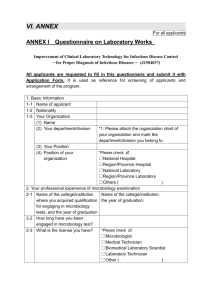
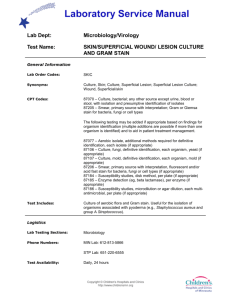
Clinical Microbiology and
advertisement

NHS GENERAL Microbiology Laboratory Users Handbook Microbiology Laboratory North Tyneside General Hospital Rake Lane North Shields Tyne & Wear NE29 8NH CONTENTS OF CLINICAL MICROBIOLOGY USERS HANDBOOK LOCATION OF COPIES 1. Q-pulse 2. Internet/Intranet 3. ICE desktop WRITTEN AND AUTHORISED BY Microbiology Speciality Board Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Speciality Board Created: 19 th December 2014 Disposal date: 19th December 2044 Page 1 of 60 NHS GENERAL CONTENTS Table of Contents Document Control, General Information, Quality Management Microbiology laboratory hours Clinical medical microbiology service telephone numbers Major incidents and outbreaks Microbiology laboratory telephone numbers Infection Control Team and telephone numbers Transport arrangements Supplies (forms, containers, bags) Consent for HIV, HCV, HBV Specimen labelling and Request Form requirements. Clinical details Multiple specimen requirements Additional tests Transport Urgent specimens Spillages and breakages Concerns, comments, complaints High risk specimens Specimen container Antibiotic prescribing Uncertainty of results Factors that may affect results Specimen Ordering on ICE/Electronic Requesting – Guidance, Contacts, Instructions for Coloured Pouches for Specimens Specimens: Test, container, volumes, storage, time to result : Microbiology Test, container, volumes, storage, time to result , reference ranges : Serology Clinical scenarios and laboratory requirements Results Referred Tests to : Newcastle Hospitals including HPA, Freeman, RVI Referred tests to :Immunology Gateshead Referred tests to : Other Laboratories Investigation and guidelines for: Blood cultures Cerebrospinal fluid Chlamydia PCR Faeces Fungal investigations Gentamicin assay Pertussis Pregnancy test Quantiferon gold Seminal fluids – post vasectomy specimens Information for patients – vasectomy semen analysis Seminal fluid - Investigation of infertility Information for patients – infertility semen analysis Sputum Threadworm+ PAGE 2-3 4 5 5-6 6 7 8-9 10 11 12 13 14 14 14 14 15 15 15 15 15 16 16 17 18 18 19-24 25-30 31-36 36 37 38 39-40 41 41 41-42 42-43 43 43 44 44 45 46 47 48 49 50 51 Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 2 of 60 NHS GENERAL Throat swabs Urethral swabs Urine culture Vaginal and cervical swabs Vancomycin assay Virology Wound swabs Appendix 1 – reference laboratories 51 51 52-53 53 53 53 54 55-60 Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 3 of 60 NHS GENERAL DOCUMENT CONTROL This handbook is subject to the document control measures used in Pathology. As this version is controlled electronically, any printed hard copy or locally saved copy will no longer be subject to the control procedures. Please ensure that any reference is made to the current active version of this document. GENERAL INFORMATION The efficiency of the service we provide is reliant on the cooperation of all our users with the necessary policies relating to safety, specimen transport and specimen/ patient identification. We hope this handbook contains all the information you require to use our service. Users of the service are encouraged to contact us to discuss any problems, issues, comments or suggestions to improve the handbook or the service. QUALITY MANAGEMENT Microbiology is committed to maintaining accreditation for its quality management system. Accreditation is undertaken by Clinical Pathology Accreditation Ltd. an independent external organisation. Details of our accreditation are available from the Pathology Service Manager. The laboratory participates in all appropriate external quality assurance schemes. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 4 of 60 NHS GENERAL MICROBIOLOGY LABORATORY HOURS The Microbiology department operates a full 24/7 shift system. For all urgent specimens where results will affect patient management decisions please contact the laboratory on either extension 2528 or 4617. CLINICAL MEDICAL MICROBIOLOGY SERVICE TELEPHONE NUMBERS Northumbria Healthcare NHS Foundation Trust Switchboard Consultant Secretary Mrs Val Twizell Dr D Tate, Clinical Lead Consultant Microbiologist Dr B Marshall Consultant Microbiologist Director of Infection Prevention & Control Dr T Oswald (Part-time) Consultant Microbiologist Trust wide Lead for Antibiotic Use Dr S Sundeep (Part-time) Consultant Microbiologist Dr J Sarma Consultant Microbiologist Specialist Registrars Based at North Tyneside General Hospital 0844 811 8111 Direct: Internal Direct: Direct: Internal Internal Air call Direct pager Direct: Internal Air call Direct pager Direct: Direct: Internal Internal Air call Direct pager Direct: Internal Air call Direct pager Direct: Internal Air call Direct pager Internal Air call Direct pager 0191 293 2538 ext:2538 0191 293 4067 (NTGH) 01670 529 702 (WGH) ext:4067 (NTGH) ext:3702 (WGH) #6984 07623 624753 0191 293 4314 ext:4314 #6518 07623 976205 01670 529 3736 (WGH) 0191 293 4316 (NTGH) ext:3736 (WGH) ext:4316 (NTGH) #6749 07623 976260 0191 293 4317 ext:4317 #6857 07623 623773 0191 293 4315 ext:4315 #6220 07659 523738 ext:4578 #6952 07623 614133 Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 5 of 60 NHS GENERAL Clinical on-call advice For advice weekday evenings after 5pm, weekends after 12.30pm and Bank Holidays after 12.30pm cover is available from the extended clinical microbiology network from Northumbria Healthcare NHS Foundation Trust, Newcastle Hospital Trusts (RVI, Freeman). Contact the hospital switchboard internal 1100, external 0344 8118111 and ask for the first on-call medical microbiologist. For advice weekends and Bank Holidays between 9.00am – 12.30pm contact the Trust switchboard on 0344 8118111 or extension 1100 and ask for the covering microbiologist. Major incidents and Outbreaks Contact the Northumbria Healthcare NHS Foundation Trust Consultant Microbiologist on call, via the Trust switchboard 0344 811 8111. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 6 of 60 NHS GENERAL MICROBIOLOGY LABORATORY TELEPHONE NUMBERS Results: please note that we need to establish the caller’s identity before giving results over the telephone. We are unable to give results directly to patients or their relatives. Please check electronic links for results, before telephoning the laboratory. Laboratory results Not available until 11.00am each morning Direct Internal 0191 293 2528 ext.: 2528 Urgent results Direct 0191 293 4617 Internal ext.: 4617 Or contact a Consultant Microbiologist General enquiries Direct Internal 0191 293 2528 ext.: 2528 Bacteriology laboratory Direct Internal 0191 293 2528 ext.: 2528 Serology & Virology laboratory, Immunology enquiries Direct Internal 0191 2932528 ext.: 4689 Consultant Secretary Direct Internal 0191 293 2538 ext.: 2538 Chief Biomedical Scientists (BMS3) Direct Internal 0191 293 4173 ext.: 4173 Senior Chief Biomedical Scientist (BMS4) Direct Internal 0191 293 4171 ext.: 4171 Pathology Services Manager Mr Mike Carr Direct Internal 0191 293 4005 ext.: 4005 Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 7 of 60 NHS GENERAL INFECTION CONTROL TEAM TELEPHONE NUMBERS Infection Control Doctors Dr B Marshall Director of Infection Prevention & Control, Trust wide Dr D Tate Clinical Lead Direct Internal 0191 293 4314 ext.: 4314 Direct Internal Direct Internal Direct Internal Direct Internal 0191 293 4067 (NTGH) ext.: 4067 (NTGH) 01670 529 702 (WGH) ext.: 3702 (WGH) 01670 529 3736 (WGH) ext.: 3736 (WGH) 0191 293 4316 (NTGH) ext.: 4316 (NTGH) Dr Sundeep Direct Internal 0191 293 4317 ext.: 4317 Dr J Sarma Direct Internal 0191 293 4315 ext.: 4315 Mrs Diane Sisterson Lead Nurse Trust wide Mobile Internal 07824 409223 ext.: 2368 (NTGH) ext.: 3742 (WGH) Mrs Ruth Henein Senior Nurse NTGH Mobile Internal 07900165296 ext.: 2385 (NTGH) Mrs Janet Wendt Clinical Nurse NTGH Mobile Internal 07770908347 ext.: 2385 (NTGH) Mrs Shelly Goodson Clinical Nurse NTGH Mobile Internal 07825 365313 ext.: 2367 (NTGH) Mrs Cathi Lang Senior Nurse WGH Mobile Internal 07776 460368 ext.: 3742 (WGH) Mrs Rachel Watson Clinical Nurse WGH Mobile Internal 07899 067793 ext.: 3397 (WGH) Ann Hindhaugh Clinical Nurse WGH Mrs Ania Swann Clinical Nurse WGH Mobile Internal Mobile Internal 07774402841 Ext: 3742 (WGH) 07824 408877 ext.: 3397 (WGH) Dr T Oswald Hospital Infection Control Nurses Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 8 of 60 NHS GENERAL Infection Control Support Nurse Carol Bailey Mobile: 07824408585 Internal ext.: 2357 Internal ext.: 2973 Infection Control Secretary Aimée Joyce (NTGH) Information Support Giles Idle (NTGH) Community Infection Control Team (Northumberland) Deb Elliott Senior Nurse Community Mobile Internal Susan Bestrode Clinical Nurse Community Alison Knowles Clinical Nurse Community Heather Lawson Clinical Nurse Community Mobile Internal Mobile Internal Mobile Internal 07919 592326 ext.: 3742 (WGH) ext.: 5077 (HGH) 07500 552979 ext.: 3742 (WGH) 07920298056 ext.: 3397 (WGH) 07799075296 ext.: 3742 (WGH) Community Infection Control Team (North Tyneside) Judith Slocombe IPC Practitioner Arlene Pattem Clinical Nurse Community Mobile Internal Mobile Internal 07771 388508 ext.: 2309 (NTGH) 07785 778470 ext.: 2309 (NTGH) Infection Control Advice, Outbreaks and Incidents For infection control advice out-of-hours contact the appropriate Medical Microbiologist on call, through the Trust switchboard. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 9 of 60 NHS GENERAL MICROBIOLOGY TRANSPORT ARRANGEMENTS GP Monday – Friday Saturday – Sunday Out of hours (5pm – 8am) Trust Hospitals Monday – Sunday Out of hours (5pm – 8am) Transport arrangements Courier Own arrangements to transport specimens to WGH, HGH or NTGH pathology specimen reception department By arrangement, otherwise please store as advised Transport arrangements Air tube to local pathology laboratory Contact the laboratory on extension 2528 to arrange transport Please ensure that specimens are forwarded to the Microbiology department on the North Tyneside site as soon as possible after collection. All specimens taken on the Wansbeck and Hexham hospital sites are subsequently forwarded to North Tyneside by courier. Please ensure that specimens are forwarded to the appropriate Pathology specimen reception as soon as possible after collection to facilitate a timely delivery to the North Tyneside site. During the Normal working day specimens taken by GP’s in the Wansbeck General Hospital and Hexham General Hospital catchment area are collected by courier and taken to Wansbeck and Hexham Pathology Specimen Reception prior to forwarding to North Tyneside. