[4] Sir Bernard Katz was a winner of the Nobel Prize in
advertisement
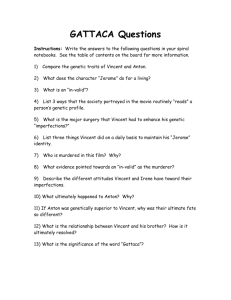
![[4] Sir Bernard Katz was a winner of the Nobel Prize in](http://s3.studylib.net/store/data/008497748_1-b579adfb19d570e6b37c2ad850d1a0d8-768x994.png)
Supplementary Data CV, Publications and Recollections A. B. C. D. E. F. G. H. I. J. K. Curriculum vitae Publications Interview with JND by Barbara W. Sommer for the American Neurological Association in 2003 Early Years by Julia Medd (twin sister)* National Service in the RAF by Commander Dayne Markham Neurology, ABN and Brain by Alastair Compston* Research and Oxford by Angela Vincent* Retirement and the Thymectomy Trial by Gary Cutter* Mentor and Clinician by Camilla Buckley* Patients’ Recollections collated by Michael Burrows Excerpt from “John Newsom-Davis 1932–2007” by Nick Willcox (Journal of Neuroimmunology, 2008) * Taken from John Newsom-Davis. A Commemoration. Royal College of Physicians, 31st March 2008. A. Curriculum vita John Newsom-Davis CBE MD DM FRCP FRS Curiculum Vitae 2007 Married; 3 children National Military Service: Degrees: Royal Air Force (Pilot), 1951-1953 BA in Natural Sciences, University of Cambridge 1957 MB, BChir University of Cambridge 1960 MD (University of Cambridge) 1966 DM (University of Oxford) 1987 Honours/Distinctions: Commander of the British Empire, 1996 Fellow of the Royal College of Physicians, 1973 Fellow of the Royal Society, 1991 Foreign Associate Member, Institute of Medicine, National Academy of Sciences, USA 2001 Prizes/Awards: Queen Square Prize in Neurology, 1965 Jean Hunter Prize, Royal College of Physicians, 1986 Moxon Medal, Royal College of Physicians, 1996 Swedish Medical Society Medal, 1999 Association of British Neurologists Medal, 1999 Galen Medal, Worshipful Society of Apothecaries, 2004 Gaetano Conte Prize, 2007 Present Appointments: Professor Emeritus, Department of Clinical Neurology, University of Oxford,1998Honorary Consultant Neurologist, Radcliffe Infirmary, Oxford, 1998(Outpatient and Inpatient care for patients with neuromuscular disorders) Previous Appointments: Resident House Physician, Academic Registrar and Resident Medical Officer, National Hospital for Nervous Diseases, Queen Square, 1966-1968 University Lecturer, Institute of Neurology, Queen Square, 1968-1969. Research Fellow, Department of Neurology (Dr Fred Plum), New York Hospital-Cornell Medical Center, 1969-1970. Consultant Neurologist, Royal Free Hospital and National Hospital for Nervous Diseases, Queen Square, 1970-1980. MRC Clinical Research Professor of Neurology, Royal Free Hospital School of Medicine and Institute of Neurology, Queen Square, 1980-1987. Professor of Clinical Neurology, University of Oxford, 1987-1998 Editor-in-Chief Brain, 1997-2004 Medical Research Council: Member of Neurosciences Grants Committee, 1978-1980 Member of Neurosciences Board, 1980-1983; 1992-96 Chairman of Neurosciences Board, 1983-1985 Chairman of Health Services Research Committee, 1986-1987 Member of Council, 1983-1987 Chairman of Neurosciences Human Health Steering Committee, 1992-1995 2 Department of Health: Member of the Central Research and Development Committee, 1994 Consultant Adviser in Neurology to Chief Medical Officer, 1994-96 Royal Society: Member of Council, 1996-97 Member of Finance and General Purposes Committee 1998Royal College of Physicians: Member of Committee on Neurology, 1981-1985 Chairman of Committee on Neurology, 1985-1992 British Association for the Advancement of Science: President of the Biomedical Section, 1982-1983 University of Oxford: Member of the Board of the Faculty of Clinical Medicine, 1990-1993 Chairman of the Animal Care Committee, 1991-94 Member of the Biosciences Research Board, 1993-96 Delegate of Oxford University Press, 1994-1999 British Council: Chairman, Health Advisory Committee, 1995-2000 Muscular Dystrophy Group: Member of Medical Research Committee, 1984-1995 Chairman of Medical Research Committee, 1996-1999 Brain: Chairman, Guarantors of Brain, 1991-1996 Editor-in-Chief, 1997-2004 Present or past Editorial work: Editorial Boards of Revue Neurologique, Journal of Neuroimmunology, Journal of Neurological Sciences, European Neurology, Muscle and Nerve, Current Opinion in Neurology & Neurosurgery, Journal of Neurology Neurosurgery and Psychiatry, Clinical and Experimental Immunology, Brain. Manuscript reviews for other scientific journals including American Journal of Pathology, Annals of Neurology, Brain, Lancet, Nature, New England Journal of Medicine etc. Association of British Neurologists: Honorary Secretary, 1981-1984 Member of Council, 1997-2001 President Elect, 1997-1999 President, 1999-2001 Scientific Societies and Associations Honorary Member of the American Academy of Neurology Honorary Member of the American Neurological Association Honorary Member of the Association of British Neurologists Honorary Member of the Australian Association of Neurologists Honorary Member of the Association of Physicians, UK Honorary Fellow of the Royal Society of Medicine Corresponding Member of the Swiss Neurological Society Ad hoc Reviews: 3 Medical Research Council, UK National Fund for Research into Crippling Disease, UK Wellcome Trust, UK National Health and Medical Research Council, Australia National Science Foundation USA Recent Named Lectures Robert Aird Lecture, San Francisco, 1989 Milton Shy Lecture, New York/Philadelphia/Washington, 1991 Henry Fuller Lecture, St George’s Hospital Medical School, June 1992 Lord Adrian Lecture, International Congress of Clinical Neurophysiology, Jerusalem, June 1992 Soriano Lecture, American Neurological Association, Boston, October 1993 Lambert Lecture, American Association of Electrodiagnostic Medicine, New Orleans, October 1993 Hughlings Jackson Lecture, Royal Society of Medicine, December 1993 Myasthenia Gravis Foundation Lecture, Salt Lake City, April 1995 Norman Allen Lecture, Columbus, Ohio, November 1995 6th Seah Cheng Siang Memorial Lecture, Singapore, January 1996 Gordon Holmes Lecture, Sydney, Australia, May 1997 Ellison-Cliffe Lecture, Royal Society of Medicine, October 1997 Oh Lecture, Birmingham, Alabama, November, 1997 FE Bennett Lecture, American Neurological Association, Montreal, Oct 1998 Association of British Neurologist Medallist Lecture, March 1999. Alan Emery Lecture, Green College, Oxford, June 2000 Dale McFarlin Lecture, International Society for Neuroimmunology, Edinburgh, September 2001 Wartenberg Lecture, American Academy of Neurology, Honolulu, April 2003 Robert A Fishman Lecture, San Francisco, June 2005 Benjamin Boshes Lecture, Tel Aviv, December 2005 Gaetano Conte Lecture, Djerba, March 2007 4 B. Publications Book Campbell EJM, Agostini E, Newsom Davis J (eds) 1970. The respiratory muscles. Lloyd-Luke, London. All peer-reviewed and selected scientific reviews. Note that in early publications his name is given as JN Davis 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. Davis JN. Contribution of somatic receptors in the chest wall to detection of added inspiratory airway resistance. Clin Sci. 1967;33:249-260 Davis JN. Phrenic nerve conduction in man. J Neurol Neurosurg Psychiatry. 1967;30:420-426 Davis JN. An experimental study of hiccup. Brain. 1970;93:851-872 Davis JN, Sears TA. The proprioceptive reflex control of the intercostal muscles during their voluntary activation. J Physiol. 1970;209:711-738 Davis JN, Plum F. Separation of descending spinal pathways to respiratory motoneurons. Exp Neurol. 1972;34:78-94 Davis JN. Autonomous breathing. Report of a case. Arch Neurol. 1974;30:480-483 Harvey PK, Davis JN. Traumatic encephalopathy in a young boxer. Lancet. 1974;2:928-929 Davis JN. The response to stretch of human intercostal muscle spindles studied in vitro. J Physiol. 1975;249:561-579 Davis JN, Stagg D. Interrelationships of the volume and time components of individual breaths in resting man. J Physiol. 1975;245:481-498 Davis J, Goldman M, Loh L, Casson M. Diaphragm function and alveolar hypoventilation. Q J Med. 1976;45:87-100 Davis JN, Loh L, Casson M. The effects of respiratory muscle weakness on the pattern of breathing. Acta Neurol Belg. 1976;76:291-292 Maton PN, Pollard JD, Davis JN. Human rabies encephalomyelitis. Br Med J. 1976;1:1038-1040 Gibson GJ, Pride NB, Davis JN, Loh LC. Pulmonary mechanics in patients with respiratory muscle weakness. Am Rev Respir Dis. 1977;115:389-395 Loh L, Goldman M, Davis JN. The assessment of diaphragm function. Medicine (Baltimore). 1977;56:165169 Davis JN, Loh L, Nodal J, Charnock M. Effects of sleep on the pattern of CO2 stimulated breathing in males and females. Adv Exp Med Biol. 1978;99:79-83 Hughes RA, Newsom-Davis JM, Perkin GD, Pierce JM. Controlled trial prednisolone in acute polyneuropathy. Lancet. 1978;2:750-75 Pinching AJ, Peters DK, Davis JN. Plasma exchange in myasthenia gravis. Lancet. 1977;1:428-429 Ito Y, Miledi R, Vincent A, Newsom-Davis J. Acetylcholine receptors and end-plate electrophysiology in myasthenia gravis. Brain. 1978;101:345-368 Newsom-Davis J, Pinching AJ, Vincent A, Wilson SG. Function of circulating antibody to acetylcholine receptor in myasthenia gravis: investigation by plasma exchange. Neurology. 1978;28:266-272 Stagg D, Goldman M, Davis JN. Computer-aided measurement of breath volume and time components using magnetometers. J Appl Physiol. 1978;44:623-633 Stranock SD, Davis JN. Ultrastructure of the muscle spindle in dystrophia myotonica. II. The sensory and motor nerve terminals. Neuropathol Appl Neurobiol. 1978;4:407-418 Stranock SD, Davis JN. Ultrastructure of the muscle spindle in dystrophia myotonica. I. The intrafusal muscle fibres. Neuropathol Appl Neurobiol. 1978;4:393-406 Vincent A, Scadding GK, Thomas HC, Newsom-Davis J. In-vitro synthesis of anti-acetylcholine-receptor antibody by thymic lymphocytes in myasthenia gravis. Lancet. 1978;1:305-307 Davis JN, Loh L. Alveolar hypoventilation and respiratory muscle weakness. Bull Eur Physiopathol Respir. 1979;15 Suppl:45-53 Loh L, Hughes JM, Davis JN. Gas exchange problems in bilateral diaphragm paralysis. Bull Eur Physiopathol Respir. 1979;15 Suppl:137-143 Molenaar PC, Polak RL, Miledi R, Alema S, Vincent A, Newsom-Davis J. Acetylcholine in intercostal 5 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. muscle from myasthenia gravis patients and in rat diaphragm after blockade of acetylcholine receptors. Prog Brain Res. 1979;49:449-458 Newsom-Davis J. The diaphragm and neuromuscular disease. Am Rev Respir Dis. 1979;119:115-117 Newsom-Davis J, Wilson SG, Vincent A, Ward CD. Long-term effects of repeated plasma exchange in myasthenia gravis. Lancet. 1979;1:464-468 Vincent A, Newsom-Davis J. Absence of anti-acetylcholine receptor antibodies in congenital myasthenia gravis. Lancet. 1979;1:441-442 Compston DA, Vincent A, Newsom-Davis J, Batchelor JR. Clinical, pathological, HLA antigen and immunological evidence for disease heterogeneity in myasthenia gravis. Brain. 1980;103:579-601 Vincent A, Newsom Davis J. Anti-acetylcholine receptor antibodies. J Neurol Neurosurg Psychiatry. 1980;43:590-600 Hawkey CJ, Newsom-Davis J, Vincent A. Plasma exchange and immunosuppressive drug treatment in myasthenia gravis: no evidence for synergy. J Neurol Neurosurg Psychiatry. 1981;44:469-475 Lang B, Newsom-Davis J, Wray D, Vincent A, Murray N. Autoimmune aetiology for myasthenic (EatonLambert) syndrome. Lancet. 1981;2:224-22 Molenaar PC, Newsom-Davis J, Polak RL, Vincent A. Choline acetyltransferase in skeletal muscle from patients with myasthenia gravis. J Neurochem. 1981;37:1081-1088 Murray NM, Newsom-Davis J. Treatment with oral 4-aminopyridine in disorders of neuromuscular transmission. Neurology. 1981;31:265-271 Newsom-Davis J, Willcox N, Calder L. Thymus cells in myasthenia gravis selectively enhance production of anti-acetylcholine-receptor antibody by autologous blood lymphocytes. N Engl J Med. 1981;305:13131318 Newsom-Davis J, Willcox N, Scadding G, Calder L, Vincent A. Anti-acetylcholine receptor antibody synthesis by cultured lymphocytes in myasthenia gravis: thymic and peripheral blood cell interactions. Ann N Y Acad Sci. 1981;377:393-402 Scadding GK, Vincent A, Newsom-Davis J, Henry K. Acetylcholine receptor antibody synthesis by thymic lymphocytes: correlation with thymic histology. Neurology. 1981;31:935-943 Vincent A, Cull-Candy SG, Newsom-Davis J, Trautmann A, Molenaar PC, Polak RL. Congenital myasthenia: end-plate acetylcholine receptors and electrophysiology in five cases. Muscle Nerve. 1981;4:306-318 Greenwood R, Newsom-Davis J, Hughes RA, Aslan S, Stott RB, Bowden AN, Chadwick DW, McLellan DL, Millac P, Gordon NS, Armitage P. British multicentre trial of plasma exchange in acute inflammatory polyradiculoneuropathy (AIP). Prog Clin Biol Res. 1982;106:189-196 Lang B, Vincent A, Newsom-Davis J. Purification of anti-acetylcholine receptor antibody from patients with myasthenia gravis. J Immunol Methods. 1982;51:371-381 Molenaar PC, Newsom-Davis J, Polak RL, Vincent A. Eaton-Lambert syndrome: acetylcholine and choline acetyltransferase in skeletal muscle. Neurology. 1982;32:1061-1065 Newsom-Davis J, Murray N, Wray D, Lang B, Prior C, Gwilt M, Vincent A. Lambert-Eaton myasthenic syndrome: electrophysiological evidence for a humoral factor. Muscle Nerve. 1982;5:S17-20 Thomas JA, Willcox HN, Newsom-Davis J. Immunohistological studies of the thymus in myasthenia gravis. Correlation with clinical state and thymocyte culture responses. J Neuroimmunol. 1982;3:319-33 Vincent A, Newsom-Davis J. Acetylcholine receptor antibody characteristics in myasthenia gravis. II. Patients with penicillamine-induced myasthenia or idiopathic myasthenia of recent onset. Clin Exp Immunol. 1982;49:266-272 Vincent A, Newsom-Davis J. Acetylcholine receptor antibody characteristics in myasthenia gravis. I. Patients with generalized myasthenia or disease restricted to ocular muscles. Clin Exp Immunol. 1982;49:257-265 Fukunaga H, Engel AG, Lang B, Newsom-Davis J, Vincent A. Passive transfer of Lambert-Eaton myasthenic syndrome with IgG from man to mouse depletes the presynaptic membrane active zones. Proc Natl Acad Sci U S A. 1983;80:7636-7640 Lang B, Newsom-Davis J, Prior C, Wray D. Antibodies to motor nerve terminals: an electrophysiological study of a human myasthenic syndrome transferred to mouse. J Physiol. 1983;344:335-345 Lerrick AJ, Wray D, Vincent A, Newsom-Davis J. Electrophysiological effects of myasthenic serum factors studied in mouse muscle. Ann Neurol. 1983;13:186-191 Scadding G, Newsom-Davis J. D-pen associated MG. Muscle Nerve. 1983;6:170-171 Scadding GK, Calder L, Newsom-Davis J. The in vitro effects of D-penicillamine upon anti-AChR 6 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. 65. 66. 67. 68. 69. 70. 71. 72. 73. 74. 75. production by thymic and peripheral blood lymphocytes from patients with myasthenia gravis. Muscle Nerve. 1983;6:656-660 Scadding GK, Sweny P, Wilson SG, Havard CW, Newsom-Davis J. Glomerulonephritis, thymoma and myasthenia gravis. Q J Med. 1983;52:187-193 Vincent A, Newsom-Davis J, Newton P, Beck N. Acetylcholine receptor antibody and clinical response to thymectomy in myasthenia gravis. Neurology. 1983;33:1276-1282 Whiting PJ, Vincent A, Newsom-Davis J. Acetylcholine receptor antibody characteristics in myasthenia gravis. Fractionation of alpha-bungarotoxin binding site antibodies and their relationship to IgG subclass. J Neuroimmunol. 1983;5:1-9 Willcox HN, Newsom-Davis J, Calder LR. Greatly increased autoantibody production in myasthenia gravis by thymocyte suspensions prepared with proteolytic enzymes. Clin Exp Immunol. 1983;54:378-386 Wilson S, Vincent A, Newsom-Davis J. Acetylcholine receptor turnover in mice with passively transferred myasthenia gravis. II. Receptor synthesis. J Neurol Neurosurg Psychiatry. 1983;46:383-387 Wilson S, Vincent A, Newsom-Davis J. Acetylcholine receptor turnover in mice with passively transferred myasthenia gravis. I. Receptor degradation. J Neurol Neurosurg Psychiatry. 1983;46:377-382 Colaco CB, Scadding G, Newsom-Davis J. Anti-cardiolipin antibodies in neurological diseases. Lancet. 1984;1:164 Greenwood RJ, Newsom-Davis J, Hughes RA, Aslan S, Bowden AN, Chadwick DW, Gordon NS, McLellan DL, Millac P, Stott RB, et al. Controlled trial of plasma exchange in acute inflammatory polyradiculoneuropathy. Lancet. 1984;1:877-879 Lang B, Molenaar PC, Newsom-Davis J, Vincent A. Passive transfer of Lambert-Eaton myasthenic syndrome in mice: decreased rates of resting and evoked release of acetylcholine from skeletal muscle. J Neurochem. 1984;42:658-662 Newsom-Davis J, Murray NM. Plasma exchange and immunosuppressive drug treatment in the LambertEaton myasthenic syndrome. Neurology. 1984;34:480-485 Willcox HN, Newsom-Davis J, Calder LR. Cell types required for anti-acetylcholine receptor antibody synthesis by cultured thymocytes and blood lymphocytes in myasthenia gravis. Clin Exp Immunol. 1984;58:97-106 Bofill M, Janossy G, Willcox N, Chilosi M, Trejdosiewicz LK, Newsom-Davis J. Microenvironments in the normal thymus and the thymus in myasthenia gravis. Am J Pathol. 1985;119:462-473 Klavinskis LS, Patterson S, Whiting PJ, Wilcox HN, Oxford JS, Newsom-Davis J. Infection of cultured human muscle cells by influenza virus. J Gen Virol. 1985;66 ( Pt 11):2335-2345 Klavinskis LS, Willcox N, Oxford JS, Newsom-Davis J. Antivirus antibodies in myasthenia gravis. Neurology. 1985;35:1381-1384 Lang B, Roberts AJ, Vincent A, Newsom-Davis J. Anti-acetylcholine receptor idiotypes in myasthenia gravis analysed by rabbit anti-sera. Clin Exp Immunol. 1985;60:637-644 Newsom-Davis J. Lambert-Eaton myasthenic syndrome. Springer Semin Immunopathol. 1985;8:129-140 Powell-Jackson J, Weller RO, Kennedy P, Preece MA, Whitcombe EM, Newsom-Davis J. CreutzfeldtJakob disease after administration of human growth hormone. Lancet. 1985;2:244-246 Prior C, Lang B, Wray D, Newsom-Davis J. Action of Lambert-Eaton myasthenic syndrome IgG at mouse motor nerve terminals. Ann Neurol. 1985;17:587-59 Robb SA, Bowley TJ, Newsom-Davis J. Variation in peripheral blood T cell subsets in serial assays. Immunol Lett. 1985;10:133-136 Robb SA, Bowley TJ, Willcox HN, Newsom-Davis J. Circulating T cell subsets in the Lambert-Eaton myasthenic syndrome. J Neurol Neurosurg Psychiatry. 1985;48:501-505 Robb SA, Vincent A, McGregor MA, McGregor AM, Newsom-Davis JM. Acetylcholine receptor antibodies in the elderly and in Down's syndrome. J Neuroimmunol. 1985;9:139-146 Roberts A, Perera S, Lang B, Vincent A, Newsom-Davis J. Paraneoplastic myasthenic syndrome IgG inhibits 45Ca2+ flux in a human small cell carcinoma line. Nature. 1985;317:737-739 Vincent A, Newsom-Davis J. Acetylcholine receptor antibody as a diagnostic test for myasthenia gravis: results in 153 validated cases and 2967 diagnostic assays. J Neurol Neurosurg Psychiatry. 1985;48:12461252 Vincent A, Newsom-Davis J. Acetylcholine receptor antibody characteristics in myasthenia gravis. III. Patients with low anti-AChR antibody levels. Clin Exp Immunol. 1985;60:631-636 Whiting P, Vincent A, Newsom-Davis J. Monoclonal antibodies to Torpedo acetylcholine receptor. Characterisation of antigenic determinants within the cholinergic binding site. Eur J Biochem. 7 76. 77. 78. 79. 80. 81. 82. 83. 84. 85. 86. 87. 88. 89. 90. 91. 92. 93. 94. 95. 96. 97. 98. 1985;150:533-539 Willcox N, Demaine AG, Newsom-Davis J, Welsh KI, Robb SA, Spiro SG. Increased frequency of IgG heavy chain marker Glm(2) and of HLA-B8 in Lambert-Eaton myasthenic syndrome with and without associated lung carcinoma. Hum Immunol. 1985;14:29-36 Willcox N, Schluep M, Bofill M, Newsom-Davis J. Isolation of germinal centre (GC) cells is greatly improved by using the protease dispase to prepare cell suspensions. Adv Exp Med Biol. 1985;186:979-984 Klavinskis LS, Willcox HN, Richmond JE, Newsom-Davis J. Attempted isolation of viruses from myasthenia gravis thymus. J Neuroimmunol. 1986;11:287-299 Mossman S, Vincent A, Newsom-Davis J. Myasthenia gravis without acetylcholine-receptor antibody: a distinct disease entity. Lancet. 1986;1:116-119 Scadding GK, Calder L, Vincent A, Prior C, Wray D, Newsom-Davis J. Anti-acetylcholine receptor antibodies induced in mice by syngeneic receptor without adjuvants. Immunology. 1986;58:151-155 Whiting PJ, Vincent A, Newsom-Davis J. Myasthenia gravis: monoclonal antihuman acetylcholine receptor antibodies used to analyze antibody specificities and responses to treatment. Neurology. 1986;36:612-617 Whiting PJ, Vincent A, Schluep M, Newsom-Davis J. Monoclonal antibodies that distinguish between normal and denervated human acetylcholine receptor. J Neuroimmunol. 1986;11:223-235 Chiu HC, Vincent A, Newsom-Davis J, Hsieh KH, Hung T. Myasthenia gravis: population differences in disease expression and acetylcholine receptor antibody titers between Chinese and Caucasians. Neurology. 1987;37:1854-1857 Engel AG, Fukuoka T, Lang B, Newsom-Davis J, Vincent A, Wray D. Lambert-Eaton myasthenic syndrome IgG: early morphologic effects and immunolocalization at the motor endplate. Ann N Y Acad Sci. 1987;505:333-345 Fukuoka T, Engel AG, Lang B, Newsom-Davis J, Prior C, Wray DW. Lambert-Eaton myasthenic syndrome: I. Early morphological effects of IgG on the presynaptic membrane active zones. Ann Neurol. 1987;22:193-199 Fukuoka T, Engel AG, Lang B, Newsom-Davis J, Vincent A. Lambert-Eaton myasthenic syndrome: II. Immunoelectron microscopy localization of IgG at the mouse motor end-plate. Ann Neurol. 