what are hip protectors? - Canadian Association of Occupational
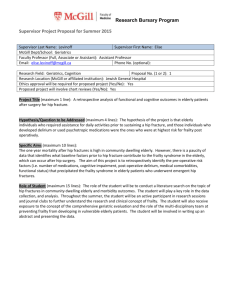
advertisement

Tools for living well: hip protectors Hip Protectors and Community-Living Seniors: A Review of the Literature Submitted to Ms. Jeannette Toews, Health Canada, Division of Aging & Seniors Prepared by Drs. Heidi Sveistrup, Donna Lockett, University of Ottawa On behalf of the Tools for Living Well Project (funded by HC/VAC Fall Prevention Initiative) October, 2003 Disclaimers: The opinions expressed in this document do not necessarily reflect the official views of Health Canada or Veterans Affairs Canada, who are not responsible for errors or any consequences arising from the use of the information published in this document. The inclusion of any activity or course of action does not imply that Health Canada or Veterans Affairs Canada accept, endorse or consider it as being superior to any other. -1- Tools for living well: hip protectors EXECUTIVE SUMMARY The Issue Approximately one third of community-living older adults 65 years and over experience one or more falls in a year with the risk of a fall increasing with advanced age. Recent Canadian figures show that, among seniors, 40% of hospital admissions following falls are related to hip fractures. Of all fall-related fractures, hip fractures cause the greatest injury and deaths. They also have a substantial impact on quality of life. The cost of hip fractures in Canada is $650 million and this cost is expected to rise to $2.4 billion by 2041. Initiatives that can reduce hospitalizations due to falls by 20% could lead to 7,500 fewer hospital stays and 1,800 fewer Canadians permanently disabled, with an overall saving of over $138 million annually. Hip protectors, assistive devices designed to absorb and or transfer energy at the trochanter associated with a fall onto the hip, have demonstrated effectiveness for prevention of hip fractures in institutional and residential settings. Objectives The general objective was to review and summarize the literature regarding the efficacy of hip protectors for community-living older adults. Additional objectives were to provide overviews of 1) prevalence and cost of hip fractures, 2) the relationship between falls and risk factors for fractures, 3) how hip protectors work, and 4) benefits of hip protectors and issues related to compliance. Methods This is a summary of English and French literature with, where feasible, inclusion of all available published and grey literature. This is not a systematic review or meta-analysis. There were no restrictions placed on publication date. The review is restricted to literature focusing in whole or part on independent community-living seniors. Literature was reviewed from journals appearing in but not restricted to specific databases as well as personal contacts with experts on hip protectors. -2- Tools for living well: hip protectors Results This document summarizes 91 relevant published documents as well as personal communication with four experts. Six intervention studies are included, although only four of these had samples that were comprised exclusively of community-living seniors Fall related hip fractures occur when an individual, typically with insufficient soft tissue to absorb the shock, fails to generate an appropriate protective response and impacts the ground or other hard surface at or near the hip with a force that exceeds the fracture threshold of the proximal femur. Individuals at risk of fracturing a hip include those who are older, frail, female, have osteoporosis, frequent fear of falling, and sedentary lifestyle. It is unclear how many risk factors must be present to increase the risk of a hip fracture. Personal costs associated with hip fractures are devastating with over 20% of individuals dieing within 12 months of the fracture and an additional 24-40% requiring nursing home care post fracture. One year post fracture, 40% of individuals remain unable to walk independently. Personal reports indicate that a significant number of community-living older adults (80%) would rather be dead than experience the loss of independence and quality of life resulting from a bad hip fracture and subsequent admission to a nursing home. Hip protectors do not prevent falls. Rather, they work to prevent fall-induced fractures through two mechanisms, energy absorption and/or energy shunting. The distinct brands available on the market are designed to incorporate different degrees of energy absorption and shunting. Initial acceptance of hip protector is relatively high in most studies, around 60%. However, adherence with hip protector use drops rapidly with reports of wear compliance decreasing with time in study. Moreover, compliance at different times during the day varies with evening/nighttime wear lowest. The effectiveness of a hip protector depends largely on its compliance with use. When studies have not controlled for adherence, they have reported no significant differences in incidence of hip fracture between hip protector and control groups. However, in two studies reviewed that adjusted for actual use of hip protectors, reductions in hip fracture risk were reported. However, -3- Tools for living well: hip protectors and likely due to small sample sizes, only one of these studies reported significant findings. Hip fractures have been reported in a small number of individuals while wearing hip protectors, but most of these occurred during falls backwards onto the posterior hip or with no observed impact on the hip protector suggesting that the individual did not land on the hip protector. Thus, when hip protectors are worn, there appears to be a preventative effect, but non-adherence is problematic in all reports and requires special mention. Conclusions The literature summarized here identifies the significant health care burden associated with hip fractures in community-living older adults and the importance of multiple interventions, including the use of hip protectors, for preventing fractures. Because all older adults likely have sufficiently compromised bone strength and other risk factors that put them at risk for a hip fracture and in light of the findings that hip protectors can attenuate the force of a fall, it is compelling to recommend widespread prescription of hip protectors However, in part due to small sample sizes and poor compliance with use, results of clinical studies with communityliving seniors do not unilaterally support the protective benefits of hip protectors in reducing hip fracture risk. To be effective, hip protectors must be position correctly and work consistently. Long-term compliance with use is a challenge. Seniors most likely to benefit from wearing hip protectors are men and women displaying multiple risk factors for hip fractures. -4- Tools for living well: hip protectors TABLE OF CONTENTS INTRODUCTION .......................................................................................................................... 6 WHAT ARE HIP PROTECTORS? .............................................................................................. 10 WHAT IS A HIP FRACTURE? ................................................................................................... 11 WHAT IS THE PREVALENCE AND IMPACT OF HIP FRACTURES ................................... 12 HOW DOES A FALL CAUSE A HIP FRACTURE?.................................................................. 14 WHO IS AT RISK FOR HIP FRACTURES? .............................................................................. 15 BENEFITS OF HIP PROTECTORS FOR COMMUNITY-LIVING SENIORS? ...................... 20 WILL COMMUNITY-LIVING OLDER ADULTS WEAR HIP PROTECTORS? .................... 28 ARE THERE SIDE EFFECTS ASSOCIATED WITH HIP PROTECTORS? ............................ 33 SUMMARY, RECOMMENDATIONS AND CONCLUSION ................................................... 34 REFERENCES ............................................................................................................................. 39 APPENDIX A: List and description of hip protectors.................................................................. 46 APPENDIX B. Demographic, health, lifestyle, and psychological risk factors for hip fractures 51 APPENDIX C: Results of community-based randomized controlled clinical trials on effectiveness of and compliance with hip protectors ................................................................... 54 -5- Tools for living well: hip protectors INTRODUCTION This literature review was conducted as part of the “Tools for Living Well” project, which was funded by the Health Canada/Veterans Affairs Canada Falls Prevention Initiative. This review has a very specific focus that is best stated by the following question: What is the current state of information about the use of hip protectors by community-living seniors? The primary objective is to review the literature regarding the efficacy of hip protectors for community-living older adults. The review begins by providing a summary of the methods used to uncover research. Next, we provide an overview of hip fractures, including the prevalence and cost of hip fractures. This is followed by an overview of the relationship between falls and hip fractures, and some indication of who, among community-living seniors, may be at highest risk for hip fractures. We explore, next, the benefits of hip protectors for community-living older adults, followed by issues related to compliance. The review concludes with recommendations for the prescription and promotion of hip protectors among community-living older adults and suggestions for future research. This is a summary of the literature, NOT a systematic review, nor a meta-analysis. As much as is feasible, we have attempted to cover all available published and grey literature. Further, the review is restricted to research conducted, in whole or part, with independent community-living seniors. It excludes research based exclusively on seniors living in long-term care facilities. A review from the Cochrane group69 of elderly people in nursing homes, residential care, or supportive living at home has documented the benefits of hip protectors for that population, concluding “hip protectors appear to reduce the risk of hip fracture within a selected population at high risk of sustaining a hip fracture. The