Consultation on draft UK Vision Strategy
advertisement
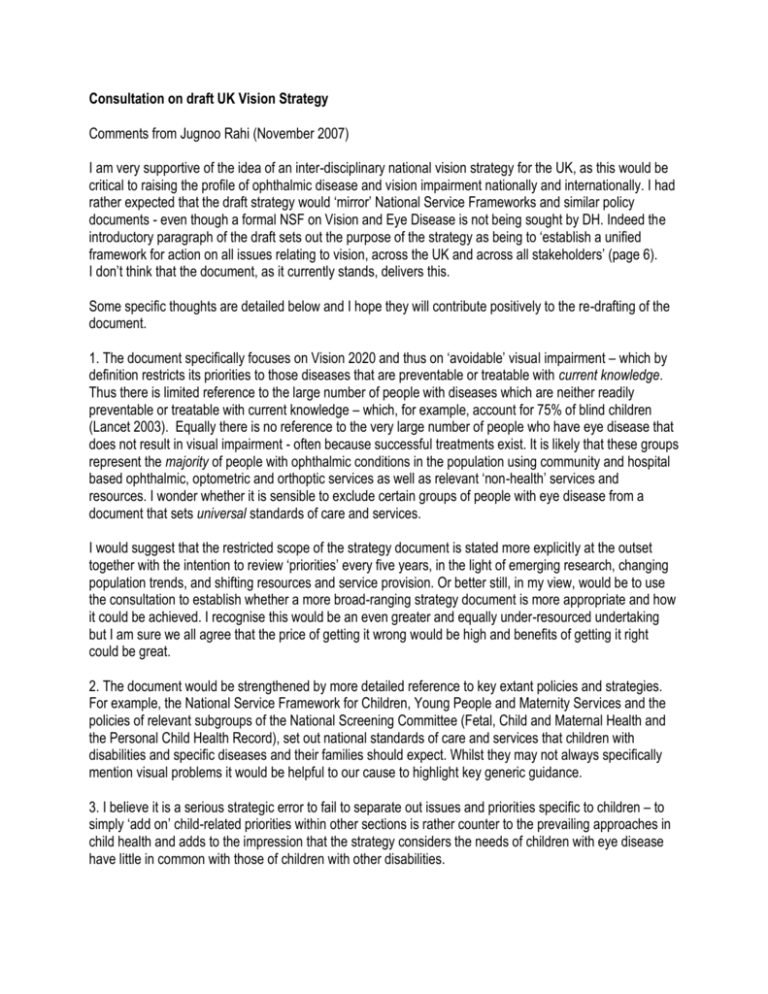
Consultation on draft UK Vision Strategy Comments from Jugnoo Rahi (November 2007) I am very supportive of the idea of an inter-disciplinary national vision strategy for the UK, as this would be critical to raising the profile of ophthalmic disease and vision impairment nationally and internationally. I had rather expected that the draft strategy would ‘mirror’ National Service Frameworks and similar policy documents - even though a formal NSF on Vision and Eye Disease is not being sought by DH. Indeed the introductory paragraph of the draft sets out the purpose of the strategy as being to ‘establish a unified framework for action on all issues relating to vision, across the UK and across all stakeholders’ (page 6). I don’t think that the document, as it currently stands, delivers this. Some specific thoughts are detailed below and I hope they will contribute positively to the re-drafting of the document. 1. The document specifically focuses on Vision 2020 and thus on ‘avoidable’ visual impairment – which by definition restricts its priorities to those diseases that are preventable or treatable with current knowledge. Thus there is limited reference to the large number of people with diseases which are neither readily preventable or treatable with current knowledge – which, for example, account for 75% of blind children (Lancet 2003). Equally there is no reference to the very large number of people who have eye disease that does not result in visual impairment - often because successful treatments exist. It is likely that these groups represent the majority of people with ophthalmic conditions in the population using community and hospital based ophthalmic, optometric and orthoptic services as well as relevant ‘non-health’ services and resources. I wonder whether it is sensible to exclude certain groups of people with eye disease from a document that sets universal standards of care and services. I would suggest that the restricted scope of the strategy document is stated more explicitly at the outset together with the intention to review ‘priorities’ every five years, in the light of emerging research, changing population trends, and shifting resources and service provision. Or better still, in my view, would be to use the consultation to establish whether a more broad-ranging strategy document is more appropriate and how it could be achieved. I recognise this would be an even greater and equally under-resourced undertaking but I am sure we all agree that the price of getting it wrong would be high and benefits of getting it right could be great. 2. The document would be strengthened by more detailed reference to key extant policies and strategies. For example, the National Service Framework for Children, Young People and Maternity Services and the policies of relevant subgroups of the National Screening Committee (Fetal, Child and Maternal Health and the Personal Child Health Record), set out national standards of care and services that children with disabilities and specific diseases and their families should expect. Whilst they may not always specifically mention visual problems it would be helpful to our cause to highlight key generic guidance. 3. I believe it is a serious strategic error to fail to separate out issues and priorities specific to children – to simply ‘add on’ child-related priorities within other sections is rather counter to the prevailing approaches in child health and adds to the impression that the strategy considers the needs of children with eye disease have little in common with those of children with other disabilities. 4. I think it is inaccurate to suggest in the document that all relevant stakeholders were represented in its preparation. For example in relation to priorities for children, I would have expected a community paediatrician and a hospital paediatrician as well as an educationalist to have been consulted on each ‘paediatric’ priority. Perhaps if ‘children’s issues’ had been a separate chapter, wider ‘paediatric’ consultation would have been more easily achieved? 