1987;22:200211 Lang B, Newsom-Davis J, Peers C, Prior C, Wray DW. The effect of myasthenic syndrome antibody on presynaptic calcium channels in the mouse. J Physiol. 1987;390:257-270 Newsom-Davis J, Willcox N, Schluep M, Harcourt G, Vincent A, Mossman S, Wray D, Burges J. Immunological heterogeneity and cellular mechanisms in myasthenia gravis. Ann N Y Acad Sci. 1987;505:12-26 Oosterhuis HJ, Newsom-Davis J, Wokke JH, Molenaar PC, Weerden TV, Oen BS, Jennekens FG, Veldman H, Vincent A, Wray DW, et al. The slow channel syndrome. Two new cases. Brain. 1987;110 ( Pt 4):1061-1079 Schluep M, Willcox N, Vincent A, Dhoot GK, Newsom-Davis J. Acetylcholine receptors in human thymic myoid cells in situ: an immunohistological study. Ann Neurol. 1987;22:212-222 Vincent A, Whiting PJ, Schluep M, Heidenreich F, Lang B, Roberts A, Willcox N, Newsom-Davis J. Antibody heterogeneity and specificity in myasthenia gravis. Ann N Y Acad Sci. 1987;505:106-120 Willcox N, Schluep M, Ritter MA, Schuurman HJ, Newsom-Davis J, Christensson B. Myasthenic and nonmyasthenic thymoma. An expansion of a minor cortical epithelial cell subset? Am J Pathol. 1987;127:447-460 Wray DW, Peers C, Lang B, Lande S, Newsom-Davis J. Interference with calcium channels by Lambert Eaton myasthenic syndrome antibody. Ann N Y Acad Sci. 1987;505:368-376 Chester KA, Lang B, Gill J, Vincent A, Newsom-Davis J. Lambert-Eaton syndrome antibodies: reaction with membranes from a small cell lung cancer xenograft. J Neuroimmunol. 1988;18:97-104 Chiu HC, de Lange GG, Willcox N, Vincent A, Newsom-Davis J, Hsieh KH, Hung TP. Immunoglobulin allotypes in caucasian and Chinese myasthenia gravis: differences from Japanese patients. J Neurol Neurosurg Psychiatry. 1988;51:214-217 Dolly JO, Gwilt M, Lacey G, Newsom-Davis J, Vincent A, Whiting P, Wray DW. Action of antibodies directed against the acetylcholine receptor on channel function at mouse and rat motor end-plates. J Physiol. 1988;399:577-589 Harcourt GC, Sommer N, Rothbard J, Willcox HN, Newsom-Davis J. A juxta-membrane epitope on the human acetylcholine receptor recognized by T cells in myasthenia gravis. J Clin Invest. 1988;82:1295-1300 Heidenreich F, Vincent A, Newsom-Davis J. Differences in fine specificity of anti-acetylcholine receptor 8 99. 100. 101. 102. 103. 104. 105. 106. 107. 108. 109. 110. 111. 112. 113. 114. 115. 116. 117. 118. 119. 120. antibodies between subgroups of spontaneous myasthenia gravis of recent onset, and of penicillamine induced myasthenia. Autoimmunity. 1988;2:31-37 Heidenreich F, Vincent A, Roberts A, Newsom-Davis J. Epitopes on human acetylcholine receptor defined by monoclonal antibodies and myasthenia gravis sera. Autoimmunity. 1988;1:285-297 Heidenreich F, Vincent A, Willcox N, Newsom-Davis J. Anti-acetylcholine receptor antibody specificities in serum and in thymic cell culture supernatants from myasthenia gravis patients. Neurology. 1988;38:1784-1788 Lang B, Newsom-Davis J, Wray DW. The effect of Lambert-Eaton myasthenic syndrome antibody on slow action potentials in mouse cardiac ventricle. Proc R Soc Lond B Biol Sci. 1988;235:103-110 Lang B, Richardson G, Rees J, Vincent A, Newsom-Davis J. Plasma from myasthenia gravis patients reduces acetylcholine receptor agonist-induced Na+ flux into TE671 cell line. J Neuroimmunol. 1988;19:141-148 Mossman S, Vincent A, Newsom-Davis J. Passive transfer of myasthenia gravis by immunoglobulins: lack of correlation between AChR with antibody bound, acetylcholine receptor loss and transmission defect. J Neurol Sci. 1988;84:15-28 Nagel A, Engel AG, Lang B, Newsom-Davis J, Fukuoka T. Lambert-Eaton myasthenic syndrome IgG depletes presynaptic membrane active zone particles by antigenic modulation. Ann Neurol. 1988;24:552558 Newsom-Davis J. Autoimmunity in neuromuscular disease. Ann N Y Acad Sci. 1988;540:25-38 O'Neill JH, Murray NM, Newsom-Davis J. The Lambert-Eaton myasthenic syndrome. A review of 50 cases. Brain. 1988;111 ( Pt 3):577-596 Schluep M, Willcox N, Ritter MA, Newsom-Davis J, Larche M, Brown AN. Myasthenia gravis thymus: clinical, histological and culture correlations. J Autoimmun. 1988;1:445-467 Walker R, Vincent A, Newsom-Davis J. Immunological and pharmacological heterogeneity of alphabungarotoxin binding sites extracted from TE671 cells. J Neuroimmunol. 1988;19:149-157 Beeson D, Brydson M, Newsom-Davis J. Nucleotide sequence of human muscle acetylcholine receptor beta-subunit. Nucleic Acids Res. 1989;17:4391 Engel AG, Nagel A, Fukuoka T, Fukunaga H, Osame M, Lang B, Newsom-Davis J, Vincent A, Wray DW, Peers C. Motor nerve terminal calcium channels in Lambert-Eaton myasthenic syndrome. Morphologic evidence for depletion and that the depletion is mediated by autoantibodies. Ann N Y Acad Sci. 1989;560:278-290 Jermy AC, Fisher CA, Vincent AC, Willcox NA, Newsom-Davis J. Experimental autoimmune myasthenia gravis induced in mice without adjuvant: genetic susceptibility and adoptive transfer of weakness. J Autoimmun. 1989;2:675-688 Lande S, Black J, Dolly JO, Lang B, Newsom-Davis J, D WW. Effects of botulinum neurotoxin and Lambert-Eaton myasthenic syndrome IgG at mouse nerve terminals. J Neural Transm Park Dis Dement Sect. 1989;1:229-242 Lang B, Vincent A, Murray NM, Newsom-Davis J. Lambert-Eaton myasthenic syndrome: immunoglobulin G inhibition of Ca2+ flux in tumor cells correlates with disease severity. Ann Neurol. 1989;25:265-271 Laroche CM, Mier AK, Spiro SG, Newsom-Davis J, Moxham J, Green M. Respiratory muscle weakness in the Lambert-Eaton myasthenic syndrome. Thorax. 1989;44:913-918 Lewis SW, Ron MA, Newsom-Davis J. Absence of central functional cholinergic deficits in myasthenia gravis. J Neurol Neurosurg Psychiatry. 1989;52:258-261 Newsom-Davis J, Harcourt G, Sommer N, Beeson D, Willcox N, Rothbard JB. T-cell reactivity in myasthenia gravis. J Autoimmun. 1989;2 Suppl:101-108 Vincent A, Lang B, Newsom-Davis J. Autoimmunity to the voltage-gated calcium channel underlies the Lambert-Eaton myasthenic syndrome, a paraneoplastic disorder. Trends Neurosci. 1989;12:496-502 Willcox N, Schluep M, Sommer N, Campana D, Janossy G, Brown AN, Newsom-Davis J. Variable corticosteroid sensitivity of thymic cortex and medullary peripheral-type lymphoid tissue in myasthenia gravis patients: structural and functional effects. Q J Med. 1989;73:1071-1087 Wray DW, Lang B, Newsom-Davis J, Peers C. Antibodies against calcium channels in the Lambert-Eaton myasthenic syndrome. Ann N Y Acad Sci. 1989;560:269-277 Beeson D, Jeremiah S, West LF, Povey S, Newsom-Davis J. Assignment of the human nicotinic acetylcholine receptor genes: the alpha and delta subunit genes to chromosome 2 and the beta subunit gene to chromosome 17. Ann Hum Genet. 1990;54:199-208 9 121. 122. 123. 124. 125. 126. 127. 128. 129. 130. 131. 132. 133. 134. 135. 136. 137. 138. 139. 140. 141. 142. 143. 144. Beeson D, Morris A, Vincent A, Newsom-Davis J. The human muscle nicotinic acetylcholine receptor alpha-subunit exist as two isoforms: a novel exon. Embo J. 1990;9:2101-2106 Chalk CH, Murray NM, Newsom-Davis J, O'Neill JH, Spiro SG. Response of the Lambert-Eaton myasthenic syndrome to treatment of associated small-cell lung carcinoma. Neurology. 1990;40:1552-1556 Clark CV, Newsom-Davis J, Sanders MD. Ocular autonomic nerve function in Lambert-Eaton myasthenic syndrome. Eye (Lond). 1990;4 ( Pt 3):473-481 Gregory RP, Loh L, Newsom-Davis J. Recurrent isolated alternating phrenic nerve palsies: a variant of brachial neuritis? Thorax. 1990;45:420-421 Mathieson PW, O'Neill JH, Durrant ST, Henderson SJ, Green PJ, Newsom-Davis J. Antibody-mediated pure neutrophil aplasia, recurrent myasthenia gravis and previous thymoma: case report and literature review. Q J Med. 1990;74:57-61 Munschauer FE, Loh L, Bannister R, Newsom-Davis J. Abnormal respiration and sudden death during sleep in multiple system atrophy with autonomic failure. Neurology. 1990;40:677-679 Newsom-Davis J. Edrophonium responsiveness not necessarily diagnostic of myasthenia gravis. Muscle Nerve. 1990;13:1186 Peers C, Lang B, Newsom-Davis J, Wray DW. Selective action of myasthenic syndrome antibodies on calcium channels in a rodent neuroblastoma x glioma cell line. J Physiol. 1990;421:293-308 Sommer N, Willcox N, Harcourt GC, Newsom-Davis J. Myasthenic thymus and thymoma are selectively enriched in acetylcholine receptor-reactive T cells. Ann Neurol. 1990;28:312-319 Elrington GM, Murray NM, Spiro SG, Newsom-Davis J. Neurological paraneoplastic syndromes in patients with small cell lung cancer. A prospective survey of 150 patients. J Neurol Neurosurg Psychiatry. 1991;54:764-767 Leys K, Lang B, Johnston I, Newsom-Davis J. Calcium channel autoantibodies in the Lambert-Eaton myasthenic syndrome. Ann Neurol. 1991;29:307-314 Morris A, Beeson D, Jacobson L, Baggi F, Vincent A, Newsom-Davis J. Two isoforms of the muscle acetylcholine receptor alpha-subunit are translated in the human cell line TE671. FEBS Lett. 1991;295:116118 Newsom-Davis J, Leys K, Vincent A, Ferguson I, Modi G, Mills K. Immunological evidence for the coexistence of the Lambert-Eaton myasthenic syndrome and myasthenia gravis in two patients. J Neurol Neurosurg Psychiatry. 1991;54:452-453 Ong B, Willcox N, Wordsworth P, Beeson D, Vincent A, Altmann D, Lanchbury JS, Harcourt GC, Bell JI, Newsom-Davis J. Critical role for the Val/Gly86 HLA-DR beta dimorphism in autoantigen presentation to human T cells. Proc Natl Acad Sci U S A. 1991;88:7343-7347 Palace J, Wiles CM, Newsom-Davis J. 3,4-Diaminopyridine in the treatment of congenital (hereditary) myasthenia. J Neurol Neurosurg Psychiatry. 1991;54:1069-1072 Sinha S, Newsom-Davis J, Mills K, Byrne N, Lang B, Vincent A. Autoimmune aetiology for acquired neuromyotonia (Isaacs' syndrome). Lancet. 1991;338:75-77 Sommer N, Harcourt GC, Willcox N, Beeson D, Newsom-Davis J. Acetylcholine receptor-reactive T lymphocytes from healthy subjects and myasthenia gravis patients. Neurology. 1991;41:1270-1276 Squier M, Chalk C, Hilton-Jones D, Mills KR, Newsom-Davis J. Type 2 fiber predominance in LambertEaton myasthenic syndrome. Muscle Nerve. 1991;14:625-632 Willcox N, Schluep M, Ritter MA, Newsom-Davis J. The thymus in seronegative myasthenia gravis patients. J Neurol. 1991;238:256-261 Yamamoto T, Vincent A, Ciulla TA, Lang B, Johnston I, Newsom-Davis J. Seronegative myasthenia gravis: a plasma factor inhibiting agonist-induced acetylcholine receptor function copurifies with IgM. Ann Neurol. 1991;30:550-557 Chavez RA, Maloof J, Beeson D, Newsom-Davis J, Hall ZW. Subunit folding and alpha delta heterodimer formation in the assembly of the nicotinic acetylcholine receptor. Comparison of the mouse and human alpha subunits. J Biol Chem. 1992;267:23028-23034 Clouston PD, Saper CB, Arbizu T, Johnston I, Lang B, Newsom-Davis J, Posner JB. Paraneoplastic cerebellar degeneration. III. Cerebellar degeneration, cancer, and the Lambert-Eaton myasthenic syndrome. Neurology. 1992;42:1944-1950 Demaine A, Willcox N, Janer M, Welsh K, Newsom-Davis J. Immunoglobulin heavy chain gene associations in myasthenia gravis: new evidence for disease heterogeneity. J Neurol. 1992;239:53-56 Hawke S, Willcox N, Harcourt G, Vincent A, Newsom-Davis J. Stimulation of human T cells by sparse antigens captured on immunomagnetic particles. J Immunol Methods. 1992;155:41-48 10 145. 146. 147. 148. 149. 150. 151. 152. 153. 154. 155. 156. 157. 158. 159. 160. 161. 162. 163. 164. 165. 166. 167. Howard RS, Wiles CM, Hirsch NP, Loh L, Spencer GT, Newsom-Davis J. Respiratory involvement in multiple sclerosis. Brain. 1992;115 ( Pt 2):479-494 Morris CS, Esiri MM, Marx A, Newsom-Davis J. Immunocytochemical characteristics of small cell lung carcinoma associated with the Lambert-Eaton myasthenic syndrome. Am J Pathol. 1992;140:839-845 Roberts A, Lang B, Vincent A, Newsom-Davis J. Search for cross-reactive idiotypes on monoclonal and myasthenia gravis acetylcholine receptor antibodies. Autoimmunity. 1992;12:53-60 Baggi F, Nicolle M, Vincent A, Matsuo H, Willcox N, Newsom-Davis J. Presentation of endogenous acetylcholine receptor epitope by an MHC class II-transfected human muscle cell line to a specific CD4+ T cell clone from a myasthenia gravis patient. J Neuroimmunol. 1993;46:57-65 Beeson D, Brydson M, Betty M, Jeremiah S, Povey S, Vincent A, Newsom-Davis J. Primary structure of the human muscle acetylcholine receptor. cDNA cloning of the gamma and epsilon subunits. Eur J Biochem. 1993;215:229-238 Harcourt G, Batocchi AP, Hawke S, Beeson D, Pantic N, Jacobson L, Willcox N, Vincent A, NewsomDavis J. Detection of alpha-subunit isoforms in human muscle acetylcholine receptor by specific T cells from a myasthenia gravis patient. Proc Biol Sci. 1993;254:1-6 MacLennan C, Beeson D, Vincent A, Newsom-Davis J. Human nicotinic acetylcholine receptor alphasubunit isoforms: origins and expression. Nucleic Acids Res. 1993;21:5463-5467 Martin-Moutot N, el Far O, Leveque C, David P, Marqueze B, Lang B, Newsom-Davis J, Hoshino T, Takahashi M, Seagar MJ. Synaptotagmin: a Lambert-Eaton myasthenic syndrome antigen that associates with presynaptic calcium channels. J Physiol Paris. 1993;87:37-41 Newsom-Davis J, Mills KR. Immunological associations of acquired neuromyotonia (Isaacs' syndrome). Report of five cases and literature review. Brain. 1993;116 ( Pt 2):453-469 Panegyres PK, Squier M, Mills KR, Newsom-Davis J. Acute myopathy associated with large parenteral dose of corticosteroid in myasthenia gravis. J Neurol Neurosurg Psychiatry. 1993;56:702-704 Shillito P, Vincent A, Newsom-Davis J. Congenital myasthenic syndromes. Neuromuscul Disord. 1993;3:183-190 Thomas MJ, Misbah SA, Chapel HM, Jones M, Elrington G, Newsom-Davis J. Hemolysis after high-dose intravenous Ig. Blood. 1993;82:3789 Vincent A, Li Z, Hart A, Barrett-Jolley R, Yamamoto T, Burges J, Wray D, Byrne N, Molenaar P, Newsom-Davis J. Seronegative myasthenia gravis. Evidence for plasma factor(s) interfering with acetylcholine receptor function. Ann N Y Acad Sci. 1993;681:529-538 Vincent A, Newsom-Davis J, Wray D, Shillito P, Harrison J, Betty M, Beeson D, Mills K, Palace J, Molenaar P, et al. Clinical and experimental observations in patients with congenital myasthenic syndromes. Ann N Y Acad Sci. 1993;681:451-460 Barrett-Jolley R, Byrne N, Vincent A, Newsom-Davis J. Plasma from patients with seronegative myasthenia gravis inhibit nAChR responses in the TE671/RD cell line. Pflugers Arch. 1994;428:492-498 Betty M, Beeson D, West L, Vincent A, Newsom-Davis J. D17S1175: dinucleotide repeat polymorphism 5' to CHRNE. Hum Mol Genet. 1994;3:2083 Burges J, Vincent A, Molenaar PC, Newsom-Davis J, Peers C, Wray D. Passive transfer of seronegative myasthenia gravis to mice. Muscle Nerve. 1994;17:1393-1400 Daenke S, Parker CE, Niewiesk S, Newsom-Davis J, Nightingale S, Bangham CR. Spastic paraparesis in a patient carrying defective human T cell leukemia virus type I (HTLV-I) provirus sequences but lacking a humoral or cytotoxic T cell response to HTLV-I. J Infect Dis. 1994;169:941-943 Goldstein JM, Waxman SG, Vollmer TL, Lang B, Johnston I, Newsom-Davis J. Subacute cerebellar degeneration and Lambert-Eaton myasthenic syndrome associated with antibodies to voltage-gated calcium channels: differential effect of immunosuppressive therapy on central and peripheral defects. J Neurol Neurosurg Psychiatry. 1994;57:1138-1139 Johnston I, Lang B, Leys K, Newsom-Davis J. Heterogeneity of calcium channel autoantibodies detected using a small-cell lung cancer line derived from a Lambert-Eaton myasthenic syndrome patient. Neurology. 1994;44:334-338 Newsom-Davis J. High hopes ... for neurology. A view from the top. J R Coll Physicians Lond. 1994;28:105 Nicolle MW, Nag B, Sharma SD, Willcox N, Vincent A, Ferguson DJ, Newsom-Davis J. Specific tolerance to an acetylcholine receptor epitope induced in vitro in myasthenia gravis CD4+ lymphocytes by soluble major histocompatibility complex class II-peptide complexes. J Clin Invest. 1994;93:1361-1369 Palace J, Vincent A, Beeson D, Newsom-Davis J. Immunogenicity of human recombinant acetylcholine 11 168. 169. 170. 171. 172. 173. 174. 175. 176. 177. 178. 179. 180. 181. 182. 183. 184. 185. 186. 187. 188. receptor alpha subunit: cytoplasmic epitopes dominate the antibody response in four mouse strains. Autoimmunity. 1994;18:113-119 Ratanachaiyavong S, Fleming D, Janer M, Demaine AG, Willcox N, Newsom-Davis J, McGregor AM. HLA-DPB1 polymorphisms in patients with hyperthyroid Graves' disease and early onset myasthenia gravis. Autoimmunity. 1994;17:99-104 Roberts M, Willison H, Vincent A, Newsom-Davis J. Serum factor in Miller-Fisher variant of GuillainBarre syndrome and neurotransmitter release. Lancet. 1994;343:454-455 Barnes PR, Kanabar DJ, Brueton L, Newsom-Davis J, Huson SM, Mann NP, Hilton-Jones D. Recurrent congenital arthrogryposis leading to a diagnosis of myasthenia gravis in an initially asymptomatic mother. Neuromuscul Disord. 1995;5:59-65 el Far O, Marqueze B, Leveque C, Martin-Moutot N, Lang B, Newsom-Davis J, Yoshida A, Takahashi M, Seagar MJ. Antigens associated with N- and L-type calcium channels in Lambert-Eaton myasthenic syndrome. J Neurochem. 1995;64:1696-1702 Gilhus NE, Jones M, Turley H, Gatter KC, Nagvekar N, Newsom-Davis J, Willcox N. Oncogene proteins and proliferation antigens in thymomas: increased expression of epidermal growth factor receptor and Ki67 antigen. J Clin Pathol. 1995;48:447-455 Gilhus NE, Willcox N, Harcourt G, Nagvekar N, Beeson D, Vincent A, Newsom-Davis J. Antigen presentation by thymoma epithelial cells from myasthenia gravis patients to potentially pathogenic T cells. J Neuroimmunol. 1995;56:65-76 Lang B, Newsom-Davis J. Immunopathology of the Lambert-Eaton myasthenic syndrome. Springer Semin Immunopathol. 1995;17:3-15 Martin-Moutot N, Lang B, Newsom-Davis J, Seagar M. Binding of Lambert-Eaton myasthenic syndrome IgG to synaptosomal proteins does not correlate with an inhibition of calcium uptake. Neurosci Lett. 1995;187:115-118 Matsuo H, Batocchi AP, Hawke S, Nicolle M, Jacobson L, Vincent A, Newsom-Davis J, Willcox N. Peptide-selected T cell lines from myasthenia gravis patients and controls recognize epitopes that are not processed from whole acetylcholine receptor. J Immunol. 1995;155:3683-3692 Motomura M, Johnston I, Lang B, Vincent A, Newsom-Davis J. An improved diagnostic assay for Lambert-Eaton myasthenic syndrome. J Neurol Neurosurg Psychiatry. 1995;58:85-87 Newland CF, Beeson D, Vincent A, Newsom-Davis J. Functional and non-functional isoforms of the human muscle acetylcholine receptor. J Physiol. 1995;489 ( Pt 3):767-778 Newsom-Davis J. The Hughlings Jackson Lecture: autoimmunity and the nervous system. J R Soc Med. 1995;88:639P-643P Roberts M, Willison HJ, Vincent A, Newsom-Davis J. Multifocal motor neuropathy human sera block distal motor nerve conduction in mice. Ann Neurol. 1995;38:111-118 Vincent A, Newland C, Brueton L, Beeson D, Riemersma S, Huson SM, Newsom-Davis J. Arthrogryposis multiplex congenita with maternal autoantibodies specific for a fetal antigen. Lancet. 1995;346:24-25 Shillito P, Molenaar PC, Vincent A, Leys K, Zheng W, van den Berg RJ, Plomp JJ, van Kempen GT, Chauplannaz G, Wintzen AR Vandijk JG, Newsom-Davis J. Acquired neuromyotonia: evidence for autoantibodies directed against K+ channels of peripheral nerves.Ann Neurol. 1995;38:714-22. Bain PG, Motomura M, Newsom-Davis J, Misbah SA, Chapel HM, Lee ML, Vincent A, Lang B. Effects of intravenous immunoglobulin on muscle weakness and calcium-channel autoantibodies in the LambertEaton myasthenic syndrome. Neurology. 1996;47:678-683 Beeson D, Amar M, Bermudez I, Vincent A, Newsom-Davis J. Stable functional expression of the adult subtype of human muscle acetylcholine receptor following transfection of the human rhabdomyosarcoma cell line TE671 with cDNA encoding the epsilon subunit. Neurosci Lett. 1996;207:57-60 Beeson D, Jacobson L, Newsom-Davis J, Vincent A. A transfected human muscle cell line expressing the adult subtype of the human muscle acetylcholine receptor for diagnostic assays in myasthenia gravis. Neurology. 1996;47:1552-1555 Glennerster A, Palace J, Warburton D, Oxbury S, Newsom-Davis J. Memory in myasthenia gravis: neuropsychological tests of central cholinergic function before and after effective immunologic treatment. Neurology. 1996;46:1138-1142 Heckmann JM, Morrison KE, Emeryk-Szajewska B, Strugalska H, Bergoffen J, Willcox N, Newsom-Davis J. Human muscle acetylcholine receptor alpha-subunit gene (CHRNA1) association with autoimmune myasthenia gravis in black, mixed-ancestry and Caucasian subjects. J Autoimmun. 1996;9:175-180 Newsom-Davis J. Autoimmunity and the nervous system. Ann Acad Med Singapore. 1996;25:309-314 12 189. 190. 191. 192. 193. 194. 195. 196. 197. 198. 199. 200. 201. 202. 203. 204. 205. 206. 207. 208. 209. Riemersma S, Vincent A, Beeson D, Newland C, Hawke S, Vernet-der Garabedian B, Eymard B, NewsomDavis J. Association of arthrogryposis multiplex congenita with maternal antibodies inhibiting fetal acetylcholine receptor function. J Clin Invest. 1996;98:2358-2363 Croxen R, Newland C, Beeson D, Oosterhuis H, Chauplannaz G, Vincent A, Newsom-Davis J. Mutations in different functional domains of the human muscle acetylcholine receptor alpha subunit in patients with the slow-channel congenital myasthenic syndrome. Hum Mol Genet. 