NCIIA Proposal - Research
advertisement

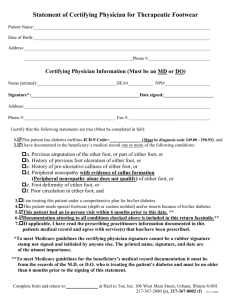
Vanderbilt University Department of Biomedical Engineering BME 272 Offloading Device for the Reduction of Foot Complications in Diabetes Patients Date Reported: November 2, 2005 Reported by: Michael Osborne Rod Aliabadi Colin Smith Patrick Gonzales ABSTRACT Diabetes is a disease afflicting more than 20 million people in the United States alone. Of these 20 million people 17% will go on to develop diabetic foot ulcerations, which often lead to amputations. The average cost for a 40-65 year old male patient who developed such an injury is $28,987 during the two years after diagnosis. The manifestations of these diabetic foot ulcerations often require specially adapted footwear. A comprehensive concept of the medical, functional, and technical requirements for this type of footwear is still lacking to date. The Diabetes Committee of the American Orthopedic Foot and Ankle Society recommends the use of pressure-dissipating noncustom insoles or custom-fabricated pressure dissipating accommodating foot prosthesis for the low-risk category patients with the diabetic foot. For patients with more advanced conditions (deformities and ulcers), only custom made prosthesis are recommended. Devices have been developed to offload pressure on the foot with the intent to reduce vertical plantar forces and shear pressures on the ailing foot. The costs and specifications of these devices bring forward the issue of socioeconomics involved in the current methods of treatment. A new device is needed that can underwrite the preceding issues. The intent is to develop a design which has generic exterior qualities but a modifiable insole. This product will need to take into consideration both shear pressures and vertical forces applied to the foot with the intent of offloading and alleviating the foot from pain and preventing future ulcerations. PROPOSAL Diabetes is a disease that affects 7% of the American population or 20.8 million people that is characterized most clearly as inadequate insulin action. It is currently the most rapidly growing disease in the country, as the incidence has been increasing by 17% per year in recent years. This increase is likely attributable to obesity and poverty in many patients. Major symptoms of well progressed diabetes include neuropathy and circulatory disorders. These effects can take a devastating toll on the feet of diabetic patients. A normal healthy person has protective sensation in their feet that allows them to avoid irritation and possible injury. However, diabetic patients have lost sensation entirely and often do not feel an injury when it occurs. In fact, 15-20% of the patients that have diabetes, about 4 million people, will experience complications of the disease in their feet. Due to neuropathy and decreased blood supply, these wounds often do not heal quickly and can actually become much worse without intervention. An ulcer can develop that may not be possible to heal, which can lead to whole limb amputation. The best strategy to combat this problem is to design protective footwear that prevents such injuries from occurring in vulnerable patients. Protection of the diabetic foot is complicated by other adverse effects of diabetic neuropathy. The foot loses its typical structure in progressed diabetes because the neural supply to the musculature in the foot becomes inadequate. This results in major structural changes and deformation, such as the loss of a longitudinal arch, which cause the distribution of the foot's loading to differ from typical the weight-bearing regions (the first and fifth metatarsal head and the heel). The displaced pressure in other areas of the foot is a major cause of diabetic ulcers. These sites must be offloaded in some fashion to remove the excess weight from them during daily tasks. A common method of accomplishing this goal is the use of custom made shoes and inserts made by a pedorthist. The insert is typically made of a material that conforms to the foot, such as foam or a gel. The custom-made shoes also provide protection, extra depth, and a loose environment to avoid injury. However, due to the labor required for customization, these shoes and inserts can be very expensive, more than $2000, which is far too costly for some patients to afford. These patients do not want to pay for shoes that are extremely expensive and sometimes unsightly when it is not economical to do so. Therefore, our group seeks to develop new insert technology that protects the diabetic foot from injuries, is adaptable to any foot shape, facilitates foot care, is affordable, and can be changed readily to adapt to further changes in foot conformation. The device will be made to fit in any extra-depth shoe with minor modifications. After researching the causes and problems involved with diabetic foot ulcers, the next step is to investigate the availability of products that already serve to alleviate and manage these symptoms. Product research and evaluation also allows analysis of cost and the contribution of Medicare and health insurance on an individual basis towards this cause. The average cost for a customized diabetic foot shoe and insert runs upwards of two thousand dollars a set. The generic (non-customized) shoe (extra deep and extra wide) can cost anywhere from $100 to $300. There are a number of companies who have devoted time and effort towards developing these podiatric-prostheses. Xilas