Parasite
advertisement

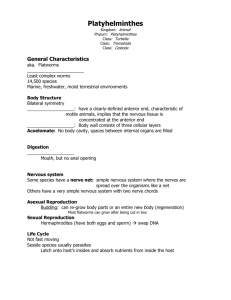
Parasitology Protozoa – Intestinal and Urogenital Entamoeba histolytica Giardia lamblia Cryptosporidium parvum Cyclospora cayatenensis Tissue and Lumen Protozoa Trichomonas vaginalis Pneumocystis carinii Toxoplasma gondii Blood Protozoa Plasmodium P. vivax, P. falciparum, P. malariae Leishmania L. donovani, L. tropica, L. mexicana, L. braziliensis Trypanosoma T. cruzi, T. gambiense, T. rhodesiense Enteric Nematodes (Roundworms) Strongyloides stercoralis Ancylostoma duodenalis and Necator americanus Ascaris lumbricoides Enetrobius vermicularis Bloodstream Trematode (Fluke) Schistosoma S. mansoni S. japonicum, S. haematobium, S. Dermatitis Enteric Cestodes (Tapeworm) Taenia saginata Taenia solium Cysticercosis Echinococcus granulosus Bloodstream Nematodes (Roundworms) Wuchereria bancrofti Brugia malayi Onchocerca volvulus Loa loa Dracunculiasis medinensis 1 Parasitology Parasitic Relationships Parasites Protozoa Metazoa Sarcodina Nemathelminthes Amebas Roundworms Sporozoa Platyhelminthes Sporozoans Flatworms Mastigophora Flagellates Definitions Definitive Host: Intermediate Host: Reservoir Host: Vector: Transport Host: Ciliates Trematoda Cestoda Ciliates Flukes Tapeworms Worms -Harbors Mature Parasite Protozoa –Harbors Sexually Reproducing Stage Worms -Harbors the Immature Parasite Protozoa – Harbors Asexually Reproducing Stage Non-Human host that maintains the infection in nature Transmits parasite from one host to next host Usually a Arthropod – Parasite undergoes obligatory lifecycle development Direct transmission of parasite ie. fecal contamination by flies 2 Parasitology Intestinal Protozoa Parasite Entamoeba Histolytica Forms Epidemiology Protozoa Cysts 8 Trophozoites extracellular Worldwide distribution High risk associated with poor sanitation Transmission/ Pathogenesis Fecal –Oral Contaminated soil and water supplies w/ untreated feces Direct contamination of food w/fingers,flies and cockroaches Transmission Stage Infection acquired by ingestion of the CYST form CYSTS are non-dividing, survives in water and dessication -Rigid cell walls Disease Stage Trophozoites hatch from each cyst and colonize Large Intestine Phagocytic, ingest bacteria, invades tissue, ingested RBC’s Giardia lamblia Trophozoite Cryptosporidium parvum Trophozoite are pearshaped 8 external flagella, two nuclei , parallel axonemes Cysts are oval, four nuclei and pair of axonemes extracelluar Apicomplexan protozoan intracelluar acid fast stain Oocysts – w/4 sporozoites Trophozoite – Tissue sections resembles a trophozoite, but is really a “merozoite” Distribution is worldwide Hi Risk – Poor sanitation U.S. – epidemic and endemic more common Unfiltered surface water in campers, children at day care and male homosexuals Humans -Worldwide Distribution Cattle and Sheep Transmission Ingestion of Cyst form -CYSTS are non-dividing, survives in water and dessication -Rigid cell walls Disease form – Trophozoite in Small Intestine Transmission Fecal-Oral ie. Minneapolis -contamination of city water supplies by water run –off from manured fields following heavy rains Infection by Oocysts (cysts) ingestion – w/4 sporozoites ea. Sporozoites released in Sm. IntestineInfect columnar epithelial cells (sm/lg intestine) Replicates in intracellular membranous sac termed trophozoite (actual merozoite) -Asexual and Sexual cycles -SexualOocytes into feces Clinical Features Diagnosis Amoebiasis Mild diarrhea to fulminating dysentery Mucus, bloody diarrhea Fever, chills, tenesmus (anal sphincter spasm) and constipation Absesses in the intestinal tissue Dissemination – Sites of colonization -Lower right liver lobe (abcesses) -2 Lung an brain ulcers Ova and Parasite Test Stool Samples are tested 3 sequential days Fecal sample is smeared on a glass slide and stained Microscopic examination Ova of worms Cysts/Trophozoites of protozoa CYSTS – Spherical with 4 nuclei Each nuclei: central dot w/dense peripheral chromatin TROPHOZOITES – divide by binary fission, disintegrate in water May contain ingested RBC’s in fecal samples Giardiasis Abdominal discomfort Foul smelling flatulence Mild to Severe Diarrhea Some individuals – Intestinal maladsorption and/or lactose intolerance O & P Test Trophozoites are fragile and difficult to ID even after staining -The two nuclei look like two eyes staring back at you String Test - If Giardiasis is still suspected, duodenal sampling for trophozoites is performed by swallowing string, then pulling out Cryptosporidiosis Diagnosis 1) Healthy Adults – Mild Diarrhea 2) Infants/Immunocompromised Adults WATERY diarrhea, fever, dehydration and weight loss May result in death AIDS – Bloody diarrhea, severe and chronic diarrhea Oocysts in fecal smears w/acid fast stain Serological Tests are NOT available Treatment DRUGS Metronizadole + Diloxanide Furoate = 90% Cure Rate Metronizadole – Lumenal and Systemic Diloxanide Furoate Lumenal Lumenal Drugs Tetracycline, Paromomycin Diloxanide Furoate Systemic Emetine Dehydroemetine Chloroquine Prevention Cysts are inactivated by boiling, filtering and some chemical agents DRUGS Metronizadole -Binds protein and DNA -inhibits RNA/DNA synthesis Prevention Cysts are inactivated by boiling, filtering and some chemical agents No effective drug therapy No vaccine or means of prevention Filter and purify drinking water 3 Parasitology Parasite Cyclospora cayatanensis Forms Epidemiology Apicomplexan parasite Human – worldwide distribution Commonly found in travelers and immunocompromised adults Humans – rare infections -Found in intestinal tract Cyanobacterium Like Body (CLB) Cysts Enterocytozoon and Septata Spores Spiral polar filaments Transmission/ Pathogenesis Clinical Features Diagnosis Fecal- Oral Contaminated Food Diarrhea (up to 6 weeks) Cysts in fecal samples -Round, Stain acid variable and fluoresces blue under UV illumination Fecal- Oral Spores -Spiral polar filaments used to characterize # coils in spore used for classification of generation -Upon infection spiral filaments protrude for penetration MICROSPORIDIOSIS Diarrhea Usually a complication of AIDS Spore in feces or in