genereralization of the results is unknown beyond high-risk populations.” We will not duplicate their efforts here. -6- Tools for living well: hip protectors PARAMETERS AND OVERVIEW OF WORK The following defined and/or limited the terms of the work: English and French language published literature that appears in selected journals and electronic databases (without consideration for publication date). Information from technical, government, and other reports was also included. As hip protectors are relatively new, no restrictions on year of publication was included. E-mail and phone contacts were made (summarized below) with selected experts on “hip protectors” to capture opinions on relevant work (literature) that the research team may have missed. The experts were contacted regardless of location. The studies reviewed were based on community living seniors, NOT studies that included exclusively institutionalized seniors or seniors living in long-term care facilities. Based on the parameters above, relevant literature was retrieved, read, evaluated and summarized by the research team in terms of the project problem. Literature Search strategy In order to locate relevant publications based on the project parameters described above, the following databases were examined: AARP AGELINE, CINAHL, Cochrane Database of Systematic Reviews, MEDLINE, AMED, and EMBASE. Searches were done using the following keywords, alone and in combination: age, senior, elder, hip protectors, assistive devices, older adults, seniors, falls prevention, hip fractures, laboratory studies, community studies In addition, searches (by author) were carried out using the names of several researchers well known in the area of hip protectors. These experts were identified through cross-references of keyword searches and reviewed literature. Searches for their work was then carried out in the above mentioned databases. They are: "Poutala, J" ; "Lauritzen, JB”; "Cryer, C"; "Parkkari, J"; "Kannus, P"; “Robinovitch s” and “Robinovitch sn"; “Hubacher, M” . -7- Tools for living well: hip protectors Telephone and e-mail contacts In addition to specific expert literature searches, key individuals were contacted via e-mail and telephone (see below). Individuals were contacted if we were unable to obtain key literature or if specific studies were mentioned in review papers or research highlights but original literature was unavailable. The information requested from each individual appears below. Dr Ian Cameron, Associate Professor, Rehabilitation Medicine and Motor Accidents Authority of New South Wales Chair in Rehabilitation Medicine. Rehabilitation Studies Unit, PO Box 6, Ryde NSW 2112 Phone: +61 2 9808 9236; Fax: +61 2 9809 9037 ianc@health.usyd.edu.au mailto:ianc@mail.usyd.edu.au Rehabilitation Studies Unit, University of Sydney, Ryde, NSW. Information requested: Study information for research project entitled “The effectiveness of external hip protectors in high-risk community-living older women”. Response: Received a list of references of work undertaken by the group. If information was available and deemed relevant, it has been incorporated into this review. Dr. Lesley Day, Senior Research Fellow Accident Research Centre, Building 70, Monash University, Victoria, 3800, Australia Phone: +61 3 9905 1811 ; Fax: +61 3 9905 1809 Lesley.Day@general.monash.edu.au Information requested: Information on current falls prevention projects including a randomised controlled trial of three falls prevention interventions in collaboration with the City of Whitehorse including “No Falls randomised trial of falls prevention among older people”. Response: Hip protectors not included in the interventions. -8- Tools for living well: hip protectors Dr Klaus Hindso, Department of Orthopedic Surgery, Rigshospitalet, University of Copenhagen DK-2100 Copenhagen 0 mail:hindso@dadlnet.dk Information requested: Information on research project entitled :Prevention of hip fractures using external hip protectors. Risk factors for falls, hip fractures, and mortality; and evaluation of the consequences of fear of falling among older orthopedic patients” Response: Received e-copy of dissertation summary (in English) and full copy of dissertation (in Danish). The work has been incorporated into this review. Dr Steven Robinovitch, Assistant Professor School of Kinesiology, Simon Fraser University. West Mall Centre 2812 8888 University Drive. Burnaby, BC V5A 1S6 Tel: (604) 291-3566 stever@sfu.ca Information requested: Current work undertaken by research group in the area of hip protectors. Response: Received a comprehensive list of references and current state of relevant research as well as summary and presentation work completed by author. The work has been incorporated into this review. Unsuccessful contacts were attempted with the following individuals: David Togerson, Centre of Health Economics, University of York Y0105 DD UK I Watt, Centre for Review and Dissemination, Department of Health Sciences, 1st Floor, Seebohm Rowntree Building University of York, York YO10 5DD Mrs S Le Masurier, Research Network Manager, University of Herfordshire -9- Tools for living well: hip protectors WHAT ARE HIP PROTECTORS? Hip protectors are hip pads that are either sewn or placed into stretchy undergarments or attached to a belt to be worn outside of clothing. Hip protectors come in a variety of shapes, models and materials. Most have a soft pad that covers the hip. Some include an additional harder more rigid outer shell that sits on top of the soft pad. Most are round or oval, although new designs are emerging. In Canada, manufacturer suggested retail prices range from $79.50 to $118 (as of October, 2003). At the time of this review, only two health insurance carriers were identified, through personal contact (phone calls) that indicated they reimbursed the costs of hip protectors. A list of different hip protector brands and their features is presented in Appendix A. Hip protectors are designed to decrease the impact of a fall from the vulnerable hip area (the femoral neck) and/or to redistribute it to less vulnerable areas.59 As a result, the force that is transferred to the hip in a fall is reduced and the potential of a hip fracture is minimized. This effect is achieved by one or a combination of two mechanisms: energy absorption and energy shunting.49 Of note, most hip protector brands purport to offer both energy absorbing and energy shunting protection, though to varying degrees. In the first mechanism, hip protectors are said to absorb energy associated with a fall onto the hip. This is achieved by placing special materials directly over the hip joint. Thus the overall force exerted on the greater trochanter and the chance of a hip fracture is decreased. The second mechanism involves an energy shunting system that diverts force away from the greater trochanter to the surrounding tissue68 so that the hip area receives less of the force generated during a fall onto the hip. There are several types of energy shunting systems on the market, including hard plastic shelled exteriors, systems that use motorcycle wear material (e.g. HipShield), airbags13 and more recently, horse-shoe-shaped designs (not yet on the market and thus not included in Appendix A).71 Figure 1. Schematic of two types of hip protector (A) worn over clothing and (B) worn within specially designed underwear - 10 - Tools for living well: hip protectors WHAT IS A HIP FRACTURE? A hip fracture is a break near the top of the thighbone (femur) where it angles into the hip socket. The break is usually detected at the femoral neck or intertrochateric region of the hip joint. A clear indication that the hip is fractured is extreme pain during weight bearing and a rotation or shortening of the leg. In most cases, hospitalization and surgery are required. A B C Figure 2. The healthy femur is shown. Hip fractures involve fracture of any aspect of the proximal femur, from the head (B) to the first 4-5 cm of the subtrochanteric area (C). - 11 - Tools for living well: hip protectors WHAT IS THE PREVALENCE AND IMPACT OF HIP FRACTURES Prevalence of fall-related hip fractures. In 1993/94 there were 23,375 hip fractures reported in Canada. With our aging population, it has been projected that this number will increase almost fourfold, to 88,124 annually by the year 2041.15 Ninety percent of fractures among people over age 70 are the result of a fall.16 Among community-living older adults, it has been estimated that one third of people 65 years and over experience one or more falls in a year, and that the risk of a fall increases even more with advancing age.31 Falls account for 86% of admissions to Ontario hospitals for people age 65 and older.62 Among seniors who fall, about 10% sustain a serious injury.84 Almost half of all serious injuries experienced by seniors who fall are fractures (49%) and, of these fractures, almost 1 in 5 is a hip fracture (19%). This makes hip fractures the third most common type of fall-related fracture, behind legs/feet and arms/hands.89 However, of all fallrelated fractures, hip fractures cause the greatest number of deaths and lead to the most severe health problems and reduced quality of life .28,90 Costs of hip fractures. The latest Canadian figures show that, among seniors, 40% of hospital admissions following falls are related to hip fractures.31 The average one-year cost of a hip fracture has been reported at $27,527.88Annual economic implications of hip fractures in Canada are $650 million and are expected to rise to $2.4 billion by 2041.88 The personal costs of a hip fracture may be even more devastating. According to the National Osteoporosis Association, up to 20 to 24% of individuals older than age 50 will die within 12 months of suffering a hip fracture62 - that’s one in 4-5 people. Mortality after hip fracture is higher for men than women, increases with age 17 and is greater with co-existing illness and poor pre- fracture functional status.66,69,52,18 The reasons for the high rate of mortality following a hip fracture are not yet fully understood. - 12 - Tools for living well: hip protectors The morbidity associated with hip fractures is also high. As many as 24 to 40 % of individuals require nursing home care.62,88 One year post-fracture, 40% of patients are still unable to walk independently,66 and 50% require an assistive device