5. I think that the ophthalmic and vision sciences research community could have been usefully consulted formally during the drafting of the document, avoiding: a) firstly, the statement that the ‘during the consultation process priority areas of research will be identified and incorporated as well as analysis of the financial investment required and the potential cost benefits of the strategy.’ (page 7) This is puzzling. The starting point for a strategy document should be a systematic review of the best quality research evidence on which recommendations are made - identifying gaps in evidence should be the first step, not the last. Whilst it is not my area of expertise, robust economic modelling is not a’ quick and easy’ task and it seems unlikely that it could be undertaken as part of a consultation. b) secondly, the several assertions in the document that are unsupported by evidence (of any quality) and which therefore serve to undermine the authority of the whole document. I am very concerned that a particularly strong theme throughout is the notion that universal and regular ‘sight tests’, referring mainly to those conducted presently in the community by optometrists, would inevitably and universally improve early diagnosis and thus lead to successful outcomes of treatment. This optimistic view (4 of the 7 case studies describe the detection of relatively rare conditions by optometrists) would be strongly challenged by a review of the most robust research evidence in relation to the detection of visually impairing or blinding eye disease in children. Although I know the ‘adult literature’ less well, I think the same would be largely true. 6. I have concerns about the following specific recommendations about children: a) Recommendation point 1.3.1.3 (page 12) regarding ‘eye health assessment’ at a number of key stages during childhood contradicts the extant UK National Screening Committee policy on vision screening in childhood. No evidence is presented in support of this recommendation. During March 2008, the National Screening Committee will be re-examining the national programme of childhood vision screening and surveillance, its implementation nationally and any new research evidence which informs policy. Mike Clarke and I, amongst others will be contributing to this process. In any case, about 75% of visually impairing or blinding eye disease in children in the UK is present from birth or diagnosed by the first year of life (Lancet 2003). Thus the role of ‘sight’ tests during later childhood is very limited. It would be important that the document clarified this. Whilst ‘sight’ tests may be appropriate for detecting sub-optimal visual acuity due to refractive error and amblyopia, there are limited robust data on the degree of refractive error that confers significant functional disadvantage and the assumption that all refractive error in childhood, however mild, must be treated is questionable. For information: i) we currently have a paper under review reporting on the prevalence (low) of undiagnosed refractive error in working age adults in the UK and the functional correlates (surprisingly few). ii) in relation to point 1.3.1.3, I have been discussing with the Personal Child Health Record Subgroup the inclusion of detailed information on visual function and the best means of achieving this through electronic data capture and record linkage – this is not a small or isolated undertaking, especially in the context of implementation of Connecting for Health, but it is on their agenda. b) Recommendations 2.3.1.8, 2.3.3.3, and 3.3.1.2 All the points made here are the subject of existing national guidance – it would probably be more powerful to refer to these explicitly and in specific detail eg The National Screening Committee’s programme of childhood screening and surveillance for eye disease, the National Service Framework for Children, RCOphth and RCPCH joint party guidance on multi-disciplinary visual impairment teams, the Warnock report on key workers etc.