Sm. Bowel biopsy ID by spore polar filaments -# of spirals indicate generation Treatment 4 Parasitology Tissue and Lumen Protozoa Forms Epidemiology Unicellular , Flagellated Eukaryote Facultative anaerobe Humans Urogenital tract of humans -Vagina and urethra for women -Seminal Vesicle, prostate and urethra for men No intermediate reservoir hosts or sexual stages 25-50% women in US have organism SEXUAL INTERCOURSE Trophozoite transmitted Cannot survive outside of host Extracellular Parasite damages epithelial layer in urogenital tract Normal commensal Causes problems w/very young children or immunosuppressed adults 75% of people have antibodies against Pneumocystis First disease to be diagnosed >>>50% of AIDS cases Intermediate Hosts Humans and other mammals Definitive Hosts Cats – Sexual gametocytes fuse to form oocysts feces Transmission Airborne Spread respiratory droplets Reactivation Latent spores are reactivated and causes disease -Inflammation process w/parasite replication Pneumonia Lung pathology fever, cough, dyspnea, tachypnea Immune response – lose compliance and compromises lungs hypoxia, fxn Sputum specimen Bronchial brushing or bronchial biopsy Transmission Contact w/feline feces Ingestion of infected undercooked meat Transplacental Transmission to human fetus – Only during pregnancy Pathogenesis Specialized structures at end of cell for receptor-mediated invasion inside cell organism w/in phagosome Inhibition of lysozome with phagosome Toxoplasmosis Immunocompetent – asymptomatic Primary infections in immunosuppressed resembling Mononucleosis, disseminated disease or encephalitis Congenital infection –abortion, stillbirth, neonatal disease , seizures, w/encephalitis, chorioretinitis, hepatosplenomegaly, fever, jaundice and intracranial calcifications -Many newborns may be asymptomatic w/manifestations years later Acute and Congenital Diagnosis Immunofluorescence assay for IgM Ab Acute Microscopic stained preps show crescent shapeed trophozoites Cysts may be seen in tissue Cell culture and innoculation into mice Parasite Trichomonas vaginalis Motile Trophozoite 4 anteriior flagella w/5th recurrent flagellum imbedded in membrane NO CYST Pneumocystis carinii Toxoplasma gondii Extracellular Fungi -Not a protozoan Cysts – w/ 8 sporozoites Non-motile and dormant Trophozoites Intracellular Apicomplexa Parasite Oocytes -cat feces Pseudocyst in meat Tachyzoite (liver) Pseudocyst w/Bradyzoites Transmission/ Pathogenesis Clinical Features Vaginitis Most common cause of vaginitis worldwide Women - >>50% symptomatic -Foul smelling, greenish discharge -Burning , itching Men – Most asymptomatic Diagnosis Saline Smear View under microscope Pathogenesis Contact dependent cytoxicity Inflammation of epithelium Hydrogenosome Organelle Proteins needed for cytoxicity Treatment Metronidazole -mixed a amebicide -Inhibit DNA/RNA synthesis -Disulfiram like rxn with ethanol -SE: GI, metallic taste, CNS –dizzy, numb, neuropathy, neurotoxicity **Need to treat both sex partners** -Acid Fast Stain -Silver Stain *able to see the cysts HIV CD4 count <200 treat prophylactically Bactrim (trimethoprimsulfamethoxazole) or aerosol pentamidine DRUGS Pyrimethamine -Drug of choice -Antifolate drug Sulfadiazine + Pyrimethamine Prevention Cook meat thoroughly Pregnant women avoid undercooked meat and cats! 5 Parasitology Blood and Tissue Protozoa Parasite Plasmodium P. vivax P. falciparum P. ovale P. malariae Leishmania L. braziliensis L. mexicana L. tropica L. donovani Forms Apicomplexa Intracellular Parasite Sporozoite Merozoite Schizont Trophozoite Gametocyte Zygotes Oocyte Intracellular Kinetoplastid Protozoa Amastigote Promastigote Epimastigote Trypomastigote Epidemiology Pathogenesis Mosquito Vector – Saliva Asexual Lifecycle Sporozoites in Mosquito biteHuman Liver (hepatocytes)multiply to form Merozoites rupture hepatocytes and invade RBC’sBecomes Trophozoite P. vivax and P. falciparum account for feeds on RBC contentsBecomes a Schizont (16-32 nuclei w/in >>>95% of all cases P. malariae ~4% RBC)Ea. Nucleus w/cytoplasm P. ovale – very rare! pinches off to form new Merozoite RBC ruptures w/new RBC P.vivax –temperate infected Repeat cycle zones, tropics and subtropics Sexual Lifecycle P.falciparum-tropics Some Trophozoites in RBC and subtropics become micro/macrogametocytes Most severe and life release in blood w/rupture of threatening RBCTranfer to feeding Children and elderly mosquitoFertilization of at risk gametesZygotes Oocytes 1000’s SporozoitesMosquito Epidemiology Salivary GlandsBite Host Blacks more susceptible than whites Sickle cell provides protection Geographic Africa, Asia, India, South/Central America 2nd most deadly single human-infectious agent Reservoir Hosts Rodents and Dogs L. braziliensis mucocutaneous/ cutaneous New World L. mexicana cutaneous New World L. tropica cutaneous Old World L. donovani Visceral Old World Clinical Features Malaria (incub 1-3wks) hemolytic anemia, splenomegaly, hepatomegaly, renal damage, GI and superinfection Synchronization of RBC rupture by mature schizonts Temp. reset to 41C, Chills, then Fever, Fever breaks, Sweat glands open and drenching sweat follows Cycle repeats in regular periodicity -P. vivax (48hr) Benign tertian malaria -P. falciparum (48hr ) Malignant tertian malaria -P. ovale (72hr )Benign quartan malaria P. falciparum – Most pathogenic Most deaths esp non-immune individual ~50% mortality Differences include: Infects all RBC’s, level of parasitemia, merozoite asexual reproduction, RBC destruction (O2 for tissues), RBC membrane b/c sticky (knobs) and adhere to endothelial wall plugged capillaries and vessels (cerebral malaria) P. falciparum and P. ovale Chronic –symptoms often disappear Recrudescence – Controllable # parasites remain in bloodstream and reactivate w/trauma/immunosuppressed Relapse –Sporozoites dormant (hypnozoites) in liver and reactivate Leishmaniasis (incub wks to months) Transmission Bite of the Sandfly saliva Lesions Bite Site –Tissue damage due Promastigotes bloodstream to lytic products of dying M’s Cutaneous Disease –Ulcerated Lesions Amastigotes infect M’s – Raised edges, wet/dry crusty