like a cane or walker.62 More than half (60%) require help with one essential activity of daily living (e.g. bathing, dressing, food preparation) and 80% are unable to perform at least one instrumental activity of daily living (e.g. driving, house cleaning).66 Pre-fracture status is a strong predictor of hip fracture outcome, with individuals who require some form of assistance pre-fracture being more likely to be admitted to a nursing home14 or to require assistive care.5 Perhaps more importantly, subjective reports of the impact of a hip fracture illustrate the significant effect the event has on an individual’s life. In one study, 194 community-living women who were 75 years and older and at high risk for a hip fracture were asked to rate their quality of life under different hypothetical post-hip fracture scenarios.75 Of the women surveyed, 80% indicated that they would rather be dead than experience the loss of independence and reduced quality of life resulting from a bad hip fracture and the subsequent admission to a nursing home. The anticipated quality of life of the women participating in the study was profoundly threatened by falls and hip fractures with any loss of ability to live independently in the community having a considerable detrimental effect. - 13 - Tools for living well: hip protectors HOW DOES A FALL CAUSE A HIP FRACTURE? A fall appears to precede a hip fracture rather than vice versa,4,10,11,23,27,87 and it has been estimated that most hip fractures are related to a direct impact on the hip resulting from a fall.20,29,43 Nevitt & Cummings20,64 identified four minimal conditions for a hip fracture to occur following a fall. These are illustrated in Figure 3 below. First, there is a requirement for a deficit in the protective postural reflexes that would normally be used to prevent a fall. These protective responses include stepping to catch ones balance or breaking the fall with the arms. The failure of a protective response during the fall – for example due to aging, cerebrovascular disease, or concurrent medication (particularly the excessive use of sedatives, and/or polypharmacy) contributes to the increased risk of fracture on the occasion of a fall. Second, the fall impact needs to be at or close to the hip. Most hip fractures (60-99%) are related to direct trauma to the hip.20,43,35 For example, one study64 reported that 66% of hip fractures occurred when the individual fell sideways and onto the hip, side of leg, or buttocks. Falling backward reduced the risk of hip fracture. Falling onto a hard surface on the hip, side, or buttocks increased risk of hip fracture over falling on a softer surface. Third, the passive energy absorption by the soft tissues (muscles, fat) anterior and posterior to the greater trochanter must be insufficient. This is based on studies reporting that individuals with more soft tissue (e.g. overweight women) are less likely to fracture in the event of a fall as compared to individuals with less soft tissue.43 Findings from laboratory studies have confirmed that the decrease in fall impact force is directly related to the thickness of soft tissue over the hip. For example, one study of female subjects showed that a threefold increase in trochanteric soft tissue softness caused a 34% reduction in fall impact force.71. Studies have suggested that the energy absorption of the soft tissue may be as, or more important than bone strength in determining hip fracture.43 - 14 - Tools for living well: hip protectors Fourth, the residual energy of the fall must exceed that needed to fracture the proximal femur. That is, the strength and/or density of the bone cannot withstand the force of the fall. Several studies have reported that people who suffer hip fractures have lower bone mineral density at the femoral neck56,57,65 and a preferential deficit of bone density at the intertrochanteric scanning site.1,70 However, using measurements of bone density as a screening test for hip fracture risk may not be reliable as some studies have reported that: a) women with hip fractures have bone mineral density values in the same range as controls when the measurements are adjusted for age19,55 and; b) most elderly men and women have lost sufficient bone for the hip to fracture if impacted during an unprotected fall.48,46 In fact, it has been suggested that even in the least severe force impact case of a female with greater soft tissue over the hip and falling in the muscle-relaxed condition, a fall to the side producing lateral impact on the greater trochanter has the potential to fracture an elderly hip every time it happens.71 Protective responses (1) Bone density Bone strength (4) HIP FRACTURE FALL Impact to hip (2) Energy absorbed (3) Figure 3. Cascade of events leading to hip fracture Adapted from Lauritzen (1996)44 Hip fractures: incidence, risk factors, energy absorption, and prevention. Bone 18:65S75S. WHO IS AT RISK FOR HIP FRACTURES? In addition to the four minimal conditions identified in Figure 3, several studies have elucidated the profile of individuals at risk for fracturing a hip. Unless otherwise indicated, the studies reported here examined risk factors in multivariate models and had samples that comprised of The energy available in a fall from standing, about 500 Joules (J), is much greater than that required to fracture the elderly proximal femur, about 25 J (Note: A joule (pronounced DJOOL) is a standard unit of energy. One joule is defined as the amount of energy exerted when a force of one newton is applied over a displacement of one meter.) - 15 - Tools for living well: hip protectors only or mostly community-living seniors. Caution in interpreting these data should be used, especially in light of different and varying results. An overview of the prospective studies reviewed here is attached in Appendix B. A summary of risk factors for hip fractures is presented in Table 1. Demographics and family history profile of people at risk Age. Three studies have reported that, after controlling for other risk factors, advanced age increases the risk of hip fracture.22,34,59 The age at which the risk increases was not specified in these studies. However, hospital data suggest that the incidence of hip fractures in women increases exponentially after about the age of 60 and more than 90% of individuals sustaining hip fractures are 70 years of age or older.12,26, Gender. One study found that, controlling for other risk factors, women are more likely to sustain a hip fracture following a fall than men.34 Hospital data suggest that women have a onein-seven chance of sustaining a hip fracture during their life compared to one-in-seventeen for men (American academy or orthopedic surgeons). However, the types of hip fractures experienced by men and women are relatively similar. In one report of women who were 60 years or more, 878/1513 (58%) hip fractures were at the cervical neck while 635/1513 (41%) were at the trochanter. In men with hip fractures, the numbers were 273/505 (54%) and 232/505 (46%) at the cervical neck and trochanteric region, respectively.42 Family history of hip fracture. One study reported that a woman whose mother had a hip fracture before the age of 80 was twice as likely to have a hip fracture herself as one without a family history.21 In contrast, a history of other fractures is not associated with increased risk of hip fracture. Of note, maternal familial history of hip fracture was independent of bone mass, height, and weight. Inherited characteristics other than bone density or a greater propensity to fall on the hip may account for this familial predisposition. Different and varying results may be due to the inclusion or exclusion of certain groups of people based on gender, age, health status and differences in the selection of risk factors that were included and examined. - 16 - Tools for living well: hip protectors Health profile of people at risk The role of soft tissue mass and low bone density and hip fractures was reviewed earlier. Other health related risk factors are reviewed here. Weight and Height. Low body weight and low body mass index is associated with increased risk of hip fracture.21,58,59 In fact, in one study, older women who weighed less than they did at age 25 had a double risk of hip fracture compared to those who did not weigh less.21 Having low body weight may be associated with a higher risk due to low hip bone mineral density24 or a less effective protective effect of soft tissue cushion in the hip region44 Loss of weight may also be a marker of underlying illness that increases one’s risk of fractures.21 Being tall58,59,64 has been found to predict hip fractures following a fall. Being tall may be associated with a higher risk of fracture resulting from the greater potential energy of the fall 30 and a longer hip axis which would result in a greater femoral arm movement requiring less force needed to break the hip.25 Health problems. The risk of fracture is reportedly greater among older adults with certain health conditions. One study reported that respiratory illness increased the risk of hip fracture. 