1997;6:767-774 Farrar J, Portolano S, Willcox N, Vincent A, Jacobson L, Newsom-Davis J, Rapoport B, McLachlan SM. Diverse Fab specific for acetylcholine receptor epitopes from a myasthenia gravis thymus combinatorial library. Int Immunol. 1997;9:1311-1318 Hanna M, Mills K, Pazdera L, Newsom-Davis J. Primary orthostatic tremor with prominent muscle hypertrophy. Neurology. 1997;49:872-874 Hart IK, Waters C, Vincent A, Newland C, Beeson D, Pongs O, Morris C, Newsom-Davis J. Autoantibodies detected to expressed K+ channels are implicated in neuromyotonia. Ann Neurol. 1997;41:238-246 MacLennan C, Beeson D, Buijs AM, Vincent A, Newsom-Davis J. Acetylcholine receptor expression in human extraocular muscles and their susceptibility to myasthenia gravis. Ann Neurol. 1997;41:423-431 Mason WP, Graus F, Lang B, Honnorat J, Delattre JY, Valldeoriola F, Antoine JC, Rosenblum MK, Rosenfeld MR, Newsom-Davis J, Posner JB, Dalmau J. Small-cell lung cancer, paraneoplastic cerebellar degeneration and the Lambert-Eaton myasthenic syndrome. Brain. 1997;120 ( Pt 8):1279-1300 Meager A, Vincent A, Newsom-Davis J, Willcox N. Spontaneous neutralising antibodies to interferon-alpha and interleukin-12 in thymoma-associated autoimmune disease. Lancet. 1997;350:1596-1597 Motomura M, Lang B, Johnston I, Palace J, Vincent A, Newsom-Davis J. Incidence of serum anti-P/O-type and anti-N-type calcium channel autoantibodies in the Lambert-Eaton myasthenic syndrome. J Neurol Sci. 1997;147:35-42 Newsom-Davis J. Autoimmune neuromyotonia (Isaacs' syndrome): an antibody-mediated potassium channelopathy. Ann N Y Acad Sci. 1997;835:111-119 Newsom-Davis J. Myasthenia gravis and the Miller-Fisher variant of Guillain-Barre syndrome. Curr Opin Neurol. 1997;10:18-21 Slater CR, Young C, Wood SJ, Bewick GS, Anderson LV, Baxter P, Fawcett PR, Roberts M, Jacobson L, Kuks J, Vincent A, Newsom-Davis J. Utrophin abundance is reduced at neuromuscular junctions of patients with both inherited and acquired acetylcholine receptor deficiencies. Brain. 1997;120 ( Pt 9):15131531 Waterman SA, Lang B, Newsom-Davis J. Effect of Lambert-Eaton myasthenic syndrome antibodies on autonomic neurons in the mouse. Ann Neurol. 1997;42:147-156 Beeson D, Bond AP, Corlett L, Curnow SJ, Hill ME, Jacobson LW, MacLennan C, Meager A, Moody AM, Moss P, Nagvekar N, Newsom-Davis J, Pantic N, Roxanis I, Spack EG, Vincent A, Willcox N. Thymus, thymoma, and specific T cells in myasthenia gravis. Ann N Y Acad Sci. 1998;841:371-387 Bond AP, Corlett L, Curnow SJ, Spack E, Willcox N, Newsom-Davis J. Diverse patterns of unresponsiveness in an acetylcholine receptor-specific T-cell clone from a myasthenia gravis patient after engaging the T-cell receptor with three different ligands. J Neuroimmunol. 1998;82:182-190 Lang B, Waterman S, Pinto A, Jones D, Moss F, Boot J, Brust P, Williams M, Stauderman K, Harpold M, Motomura M, Moll JW, Vincent A, Newsom-Davis J. The role of autoantibodies in Lambert-Eaton myasthenic syndrome. Ann N Y Acad Sci. 1998;841:596-605 Maddison P, Newsom-Davis J, Mills KR. Effect of 3,4-diaminopyridine on the time course of decay of compound muscle action potential augmentation in the Lambert-Eaton myasthenic syndrome. Muscle Nerve. 1998;21:1196-1198 Maddison P, Newsom-Davis J, Mills KR. Distribution of electrophysiological abnormality in LambertEaton myasthenic syndrome. J Neurol Neurosurg Psychiatry. 1998;65:213-217 Maddison P, Newsom-Davis J, Mills KR. Decay of postexercise augmentation in the Lambert-Eaton myasthenic syndrome: effect of cooling. Neurology. 1998;50:1083-1087 Moody AM, Reyburn H, Willcox N, Newsom-Davis J. New polymorphism of the human T-cell receptor AV28S1 gene segment. Immunogenetics. 1998;48:62-64 Nagvekar N, Moody AM, Moss P, Roxanis I, Curnow J, Beeson D, Pantic N, Newsom-Davis J, Vincent A, Willcox N. A pathogenetic role for the thymoma in myasthenia gravis. Autosensitization of IL-4producing T cell clones recognizing extracellular acetylcholine receptor epitopes presented by minority class II isotypes. J Clin Invest. 1998;101:2268-2277 13 210. 211. 212. 213. 214. 215. 216. 217. 218. 219. 220. 221. 222. 223. 224. 225. 226. 227. 228. 229. 230. 231. Newsom-Davis J. A treatment algorithm for Lambert-Eaton myasthenic syndrome. Ann N Y Acad Sci. 1998;841:817-822 Newsom-Davis J. Autoimmune and genetic disorders at the neuromuscular junction. The 1997 Ronnie Mac Keith lecture. Dev Med Child Neurol. 1998;40:199-206 Palace J, Newsom-Davis J, Lecky B. A randomized double-blind trial of prednisolone alone or with azathioprine in myasthenia gravis. Myasthenia Gravis Study Group. Neurology. 1998;50:1778-1783 Pinto A, Gillard S, Moss F, Whyte K, Brust P, Williams M, Stauderman K, Harpold M, Lang B, NewsomDavis J, Bleakman D, Lodge D, Boot J. Human autoantibodies specific for the alpha1A calcium channel subunit reduce both P-type and Q-type calcium currents in cerebellar neurons. Proc Natl Acad Sci U S A. 1998;95:8328-8333 Verschuuren JJ, Dalmau J, Tunkel R, Lang B, Graus F, Schramm L, Posner JB, Newsom-Davis J, Rosenfeld MR. Antibodies against the calcium channel beta-subunit in Lambert-Eaton myasthenic syndrome. Neurology. 1998;50:475-479 Vincent A, Jacobson L, Plested P, Polizzi A, Tang T, Riemersma S, Newland C, Ghorazian S, Farrar J, MacLennan C, Willcox N, Beeson D, Newsom-Davis J. Antibodies affecting ion channel function in acquired neuromyotonia, in seropositive and seronegative myasthenia gravis, and in antibody-mediated arthrogryposis multiplex congenita. Ann N Y Acad Sci. 1998;841:482-496 Croxen R, Newland C, Betty M, Vincent A, Newsom-Davis J, Beeson D. Novel functional epsilon-subunit polypeptide generated by a single nucleotide deletion in acetylcholine receptor deficiency congenital myasthenic syndrome. Ann Neurol. 1999;46:639-647 Hill M, Beeson D, Moss P, Jacobson L, Bond A, Corlett L, Newsom-Davis J, Vincent A, Willcox N. Early-onset myasthenia gravis: a recurring T-cell epitope in the adult-specific acetylcholine receptor epsilon subunit presented by the susceptibility allele HLA-DR52a. Ann Neurol. 1999;45:224-231 Hill M, Moss P, Wordsworth P, Newsom-Davis J, Willcox N. T cell responses to D-penicillamine in druginduced myasthenia gravis: recognition of modified DR1:peptide complexes. J Neuroimmunol. 1999;97:146-153 Hill ME, Ferguson DJ, Austyn JM, Newsom-Davis J, Willcox HN. Potent immunostimulatory dendritic cells can be cultured in bulk from progenitors in normal infant and adult myasthenic human thymus. Immunology. 1999;97:325-332 Janer M, Cowland A, Picard J, Campbell D, Pontarotti P, Newsom-Davis J, Bunce M, Welsh K, Demaine A, Wilson AG, Willcox N. A susceptibility region for myasthenia gravis extending into the HLA-class I sector telomeric to HLA-C. Hum Immunol. 1999;60:909-917 Li FY, Tariq M, Croxen R, Morten K, Squier W, Newsom-Davis J, Beeson D, Larsson C. Mapping of autosomal dominant progressive external ophthalmoplegia to a 7-cM critical region on 10q24. Neurology. 1999;53:1265-1271 Maddison P, Newsom-Davis J, Mills KR. Strength-duration properties of peripheral nerve in acquired neuromyotonia. Muscle Nerve. 1999;22:823-830 Maddison P, Newsom-Davis J, Mills KR, Souhami RL. Favourable prognosis in Lambert-Eaton myasthenic syndrome and small-cell lung carcinoma. Lancet. 1999;353:117-118 Maddison P, Pinto A, Newsom-Davis J. Endocrine function in Lambert-Eaton myasthenic syndrome. Ann Neurol. 1999;45:414-415 Meager A, Wadhwa M, Bird C, Dilger P, Thorpe R, Newsom-Davis J, Willcox N. Spontaneously occurring neutralizing antibodies against granulocyte-macrophage colony-stimulating factor in patients with autoimmune disease. Immunology. 1999;97:526-532 Newsom-Davis J. Autoimmune syndromes at the neuromuscular junction. J Child Neurol. 1999;14:41-43 Nichols P, Croxen R, Vincent A, Rutter R, Hutchinson M, Newsom-Davis J, Beeson D. Mutation of the acetylcholine receptor epsilon-subunit promoter in congenital myasthenic syndrome. Ann Neurol. 1999;45:439-443 Brueton LA, Huson SM, Cox PM, Shirley I, Thompson EM, Barnes PR, Price J, Newsom-Davis J, Vincent A. Asymptomatic maternal myasthenia as a cause of the Pena-Shokeir phenotype. Am J Med Genet. 2000;92:1-6 Mygland A, Vincent A, Newsom-Davis J, Kaminski H, Zorzato F, Agius M, Gilhus NE, Aarli JA. Autoantibodies in thymoma-associated myasthenia gravis with myositis or neuromyotonia. Arch Neurol. 2000;57:527-531 Newsom-Davis J. A message from the editor. Brain. 2000;123 (Pt 1):1-2 Warlow CF, Newsom-Davis J, Humphrey PR, Miller DH, Stevens DI, Kennard C. GIM and specialty 14 232. 233. 234. 235. 236. 237. 238. 239. 240. 241. 242. 243. 244. 245. 246. 247. 248. 249. 250. 251. 252. 253. 254. medicine. J R Coll Physicians Lond. 2000;34:111-112 Brownlow S, Webster R, Croxen R, Brydson M, Neville B, Lin JP, Vincent A, Newsom-Davis J, Beeson D. Acetylcholine receptor delta subunit mutations underlie a fast-channel myasthenic syndrome and arthrogryposis multiplex congenita. J Clin Invest. 2001;108:125-130 Buckley C, Douek D, Newsom-Davis J, Vincent A, Willcox N. Mature, long-lived CD4+ and CD8+ T cells are generated by the thymoma in myasthenia gravis. Ann Neurol. 2001;50:64-72 Buckley C, Newsom-Davis J, Willcox N, Vincent A. Do titin and cytokine antibodies in MG patients predict thymoma or thymoma recurrence? Neurology. 2001;57:1579-1582 Hoch W, McConville J, Helms S, Newsom-Davis J, Melms A, Vincent A. Auto-antibodies to the receptor tyrosine kinase MuSK in patients with myasthenia gravis without acetylcholine receptor antibodies. Nat Med. 2001;7:365-368 Maddison P, Lang B, Mills K, Newsom-Davis J. Long term outcome in Lambert-Eaton myasthenic syndrome without lung cancer. J Neurol Neurosurg Psychiatry. 2001;70:212-217 Newsom-Davis J. Lambert-Eaton Myasthenic Syndrome. Curr Treat Options Neurol. 2001;3:127-131 Croxen R, Hatton C, Shelley C, Brydson M, Chauplannaz G, Oosterhuis H, Vincent A, Newsom-Davis J, Colquhoun D, Beeson D. Recessive inheritance and variable penetrance of slow-channel congenital myasthenic syndromes. Neurology. 2002;59:162-168 Croxen R, Vincent A, Newsom-Davis J, Beeson D. Myasthenia gravis in a woman with congenital AChR deficiency due to epsilon-subunit mutations. Neurology. 2002;58:1563-1565 Hart IK, Maddison P, Newsom-Davis J, Vincent A, Mills KR. Phenotypic variants of autoimmune peripheral nerve hyperexcitability. Brain. 2002;125:1887-1895 Pinto A, Iwasa K, Newland C, Newsom-Davis J, Lang B. The action of Lambert-Eaton myasthenic syndrome immunoglobulin G on cloned human voltage-gated calcium channels. Muscle Nerve. 2002;25:715-724 Rosenberg RN, Aminoff M, Boller F, Soerensen PS, Griggs RC, Hachinski V, Hallett M, Johnson RT, Kennard C, Lang AE, Lees AJ, Lisak R, Newsom-Davis J, Pedley TA, Selzer ME, Zochodne D. Reporting clinical trials: full access to all of the data. Arch Neurol. 2002;59:27-28 Roxanis I, Micklem K, McConville J, Newsom-Davis J, Willcox N. Thymic myoid cells and germinal center formation in myasthenia gravis; possible roles in pathogenesis. J Neuroimmunol. 2002;125:185-197 Wiles CM, Brown P, Chapel H, Guerrini R, Hughes RA, Martin TD, McCrone P, Newsom-Davis J, Palace J, Rees JH, Rose MR, Scolding N, Webster AD. Intravenous immunoglobulin in neurological disease: a specialist review. J Neurol Neurosurg Psychiatry. 2002;72:440-448 Beeson D, Webster R, Ealing J, Croxen R, Brownlow S, Brydson M, Newsom-Davis J, Slater C, Hatton C, Shelley C, Colquhoun D, Vincent A. Structural abnormalities of the AChR caused by mutations underlying congenital myasthenic syndromes. Ann N Y Acad Sci. 2003;998:114-124 Burke G, Cossins J, Maxwell S, Owens G, Vincent A, Robb S, Nicolle M, Hilton-Jones D, Newsom-Davis J, Palace J, Beeson D. Rapsyn mutations in hereditary myasthenia: distinct early- and late-onset phenotypes. Neurology. 2003;61:826-828 Lang B, Pinto A, Giovannini F, Newsom-Davis J, Vincent A. Pathogenic autoantibodies in the lamberteaton myasthenic syndrome. Ann N Y Acad Sci. 2003;998:187-195 Maddison P, Newsom-Davis J. Treatment for Lambert-Eaton myasthenic syndrome. Cochrane Database Syst Rev. 2003:CD003279 Meager A, Wadhwa M, Dilger P, Bird C, Thorpe R, Newsom-Davis J, Willcox N. Anti-cytokine autoantibodies in autoimmunity: preponderance of neutralizing autoantibodies against interferon-alpha, interferon-omega and interleukin-12 in patients with thymoma and/or myasthenia gravis. Clin Exp Immunol. 2003;132:128-136 Newsom-Davis J. Therapy in myasthenia gravis and Lambert-Eaton myasthenic syndrome. Semin Neurol. 2003;23:191-198 Newsom-Davis J, Buckley C, Clover L, Hart I, Maddison P, Tuzum E, Vincent A. Autoimmune disorders of neuronal potassium channels. Ann N Y Acad Sci. 2003;998:202-210 Vincent A, Bowen J, Newsom-Davis J, McConville J. Seronegative generalised myasthenia gravis: clinical features, antibodies, and their targets. Lancet Neurol. 2003;2:99-106 Vincent A, McConville J, Farrugia ME, Bowen J, Plested P, Tang T, Evoli A, Matthews I, Sims G, Dalton P, Jacobson L, Polizzi A, Blaes F, Lang B, Beeson D, Willcox N, Newsom-Davis J, Hoch W. Antibodies in myasthenia gravis and related disorders. Ann N Y Acad Sci. 2003;998:324-335 Wolfe GI, Kaminski HJ, Jaretzki A, 3rd, Swan A, Newsom-Davis J. Development of a thymectomy trial in 15 255. 256. 257. 258. 259. 260. 261. 262. 263. 264. 265. 266. 267. 268. 269. 270. 271. 272. 273. 274. 275. 276. 277. 278. nonthymomatous myasthenia gravis patients receiving immunosuppressive therapy. Ann N Y Acad Sci. 2003;998:473-480 Zhang W, Liu JL, Meager A, Newsom-Davis J, Willcox N. Autoantibodies to IL-12 in myasthenia gravis patients with thymoma; effects on the IFN-gamma responses of healthy CD4+ T cells. J Neuroimmunol. 2003;139:102-108 Burke G, Cossins J, Maxwell S, Robb S, Nicolle M, Vincent A, Newsom-Davis J, Palace J, Beeson D. Distinct phenotypes of congenital acetylcholine receptor deficiency. Neuromuscul Disord. 2004;14:356364 McConville J, Farrugia ME, Beeson D, Kishore U, Metcalfe R, Newsom-Davis J, Vincent A. Detection and characterization of MuSK antibodies in seronegative myasthenia gravis. Ann Neurol. 2004;55:580-584 Newsom-Davis J. Neuromyotonia. Rev Neurol (Paris). 2004;160:S85-89 Newsom-Davis J. Lambert-Eaton myasthenic syndrome. Rev Neurol (Paris). 2004;160:177-180 Vincent A, McConville J, Farrugia ME, Newsom-Davis J. Seronegative myasthenia gravis. Semin Neurol. 2004;24:125-133 Webster R, Brydson M, Croxen R, Newsom-Davis J, Vincent A, Beeson D. Mutation in the AChR ion channel gate underlies a fast channel congenital myasthenic syndrome. Neurology. 2004;62:1090-1096 Leite MI, Strobel P, Jones M, Micklem K, Moritz R, Gold R, Niks EH, Berrih-Aknin S, Scaravilli F, Canelhas A, Marx A, Newsom-Davis J, Willcox N, Vincent A. Fewer thymic changes in MuSK antibodypositive than in MuSK antibody-negative MG. Ann Neurol. 2005;57:444-448 Maddison P, Newsom-Davis J. Treatment for Lambert-Eaton myasthenic syndrome. Cochrane Database Syst Rev. 2005:CD003279 Newsom-Davis J. Can tacrolimus replace ciclosporin and prednisone to treat myasthenia gravis? Nat Clin Pract Neurol. 2005;1:14-15 Newsom-Davis J. Neuromuscular junction channelopathies: a brief overview. Acta Neurol Belg. 2005;105:181-186 Vincent AC, McConville J, Newsom-Davis J. Is "seronegative" MG explained by autoantibodies to MuSK? Neurology. 2005;64:399; author reply 399 Beeson D, Higuchi O, Palace J, Cossins J, Spearman H, Maxwell S, Newsom-Davis J, Burke G, Fawcett P, Motomura M, Muller JS, Lochmuller H, Slater C, Vincent A, Yamanashi Y. Dok-7 mutations underlie a neuromuscular junction synaptopathy. Science. 2006;313:1975-1978 Farrugia ME, Kennett RP, Newsom-Davis J, Hilton-Jones D, Vincent A. Single-fiber electromyography in limb and facial muscles in muscle-specific kinase antibody and acetylcholine receptor antibody myasthenia gravis. Muscle Nerve. 2006;33:568-570 Farrugia ME, Robson MD, Clover L, Anslow P, Newsom-Davis J, Kennett R, Hilton-Jones D, Matthews PM, Vincent A. MRI and clinical studies of facial and bulbar muscle involvement in MuSK antibodyassociated myasthenia gravis. Brain. 2006;129:1481-1492 Jitpimolmard S, Taimkao S, Chotmongkol V, Sawanyawisuth K, Vincent A, Newsom-Davis J. Acetylcholine receptor antibody in Thai generalized myasthenia gravis patients. J Med Assoc Thai. 2006;89:68-71 Maddison P, Mills KR, Newsom-Davis J. Clinical electrophysiological characterization of the acquired neuromyotonia phenotype of autoimmune peripheral nerve hyperexcitability. Muscle Nerve. 2006;33:801808 Newsom-Davis J. Neuromyotonia: a diverse disorder. Neurol India. 2006;54:350 Farrugia ME, Kennett RP, Hilton-Jones D, Newsom-Davis J, Vincent A. Quantitative EMG of facial muscles in myasthenia patients with MuSK antibodies. Clin Neurophysiol. 2007;118:269-277 Newsom-Davis J. The emerging diversity of neuromuscular junction disorders. Acta Myol. 2007;26:5-10 Palace J, Lashley D, Newsom-Davis J, Cossins J, Maxwell S, Kennett R, Jayawant S, Yamanashi Y, Beeson D. Clinical features of the DOK7 neuromuscular junction synaptopathy. Brain. 2007;130:15071515 Aban IB, Wolfe GI, Cutter GR, Kaminski HJ, Jaretzki A, 3rd, Minisman G, Conwit R, Newsom-Davis J. The MGTX experience: challenges in planning and executing an international, multicenter clinical trial. J Neuroimmunol. 2008;201-202:80-84 Beeson D, Webster R, Cossins J, Lashley D, Spearman H, Maxwell S, Slater CR, Newsom-Davis J, Palace J, Vincent A. Congenital myasthenic syndromes and the formation of the neuromuscular junction. Ann N Y Acad Sci. 2008;1132:99-103 Hill ME, Shiono H, Newsom-Davis J, Willcox N. The myasthenia gravis thymus: a rare source of human 16 279. 280. 281. 282. 283. 284. autoantibody-secreting plasma cells for testing potential therapeutics. J Neuroimmunol. 2008;201-202:5056 Maclennan CA, Vincent A, Marx A, Willcox N, Gilhus NE, Newsom-Davis J, Beeson D. Preferential expression of AChR epsilon-subunit in thymomas from patients with myasthenia gravis. J Neuroimmunol. 2008;201-202:28-32 Newsom-Davis J, Cutter G, Wolfe GI, Kaminski HJ, Jaretzki A, 3rd, Minisman G, Aban I, Conwit R. Status of the thymectomy trial for nonthymomatous myasthenia gravis patients receiving prednisone. Ann N Y Acad Sci. 2008;1132:344-347 Strobel P, Moritz R, Leite MI, Willcox N, Chuang WY, Gold R, Nix W, Schalke B, Kiefer R, MullerHermelink HK, Jaretzki Iii A, Newsom-Davis J, Marx A. The ageing and myasthenic thymus: a morphometric study validating a standard procedure in the histological workup of thymic specimens. J Neuroimmunol. 2008;201-202:64-73 Vincent A, Leite MI, Farrugia ME, Jacob S, Viegas S, Shiraishi H, Benveniste O, Morgan BP, Hilton-Jones D, Newsom-Davis J, Beeson D, Willcox N. Myasthenia gravis seronegative for acetylcholine receptor antibodies. Ann N Y Acad Sci. 2008;1132:84-92 Croxen R, Hatton C, Shelley C, Brydson M, Chauplannaz G, Oosterhuis H, Vincent A, Newsom-Davis J, Colquhoun D, Beeson D. Voluntary partial retraction of: Recessive inheritance and variable penetrance of slow-channel congenital myasthenic syndromes. Neurology. 2009;72:294 Payne M, Bradbury P, Lang B, Vincent A, Han C, Newsom-Davis J, Talbot D. Prospective study into the incidence of Lambert Eaton myasthenic syndrome in small cell lung cancer. J Thorac Oncol;5:34-38 17 C .Interview with John Newsom-Davis. M.D. Professor Emeritus, Department of Clinical Neurology University of Oxford Honorary Consultant Neurologist, Radcliffe Infirmary, Oxford London, England American Neurological Association Oral History Project American Neurological Association Meeting San Diego Marriott Marina Hotel San Diego, California September 26, 2005 Interviewed by Barbara W. Sommer The following oral history interview took place with Dr. John Newsom-Davis on September 26, 2005. During the interview Dr. Newsom-Davis talked about his early education and service with the RAF[Royal Air Force], his years at Cambridge, decision to go into medicine, his decision to become a neurologist and his training, his years at Queen Square and The Royal Free Hospital, his research into breathing disorders, including his work with Dr. Fred Plum in the United States, his teaching, clinical work and research at Cambridge and Oxford on myasthenia gravis, his current work including NINDS grant, his editorship of “Brain”, and his comments on the ANA awards he’s received, and on the future of neurology. This interview was made for the American Neurological Association Oral History Project and the interviewer is Barbara W. Sommer. Dr. John Newsom-Davis: JND Barbara W. Sommer: BWS Tape One Side A BWS: The date is September 26, 2005, as part of the American Neurological Association Oral History Project, I am talking with Dr. John Newsom-Davis from Great Britain, from Oxford, and also formerly from Cambridge. We are going to be talking about his work in Great Britain and around the world. Would you like to start by telling us how you began to think about going into medicine? JND: At school I’d read arts subjects. I didn’t do any science there and was going to read English at Cambridge. I was offered a place at Pembroke College to do that, but the Government required one to do 2 years military service and I thought it would be good fun to fly, certainly better than being in the Army. So in 1951 I joined the Royal Air Force [RAF] and was fortunate to be selected for pilot training, which very few of us were. Training started in Tiger Moths, a biplane with an open cockpit designed in the 1930s, followed fortunately by more advanced planes. I obtained my Wings in 1953 which was a proud moment. I then graduated to the twin jet-engined Meteor, which was exhilarating to fly. But it was during that time while I was flying that I began to rethink my career. My mother’s father had been a doctor and she had always been keen that I should do medicine – mothers know best! I had the idea that perhaps I would become a psychiatrist. [mother: Eileen Newsom-Davis, father: Kenneth NewsomDavis] [Brief pause in interview] JND: So, while still serving as a pilot, I started covertly to read biology in preparation for applying to medical school. I say covertly because I didn’t let on to my commanding officer what I was up to. The Air Ministry wanted to keep us all in the RAF in case of future wars and the like. A friend of mine was rash enough to say at one Mess dinner that he was planning to enter the Church on leaving the RAF. Our Commanding Officer immediately grounded him because they had no wish to train a flying priest. So I kept quiet about my medical intentions and declined to stay on beyond the statutory 2 years. 