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 10 of 60 NHS GENERAL SUPPLIES All supplies including request forms, specimen containers and transport bags are issued by the local pathology specimen reception departments. It is important to ensure that requests for supplies are made between the hours of 9am - 4pm Monday to Friday. Wansbeck General Hospital: Monday – Friday 9am - 4pm By telephone: (01670) 521212 ext. 3758. If no one is available please leave a message on the answer-phone By completion of a laboratory supplies requisition form this may be posted Hexham General Hospital: Monday – Friday 9am - 4pm By telephone (01434) 605001 By completion of a laboratory supplies requisition form. This may be posted in or faxed to (01434)655017 North Tyneside General Hospital: Monday – Friday 9am - 4pm By Telephone : 0344 811 8111 ext. 2031 (Pathology Specimen Reception) By completion of a laboratory supplies requisition form This may be posted in or faxed to (0191)2934137 Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 11 of 60 NHS GENERAL PATIENT CONSENT It is important to ensure patient consent has been obtained prior to submitting specimens for testing where there are clinical grounds for suspecting HIV, Hepatitis B and Hepatitis C Infections. Patient consent must be given for all HIV testing, pre and post counselling must be offered. Indication that consent has been given must be made clear on the request form. For Hepatitis B markers performed on staff involved in Exposure Prone Procedures through Occupational Health, written consent must be provided and submitted with the specimens. Specimens MUST be labelled with “Danger of Infection” stickers on the specimen, bag and form. The form must be folded to ensure confidentiality. The specimen must be sealed in the plastic transport bag. The specimen must then be placed in a second plastic bag and sealed. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 12 of 60 NHS GENERAL GENERAL REQUIREMENTS FOR MICROBIOLOGY SPECIMENS REQUEST FORMS To fall in line with Trust Policy and to comply with the Safer Practice Notice from the National Patient Safety Agency (NPSA/2009/SPN002) the laboratory will no longer accept request forms/samples with less than 3 patient identifiers. All request forms must include the following: NHS number Full patient name Trust Number Date of birth Location Date and time of specimen collection Requesting Doctor/Practitioner and Consultant/GP All appropriate Clinical Information relevant to tests requested In the event that it is not possible to use electronic requesting then a manual request form should be submitted along with the sample. It is IMPORTANT to ensure that the manual request form includes the information as detailed above. SPECIMEN LABELLING All specimens must be labelled with the following: Full patient name Date of birth NHS or Trust number and should have Date and time of specimen collection Location Please note unlabelled or inadequately labelled specimens will be rejected in all but exceptional circumstances. ALL HIGH RISK specimens MUST have hazard stickers attached to both specimen and request form. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 13 of 60 NHS GENERAL CLINICAL DETAILS When sending a sample for analysis, it is very important that the laboratory is given sufficient, relevant, clinical information including antibiotic therapy to enable the department to determine the type of examination required. Certain pathogens require special techniques and may not be detected in the routine examination of a sample. Failure to include clinical information could compromise patient care. Relevant details may include: Types of symptoms Other recent infections Date of onset of illness Underlying conditions e.g. diabetes, cystic fibrosis Pregnancy Foreign travel Mention of antibiotic therapy in diarrhoea will alert the laboratory to the possibility of C.difficile. It is important that wherever possible specimens should be taken before the commencement of antibiotic therapy. An important exception to this is when a patient is suspected of having meningitis where antibiotics should always be given as soon as possible as it may be lifesaving. MULTIPLE SPECIMEN REQUIREMENTS Separate clotted blood samples are required when requesting Microbiology and Immunology tests. If only one tube is received for multiple testing including Biochemistry, Microbiology/ Immunology investigations only the Biochemistry assays will be performed. Repeat samples will be requested. Specimens for Microbiology including Virology, Serology and Immunology should be placed in a blue specimen pouch. ADDITIONAL TESTS If additional examinations are required after the sample has been received at the laboratory please contact a Medical Microbiologist who will advise. An additional request form will always be required for additional tests. TRANSPORT All specimens must be transported in sealed blue pouches with the laboratory request forms. It is important for specimens to reach the laboratory as soon as possible, ideally, the same day. If there is to be a delay in transport keep specimens cool, preferably refrigerate. NB.CSF and blood cultures must be sent to the laboratory immediately. Please ensure that containers are properly sealed to prevent leakage and that the request forms are not placed in same bag as the specimen. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 14 of 60 NHS GENERAL URGENT SPECIMENS During normal laboratory hours please telephone the Microbiology department to arrange for urgent samples to be processed urgently. You will be advised by the laboratory where to send the sample. SPILLAGES AND BREAKAGES Make safe all spillages and breakages promptly according to local protocols. NB. It is essential that specimens are not contaminated with disinfectant please contact the Laboratory for advice if required. CONCERNS, COMMENTS AND COMPLAINTS Please contact the Laboratory either by telephone or in writing, so you can be referred to the most appropriate person to deal with your concern. Written complaints should be addressed to Mr. M Carr, Pathology Services Manager or the Lead Consultant Microbiologist. Serious complaints will be passed to the Trust Complaints Department or the Complaints Department can be contacted directly. HIGH RISK SPECIMENS Include those from known or suspected cases of: HIV infection Hepatitis B Hepatitis C E.coli O157 Mycobacterium tuberculosis (TB) Salmonella typhi (Typhoid fever) All other Category 3 and 4 organisms (Advisory Committee on Dangerous Pathogens) Coccidioides immitis NB Specimens MUST be labelled with “Danger of Infection” stickers on the specimen, bag and form. The form must be folded to ensure confidentiality. The specimen must be sealed in the plastic transport bag. The specimen must then be placed in a second plastic bag and sealed. SPECIMEN CONTAINER It is important that the laboratory receives the correct specimen type in the correct container. Specimens for bacteriological investigation should be collected into a sterile, laboratory specified container, see section entitled ‘Microbiology Specimens’. This ensures that there are no contaminating organisms that may interfere with the interpretation of the investigation and that there are no substances present in the container which may affect the culture of any microorganisms. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 15 of 60 NHS GENERAL ANTIBIOTIC PRESCRIBING Please refer to the following guidelines: Guide to the use of antimicrobials in adults (http/intranet/antibiotics/handbook/default.asp) Trust policy for The Prudent use of Antimicrobial Drugs (CG46/MM10) North of Tyne Area Prescribing Committee, Primary Care Guidelines for the Management of Infection Contact the Clinical Microbiologists for advice through the Microbiology Consultant’s Secretary, on 0191 293 2538 UNCERTAINTY OF RESULTS The laboratory must ensure that there are no adverse effects which may compromise the certainty of results obtained within Microbiology. There are various factors that can influence the precision of the microbiological results and require appropriate quality control procedures to minimise variation. Sources which may have an effect on the microbiology results include: Sampling and transportation – The method of sampling must be appropriate to the specimen type as stated in the user handbook. The sample must be transported to the laboratory in a timely manner under suitable conditions. Any delay in the receipt of the sample arriving in the laboratory may affect the quality of the result. Storage time and temperature of sample - the sample must be suitably stored on receipt until the analysis is performed. Method of analysis – All methods used within the laboratory have been appropriately validated. The laboratory subscribes to a number of National External Quality Assurance schemes to ensure the proficiency of testing. Culture media and reagents –internal quality control is performed on all reagents used within the laboratory to ensure consistency of performance. There are performance sheets available for all culture media used in the laboratory. Daily temperature monitoring is undertaken to ensure that media and reagents are stored under the correct conditions and expiry dates are monitored on a weekly basis. Analysis of samples – internal quality control is performed on all reagents and kits prior to use within the laboratory. Equipment – all equipment including analysers are regularly maintained, calibrated and quality controlled to ensure the accuracy and precision of the results. Personnel – all staff undertake regular competency assessments appropriate to their grade to ensure they are proficient in the testing repertoire. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 16 of 60 NHS GENERAL FACTORS THAT MAY AFFECT RESULTS Delay in transport: May affect the viability of pathogens and allow overgrowth of normal flora or contaminating organisms. Morphological appearance of cells may also be affected. Excessive temperatures: Serology Leave fresh blood at room temperature to clot. Do not freeze or overcool any whole blood samples. Bacteriology Increases in temperature may increase bacterial activity leading to misleading high counts for pathogens (fluids) or overgrowth of normal or contaminating flora (swabs). Excessive high or low temperatures may kill the target organisms. Inappropriate specimen, site or If the specimen is taken from the wrong site (e.g. transport medium: vaginal rather than cervical), or it is the wrong type of specimen (e.g. swab rather than pus), or it is put into the wrong transport medium (e.g. viral transport rather than bacterial transport) then optimal recovery of the target organisms will not be possible. Clinical Information: It is essential that appropriate clinical information is supplied. This will include the specific anatomical site, the nature of the sample, and history of foreign travel, occupation if relevant, and contact with animals. Failure to provide relevant information may mean that the most appropriate investigation is not performed. Haemolysis: Severe haemolysis may compromise the results of serology assays. Onset of illness: There are some serology tests where the onset of illness needs to be specified as this will affect results and interpretation of results. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 17 of 60 NHS GENERAL Specimen Ordering on ICE/Electronic Requesting Guidance for Use There are comprehensive manuals built into ICE, available to all users. Shorter guides and demonstrations are also available on the Trust Intranet training pages. External link: http://intranet/it_training/icedesktop.htm Contact Names for ICE For Pathology Trust wide: Application Management Team, Tel: 0191 2031306 (Cobalt Ext: 1306) For Microbiology: Denise Izon, Tel: 0191 2934171 (NTGH Ext: 4171). Instructions for Use of colour coded specimen pouches and transport bags Microbiology, Serology and Immunology (blue pouch) Label sample and request form with a minimum of 3 unique patient identifiers (name, DOB, NHS/Trust Number). All microbiology, serology and Immunology tests are highlighted in blue on the request screen. Select ‘New Request’ followed by the required test and print the request form. In the event that you are unable to print an electronic request form, please complete the reverse side of the printer paper, ensuring patient’s name, DOB and NHS/Trust number, requestor, location and date taken are competed. NB Only to be used in the event of a system failure. Place the sample and the request form in the blue pouch as indicated on the pouch. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 18 of 60 NHS GENERAL MICROBIOLOGY SPECIMEN REQUIREMENTS Investigation time = time from receipt of the specimen into the laboratory to 90% of reports leaving the laboratory. Type of Specimen Container/ Volume Storage (if necessary) Investigation Time Comments Blood culture Blood 7-10ml of blood into each of 1 aerobic and 1 anaerobic bottle Paediatric bottles are available for small volumes of blood. Send to the laboratory as soon as possible Negative: 5 days Positives will be telephoned to ward nursing staff. Usually 24-48 hours. If clinical advice is required contact a medical microbiologist. Special swabs required, available from laboratory 2 - 27oC for up to 3 days 48 hours Specimens are batched Neonatal eye swabs become positive at about 10 days post-partum Sterile white topped universal bottle 15-20ml Refrigerate for 4-6 days 4oC 48 hours Specimens are batched. First voided urine 15-20ml preferred or a wait of one hour since last voided sample. Rectal swab Liquid transport swab 24 hours Must be discussed with medical microbiologist before taking specimens Faeces Blue screw capped bottle with spoon Send to the laboratory as soon as possible Send to the laboratory as soon as possible 24 hours Must be discussed with medical microbiologist before taking specimens Always urgent Microscopy – urgent. Culture: 3 days. Always contact the microbiology laboratory to notify them that the sample has been taken, they will arrange appropriate transport. Chlamydia PCR Chlamydia PCR: Endocervical and Urethral swabs Neonatal eye swabs Chlamydia PCR: Early morning urine Carbapenemase PCR CSF CSF for microscopy, culture, virology, PCR or AFB Sterile white topped universal bottle Packs available from Lab. AFB provisional smears – 24 hours. AFB culture: 6-12 weeks. Virology: 1 week PCR: 1 week Microscopy and positive cultures will be telephoned. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 19 of 60 NHS GENERAL Type of Specimen Container/ Volume CSF for CJD (prion) Storage (if necessary) Always urgent Investigation Time Comments Must be discussed with medical microbiologist before taking specimens. Faeces Faeces for culture, parasites, Cryptosporidia or virology Blue screw capped bottle with spoon 4oC overnight Negative :48 hours Positive :72 hours Faeces for Clostridium difficile Toxin testing Blue screw capped bottle with spoon – a ¼ of the bottle must be filled Blue screw capped bottle with spoon Blue screw capped bottle with spoon 4oC overnight 24 hours 4oC overnight 2 - 3 days Tests batched. 4oC overnight 24 hours (winter months) Batched over summer months. Seasonal disease. Faeces for H.pylori Faeces for Norovirus Follow up specimens of asymptomatic patients and contacts of gastro-enteritis NOT required unless requested by the Environmental Health Officer. Test will not be carried out on formed or semi-formed stools. Fluids: Ascitic, synovial and peritoneal fluids Sterile white topped universal bottle Always urgent Pleural fluid Sterile white topped universal bottle Suitable sterile leak-proof container 4oC overnight Transport packet available from laboratory BAL Send as urgent specimen. Culture – 72 hours (+ 24 hours if positive) 72 hours Microscopy results will be telephoned as appropriate. Must be sent urgently Culture 72 hours Provisional AFB film 24 hours PCP 24 hours Inform lab prior to sending and state which tests are required. Room temperatu re 4 weeks for negative culture Microscopy – interim report issued. Fungal Culture: Nails & clippings Skin scrapings Hair 48 hours for Microscopy IUCD Sterile container 4oC 10 days for Actinomyces Not routinely cultured. GC PCR (STI patients only) GC PCR: Endocervical and Urethral swabs Special swabs required, available from laboratory 2 - 27oC for up to 3 days 48 hours Specimens are batched Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 20 of 60 NHS GENERAL Type of Specimen GC PCR: Early morning urine Container/ Volume Sterile white topped universal bottle 15-20ml Storage (if necessary) Refrigerate for 4-6 days 4oC Investigation Time 48 hours Comments Specimens are batched. First voided urine 15-20ml preferred or a wait of one hour since last voided sample. Helicobacter antigen Test : Faeces Blue screw capped bottle with spoon 4oC overnight 2-3 days Tests batched. Sterile white topped universal bottle 4oC overnight 24 hours for routine specimen Urgent test can be discussed with medical microbiologist. Sterile white topped universal bottle 4oC overnight 24 hours for routine specimen Urgent test can be discussed with medical microbiologist Pus Sterile white topped universal bottle 4oC overnight Microscopy – same day Culture – 3 days This is always preferable to a swab Intra-operative pus Sterile white topped universal bottle Send urgently Culture – 3 days Telephone Laboratory if urgent. Ext 4617 Sputum for culture 60 ml sterile screw capped container 4oC overnight Negative : 48 hours Positive : 72 hours Sputum AFB 60ml sterile screw capped container 4oC overnight Provisional AFB film – 24 hours Culture 6-12 weeks Legionella Urinary antigen test Pneumococcal Urinary antigen test Pus Sputum: If urgent, contact medical microbiologist. Specimen sent to Mycobacterium Reference Laboratory for culture. Swabs Ear Swab Liquid transport swab 4oC overnight Negative : 48 hours Positive : 72 hours Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 21 of 60 NHS GENERAL Type of Specimen Container/ Volume Storage (if necessary) Endocervical and urethral swabs for N.gonorrhoeae Liquid transport swab Preferably same day or 4oC overnight Investigation Time Negative :48 hours Positive : 72 hours Comments Must be a cervical swab taken under direct vision. NB. HVS unsuitable for GC Eye swab for N.gonorrhoeae Liquid transport swab Preferably same day or 4oC overnight Negative :48 hours Positive : 72 hours Eye Swabs (routine culture) Liquid transport swab 4oC overnight Negative :24 hours Positive : 48 hours Eye Swabs for Chlamydia from neonates Special Liquid transport swab available from the laboratory Liquid transport swab 2-27oC for up to 3 days 24-48 hours 4oC overnight Negative :48 hours Positive : 72 hours Urethral and penile swabs for routine culture Liquid transport swab 4oC overnight Negative :48 hours Positive : 72 hours Examined for routine bacteriology including Candida and N.gonorrhoeae MRSA Screening Swabs Liquid transport swab (dual) 4oC overnight Negative : 24 hours Nose and groin swabs only required for screen Pertussis Swabs Special per nasal transport swab available from the laboratory NB. Send as soon as possible Cultured for 7 days Phone laboratory for swabs. Blood test is now available (clotted sample) High vaginal swab Swabs for ? sexual abuse Nasal swab Always urgent Liquid transport swab 4oC overnight Specimens are batched. Neonate eye swabs become positive at about 10 days post-partum. Examined for routine bacteriology including Candida, Trichomonas & Clue cells. Not examined for N.gonorrhoeae Discuss with a Medical Microbiologist Negative : 24hours Positive : 48 hours Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 22 of 60 NHS GENERAL Type of Specimen Container/ Volume Liquid transport swab Storage(if necessary) 4oC overnight Throat Swabs Liquid transport swab 4oC overnight Negative : 24 hours Positive : 48 hours Wound Swabs Liquid transport swab 4oC overnight Negative :48 hours Positive : 72 hours Leg ulcer swab Liquid transport swab 4oC overnight Negative : 48 hours Positive : 72 hours Tips: Line Tips Sterile container Preferably same day or 4oC overnight Negative: 48 hours Positive: 72 hours Sterile Universal Bottle Always urgent Mouth swab Investigation Time Comments Negative : 48 hours Positive : 48 hours Please record persistent or recurrent infection on request form Routine swabbing is unnecessary unless there is indication of infection Tissue: Theatre Tissues Urine (see also section on urine) Urine for routine Red topped culture MSU, CSU universal with boric acid NB: filled to line on label 4 days Telephone if urgent, ext. 4617 Microscopy telephoned to requestor as appropriate. *send to lab ASAP* 4oC overnight Negative ; 24 hours Positive : 48 hours Minimum acceptable volume 5ml. If white topped bottle received, specimen will be rejected. Negative : 24 hours Positive : 48 hours Only to be used when unable to collect more than 5ml. Minimum acceptable volume 1ml Paediatric/ Elderly Medicine Paediatric 5ml urine collection tube with boric acid 4oC overnight Urine for AFB/TB Culture (early morning specimens) Sterile white topped universal bottle (20ml) or red topped universal with boric acid. NB: filled to line on label 4oC overnight Culture 2-12 weeks 3 separate EMU specimens Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 23 of 60 NHS GENERAL Type of Specimen Urine for Chlamydia Urine for Legionella and Strep pneumoniae Urine for pregnancy test Container/ Volume White topped sterile universal container White topped sterile universal containers White topped sterile universal container Storage(if necessary) 4oC for 4-6 days Investigation Time Comments 24–48hr First voided early morning urine 15-20ml. Specimens batched. 4oC overnight 24hrs for routine specimens 4oC overnight 24 hours Minimum 5ml. Urgent tests can be performed. Contact medical microbiologist. Early morning urine preferred. Viral Investigation Culture Skin scrapings for viral immunofluorescence Viral Culture is no longer performed Single well Teflon coated slide, available from the laboratory Electron Microscopy Swabs Special virology Liquid transport swab available from laboratory Swabs for Herpes simplex Special virology Liquid transport swab available from laboratory 2 - 27 oC for up to 3 days 7 days Must discuss with medical microbiologist Discuss with medical Microbiologist This transport medium contains antibiotics – unsuitable for bacterial culture. Swabs used for PCR testing Tests batched. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 24 of 60 NHS GENERAL SEROLOGICAL INVESTIGATIONS NB. Severe haemolysis may compromise the results of serology assays. Fresh blood is best left at room temperature to clot. Do not freeze or overcool any whole blood samples. Type of Investigation Antibiotic Assay Gentamicin Vancomycin Container/ Volume 5-10ml clotted blood (Vancomycin test now referred to FRH, Newcastle) http://intranet/anti biotics/handbook/ default.asp Storage Always send to laboratory before 4.00pm Monday – Friday and before 1pm Saturday and Sunday. Investigation Time Gentamicin 2 hours/result telephoned to medical staff Comments Please telephone laboratory before sending sample. Ext 4689 If out of hours contact Microbiologist on-call. Vancomycin 6 hours/result telephoned to medical staff ASO titre & anti DNase B 5-10ml clotted blood 4oC overnight 1 week Tests batched Bordetella pertussis toxin IgG/IgA 5-10ml clotted blood 4oC overnight 1 week Test batched Borrelia IgM/IgG (Lyme Disease) 5-10ml clotted blood 4oC overnight 24 hours for negative specimen NB. sample must be taken 6 weeks after tick bite Reactive specimens sent to reference lab. Brucella 5-10ml clotted blood 5-10ml clotted blood 4oC overnight 4oC overnight Approximately 1 week 3-4 days Test referred to Ref. Laboratory Avidity testing may be performed dependent upon the IgG/IgM result and CMV IgG, IgM Reference Ranges (where applicable) Please consult antibiotic handbook on the intranet for reference ranges. Contact Consultant Microbiologist if unsure ASO normal range: 0-200 IU/ml ASD normal range (Adult): 0-200 IU/ml ASD normal range (Child): 0-300 IU/ml <40 IU Negative >100 IU Positive in the absence of vaccination. >40 - 100 IU a repeat sample may be required depending upon date of onset. N/A N/A Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 25 of 60 NHS GENERAL Type of Investigation Container/ Volume Enterovirus PCR Epstein Barr virus Erythrovirus B19 (Parvovirus) CSF Flu A&B including swine flu (Adults) Hepatitis A IgG/IgM (HAV) Hepatitis C antibody (HCV) Storage Investigation Time Send urgently 4oC overnight 4oC overnight 24 hours Special virology Liquid transport swab available from laboratory 5-10ml clotted blood 4oC overnight 24 hours 4oC overnight 2 days 5-10ml clotted blood 4oC overnight 2 days 5-10ml clotted blood 5-10ml clotted blood patient information Comments 2 days 3-4 days. HCV RNA EDTA Hepatitis B surface Antigen (HBsAg) 5-10ml clotted blood 4oC overnight 2 days Hepatitis B surface Antibody 5-10ml clotted blood 4oC overnight 2 days Hepatitis B core total 5-10ml clotted blood 4oC overnight 3-5 days Reference Ranges (where applicable) N/A Telephone if urgent, ext. 4689. If pregnant please give details of pregnancy, date and nature of contact with erythrovirus infection. N/A N/A Reactive specimens sent to Reference Laboratory for confirmation Referred N/A Reactive specimens sent to Reference Laboratory for confirmation Urgent results if required in about 4 hours during the normal working day N/A N/A <10 IU/ml = Not Detected 10-100 IU/ml = Detected >100 IU/ml = Detected Test batched. Reactive specimens sent to Reference Laboratory for confirmation. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 26 of 60 NHS GENERAL Type of Investigation Container/ Volume Storage Hepatitis B other markers including viral load HIV 5-10ml clotted blood 4oC overnight 7 days 5-10ml clotted blood 4oC overnight 2 days HIV Viral Load EDTA Infant Respiratory Screen Infant Nasorespiratory Pharangeal screen for secretions RSV, Adenovirus, Flu A & B, Paraflu's and Human metapneumo virus Legionella, Pneumococcal antigen Legionella & Sterile 4oC Pneumococcal white overnight antigen, topped in urine universal container Measles - IgG Mumps - IgG Mycoplasma Pneumococcal and Haemophilus (HIB), antibody test 5-10ml clotted blood 5-10ml clotted blood 5-10ml clotted blood 4oC overnight 5-10ml clotted blood 4oC overnight 4oC overnight 4oC overnight Investigation Time Comments Sent to Reference Laboratory Urgent testing can be arranged Reactive specimens sent for confirmation. Urgent results in about 4 hours during the normal working day. Always obtain informed consent and indicate on form Referred Reference Ranges (where applicable) N/A N/A N/A Same day Specimens before 3.00pm.RSV screen performed first, then if negative immunofluorescence test for full screen N/A 24 hours for routine specimens Urgent tests can be performed, discuss with Medical Microbiologist Minimum 5ml required N/A 24 hours for routine specimens 24 hours for routine specimens Tests batched 1 week Up to 14 days N/A N/A Telephone 4689 if results required earlier Titres of 1:40 or greater = IgM test performed Any concerns please contact Consultant Microbiologist Pneumococcal antibody protective level: >35 mg/L HIB antibody Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 27 of 60 NHS GENERAL Type of Investigation Pregnancy Test on EMU Procalcitonin (PCT) Quantiferon Gold Rubella Rubella IgG Rubella IgM Semen Semen for vasectomy Semen for infertility investigation Container / Volume Sterile white topped universal 5-10ml clotted blood Specific blood collection tubes available from Lab. Storage Investigation Time Comments 4oC overnight 24 hours Tested routinely at 25 IU/Litre HCG 4oC overnight 24 hours Test performed Monday – Sunday 8am – 5pm. MUST be authorised by Consultant Microbiologist Notify laboratory when sending. Monday to Thursday only. See instruction in main text. Quantiferon protective level: >1.5 mg/L Reference Ranges (where applicable) >=25 IU/L = Positive <25 IU/L = Negative Please refer to the following link for interpretation and guidence. http://intranet/a ntibiotics/handb ook/Z%20(5).% 20PCT%20Algo rithm.pdf N/A Must be received by Lab. before 4:00pm Monday to Thursday only up to 14 days 5-10ml clotted Blood 4oC overnight 48 hours 5-10ml clotted blood 4oC overnight 60ml screw capped container that has been toxicity tested 60ml screw capped container that has Send to laboratory ASAP before 4pm 24h Monday to Thursday only N/A Send to laboratory ASAP before 4pm 24h Monday to Thursday only >20x109/L = Fertile range 10-20x109/L = Subfertile range Sent to Reference Laboratory <10 IU/ml = Not Detected >10 IU/ml = Detected N/A Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 28 of 60 NHS GENERAL been toxicity tested Type of Investigation Container/ Volume Storage Investigation Time Comments Syphilis serology, Treponema 5-10ml clotted blood 4oC overnight 48 hours Reactive specimens referred to Reference Laboratory Toxoplasma 5-10 ml clotted blood 4oC overnight 48 hours Positives sent to Reference Laboratory Virology Screen 5-10ml clotted blood 4oC overnight 2 weeks Needs to be authorised by Consultant Microbiologist. Acute and convalescent specimens required. These are sent to Reference Laboratory. Convalescent specimen 10 to 14 days post onset of illness VzV IgG 5-10ml clotted blood 4oC overnight VZV IgM 5-10ml clotted blood 4oC overnight 7-10 days Referred to reference laboratory VZV PCR Special virology Liquid transport 4oC overnight 7-10 days Referred to reference laboratory 24h Telephone if urgent ext. 4689. If pregnant please give details of pregnancy, date and nature of contact with VZV infection <10x109/L = Infertile range >=4% normal morphology = normal result <4% normal morphology = abnormal result Reference Ranges (where applicable) N/A N/A N/A Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 29 of 60 NHS GENERAL Widal swab available from laboratory Test no longer performed Please contact Medical Microbiologist N/A Malaria Testing Blood Film: Test performed by Haematology department. Screening for Malarial Parasites requires EDTA Purple top tube, for further information please refer to the Haematology handbook. Malarial Antibody Test: Tests performed by Haematology department. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 30 of 60 NHS GENERAL Clinical Scenarios and Laboratory Requirements CONDITION or SPECIMEN TYPE CLINICAL INFORMATION REQUIRED Clinical presentation Time and date of onset of symptoms. Meningitis/ Encephalitis Details of any recent foreign travel. Presence of rash, respiratory signs, conjunctivitis, head injuries, operations etc. Recent antibiotic treatment. APPROPRIATE SPECIMENS CSF (if more than one bottle please label sequentially) Try to obtain at least 1ml. Keep 1 bottle separate for PCR Blood culture: add 7-10ml of blood to each bottle. Paediatric bottles are available for small volumes of blood. CONTAINERS Sterile universal container Blood culture bottles available from the lab. EDTA blood for PCR including viral PCR TURNAROUND TIMES Microscopy - report telephoned Culture result 24 – 72 hours. Positive result telephoned. Incubation continued for 5 days. Referred test. Result normally telephoned within 48 hours. 5ml blood from adult 1ml blood from child Clinical presentation Time and date of onset of symptoms Details of any recent foreign travel Septicaemia Presence of rash, respiratory signs, conjunctivitis, head injuries, operations etc. Any recent infections which may be the source of the illness Blood culture: add 7-10ml of blood to each bottle. Paediatric bottles are available for small volumes of blood. Consecutive blood cultures (at least 30 minutes between) should be taken if SBE suspected Blood culture bottles available from the lab Positive result telephoned. Incubation continued for 5 days. Recent antibiotic treatment Clinical presentation Time and date of onset of symptoms Details of any recent foreign travel Meningococcal sepsis Presence of rash, respiratory signs, conjunctivitis; head injuries; operations etc. Any recent infections which may be the source of the illness Blood culture: add 7-10ml of blood to each bottle Paediatric bottles are available for small volumes of blood. EDTA for PCR 5ml blood from adult 1ml blood for child Blood culture bottles available from the lab Positive result telephoned. Incubation continued for 5 days Referred test. Result normally telephone within 48 hours Recent antibiotic treatment Vaccination history Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 31 of 60 NHS GENERAL CONDITION or SPECIMEN TYPE CLINICAL INFORMATION REQUIRED APPROPRIATE SPECIMENS CONTAINERS TURNAROUND TIMES ENT and eye infections Clinical presentation State if recurrent infection Sore throat Date of onset Liquid transport swab Throat swab Details of recent foreign travel Special virology Liquid transport swab available from laboratory if virus suspected 48 hours Recent antibiotic therapy Clinical presentation Date of onset Otitis media Details of recent foreign travel Ear swab Liquid transport swab 48-72 hours Recent antibiotic therapy Liquid transport swab Clinical presentation Conjunctivitis Date of onset Eye swab Recent antibiotic therapy Use Chlamydia collection kit if chlamydia suspected Bacteriology 48 hours Chlamydia 3-4 days Virology 3-4 days. Swab in viral transport media if virus suspected Clinical presentation Date of onset Epiglotitis Recent antibiotic therapy Neonatal infections Blood cultures **DO NOT attempt a throat swab as this could compromise the airways** As for septicaemia As for septicaemia Per nasal swab 7 days Ensure rapid transport to the laboratory Contact Medical Microbiologist at laboratory for advice Vaccination history (Hib) Vaccination history Pertussis Date of onset Severity Per nasal swab Always contact laboratory before taking swab Blood specimen Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 32 of 60 NHS GENERAL CONDITION or SPECIMEN TYPE CLINICAL INFORMATION REQUIRED APPROPRIATE SPECIMENS CONTAINERS