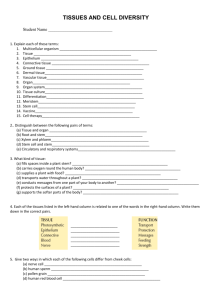
James Kim WRIT 340 Aubertin Section 66813 How 3D Printing and
advertisement

James Kim WRIT 340 Aubertin Section 66813 How 3D Printing and Stem Cells May Lead to Growing Artificial Organs Introduction In the past several years, 3D printers have gained attention and become more accessible due to their applications in countless industries and fields. Three-dimensional printers were initially utilized by commercial manufacturers when prototyping new products for development. By allowing companies to design their own models and produce exact three-dimensional replicas within a few hours, 3D printers have saved significant amounts of cost, time, and effort during the prototyping process. These printers have since branched out in their versatile utility to different fields such as architecture, aerospace and civil engineering, and medical industries. The types of objects that can be printed are essentially limitless: footwear, jewelry, aircraft parts, and even medical implants and prosthetics customized for individual patients. Now, we are able to print human stem cells, putting us on the brink of growing artificial organs. In a recent study, researchers at the Heriot-Watt University in Scotland were the first to successfully print human embryonic stem cells by utilizing custom 3D printing technology. By placing stem cells collected from an embryonic kidney in a “bio-ink” dispenser, researchers were able to print and cultivate multiple layers of living cells into spheroid shapes [1]. Since human embryonic stem cells are able to differentiate into more specialized types, this breakthrough makes the idea of humans growing artificial organs at will feasible in the future, yielding potentially considerable implications on future disease treatments, organ transplants, and drug development and testing. What Are Stem Cells? 1 James Kim WRIT 340 Aubertin Section 66813 Stem cells are unspecialized biological cells, found in both humans and animals, which are able to differentiate into more specific cells found in muscle, blood, and other tissues. Stem cells are defined by their ability to undergo cellular division to produce undifferentiated cells as offspring and their capacity to differentiate, or give rise to more specialized cells. Unlike most cells in adults, stem cells do not assume specific roles or responsibilities until they are differentiated at later stage of growth. There are three main types of stem cells found in humans: totipotent and pluripotent, found in human embryos during fetal development, and multipotent, or adult stem cells [2]. Stem cells are categorized into different types based on their origin and capacity to differentiate. Totipotent cells refer to stem cells that can adapt into all cell types and give rise to an entire organism. Found in the first stage of embryonic development, these cells possess the potential to differentiate into any cell found in the body. Following the fertilization of an egg by a sperm cell, a totipotent cell is created. This single stem cell then undergoes a first differentiation into a blastocyst, or hollow, embryonic sphere comprised of an embryoblast and an outer cell layer. The embryoblast is an inner cell mass from which embryonic stem cells are derived from. On the inside of the blastocyst, the cellular mass eventually forms three germ layers, which are the sources from which all eventual tissues and cells formed in the body collectively originated. Since embryonic stem cells are formed from these germ layers, they are capable of generating into any cell but are unable to create an entire organism, such as a human or animal, thereby making them pluripotent stem cells. Multipotent stem cells are found in adult tissues but limited in the types of cells they can generate. Adult stem cells cannot differentiate into any specialized cell, instead restricted to a single lineage, depending on where they are found in the body. Adult stem cells are not as 2 James Kim WRIT 340 Aubertin Section 66813 abundant or expansive as their embryonic counterparts since they are only present in specific tissues and organs of the human body. For example, adult stem cells can be found in the human adult’s bone marrow, skin, blood, liver, and pancreas; however, the cell types of the progeny of multipotent stem cells following differentiation are limited to those of the tissue source [2]. Application of Stem Cells in Medicine The capacity of human embryonic stem cells to extensively proliferate in addition to their pluripotency has led to a great increase in interest, studies, and clinical research surrounding stem cells as a possible treatment in regenerative medicine by both the public and medical community over the past decade. While the method of collecting stem cells from human embryos and fetuses has been a subject of ethical controversy, there has been sufficient evidence to suggest directions for applying stem cell therapy in treating diseases, disorders, or damaged tissues. One area of stem cell therapy that has shown considerable promise is the treatment of Parkinson’s disease, a degenerative disorder that afflicts and worsens a patient’s motor skills, coordination, and cognitive functions. These symptoms are caused by the lack of dopamine neurons, or nerve cells responsible for synthesizing the neurotransmitter dopamine, found in the midbrain. Dopamine is responsible for transmitting coordination and body control signals from the substantia nigra area of the midbrain to the corpus striatum [3]. These distinct areas of the brain must effectively communicate and work with one another through relaying motor signals in order for proper muscle movement and control to occur. A study done by the National Institute of Neurological Disorders and Stroke in 2002 used embryonic stem cells from mice as a cellreplacement treatment for dopamine neurons in mice suffering from Parkinson’s. The team used a five-stage