Medical of San Antonio, Texas developed a product labeled Glidesoft. This item featured a multilayer Viscoelastic insole. The low friction allows the insole to “slide” within its inner layers under shear forces, thus reducing the peak shear by 57% compared with standard insole configurations. The problem with this design is that it did not cause for any lowering of the vertical pressure applied to the foot. A design that follows a different methodology and theory is that of the F-scan developed by Teksan, INC, in Boston, Massachusetts. Their technology provides vertical plantar force measurements at the foot-shoe interface. A feature product combining the two technologies has not yet come into existence. The present day approach to the issue is taken in two separate forums, that of the shoe and that of the insert. With the growing population of thirteen million Americans with diabetes, the demand for disease management products is constantly rising. With the advent of more and more need, comes a more customized approach to the health care of the patients. Customization brings excess costs. The biomaterials and actual development of the product are not the areas that incur the majority of the cost. In reality the large portion of the cost goes to the foot-care specialists who are custom designing each and every shoe. Medicare has taken measures to comply with the needs of patients suffering from diabetic foot complications. There following policy implemented by the Medicare agency describes the discrepancies. 1. The patient has diabetes mellitus (ICD-9 diagnosis codes 250.00-250.91); and 2. The patient has one or more of the following conditions: • Previous amputation of the other foot, or part of either foot, or • History of previous foot ulceration of either foot, or • History of pre-ulcerative calluses of either foot, or • Peripheral neuropathy with evidence of callus formation of either foot, or • Foot deformity of either foot, or • Poor circulation in either foot; and 3. The certifying physician who is managing the patient’s systemic diabetes condition has certified that indications (1) and (2) are met and that he/she is treating the patient under a comprehensive plan of care for his/her diabetes and that the patient needs diabetic shoes. For patients meeting these criteria, coverage is limited to one pair of shoes with protective inner soles within one calendar year. According to these regulations coverage is limited to one pair of shoes with protective inner soles during one calendar year. This has the potential to become a large issue and problem in the patient’s life due to the fact that additional ulcerations might occur. If they do, the shoes they have will be insufficient and will not be replaced for a long period of time. This combined with the economic insufficiency portrayed by the industry as a whole are key factors in our innovative and comprehensive design. Our preliminary plan for design after the completion of our research, market analysis, and receipt of customer input is to design a readily customizable insert as a less expensive option for therapeutic footwear. Additionally, we plan for it to offer versatility by fitting snuggly into standard sized diabetic footwear with minor modifications. Many shoe companies, like New Balance, offer extra depth shoes that would facilitate such an insert. The insert would mostly likely surround the bottom of the foot, providing padding and support. At the base would be a layer of shaped hard plastic to act as a defensive barrier to injury. This base would form a box around the toes, a protective heel structure, and a hard sole. Inlaid into this would be the insert design, which would likely consist of a number of carefully designed foam layers to provide maximum adaptation and support for a deformed foot. The least important layers will be placed closest to the surface. A layer or more could be removed from the insert in areas of high pressure, as determined by computer analysis of a patient's gait or structural analysis of the foot. In areas of frequent ulceration, the layers would be perforated to simplify layer removal. In unusual areas, the layers could still easily be cut away. A booklet describing the ideal offloading strategy for a typical morphological change is planned for inclusion. Such a device would facilitate simple customization by any specialized health care worker or the patients themselves, greatly reducing the labor cost of personalizing an entire insert and shoe. The shoe would also be readily changed to adapt to changing foot morphology. Previous changes would be reversible by affixing the removed section back into the insert. The costs for using such a device would essentially be for the insert, the exterior extra depth shoe, and the structural analysis. The adaptability of our product would eliminate the risk associated with receiving only one pair of shoes per year. Also, the insert would be able to be cleaned with standard sterilizing agents, and it would do nothing to obstruct a user's daily foot care. In summary, this product would be more affordable and practical for all at-risk patients than existing technology. It would also satisfy the desire to have further control over the exterior shoe they are wearing. Hopefully the versatility and reduced cost of such a product would have a broad market appeal for insurance providers and government subsidized medical programs to gain further approval for device funding