center (ingested)-attachment with w/ spontaneous healing in 6-12 months LipoPhosphoGlycan (LPG) Glycoprotein 63kDa (gp63), CMI response and immunity complement receptor on Mucocutaneous Disease – mon-yrs MAmastigotes survive @pH4 later destruction of mid-face Death w/starvation or aspiration Visceral Disease (Kala Azar)– Hi risk to military, travellers, Amastigotes replicate in cells of AIDS pts. reticuloendothelial system Liver, Spleen, BM w/incub wks-yrs -Diurnal fever, hepatosplenomegaly, immunosuppression, wt. Loss, diarrhea, cough, nose bleeds, lymphadenopathy Diagnosis Hemozin –Insoluble product of Hb degradation (heme) You can diagnose w/ presence of malarial pigment – in parasitized cells Blood Smear and stain Signet ring shaped trophozoites P. falciparum gametocytes are crescent shaped Others are spherical Treatment ANTIMALARIAL DRUGS Primaquine (oral) -Tissue schizonticide -Gametocidal (all 4) -Cures only P. vivax and ovale -Hemolytic anemia Chloroquine -Blood schizonticide Quinine -Blood schizonticide Pyrimethamine Chloroguanide Mefloquine -Blood schizonticide -Unknown mechanism -membrane damage -P. faliparum is resistant -CNS effects *Many are drug resistant No vaccine! Diagnosis Visceral Disease L. donovoni Amastigotes in BM, Spleen, Lymph node biopsy specimens Smears or Culturing of WBC’s or BM Visceral Disease Sodium Stibogluconate -IV -inhibition of parasite glycolysis (exact mech. unknown) -Eliminated by urine No vaccine Mucocutaneous/Cutaneous Amastigotes in skin lesions 6 Parasitology Parasite Trypanosma T. gambiense T. rhodesiense Forms Epidemiology Transmission/ Pathogenesis Clinical Features Diagnosis Treatment Trypomastigotes Procyclic Stage Metacyclic Stage T. gambiense – Humans ONLY W.Africa Death – Months/Yrs T. rhodesiense Wild animals (zoonosis) E. Africa Death – Wks/Months Tsetse Fly Bite Short Stumpy trypomastigotes (nondividing) ingested during blood meal of Tsetse FlyMidgut -Procyclic StageMetacyclic trypomastigotes in salivary glandsBite Local multiplication at bite site inflammation Dissemination through bloodstream and lymphatic system parasitemia and antigenic variation Trypanosomiasis –African Sleeping Sickness Chancre at site of bite, weekly fever, lymphadenopathy Myocarditis, Gamma-Globulinemia and generalized immunosuppression Chronic Infection Invasion of CNS-lethargy, personality changes and insomnia Coma due to demyelinating encephalitis headache, insomnia, mood changes, ms tremors, slurred speech, apathy then somnolence, coma Untreated disease is fatal pneumonia Blood smear Culture of blood, lymph or CSF Melarsoprol (IV) -CNS SE -Short t ½ -Hemolytic anemia -SE: hypersensitivity, abdominal pain, vomit -meningoencephalitis Rx for T. gambiense and T. brucei Suramin -prophylactic -inhibits enzymes inhibits nrg metabolism -SE: GI, shock, unconscious, urticaria, neurological Antigenic Variation Allows parasite to evade humoral response Variant Surface Glycoprotein -VSG -10% of parasite protein w/>100genes for Antigenically Different Genes Cyclic fever as result of Ag variation T. brucei Trypanosma cruzi Trypomastigot es Intracellular amastigote Infects Cattle Does Not infect Humans Habitat Humans and animals South and Central America Wild animals in U.S. -No vectors for human infection Infection – Most common in children under 10yrs old Reduviid Bug (Kissing Bug) -Parasite in natural cycle -Transmitted when feces wiped into abraded skin or puncture wound/mucous membranes (eye) -Local replication in M and consquent infiltration of cells and fluid swelling (chagoma) Also transmitted by ingestion, blood transfusions and organ transplants Pathogenesis Amastigotes can kill cells and cause inflammation w/mononuclear cells CHAGA’s Disease – American Trypanosomiasis Acute Disease May last up to 2 months Fever, malaise, lymphadenopathy, splenomegaly, hepatomegaly and myocarditis Amastigotes nests in muscle cells Intermediate Stage No evidence of parasite in blood or disease Chronic Stage Years to decades later Cardiomyopathy, Cardiac Arrythmia, CHF, Megasyndrome (heart, colon, esophagus), Meningoencephalitis in AIDS pts. Pentamidine -T. gambiense nematologic stage only Acute Disease Trypomastigotes in Blood Smears Amastigotes in muscle cells or BM -Bone marrow biopsy or muscle biopsy Nifurtimax -ONLY suppresses does NOT CURE acute Chaga’s disease -SE: CNS, hypersensitivity, GI Chronic Disease Serologically Xenodiagnosis 7 Parasitology Bloodstream Nematodes - Roundworms Parasite Wuchereria bancrofti Forms Epidemiology Transmission/ Pathogenesis Clinical Features Diagnosis Treatment Microfilaria -Sheathed -L1 Larva -L2 Larva -L3 Larva Adult Form Humans are Definitive Hosts Occurs in humid tropic areas with mosquito distribution 200-300million people are infected Female Mosquito Bite Mosquito acquires microfilaria stage L1 larva fr. Bloodmeal Mosquito muscle L2 Larva Salivary Gland L3 Larva Human via bite FILARIASIS Spectrum of Disease dependent on worm burden with pathology due to Death of ADULT worms Asymptomatic w/low level infection igher levels of infection Filarial Fevers, Tropical Pulmonary Eosinophilia & Blocked Lymphatics Fibrosis and calcification around dead adultLymphadenitisLymphangitis (2 infection) distal to node w/trapped adult Acute Fever, Local Edema,Back/Head Aches, Lymph Hydrocele Chyluria- Rupture of Lymph Gland Hydrocele releasing fluids into urine Elephantiasis-Legs, Arm, Scrotum, Breasts (HUGE!) Diagnosis Problem is nocturnal periodicity Provocative Challenge Microfilaria can be induced to migrate from deeper blood vessels to peripheral bloodstream with diethylcarbamizine Diethylcarbamizine -Rapid GI absorption -muscle activity and paralyzes leaving susceptible to host defense -partial metab. elimin. in urine -SE due to dying worms: GI, lymphadenopathy, joint pain, fever, chororetinitis Characteristics Adult worms live in lymph nodes for 5-8 years Females give rise to live microfilaria larva (live 1-2yrs) -Appear in bloodstream with Nocturnal Periodicity (peak 10pm-2am) -Coincides w/mosquito feed time Wuchereria – microfilaria are sheathed w/ NO nuclei in tail Ivermectin Being tested successfully Brugia