58 Others have reported increased hip fractures among older adults with a history or current condition of hyperthyroidism,21 cerebral stroke,59 diabetes,59 and tachycardia (elevated resting heart rate).21 The extent to which these conditions independently increase hip fractures or do so by virtue of an association with other risk factors, such as osteoporosis (respiratory illness)58 direct or indirect impaired bone and muscle strength (hyperthyroidism, cerebral stroke, tachycardia),21 or altered bone status due to peripheral neuropathy or diabetic retinopathy (diabetes)59 is unclear. The occurrence of hip fractures is also related to factors that represent frailty which might reduce the seniors’ ability to react in the event of a fall (e.g., extend their arms) and thus limit the ability to decrease the force of the fall on a hip. These include poor health or physical impairments,21,34,51,58 functional impairment,21,58 perceptual impairments such as depth perception, poor frequency contrast sensitivity and poor visual acuity21,51 and cognitive - 17 - Tools for living well: hip protectors impairments.34 Similarly, medication use, in particular long-acting benzodiazepines and anticonvulsant drugs that diminish alertness and increase the risk of falling, have been found to independently increase the risk of hip fractures among older women.21 Lifestyle profile of people at risk Exercise habits and muscle strength. One study reported that women who walk regularly had a 30% lower risk of hip fracture as compared to women who do not walk regularly.21 Similarly, women who spent less than four hours on their feet per day had twice the risk for fractures of the hip as compared to women who spent 4 hours or more on their feet per day. Although exercise may be a marker for health or bone density, that is, those who exercise regularly have higher bone mass,38 even after controlling for self-rated health and bone density the relationship persisted, indicating an independent relationship between exercise and hip fractures. Some studies have reported specifically that knee strength and tricep muscle strength,51,64 are important in preventing hip fractures. Tricep muscle weakness as an independent risk factor for hip fracture suggests that protective arm responses may be a less effective defense against hip fracture among those with weak arm extensors.64 . Knee extensor weakness may increase the velocity of falling, leading to a higher risk of fracturing.51 Caffeine intake. Cummings et al.21 reported that caffeine consumption increases risk of hip fractures in women. Although high caffeine has been associated with low bone mass, even after controlling for bone mass, caffeine intake predicted hip fracture. This suggests that the relationship may be due to some other, as yet not understood, mechanism. Smoking. Smoking has been found to predict hip fractures in some studies.21,34 Smoking may increase risk of hip fracture by limiting normal weight gain and by its adverse effects on health, in particular obstructive respiratory disease and osteoporosis59 or neuromuscular fitness and exercise patterns.63 - 18 - Tools for living well: hip protectors Psychological profile of people at risk Fear of falling. A relationship between fear of falling and falls leading to fractures has been reported.51 Fear of falling can result in the use of inadequate postural strategies during postural perturbations36 potentially exposing the person to falling when their balance is challenged. This, in turn, may lead to simultaneous contraction of muscle agonist and antagonists, 2 which increases joint stiffness and may lead to increased force of impact during a fall.51 Table 1. Risk factors for hip fractures in community-living older adults based on multivariate analyses Demographic and family history related risk factors Advanced age (over 70) Being female Maternal family history of fracture before age 80 Health related risk factors Low body weight / body mass Low bone density Being tall Co-morbid medical conditions respiratory illness hyperthyroidism diabetes cerebral stroke tachycardia Frailty (increased risk of falling) poor health or physical impairment functional impairment cognitive impairment diminished visual abilities use of benzodiazepines or anticonvulsants Lifestyle related risk factors Reduced muscle strength and low level of physical activity Caffeine use Smoking Psychological risk factors Fear of falling - 19 - Tools for living well: hip protectors BENEFITS OF HIP PROTECTORS FOR COMMUNITY-LIVING SENIORS? Before exploring what hip protectors can do, it may be important to note what hip protectors cannot do! What hip protectors CANNOT do Hip protectors cannot prevent falls. Further, hip protectors are not designed to protect against and have limited effectiveness for less common falls that may fracture the hip such as indirect rotational injuries40,47, or falls where a person lands on the buttocks or other body parts.73 Thus, complete protection of the hip cannot be taken for granted even when using a hip protector. Finally, hip protectors cannot protect the proper area if they are not worn or if they are worn incorrectly. What hip protectors CAN DO: results of laboratory studies Several laboratory studies have looked specifically at the impact energies and forces that are recorded at the femur when different hip protectors are used. Although the information cannot be directly transferred to the “real-life” situation, the data provide an idea of the efficacy of certain devices. For the most part, results of laboratory data demonstrate that the hip protectors studied were successful at providing some degree of force attenuation and that their efficacy varied as a function of the design and material composition. In one laboratory study, eight different hip protector pads (Inpant pad, Hip Guard, Strock pad, Wortberg pad, IOWA FICSIT pad, Lauritzen pad, Inverted U-shaped shunting pad, and a pad supplied by Heikenheimo) were tested using an impact machine with a dummy femur. The pads ranged in absorption and shunting characteristics with two extremes, the Wortberg pad defined as primarily energy absorbing and the inverted U-shaped pad defined as primarily energy shunting. Results showed that six of the eight pads tested failed to reduce femoral impact force below the mean force that would be required to fracture the elderly femur, although all of them provided some degree of force attenuation.72 The authors concluded that certain impact situations may arise where these six less effective padding systems could be capable of preventing fracture. These situations would include: a) falls that result in impacts that are spread over a larger region of the body, as opposed to being absorbed entirely by the hip, and b) falls by people who have - 20 - Tools for living well: hip protectors femoral bones that are stronger than average for their age. The two pads that reduced the impact force to levels below fracture threshold for seniors were the pad supplied by Heikinheimo (Tampere Finland SF-33210) and the U-shaped pad. Although some results regarding the pad used by Heikinheimo and colleagues have been reported, the specific characteristics of the pad are unclear32 but are reported to be similar to those used by Villar et al,84 SafeHip. The inverted U-shaped pads overlie soft tissue anterior, posterior and superior to the proximal femur. The pads consist of inner and outer flexible membranes containing a suspension that sharply increases in stiffness during impact to provide effective energy shunting. Another lab study determined the force attenuation capacity of four different hip protectors made with materials of varying characteristics that provided varying amounts of energy absorbing and energy shunting protection – (KPH1, KPH2, Safehip & Safetypants).40 The KPH pads consist of semiflexible exterior and inner absorbing materials and are primarily designed for shunting energy away from the trochanter. The Safehip, designed to shunt and absorb, have relatively flexible foam exteriors with an internal reinforcing membrane of higher density foam. Finally, the Safetypants, primarily absorbing, are constructed with low density foam. A pendulum was used to deliver impact forces of different amounts to a substitute (dummy) pelvis and femur. When the impact forces were low, all of the protectors reduced the impact force at the femur below the average fracture threshold level (reported in this study to be 3100 +/- 1200 N) of the proximal femur of older women. At moderate and high impact forces, only the KPH protectors reduced the force at the proximal femur to levels below the fracture threshold levels. The differential effect is explained by the firm and adequately convex structure of the KPH pad with force attenuation relying primarily on energy-shunting mechanisms. In a third study, young volunteer subjects tested two types of pads, one firm and one soft, by doing pad protected lateral falls from a standing position onto the hip as well as impact drop weight tests onto the pads.86 Although not specified, the two pads appear to be designed with both energy shunting and absorbing characteristics. In impact drop weight testing, the pads reduced the forces recorded between the outside and inside of the pads by 87.4% and 84.8% in a .9m drop and 91% and 90.8% in a .6m drop for the firm and soft pads, respectively. The maximum forces transmitted to the skin area over the trochanter versus on the outside of the pad - 21 - Tools for living well: hip protectors were significantly lower. Specifically, the average forces at the skin were 603 +/- 43N (SE reported) and 352 +/- 78N for the firm and soft pads, respectively. The forces on outside surface of the pads ranged between 7031 and 26517 N. Thus, the pads were able to attenuate some of the impact force that would normally be transmitted to the bone. The forces at the bone however were not measured. Thus force attenuation of the femur could not be determined. Moreover, the actual impact forces transmitted to the proximal femur, the direction of force application at the bone, and the state of muscle contraction during the fall were also not controlled or recorded. Laboratory studies have shown that, in general, hip protectors can attenuate some of the forces that would be generated at the hip resulting from an impact due to a fall. However, the amount of reduction depends on the materials, composition and design of the hip protector pad. Moreover, no hip protector can guarantee 100% protection. The greatest amount of protection has been reported from pads that use an energy shunting mechanism. The experimental limitations must be considered when interpreting the results. For example, there are differences in the characteristics of cadaveric and dummy soft tissue relative to real/live tissue, voluntary impacts with the floor may not replicate exactly the impact during an involuntary fall, and younger adults may use different fall mechanisms and have differing tissue responses relative to older adults. Another limitation of these studies is that some were carried out by the manufacturer of the hip protector, and not independent research teams. What hip protectors CAN do: results of clinical studies Randomized controlled trials of hip protector effectiveness with community-living older adults are extremely limited. We present summaries for five studies (more details are provided in Appendix C). Of these, two were strictly community studies while three included participants from the community as well long-term care facilities. In one of the largest studies of community-living older adults, 384 men