Guide For Medical History
advertisement

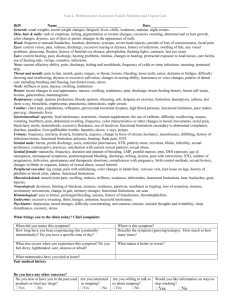
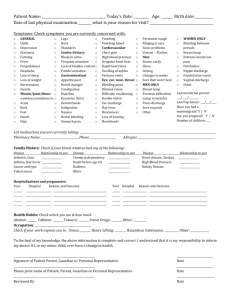
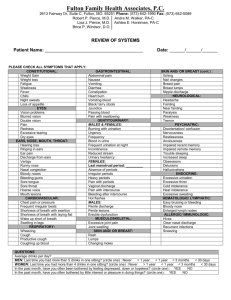
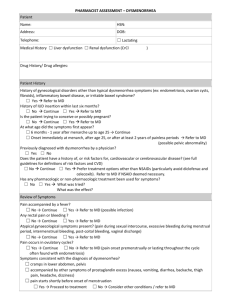
ge: state of health) Guide For Medical History Topic CC:Chief Complai nt HPI History of Present Illness Description This is patient’s major presenting complaint and its duration. Use patient’s own words if possible, i.e. chest pain x 2 hr. Limit CC to one (1) complaint. if there is no complaint and patient is presenting for routine hx and P/E. then so state, i.e—CC: none. Diagnostic procedures, operations are not to be used as CC. instead, use that complaint that necessitates the procedure or operation This is the filling in of background information relevant to the chief complaint. It must be a chronological narrative of the CC that is brief, lucid, and easily digested 1. Your opening sentence will be clumsy: include patient’s age, race, occupation, sex and general state of health prior to onset of presenting illness, in addition, include pertinent chronic diseases; the details of which will go in past medical history. I.e.—This is the second hospitalization with a 3 yr. History of Diabetes Mellitus and 10 yr. history of High Blood Pressure who was in his usual state of health until this 9 a.m. today when he developed Give complete analysis of symptoms: (See Chart: ANALYSIS OFA SYMPTOM)_”LORCATES” a. Onset i. Date of onset (also determines total duration) ii. Manner of onset (gradual or sudden) iii. Precipitating and predisposing factors related to onset (emotional disturbance, physical exertion, fatigue, bodily function, pregnancy, environment, injury, infection, toxins and allergies, therapeutic agents). b. Characteristics at onset (or any other time) i. Character (quality) sharp, dull. ii. Location and radiation (for pain). iii. Intensity or severity - rate on scale of 1-10 if pain. iv. Temporal character (continuous, intermittent, rhythmic; duration of each; relationship to other events). v. Aggravating and relieving factors. c. Associated symptoms Course since onset i. Incidence 1. Single acute attack 2. Recurrent acute attacks 3. Daily occurrences 4. Periodic occurrences 5. Continuous chronic episode ii. Progress (better, worse, unchanged) iii. Effect of therapy 3. When symptoms point to a particular system(s), all questions included under that review of system(s) should be asked with positives and negatives recorded in the HPI. 4. Mention pertinent medical problems and give details in PMHX. 5. Include pertinent family history; i.e., Renal, Heart Disease, HBP, Anemias, etc. 6. include pertinent social factors, i.e., tobacco, ETOH abuse, occupational hazardous exposures, stresses, etc. 7. Allergies: Include positives and/or negatives. 8. Medications: List all current prescription and OTC drugs. Note dosages, frequency and duration. (include laxatives,ASA, vitamins, etc.) a. 1. Medical a. Child:Measles, rubella, chicken pox, mumps, whooping cough, scarlet fever, rheumatic fever, diphtheria, poliomyelitis, general picture of health as child. b. Adult:List all past illnesses, the time of occurrence, the nature of the symptoms in the illness, the type of therapy, the complications, and the diagnostic label, if known - do not list diagnosis only as these can be misleading. Specifically inquire about common diseases: stroke, heart disease, kidney disease, hypertension, tuberculosis, diabetes, venereal disease, anemia. 2. Surgery: Date of each operation, nature of symptoms prior to operation, type of operation, complications, results of operation. 3. Hospitalization: Patients will often forget disease processes; therefore, ask specifically about hospitalization and record major symptoms leading to hospitalization, studies carried out, diagnosis, treatment, and results of treatment (outcome). 