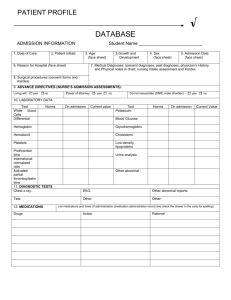
Client Profile Database
advertisement

UCN/UM Joint BN Program Course Number ______________________ CLIENT PROFILE DATABASE Student Name _____________________ ADMISSION INFORMATION Date of Care Client Initials Age Growth & Development Sex Admission Date Medical Diagnoses (present diagnoses, past diagnoses; physician’s history and physical notes in chart; nursing database; kardex) Reason For Hospitalization\Placement Surgical Procedures (consent forms and kardex) ADVANCE DIRECTIVES (Nurse’s Admission Assessments) Living Will : □ Yes □ No Power of Attorney: □ Yes □ No Do Not Resuscitate (DNR) Order □ Yes □ No LABORATORY DATA Test Red Blood Cells (RBC) Hemoglobin (Hgb) Hematocrit (HCT) Mean Corpuscular Vol. (MCV) White Blood Cells (WBC) Differential Platelets (PLT) Prothrombin time (PT) International normalized Ratio (INR) Activated Partial Thromboplastin time (APTT) Potassium (K+) Norms Current Value Interpretation/Why Test Norms Current Value Interpretation/Why Sodium (Na+) Chloride (Cl-) Calcium (Ca 2+) Blood Glucose Circle type FBS RBS ACCU Glycohemoglobin (Hgb A1C) Urine Analysis (UA) Lipid Profile: Cholesterol LDL Triglycerides Adapted from Shuster, P. (2002). Concept mapping: a critical-thinking approach to care planning by Fraser, K. & Kellett, P. (2004) DIAGNOSTIC TESTS Including all X-Ray, CT Scan, MRI, EEG, Ultrasound, Bone Scan, and other studies Chest X-Ray EKG ALLERGIES/PAIN Allergies (MAR) When was last pain Medication given? What was given? (medication administration record) Where is the Pain? Quality? Any radiation? (nurse’s notes) How much pain is the client in on a scale of 0-10? (nurses notes) TREATMENTS List Current Treatments Consultations and Support Services DIET/FLUID BALANCE Type of Diet (kardex): Restrictions (kardex): Gag Reflex Intact □ Yes Appetite: Breakfast Lunch Supper □ No ______% _____% _____% Circle Those Problems That Apply: Problems swallowing, chewing, dentures (nurse’s notes) Needs Assistance with feeding (nurse’s notes) Nausea or vomiting (nurse’s notes) Overhydrated or dehydrated (evaluate total intake and output) Belching Other ________________________________________________ Fluid Intake: 24 hours (I&O Sheet) Tube Feedings: Type & Rate (kardex) Intravenous Fluids (IV therapy record; kardex) Solution and Rate: IV dressing dry, no edema, redness of site □ Yes Other: □ No Adapted from Shuster, P. (2002). Concept mapping: a critical-thinking approach to care planning by Fraser, K. & Kellett, P. (2004) ELIMINATION (flow sheet, I&O) Last Bowel Movement 24- hour urine output (I&O) Foley/Condom Catheter □ Circle those problems that apply Bowel: constipation Urinary: hesitancy Other _________ diarrhea frequency Yes flatus burning Size □ No incontinence incontinence belching odor ACTIVITY (ADL’s) (Kardex, flow sheet) Ability to walk (gait) Number of side rails required (kardex): Type of activity orders: Restraints and type (kardex) □ Yes □ No Use of assistive devices: cane, Walker, crutches, prosthesis: Falls-risk assessment rating: Weakness Location □ □L □R Trouble Sleeping (nurse’s notes) Yes □ No □ Yes □ No PHYSICAL ASSESSMENT DATA BP (flow sheet): TPR (flow sheet): Height: _______ T= _____ REVIEW OF SYSTEMS P= _____ Weight: _______ (nsg. intake assessment) R= _____ Write WNL (within normal limits) if normal and describe abnormalities in the space provided. (Check nurse’s notes and shift assessments for the latest information you can get) NEUROLOGICAL/MENTAL STATUS ________ LOC: alert and oriented to person, place, time (A&O x3), confused etc. Motor: ROM x4 extremities Sensation: 4 extremities