malayi Same as above Same as above Same as above except: -microfilaria are sheathed with 2 nuclei in tail Same as above Same as above Same as above Onchocerca volvulus Microfilaria -Unsheathed Adult Form Habitat Central Africa – fast rivers Central America-slow rivers Black Fly Bite Adults live as pairs in subcutaneous nodules (10-15yrs) 6-12months after infection Female gives rise to live microfilaria ONCHOCERCIASIS-River Blindness Nodules –Over bony areas such as the head, spine, pelvis and knees C. America – Upper body C. Africa – Lower body (flight height) Diagnosis oscopic observation in skin snips (migration out onto saline) Suramin Disease- Cellular immune response to the DEATH of the Microfilaria Microfilaria (nonsheathed) - Lesions in cornea, iris, Spend 1-2 yrs migrating thru retina causes iritis and corneal keratitis subcutaneous tissue including the – Death in EYES Loa loa thickening of skin and loss of elasticity Loiasis-African Eye Worm Central W. Africa -Sheathed Deep tissue 3-7cm Dracunculiasis medinensis L1 Larvae L3 Larvae Adult 60-100cm Infected copepodingested in Humans unfiltered water then migrates Copepod is vector Africa, India, Pakistan -Ruptured nodule contaminates water copepod ingests L3 travelled route of migration Calabar Swellings (Lasts 2-3 days) Bumping of limb illicits release of irritants from worm (hypersensitivity reaction) Migration over nose is painful Dracunculiases-Guinea Worm Painful Nodules – Adult lives in; lower extremities of leg Nodule eruptsL1 into environment Shock, Unconsciousness, neurological, urticaria Ivermectin –sterilizes females for ~6months *Diethylcarbamizine increases pathology of disease Diagnosis Blood Smear visualization Diethylcarbamazine eliminates microfilaria Surgically removed during passage to eye Head of worm in the skin ulcer Adult is wound out on a stick 2cm/day Prevention –Boiled filtered drinking water 8 Parasitology Enteric Nematodes – Roundworms Parasite Strongyloides stercoralis Angylostoma duodenale Necator americanus (Hookworm) Forms Adult females 2-3mm Adult male Larvae Filarial -infective Rhabditiformnon-infective Epidemiology Transmission/ Pathogenesis Clinical Features Habitat Female worms are embedded in mucosa of duodenum and jejunum Worldwide Warm, humid environments w/poor sanitation and soil is contamninated w/human feces,fecal material for fertilizer approx. 100million infected Transmission Direct contact with soil containing infective larvae Larvae penetrate unbroken skin Direct Cycle Infective larva in soilLarva penetrates skinLarva carried to lung via blooddeveloping larva in sputumAdult worm in GI (swallowed) Noninfective larva in feces Non-Direct Cycle Non-infective larva in soilFree living adult in soileggs in soilnon-infectiveinfective larva in soilPenetrate skinLungSputumGI Non-infective larva in feces Repeat of cycle Autoinfection – Larva in intestine may develop into infective larva, penetrate mucosalungs for another cycle of development STRONGYLOIDIASIS Skin penetration – unnoticed w/low worm burden or local erythema/pruritis Epigastric Pain Diarrhea Urticarial rash (hives) common in chronic infection Loeffler’s Syndrome Coughing, wheezing and transient pulmonary infiltrates Eosinophilia Hyperinfection –Large numbers of larvae transform into infective stages Invade intestine and/or lungs -Severe, bloody diarrhea -Cough, dyspnea, wheezing and hemoptysis Disseminated Strongyloidiasis Migrating larvae in other organs: Liver, Heart, Kidneys or CNS Usually in malnourished or immunosuppressed (AIDS) pts Hi doses of corticosteroids ppt dissemination Habitat Transmission Hookworm Infection Adult 1cm Adult worms attach to Direct contact w/soil containing Erythematous and Pruritic Lesion at Embryo mucosa of duodenum infective larvae penetration site 1st stage larva and proximal small A. duodenale – Infection via Loeffler’s Syndrome Infective larva ingestion of larva w/buccal intestine -Transient pulmonary infiltrates and Life span of cavities that have cutting plates Warm and Moist eosinophilia during lung migration adult is 1-5yrs N. americanis – buccal cavities climate have pairs of teeth Symptoms Regions w/poor Adult Parasite Proportional to Worm Burden Anterior end is sanitation Rural areas up to 90% Life Cycle– Eggs passed in Light infections – GI asymptomatic hooked infection rate stoolDevelop into 1st larvae and Moderate –Epigastric Pain, Diarrhea Specialized hatches w/in 48hrsFeed on and mild Eosinophilia buccal capsules 1/4 of world organic material in soilNonpopulation infected Anemia – secondary to blood loss will for sucking on infective larvaInfective depend on the numbers of worms, intestine mucosa larvaPenetrates skinLung by dietary iron intake and iron stores in pt Males have bloodDeveloping larva in copulatory bursa sputum Swallowed into GI at posterior end Eggs in feces Intestine –Attaches to mucosa and sucks blood, mate in lumen and female lays eggs Diagnosis Diagnosis See Larvae in Fecal Wet Mounts See Larvae in formalinethyl acetate fecal concentrates Serology Elisa will detect Ab, but cannot distinguish present or past infection Treatment Thiabendazole Used to treat very ill side effects microtubule inhibitor and glucose uptake toxicity Nausea, dizzy, vomit, anorexia allergic hepatitis if >2days 2day course Diagnosis O&P 3X Examine Fecal Specimens by concentration techniques -Larvae may hatch in fecal specimens that are not fresh therefore 3X Mebendazole Microtubule disassembly Pyrantel Pamoate Depolarization of neurons blockade Paralysis and expulsion from intestine 9 Parasitology Parasite Ascaris lumbricoides (Giant Round Worm) Forms Epidemiology Transmission/ Pathogenesis Adults Form 20-35cm -Largest intestinal nematodes -Lives up to 1yr -Look like large earthworms Larva Habitat Lumen of Small Intestine Worldwide Poor sanitation Highest rates in areas w/human excreta used for crop fertilization Up to 1 billion infections Transmission Ingestion of embryonated eggs from fecally contaminated food or beverages, fomites or dirty fingers Adult -Female 1cm and have a sharp pointed posterior end like a pin Habitat Adult Worms live in colon, cecum