procedure they developed to differentiate the mice’s embryonic stem cells into 3 James Kim WRIT 340 Aubertin Section 66813 enriched neurons, which were then transplanted to the afflicted mice to replace its lost neurons. Results were positive, indicating that the neurons generated from stem cells in these mice successfully produced dopamine with behavioral and electrophysical properties consistent with that of those originating in the midbrain [4]. While further trials need to be completed to fully evaluate the long-term safety and viability of stem cell therapy for Parkinson’s disease in humans, studies such as this have convinced scientific experts to agree that further stem cell research will ultimately lead to a cure for the disorder [3]. The Technology Behind The Cell Printer The stem cell printer recently developed by the research team at Heriot-Watt University uses a method of extruding and layering material to print microscopic droplets of stem cells. Three-dimensional printers are unique with respect to the process used to produce solid objects in comparison to other traditional methods. Unlike most machining techniques that cut and remove material- known as a subtractive process- 3D printers use an additive process. Rather than removing material to produce a desired shape, these printers successively layer material in various orientations and sizes on top of each other. There are three primary types of 3D printers currently available that differ in their respective underlying technology: stereolithography (SLA), fused deposition modeling (FDM), and selective laser sintering (SLS) [5]. Each type has its own process for 3D printing; the researchers credited with creating the cell printer essentially modified the FDM method to allow greater precision and delicacy when handling the cells. The fused deposition modeling method was invented and patented by S. Scott Crump in 1989 as an alternative and less expensive method of printing. FDM printers produce a solid shape by using a nozzle to extrude beads made of melted thermoplastics such as ABS or PLA, which are used in commercial plastics, into layers [5]. Once formed into layers, the thermoplastic 4 James Kim WRIT 340 Aubertin Section 66813 material solidifies as it cools down. The stem cell printer developed at the Heriot-Watt University borrows this concept. However, as opposed thermoplastic material as the printer’s “ink,” the cell printer utilizes a unique “bio-ink” comprising of a nutritious “soup” for holding stem cells [1]. Overall, the printer has four primary components that allow functionality: microvalves, dual nozzles, pressurized air supply chambers, and “bio-ink” (Figure 1). The research team behind the cell printer used embryonic stem cells from a kidney and cultured them prior to printing. There are two pressurized air supply chambers, one of which is filled with both the “bio-ink” and stem cells, and the other filled with just the “bio-ink” medium. The pressurized air supply acts as a pump to transport and collect the cells from the chambers into an adjustable micro-valve Figure 1: Schematic drawing of the 3D printer, showing nozzle, valve, microcontroller, bio-ink, and air supply chamber components (Kim/Biofabrication) containing pressurized nozzles at each end. The microvalves were a necessary modification to preserve the cells. The cells are then printed as droplets by the nozzles, which dispense them in successive layers on top of one another [6]. The dual nozzles also feature adjustable diameters to control the rate and size at which the cells are dispensed, displaying remarkable precision by printing droplets as a small as two nanoliters, or approximately five cells. The stem cells are then dispensed onto a well dish, which is flipped to hang the stem cells and enable them to aggregate, or clump into spheroids. Following tests and results have shown that at least 95 percent of the cells were alive after one day, and greater than 89 percent survived the following three days and successfully retained their pluripotency [7]. The primary 5 James Kim WRIT 340 Aubertin Section 66813 breakthrough in the 3D stem cell printers is the process developed by the researchers in handling the extremely sensitive nature of human embryonic stem cells. The controllable valve system in the stem cell printer allows it to create programmable patterns of the stem cell droplets from two different types of “bio-ink”. The remarkable level of control displayed by the micro-valves when dispensing the cell droplets on top of one another is kind and gentle enough to maintain the stem cell’s pluripotency, and precise enough to produce uniform spheroids. Despite the microscopic and Figure 2: Logo of Heriot Watt University recreated by arranging printed stem cell spheroids (Kim et al./Biofabrication) delicate nature of cells, the research team was able to arrange the droplets to recreate the university’s logo (Figure 2). Future Implications of Stem Cell Printing Embryonic stem cells offer momentous potential to treat and cure a broad spectrum of health complications based off their ability to proliferate rapidly and differentiate. Able to generate into any type of somatic cell, stem cells are capable of replacing any lost or damaged tissues or organs, which are comprised of a group of cells performing the same function. With the advent of 3D printing complementing ongoing stem cell research, the idea that we can eventually grow artificial organs becomes a much more feasible option. By manipulating the shape and size of the cells, 3D printers will eventually be capable of printing human organs of dimensions tailored for individual patients in need of transplants. This would effectively eliminate the need for organ donations from other human beings in the future, since embryonic 6 James Kim WRIT 340 Aubertin Section 66813 stem cell printing theoretically enables tissues and organs of any type or proportion to be produced at will. Thousands