Speech: clear, appropriate/inappropriate Pupils: PERRLA Sensory deficits for vision/hearing/taste/smell MUSCULOSKELETAL SYSTEM _______ Bones, joints, muscles (fractures, contractures, arthritis, spinal curvatures, etc.) Extremity circulation checks (pulses, temperature, sensation, edema): TED hose/ plexi pulses/ compression devices: type: Casts, splint, collar, brace: CARDIOVASCULAR SYSTEM ________ Pulses (radial, pedal) (to touch or with Doppler): Neck vein (distension): Capillary refill (<3 s): □ Yes Edema, location, pitting vs nonpitting □ No Heart Sounds: S1, S2, regular, irregular: Any chest pain: Adapted from Shuster, P. (2002). Concept mapping: a critical-thinking approach to care planning by Fraser, K. & Kellett, P. (2004) RESPIRATORY SYSTEM _______ Depth, rate, rhythm Use of accessory muscles Use of oxygen: nasal cannula, mask, trach collar Cyanosis: Flow rate of O2 Sputum: color, amount Oxygen humidification □ Yes □ No Cough: Productive, nonproductive Pulse oximeter: Breath sounds: clear, rales, wheezes Smoking _____% O2 saturation □ Yes □ No GASTROINTESTINAL SYSTEM _______ Abdominal pain, tenderness, guarding; distension, soft, firm: Bowel sounds x4 quadrants: Ostomy: describe stoma site and stools: Other: NG tube: describe drainage SKIN AND WOUNDS ________ Color, turgor: Rash, bruises Describe wounds (size, location) Edges approximated □ Characteristics of drainage Dressings (clean, dry, intact): Yes Sutures, staples, steristrips, other: Type of wound drain □ No Risk for decubitus ulcer rating: Other: EYES, EARS, NOSE, THROAT (EENT): ______ Eyes: redness, drainage, edema, ptosis Ears: drainage Nose: redness, drainage, edema Throat: sore PSYCHOSOCIAL AND CULTURAL ASSESSMENT Religious preference: (face sheet) Marital Status (face sheet) Occupation (face sheet) Emotional State (nurse’s notes): RELEVANT SOCIAL HISTORY ______ Adapted from Shuster, P. (2002). Concept mapping: a critical-thinking approach to care planning by Fraser, K. & Kellett, P. (2004) DISCHARGE PLANNING_______ Expected Discharge Date: Discharge Planning Meeting Date Referrals needed for discharge: Discharge Plans: ADDITIONAL RELEVANT INFORMATION: Adapted from Shuster, P. (2002). Concept mapping: a critical-thinking approach to care planning by Fraser, K. & Kellett, P. (2004) MEDICATIONS: ROUTINE & PRN * Note: Students may attach drug printouts which contain the appropriate information, but relevant information must be highlighted or circled Dose, Route Frequency (generic name) Class/ Mechanism of Action Why is this client on this medication? Pertinent nursing implications Evaluation of drug’s effectivness Adapted from Shuster, P. (2002). Concept mapping: a critical-thinking approach to care planning by Fraser, K. & Kellett, P. (2004) PATHOPHYSIOLOGY: TEXTBOOK EXPLANATION-CITE REFERENCE Priority Health Problem Etiology (What Causes the Problem?) Risk Factors that contribute to the development of the problem List and lab or diagnostic Studies that may be utilized to evaluate this condition List Clinical Manifestations (Signs & Symptoms) and potential complications with a pathophysiological explanation for why they occur : Adapted from Shuster, P. (2002). Concept mapping: a critical-thinking approach to care planning by Fraser, K. & Kellett, P. (2004) POTENTIAL NURSING DIAGNOSES (List in priority order and give rationale as to why you have prioritized in this manner) ORGANIZATIONAL PLAN FOR DAY (Optional except in year 2) Time Plan Supplies and Equipment Needed Adapted from Shuster, P. (2002). Concept mapping: a critical-thinking approach to care planning by Fraser, K. & Kellett, P. (2004)