and appendix Worldwide w/high prevalence in school children (20-40%) Most common helminthic infection in U.S. Male Female Enterobius vermicularis (Pinworm) Trichuris trichiura (Whipworm) Habitat Soil Human intestine (colon) Worldwide Clinical Features Ascariasis Lung Phase Larval migration in lung is usually asymptomatic except in heavy infections or in sensitized individuals Pneumonia Life Cycle Loeffler’s Syndrome Embryonated egg in soilEgg Intestinal Phase ingestedLarva hatches and Abdominal Pain penetrates intestineLarva Diarrhea carried to lungDeveloping larva Non-specific GI complaints in sputum and swallowedAdult Intestinal obstruction –esp. heavy worm develops in intestine infections in children Eggs in feces Invasion of Bile Ducts-Liver abscesses, cholangitis, bile duct Female adult deposits >200K obstruction, pancreatitis eggs per day Worms may be vomited or actively migrate up esophagus and out of nasopharynx Mild-Moderate EOSINOPHILIA is common Transmission Enterobiasis Ingestion of eggs from Majority asymptomatic environment Anal pruritus Autoinfection -Fecal-Oral route Vagina pruritis (due to migration) via fingers, etc. NO evidence of causing appendicitis Inhalation of eggs that adhere to mucus membranes and swallowed Life Cycle Embryonated egg in environment or on fingersEgg ingested egg hatches in intestineAdult worm in intestineGravid female migrates to anusEggs deposited on perianal skin Transmission Ingestion of Eggs in soil IntestineImmature adults migrate to colonmate1000’s eggs/dayfeces Mostly asymptomatic Diarrhea Diagnosis Treatment Diagnosis Microscopic detection of eggs in stools -Eggs are brownish in color and bumpy outer coat -infectious after 2-3wks of larval development in eggshell Worms in feces Mebendazole, Pyrantel Diagnosis SCOTCH TAPE applied to anal folds and perianal skin in morning b/f going to bathroom or bathes Microscopic examination of tape for pinworm eggs 3-4X will diagnosis infection 7X consecutive (-) swabs to exclude Treatment Mebendazole and Pyrantel Pamoate in single dose O&P Mebendazole 10 Parasitology Trematodes -Flukes Parasite Forms Epidemiology Transmission/ Pathogenesis Clinical Features Diagnosis Trematodes and Cestodes Adaptations by Trematodes and Cestodes Adhesive organs for attachment to host Anterior suckers or hooks 2) Modifications for obtaining nutrientsAbsorbance thru body wall, specialized ingestion and storage organs 3) Increased reproductive capabilities Evolved larval stages for passage from host to host Schistoma mansoni Cercaria Larva -human infective form Schistosomula -human migratory form Adult -Liver -Live 5-30yrs Eggs Miracidium Larva -Ciliated Snail infective form Habitat Affects GI Tract Definitive Hosts Humans Endemic areas patients 2-30yrs old Infection rare in middle or old age Same as above Affects GI Tract China, Japan, Philippines Affects Urinary Tract Africa, Middle East Found in lakes throughout the world (Trematode) Schistosoma japonicum Schistosoma haematobium Schistosomal Dermatitis Same as above Intermediate Hosts Aquatic Snails Africa, Middle East, Carribean, South America ~200 million people infected 2nd to malaria for infectious deaths ~200K deaths/yr Transmission Fresh water cercaria larva bores under skin Treatment SCHISTOSOMIASIS Itching and dermatitis followed by fever, chills, diarrhea, lymphadenopathy Life Cycle Cercaria Larva hatches fr. Snails Granulomas in liver due to eggs fibrosis, hepatomegaly, portal Bores under skin hypertension (splenomegaly) SchistosomulaMigrate to -Due to Antigens secreted by eggs lymphatics and blood vessels -Hepatocytes are usually undamaged Liver dev. Adult Worms (100Liver function tests remain normal 1000 eggs/day)Portal Veins, Intense Eosinophilia Superior/Inferior Mesen-teric veinsMateEggs work out of Chronic Salmonella Infection Acute hepatitis, Cirrhosis veinsBladder, Intestines Calcified bladder Eggs passed in urine/feces Fresh water Environment devel. Bladder carcinoma Miracidium larvaInfects Neurological Problems (parasites or SnailCercaria Larva and eggs in CNS) released Liver Stages Pathogenesis Hepatosplenomegaly, eosinophilia, and Due to presence of EGGS in in severe cs abdomen becomes filled Liver, Spleen, or Gut/Bladder w/fluid and hepatosplenomegaly Wall Immune Response Ab dependent; CD4 Tcells IgE M, IgE/IgG eosinophils, IgE dependent platelets/mast cells Schistosomula susceptible to immune attack Same as above Same as above Diagnosis Eggs in stool, Blood in stool or Rectal biopsy Praziquantel Calcium permeability and Ab adherence for leukocyte attack Rapid absorption in CSF Short t ½ - liver CNS SE: dizzy, anorexic, malaise, GI Same as above Same as above Same as above Same as above Eggs in urine, blood in urine or bladder biopsy Same as above Bird infective schistosomes Humans are dead end hosts Swimmer’s Itch Rashes from cercaria boring into human skin 11 Parasitology Human Cestodes - Tapeworms Parasite Forms Epidemiology Transmission/ Pathogenesis Clinical Features Diagnosis Treatment Adults –Attachment organ , scolex (four muscular suckers) w/ undifferentiated area behind the scolex. Chain Characteristics of Cestodes Life Cycle: 1. Adult worms always in the intestine of segments behind scolex (proglottids) 2. Eggs or proglottids are excreted in the stool Immature – Contain developing organs 3. Larval development always requires intermediate host Mature – Contain male and female reproductive organs -Eggs are ingested by intermediate host grow to larvae Gravid – Contain eggs in the uterus 4. Definitive host ingests intermediate host tissue w/larvaeAdults in intestine Definitive Hosts Transmission TAENIASIS Diagnosis and Prevention Worm Taenia saginata Adult Differentiation -Scolex or Humans Adult tapeworm causes little damage Cooking beef adequately Ingestion of raw or rare organ with 4 BEEF containing cysticercus Stool Specimen Adult Attached in Most infected pts are asymptomatic Prevent cow from suckers and larvae Morphology of gravid consuming human feces Small Intestine GI complaints – sometimes vague (Beef grooves, no Cattle ingest eggs proglottids in stool sample Worldwide w/high Migration or