Dear Notetaker - My ICO Portal
advertisement
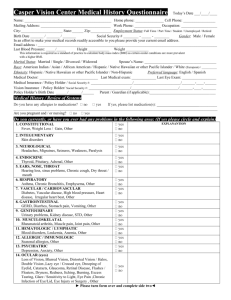
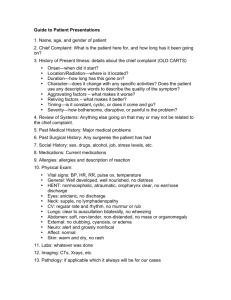
CLE 162.1 – Intro to Optometric Procedures Notetaker: Jonathan Dong Date: 8/30/2012, 1st hour Page1 Case History The first part of an exam, in some ways the most important. Problem vs. Data Based Testing - (notes in handout) o Data-based tests are done for all patients; in an established patient, less data-based may be done, in follow-up, even less data-based may be done. o Problem-related tests may be done for patient complaints or for any problems that may come up from data-based testing. o Data-based tests may become problem-based, but problem based tests never become problem-based. Case History Importance o Starting patient rapport – Introduce self, etc. o Prioritizing concerns (what data-based tests to focus on, what problem-based tests to do) o Establish how to approach patient – stern or more coddled, in order to help exam go smoothly and improve compliance Factors in selecting a doctor? “Above all you want to have a doctor who is a fellow human being, whose concern for patients is actuated by the joy of serving, regarding it as an incomparable privilege.” EX: A patient comes in worried about cataract surgery in a hospital where there were bad experiences. EX: A patient comes in worried about the eye puff test, be reassuring… don’t lie. Many elderly patients, as a young doctor, learn to stay in control of the exam situation. o By the end of case history, have a pretty good idea of what’s going on (Ddx). Exam may just support what is going on from history, sometimes it contradicts, that’s why you have to look. o Think before you talk, no off-the-cuff remarks Things not to say: “Uh oh”, no guilt tripping (why didn’t they come in, why aren’t they taking medications), remember HIPAA, show incompetence (“I’ve never done that before”)… Social History (In lab, try to act like a patient when working with other students, simulate real life as much as possible.) o Demographics Age, name, verifying address, phone, ethnicity, language, etc. Verifying you have the right patient, right info. Chief Complaint o Open ended questions: “What brings you in today” o EHR Entry: Must be in the patient’s words, NOT what the doctor thinks is going on, quotes or paraphrase Chief complaint, secondary complaint, tertiary complaint… etc., as many complaints as the patient has (relevant), all will be examined. o Closed-ended questions, questions with short answers May move more quickly to closed-ended questions for wordy patients o Leading questions: Avoid – may be judgmental (ex. Medication compliance) o Laundry List questions, questions with several options: good for patients that can’t come up with specific answers/quiet (multiple choice) CLE 162.1 – Intro to Optometric Procedures Notetaker: Jonathan Dong o Date: 8/30/2012, 1st hour Page2 Facilitative questions: encourage patient to keep talking (can help seem like clinician is listening, especially if you need clarification), or if stories change. o Summarize what they said back to the patient, before you need to write it down, just to clarify the information and make sure it is accurate. History of Present Illness - (description in handout) o FOLDARQ: Frequency, onset, location, duration, associations, relief, quality On NextGen EHR: Pick list comes up for each option, or just type in whatever Must fill out at least four of the fields for each patient (insurance thing…) o Must find some complaint that brought them in, otherwise insurance may not cover exam (“Blurry vision without glasses”) Ocular History o General health questions o Refractive history (glasses/contacts) o Ocular health history: Family history of eye disease, any ocular medications/eye drops Patient Medical History o Usually a form patient has already filled out o Past/Current illness o Systemic medications, sometimes list o Allergies, NKA, NKDA, NKMA, see handout o Family ocular history (FOH), family medical history (FMH) o MGM, PGF, other family abbreviations (maternal grandmother, paternal grandfather) Social History o Visual demands, work life, hobbies, whatever needs vision o History of smoking, drug use, alcohol use, possible risk of STDs Remember you’re the doctor, less uncomfortable you are asking, the less uncomfortable the patient will be o Any caretaker relationships, parent/child, elderly patients with younger caretakers o Make sure you know who else is in the room. Don’t just assume who the other person is. Assess how involved that other person is with care. Wrap Up o Order of Case History: Chief Complaint: Sit square with the patient, be attentive Summarize CC back to patient, and put into computer Ask demographic/medical/social history battery while putting them into the computer Summarize main concerns, then move on to exam