18 To round off the account of my RAF experience, I can add that a group of us met in 2003 on the fiftieth anniversary of our obtaining our Wings, We stayed in a pub in the West Country close to the airfield where we trained and had a terrific time. As it happened, linking the present with the past, I had a patient with myasthenia who was in air reconnaissance and who offered to take an aerial photo. So, as agreed with him, we arranged our cars on the runway to form the letter L (for ‘fifty’ of course) at precisely 1100 hours. As so often in England, the cloud base was about 50 feet but fortunately he had an infrared camera. He went over at 30,000 feet or whatever and got the photograph of us all there in L formation. When that was over, we got into our cars with our partners beside us, drove down runway in formation and peeled off just as we used to do when flying. So it was a great time. I left the RAF in 1953 but because I had done no advanced science at school I had to go to a ‘crammers’ i.e. a tutorial college and take senior school exams in physics, chemistry, botany and zoology in about nine months.. Cambridge University had allowed me to switch subjects from English to Natural Sciences (the pre-clinical basic science medical degree). During my 3 years at Cambridge I had a good time, played tennis and hockey for the college but was not very industrious. I remained more interested in arts subjects at that time and my friends were in those fields. I didn’t really get excited by medicine until I went to do the second (clinical) half of my training at the Middlesex Hospital Medical School in London to do the clinical work. But then I began to see how tricky studying psychiatry might be and I became very much less sure that that was the way I wanted to go. BWS: Why tricky? JND: At that time, at least to a medical student, there seemed to be too few landmarks in a vast ocean! Biological psychiatry was not well developed, as it is now, and the different theories (Freudian, Adlerian, Jungian), while intellectually interesting, seemed to me to be of uncertain validity at least in the context of therapeutic medicine. So, I found myself becoming increasingly interested in neurology. BWS: How did that happen? JND: While I was on the neurology wards as a medical student I came under the influence of two impressive neurologists. The first was Dr Michael Kremer, a neurologist who was extraordinarily sharp and who had a remarkable flair for diagnosis, (though it was not always possible – for a medical student - to follow the thought processes by which he reached the right conclusion). But one of his axioms was ‘If you can’t make the diagnosis, take the history again’ – valuable advice that is as relevant now as it was then. The other neurologist who taught me at that time was Professor Roger [W.] Gilliatt who had a joint appointment between the Middlesex Hospital and Queen Square [The Institute of Neurology and National Hospital for Neurology and Neurosurgery, London]. He was a very powerful figure, and a pretty daunting one for a medical student. He was a very good teacher, if somewhat didactic. I believe my interest in neurology – and decision to make that my career goal – stemmed from student experiences then. I got my first ‘house job’, i.e. my first internship, on the Professorial Medical Unit. This was a prestigious appointment and I never quite understood why I was selected. I got an undistinguished degree at Cambridge where I didn’t work all that hard and had no interest in research. I passed my clinical finals OK but not with any particular distinction (except that I won the Psychiatry prize), and at that time I had no academic aspirations. I was selected for the post by the First Assistant to the Professor of Medicine, E. J. [Edward James] Moran Campbell. Moran later became Professor of Medicine at McMaster [McMaster University Medical School, Hamilton, Ontario, Canada]. His selecting me suggests that he knew something about me that I didn’t know myself! In any event, he was a crucial figure in my finding that investigative/academic medicine was what I liked doing. He himself was passionately interested in research, and a great teacher and I reckon I owe my career to him. He remained immensely supportive through my early career, and I co-authored a monograph with him and Emilio Agostoni, ‘The Respiratory Muscles: Mechanics and Neural Control,‘ while I was still a junior doctor. In order to pursue a career in Neurology I applied for and got the neurologist houseman [intern]. post on Roger Gilliatt and Michael Kremer’s firm at the Middlesex Hospital. As anticipated, it was very daunting. Roger was extremely tough. He seemed to think well of me and a future in neurology began to look possible. He even suggested a period of research with David Whitteridge [Professor of Physiology in Edinburgh]. But suddenly there 19 was a problem. He discovered how old I was. I’ve always looked young and I suppose he thought that, like him, I had qualified at a very young age. Well, I was 30 I suppose at that time – disastrously old in his eyes. And so he said, “You must know that you are too old to go into neurology. Would you be interested in a career in Industrial Medicine?” He was (to my consternation) absolutely serious. So I realized that I would need to distance myself from Roger. My next post, as part of my general training in medicine, was at the Royal Brompton Hospital for Diseases of the Chest (as it was pedantically known) [London]. Because of my neurological interests, I suppose, I became interested in the neural control of breathing. And through Moran Campbell, I obtained a research fellowship to work with Tom Sears, [now Professor TA Sears] who was to become the Professor of Neurophysiology at the National Hospital, Queen Square. With Tom as my supervisor, I wrote an M.D. thesis on respiratory sensation. Tom was both encouraging - and tolerant - of someone like myself with no previous background in research. Crucially, too, he protected me from Roger Gilliatt! He was a wonderful teacher, and is still very active in research. So I was awarded my M.D. (by thesis) and life became a little easier. I was appointed to the House at Queen Square [equivalent to a Residency], working for many different neurologists. BWS: You received the Queen Square prize for neurology. JND: That was really for the M.D. thesis that I had written on sensation in breathing.1 Queen Square was unquestionably an interesting place. Perhaps there has always been a tendency toward ancestor worship in the UK. There were a number of well known names at the time I went there. Macdonald Critchley had retired by then, but visited for special Grand Rounds. and was a skilful performer though – before the time of CT and MR imaging – the only check on the accuracy of localization was the autopsy, that could be many years away… So his conclusions could never be challenged. My first chief was Sean McArdle, not well known internationally but an acute and entertaining diagnostician of peripheral nerve disorders. He was the first to describe the carpal tunnel syndrome. He was an Irishman and, at the time I worked for him, had no family life I believe (he married later), so he would work Saturdays, especially Saturday afternoons. It drove my wife [Rosemary] crazy, wondering why/how this man ‘could do this to you’ (and I, so recently married) on a Saturday afternoon. I also worked for Dennis Williams (at the time when his son – now an internationally recognized authority on rectal diseases - was the Intern – a well-known figure in the field of epilepsy and the EEG). He was also Editor of Brain at that time and my opinion was sometimes sought on the submissions… BWS: These were people who actually had come up learning neurology through an intense look at patients and understanding, an intuitive process? JND: Absolutely, because in those days, scanning was in its infancy. There were cerebral arteriograms and the (dreadful) air encephalogram, when air was injected at lumbar puncture and the patient positioned so as to get air into the ventricular system usually with the patient vomiting. It was the most horrible thing! Patients have every reason to be grateful for the medical physicists who made computerised tomographic and MR imaging possible. BWS: What would you say you took away from that time? JND: Learning is a selective process, I suppose, and I think also that what made the subject really interesting for me was thinking about investigative possibilities in the research sense, not just in investigating a patient, but what studying the disease might tell you about pathogenesis. I finished at Queen Square as the Resident Medical Officer (RMO), equivalent to Senior Resident. That was the time (1968) of the Daniel Cohn-Bendit riots in Paris,2 which, curiously, impacted on the behaviour of the hospital 1 2 CITATION PLEASE The May 1968 student riots against the government of Charles de Gaulle in France. 20 junior staff. Traditionally, as well as looking after the NHS patients, the junior staff cared for the private (feepaying) patients of their consultants who were accommodated in a separate wing of the hospital.. This often meant a lot of extra work, getting in early in the morning, clerking these patients, organizing blood tests, doing lumbar punctures, and so on. Although the Consultant received fees from the Private patients, in most cases the junior staff did not. Perhaps influenced by the events in Paris, the Junior Staff gave notice to the Consultants that they would no longer look after the Private Patients free of charge. I remember that the junior staff member who was expected to look after Dr. MacDonald Critchley’s patients announced that he would no longer do so. So I had of course to give this unwelcome news to Dr. Critchley, offering to see his patients myself free of charge for the final 3 months of my tenure as RMO, but informing him that thereafter he would either have to look after them himself or pay a fee to have a member of the junior staff do the work. I was later told that I was branded a “Communist” at a meeting of the National Hospital Medical Committee (learning of this, my wife said, “You, a Communist?”). [Laughs] Anyway, the fact is that, thereafter, Consultants started to pay their junior staff and so a small social change was achieved. Then I had another stroke of good fortune. Partly because of my interest in breathing, I came to work with Dr. Fred Plum (New York Hospital-Cornell Medical Center) who obtained a research fellowship for me in 1969. As a result of that, my wife and I (we had no children at that time) spent a wonderful year in Manhattan. Fred was terrific! He was a fantastic teacher, hugely knowledgeable, and an excellent clinician. To digress for a moment, I saw him last night with Susan. He is not well now, but nevertheless he greeted me most warmly. It’s great that there’s going to be a Symposium in his honor this afternoon. Fred Plum was already an international authority on the neurology of breathing which was the field of my research. I learned a lot. He was a busy man and he couldn’t spend a lot of time in the lab, but he did what he could to support me. Also, as a research fellow, I went on his teaching rounds and did a bit of teaching myself, I guess. He was a superb teacher, but he was also a very hard taskmaster. He was kinder to me than to the Residents! He was a bit like Roger Gilliatt in some ways; he was very tough on them. But I think one has to say that that worked. A number of his Residents have gone on to head neurology departments or to have successful research careers such as Marc Raichle, Clif Saper, and Fred Lublin, who were contemporaries of mine there. Such an outcome is a sign of a great teacher – and also of someone who selects well! My wife and I had a great time in Manhattan, and Fred was most welcoming socially, as was his then wife, Jean. Happily, too, we conceived our first child there. I have kept in touch with Fred ever since and he has remained over the years a great source of support and guidance. Looking back, I have to say how grateful I am to the individuals who have helped me throughout my career. The next was P. K. Thomas, Professor P. K. Thomas, who now unfortunately is terribly damaged from a major stroke. I saw him not long ago and he’s a shadow of his former self. For some reason that I never quite understood, he encouraged me to apply to join the consultant neurology staff of the Royal Free Hospital. I was interviewed and got the post. That was in 1970 when I was still doing work on the Control of Breathing. I was interested in the pattern of breathing in disease and was recording from patients during the night - and it was pretty demanding. I think my wife became quite suspicious of what I was up to, so many nights away… With David Stagg, we developed a computer-assisted method for recording breath-by-breath changes in breathing during sleep. It was very often the case that the patient was awake while the investigator was asleep. [Laughs] At that time, I also began to study human intercostal muscle spindles in vitro, wishing to characterize their response to stretch. This meant my obtaining human intercostal muscle from patients undergoing thoracotomy, then isolating them under the dissecting microscope and recording from their afferents in vitro under conditions of controlled stretch. This research on human muscle spindles resulted in a paper in the Journal of Physiology3 and I was pleased about that, but – fortuitously really – it led to a complete switch in the direction of my career. It was in about 1973, and came about in this way. [Sir] Bernard Katz, the Nobel Prize winner, 4 and Ricardo Miledi (now at UC, Irvine) who worked with him in the Department of Biophysics, University College, London were world authorities on the neuromuscular junction and had become interested in myasthenia. They wanted to obtain human intercostal muscle 3 4 INSERT CITATION Sir Bernard Katz was a winner of the Nobel Prize in Physiology or Medicine in 1970. 21 to count the number of acetylcholine receptors using radio-labeled alpha-Bungarotoxin. Ricardo Miledi knew Tom Sears, my ex-supervisor, who put him in touch with me. Naturally I was glad to assist and so obtained human intercostal muscle for their in vitro studies. I was rewarded by being able to see Katz and Miledi working together in the laboratory, a real privilege because I gather that normally no one was allowed in the room when they were experimenting. As I remember it, Ricardo was doing the experimentation and Bernard Katz, was walking up and down, making comments and suggestions. I felt immensely privileged to be present. I remember some years later that he told me how much he would have liked to have been, like me, a doctor. He was of course a refugee from Europe, and that career – perhaps fortunately for neuroscience – would not have been open to him in the UK, though I am sure that he would have been a wonderful doctor. The contact with Katz and Miledi had two important outcomes for me. The first was an awakening of my interest in the neuromuscular junction. The second was my meeting Angela Vincent who at that time was their lab assistant. (As it happens, she is here at the meeting today). She had qualified in medicine but didn’t really want to be a doctor and had always been interested in research. At that time I was also running the intensive care unit at Queen Square with Roger Bannister (now Sir Roger Bannister, famous as the first 4-minute miler), where we looked after a number of patients with Myasthenia Gravis. We had a very bright, young houseman called Tony Pinching (now Professor AJ Pinching) who had worked with Keith Peters (now Professor Sir Keith Peters). In 1976, we decided to plasma exchange a woman with severe myasthenia gravis because it was suspected that antibodies might be causing the disorder. Dan (Daniel B) Drachman had already shown that immunoglobulins from these patients can produce a disorder of neuromuscular transmission in mice, I had first encountered the patient when I was a medical student. She had very severe myasthenia and was in and out of respiratory care. Within 72 hours she showed a truly fantastic improvement, consistent with the known antibodies to muscle acetylcholine receptors being the effector mechanism underlying myasthenic weakness. Our paper – the first describing the benefits of plasma exchange in myasthenia was published in the The Lancet5 on December 26th, the day after Christmas, and perhaps because of its timing, was little commented upon. This was the final event in my career conversion from neurophysiology to neuroimmunology. I saw this area as having real potential. But, trained in neurology and neurophysiology, I had become out of touch with current developments in immunology. The subject had moved on since I had been at Cambridge 15 years before. So I went to night school – I was then over 40 years old, and retrained. I was very glad I did because the field was taking off in neurology. Its main attraction for me was its potential to provide insights into disease pathogenesis that seemed so rarely to be provided by neurophysiological studies. So with Angela Vincent, I successfully applied for a project grant from the MRC [Medical Research Centre] to follow up the plasma exchange work and we started doing some experimental studies in P. K. Thomas’ department at the Royal Free Hospital. PK was extraordinarily supportive and generous. He was passionately interested in research himself and was a superb experimenter, being an international figure in the field of Peripheral Neuropathy. He protected me from having to do excessive amounts of clinical work and allowed our group to grow. Angela and I later obtained a 5-year MRC program grant and the group steadily expanded. In 1980 I was awarded the (first) MRC Clinical Research Professorship. Angela Vincent and I were joined by key individuals: Nick Willcox (now Prof Nick Willcox, cellular immunologist), David Beeson (now Prof David Beeson, molecular biologist), and Beth Lang (immunochemist). Interestingly, we are still together 25 years later (I am Emeritus, and Angela heads the group – and incidentally is also Chairman of the Department of Neurology now). Keeping research teams together is something that may be easier to achieve in the UK than in the US. This may be because funding agencies in the UK recognize that it’s a sensible thing to do! In the U.S., researchers seem required to demonstrate their research virility, as it were, by leaving the group and moving elsewhere. This can be highly disruptive to long-term programs of clinical research. We then became interested in the Lambert-Eaton Myasthenic Syndrome [LEMS] and, with Beth Lang and Denis Wray (a neurophysiologist working at the Royal Free Hospital) we showed that the impaired neurotransmitter release was due to antibodies against nerve terminal voltage-gated calcium channels. I actually first presented those data at a meeting in Ed Lambert’s honor, as I recall. He was the first to define its neurophysiological features. To 5 INSERT CITATION 22 be able to present evidence on such an occasion that the syndrome named after him was antibody-mediated disease was very exciting. Our discoveries in myasthenia and in LEMS encouraged us to look further for antibody-mediated diseases. In 1990, I was doing a clinic in Athens with a colleague of mine, Professor Alex Papadimetriou, when he showed me a major in the Greek Army who had widespread muscle twitching called neuromyotonia. I’d not seen it before and by then (I’ll come back to that in a moment) I’d moved to Oxford. But keeping the research theme going for a moment, when I got back to Oxford, I did a Medline search that revealed its reported association with thymoma, myasthenia gravis and small cell lung cancer. This strongly suggested to me that the disorder must be antibody-mediated, and that the likely target would be voltage-gated potassium channels (VGKCs), because their loss would lead to nerve hyperexcitability (that characterizes neuromyotonia). A series of experiments in our lab over the next few years confirmed this, and later led to the recognition that the these antibodies can associate with limbic encephalopathy and may be targeting CNS VGKCs, work with which Angela Vincent has been especially involved (she is talking about this work here at this meeting). So over the years we’ve been able to move from the postsynaptic AChR to the presynaptic VGCCs, to peripheral nerve VGKCs and finally to CNS VGKCs. BWS: With this, you were able to develop something that provided potential to understand? JND: Exactly. It turned out to be an experimental paradigm that we could move from disease to disease to disease. And in work led by Angela, we have very recently discovered another antibody in myasthenia against MuSK [muscle-specific receptor tyrosine kinase] that’s actually not an ion channel but a transmembrane postsynaptic protein that plays a key role during muscle development in clustering AChRs under the in-growing motor nerve terminal. So antibody-mediated autoimmunity turned out to be a very good area to be in – and a field in which it was much easier to see the way ahead than in MS, for example. Importantly, too, it has opened the way for new treatments. BWS: Was MG a relatively obscure condition? JND: Well, although it was known to be a disorder of the neuromuscular junction, its pathogenesis certainly was obscure up until 1973, and the crucial observation by Patrick and Lindstrom that rabbits immunized with Torpedo (electric eel) AChRs developed an MG-like illness and had AChR antibodies in their serum. But the clinical disorder has always interested physicians. It is usually said that the first description of MG was by Thomas Willis in the 17th century;6 it was certainly a very convincing account. But actually I’m fairly sure that the story of Samson (Old Testament, Book of Judges) is the first description of MG, and I presented the evidence for this to the British Association for the Advancement of Science when I was president of the Biological Section quite a number of years back now. You may recall that Samson, a man of exceptional strength, became extremely weak at the same time as he lost his hair. I have more than one patient with MG and alopecia (hair loss) and both are, of course, autoimmune disorders. The Biblical account, written by his own tribe, was that Delilah (who was of a different tribe) seduced him, discovered (allegedly) that his strength depended on his hair, and arranged to have it shaved off. There is a wonderful Rubens’ painting in the National Gallery of Samson in ‘myasthenic crisis’ with bilateral ptosis and lying in a posture of extreme fatigue with his head on Delilah’s lap – she’s naked from the waist up – with the barber in the process of cutting off his hair. To my surprise, the morning after my presentation, The [London] Times carried an article with the headline: “Samson and Delilah Story Re-told” and it was even reported in The Boston Globe. The UK Daily Express (a scurrilous paper in my view) dismissed the evidence, simply concluding that ‘this feminist story was concocted to hide the fact that one of the worst examples of sexual harassment in history was committed by a woman.’ [Laughs] So let me go back now to my career. I was MRC Clinical Professor in 1980 and was doing my research at the Royal Free, and my clinical work mainly at the National Hospital, Queen Square. I was then approached by an Oxford colleague asking if I would be interested in the Chair of Neurology at Oxford. Naturally I said I would be! I duly prepared my CV but was never formally interviewed. When I was offered the position in 1987 I had a group of 12 or more researchers at the Royal Free Hospital, and would not have been prepared to move if they had not wished to 6 Described in 1672. 23 come with me. Happily for all of us, they did. We were the first group to move into the new Institute of Molecular Medicine (IMM) which had been founded by Professor David Weatherall, [now Professor Sir David Weatherall]. Five large furniture removal vans filled with our deep freezers containing serum samples and plasma came with us, on which much of our research was based. BWS: What were the differences between the Royal Free and Oxford? JND: The Royal Free environment had been extremely supportive, but molecular medicine there was on a much smaller scale. At the IMM, other groups with other experimental skills soon joined us, providing an exceptional research environment. The building was newly designed, spacious and with excellent laboratory facilities – and the first Institute of its kind in the UK. But I was also at Oxford the Head of the Department of Clinical Neurology that carried with it many other new responsibilities. BWS: What were your goals? What did you want to do in the department? JND: My principal aim was to advance research in the department. My predecessor was a superb clinician, Professor Bryan Matthews, and wrote a wonderful book on Practical Neurology. He did some really interesting and important work on CJD [Creutzfeldt-Jakob disease] that was to prove of great importance some years later with the epidemic that developed in the UK. My anesthetist colleague with whom I had worked for many years at Queen Square looking after MG patients, Dr. Laurie Loh, fortunately for me agreed to come to Oxford too, as did my clinical neurophysiologist colleague Dr. Kerry Mills [now Professor Kerry Mills] neurophysiologist. The clinical and teaching demands were heavy. I was always expected to do two or three outpatient clinics a week, as well as departmental administration, sitting on national committees, (for example, as Chairman of the MRC Neurosciences Board), so life was busy. But I always went to the lab twice a week and, though I wasn’t doing experiments, I knew what was going on and had this excellent working relationship with Angela, Nick Willcox, David Beeson and Beth Lang, which indeed continues because I continue my clinical research there and still attend the lab meetings. BWS: Still working on myasthenia? JND: Yes, and on the other antibody-mediated disorders. But additionally, headed by David Beeson, we have for 15 years now been working on the inherited (‘congenital’) myasthenic syndromes – a field pioneered by Dr. Andrew Engel at the Mayo Clinic. I still do a monthly ‘Congenital Myasthenic Syndrome’ clinic to which patients come from all over the country (supported by the UK Department of Health). These disorders have turned out to be genetically heterogeneous and novel genes continue to be identified as sites of mutations . BWS: Yours has been described as a superb research and clinical team at Oxford. JND: That’s definitely because of excellent teamwork! For me, being elected in 1991 a Fellow of the Royal Society [FRS] was an honor as much for the team as for me. BWS: How did that come about? JND: Clinicians are not often elected as Fellows, and the selection process is long (up to 7 years) and a successful outcome is very uncertain! When you are nominated, you have to provide an outline of your research and a list of publications. BWS: You have an M.D. from Cambridge and D.M. from Oxford? JND: That’s a slightly strange story. The medical degree in Cambridge (where I studied) is called ‘MB, BChir:‘ Bachelor of Medicine and Bachelor of Surgery. That is equivalent to M.D. in the US. I obtained those in 1960. In England you get an M.D. on the basis of writing a thesis on a piece of experimental work, and this I was awarded in 1966. Oddly, you can’t be appointed to a Chair in Oxford without an Oxford degree. So in order to allow me to be appointed to the Chair, I was awarded an Honorary DM. I’m very proud of it, but did no work for it! 24 BWS: Your CBE [Commander of the British Empire] was in 1996. That was quite an honor as well. JND: I guess so, but those awards are decided by civil servants, on the basis of testimonials I suppose, and there is an element of chance involved. But with my wife and two of our children we had a jolly day at Buckingham Palace. One shakes hand with the Queen (even the boldest of men – and women - find this an anxiety-provoking experience, I suspect, despite her mildness of manner). She wears gloves and one can also do so oneself, but the rules are that one wears either gloves on both hands or no gloves; you’re not allowed to wear a glove only on one hand! The Queen asks everyone a question, prompted by an aide. I was asked where I worked. It is said that if you are interested in horses you may get several questions, but I have no evidence to support that! BWS: Did you wear gloves or no? JND: No gloves. BWS: But she did, and she shook your hand? JND: She did! BWS: How does funding come about? JND: Almost everything we have done has been dependent on raising research money. Apart from my salary, and some minimal support from the University, we have been dependent principally on five-year Program grants from the MRC. Rather like the American system, I believe, we had to apply for renewal every 5 years, and were fortunate in be successful over 20 years. But we also got support from other funding sources as well, Medical Charities and private Research Foundations. I sometimes thought that, in trying to bankroll the activity, it would have been better had I trained as a merchant banker rather than as a scientist! The MRC also seemed genuinely keen to support clinically-orientated research. BWS: They saw value in the kind of clinical research, the obligations of research to clinical patients? JND: Absolutely. I guess they could see the progress we made each time we applied. Having enough money to do what you wanted for 20 years and never having to apply for it would be very nice but, agonizing as those the fiveyearly re-applications were, they certainly focused the mind! Also, as head of the group, one found it easier to say to some people, “You know, we can’t do this, we can’t go in that direction.” I think we were a reasonably happy group – perhaps our staying together for so long is evidence of that. Angela Vincent and I have always got along extremely well and she was a key person in our success. Each of us brought something different to the group. She has a superb critical mind and essentially managed the lab, while I brought the clinic on board, as it were. I think that the union, scientifically speaking, between a clinician who’s passionate about science and a scientist who is strongly motivated to work on clinical problems, is hugely valuable. I am sure it has been crucial to our achievements. BWS: So you have the exchange between the two and you’re actually both learning and bringing that what you’re learning? JND: Absolutely. So I continued working at Oxford doing 2 or 3 clinics a week until, in 1998, I became Emeritus. In 1997 I was asked to be the editor of Brain. I’d been the Secretary and Treasurer some years before. Brain is nominally ‘owned’ by its Guarantors , a group of neurologists and neuroscientists. My predecessor as Editor was Professor Ian McDonald for whom I have the highest regard. When I took over Brain, there were about 500 papers a year. The first year was really tricky because I was living in Oxford and I was commuting to the Brain office in London several times a week, but when I became Emeritus, I could focus a bit more. I decided that I really wanted to try to change how the journal was perceived and what it did. I had a very good deputy editor, Professor John Rothwell, a neurophysiologist, who looked after the manuscripts in that area, while I dealt with almost everything else. Very early on I decided to take the journal on-line, which was kind of bold because the systems for that weren’t all that well developed at that time. There were inevitable teething problems, but it proved undoubtedly the right thing to have done. From then on, the impact factor steadily rose, followed by an equally steady increase in the number of submissions. I used a large number of new North American referees which may have led some to see – 25 for the first time – how good the journal was and to consider submitting manuscripts themselves. Probably the most important move was putting the journal submission process on line so that delays were minimized. Manuscripts from Australia or the USA, for example, could be viewed as quickly as those from the UK. I managed everything from my laptop – no paper manuscripts - and I had superb support not only from John Rothwell but from the Editorial Office staff, Carol Lovelidge (Assistant Editor) and Lubna Zafar. A very small team! But the much faster turnaround time and the great increase in the number of submissions meant that the workload got heavier and heavier. I genuinely never took a holiday from the journal for 7 years - for example, on holiday in the West Indies or wherever, my latest little grandson vomiting down my back, being bitten by mosquitoes, I was still working away at the laptop, connecting – somewhat uncertainly - with the online system via dial-up (no fast Internet connections there in those days). Somehow I managed to get on-line in Barbados – that was always difficult I remember. Evidently the readership liked that, as shown by the steadily increasing number of papers – from about 500 a year when I took over the journal to about 1200 when my term as editor ended. I was taking decisions on 3 or 4 papers a day, every day. People sometimes said to me, “Do you read them all?” and I would reply, “Just think about that. How could I read four manuscripts of 6000-8000 words (or more) every day and get anything else done?” BWS: How did you decide? JND: I read the Introduction and the Summary. I got good referees. Referees are much more important than authors! And if occasionally a referee didn’t deliver, I would never use them again. But some referees are fantastic, they would write 2 or 3 pages of cogent criticism; authors don’t always realize how lucky they are to have somebody read and comment so carefully. As time went on, we had to turn down more and more papers and we were only accepting 1 in 5 by the time I left. I rejected 10-15% without sending them out for review because I judged them unsuitable for the journal and didn’t want to overload the referees. Quite surprisingly really, I got very few angry letters. I always provided a brief statement of the reasons for rejection. We all feel bad when out paper is turned down, and sometimes I would remind a distressed rejected author that editors have had their papers turned down too! You know, it’s very, very upsetting if you think you’ve got something good there, particularly if you think the journal’s been unfair. Over my years as editor, the impact factor of Brain had been steadily increasing finally, in my last year, overtaking the Annals of Neurology, which for year after year had had the highest impact factor of any neurological journal. Impact factors are certainly not the only criterion by which a journal should be judged, but authors (and their Deans!) like their papers to be published in journals with high impact factors. Additionally, it says something positive about clinical research being done in Europe, because many of our papers came from there. So when we see our impact factor actually slightly higher than the Annals, it underscores the quality of the research being done in Europe – Germany, Italy, France and the UK. There is no denying my satisfaction had having achieved this. Maybe I shouldn’t be saying that on an ANA interview. BWS: Well, you can tell me a little about ANA and your thoughts about it. JND: It’s a meeting I really like coming to. It’s very different from the AAN meeting – it’s much more focused on academia, it’s smaller, the meetings are much easier to encompass because there are no parallel sessions, and of course I have many friends amongst the members. BWS: But you are an honorary member of ANA? JND: Yes I am, and that was a very nice thing to happen and I’ve also become a Foreign Member of the Institute of Medicine. One’s colleagues, I suppose, put you up and vote for you, and that’s very nice. Science has been very good to me. I think if I’d done nothing but clinical work in my career, I would soon have become be bored. Always the exciting thing for me was the research element. That’s no doubt why, though Emeritus, I am continuing clinical research. and I think people who like what they do, go on doing it. To illustrate that, I will tell you what I am doing now. You may know there’s an operation called thymectomy recommended for patients with (non-thymomatous) myasthenia. The first thymectomy on a myasthenia patient was actually done in Zurich in 1911 and neurologists have been recommending the operation for many of their patients, but nearly 100 years later we still don’t really know whether its of benefit or not. So I thought I can’t leave the field until I get an answer. Suppose one of my children [daughters: Amelia and Imogen, son: Thomas] comes to me and says, “Dad, I’ve been told I have got myasthenia; should I have a thymectomy?” I would have to say “I don’t know.” “You don’t know, Dad? But this is 26 your disease!” So, about 3 or 4 years ago I got a small group of interested people from the US together to try to get research funding for a Randomized Controlled Trial of thymectomy in Myasthenia. The MRC (UK) didn’t want to support it. We put our first grant into NINDS (National Institute for Neurological Disorders and Stroke) in 2001, with further applications in 2003 and 2004, when the grant was finally awarded (a few days ago, in fact), with Gary Cutter (Dr. Gary Cutter, Professor of Biostatistics, UAB), as my co-applicant. We are strongly supported by the other members of the Executive Committee, Gil Wolfe, Henry Kaminski and Alfred Jaretzki III. We now have nearly 70 centers worldwide, 27 in the United States, and the clinical coordination is done from my laptop. Briefly, the aim is that both groups will receive the minimum dose of prednisone necessary to achieve and maintain ‘remission,’ administered by a blinded doctor. One group will be randomized to thymectomy. The outcome measure is essentially the cumulative prednisone dose. If this is substantially lower in the thymectomy group, the operation will be judged to be beneficial. BWS: What do you see for the future for this type of project and work? JND: Well I have comments about that. First I think the review process by NINDS is very good, it’s very, very thorough and you actually meet not only the NINDS staff but also the review committee. But it’s extraordinarily lengthy, and time-consuming, and one can be at the mercy of a single review committee member whose quirky views can torpedo the application. The process of obtaining IRB/Ethics committee approval is also becoming increasingly difficult, especially in Europe, where the review committees seem more concerned about protecting themselves from having overlooked even the most minor of issues, losing sight of the fact that the outcome of the study could be of great significance to patients with the disease. In our case, the treatments are both regularly in use in the clinic – we are not testing anything new, just seeing whether a treatment used for nearly 100 years is actually helpful to patients! There is even an unpleasant reminder in the Ethics application form that if you make any false entries, you’re liable to criminal prosecution, as if those of us applying to do clinical studies should be regarded as inherent felons. Soon younger clinicians may no longer want to undertake studies of this kind. So maybe it’s the sort of thing that’s only good as occupational therapy for an older man. BWS: You inform the patients obviously of the trials? So they have to be aware? Which may be off-putting? JND: Certainly everything – rightly – has to be explained to the patient, who is under no duress to take part. BWS: Where do you see things going in the future in general? How do you see things developing? JND: That’s a very difficult question to answer. It may depend in part on which country you work in. In the immediate area I think clinical research may become difficult to do. In this country, as I see it, a lot of research is done by people from other countries who come here on fellowships and then often go back to their own countries. I was at UCI, as I mentioned, a couple of weeks ago – talking to the residents there – and I’m sure what they told me reflects what residents do elsewhere. Many doctors by the time they qualify are deeply in debt and if you’re in debt, research isn’t the area to go because you’re not going to make much money. In England, long ago (in the 1950s and ‘60s), the only people who could afford to do research were people who had private means. That’s changed now, fortunately. But research, with all its uncertainties, can be a daunting prospect especially if you are in debt since your student days, married perhaps with a young family and a mortgage. Will you be able to get funding? Will you run out of ideas? But I hope that clinicians will always continue to do research and that research will not be dominated by non-medically trained Ph.D.s. I think that that would be a pity because many research opportunities will be lost if that happens. A lot of excellent clinical science has come out of U.S. neurology departments headed by really good scientists, who also see patients. I believe that to be very important. I don’t want to speculate on the way medical advances may go. To medics starting out and considering a research career, I say that they have to try to find a research area that they think has ‘lift’. Don’t necessarily stay working too long with a great clinical scientist. He may write you a good reference but his research may be in an area that is fading. BWS: Is there anything else? You’ve seen neurology during the period and very interesting changes and growth, any comments you want to talk about? 