protrusion of proglottids Tapeworm) hooks contaminating grass or feed -15-20 uterine branches Rx prevalence w/poor from anus Immature Niclosamide sanitation and eating Adult – No hooklets Ingestion of EGGS Cysticercus-Larvae go to small Mature of raw beef Laxative 1st to purge Life Cycle intestine and grow to adult worms eggs form intestine Gravid Eggs or proglottids in -Usually only one adult tapeworm Paromomycin Cysticercus humanIngestion by survives and matures -cystic structure cattlecysticercus in BEEF contains fluid Ingestion of beef by and single humanAdult worm in human inverted scolex intestine Proglottids Definitive Hosts Transmission TAENIASIS Diagnosis and Prevention Adult Worm Taenia solium Differentiation -Scolex or Humans Same as above Cooking pork Ingestion of raw or organ with 4 adequately undercooked PORK Cysticercosis Stool Specimen Adult Attached in suckers and containing cysticercus larvae Morphology of gravid Prevent pigs from Small Intestine (Pork Proglottids- Ingested, carried and grooves, circle proglottids in stool sample consuming human feces Predominant in -Usually only one adult disseminate in organs, EYES and Tapeworm) of hooks -5-10 uterine branches countries where BRAIN Life Cycle Immature Rx undercooked pork is Adults – Circle of hooks Space occupying lesionseizures, Eggs or proglottids in Niclosamide Mature eaten –Mexico, Latin uveitis, retinitis, headache, vomiting humanIngestion by Paromomycin America, Spain, Gravid Disease dependent on locations and pigscysticercus in PORK Portugal, Africa, Cysticercus numbers of cysticerci and host cell Ingestion of pork by -cystic structure India, SE Asia, China humanAdult worm in human response -Rare in U.S. contains fluid intestine and single SEE BELOW FOR MORE INFO Eggs are infectious for inverted scolex humans and may produce Proglottids CYSTICERCOSIS Cysticercosis Diagnosis Treatment Egg Humans are all Source is always human Taenia solium Asymptomatic cysts and accidental intermediate Ingestion of food or beverage Found in all tissues, esp. muscle, CNS, Clinical manifestations Embryo easily controlled seizures hosts eye and subQ tissue contaminated with EGGS Exposure history Cysticercus do not need Rx Nearly all infected pt Person w/infected ADULT may SubQ –stationary subQ masses CT and MRI Scans Cysticercosis Hydrocephalus – CSF are immigrants from disseminate eggs to others and/or Ocular-Occur in aqueous/vitreous humor Serology on serum and shunting procedures infected areas cause autoinfection and interfere with vision CSF Life Cycle Infects all tissues CNS-Cerebral cysticercosis Rx Ingested Eggs hatch in intestine 1. Parenchymal cysts –Seizures, mass Niclosamide Embryo penetrates mucosa 2. Meningeal involvement -Meningitis, BloodstreamSite of CSF obstruction, Hydrocephalus developmentCysticercus 3. Intraventricular cyst -Hydrocephalus Spinal Cysticercosis – Spinal Cord 12 Parasitology Parasite Echinococcus granulosus Forms Epidemiology Transmission/ Pathogenesis Clinical Features Diagnosis Eggs Hydatid Cysts -Larva Adult Worm Embryo Protoscolex Habitat Humans are accidental intermediate hosts Sheep raising areas S. America, Africa, Mediterranean, Middle East, Central Asia, and areas of Australia & New Zealand Foci areas include CA, AZ, NM, Utah, Alaska and Canada Transmission Ingestion of EGGS of parasite from dogs (wolves, foxes, etc) Eggs in dog feces contaminate environmentEgg ingested by sheephydatid cyst in sheep liver Liver fed to dogAdult worm in dog intestineEggs in dog feces ingested by human Hydatid cyst develops Hydatid Disease Hydatid cysts develop most frequently in LIVER -other sites include: lung, brain, kidney, spleen, bone, heart Cysts develop very slowly (1cm/yr) Symptoms due to mass, leakage or rupture, calcification (older cysts) Liver Cysts – Pain when reach lg size Lung Cysts – Asymptomatic and found on chest X-ray Hydatid Cysts – Can become infected with 2 bacterial infection Diagnosis Imaging techniques of ultrasound, CT scans and MRI History of exposure Serologic tests-15% of liver cysts and 50% of lung cysts may have negative serologies Operation and finding hydatid sand (protoscolices, hooks) in fluid Humans are DEAD END hosts Treatment Treatment Surgical removal of accessible cysts is preferred 13 Parasitology Basic Mycology Characteristics Fungi are Eukaryotic Organisms (bacteria are prokaryotes) Chromosomes, mitochondria, nucleus w/membrane Fungal Cell Wall – Complex Polysaccharides, chitin, glucans, mannans, chitosan (bacterial walls are peptidoglycan) Insensitive to antibiotics such as penicillin that inhibits peptidoglycan These structural elements can be stained (See cell wall stains) Fungal Cell Membrane contains ergosterol and zymosterol (humans-cholesterol) Two Types of Fungi: Yeast and Moulds Yeasts Unicellular Reproduce by budding/fission Reproduction by budding is unique Colonies are soft and similar to bacteria Cell Wall Stains 1) PAS – Periodic Acid-Schiff Stain 2) GMS – Gomori’s Methenamine Silver Stain 3) CF – Calcifluor Stain Moulds/Molds Multicellular Reproduce by germination of reproductive structure (into germ tube) -Apical Extension germ tube/filament grows from tip (apex) -Continued extension results in hyphae or network of filaments Hyphae – 1) Septate 2)Nonseptate hyphae-coencytic or multinucleated Mycelium or thallus – Collection of hyphae in a cottony colony Reproduction –Two major ways of reproduction, certain fungi may reproduce, one way or both ways Most fungi of medical interest reproduce asexually ASEXUAL REPRODUCTION 1) Vegetative – Hyphae grow vegetatively and initiate new mycelium with transfer to new medium 2) Asexual Reproduction by Propagules – Anamorphic state and is accomplished by reproductive propagules called conidia or spores depending on their mode of production Conidia - Asexual spores formed from ends/sides of structures A. Arthroconidium-Thallic conidia that grow from entire hyphae by germination and apical extension B. Blastoconidium-Most yeast reproduce by blastic or budding process O O -Pseudohyphae – Blastoconidia sometimes do not separate at maturity but continue to grow and elongate into