4. Injuries: a. Date, cause, type, complication, outcome. Immunization and Vaccination: Record the time and results of any and all vaccinations and immunization - include specifically tetanus, smallpox, measles, german measles, mumps, hepatitis, pneumococcal, influenza, typhoid, para-typhoid, tuberculin testing, poliomyelitis. The Family History should contain the medical history of the patients spouse, siblings, parents and 2. PMH:Past History Family History grandparents (2 generation regression) Details should include the following information if applicable: 1. Diseases 2. Cause of death 3. Age of death The above data can be recorded in the following tabular form: 4. History of familial disease; cancer, leukemia, lymphoma, migraine, tuberculosis, coronary artery disease, hypertension, nephritis, strokes, nervous or mental disturbances, anemia or other hematological disorders, diabetes, obesity, thyroid disturbances, allergy, and other disease suggested by the patient’s history. Include positives and negatives. 5. Genetic history- sufficient information should be included to ascertain the patients risk of genetic diseases, The table demonstrated above represents an effective mechanism to track both known genetically inheritable diseases as well as familial patterns of diseases without known genetic patterns Social History Place of birth, ethnic lineage, residence and travel (foreign and domestic) include military. 1. Habits a. Sleep b. Tobacco-(quantitate in pack years or other) c. Diet d. Laxatives, sedatives, other drugs e. Fluid Intake f. Vitamins g. Coffee/tea h. Avocation and recreation i. Alcohol Intake (quantitate) j. Exercise 2. Education: Schooling 3. Occupational History: 4. Past and present work and exposure to known physical/environmental hazards. 5. Frequency of jobs and duration of each job. 6. Work environment and the number of hours at work. 7. Attitude (satisfaction, security) toward work and employer. 8. Marital status - # marriages, quality of relationships, children. 9. Environment (community, living conditions, number in household, flights of stairs, amount of housework). 10. Support system (friends, community involvement, quality of relationships). ROS:Revie w of Systems This is basically a comprehensive screening process designed to: 1. uncover additional problems related to the CC 2. uncover concurrent problems. Be sure to indicate to the patient that this review is a routine procedure. Question the patient for symptomatology generally within the last six (6) months. Positive responses must be elaborated upon. If symptoms have persisted for longer than 6 (six) months, put in past medical history. When particular system has been included in your HPI then so state: i.e. — G.I. see HPI. Arrange ROS in the following order: General: Present weight (amount of loss or gain over what period of time and contributing factors; i.e., dieting, anorexia, etc.), weakness, fatigue, malaise, fever, chills, sweats or night sweats. Skin: Lesions, color changes, pruritus, tendency to bruising, excessive dryness, texture, hair and nail changes, use of hair dyes or other possibly toxic agents. Head: Cephalgia, trauma, syncope, lightheadedness. Eyes: Vision (general), glasses (reason for glasses), pain, diplopia, scotomata, photophobia, lacrimation, inflammation, injection, discharge, field cut, injury, previous surgery, medications, date of last eye exam. Ears: Injury, past disease, decreased hearing, discharge, pain, vertigo, tinnitus. Nose: Obstruction, headcolds, discharge, epistaxis, loss of smell, abnormal odors, frequent sneezing. Mouth: Excessive salivation or dryness, pain ulceration, bleeding. Tongue: Enlargement, soreness, coating, loss of sense of taste, injury. Teeth: General condition, pain, abscess, impaction, dental extraction. Gums: Bleeding, swelling, ulceration, and discoloration. Throat: Sore throat, tonsillitis, abscess, difficulty in swallowing, nasal discharge. Neck: Stiffness pain, welling, pulsations, limitation of motion larynx, hoarseness, change in voice, aphonia, respiratory stridor. Nodes: Tenderness or