and women were recruited from orthopedic wards after their first hip fracture or through general publicity about the trial.33 The study was part of a randomized controlled trial of hip protectors. Participants were over 70 years of age, with an intact hip and were able to give informed consent. All participants were living in or were to be discharged from the orthopedic ward to their own home. - 22 - Tools for living well: hip protectors Participants were randomized to either a hip protector or a control group and were followed for approximately 18 months. During the follow-up period, eight hip fractures occurred (the number of falls that occurred during the corresponding period was not reported) - six in the hip protector group and two in the control group. Of note, only one of the fractures in the hip protector group occurred when the participant was actually wearing the hip protectors. The increase in hip fractures among participants in the hip protector group was non-significant. A second randomized controlled trial with 561 primarily institutionalized adults from homes for the elderly and nursing homes included older adults living in apartment houses for the elderly.83 The participants were over 70 years of age with low bone mineral density and at a high risk for falling. Participants were randomized to either a Safehip intervention group or a control group. Of the individuals in the intervention group, 144 were nursing home residents with 132 living in either homes or apartment houses for the elderly (analyses were not performed separately for the two groups). The primary outcome measurement was time to first hip fracture. According to an intention to treat analysis, hip protectors were not effective in preventing hip fractures. However, when a per protocol analysis was performed including only those participants who actually wore hip protectors, a non-significant reduction (23%) in the incidence of hip fractures was observed in the intervention compared with the control group. It is important to note that four persons in the study fractured a hip while wearing the hip protector. The authors reported that the impact efficacy of the studied protectors was less than expected. Kannus et al39 compared the incidence rates of hip fracture (per 1000 person-years) among a group of older adults who were provided with hip protectors versus a control group that were not given hip protectors. All study participants were at high risk for falls with at least one easily identifiable risk factor for hip fracture. The rate of hip fractures among the treatment group was 21.3 versus 46 among control participants. Four participants in the hip protector group had hip fractures (among 1034 falls) while wearing the hip protector (.39 fractures/100 falls) whereas nine had hip fractures while not wearing hip protector (2.43/100 falls). Limited information about a hip protector trial was obtained through an English summary of a Danish thesis.34 The users reported 143 falls with impact on the hip protector. Only two hip - 23 - Tools for living well: hip protectors fractures occurred while the hip protectors were worn. For both of these falls there was no impact on the hip protector. An initial intention-to-treat analysis was performed comparing hip fracture rates in a group of individuals who received hip protectors to hip fracture rates in a group of individuals with no hip protectors. There was no significant difference in the risk of new hip fractures between the intervention and the control group. However, when the authors adjusted for compliance with use, a statistically non-significant reduction of hip fracture risk was found among regular users. Finally, a study by Cameron et al.7 compared rates of falls and hip fractures among older women who were at risk of falling and who were prescribed hip protectors vs similarly at-risk women who were not provided with hip protectors. There was no difference in rate of falls between the two groups, suggesting the wearing of hip protectors does not necessarily increase risk behavior. However, the risk of hip fracture following a fall among those who fell while wearing hip protectors was significantly reduced compared with a fall with no hip protectors (RR = .23, CI: .08-.67). Of note, three participants who fell while wearing hip protectors fractured their hips. In general, these studies suggest that use of hip protectors by people in the community prevents hip fractures if the protectors are worn regularly. However, the relative risk of hip fractures in the hip protector groups versus the control groups were equivocal with one study reporting a significant effect39 and four reporting non-significant differences.7,33,34,83 Variable results may be due to different hip protectors studied, small sample sizes yielding low statistical power and poor compliance for wear. This highlights the multifactorial nature of hip protector efficacy. Specifically, the biomechanics of the devices and their ability to attenuate or decrease the impact at the hip is crucial for fracture prevention. However, the compliance and acceptance of the devices by users are equally important since the hip protectors can only decrease impact forces if they are worn at the time of the fall. More research is needed to better understand the role of hip protectors in reducing hip fractures and factors that influence compliance. What hip protectors CAN do: reduce fear of falling Fear of falling is common among older adults, especially those who have fallen.81 Although the literature on the role of fear of falling and falls is mixed (e.g. see Maki et al.), fear of falling has - 24 - Tools for living well: hip protectors been associated with an increased risk of hip fractures51 and reduced quality of life.49 The potential and benefits of hip protector use to reduce fear of falling has been studied in controlled trials with community-living older adults.9,33,34,54 Cameron et al.9 studied the effect of using hip protectors on fear of falling among older women who were at high risk of hip fracture and who were living in their own homes participated in the study. The women were all over 74 years of age and had either two or more recent falls or one fall requiring hospital treatment. The women were randomly assigned to either an intervention (n=61) or control (n=70) group. Individuals in the intervention group were issued four pairs of Safehip hip protectors. Each individual was tested on falls efficacy when they started and four months after starting the study. The percentage of participants who stated that they were afraid of falling at follow-up was 43% in the hip protector group and 57% in the control group. One proposed confounding factor was that the intervention group received visits from the adherence nurse while the control group did not. The visits alone may have lessened fear of falling. Another study of patients admitted to an orthopedic unit following a fall34 reported that at baseline, nearly one-half of the participants patients reported fear of falling and 40% to 60% of the patients reported restricting their mobility out of home because of the risk of falling. By the third month, about one-third of the users indicated that the hip protectors gave more confidence when walking in and outdoors respectively and 15% had spent more time being outdoors because of the use of hip protectors. These findings suggest that users of hip protectors have less fear of falling. This is important as with lower fear, older adults may be better encouraged to maintain activities of daily living and to continue to enjoy activities outside of the home. As a result, they may become more physically active, require less assistance from others, and enjoy greater independence. Cost effectiveness of hip protectors According to one study, 41 persons would have to wear hip protectors for one year to prevent one hip fracture.39 Only two studies were identified that reported on the cost-effectiveness of hip protector use for older adults. - 25 - Tools for living well: hip protectors In the first study, reported in pounds sterling,41 cost effectiveness was calculated using hip protector compliance and effectiveness data from five randomized studies that were identified in the Cochrane review.68 The cost of hip protectors was obtained from manufacturers. The reduction of hip fractures identified in the five studies reviewed ranged from 6.5% to 2.3%. The average cost to treat hip fractures was reported to be 7200 pounds sterling (CND $16,560). The cost of providing hip protectors based on the provision of three pairs each year for all those who complied with use was calculated to be 113 pounds sterling per year (CND $260). Compliance among institutionalized older adults was estimated to be 36%. They computed from this date that it would cost about 40,680 pounds sterling (CND $9356) per 1000 population/year to provide hip protectors. Results indicated that the cost per fracture prevented using hip protectors, in pounds sterling, was 1827 (CND $4202) for institutionalized older adults; 2485 (CND $5715) for those aged 85 and older, and; 5283 (CND $12,150) for those age 80-84. The cost per fracture prevented for younger age groups was significantly higher, ranging from 9801 (CND 22,545) for those aged 75-79 to 508,500 (CND $ 1,169,550) among those age 50-59. From this study, the authors concluded that for individuals who are 80 years or more and for institutionalized older adults, wearing hip protectors is cost effective. The second study76 reported in US dollars, estimated savings of hip protector use. The study was based on hypothetical cohorts and data inputs collected from secondary sources for men and women over age 65. They assumed a cost of $50 USD for hip protectors per year and 100% compliance with use. Using these estimates, the use of hip protectors among women led to cost savings of $1.215 billion USD, 5,906 fewer hip fracture-related deaths, and 32,000 qualityadjusted-life years. Savings for women were particularly large from the ages of 75 to 84 years. The use of hip protectors among men led to an overall net cost savings of over $135 USD million, 5,962 hip fracture related deaths averted, and a net loss of 25,000 quality-adjusted-lifeyears. However, cost savings were identified only for men over 75 and a net quality-adjustedlife-year was only found beyond age 85. These