development Reducing Length of Stay for Vascular Patients- test of change –managing patients as a day case rather than inpatients Review and reduction of cancellations of operations on the day – in development Maximising day surgery capacity and 23 hour stay in QMH- underway Telephone clinics- GI nurses- in development Evening clinics- in development Using visual data in outpatients to manage DNA rate- in development Development of accurate utilisation data- underway Roll out of appointment reminder system to community- in discussion Detailed Capacity management – ophthalmology GI Gynaecology E-advice for GPs Direct access to diagnostics- under 30 Getting Better in Fife Reshaping Older Peoples Services Reducing Falls in community and acute hospital in people over 65 ICASS and Hospital at Home Introducing and testing bundles of care to reduce falls specifically a trigger bundle an assessment bundle an intervention bundle a monitoring bundle Safe and Accessible Mental Health Services Safe and Effective Medicines Management discussion Enhanced recovery for Colorectal patients- being developed Electronic referral management for referrals suspicious of cancerunderway Demand and Capacity review and modelling for Colorectal, Lung and Breast sites Early supported discharge – in reach from community teams to VHK and QMH Direct referral and fast track home care assessments for patients in hospital at home virtual ward Referral pathway to ICASS from minor injuries unit at QMH Single points of access Community hospitals Work currently being scoped Patient Safety in Mental Health National Programme of workunder development Improving access to CAMHS and Psychological Therapies Focus on redesign of high demand specialist services and scoping work in psychological therapies Streamlining processes to improve medicines reconciliation and patient flow across primary and secondary care. Work underway to identify 31 Getting Better in Fife Minimising medicines waste and maximising efficiency within the pharmacy service. Work underway to identify Reducing multiple medication use (polypharmacy) in frail elderly people with multiple long term conditions. Work underway to identify Improving patient safety Work underway to identify through the redesign of medicine governance processes (initial priority being safety messages) 32