enlargement of neck, axillary, epitrochlear or inguinal nodes. Breasts: Masses, tenderness, deformity, abnormal discharge. Cardiovascular: Dyspnea, orthopnea, paroxysmal nocturnal dyspnea, edema, palpitation, irregular heart action, chest pain (characteristics, radiation, duration, relation to exercise, relation to posture, eating, effects of drugs) -edema, coldness of extremities, claudication, night cramps, ulceration of extremities, gangrene, color changes in extremities, etc., date of last IEKG (if appropriate) and results Respiratory: Cough, sputum (character, amount, color, odor), hemoptysis, night sweats, chills, fever, wheezing, shortness of breath, pleural pain, injury, date of last chest x-ray; if abnormal, what was problem. Gastro-Intestinal: Appetite, food allergy, nature of diet, selective dyspepsia, dysphagia, beichi heartburn, sour stomach, nausea, vomiting, hematemesis, jaundice, epigastric distress (relation to meals, relief by antiacids, eating or belching), abnormal pain (location, radiation, causation, and characteristics - sharp, knifelike, colicky, dull, aching, gnawing, constant, intermittent, severity (patient’s relation to pain), mode of obtaining relief, and so forth: gas - excessive belching, flatus, borborygmus; bowel movements regularity, frequency, change in habit, laxatives; stools color, consistency, size, shape, odor, bloody or tarry; painful defecation, tenesmus, hemorrhoids. Has Barium enema ever been performed? If yes, why and what were results? Genito-Urinary: Voiding per day, dysuria, urgency, frequency, hematuria, pyuria, incontinence, difficulty in starting or stopping stream, size of stream, appearance of urine, stones or gravel, past venereal disease, previous surgery, lumbar or flank pain, uretheral discharge, penile and perineal sores, sexual contacts, change in sexual drive or activity, testicular pain, scrotal changes. Have kidney x-rays or bladder diagnostic procedures ever been necessary? If yes, what and what were results? Gynecological: Age of onset of menstruation, frequency of menstruation, duration, amount of flow, presence of clots, dysmenorrhea, date and character of last period, leukorrhea, recent change of cycle, date and age of menopause, menopausal symptoms, coital bleeding, post-menopausal bleeding, pregnancy, (with or without complications of each pregnancy), previous surgery, time of last pelvic examination, venereal disease, changes in sexual drive or activity, birth control. Extremities: Vascular: Intermittent claudication, varicose veins, ulceration, color changes. coldness of extremities, hair loss, gangrene, thrombophlebitis. Pain (note location, migratory nature, relation to known cardiac involvement), swelling, limitation of motion, pain on motion, morning stiffness. Bones: Flat feet, fracture. Muscles: Pain, cramps. Joints-stiffness, immobility Back: Pain (location and radiation, especially to the extremities), stiffness limitation of motion, injury. Central Nervous System: General: syncope, loss of consciousness, convulsions, dizziness. Mentative: speech disorders, emotional status, orientation, memory disorders, change in sleep pattern, history of nervous breakdown. Motor: tremor, weakness, paralysis, clumsiness of movement. Sensory:anesthesia, parasthesia, pain. Hematopoietic: Bleeding tendencies of skin or mucus membrane, anemia and treatment, blood type, transfusion(s) and reaction, exposure to toxic agents or radiation. Endocrine: Inquire specifically about symptoms of diabetes (polydipsia, polyphagia, and polyuria), hyperthyroidism, hypothyroidism, weight loss or gain (specify pounds per unit time), estimation of food intake, unusual sensitivity to cold or heat, excessive perspiration, excessive nervousness, fine tremor, development of striae, alterations in bodily contour. Emotional State: Nervousness, excessive crying, depression, euphoria, hallucination, sleep pattern, concentrating ability, previous treatment, drugs, or hospitalizations.