27 JND: There have been huge changes. But here is a slightly wry comment. I think we’ve been lucky to work in a disease where the drug companies don’t have any input. And you can see the evidence for that because we don’t get paid to go to meetings because no drug company is interested in our disease! It’s too rare. But that does, in a sense “keep you pure,” – it means that you follow the science really. So I don’t regret that. And, our approach has been highly focused. BWS: As you look back, what about MS? JND: There are so many other outstanding clinical scientists working in that area, and so much research has been done, but – as I speak – understanding the pathogenesis of MS remains elusive. I could not see the way ahead in that disease. For us at least, it has been more profitable scientifically to have worked on antibody-mediated ion channelopathies. BWS: Thank you. End of interview ADDENDUM Dr. Newsom-Davis also described several personal experiences regarding experiments on himself. This was prior to the ethics controls now in place: JND: When working as a resident at Queen Square, I started doing some studies with Tom Sears. I never let on that I was experimenting because you were expected to be looking after patients all the time. We were doing some experiments in which we were looking at the stretch reflex in the intercostal (breathing) muscles. The experiment we set up was quite complicated. The subject’s airway was connected to a drum that was a high pressure source. It was very briefly opened and when it opened, the chest was suddenly forcibly expanded. We recorded the associated electrical activity in the breathing muscles with a pair of insulated wires cut off at the tips that served as the recording electrodes. These were fed down an ordinary serum needle and inserted into the chest. The location of the needle was determined by listening to the EMG activity. The external intercostal muscle is inspiratory and the internal layer is expiratory. In one of these experiments we were recording from the diaphragm, which is a bit more difficult – you have to try to insert the needle below the lowest point of the lung. We got some nice recordings from my diaphragm, but I got a lot of pain. My vital capacity dropped which I attributed to pain. So I went home and to bed that night. As I lay back in bed I remember saying to Rosemary, “There’s something moving in my chest.” So I sat up – and felt my collapsed lung (as it turned out to be) hit the inside of my chest – it felt like a wet fish. One tries to disbelieve something like this so I didn’t do anything that night – I think Rosemary was a bit worried. But I went to the X-ray department at Queen Square next day which was (then) at the top of 3 flights of stairs. I was very breathless by the time I had run up to the top, and sure enough, the X-ray showed a pneumothorax. So I rang up Moran Campbell, my old mentor, for advice. In those days treatment often involved inserting a big rubber tube into the chest. I didn’t want that, so Moran kindly referred me to a very conservative chest physician who said, “I’m sure it will re-expand, but just be careful.” There is one nasty complication called a tension pneumothorax when the opening in the lung acts as a valve so that every time one breathes in the pneumothorax gets bigger and the lung gets smaller. In the limit, it pushes the heart across and compresses the other lung and you’re in bad trouble. The ‘cure’ is to insert another needle into the pneumothorax to relieve the tension. So for several days I carried a needle around with me, just in case. Happily, I never needed it. BWS: You were experimenting on yourself? JND: Yes. We had no ethics approval; one never did in those days. With Moran Campbell I was involved in some control of breathing experiments. He wanted to see how long he could breath-hold and whether the breathing muscles themselves had anything to do with that. To test this, he allowed himself to be totally paralysed with curare. Now curare paralyzes the neuromuscular junction and causes complete paralysis in its victims. To enable him to communicate while paralysed, a cuff was placed around one arm allowing him to signal with the unparalysed hand. The upshot of it was that in that situation he could breath-hold indefinitely. They were quite frightening 28 experiments! But they showed that the distress we all feel at the breaking point of breath-holding – when coming up for air when swimming under water for example - appears to require the normally intense activity of the breathing muscles at that point, driven by afferents from the vagus nerve. I went on to show with Tom Sears in some similar recordings, again from my diaphragm, that during a breath-hold the breathing muscles are at first silent. Then, as the CO2 stimulus increases, the diaphragm starts to contract rhythmically associated with the first feelings that one needs to breathe. As the breath-hold continues, the alternating contractions of inspiratory and expiratory muscles become more and more vigorous and the distress progressively increases too, up to the breakpoint. But when your breathing muscles are paralysed, no breathlessness develops. 29 D. John’s Early Life Julia Medd My remit was to start at the beginning! John and I were twins and born in our paternal Grandparent’s home in Harpenden Hertfordshire, on October 18th 1932. I believe I am right in saying we were born in our Aunt Rosemary’s bedroom and I am delighted she is here with us to-day. John was a rather delicate and small baby, in contrast to his robust and rather larger sister. However he was 10 minutes older than me, something I was not allowed to forget! We had various nurses and nannies in our lives for our first few years. Finally a rather strict Scottish Nanny arrived into our world, to take control of the nursery and the twins. When we were 5½ our youngest sister Anthea was born. Rosemary was reminding me recently of John’s intense dislike of going for walks. This stemmed back I’m sure to the time when every afternoon we were made to walk out with our Scottish Nanny who was pushing a large black pram in which lay her latest pride and joy, our new baby sister. I’m afraid we did not share her delight over this latest arrival! During these walks there were frequent commands such as pick up your feet Julia or stop shuffling John, these put him off going for walks for life! John was sent to boarding school at 7 still small for his age, Dad took a photo of him standing by his upturned trunk. The trunk was almost taller than he, his shorts almost down to his ankles and socks up to his thighs. John hated boarding school; he was a quiet thoughtful child who was not a typical school boy. Years later I met a friend of my mother’s who said to me “Oh yes I remember you, one of the twins, John had the long face of the thinker and you the round face of the doer”. Although we saw little of our Father in our early years, due to boarding school and the war; there is no doubt John inherited some his sense of discipline, focus and social awareness from him. Dad was a prominent member of the Industrial Welfare Society; he was the managing director of his company and was much loved and respected by all his staff including those on the shop floor. John’s love of music came from both our parents and his love of literature, poetry, cooking and gentleness from our Mother. At 13 years old John went on to his public school Sherborne; here he developed his skills on the tennis court and the hockey field and gained a place at Pembroke College Cambridge to read History and English. His place was deferred until after his 2 years National Service which he served in the RAF. Because of the Korean War he was one of a fortunate group of young men to be offered full pilot training. He obtained his wings in October 1952 and was justly proud of the fact that he had also piloted the Meteor Jet. In a recent letter that Angela received from an old RAF mate of John’s, I read of a somewhat Tom and Jerry scenario, when John having landed a twin engine plane saw and undercarriage wheel bouncing down the tarmac in front of him he just had time to report the incident to the control tower when his aircraft slewed off the runway, it was apparent it was one of his wheels. The plane was making straight for a radio control van; the radio crew saw the plane coming, bailed out and ran for their lives. As the aircraft slowed up however, it appeared to be chasing them round their van! John was as helpless to do anything about this, as were his audience in the crew room with mirth. It was during these 2 Years in the RAF that John decided he wanted to become a doctor. Pembroke College was prepared to allow him to change faculties as long as he passed his first MB. This he achieved, studying at a crammers in London, and he went up to Cambridge one year later than he’d originally planned. At Cambridge John worked hard but this did not prevent him taking part and enjoying university life, he also eventually captained his College Hockey team. During his clinical training at The Middlesex Hospital, he played hockey and tennis and made frequent visits to the theatre, concerts and to the opera. He had a wide and varied circle of friends. Clinically he developed a special interest in respiratory physiology and neurology. It was these two special interests that were the fore-runners of his future clinical research in myasthenia. John was amazingly generous with his time and knowledge and family and friends alike frequently called on him in times of trouble. As Rosemary said to me recently “if only John was here he would sort everything out”. It goes without saying that both Anthea and I are immensely proud of all that John has done and achieved in his life, but above all our happiest memories are of him as a proud and loving husband of Rosemary and Father and Grandfather of his children and grandchildren. 30 E. National Service in the RAF Dayne Markham (BOAC/BA retd). John was a member of a very fortunate group of National Service men who because of the Korean War were offered full pilot training in the RAF for their 2 years service. The part of that group of which we were about 45, were called up in Sept 1951 and stayed together for all stages up to and including Wings at RAF Pershore in Oct 1952. We had all got along very well together despite not previously knowing each other and despite quite a disparity of backgrounds. We all felt even at that time that National Service had been a very positive experience for us. In 1992 when I retired aged 60 I resolved to find all the members of the course of 1952 that I could for a Reunion. I had no idea what John had done since the RAF but recalled he had been to Sherborne and they gave me his address, telling me he was probably their most distinguished old boy. I remember being pleasantly surprised and wondering then what had he been doing as he gave no inkling in the RAF other than being very clearly a very good sort. When we met at the 40th Reunion in 1992 he was in appearance and manner little changed from 1952, to my amazement. During the weekend my wife fell down the stairs at the ancient hotel and John took over, recommending my daughter took her to the nearest hospital to check out her hand. He subsequently kept in close touch in RAF matters giving absolutely no clue as to his eminence in his field but being very thoughtful, enthusiastic and always available to help with anything. He said that his time in the RAF had given him the confidence to pursue his career, as before he had no idea what he wanted to do. Subsequently I had a minor scare of an apparent ministroke and he advised my course of action for several years afterwards and he was, of course, spot on. During his flying at Pershore one day in the redoubtable Airspeed Oxford twin he had just landed normally when he saw an undercarriage wheel bouncing down the runway in front of him. He just had time to report the incident to the control tower when the aircraft heeled over and slewed off the runway. It was apparent it was one of his wheels. The aicraft continued to slew round in an arc as the wheel-less leg dug into the turf and threatened to collide with the adjacent Radio Homer Van. The radio crew saw the aircraft coming f or them as they thought and baled out of the van running for their lives. But the aircraft tightened its turn as it slowed up and actually seemed to chase them round the van. Before coming to rest one wing on the turf next to the van. This Tom & Jerry scenario was viewed from the crew room and provoked much merriment. But there was little John could have done about it, he thought he was going to touch the radio van and was more or less helpless, as his audience were with mirth. F. Neurology, ABN and Brain Alastair Compston, Professor of Neurology, University of Cambridge In John were combined the qualities of a fine doctor and a distinguished scientist. He flourished at a time when developments in other branches of medicine threatened to leave neurology in their wake. And whilst many researchactive contemporaries were re-cycling the classical sciences of descriptive neurology, with which academic medicine was losing sympathy, John’s legacy is to have made clinical neuroscience scientifically authoritative in the molecular age. The respect he commanded made John an influential and persuasive spokesman for our subject in many contexts. He was the leading clinical neuroscientist of his generation in the United Kingdom, and a crucial figure in the late-20th century history of world neurology. John was an excellent clinician. Junior staff attached to the Batten Unit at Queen Square, run by John and Roger Bannister in the 1970s, were guaranteed an elite education. The demonstration by John of the most elegant sign in clinical neurology - post-tetanic potentiation of the tendon reflex – might, for example, neatly correct the erroneous diagnosis of myasthenia gravis in a patient referred by a consultant colleague from the Royal Free; anonymous of course but, happily, with us today - Dr Harvey. Brief conversations have far-reaching consequences. In 1976, because antibody had already been implicated in the pathogenesis, Tony Pinching suggested to John that plasma exchange might be used to treat myasthenia gravis. The remarkable effect inspired John to train in immunology, later attending the post-graduate course run by Ivan Roitt and Deborah Donniach at the Middlesex. By now, with a joint consultant appointment also at the Royal Free, John 31 had teamed up with Angela Vincent. This was a formidable combination: the charismatic and energetic clinicianscientist complementing these same qualities in the imaginative and technically versatile scientist-clinician. John first studied the neural control of breathing with Tom Sears at Queen Square. Later, he held a research fellowship with Fred Plum at Cornell Medical Centre, New York, where he met many future stars of north American and world neurology – some of whom are with us today. Tom Sears recalls: “John arrived at my door unannounced, an earnest and enthusiastic young man who pointed out that he was older than he looked and had flown Meteors during his National Service, and as an Officer. I had been an Aircraftman 2 during my own National Service, achieving the second lowest possible rank, and this conversation set the seal on a lifelong professional relationship and friendship. John worked on breathlessness in patients with lesions of the dorsal spinal cord. Later, Ricardo Miledi asked if anyone had access to human intercostal muscle and, since we had made just such recordings by stabbing each other in the back, I was able to recommend the very person”. And as John himself recalled later, this was also the cause of a nasty pneumothorax described to Rosemary during the night that it developed as “like a wet fish - the collapsed lung – flapping in my chest”. The introduction to Tom Sears came through Moran Campbell who had attracted John into investigative medicine after qualification in 1960. And, as with many others of his generation, John was also influenced at the Middlesex Hospital by Michael Kremer. But, unexpectedly and disappointingly, Roger Gilliatt advised John against a career in neurology. We cannot now eavesdrop on that conversation. Gilliatt - the ultimate controller of careers in neurology, scientifically ambitious and motivated by the prospect of great discovery but, in that respect, destined not to make a lasting contribution; and John – older than he looked, attracted to neurology, later elected to Fellowship of the Royal Society for his lasting contributions to medical science, being advised to specialise in Industrial Medicine. The episode rankled and it has a footnote. In 1970, John published The Respiratory Muscles with Moran Campbell and Emilio Agostini. Years later, the copy of this monograph that he dedicated to Roger Gilliatt, turned up in a second-hand bookshop, priced at 50p - a purchase that was brought to Roger’s attention on the occasion of John’s talk at his festschrift in 1986 – provoking a lengthy private explanation from Gilliatt that the book must have been commissioned for sale and without authority by Molly Jenkins, his loyal secretary. Writing a book in his 30s made John wary of repeating that experience, and he did not consider himself to be an especially natural writer, at least of reviews. But he approached original data with appetite and enthusiasm showing a fluency that led to papers of lasting value. He understood and could guide younger colleagues through the many and complex processes of academic life – the ups and downs of presentations, papers, funding and career advancement. He always had the right word of encouragement: made the thoughtful telephone call; sent the sensitive hand-written letter or (later) email; and showed personal interest in those with whom he worked. A locum registrar might be surprised to find a case of wine lobbed through the window of her flat as a wedding present with a friendly note from the delivery boy – John; the 3 year-old daughter of a colleague hosting a professional visit might receive an envelope next day containing several Mr Men books with a note from John indicating that these are ‘rather jolly’ and come with the imprimatur of a highly-respected educational psychologist Rosemary; the lonely delegate at a scientific conference would be asked to join John’s group for dinner; and to spot John and Rosemary across a crowded room somewhere abroad always promised an evening in the company of lively and amusing friends. Few could rival John as a communicator. Nor, in this respect, was there false modesty on his part. Lectures were carefully crafted: the preparation meticulous; the delivery lively; the arguments presented with impeccable logic; the language precise but never indulgent; and the satisfaction of good performance sincerely given and gladly received. On his day, and mostly they were, there was no more intelligent, intelligible or instructive a lecturer. And well into his 70s, John was the preferred speaker on plenary platforms and teaching courses at conferences such as the American Academy of Neurology where he gave the FE Bennett and Soriano lectureships, and at the European Neurological Society, founded in 1986 on the initiative of his friends Gérard Said, Andreas Steck, Anita Harding and ‘PK’ Thomas, and where he was due to feature again in June. 32 In 2005, John was interviewed as part of the oral history archive of the American Neurological Association, to which he had been elected as a foreign member in 1980: Perhaps, a careless remark - needlessly overheard – and made many years earlier suggesting that John may have felt threatened by history, piqued him into historical revisionism on that occasion. Rehearsing arguments offered to the British Association for the Advancement of Science when he was president of the Biological Section in 1982, John explained: “It is usually said that the first description of myasthenia gravis was by Thomas Willis. But, actually the wonderful Rubens’ painting in the National Gallery shows Samson in a myasthenic crisis with the typical bilateral ptosis and posture of extreme asthenia whilst also losing his hair from the associated autoimmune alopecia” – beyond any reasonable doubt the correct diagnosis, and one that naturally hit the global media headlines. Some thought that John’s loyalty to Queen Square was measured. It is true that he did not seek to conceal his unambiguous excitement at moving to Oxford in 1987 to be part of the medical phenomenon being nurtured in that University by David Weatherall. It is the case that he remained to be convinced that some branches of clinical science had progressed commensurate with the levels of investment at Queen Square. There is no doubt he felt uncomfortable with the style of uncritical hagiography that characterised Queen Square when he first