TURNAROUND TIMES Lower respiratory tract disease Sputum – fresh sample 60ml sterile screw capped container Bronchial washings 72 hours Endotracheal secretions Clinical presentation Nasopharyngeal aspirate Date of onset Lobar pneumonia Atypical pneumonia Acute exacerbations of chronic bronchitis Bronchiectasis Recent antibiotic therapy Underlying disease: COAD, emphysema, cystic fibrosis, cancer Aspiration (anaerobes suspected) Whether immunosuppressed Details of recent foreign travel Blood culture (especially lobar pneumonia) If blood culture, as for septicaemia Severe acute community acquired pneumonia – urinary antigen testing available for pneumococci White topped universal If Legionella spp suspected, sputum for culture or urine for antigen detection of Legionella pneumophilla sero group 1 (contact laboratory for advice) 60ml sterile screw capped container or white top universal for urine For Mycoplasma/ chlamydiae – please discuss with a Microbiologist Clotted blood sample Positive result telephoned. Incubation continued for 5 days Normally same day Contact laboratory before sending Contact laboratory before sending 10-14 days for Legionella culture Normally same day for antigen testing 1-2 weeks for atypical pneumonia Minimum 5ml Suspected TB Pulmonary Relevant history including any previous isolation, contacts etc. 3 independent sputum samples for pulmonary TB 60ml sterile screw cap container Film normally 24 hours Urine, pus, CSF, biopsy etc. for non-pulmonary TB Non-pulmonary Relevant history including any previous isolation, contacts etc. If sending blood, contact laboratory for advice first Rapid PCR testing available for some specimens. Contact laboratory for advice Sterile containers EDTA bottle for blood Culture 10 weeks Less with rapid culture. Referred test. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 33 of 60 NHS GENERAL CONDITION or SPECIMEN TYPE CLINICAL INFORMATION REQUIRED APPROPRIATE SPECIMENS CONTAINERS TURNAROUND TIMES Type of wound e.g. post-operative/trauma Wound: Wound infection/abscess Give specific description of anatomic site Clinical history including occupation if relevant to wound Wound: Pressure sore/ulcer Give specific description of anatomical site Swabs are of little value Send biopsy of aspirate of base Skin lesions: Suspected fungal infection Skin lesions: Bacterial e.g. burns and superficial injuries Pus Sterile universal (for pus) Send a swab only if aspirated pus is unavailable Liquid transport swab Biopsy or aspirate If swab is taken, ensure the edge of ulcer is sampled or debride wound and swab base Date of onset Distribution Skin scraping from edge of lesion Type of rash, site 48-72 hours Biopsy or aspirate in sterile container Liquid transport swab In folded black paper inside a labelled envelope Dermapaks are available from the laboratory 48-72 hours Microscopy 1-5 days Culture 4 weeks Give specific description of anatomical site Swab Date of onset Liquid transport swab 48-72 hours Blister fluid Distribution Type of wound Skin lesions: Fish tank granuloma or tropical ulcers Give specific description of anatomical site Contact microbiologist Date of onset Biopsy Distribution Swab is NOT appropriate Variable depending on culture required Biopsy or aspirate in sterile container Some tests are referred to other laboratories Foreign travel Relevant clinical history MRSA Screens Previous MRSA Recent antibiotic therapy Nose and groin swabs Specific lesions if appropriate (e.g. ulcers and surgical wounds) Liquid transport swab 24hours if negative Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 34 of 60 NHS GENERAL CONDITION or SPECIMEN TYPE CLINICAL INFORMATION REQUIRED APPROPRIATE SPECIMENS CONTAINERS Sterile universal Aspiration or biopsy. Bone and joint infections Site, date of onset; presence of prosthesis; other pathology e.g. rheumatoid arthritis, osteomyelitis Blood cultures (see as for septicaemia) Clotted blood for antistaphylococcal antibodies by arrangement Biopsies in saline NOT formalin For blood cultures (see as for septicaemia) Clotted blood TURNAROUND TIMES 48-72 hours 5 day anaerobic culture For blood culture (see as for septicaemia) Referred test Urinary Tract Infection Specimen type Relevant clinical information Any antibiotic therapy within the last 2 weeks Suspected TB Relevant clinical information Mid-stream specimen Suprapubic aspirate Early morning specimen x3 Boric acid container (red top) Instruct patient on correct sample collection Universal white top container Boric acid container (red top) 24-48 hours Culture up to 12 weeks Why TB suspected Age, date, time of onset, visits abroad, affected family/friends Diarrhoea and vomiting 48-72 hours Faeces Antibiotic therapy prior to onset Vomit is NOT an appropriate sample Blue screw capped bottle with spoon Clostridium difficile toxin result available within 24 hours Blue screw capped bottle with spoon 3-4 days Nature of food consumed if food poisoning suspected Helicobacter Faecal Antigen Test Relevant clinical information Faeces Vaginal discharge HVS for Trichomonas vaginalis and Candida spp. Also other bacterial infection if appropriate. Vaginal discharge Suspected STD Pelvic inflammatory disease Full clinical history Serological screening for syphilis may also be advisable Urethral & endocervical swabs for Neisseria gonorrhoea Rectal & throat swabs may be indicated by history Liquid transport swab 72 hours For chlamydia use a chlamydia collection kit Please always label swabs with the specific site Urethral & endocervical swabs for chlamydia Urine for chlamydia White topped universal Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 35 of 60 NHS GENERAL CONDITION or SPECIMEN TYPE CLINICAL INFORMATION REQUIRED HVS for Trichomonas vaginalis and Candida spp. Also other bacterial infection Post-operative infection Post natal APPROPRIATE SPECIMENS Full clinical history Urethral & endocervical swabs for Neisseria gonorrhoea if indicated Urethral & endocervical swabs for Chlamydia Ante natal Urine for chlamydia CONTAINERS TURNAROUND TIMES Liquid transport swab For Chlamydia use a chlamydia collection kit Please always label swabs with the specific site 72 hours White topped universal for chlamydia Full clinical history Pre-puberty If medico-legal implications suspected, please contact the Medical Microbiologist before taking samples LVS Vulval swab Liquid transport swab Please always label swabs with the specific site 72 hours RESULTS OF INVESTIGATIONS Currently the laboratory sends results out in a hardcopy and electronic format. Please note many of our users have now switched off hardcopy reports. If you would like to switch off hard copy reports please contact the laboratory to discuss further. Some preliminary results are also delivered electronically as soon as they are available. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 36 of 60 NHS GENERAL TESTS REFERRED BY MICROBIOLOGY TO OTHER LABORATORIES Some investigations are not performed at North Tyneside General Hospital Microbiology laboratory but are referred to a network of specialist laboratories in the UK. The list of laboratories is extensive and is listed as an appendix at the end of this document (Appendix 1). Please contact the Microbiology laboratory if you require further details regarding the referral laboratory so that you can be directed to the relevant person or department. Tests referred to Newcastle Hospitals including HPA, Freeman and RVI Request Adenovirus PCR Cryptococcal antigen CMV PCR IgM Epstein-Barr Virus PCR Hepatitis B confirmation Hepatitis B viral load Hepatitis B core/markers Hepatitis B e antigen/antibody Hepatitis C confirmation Hepatitis C PCR Herpes IgG, IgM Herpes PCR HIV confirmation HIV Viral Load Legionella antibody Mumps IgM antibody Mumps PCR Quantiferon gold Rubella IgM Swine flu Syphilis confirmation Syphilis antibody (CSF) TORCH screen Vancomycin Varicella IgG Varicella IgM Comments EDTA sample CSF sample or clotted blood sample EDTA sample or urine from child EDTA sample Not Occupational Health EDTA Not routinely tested EDTA blood sample or CSF EDTA blood sample must be received by the HPA within 2 days of venesection Only in outbreak situations Refer to Consultant Microbiologist Specific blood collection packs to be received at lab by 16:00 on the same day Monday Thursday only ITU patients Serum sample preferred Refer to Consultant Microbiologist Includes Parvovirus Serum sample Confirmation of an equivocal result Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 37 of 60 NHS GENERAL Tests referred to Immunology Gateshead Request Acetyl Choline Receptor antibody Adrenal antibody ANCA (pANCA / cANCA / MPO/PR3) AP100 Autoantibodies CCP CH100 Cardiac Muscle antibody Coeliac Endomysial antibodies Epidermal antibody (Pemphigus / Pemphigoid) GAD antibody Ganglioside antibody Gastric parietal cell GBM (glomerlular basement membrane) Insulin antibody Islet Cell antibody Liver Cytosol antibody M2 Mitochondrial antibody Manin binding lectin MNDA MUSK Neuronal Nuclear antibody Ovarian antibody Pituitary Gland antibody Purkinge Cell antibody RAST Rheumatoid factor Soluble Liver antigen antibody Striated Muscle antibody Tetanus Comments Acetyl Choline Receptor antibody Immunology at Gateshead must receive the sample within 4 hours of venesection Immunology at Gateshead must receive the sample within 4 hours of venesection Haematology tests if patient has low B12 Urgent if pulmonary bleeding/haemorrhage, Goodpasteurs syndrome Test performed by Clinical Chemistry Only if infection or possible infection and requires status or if specimen from child Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 38 of 60 NHS GENERAL Tests referred to laboratories other than Newcastle and Gateshead Request Adenovirus CFT Amoebic IFAT serology Anti Staphylococcal antibodies Aspergillus galactomanin Aspergillus precipitins Avian precipitins Bartonella (cat scratch fever) Bilharzia (see Schistosomiasis) Borrelia serology (see Lyme disease) Bordetella pertussis (PCR) Brucella antibodies Campylobacter antibodies Candida manin antibodies Channel antibodies (potassium, calcium) Chlamydia pneumoniae Chlamydia psittaci Chlamydia trachomatis Coccidioides antibody Convalescent sera (single) Convalescent sera (paired) Coxsackie Dengue fever Diphtheria Echinococcus serology/Hydatid E.coli O157 Ethambutol assay Entamoeba histolytica serology Enterovirus IgM serology Enterovirus PCR Farmer’s Lung Giardia H.pylori culture Hepatitis B core antibody Hepatitis B viral load Hepatitis D Hepatitis E HUS - Haemolytic uraemic syndrome Histoplasmosis antibody Comments Referred for confirmation Per nasal swab or NPA <12 months old for PCR Not routinely performed. 