results were robust to extensive sensitivity analyses that adjusted for different levels of compliance. Based on these findings, the authors concluded that hip protectors are cost-effective for both men and women and may also extend quality-adjusted-life-years for women over 65 and men over 85 years (there was a net loss of - 26 - Tools for living well: hip protectors quality-adjusted–life-years for men under 85 due to inconveniences in wearing hip protectors). To maximize cost-effectiveness, the authors recommended that hip protectors be worn by all women over age 65 and by men over age 85. In sum, only two studies have examined the cost-effectiveness of wearing hip protectors. Both were based on populations of mostly institutionalized older adults. One suggested that for individuals who are 80 years or more and for institutional care patients, wearing hip protectors is cost effective. The other suggested that hip protectors are likely to be cost effective for women over 65 and men over 85. Such limited, and inconclusive research suggests that additional cost effectiveness studies, especially in Canada, are needed. - 27 - Tools for living well: hip protectors WILL COMMUNITY-LIVING OLDER ADULTS WEAR HIP PROTECTORS? Compliance with wearing hip protectors It has been suggested that hip protectors should be used at all times when the person is at risk of falling.82 For many older people, this will mean that the hip protector should be used both during the day and night (to protect the user when getting up at night to go to the washroom). This is problematic, as one study that involved women in focus groups revealed that the majority of the participants indicated that they would not use hip protectors even though half had sustained a hip fracture.8 Controlled studies (detailed in Appendix C) have confirmed that acceptance and compliance with hip protectors is generally poor. In a large primarily community-based study,34 1006 patients from an orthopedic department were offered three pairs of energy dispersing hip protectors. The hip protector used was the Safehip. All participants were followed for 1 to 2.5 years. Compliance with hip protector use was evaluated through questionnaires that were mailed to the participants every 3 months. Primary acceptance of the hip protectors was 57%. At 6 and 12 months following inclusion in the study, 77% and 58% of the participants continued to report regular use. Three other studies of the same hip protector (Safehip) have reported lower rates of acceptance and/or use. One study based on a sample of forty-nine patients with osteoporosis,54 reported an initial acceptance rate of the hip protectors to be 59%. At 6 months, a questionnaire to assess usage rate revealed that compliance with wear had dropped to 35%. In a second study, 83 276 elderly people who lived in a nursing home or community (results are not presented separately for the two groups) were given hip protectors. Compliance with use during unannounced visits was reported to be 61% after 1 month, 45% after 6 months, and 37% after 12 months. At 12 months, fewer than 16% used their hip protectors at night. The third study that randomized 302 at risk seniors to a Safehip hip protector intervention7 encouraged and assessed compliance through visits to the participants by a study “adherence” nurse. Compliance in early phases of the study was 81%. At one year, 57% of participants reported that they wore the hip protector for at least half of every day. Adherence at 18 and 24 months dropped to 50% and 42% of surviving participants. - 28 - Tools for living well: hip protectors A final study39 measured compliance with a different hip protector, the KPH, in a large group of ambulatory but frail elderly adults from community-based healthcare centers in Finland. The participants lived either in geriatric long-stay facilities or had supported living for staying at home (data were not reported separately for the community-living adults only). Of the 1725 participants recruited from community-based health care centers, 650 were randomized to the KPH hip protector intervention group. Initial acceptance to wear the hip protector or willingness to participate by individuals randomized to the intervention group was 69%. Compliance was measured by self-report diary and was reported as the number of days the protector was worn a minimum of one hour as a percentage of all follow-up days. The mean degree of compliance was 48%. Of significant concern, 31% of the subjects who were eligible for the trial refused to wear the hip protector and thus remained without protection. In summary, results of community-based controlled studies suggest that compliance with wearing hip protectors is, for the most part, problematic, with initial acceptance of hip protectors ranging from 57%7 to 69%.39 This suggests that a large proportion of individuals who are at risk of a hip fracture may not wear them at all. Among participants who initially wear hip protectors, compliance tends to drop with time, with noncompliance estimates dropping as low as 35% at 6 months54 to less than 16% compliance with night wear at 1 year.83 Variability in study results may be attributed to varying methodologies used to measure compliance (e.g. diaries, interviews); the assessment of different hip protectors; and differing populations under study. In addition, analysis of compliance differed across different studies, with some assessing compliance based on percentage of time of use and others basing compliance on number of participants who reported regular use. Determinants of hip protector acceptance and use Several studies have explored who, among people at risk for hip fractures, are most likely to accept and wear hip protectors. Results of these studies suggest that determinants and barriers to hip protector use can be categorized as person-based factors, device-based factors, and practical factors related to cost. Person-based factors. In general, and probably due to the added supports offered in the settings, - 29 - Tools for living well: hip protectors individuals living in a care facility are more likely to comply with the use of hip protector than older people living in the community.82 One study found that the acceptance of hip protectors is greater among men,34 although other studies have reported it to be greater among females.61,91 Other characteristics of people that have consistently been found to predict acceptance and/or use of hip protectors include: having a history of or being at risk for hip fractures;34,37,74,80,82,91 mobility problems or frailty;34,74,78,91 history of falling outside of the home,61 and; fear of falling.8,34 In contrast, seniors who have difficulty with toileting, have muscle weakness78 or have dementia are less likely to wear their hip protectors.74 Contradicting other studies, one study reported that people who have experienced one or more falls or are physically inactive and thus at risk for falling had poor compliance with wearing their hip protectors.83 Possibly for these individuals, the hip protectors were “another” indicator of their frailty. Attitudes and beliefs related to falls and hip fractures can influence acceptance and compliance with hip protectors. For example, in one focus group study8 with seniors who had been hospitalized for a fracture, joint replacement or fall, several comments made by participants indicated that participants either did not see themselves at risk of a fracture, or felt that there was nothing they could do to prevent a fracture. Misconceptions about the cause (e.g. belief that the fracture occurs THEN the person falls) of hip fracture are also barriers to use.8 Familiarity with and knowledge of hip protectors and how they work can also influence acceptance and use. In one study,8 seniors indicated that they would be more willing to try hip protectors if they could try them before purchasing them. Beliefs regarding the protective benefits of hip protectors can also influence acceptance and use.6,8,37,53,61 For example, in one study, participants who wore protectors were approximately three times more likely to believe that the hip protectors offered protection from hip fractures as compared to those who did not wear hip protectors (86% versus 30%).53 Another study reported that seniors who attributed a good protective effect to the hip protector were 3.5 times more likely to wear it than individuals with doubts about its protective effect.37 Knowledge (or lack of knowledge) related to how and when to use hip protectors (e.g. whether they should be worn at night) can also influence use.8 Device based factors. A study that asked for seniors’ feedback following a two month trial of wearing hip protectors37 reported that, overall, opinions about the hip protectors tended to be - 30 - Tools for living well: hip protectors negative. In fact, only 25% rated the hip protector as good or very good with almost 50% rating it as poor or very poor. Three major design issues have been identified. These are comfort, appearance, and fit8 Comfort and perceived comfort have been identified as the most important device-based determinants of hip protector use6,37,61,83 - more important than cost or protective effect.79 One study reported that individuals with a positive opinion of hip protector wearing comfort were almost 3 times more likely to wear a protector than those with a negative opinion of comfort.37 This is problematic as the wearing comfort of the hip protector was generally considered to be relatively poor by 70% of participants in that study.37 and others have reported that if uncomfortable, hip protectors are not likely to be worn at night.6 Other studies have reported that participants felt that hip protectors were hot and that the waistband of the undergarments were uncomfortably tight.6,54,78 Features related to appearance include what the garment looks like and how visible it is when worn.6,8,37,61 In terms of the look of the garment, seniors have expressed dissatisfaction related to hip protectors being bulky,54 and to the plastic cover in hard shells. Seniors have also expressed concern that the hip protector undergarments were longer than conventional undergarments, and not very “sexy”.8 Of note, one study8 reported that white was an acceptable color for hip protectors and that soft material was preferred. Hubacher et al.37 reported