of human lives would be saved, as patients in dire need of kidney or liver transplants would no longer be subjected to a waiting list or compatible donors. Moreover, printing organs and tissues would be advantageous since patients would not have to deal with the issue of immune suppression or organ rejection. Although organ donations may save a patient’s life, there is always the potential risk of the body rejecting the newly transplanted tissues. The human immune system at times will mistakenly identify a donated organ such as a kidney, heart, or liver as a foreign threat to the body, thus responding by attacking and destroying it. Stem cell printing avoids this complication altogether as the cells of the new organ would be the same as those found in the patient’s body. Printing stem cells implicitly affects the future of the pharmaceutical industry as well. Clinical trials would be much safer and effective since researchers would no longer require human or animal subjects. Instead, experts would be able to test the effects of newly developed drugs on artificial livers and tissues they print. As a result, there would be far less liability, ambiguity, and regulation during these trials without the need for living patients. Utkan Demirci, a biomedical engineer at Harvard Medical School who has pioneered similar work in cell printing, optimistically believes “this technology could be really good for high-throughput drug testing” as it is currently capable of printing small tissues [7]. Despite these promising strides made in cell printing technology, Demirci has also admitted that the ability to print entire organs “may be quite far from where we are today” [7]. There are current hurdles associated with the printing technology and stem cell viability that prevent us from directly printing organs. Up until the recent breakthrough by the Heriot-Watt researchers, human stem cell cultures have been too sensitive for the 3D printing process. The 7 James Kim WRIT 340 Aubertin Section 66813 improvements made to the stem cell printer’s precision and gentleness has been the first development of its kind, yet the overall process is far from being polished or refined. The stem cell printer is limited to printing smaller tissue models, as it is not advanced enough to maintain the viability of human cells composing of larger tissues and organs over extended periods of time. Printing biological structures such as kidneys or hearts, which serve invaluable roles necessary for human survival, that will remain stable over long periods of time is a difficult challenge. In order to some day print viable human organs, the underlying technology and process behind 3D stem cell printing must be completely mastered or perfected. While initial test results showed that over 89 percent of the stem cells printed were alive and retained pluripotency three days later, this is a far cry from implying that human organs can be successfully printed. The 3D printing technology must first prove that it is capable of printing tissues of larger dimensions that will retain their viability for multiple years before it is accepted as a legitimate, safe method for producing human organs for transplant. The current 3D stem cell printer is capable of manipulating the size of the cell droplets, but has yet to prove it possesses the capability to print entire organs of larger, complex dimensions. Additionally, the fact that there is an 11% failure rate among the printed stem cells in surviving past three days provides a sense of relativity in judging how far we are from printing viable, long-term artificial organs. Conclusion Stem cell research is still an ongoing process that faces several hurdles before it is fully accepted as a viable medical treatment by mainstream society. The method required for collecting human embryonic stem cells is marred by political, ethical, and religious controversy as it often ends in the destruction of the embryo. This issue, in addition to the current technological limitations on the 3D cell printing process, has largely precluded stem cell research 8 James Kim WRIT 340 Aubertin Section 66813 and clinical studies from progressing to the extent many scientific experts had anticipated. However, this should not detract from the immense potential of stem cell printing in permanently changing both the medical industry and the way we treat patients in need of organ transplants. Improvements to the technology of 3D printers in conjunction with stem cells will implicitly reinforce the need for future applications of stem cell therapy in treating a bevy of “incurable” health complications. 9 James Kim WRIT 340 Aubertin Section 66813 References [1] A. Faulkner-Jones et al., “Development of a valve-based cell printer for the formation of human embryonic stem cell spheroid aggregates,” Institute of Biological Chemistry, Biophysics and Bioengineering, School of Engineering and Physical Sciences, Heriot-Watt Univ, Edinburgh EH14 4AS, UK, Rep. 015013, Feb. 2013. [2] Stem cell (biology) [Online]. Available: http://www.britannica.com/EBchecked/topic/565211/stem-cell [3] C. Norddqvist. (2012, Oct. 4). Parkinson’s Disease Cure May Be In Stem Cell Research, But.. [Online]. Available: http://www.medicalnewstoday.com/articles/251154.php [4] J. Kim et al., “Dopamine neurons derived from embryonic stem cells function in an animal model of Parkinson’s disease,” National Institute of Neurological Disorders and Stroke., Bethesda, MD, vol. 418, 2002. [5] What is 3D Printing? An Overview [Online]. Available: http://www.3dprinter.net/reference/what-is-3d-printing [6] J. King and W. W. Shu. (2012, Jul. 1). Organ Printing from Stem Cells [Online]. Available: http://www.genengnews.com/gen-articles/organ-printing-from-stem-cells/4171/ [7] T. Lewis (2013, Feb. 06). 3D printer spits out human embryonic stem cells [Online]. Available: http://www.foxnews.com/science/2013/02/06/3d-printed-human-embryonic-stemcells/ 10