10 – 14 days after onset of symptoms. Discuss with Microbiologist Not routinely performed. Acute sample at onset of illness and convalescent 10-14 days after onset This MUST be authorised by Microbiologist This MUST be authorised by Microbiologist EDTA sample. This MUST be authorised by Microbiologist Stool for PCR when indicated Discuss with medical Microbiologist Referred for confirmation 2 specimens, minimum of 10ml clotted blood taken one week apart. Referred if Hepatitis B surface antigen positive Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 39 of 60 NHS GENERAL HTLV 1 and III Human Papilloma virus (HPV) Hydatid /Echinococcus serology Leishmania IgE Isoniazid assay Itraconazole assay Legionella urinary antigens Leptospiral antibodies LGV Listeria PCR Lyme Disease Malaria antibodies Menigococcal antibody Meningococcal PCR Neisseria meningitis antibodies (paired sera) Orf Parvovirus Pertussis antibodies (see Bordetella) Pneumococcal PCR Pneumococcal serotype specific antibody Polio Pyrazinamide assay Q Fever/Coxiella Rabies Respiratory screen Rifampicin assay Rickettsia Schistosomiasis serology Swine flu Teicoplanin Toxocara antibodies Toxoplasma confirmation Typhoid (Immunoblot) Viral load- Hepatitis B Weils Disease (see Leptospiral antibodies) Widal Virology screen Voriconazole levels Yersinia antibodies Swab for PCR Test performed by Clinical Chemistry Referred for confirmation Referred for confirmation Test performed by Haematology EDTA or CSF Swab for Electron microscopy IGM confirmation by PCR Refer to Consultant Microbiologist Referred for confirmation Discuss with Microbiologist 2 specimens of a minimum of 10 ml clotted blood taken one week apart Test no longer performed see above for typhoid Immunoblot. Acute and Convalescent sera. Discuss with Microbiologist Pre dose only Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 40 of 60 NHS GENERAL INVESTIGATIONS AND GUIDELINES BLOOD CULTURES Guidelines for taking blood cultures are available via the Intranet. They are located in the Infection Control Team – Documents. 1. Once taken, send to laboratory as follows: Place the blood cultures in an air tube pod and send to the laboratory through the air tube system. No other specimens must be sent in the same pod. Ensure they are well packed to prevent leakage or breakages. 2. All positive results will be communicated as soon as they become available. CEREBROSPINAL FLUID (Packs of specimen containers available from Specimen Reception) 1. These samples are classed as urgent therefore it is important to contact the Microbiology laboratory on extension 2528 to inform them that the specimen has been taken. Send the specimen to the laboratory as soon as possible. 2. An immediate cell count and Gram film will be performed and the result telephoned. Cell count will not be reported if the specimen is more than 4 hours old on receipt in the laboratory. For Xanthochromia – refer to Clinical Chemistry handbook. CHLAMYDIA TRACHOMATIS / GC (PCR) COLLECTION KIT FOR ENDOCERVICAL SPECIMENS A single endocervical or urethral swab is sufficient using PCR. NB GC PCR only tested when STI patient Specimen Collection and Transport DO NOT EMPTY THE FLUID OUT OF THE TUBE. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Remove the large cleaning swab from packaging Using cleaning swab, remove excess blood and mucus from the cervical mucosa Discard the used cleaning swab Remove the collection swab from the packaging Insert the collection swab into the cervical canal and rotate for 15-30 sec. Withdraw the swab carefully. Avoid contact with the vaginal mucosa Uncap the CT/GC Diluent tube Fully insert the collection swab into the CT/GC Diluent tube Break the shaft of the swab at the score mark. Use care to avoid splashing of contents Tightly recap the tube Label the tube with patient information and date/time collected Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 41 of 60 NHS GENERAL 12. Transport to the laboratory Swab Storage and Transport The CT/GC Diluent tube with swab must be stored and transported to the laboratory and/or test site at 2 – 27oC within 4-6 days of collection. CHLAMYDIA TRACHOMATIS / GC (PCR) COLLECTION KIT FOR MALE URETHRAL SPECIMENS NB GC PCR only tested when STI patient Specimen Collection and Transport DO NOT EMPTY THE FLUID OUT OF THE TUBE. 1. 2. 3. 4. 5. 6. 7. 8. 9. Remove the swab from packaging Insert the swab 2 – 4 cm into the urethra and rotate for 3-5 sec. Withdraw the swab Uncap the CT/GC Diluent tube Fully insert the swab into the CT/GC Diluent tube Break the shaft of the swab at the score mark. Use care to avoid splashing of contents Tightly recap the tube Label the tube with patient information and date/time collected Transport to laboratory Swab Storage and Transport The CT/GC Diluent tube with swab must be stored and transported to the laboratory and/or test site at 2 – 27oC within 4-6 days of collection. URINE FOR CHLAMYDIA TRACHOMATIS / GC PCR TEST NB GC PCR only tested when STI patient Early morning first void urine is preferred. If this is not available, it is recommended that the sample is taken one hour from the last voided urine. 15 – 20ml of urine in a sterile universal container is required. This can be stored at room temperature for 30 hours or at 4-8oC for 4-6 days. FAECAL SPECIMENS 1. Ask patient to pass stool into a clean dry container such as a bedpan or pot. Use the screw capped universal with spoon to collect a sample of faeces. Do not contaminate the outside of the container and ensure that the cap is securely screwed down. It is not necessary to fill the container, but please fill at least ¼ to half of the container. 2. Provide as much information as possible, e.g. date of onset of symptoms, travel history and any antibiotic therapy. This determines the way in which the specimen is processed in the laboratory. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 42 of 60 NHS GENERAL 3. If Ova, cysts & parasites are required this test should be requested on ICE. Please discuss investigations for trophozoites with the Microbiologist. 4. Clearance specimens are not indicated, unless requested by an Environmental Health Officer. 5. Rectal swabs are not indicated for the diagnosis of gastro-intestinal infections. FUNGAL INVESTIGATION 1. Skin: the skin should be taken free of ointments or other applications. Scrapings should be taken with the blunt edge of a sterile scalpel or similar from the periphery of any lesion. The tops of any vesicles should be snipped off. Nails: these should be clipped off using nail clippers and any material underneath the nail also obtained. Hairs: these should be pulled out to include the root. The scalp can be brushed to obtain scales. 2. Any of the above should be placed in the special transport packets provided by the laboratory and kept dry at room temperature. 3. Mucosal surfaces should be sampled with the standard cotton-wool swab and transport medium. 4. Sputum and body fluids should be placed in sterile universal containers. GENTAMICIN ASSAYS See Antibiotic Handbook http://intranet/antibiotics/handbook/default.asp Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 43 of 60 NHS GENERAL INVESTIGATION FOR PERTUSSIS Swabs Method for taking sample for pertussis culture: 1. Ask an assistant to sit the child on her lap and hold the head firmly. 2. Use a special per nasal swab available from your local pathology specimen reception. DO NOT USE AN ORDINARY COTTON WOOL SWAB 3. Insert the swab gently into the nose and guide it along the floor of the nasal cavity beneath the inferior nasal concha until a resistance is felt due to the swab impinging on the posterior wall of the pharynx. This causes an unpleasant but not painful sensation. 4. Remove the swab and place it into transport medium. Laboratory diagnosis of Bordetella pertussis infection Culture Culture in the first 5 weeks of untreated illness. Preferably with flexible per-nasal swab (available from the lab.) or otherwise with throat swab which is less sensitive. Sensitivity of per nasal swab culture is 50%. The lab needs to know to culture for Bordetella pertussis so this needs to be highlighted on the form. Even if the child has had antibiotic treatment, it may be worth sending a swab for culture in the first 3 weeks of the illness. Anti-pertussis toxin IgG antibody levels by EIA Paired sera with the second specimen taken >2 weeks after onset of cough, or single sera taken >2 weeks after onset of cough. PCR A PCR service for diagnosis is available for children aged less than 12 month admitted to the paediatric ward with a respiratory illness compatible with pertussis. This is performed on either a Nasopharyngeal aspirate or a per nasal swab. The specimen must be less than 72 hours old on arrival at the reference laboratory. PREGNANCY TEST The standard test detects a level of 25 IU HCG/L. If menstruation has not started within one week of a negative result, then the test should be repeated. The test uses a monoclonal antibody and is highly specific for human chorionic gonadotrophin. 1. Early morning urine is preferred and should not be obviously blood stained or turbid. 2. Specimens must be sent in a white topped sterile universal container and not in a home produced container. The link to the following DH website ‘Pregnancy Testing Top Tips’ might be useful http://www.mhra.gov.uk/Publications/Postersandleaflets/CON014278 Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 44 of 60 NHS GENERAL QUANTIFERON GOLD Bloods can only be accepted at the laboratory Monday – Thursday before 4pm Blood collection packs Available as single packs from: Microbiology department North Tyneside Pathology specimen reception Wansbeck Pathology specimen reception Hexham Procedure for Nursing/Clinical Staff 1. Ensure all 3 tubes are in date. 2. Fill each tube with exactly 1ml of blood (Red, Grey and Purple). All three must be filled or the test cannot proceed. 3. Shake tube vigorously (until the blood foams) – lack of shaking may result in false negative results. 4. Ensure all tubes and request forms are labelled with patient information and provide all relevant clinical information. 5. It is important to ensure that the date the blood was drawn is clearly marked on the request form. Failure to do this may result in the sample being rejected by the reference laboratory. 6. Notify the Microbiology laboratory at North Tyneside on extension 4689 that you are sending the pack & you will be advised on how to transport the sample to the laboratory. 7. Return the packs urgently to the microbiology department NTGH to arrive no later than 4pm. Failure to do this may result in the sample being rejected by the reference laboratory. These tests are forwarded on to the Regional Centre for Mycobacteria in Newcastle. The tests are batched with an average turnaround time of up to 2 weeks. This may change with increasing demand; however it is important to understand that single tests will not be carried out on an ‘urgent’ basis. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 45 of 60 NHS GENERAL SEMINAL FLUID A. Post vasectomy Introduction After their operation a patient may resume having sexual intercourse as soon as they feel able. Contraception must be used until the doctor who performed the vasectomy operation informs the patient that the post-vasectomy semen samples are clear. The referring doctor will be notified of the results. If there are still sperm in the specimens, the doctor will re-refer the patient, if, necessary, for further post-vasectomy checks until two consecutive specimens are free from sperm. These instructions are based on the British Andrology Society Guidelines 2002. When to bring the first specimen The first specimen should be passed at least 16 weeks after the operation and after producing at least 24 ejaculates. When to bring the second specimen The second semen specimen should be passed and brought in two weeks later. Delivery of your sample A fresh sample is essential for this test and the sample must be received by the laboratory within four hours of it being passed. The sample must be brought to the Pathology Specimen Reception at North Tyneside General Hospital between 8.30am and 4:30pm, Monday to Friday. Instructions for collecting the semen sample The patient should abstain from intercourse or masturbation for 2 to 7 days prior to providing the specimen The sample must be obtained by masturbation (manual stimulation) and ejaculated into a clean wide mouthed container made of plastic that has been toxicity tested. A condom or artificial lubrication must not be used for semen collection as it will kill the sperm. The complete specimen is needed for this examination, so if any of the specimen is spilt the laboratory must be notified as a repeat specimen is required. The specimen container must be labelled with the patients’ full name, date of birth and the date and time the specimen was taken. Please include name of surgeon on the request form. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 46 of 60 NHS GENERAL Information for Patients – Vasectomy Semen Analysis Introduction After your operation you may resume having sexual intercourse as soon as you feel able. Use contraception until the doctor who performed your vasectomy operation informs you that the post-vasectomy semen samples are clear. Your referring doctor will be notified with the results. If there are still sperm in the specimens, your doctor will re-refer you, if, necessary, for further postvasectomy checks until two consecutive specimens are free from sperm. These instructions are based on the British Andrology Society Guidelines 2002. When to bring the first specimen The first specimen should be passed at least 16 weeks after your operation and after producing at least 24 ejaculates. When to bring the second specimen The second semen specimen should be passed and brought in two weeks later. Delivery of your sample A fresh sample is essential for this test and the sample must be received by the laboratory within four hours of it being passed. The sample must be brought to the Pathology Specimen Reception at North Tyneside General Hospital between 8.30am and 4:30pm, Monday to Friday. Instructions for collecting the semen sample You should abstain from intercourse or masturbation for 2 to 7 days prior to providing the specimen The sample must be obtained by masturbation (manual stimulation) and ejaculated into a clean wide mouthed container made of plastic that has been toxicity tested. A condom or artificial lubrication must not be used for semen collection as it will kill the sperm. The complete specimen is needed for this examination, so if any of your specimen is spilt you must tell us, as a repeat specimen is required. Label the specimen container with your full name, date of birth and the date and time the specimen was taken. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 47 of 60 NHS GENERAL B. For investigation of infertility (Screening Test Only) Delivery of the sample A fresh sample is essential for this test, and the sample must be brought to the Pathology Specimen Reception at North Tyneside General Hospital preferably within one hour of collection. The sample must be brought to the laboratory between 8.30am and 4:30pm, Monday to Friday. Instructions for collecting the semen sample. The sample should be collected after a minimum of 2 days and a maximum of 7 days of sexual abstinence. If additional samples are required the number of days of sexual abstinence should be constant as possible. The sample must be obtained by masturbation (manual stimulation) and ejaculated into a clean wide mouthed container made of plastic that has been toxicity tested. A condom or artificial lubrication must not be used for semen collection as it will kill the sperm. The complete specimen is needed for this examination, so if any of your specimen is spilt the laboratory must be notified, as a repeat specimen is required. The specimen container must be labelled with the patients’ full name, date of birth and the date and time the specimen was taken. Factors That May Affect Results The following are important considerations when submitting samples for bacteriological investigation: Delay in transport: Semen samples should be delivered to the laboratory as soon as possible after production. Any delay will result in loss in viability of the sperm. Temperature: To maintain viability of sperm, samples should be kept as near to body temperature as possible. At this temperature contaminating bacteria will rapidly overgrow and the quality of the sample will significantly deteriorate hence it must be transported to the laboratory as quickly as possible. Inappropriate specimen, site or Samples should not be collected into a transport medium: condom as these may contain a spermicide. The sample should be collected into a sterile laboratory specified container that has been toxicity tested with no additives. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 48 of 60 NHS GENERAL Information for Patients – Infertility Semen Analysis Introduction As a routine part of infertility investigation, you have been asked to provide a semen sample for assessment of sperm number and quality. Delivery of your sample A fresh sample is essential for this test, and the sample must be brought to the Pathology Specimen Reception at North Tyneside General Hospital preferably within one hour of collection. The sample must be brought to the laboratory between 8.30am and 4:30pm, Monday to Friday. Instructions for collecting the semen sample. The sample should be collected after a minimum of 2 days and a maximum of 7 days of sexual abstinence. If additional samples are required the number of days of sexual abstinence should be constant as possible. The sample must be obtained by masturbation (manual stimulation) and ejaculated into a clean wide mouthed container made of plastic that has been toxicity tested. A condom or artificial lubrication must not be used for semen collection as it will kill the sperm. The complete specimen is needed for this examination, so if any of your specimen is spilt you must tell us, as a repeat specimen is required. Label the specimen container with your full name, date of birth and the date and time the specimen was taken. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 49 of 60 NHS GENERAL SPUTUM It is important that sputum is collected properly so as to avoid contamination with mouth flora and that it is transported to the laboratory promptly as sputum provides excellent conditions for bacterial growth. Genuine sputum must be obtained which should be purulent or at least show purulent flecks in order to yield any useful information. Therefore, saliva or mucoid sputum will not normally be cultured. Please provide relevant clinical details e.g. immunocompromised patient, bronchiectasis, recent antibiotic therapy, so that culture results can be interpreted appropriately. Sputum should be collected as follows: 1. Encourage the patient to expectorate genuine sputum. It may be necessary to employ some form of postural drainage with the help of a physiotherapist. 2. All specimens should be sent in 60ml containers which should be securely closed. 3. If a delay is anticipated the specimen may be refrigerated at 4oC although this is not ideal. 4. Specimens from patients with endotracheal tubes and tracheotomies should be obtained with a sterile suction catheter and mucus extractor. 5. For investigation of tuberculosis, three specimens, taken at different times, should be collected. In cases where the patients cannot produce any sputum bronchial lavage or fasting gastric juice should be provided. Please inform the laboratory if there is to be any deviation from the above protocol. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 50 of 60 NHS GENERAL THREADWORM Adult Enterobius vermicularis (threadworm or pinworm) inhabit the large intestine and rectum but eggs are not normally found in the faeces as the adult female migrates out of the anal opening to deposit her eggs on perianal skin. 1. Sampling should be done first thing in the morning before bathing or showering. 2. A moist swab should be used to sample skin round the anus. This is placed in a sterile Universal container containing a few drops of saline. THROAT SWABS Throat swabs are routinely examined only for beta-haemolytic streptococci. If abscess, quinsy, meningococcal, gonococcal, epiglottitis or diphtherial infection is suspected please indicate in the Clinical Details on the request form. 1. Use a tongue depressor and a good light source. 2. Rotate the swab firmly over the tonsillar area and posterior pharynx if this is clinically inflamed. Avoid the tongue and uvula. 3. Place the swab in the tube of transport medium. URETHRAL SWABS Specimens for the diagnosis of STIs are best collected at a GU clinic. In females, cervical swabs should be collected at the same time. Males 1. No urine should be passed for 1-2 hours before swabbing. 2. The area around the external urethral meatus should be cleansed with sterile saline 3. The specimen is collected by rotating the swab gently in the urethral canal. 4. If a specimen for Chlamydia infection is to be taken, a special swab is required from the Microbiology Department. Instructions are contained in the kit. Females 1. The patient should not douche or apply other treatment for 12 hours previous nor pass urine for 1-2 hours prior to swabbing. 2. The external genitalia and urethral meatus should be cleansed with sterile saline. 3. The urethra is compressed against the pubis with a gloved finger in the vagina and the finger is drawn downwards to express an exudate while swabbing. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 51 of 60 NHS GENERAL URINE FOR CULTURE Normal urine is a sterile fluid but is easily contaminated with microorganisms during voiding. It acts as a culture medium and large numbers of contaminating bacteria can grow if there is any delay in transport. For this reason containers using boric acid preservative are used. Red topped universals are used for adult urines and paediatric containers are used for babies and where only small samples can be obtained. The containers must be filled to the indicator line for optimum results. The specimens must be sent to the Microbiology Department as soon as possible. All urines are processed by flow cytometry and those with bacteria and/or increased leucocytes are selected for culture and sensitivity. Most negative results are reported on the same day as receipt of the specimen. Positives will be reported within 2-3 days. URINE CULTURE & MICROSCOPY REFERENCE RANGES Culture: 0 organisms/ml = No Growth 1 – 10,000 organisms/ml = No significant growth 10,000 – 100,000 organisms/ml = No significant growth or Doubtful positive result when certain clinical information or criteria are met >100,000 organisms/ ml = Positive result When the culture yields three or more different organism types = Mixed growth Microscopy: <40WBC/mm3 AND <1,000 bacterial cells = Culture NOT performed Culture is performed when EITHER one or both values exceed these parameters (i.e. >40WBC and/or >1,000 bacterial cells). N.B. Culture is routinely performed on paediatric patients, antenatal patients, immunocompromised and Urology patients Collection In males the prepuce should be retracted. In females the labia should be separated and the vulva cleansed with sterile saline and dried with gauze. If vaginal secretions are likely to contaminate the specimen as occurs commonly in pregnancy, a vaginal tampon may be inserted. The labia should be separated while the specimen is passed. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 52 of 60 NHS GENERAL VAGINAL AND CERVICAL SWABS The “HVS” is only really a suitable specimen for the diagnosis of Candida infection, non-specific vaginitis and Trichomonas. Other organisms such as streptococci and anaerobes are cultured for but are often of doubtful significance. Group B streptococci are normal flora in women of childbearing age. A cervical swab obtained under direct vision is essential for the diagnosis of chlamydia and Gonococcal infections. It is essential to state the reason why the swab has been taken. 1. Wear gloves 2. Exclude the use of any cream lubricant or medication. 3. For an HVS the swab should be inserted into the vaginal fornices. 4. The swab should be placed in transport medium. 5. Endocervical/Urethral specimens for Chlamydia testing by PCR are taken using a special swab obtained from Microbiology. VANCOMYCIN ASSAYS See Antibiotic Handbook http://intranet/antibiotics/handbook/default.asp VIROLOGY Swabs for PCR: Dedicated swabs (which contain antibiotics) are available from the Microbiology laboratory. Tissues and Fluids: Send in sterile universal container. Skin scrapings for Immunofluorescence: special single well slide from lab. Must contact Medical Microbiologist Faeces: Send in sterile universal container with spoon. PCR: Discuss with laboratory. Viral culture is no longer performed. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 53 of 60 NHS GENERAL WOUND SWABS Swabs should only be taken when indicated i.e. wound looks infected. It is essential to state the exact nature of the wound, site, antibiotic therapy and whether postoperative. Avoid the use of local antibiotics. 1. It is often best to clean a wound with sterile saline before taking the swab. Superficial serous exudates are often colonised by saprophytic Gram negative organisms of no pathogenic significance. 2. Take the swab by rotating it in the deepest regions of the wound. 3. For eye swabs, wipe away any superficial exudates and swab under the conjunctivae. 4. For ear swabs, remove any crust or exudates before taking the swab Do not repeat unnecessarily. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 54 of 60 NHS GENERAL APPENDIX 1 – REFERENCE LABORATORIES The following is a list of all the reference laboratories to which the Microbiology Department of North Tyneside General Hospital refer work. Included with each is a list of tests that may be referred to that laboratory. Anaerobe Reference Laboratory (ARL) NPHS Microbiology Cardiff University Hospital of Wales Heath Park Cardiff CF14 4XW Tel: 0292074 2171(Lab) or 2378 (Office) Antimicrobial Assay Service Dept of Medical Microbiology North Bristol NHS trust South Mead Hospital Bristol BS10 5NB Tel: 01173235658 The Antibiotic Resistance Monitoring & Reference Laboratory (ARMRL) HPA Centre for Infections Colindale London NW9 5EQ Tel: +44 (0)20 8327 6511 Fax: +44 (0)20 8327 6264 Email: armrl@hpa.org.uk Aspergillus precipitins Cumberland Infirmary, Newton road Carlisle, Cumbria CA2 7HY Tel. 01228 23654 Brucella Reference Unit (BRU) Liverpool Clinical Laboratories Virology Reception, Ground Floor Royal Liverpool & Broadgreen University Hospital NHS Trust Duncan Building, Prescot Street L7 8XP Tel. 0151 7064410 Campylobacter antibodies Preston Microbiology Laboratory Royal Preston Hospital Sharoe Green Lane North Fulwood, Preston Lancashire PR2 9HT Anaerobes (particularly Clostridium difficile), Actinomyces sp., metronidazole resistance in anaerobes Various antibiotic assays All aspects of antibiotic resistance, in particular confirmation and molecular investigation of new or unusual resistance Aspergillus precipitins, Avian precipitins, Chlamydia sp, Farmer’s Lung. Candida. Brucella Campylobacter antibodies (see also Laboratory of Gastrointestinal Pathogens) Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 55 of 60 NHS GENERAL Tel: 01772 716 565 Cryptosporidium Reference Unit (CRU) Singleton Hospital Sketty Swansea SA2 8QA Cryptosporidia, Giardia Immunofluorescence Tel: +44(0) 1792 285341 Clostridium difficile Ribotyping Network (CDRN) Department of Microbiology Freeman Road Hospital Freeman Road High Heaton NE7 7DN Tel: 0191 2138192 (enterics) or 0191 2448890 (serology) Hepatitis B viral Load HPA West Midlands, Birmingham Laboratory Birmingham Heartlands Hospital Bordesley Green East Birmingham B9 5ST Telephone: 0121 424 2000 ext 42240 Fax: 0121 772 6229 Immunology Department Queen Elizabeth Hospital Sheriff Hill Gateshead NE9 6SX Tel: 0191 4453298 Laboratory of Gastrointestinal Pathogens HPA Centre for Infections 61 Colindale Avenue London NW9 5EQ Tel: 020 8327 7116 Fax: 020 8905 9929 Laboratory of HealthCare Associated Infection (LHCAI) HPA Centre for Infections 61 Colindale Avenue London NW9 5EQ CDRN consists of seven regional microbiology laboratories in England for C. difficile culture and ribotyping Clostridium difficile Refer to Medical Microbiologist regarding where to send isolates when required Serology, Enteric outbreaks Hepatitis B viral Load. Occupational Health patients only. Please speak to a senior member of staff. Immunology Bacillus, Clostridium perfringens, Clostridium botulinum, Clostridium tetani neurotoxin detection, Listeria, Staphylococcal toxins, scombrotoxin, Water and Environmental, Food and Environmental Proficiency Testing Schemes, Water and Environmental microbiology. Salmonella E. coli, Shigella, Vibrio, Yersinia, Campylobacter culture, Helicobacter, Citrobacter Staphylococci, MRSA, Clostridium difficile, Enterococci, Klebsiella, Enterobacter, Serratia, Pseudomonas, Stenotrophomonas, Burkholderia, Acinetobacter, Hospital Infection advice Tel: 020 8200 4400 Fax: 020 8200 7449 Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 56 of 60 NHS GENERAL Email: lhcai@hpa.org.uk Leptospira Reference Unit (LRU) Hereford County Hospital Stonebow Road Hereford HR1 2ER Tel: 01432 277 117 Fax: 01432 351396 Email: leptospira.lru@hhtr.nhs.uk Department of Microbiology St Helier University Hospital Trust Wrythe Lane Carshalton SM5 1AA Tel: 01372735994 Newcastle HPE Molecular Laboratory Level 3 Medical School Royal Victoria Infirmary Newcastle upon Tyne NE1 4LP Leptospira Enterovirus IgM and PCR PCR Tel:0191 2821150 Mycology Ref Laboratory and Antimicrobial Ref Lab South West HPA Laboratory, Myrtle Road, Kingsdown, Bristol BS2 8EL Identification service for yeasts and moulds, including dermatophytes. Reference antifungal susceptibility testing. Serology for dimorphic pathogens and other unusual infections. Examination of histology slides. National Collection of Pathogenic Fungi. Tel: 0117 342 5028 Fax: 0117 922661 The Regional Mycology Laboratory, Manchester (RMLM) 2nd Floor laboratory, Education and Research Centre, Wythenshawe Hospital, Southmoor Road, Manchester. M23 9LT. Antifungal level assays Tel: 0161 2912124 Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 57 of 60 NHS GENERAL Meningococcal Reference Unit Manchester Medical Microbiology Partnership PO Box 209 Clinical Science Building Manchester Royal Infirmary Manchester Meningococcal and Pneumococcal PCR M13 9WZ Tel: 0161 276 6757 Fax: 0161 276 5744 Out-of-hours 0161 276 1234 ask for Microbiologist on call Newcastle HPE Regional Mycobacterial Reference Laboratory Level 2 Freeman Road Hospital Freeman Road High Heaton NE7 7DN Tel: 0191 2138784 HPE Parasitology Reference Laboratory Department of Clinical Parasitology Hospital of Tropical Diseases 3rd Floor Mortimer Market Capper Street London. WC1E 6JB Parasites and amoeba Tel: 020 7387 4411 ext. 5418 The Respiratory and Systemic Infection Laboratory (RSIL) HPE CfI Colindale 61 Colindale Avenue London NW9 5HT Tel: Fax: 020 8200 4400 020 8205 6528 Sexually Transmitted Bacteria Reference Laboratory (STBRL) HPA Centre for Infections 61 Colindale Avenue London NW9 5HT Streptococci (Groups A, B, C and G and all other streptococcal species, related genera), Streptococcus pneumoniae, potentially toxigenic Corynebacteria (Corynebacterium diphtheriae, C ulcerans, C pseudotuberculosis), Diphtheria serology, Tetanus (serology), Legionella spp, Mycoplasmas, respiratory Chlamydiae, Bartonella spp, Haemophilus influenzae, Bordetella spp. Anti Staphylococcal antibodies, Ureaplasm Bacterial sexually transmitted pathogens: Neisseria gonorrhoeae, Treponema pallidum, Chlamydia trachomatis, Haemophilus ducreyi Tel: 020 8327 6464 Fax: 020 8327 6081 Email: stbrl@hpa.org.uk Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 58 of 60 NHS GENERAL Rare and Imported Pathogens Laboratory (RIPL) Health Protection England, Porton Down, Salisbury, Wiltshire, SP4 0JG Arboviruses, Haemorrhagic Fever viruses, Nipah and Hendra viruses, Rickettsiae and Coxiella burneti, Bacillus anthracis. Dengue virus (Flavivirus). Lyme disease confirmation. Tel: +44 (0) 1980 612100 (24 hour switchboard) Fax: +44 (0) 1980 612695 Toxoplasma Reference Laboratory (TRL) Health Protection Agency Singleton Hospital Sketty Swansea. SA2 8QA Toxoplasma Tel: 01792 205666 Medical Toxicology Unit 3rd Floor, Block 7, South Wing, St. Thomas’ Hospital Lambeth Palace Road, London. SE1 7EH Pyrazinamide levels Toxicology Centre The Academic Centre University Hospital Llandough Penarth Vale of Glamorgan CF64 2XX Ethambutol and Isoniazid levels Veterinary Laboratories Agency New Haw Addlestone Surrey KT15 3NB Rabies Specialist Virology Centre South West Health Protection Agency Myrtle Road Kingsdown Bristol BS2 8EL Viral CFT’s, respiratory virology (Influenza A, B, Adenovirus, RSV) Atypical respiratory (Chlamydia, Q fever and Mycoplasma) Tel: 0117 3425551 Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 59 of 60 NHS GENERAL Reference laboratories will, if possible, be accredited with CPA (UK) Ltd. Status of the referred Department will be checked on an annual basis from information held on the CPA (UK) Ltd. website – www.cpa-uk.co.uk. Letters are sent out to the referral laboratories on an annual basis requesting confirmation that they have an acceptable EQA performance. They are asked to notify this laboratory if their performance falls outside of the acceptable criteria at any time to enable the department to determine whether any actions may be required. Selection of the reference laboratory is based on ability to meet minimum turnaround times (currently between 2 - 6 weeks depending upon the test) and cost. Title: Clinical Microbiology Users Handbook QP ref: LP-MIC-GEN-N-181v11.0 Author: Microbiology Speciality Board Authorised by: Microbiology Specialty Board Created: 19th December 2014 Disposal date: 19th December 2044 Page 60 of 60