that seniors who were convinced that the hip protector was not visible from the outside wore it roughly four times longer than persons who did not share this view. Ease of use and fit have also been identified as influencing acceptance and use. In one study, senior hip protector users expressed displeasure with the limited sizes of underwear6 Another study reported that 48% of senior participants rated hip protectors as difficult to get on and off, and 40% felt they would be difficult to put on and take off to use the toilet.53 The difficulty with use was greater during the initial period of the study. Ease of use is especially likely to be a barrier when potential users have multiple disabilities, including incontinence – in this case, hip protectors may be perceived as requiring extra effort in their activities of daily living, in particular toileting, and may lead to loss of independence as more assistance is required.6,8,54 - 31 - Tools for living well: hip protectors Seniors also expressed concern that if the hip pads were not correctly positioned, they may not stay in place and offer protection in the event of a fall.8 Other features related to product design that may diminish acceptance and use include the noise that is made on movement with hard shelled hip protectors56 and ease of, and resilience to, care (i.e. wash and dry).6,8,61 Practical issues. Cost, or perceived cost, of purchasing hip protectors can be a barrier for many older people.6,8,61 Cost, however, is often considered in relation to the attributes of the hip protectors. For example, Telser & Zweifel79 interviewed 522 seniors aged 70 or older who were shown hip protectors and asked how much they would pay for them. Their results suggested that seniors are willing to pay more if hip protectors are comfortable and easy to handle. The extent to which the hip protector protected against a hip fracture was secondary to both comfort and ease of handling. - 32 - Tools for living well: hip protectors ARE THERE SIDE EFFECTS ASSOCIATED WITH HIP PROTECTORS? Few studies with community-living seniors have identified adverse effects associated with hip protector use. In one study,39 of 1725 participants using the KPH hip protector, 15 subjects had skin irritation or abrasion, 1 reported that the protector caused swelling of the legs, 1 reported that it caused bowel irritation. None of the participants reported allergic skin reactions to the device. In another study by Cameron et al.,7 of the 302 participants who wore hip protectors, only 16 (5%) experienced adverse effects. These included minor skin irritations or infection and bruising to upper thigh. Of particular interest, one study cautioned that energy-shunting protectors may influence the risk of other fractures such as pelvic ring or femoral shaft fractures if not worn correctly. 40 This is a particular concern as one study noted that at a one-month follow-up, 13.3% of participants were not wearing their hip protectors properly.82 Incorrect wear was usually wearing the hip protectors backwards or wearing them despite the fact that they had been damaged. And, another study reported that difficulty placing protectors correctly on hips was significantly more common among seniors with high fall risk than the seniors with the low fall risk category.37 Note: studies with people in long-term care facilities have reported pressure ulcers among residents wearing the hip protectors at night. - 33 - Tools for living well: hip protectors SUMMARY, RECOMMENDATIONS AND CONCLUSION In 1993/94 there were 23,375 hip fractures reported in Canada. It is estimated that this figure will increase almost fourfold to 88,124 annually by the year 2041.15 Hip fractures are costly from a health care perspective and from an individual’s perspective. From a health care perspective, we spend an estimated $650 million annually in Canada on hip fractures.88 From the individual perspective, costs include loss in mobility, independence, quality of life, and death. 62 The majority of these fractures are attributed to falls. Although it is unclear how many risk factors need to be present before an individual is at risk of fracturing a hip, the profile of the senior who might be at greatest risk of fracturing a hip suggests that she is female and over age 65. She has a slight build and low body mass (but may be tall), may be frail, and has a maternal family history of hip fracture. She will have lost bone strength due to osteoporosis or some other medical condition or due to lifestyle choices, such as physical inactivity, smoking, or caffeine use. She may have fallen in the past causing a fear of falling which may lead her to alter her gait in such a way that should she fall, she may increase her risk of fracturing her hip. Hip protectors are hip pads designed to decrease the impact to the hip area in the event of a fall and, in the case of energy-shunting protectors, to divert the force from the vulnerable spot (the femoral neck) to less vulnerable areas.60 As little as five years ago there were only a few types of hip protectors on the market and, for the most part, these were viewed as cumbersome, uncomfortable, and socially unacceptable. However, new designs and products are constantly being developed to address various wearer needs and issues. Some models now provide handles for people with arthritis or other restrictions in their hands to facilitate pulling them up or down. Others have Velcro attachments. Still other hip protectors have been developed for people with incontinence allowing for quick removal of the bottom panel for quick relief. Research on the benefits of hip protectors has, until recently, been restricted to residents of longterm care facilities or supportive care. Among this population, the evidence clearly indicates that hip protectors can reduce the risk of hip fracture.68 Similarly, laboratory studies have shown that, in general, hip protectors can attenuate some of the forces that would be generated at the hip - 34 - Tools for living well: hip protectors resulting from an impact due to a fall. However, the amount of impact force attenuation depends on the materials, composition and design of the hip protector pad. The greatest amount of protection has been reported from pads that use an energy shunting mechanism. Because all older adults likely have sufficiently compromised bone strength and other risk factors that put them at risk for a hip fracture,71 and in light of the findings that hip protectors can attenuate the force of a fall, it is compelling to recommend widespread prescription of hip protectors. However, in part due to low power and poor compliance, results of clinical studies with community-living seniors do not unilaterally support the protective benefits of hip protectors in reducing hip fracture risk. Further, the evidence suggests that providing hip protectors to all older adults, while prudent, may not be cost-effective. One cost-effectiveness study suggested that hip protectors be worn by men and women over the age of 80 who are under institutionalized care,41 while another suggested that they are cost effective for women over age 65 and by men over age 85.76 However, given that controlled community studies included in this review restricted their samples to seniors aged 75 or older, further evidence is needed to support either of these recommendations. To be effective, hip protectors must be positioned correctly. In fact, they can carry some risk if not positioned correctly, for example, if an energy-shunting hip protector is applied with the rim on the trochanter, the energy will not be transferred as per the device specification. 50 And, of course, hip protectors can only work if worn. Many community-living older adults are resistant to accepting hip protectors. Long-term compliance with use is also a challenge. In general, people who have a history of or who are at risk for hip fractures, have mobility problems or frailty, have fallen outside of the home and/or exhibit fear of falling are more likely to accept and wear hip protectors. Several person-based, device-based, and practical issues related to cost, especially for seniors living on fixed and limited incomes, will need to be addressed to improve acceptance and compliance with use. - 35 - Tools for living well: hip protectors Recommendations for prescription of hip protectors Results of this review suggest that seniors most likely to benefit from wearing hip protectors are men and women who display multiple risk factors for hip fractures. Risk factors to consider may include various combinations of the following: o advanced age o at risk for falling or fear of falling o low bone density and/or low body mass o frailty o a maternal history of hip fractures o unhealthy lifestyle consisting of one or more physical inactivity, smoking, or caffeine use . It is also recommended that seniors wear hip protectors when conditions increase the risk of falling (e.g. walking for exercise).77 Recommendations for increasing compliance with hip protector use Although no studies were identified that systematically assessed strategies to improved acceptance or compliance with hip protectors, several recommendations can be made based on our knowledge of determinants of use. These include education and awareness, better product designs, cost subsidies, and informal and formal support for use. Education and awareness. Strategies are needed to alter beliefs, attitudes and increase knowledge of hip protectors. Education should adress: a) who is at risk for fractures; b) how to prevent hip fractures; c) hip protectors, what they are, their benefits, proper use, and the importance of wearing the hip protectors at night.8,82 Promotional campaigns should promote hip protectors as a tool to help them maintain their independence and well-being, not as a device for the frail or disabled. Education and communication strategies should be offered at the personal level (e.g. awareness raising, providing education and giving advice through the mediation of family doctors) and - 36 - Tools for living well: hip protectors through mass media advertising.79 Additional measures will also be needed to reach the more isolated at-risk seniors, typically women.83 Better product design. Compliance with hip protectors may be increased by making them more comfortable so people wear them, especially at night.82 