arrived, being branded a ‘communist’ by the Medical Committee in 1968 when, as Resident Medical Officer, it fell to him to inform Macdonald Critchley and Denis Williams that henceforth payments would be required to junior staff for looking after private patients. But he held in great affection and respect those who had taught him clinical and experimental neurology and shaped his own professional development – Tom Sears, Sean McArdle, Michael Kremer, ‘PK’ Thomas, and younger colleagues such as Laurie Loh and Kerry Mills who moved with him to Oxford. And as a Brain Research Trustee until 2006 under the chairmanship of John Read, David Corsan and then Neil Payne, John helped a series of Deans and Directors to support research at the Institute of Neurology, supported by these privileged funds, that was internationally competitive. John brought authority and the international perspective of someone who had served academic medicine for many years to this and related administrative work: as chairman of grants committees and boards at the Medical Research Council – who supported his work at programme level for >20 years - the British Heart Foundation, the Muscular Dystrophy Group and the Mysathenia Gravis Association; as consultant adviser to Chief Medical Officers Donald Acheson and Kenneth Calman (1985-1994); as vice-president of the International Society for Neuroimmunology founded by Cedric Raine; and as a member of two Research Assessment Exercise panels in hospital-based medicine in the 1990s. These and the impressive catalogue of scientific achievements were recognised, inter alia, through election to Fellowship of the Royal Society (1991), Foundation Fellowship of the Academy of Medical Sciences (1999), Foreign Associate Membership of the Institute of Medicine of the National Academy of Sciences of the USA (2001), and appointment to the order of Commander of the British Empire (1996). Many of these distinctions came during John’s time in Oxford where he and Angela, and their loyal team, systematically illuminated mechanisms of diseases affecting the neuromuscular junction and other parts of the nervous system. They were a formidably competitive pair. In the Oxford years, an annual contest was established with Cambridge at which – home or away – the neuroscience Varsity Match put 6 papers from each side into the ring, a tie on comparative excellence always being declared. But the papers served merely as aperitif to a much more gladiatorial event - tennis doubles in which the exhibition match provided annual humiliation for the head of department in Cambridge, mesmerised by the unfolding arachnoid Newsom-Davis service discharging its payload like quantum emerging from some secret vesicle to spin improbably over the net and land on its receptor with unfailing accuracy; such that the Oxbridge plate records 12 straight victories for Oxford between 1989 and 2001. I may be wrong but – amongst friends and young people with whom he interacted so easily being himself eternally youthful in appearance and spirit - I do not think that John was ever happier professionally than on these occasions. In retirement John took an office in Boswell Street: not in order to watch over his former colleagues at Queen Square but as president of the Association of British Neurologists. As a former secretary (1981-1984), medallist (1999), author of many papers presented over several decades, and a regular attendee at meetings, it was natural that the membership wanted John to serve as president (1999-2000). He felt that the Association had drifted away from its origins in 1932 as a forum for discussing the best of British scientific neurology. And as a first step towards bringing back the clinical scientists, he established a Clinical Research Advisory Committee. The office in Boswell Street served another purpose. 33 As he prepared to leave Oxford, John agreed to serve as editor of Brain, a journal of neurology that has published across the spectrum of clinical neurosciences since 1878; and which he had looked after as secretary and treasurer (1977-1981) and as chairman of the Guarantors and Board of Management (1994-1999). Brain had acquired a reputation for being fusty, and serving as the ‘Queen Square house journal’, but John had a knack for sniffing out work that was forward looking and contemporary; and he introduced electronic processing and on-line publication well ahead of other journals in the field. He recalled later: “I wanted to change how the journal was perceived and what it did. John Rothwell looked after neurophysiology, and I dealt with everything else. We had superb support from Carol Lovelidge and Lubna Zafar. Early on I decided to take the journal on-line, which was kind of bold because the systems for that were not well developed and there were teething problems. I never took a holiday from the journal for 7 years. There were no fast Internet connections and in the West Indies, or wherever, my latest little grandchild vomiting down my back, being bitten by mosquitoes, perched on the edge of a bath, I was still connecting – somewhat uncertainly - with the online system via dial-up. Evidently the readership liked that since, from then on, the impact factor rose steadily, as did submissions. We were only accepting 1 in 5 papers by the time I left but quite surprisingly, I got very few angry letters, and I would remind any distressed author that editors have their papers turned down at Brain too!” Berch Griggs of Neurology would add: “as a fellow editor, I watched with admiration and a little envy as John took Brain to a new level of excellence, and with astonishing rapidity”. John changed the lives of people with myasthenia gravis: he earned respect for the clinical neurosciences in a changing climate of academic medicine; he led by example and motivated others to stick to careers in clinical science; he valued ability, intellectual honesty and curiosity; he inspired loyalty and affection and reciprocated both especially to young people, with whom he interacted so easily at home and aboard. For none of us will his memory fade. G. Research and Oxford Angela Vincent Professor of Neuroimunology, University of Oxford In 1973 Ricardo Miledi in the Biophysics Department at UCL suggested that I, as the medic in the lab, should pick up the first muscle biopsies of patients with the autoimmune disease myasthenia gravis. John came with the highest recommendations from Tom Sears, so it was with some curiosity that I found my way to his rather cramped laboratory opposite the old RFH in the Grays Inn Road. John was hunched over his recording equipment, placing an electrode in a tiny piece of human muscle. He turned slowly round, smiled and said “Hi” in a way that combined friendliness and openness but with a hint of tease or questioning. The quizzical tone or glance was one that we learned to recognize and was most evident when he knew you were talking rubbish but was too polite to say so! We met frequently after that and in 1977 I moved to the Royal Free to work with him. I remember how excited John was to be starting research into myasthenia – he seemed to know that it was going to be successful and he certainly had strong support from the Head of Neurological Sciences at the RFH, the late Prof PK Thomas, who was very welcoming – and extremely tolerant over the next ten years as the research group expanded. The early days were exhilarating. With Alastair Compston and Richard Batchelor, we stratified the MG patients into groups, and we helped Glennis Scadding (now Pearson) to show that the white blood cells from the thymus gland made the offending antibodies. It was while culturing these cells that I saw another side to John’s abilities. Generally speaking John’s movements were unhurried, and he admitted to being a little dyspraxic. In those days one had to clean the dissecting instruments with alcohol and we often flamed them through a Bunsen burner just to be sure that they were really sterile. One of us managed to set the alcohol on fire and it made an impressive blaze. I was then, and still am, amazed at the rapidity with which John found the appropriate fire extinguisher and put out the fire. Of course, we probably have his RAF training to thank for his speed and decisiveness and for saving the Department from an embarrassing incident! Perhaps it was that incident that made John determined to recruit a real immunologist and Nick Willcox joined us in 1979, shortly after we had taken on Bethan Lang who like me was a biochemist. Things between the four of us went so well that John was awarded the first MRC Clinical Research Professorship and his first Programme Grant, providing the core support that was essential to keep the team together and allow new developments. And new discoveries did follow as John used his clinical acumen to recognize other autoimmune diseases, the Lambert Eaton 34 myasthenic syndrome, seronegative myasthenia, and then later acquired neuromyotonia. We on our part did our best to keep up with the experiments required to investigate the immunopathology and mechanisms in these conditions, collaborating very fruitfully with Peter Molenaar in Holland, Dennis Wray at the RFH and Andrew Engel at the Mayo Clinic. One of the early observations was that plasma exchange did not have any effect in those patients who developed the disease from birth or in early childhood. Further investigations convinced us that these patients had a genetic rather than autoimmune condition, and the fifth member of the team, David Beeson, joined to develop the genetic aspects of myasthenia. This project has been loyally supported by the Muscular Dystrophy Campaign ever since and is flourishing with collaborations with Clarke Slater in the UK, Yuji Yamanashi in Tokyo, and many neurologists worldwide. Meanwhile John had been invited to become the next Action Research Professor of Neurology in Oxford and after ensuring that we would all come with him, he accepted the post. Martin Brydson joined us to coordinate the move. In fact, sixteen of our team moved from London, to become the first group in the newly created (Weatherall) Institute of Molecular Medicine. Here we were able to enjoy daily coffee room chats with immunologists like John Bell, Alain Townsend and Andrew McMichael greatly enhancing our ability to apply molecular techniques to the immunology of our diseases. But of course John’s life changed considerably at Oxford. Until then he was the protégée of PK Thomas and the MRC, and could concentrate on his research. But in Oxford, he was thrown into the situation of all university academics - juggling clinical leadership, clinical practice, research and fund-raising with teaching and administration; he also held a Professorial Fellowship at St Edmund’s Hall, “Teddy Hall”, where he helped to secure charitable funds and provided very perceptive and accurate assessments of potential medical students. But as Berch Griggs, the President Elect of the American Academy of Neurology has written “John had an amazing ability --unique in my experience --- to master new areas and to quickly contribute to them”. The demands of University life meant that he had relatively few hours in the week which could be spent with us, but John clearly was at his most relaxed when in the lab and his time there was marked by notable habits. Firstly, shortly after arrival, the door to his office would close and after some clanking of wire hangers, John would emerge changed from his immaculate dark suit into navy blue cord jeans and a sweater – both clearly from Marks and Spencer, and subsequently replaced by the Lab one Christmas when even we thought they were becoming too threadbare. Secondly, John would whistle – often choruses from oratorios or arias from operas. In fact, Nick Willcox recalls how in the early years when John still had time to work late into the night with him, the tunes would start adagio and become more allegro as they came closer to completion of the day’s experiment. The lab work continued to be strongly supported by the MRC, the Muscular Dystrophy Campaign and increasingly by other charities such as Action Research, the Welton Trust and the Sir Jules Thorne Trust. At its height the group numbered about 35 scientists, including many foreign visitors, some of whom are here today, and loyal administrative staff such as Jill Ratcliffe, Anne Taylor, and Mary Tinker. But that was not all. When John joined the department in 1987 there was already a strong tradition of clinical research from Charles Warlow and Bryan Matthews and he strengthened it further. His clinic became an MDC-supported myasthenia gravis centre, under the gentle but firm hand of Sister Eve Goodger who had followed him from Queen Square and continued to plasma exchange the patients until very recently. Kerry Mills was appointed as Reader in Neurophysiology, and Margaret Esiri was invited to move to the department as Reader in Neuropathology, both key people for the success of the clinical and academic work. He recruited Peter Rothwell as Clinical lecturer which enabled Peter to establish an internationally-renowned group in Stroke Prevention; and then in the mid 1990s John, with Alan Cowey and Sir George Radda, convinced the MRC to create a new Functional Imaging centre to complement the structural and spectroscopic imaging that George Radda had first developed in Oxford. They brought back Paul Matthews from Montreal to direct it, and the FMRIB as it is known, now directed by Prof Irene Tracey, has flourished. When John retired, the department overall had more than 70 researchers and existed on three different sites. Sir David Weatherall writes “What John achieved was to perpetuate and expand the very high standards in clinical neurology that had been established by his predecessor yet, at the same time, successfully establish and pursue the role of molecular and cell biology in the neurological sciences. He was one of the absolutely central figures in linking clinical and basic biomedical research. “ 35 My colleagues and I have spent many hours since last August thinking about John and what was so special about him and how he achieved so much. Others talk about his energy, but in fact he seldom appeared to hurry, and managed to maintain a casual, almost sauntering style in all he did. We wonder at his extraordinary tolerance and ability to devote time to people at every level, making each of them feel that he was their friend and they were his equal. His enviable eloquence meant that he could defuse any situation, however tense. His work was always thorough, never sloppy or rushed – if it needed more time, he would find it – presumably by getting up an hour earlier. His door was always open and we were often very demanding – little appreciating then the number of other demands on his time. The only time I can remember him drawing attention to – not complaining about – his work load was when, as Chair of the Board, the crate of MRC grant proposals to read through would arrive from Megan Davies at the MRC. And all of this was conducted in a most unpompous manner – not the typical neurologist! Nick puts this down to the good influence of his sisters, Rosemary and his children. We are particularly impressed by the gracious way he managed his retirement. The easiest and most tempting thing would have been for him to continue to lead the research – but he made it quite clear in the early 1990s that he would hand over to the rest of us. Throughout the next years he carefully nurtured external commitments both within and outside the University for himself, and strengthened our positions so that we were ready to take over. After his retirement, he was an extremely welcome guest at our weekly meetings but always took a back seat. In the clinical arena, however, he continued to see the patients, helping Jackie Palace and David Beeson to obtain DoH funding to support the genetic service and the related research, and gradually passing the autoimmune baton to David Hilton Jones and Camilla Buckley. As a result, he has not only left a major mark on Oxford’s clinical science but ensured that the group has stayed together and the work continues. We were very lucky to have experienced for so long John’s particular blend of intelligence, enthusiasm, consideration and tolerance. I suspect that we don’t realize the full extent of his influence on us but nevertheless subconsciously try to emulate him in our daily lives. He was a truly remarkable person and it was a privilege to have been his colleague and friend. H. Retirement and the ThymectomyTrial Gary Cutter 31/03/2008 Professor of Biostatistics, Birmingham, Alabama I am extremely honoured and humbled to be invited to convey my thoughts and the thoughts of hundreds of neurologists from around the world who were part of what some may say were John’s RETIREMENT years. I cannot adequately represent the thoughts and feelings of the hundreds of colleagues around the world who were part John’s retirement years – so, I asked them to represent themselves in this Commemorative Book that has been compiled for the family. In this way, the family can truly know that these are not just my words, but echo the words and the hearts of legions of scientists around the globe touched by a unique individual that thankfully shared time with each of us. I discovered John’s kindness when he accepted a paper of mine in 1999 into the journal Brain. That acceptance, which I doubted would occur, left me with a sense of obligation to him. When several years later I was asked if I could help to get the MGTX Trial funded from the US’s National Institutes of Health – this sense of gratitude made it easy to say yes. At that moment, I didn’t realize the gift I had been handed by this opportunity. From day one I was impressed with his acumen, energy and grasp of so many intricate details of clinical trials. Equally important, I observed his incredible tolerance of nitpicky comments, which he knew were often trivial; His mastery of teamwork and leading by example amazed me, given his stature in the world. He answered the endless stream of comments and criticisms with the thoughtful and careful nature to which he always approached problems. But all of you know of John’s infinite wisdom, knowledge, scholarly accomplishments and talents. It will suffice to just note this as I digress to more personal topics. What I never imagined was that someone I could know for so few years would have such profound impact on me and others around me. I traveled with John to various countries around the world. He was sought out by so many with pride for he was THEIR friend. It was genuine friendship and that is what they relished – not star struck contact with this international scientist. You could see it in their stories, their eyes when the met the man who meant so much to them professionally and even much more personally. John knew them and their families and was first to 36 inquire about their personal as well as professional lives- Always available for quick advice – the consultant’s consultant. I became amazed at his willingness and ability to travel – always reminding us he needed to be back in London by Saturday for a play or Rosemary would be quite upset; or that he had a date with the grandchildren, which was not possible to miss, even if it meant less than 24 hours in the locale where he had just arrived. He would surface after long trips and say he wasn’t very hungry, but he would go with us to dinner so we could begin to work. John and I used to talk a lot about food and cooking. He would smile when he was telling stories of picking up ingredients for a dinner at the cottage or at his shops in Hammersmith and which wines, usually a white, that could be had with dinner. He was pretty tough when it came to wines. At the first of John’s Myasthenia Gravis Trial training meetings, there were 150 neurologists present – this was in San Francisco where we hosted a dinner for half of the study’s investigators. The wine was a New Zealand Sauvignon Blanc that dismayed one American member of the Executive Committee, Henry Kaminiski, because I hadn’t selected a California wine. John proceeded to educate Henry with two facts – First: there are no good California Sauvignon Blancs and Second: it is the Americans’ appetite for the New Zealand wines that are driving up the price in London. Back and Forth this conversation went throughout the dinner. The “guests” of course convinced John was explaining the finer details of the trial to all of us, which we delicately kept private. After this international “incident” it was time of course for the Americans (us) to retaliate against the Brits once again. Searching over the weekend for the finest bottles of California Sauvignon Blanc, Henry selected the best small vintage California Sauvignon Blanc’s. At the study training meetings for the second half of the investigators, which took place at Oxford that next week, we surprised John with a blind wine tasting –he was summoned unknowingly to the front of the room and challenged to pick the winner of 3 Sauvignon Blanc wines to be blindly tasted – 2 of which were American and 1, of course, from New Zealand. John hated being the center of attention, but he played along with the aplomb of acting he so adamantly admired in the theaters of London. And, well, you know the ending - he picked the New Zealand as best – to the cheers of 150 worldwide friends and colleagues. John’s wisdom and infinite patience and kindness was so immediately felt by all whom he came to meet. When John was in Birmingham Alabama last August, he insisted that we go out to lunch with the entire coordinating center of the project. He spent the lunch engaged in a most amazing conversation with two of our young data entry people - both who just finished high school. He quizzed them on what they did for the study and how they felt about their job. In the period of 5 minutes he made them feel as important as the old folks around the table. His ability to connect with people was uncanny. These two young individuals still talk of that lunch and as they learn more and more about John’s accomplishments are inspired by how he actually talked with them. It is of course hard to maintain the brevity required in this Memorial Service of a life that is so large in the lives of many. I just want express my personal gratitude for the honor of knowing someone who touched so many people and who touched me so personally. John made me think, not respond. He taught me the wisdom of openness in thought and the judiciousness of when to just watch. I speak for several hundred neurologists and colleagues from the Post Retirement era and equally for myself. My life has been enriched because of the privilege of being allowed to call John my friend. Another one of John’s MGTX Colleagues, Alfred (Fred) Jaretzki, an internationally known thoracic surgeon, 12 years John’s senior said on another occasion commemorating John’s life and contributions: “John became my teacher, my tutor, my advisor, my confidant, and most importantly a close friend.” I think this is the way he touched others as well. I. Mentor and Clinician Camilla Buckley MRC Clinical Scientist, University of Oxford I have been asked to say a few words about John as a mentor and senior clinician under whose guidance I, and a whole generation of neurologists trained. He inspired, taught and mentored so many of us, in whose place I am honoured to speak here today. 