sausage shaped filaments C. Chlamydoconidium – Thick walled asexual unit arises by thallic process D. Macroconidium/Microconidium – Large and small conidia/spores -Produced blastically and thallically E. Sporangiospore – Spore produced by cytoplasmic cleavage w/in a structure called a sporangium SEXUAL REPRODUCTION Some Fungi reproduce sexually by mating and produce sexual spores -zygospores, ascospores and basidiospores -not used in lab diagnosis Dimorphism Many fungi grow in two morphologically distinct forms at different temperatures Saphrophytic Form – Exist as molds in free- living state at ambient temps Yeast Form – Exist as yeast in host tissues at body temperature Opportunistic Infections Factors that predispose individuals to opportunistic fungal diseases Diabetes Lymphomas Broad Spectrum Antibiotics Immunosuppression (corticosteroid,chemotherapy, etc.) 14 Parasitology Dermatomycosis-Fungal Skin Disease Parasite Dermatophytoses Forms Ringworm Epidermophyton Trichophyton Microsporum Tinea capitis Tinea barbae Epidemiology Transmission/ Pathogenesis Anthropophilic – Only on humans w/dec. conidiation Zoophilic – Mostly on animals and occasionally on humans Geophilic – Found in soil Transmission Direct Contact w/lesions or materials (hair, infected scales) Fomites – Infected material on inanimate objects used by humans (toilet, door handle) Materials Infectious up to 1yr Ringworm/ Dermatophytoses Involve ONLY the non-viable superficial keratinized layer of skin Tinea – Diseases w/defined areas of involvement Pruritic papules, vesicles, broken hairs, thickened, broken nails Very contagious Scalp and Hair Clinical Features Chronic infection of bearded face/neck Ringworm of glabrous/smooth skin Superficial scaling to deep granulomas Jock Strap Itch –Ringworm of the groin, perineum and perianal regions Athlete’s Foot –Feet, toe webs, soles Tinea corporis Tinea cruris Tinea pedis Tinea unguim Nails – difficult to treat Diagnosis Direct Mount Scrapings of skin or nail placed in 10% KOH on a glass slide -See hyphae w/microscope -Patterns of arthroconidial Ectothrix-hyphae surrounds the hair shaft Endothrix- hyphae within the hair shaft Wood’s Light Some Microsporum cause hairs to fluoresce when exposed to UV light (365nm) Usually tinea of cats/dogs Treatment Treatment Anti-fungal creams ORAL GRISEOFULVIN -Ketoconazole Culture Culture on Sabourauds’s Dextrose agar w/antibiotics (chloramphenicol) and antisaprobic mold(cycloheximide) at Room Temp Growth of hyphae and conidia Dermatomycoses Genera Microsporum Macroconidia Spiky Spindle Shaped Thick-walled Born singly (single) Trichophyton Macrocondia Cylindrical Smooth Thin-walled Born singly (single) Epidermophyton Macroconidia Club Shaped Smooth Moderate Thick-walled Borne in clusters of two or three 15 Parasitology Yeast Infections -Opportunistic Mycoses Parasite Candida albicans Forms Epidemiology Transmission/ Pathogenesis Unicellular fungi Predominant Asexual Reproduction Blastoconidium Hyphae Pseudohyphae Zoopthogenic sp. Are commensals of GI, Vaginal and Oral mucosa ENDOGENOUS Usually commensals with source of infection being endogenously precipitated by predisposed events such as: Physiological Change -infancy, pregnancy Traumatic Changes -maceration (skin softened by moisture), post-operative infectxn Malnutrition Malignancy Anemia Antibiotic or Immunosuppressants 70-80% of all yeast infections EXOGENOUS Sexual Contact with Candida infection Clinical Features CANDIDOSIS/CANDIDIASIS Acute or Subacute superficial infection -Skin, nails and mucus membranes Sometimes involve deep seated areas of body Cutaneous Lesions –Lesions resemble dermatophytes Nail infection Clubbing around nail Sites of accumulated moisture Mucous Membranes Thrush –Recurrent Perleche – Corners of mouth due to saliva accumulation Vulvovaginitis – Vagina mucosa, may be contagious CMC- Chronic Mucocutaneous Candidiasis – Pt w/immunological defects in CMI ie. AIDS Repeated attacks, localized w/no spread to deeper organs or tissues Systemic Disseminated Disease – Seen in advanced malignancies (bladder/ bowel cancer) or conditions with NEUTROPENIA C. glabrata C. guilliermondii Cryptococcus neoformans Same as above except: NO hyphae and pseudohyphae Same as above except: REDUCED pseudohyphae SEE PULMONARY MYCOSES Diagnosis Treatment Diagnosis Fluconazole Flucytosine Appearance in Tissue Ketoconazole Exudates – Yeast Cells (blastoconidia) and hyphal elements (pseudohyphae) Appearance in Cultures Soft, Cream colored colonies of unicellular organisms (blastoconidia) Pseudohyphae Germ tubes (C. albicans) true mycelium Germ Tube Test Emerse small portion of isolated colony in serum -Incubate at 37C for 3hrs -Examine for germ tubes Positive = C. albicans CMA- Corn Meal Agar Culture isolate on agar Produces pseudohyphae at room temp. Chlamydoconidia /vesicle formed by C. albicans on CMA Creamy white colony Substrate Assimilation ID by assimilation pattern of carbon sources Does NOT form hyphae or pseudohyphae Forms REDUCED number of pseudohyphae 16 Parasitology Yeast Infections – Opportunistic Mycoses Parasite Cryptococcus neoformans Coccidioides immitis Forms Epidemiology Transmission/ Pathogenesis Clinical Features Diagnosis Oval Budding Yeast NOT Dimorphic Habitat Worldwide C. neoformans var. neoformans – Avian habitat (pigeon) -Only natural form is in debris from Eucalyptus tree C. neoformans var. gattii -Tropical and subtropical Transmission Inhalation of infectious conidia from exogenous source CRYPTOCOCCOSIS Chronic, wasting, frequently fatal disease CNS symptoms Often occurs in immunosuppressed pts -AIDS (4th cause of death in AIDS pt) Growth on Selective Media Biotypes can be distinguished by physical attributes CGB medium Tissue Stain Blastoconidium in capsule India ink for visualization in fluids Habitat Soil of arid or semiarid regions -alkaline soil, hot, dry seasons, no frost w/months of rain New World organism Soil of North, Central and South America 10-15% occur outside endemic area (travel or shipped out) CA – Kern, Tulare, King and Fresno Counties AZ – Maricopa and Pima Counties Transmission Inhalation Not contagious from