for the patients who need help from such a device. Nevertheless, this device should have a great appeal for low income patients, if its effectiveness is shown to be equivalent to that provided by costly custom made shoes. Our design team includes a group of three senior undergraduate biomedical engineers, who have educational backgrounds in physiology and biomechanics, and one senior undergraduate mechanical engineer, who has knowledge of materials, mechanics, statics, and dynamics. Due to our different majors, we hope to incorporate wide aspects of our engineering backgrounds. All members of our design team have completed three years of education at Vanderbilt University, an institution accredited by Accreditation Board for Engineering and Technology. We hope that by incorporating our knowledge we can be better to face the challenges of developing our design. Our team is also supported by several faculty advisors and medical experts at Vanderbilt University and the Vanderbilt University Medical Center. These advisors include our primary advisor, Dr. Paul King, a professor of Biomedical Engineering and a licensed professional engineer, and our primary investigator, Dr. Naji Abumrad, Chairman of Vanderbilt University Department of Surgery. Additional support is being provided by Michele Frisbie, a nurse at The Vanderbilt Wound Clinic. We also intend to receive advice from Dr. Robert Schwartz, a vascular surgeon in Syracuse, and Dr. Horace Watson, an orthopedic surgeon who works with the Vanderbilt Eskind Diabetes Clinic. The group also plans to consult experts in the industry of orthotics and shoe design. There are aspects that will need to be further researched for our project other than our aforementioned design. A search for prior patents involving diabetic footwear should be conducted in order to conclude that our design is in fact a new idea. Next, a survey is currently being conducted to directly determine the needs of patients that suffer from this problem and are in need of help. From this information we can utilize their input to address issues such as comfort, cost, and style. This contact is necessary before finalizing our design and could also be beneficial after a prototype is constructed for first hand testing. We have been advised to continue our research by contacting shoe and insole companies that specialize in this field. We are researching the specific companies that would custom design stylish shoes that are deeper to allow for large insoles. A search for plausible biomaterials would need to be conducted from a monetary and comfort standpoint. The foam material must conform to any shoe and fit snugly around the patient’s foot, providing extra support around the side and toe areas. There will be numerous materials tested for each layer in terms of stability, comfort, and distribution of pressure in order to optimize our shoe design. Extra support for the top of the foot and ankle is also a possible option. This would entail either a type of elastic band or other padded material in order to prevent slippage from the insole. Another major necessity of the project includes devices to facilitate testing of the distribution of pressure on the bottom of a foot. A lab that performs these types of tests is located nearby at Belmont University. Finally, typical mechanical tools will be required to construct the prototype model of the insert. Many of these are readily available. In conclusion there is an ever increasing need for an inexpensive but effective alternative to customized orthotic shoes. A product that offers the combination of versatility, decreased cost, and preventative technology is sought by this growing market, including the government and insurance agencies that provide it coverage, in order to reduce the risk of foot complications due to diabetes. A preliminary design is in place, and with the support of a variety of medical and design experts, further research, and patient input, it can hopefully be optimized to change the current approach to providing healthcare to this significant portion of the population. The project is to be concluded by early May. As such, the preliminary design work and research must be complete by the start of next semester. The design will be fine tuned to prepare detailed drawings of a prototype design in January. We plan to produce a prototype by March and spend the remaining time testing and improving the design. The total cost for the project is approximately $2000. The cost includes estimates of the costs of lab use for gait analysis, materials, and prototype construction. A description of the project and its innovative features. If the institution has received previous NCIIA funding for this or a related project, a description of the results of the funded project A discussion of your project’s market potential, including o the size of the potential market, o competitive advantages o the project’s consumer appeal o a survey of the existing art, basic competitive intelligence, and a clear development strategy. A description (if applicable) of the project’s social and environmental impact. A list E-Team members, their skills, and their roles in this project, including students, faculty, industry experts, mentors, and other advisors. A work plan and timeline for the project. A list of equipment and other resources necessary for the project. Indicate whether your institution will provide access to these resources and, if not, how you will access them.