37 I had the tremendous privilege of sitting in on his myasthenia clinics for three years as a research registrar and more recently of doing joint clinics with him as a fellow consultant. Quite simply, he was the best doctor I have ever worked with. His patients knew this: many of them followed him from London to Oxford and subsequently continued to come and see him in Oxford even after they had moved hundreds of miles away, His colleagues knew it. Several members of the clinical team, namely Laurie Loh, Kerry Mills and Eve Goodger came to Oxford with him, and the reason that so many neurologists agreed to take part in the forbiddingly ambitious and complex MGTX trial was because of the respect they had for John. GMC booklets apart, it is difficult to put into words what makes a good doctor so I will mention a few of the characteristics in John that I think contributed. First and foremost, he was kind and thoughtful, and took a genuine interest in patients and colleagues as individuals with a life outside the consulting room. I was always struck by how he remembered not only the pattern of a patient’s disease but also their jobs, families and significant life events. This allowed patients to relax and feel safe in the knowledge that treatment decisions were being made in the context of their life as a whole rather than simply on their disease in isolation. In part this stemmed from his own pride in his family and his achievements outside of medicine. I can remember to this day sitting in the Thomas Rowney outpatients at the Radcliffe Infirmary with John taking a history when it emerged that the patient had flown in the RAF. There was some hesitation, before John, unable to hold back any longer, succumbed to temptation and admitted that he too had flown Meteors. There followed a lengthy and animated discussion which made me realise that he was at least as proud of his real-life Meteors as he was of his subsequent meteoric career as a scientist and a doctor. John took particular care about his teaching, and great interest in his students, as I discovered to my embarrassment. As a clinical student, I failed to turn up to our first group teaching session with him as a 5 th year medical student. Since there were 10 of us in the group, such an absence would usually go unnoticed, so I was surprised and taken aback when my a colleague phoned later that day to say it had been noticed, and that John had asked for me by name. I subsequently learnt that he always asked for the names and photographs of each new cohort of students and memorised them so that he could fully involve everyone in his teaching sessions John had unflagging energy and capacity for hard work, and total dedication to the care of his patients. I am sure Gary will remind us of the huge amount of time and effort John devoted to the thymectomy trial over the last 8 years. However despite this, and the fact that he was supposedly retired, he still regularly did his MG clinics with enthusiasm, identifying clinical features worthy of further research, and instituting the use of new treatments in patients with intractable disease. As a mentor he was everything one could ask for, and more; a superb role model who led by example. Despite his hectic schedule he always seemed to have time for his charges. He responded to emails promptly no matter where he was in the world or what time of day or night. He would make the time to discuss a clinical case, review a manuscript, or give career advice, and never made one feel rushed or as if it were an imposition on his valuable time. He only delegated tasks to people if he thought it would be useful for them, and if ever he involved one in something that turned out to be more time-consuming than he expected he was always apologetic and readily offered, and gave, assistance. On his last day at work I recruited the first oxford patient to his beloved thymectomy trial. When I told him the patient had agreed to take part his face lit up with the comment “you have made my week”. Later that evening I got a call at home from a slightly anxious-sounding John querying the patient’s drug dose. There followed a rustling of papers as he double checked the inclusion criteria, and relief in his voice as he confirmed that yes indeed the patient was eligible. This was typical of John. He was thorough and careful, paying attention to detail. This attitude in the clinic contributed hugely to the success of the research as it meant that in the lab we could be sure that whatever came from John’s clinic was exactly what it said on the label. In this, as in so much else, he was an instinctive and natural clinician-scientist. 38 We have heard already about how successfully John mastered the very different worlds of clinical neurology and laboratory science. This is more than most can manage, but his true talent was that he could do this and remain such a warm, generous, humble and kind human being. J. Patients’ recollections Collated by Michael Burrows PhD As a patient of Professor Newsom-Davis for over 20 years, it is a privilege to be asked to say a few words about him and what he meant to many of his patients. My tribute is based on warm letters of appreciation received from some of his patients, many of whom had known Prof. since the great days of the National Hospital in Queen’s Square. That great haunted Victorian edifice in the centre of London, which we miss so much! A number of those who have written have asked to remain anonymous and consequently I have tried to respect these wishes in what follows. Rather than read out the letters one by one, I have attempted to draw out of them the qualities which Prof. demonstrated and which seem to be mentioned time and time again. In the letters, adjectives describing Prof. such as; kind, loving, warm hearted, brilliant, skilful, well mannered, supportive, encouraging, good natured, humorous, youthful, a good listener, honest, modest and humble have been mentioned several times over. An over-riding feature of those who wrote has been a sense of gratitude to Prof. and a recognition of the fact that without his input, his brilliance and compassion, the lives of so many of his patients and their families would be very different. He, and his team, have enabled many of those with MG, and other related conditions, such as Lambert Eaton Myasthenic Syndrome to lead fuller and more active lifestyles than would otherwise have been possible. Prof. had a marvellous way of putting at ease both patients, most of whom initially came to see him in a very distressing condition, and their families. He was very easy to talk to and an extremely good listener who would heed, and taken into account, a patient’s questions, concerns and fears without being at all dismissive. I remember very well as a teenager meeting Prof. for the first time with my mother and father at the National hospital. Physically I was in a mess and although they did not show it at the time, I suspect my parents, like many parents would be, were in a mess emotionally. Yet Prof. was able to put my parents at ease and reassure them of the future well being of their son. He did this with a combination of honesty and the calm authority and confidence in his methods and fellow members of staff which is often exhibited by the exceptionally gifted. At the same time a young chap, Simon, who was only about 12 years old also had an appointment with Prof. for the first time with his mum. As a result of seeing Prof. we were admitted to hospital straight away and put in beds next to each other. Understandably, Simon’s mum was beside herself with worry. Yet Prof. was able to calmly reassure her and her son and explain things to Simon in a way which was neither patronising nor complicated. Simon’s mum remarked afterwards that she could not believe that such an eminent Professor was so down to earth and could explain things to her in a language to which she could relate. Several of those who wrote in have also shared similar experiences. Prof. would spend a considerable amount of time getting to know his patients so that he could understand a patients’ problems and know when to cajole and when to sympathise, showing a genuine empathy with those who struggled with daily living. Much of his empathy was borne out of the genuine interest he took in the lives of his patients and the fact that he seemed, despite being very busy indeed, to have time for every one. Several people have written to say how at their regular clinic with Prof. they would discuss a variety of topics such as the well being of their families, the state of the NHS (something very dear to Prof.’s heart), Prof.’s family and so on. It was no doubt in Prof.’s nature to be so convivial, but part of the reason for these very genial discussions, was perhaps Prof.’s way of helping him to remember the patient. Also they helped relax the patient so that Prof. could 39 determine and properly understand the patient’s wellbeing. He truly tried, it seemed, to understand the individual and what made them tick so that they could be treated most appropriately. David Barrington wrote to say that they shared a common interest in the Opera and horticultural matters which they would discuss from time to time. When it came to roses however, it was David who gave the advice, rather than the other way around! Prof. apparently fed his roses on Phostrogen, however they were not exactly flourishing on their diet, shall we say! Consequently, on David’s recommendations he switched to horse manure, with great results. Apparently, David even brought bags of well-rotten manure with him to his appointments. So now some of you will know why there was often a funny smell in the waiting area at the Radcliffe Infirmary! Of course an appointment with Prof. was not all about reminiscing, and shooting the breeze, and the topic of conversation would always turn to the level of medication and the symptoms a patient exhibited. With the knowledge gained from the discussion of the patients’ activities together with those gleaned from the results of clinical tests, which he may have he requested, Prof. was able to make very informed and skilful judgements regarding the types and levels of medication appropriate for a particular patient at a particular time. Mindful of the side effects of the medications which had to be prescribed, the goal was to reduce the amount required to the minimum necessary. I distinctly remember one visit to see Prof. where he studied the results of some blood tests for a quite a while longer than normal. Then, quite unexpectedly, he said that my future health would benefit from a change in the levels of the medication prescribed. Sure enough he was proved right, and I have often wondered exactly what it was he was weighing up in his mind. During a consultation Prof. could be straight and to the point it mattered. Many are his patients who have been encouraged, where appropriate, to push themselves so that they could lead as normal lives as possible, be that in work, leisure or study. Often Prof. would use examples of his other patients as a spur to those who were undergoing difficulties. Indeed, he would even encourage patients who had concerns about a particular treatment, or who were struggling in a particular way, to talk with those who had been through the process before. Often Prof. would discuss, very openly, the various alternative treatments available and their advantages and disadvantages. These healthy discussions were much valued by patients who as a consequence developed a great deal of trust in Prof. and his methods. As an example, Robert Wright wrote to say how he had struggled for a number of years on Mestinon and Neostigmine, gradually finding his dexterity and ability to lead anything like a near normal way of life become severely impaired, so that he even had to give up his beloved skiing trips. The one sport Robert reports at which he was any good. Robert, fed up with the situation, sought an appointment with Prof. and during the resulting consultation, Prof. offered Robert what he described as a "choice" as to whether or not he should try steroids. The choice being between being able to lead a more active life versus the problems of the potential side-effects of the drugs. Having made the decision to take steroids, Robert has been able to do away with the Mestinon and Neostigmine, and has led, in the subsequent 10 years or so, a near normal and very active life as a (recently retired) criminal lawyer (and MGA Trustee) who regularly takes to the ski slopes. As Joanne Gilbert who suffers from LEMS put it: “His team, I have always thought, reflected his ethos on patient care. Always aware that outside of the hospital walls patients have lives to lead and the treatment needs to reflect this.” Sometimes the situation, as several have written to say, was clouded by the patient suffering from other serious conditions such as ME, MS and so on. Here his great skill was in being able to distinguish the symptoms due to MG 40 and treat those, whilst always being aware and mindful of the symptoms due to the other disease; and indeed the side-effects of various medications. Prof. was extremely supportive and understanding of the needs of his patients. He would willingly go out of his way to write letters of support for patients where necessary. One of his patients recounts how Prof. stood as an expert witness confirming that an onset of MG had been stimulated as a result of a car accident. I remember well the letter he wrote, at his own suggestion, to an examining board saying I might struggle in my Spanish oral GCSE exam. I hope that this was because of my difficulties in speaking for a long period of time, rather than my ability to speak Spanish. A good excuse you might say! Prof.’s concerns for his patients went much further than that of a typical consultant/ patient relationship. As some of you, will know he kept his “baby book” which is a gallery of the photos of babies born to mums who were suffering from MG. One lady wrote to say how he had used the photos in the book to encourage her to try for children, reassuring her that help was always at hand for her or any new born. As a result she has two lovely healthy children of her own. This story I am sure has been repeated over and over with a number of patients. In my case, conversation often turned, not to babies, but to golf. Prof. always reckoned that he could gauge my health from my form on the golf course. He thought it important that I played for my general well being and so I take great delight in telling anyone who will listen, including my boss when it matters, that I spend so long on the golf course because my specialist has prescribed me golf! Like all of his patients, I was devastated when I learnt of the news of his tragic accident. I happened to be in the latter stages of a golf competition at the time and the news of Prof.’s death inspired me to go on and win the event, dedicating it to his memory. Amongst many of Prof.’s great skills and abilities was being able to choose talented and like-minded people to work with him. His care for patients was very well supported for many years by Eve, for whom he had the highest regard, and latterly Christina, and also by his secretaries Annabel and Claudia. They were very often the first contact patients would have with the MG clinic and their support and competence was vital. On the research side, of course Prof. put together a brilliant team led by Profs. Angela Vincent and Nick Wilcox and, as far as patient treatment is concerned, Drs David Hilton Jones, Jackie Palace and Camilla Buckley carry on in Prof.’s style. So amongst the many legacies Prof. has left, perhaps one of the most important is the very able and talented team he has assembled. Prof. will be missed, very, very much by many people, not least his former patients. However, his legacy means that we are in excellent hands as Prof. would remark when he mentioned the prospect of a full retirement. Something which he never experienced. I will leave the last words to Joanne Gilbert: “I was dreading my last appointment, no Prof., no Eve and a new location, big changes to absorb. Then I saw Christina and David Hilton Jones and all seemed as it should be.” K. from “John Newsom-Davis 1932–2007” Journal of Neuroimmunology 2008 by Nick Willcox Combining excellence in clinical medicine and research remains especially challenging in the UK, but John had very few equals. Orchestrating and sustaining the funding for all of the above made brilliant use of his many attributes. These included his boundless youth, energy and optimism (vital in a research team), his efficiency, strategic planning and skillful opportunism; especially also his abilities to delegate, to juggle many balls at the same time and rapidly to become expert in fields totally new to him (e.g. immunology). Together, these made him an excellent ambassador and a tireless front-man. 41 John remained extremely active after ‘retiring’ (1998), still doing fortnightly MG clinics and devoting enormous energy to the ongoing international NIH thymectomy trial (2005– present). Known and loved by so many neurologists both nationally and internationally, he was ideally suited to this demanding role. Being also a true gentleman, John was modest and not pompous despite his eminence, and was content to take a back seat in his later years. His kindly encouragement and advice were hugely appreciated not only by his colleagues and numerous students and trainees in his own institutions: they also won him countless friends around the world. Sensitive, egalitarian and approachable, John was a very good listener, and greatly loved by his staff and innumerable patients. Because of his sound judgement and vast experience, he was frequently used as a referee, editor (of Brain) and to advise behind the scenes, e.g. in setting up the Centre for Functional Imaging of the Brain at Oxford (1996), by the UK Ministry of Health, and by many Patient and Research Charities. Remarkably too, he did it all without neglecting his devoted wife and family, which now includes three children and seven grandchildren. He leaves a major vacuum in many fields. John was a classic exemplar of two time-honoured rules:-“If you want something done, ask a busy man”; he delivered promptly, succinctly and constructively: “From those to whom much is given, much is expected”; he lived a privileged and very full life – which he continued to repay with interest – at a high rate – right until the end. Very typically, an early task on his last holiday, in Romania, was to visit the local Myasthenia Patients' organisation; he had recently lent his weight to their campaign for free pyridostigmine treatment. To me personally, John's passing seems a waste more than a tragedy; he was still brimming with energy and activity, but at least he was spared any long-term incapacity. Above all, we should be grateful; as one ex-colleague wrote, “I always thought he was one of those people who will never die. In a way, he never will — thanks to all the knowledge and encouragement that he transmitted to subsequent generations”. Now it is for us all to carry the torch forwards. 42