person to person Dimorphic -MOLD mycelium/ hyphae -SPHERULE spherules w/ endospores Anamorphic Form Encapsulated yeast w/two biotypes -C. neoformans var. neoformans (serotypes A and D) -C. neoformans var. gattii (serotypes B and C) Teleomorphic Form Sexual form of growth Pulmonary Disease Usually subclinical and overlooked Primary infection may disseminate Disseminated Disease Meningitis meninges and brain parenchyma common sites of spread Skin lesions occur in 20% cs of dissemination COCCIDIOIDOMYCOSES (Valley Fever) Primary infection – asymptomatic, subclinical, self-limiting (60% pts) Pulmonary Disease w/various degrees of severity -Influenza like, fever and cough - some lung cavitation -Erythema nodosum (10% of pts)-Red tender nodules on extensor surfaces ie. shin. (DTH rxn to fungal Ag) Disseminated Disease Increased prevalence in non-caucasion population - in Filipino population Small % of pts chronic or acute malignant disease that involves every tissue and organ system in body Culture Mucoid colonies (looks like snot) w/ encapsulated yeast cells seen w/india ink Melanin deposits w/certain catecholamines in growth media (ie thistle seed agar) Dimorphism Room Temperature – mycelium w/hyphae forming arthroconidia (highly infectious) 37C consists of large spherules w/small endospores Tissue Appearance Endospore filled Spherule Tissue or Exudates (CSF, Sputum, Pus) Culture Spherules hard to culture Room Temp cultures used Antibody Tests Ag – IgM,G,A,E classes Tube Preciptin Ab –IgM isotype early in symptomatic illness Complement Fixation Test (CF) IgG Ab produced later in infection titer Titer correlates w/severity 1:16 1 disease, 1:32 severe *note: CNS sole area of involvement titers are 1:16 (low) Treatment Rx Ketoconazole Fluconazole meningoencephalitis Diagnosis cont’d Serological Tests Latex Agglutination w/Ab attached to beads CSF, Urine, Serum Immunity to reinfection (+) Skin test indicates previous infection and immune to 2nd attack of disease Rx Fluconazole Ketoconazole 17 Parasitology Parasite Forms Histoplasma capsulatum Facultative intracellular parasite Dimorphic Yeast Mold Asexual Spores macroconidia microconidia Epidemiology Transmission/ Pathogenesis Clinical Features Diagnosis Habitat Soil contaminated w/bird droppings Chicken, Starling and Bats (disease found only in birds) Zoogenic (dogs, cats, mice, rats,etc can be infected) Worldwide w/concentration in U.S. -Ohio, MO, Missippi Transmission Inhalation of spores and M engulfdevelop into yeast form Not contagious from person to person HISTOPLASMOSIS Asymptomatic and Subclinical (95%) Pulmonary Infection -Influenza-like, fever and congestion Cavitation of lungCalcification of small granulomatous foci in lung and spleen Pneumonia Appearance in Tissue Oval budding Yeast cells found in M w/in tissue -Tissue biopsy -BM aspirates Dimorphism Mold (saprophytic form) in soil/Room Temperature -hyphae form w/mycelium -macroconidia -Infectious Element -Small Spherical MICROCONIDIA Ovoid budding Yeast (parasitic form) in tissue/37C -blastoconidium Disseminated Disease Progressive and involves cells in : Liver, Spleen and Lymph Nodes Hepatosplenomegaly Usually immunosuppressed CMI and infants Appearance in Culture Room TemperatureHyphae and mycelium w/micro and macroconidia -Microconidia are infectious C converts yeast form Treatment Ketoconazole -fungicidal and fungistatic Fluconazole -disseminated histoplasmosis Serological Tests Complement Fixation (CF) -titer of 1:32 -X-reactions occur (ie Blastomyces) Immunodiffusion (ID) -ppt Ab form 2 bands on agar assay RIA’s DNA/RNA Hybridization Blastomyces dermatitidis Dimorphic Mold Yeast -round w/ single broad-based bud Conidia Habitat Moist, rich soil in organic material Infects humans and animals (note dogs) Worldwide distribution Males outnumber females 10 to 1 Transmission Inhalation of conidia Not contagious from person to person Dimorphism Mold at Room Temperature w/ mycelium and hyphae -Ovoid conidia (Infectious Element) Yeast at 37C – Blastoconidia w/thick walls, wide base w/budding daughter cells Teleomorphic form of growth Blastomyces Pulmonary infection (1st stage) -Asymptomatic or subclinical -Self-limiting, but frequency than histoplasmosis and coccidioidomycosis Chronic Infection Chronic infectio of skin w/suppurative granulomas that heal spontaneously or w/therapy -Foot, Leg and Face Pronounced Scar formation Indolent form – recurrent for many yrs Tissue Appearance Tissue Biopsy Large solitary yeast cells embedded in abscesses w/single broad-based buds attached to mother cell Thick walls and not intracellular -Sometimes seen in giant cells Culture Appearance White mycelium-hyphae w/single lateral conidia Pentamidine 18 Parasitology Opportunistic Fungal Diseases Parasite Aspergillus fumigatus A. Flavus A. terreus A. niger Cryptococcus neoformans Candida albicans (sp.) Forms Epidemiology Molds ONLY conidia conidiophore septate hyphae Habitat Grow on decaying vegetation Worldwide affecting all ages and sexes Immunocompromised Hosts Transmission/ Pathogenesis Transmission Airborne Conidia Inhalation Ingestion Abraded Skin Clinical Features Diagnosis ASPERGILLOSIS Allergic Bronchopulmonary Aspergillosis Induction of allergies (DTH) Asthmatic Symptoms –IgE mediated Tissue Invasion Infectious Invasion of Tissues Grow in lung pulmonary cavitation (from other disease processes, ie TB) Fungus Ball – seen on CXR Hemoptysis and granulomas Toxin Toxins contaminate feed or food Toxemia Grow on rice, cereals, nuts producing aflatoxins that may be carcinogenic and/or toxic Disseminated Disease Immunocompromised Hosts Skin, CNS, heart, lung, nasal-orbital area, cornea Culture Fast growing, flat, velvety, bluish green colony Brown w/aging Physical appearance of chains of enteroblastic phialoconidia produced by one row of phialides pointing upward from upper part of vesicle (in other words it looks like a Hairy Q-tip) Treatment Tissue Appearance Septate hyphae that branch at acute angles See Pulmonary Mycoses See Yeast Infections *Note: Opportunistic Fungi fail to induce disease in most normal persons, but may do so in those with impaired host defenses 19