Given that perceived comfort and appearance are probably linked, efforts to optimize the feel and appearance of protectors are important. Attention needs to be paid to design to optimize comfort and appearance.8 Washing external hip protectors in a washer and dryer can damage them and increase the risk that an individual will wear them damaged. To improve correct wearing of hip protectors, the front and backside of underpants should be better marked. Of note, although several design aspects have been identified as barriers to the use of hip protectors, modifying the design has significant implications. Specifically, although changes in the design of hip protectors may improve the compliance, the effectiveness of new designs will need to be evaluated.41 Cost Subsidies. Financial incentives to those interested in wearing hip protectors might increase use, especially by making hip protectors free of change (e.g. by including them in obligatory basic insurance or issuing vouchers).79 Lobbying insurance companies to reimburse the cost of hip protectors will be an important strategy to support their use. Support for use. Compliance may also be improved with supervised initial use, for example, while the user is in hospital.8 Encouragement from family members and health professionals, in particular, family physicians is likely to be beneficial.8 Other strategies such as monitoring the use by asking the patient, providing reminders, giving positive reinforcement for use may be useful.8 Finally, follow-up face-to-face and telephone support from an “adherence” nurse to supply and fit the protectors and encouraged their use may improve compliance with use7 who. Recommendations for future research Randomized controlled trials are needed to identify who, among Canadian seniors, might most benefit from hip protectors. These studies will need to employ multivariate designs to ensure control of appropriate potential confounds (e.g. bone strength). - 37 - Tools for living well: hip protectors As products are developed or modified, their efficacy will need to be examined under strict laboroatory conditions. In addition, effectiveness in the field, cost-effectiveness and compliance will need to be evaluated in unbiased, controlled trials. Studies are also needed to better understand and assess interventions to increase acceptance and compliance with hip protector. Conclusion A recent report concluded that initiatives that can reduce hospitalizations due to falls by 20% could lead to 7,500 fewer hospital stays and 1,800 fewer Canadians permanently disabled, with an overall saving of over $138 million annually.31 The data from studies of community-dwelling older adults suggest that hip protectors, in particular protectors that offer both energy absorbing and shunting features, may be beneficial as a fall prevention intervention for women over 65 and men over age 85. The benefits in terms of reduced risk for hip fracture suggest that education and advocacy for greater access and availability to hip protectors are worthwhile endeavors. Concurrent with these efforts, product design and development will need to reflect the varying and changing needs of our senior population. Wearing hip protectors may take a little getting used to, just like wearing a seat belt, a bicycle helmet or eyeglasses. However, in time, hip protectors may become our “Hockey Pads for the game of Life!” - 38 - Tools for living well: hip protectors REFERENCES 1. Aloia, J.F., McGowan, D., Erens, E., Miele, G. (1992). Hip fracture patients have generalized osteopenia with a preferential deficit in the femur. Osteoporosis International,2(2),88-93. 2. Alexander,N.B.(1994). Postural control in older adults. Journal of American Geriatrics Society,42,93-108. 3. American Academy of Orthopedic Surgeons. Falls and hip fractures. Available at: http://orthoinfo.aaos.org/fact/thr_report.cfm?Thread_ID=25&topcateogory=Hip 4. Backman. (1957). The proximal end of the femur. Acta Radiologica (Suppl),146,10-166. 5. Baudoin, C., Fardellone, P., Bean, K., et al.(1996). Clinical outcomes and mortality after hip fracture: a 2-year follow-up study. Bone,18(suppl 3),S149-S157. 6. Birks, C., Lockwood, K., Cameron, I., et al. (1999). Hip protectors: Results of a user survey. Australian Journal on Aging,18,23-6. 7. Cameron, I.D., Cumming,R.G., Kurrle,S.E.,Quine,S., Lockwood,K., Salkeld,G., Finnegan,T.(2003). A randomized trial of hip protector use by frail older women living in their own homes. Injury Prevention,9,138-141. 8. Cameron, I.D., Quine, S.(1994). External hip protectors : likely non-compliance among high risk elderly people living in the community. Archives of Gerontology & Geriatrics,19,273-281. 9. Cameron, I.D., Stafford, B., Cumming, R.G., Birks, C., Kurrle, S.E., Lockwood, K., et al. (2000). Hip protectors improve falls self-efficacy. Age and Ageing,29,57-62. 10. Campbell, A.J., Borrie, M.J., Spears, G.F. (1989). Risk factors for falls in a communitebased prospective study of people 70 years and older. Journal of Gerontology,44,M112-7. 11. Campbell, A.J., Reinken, J., Allan, B.C., Martinez, G.S. (1981). Falls in old age: a study of frequency and related clinical factors. Age and Ageing,10,264-70. 12. Capezuti. (1996). Falls. In lavizzo-Mourey RJ & Forciea MA (Eds) Geriatric Secrets physildelphia PA: Hanley & Belfus,110-5. 13. Charpentier. (1996). A hip protector based on airbag technology. Bone,18(supplement 1),1175. 14. Chrischilles, E.A., Butler, C.D., Davis, C.S., Wallace, R.B. (1991).A model of lifetime osteoporosis impact. Archives of Internal Medicine,151,2026-2032. - 39 - Tools for living well: hip protectors 15. Papadimitropoulos,E.A., Coyte,P.C., Josse,R.G., Greenwood,C.E.(1998). Current and projected rates of hip fracture in Canada[comment]. CMAJ Canadian Medical Association Journal,158(7),870-1. 16. Conner-Kerr,T. (2002).Forgetting the apple: a hip protector a day keeps the doctor away. Wandering/Fall Prevention, July/August,8-10. 17. Cooper, C., Atkinson, E.J., Jacobsen, S.J., et al. (1993). Population-based study of survival after osteoporotic fractures. American Journal of Epidemiology;137,1001-1005. 18. Cree,M., Soskolne,C.L., Belseck,E., Hornig,J., McElhaney,J.E., Brant,R., and SuarezAlmazor,M. (2000). Mortality and institutionalization following hip fracture. Journal American Geriatrics Society,48,283-288. 19. Cummings,S.R. (1985). Are patients with hip fractures more osteoporotic? Review of the evidence. American Journal of Medicine,78,487-494. 20. Cummings & Nevitt. (1989). A hypothesis: the cause of hip fractures. Journal of Gerontology, 44, M107-11. 21. Cummings,S.R., Nevitt,M.C., Browner,W.S., Stone,K., Fox,K.M., Ensrud,K.E., et al. (1995). Risk factors for hip fracture in white women. Study of osteoporotic fractures research group. New England Journal of Medicine,332,767-73. 22. Cummings,S.R., Black,D.M., Nevitt,M.C., et al.(1993). Bone density at various sites for prediction of hip fractures. Lancet,341,72-5. 23. Dias, J.J.(1987). An analysis of the nature of injury in fractures of the neck of the femur. Age and Ageing,16,373-7. 24. Ensrud,K.E., Lipschutz,R.C., Cauley,J.A., Seeley,D., Nevitt,M.C., Scott,J., et al. (1997). Body size and hip fracture risk in older women: a prospective study. Study of Osteoporotic Fractures research Group. American Journal of Medicine,103,274-80. 25. Flicker,L., Faulkner,K.G., Hopper,J.L., Green,R.M., Kaymacki,B., Nowson,C.A., et al. (1996).Determinants of hip axis length in women aged 10-89 years: a twin study. Bone,18,41-5. 26. Fuller. (2000). Falls in the elderly. American Family Physician,61,2159-68, 2173-4. 27. Grisso, et al.(1991). Risk factors for falls as a cause of hip fracture in women. New England Journal of Medicine,324,1326-31. 28. Hall, S.E., Williams, J.A., Senior, J.A., Goldswain, P.R., Criddle, R.A.(2000). Hip fracture outcomes: quality of life and functional status in older adults living in the community. Australian and New Zealand Journal of Medicine,30(3),327–32. - 40 - Tools for living well: hip protectors 29. Hayes, et al.(1991). Relative risk of fall severity, body habitus and bone density in hip fracture among the elderly. Orthop Research Society Trans,16,139. 30. Hayes,W.C., Myers,E.R., Morris,J.N.,Gerhart,T.N., Yetts, H.S., Lipsitz,L.A. (1993). Impact near the hip dominants fracture risk in elderly nursing home residents who fall. Calcif Tissue International, 52,192-8. 31. Health Canada.(2003). The economic burden of unintentional injury in Canada. Available at:www.hs-sc.gc.ca/pphb-dgspsp/injury-bles/ebuic-febnc/index.html. 32. Heikinheimo, R., Jantti, P., Aho, H., Maki-Jokela, P.L.)1996). To fall but not to break – safety pants. Bone,18 (suupl 1),117S. 33. Hildreth, R., Campbell, P., Torgerson, I.(2001). A randomized controlled trial of hip protectors for the prevention of second hip fractures. Osteoporosis International,12,S13. 34. Hindso, K.(1998). Prevention of hip fractures using extermal hip protectors. Risk factors for falls, hip fractures, and mortality; and evaluation of the consequences of fear of falling among older orthopaedic patients. A clinical controlled open intervention study including 1684 patients, older than 74 years of age, followed for 1-2.4 years after admittance to one of two university hospitals in Copenhagen. PhD thesis, University of Copenhagen. 35. Hipp, J.A., Myers, E.R. Greenspan, S.L., et al, (1991). Soft tissue thickness and energy absorption capacity as potential determinant of hip fracture risk. Trans Orthopaed Research Society,16,135. 36. Horak,F.B., Shupert,C.L., Mirka,A. (1989). Components of postural dyscontrol in the elderly: a review. Neurobiology Aging,10,727-738. 37. Hubacher, M., Huguenin, R.D. (2000). The acceptance of hip protector by senior citizens aged over 70 living at home. English abstract of German technical report 38. Jacobsen,P.C., Beaver,W., Grubb,S.A., et al. (1984). Bone density in women: college athletes and older athletic women. Journal of Orthopedic Research,2,328-332. 39. Kannus, P., Parkkari, J., Niemi, S., et al,(2000). Prevention of hip fracture in elderly people with use of a hiop protector. New England Journal of Medicine,343,1506-13. 40. Kannus, P., Parkkari, J., Poutala, J. (1999). Comparison of force attenuation properties of four different hip protectors under simulated falling conditions in the elderly: an in vitro biomechanical study. Bone, 25,229-235. 41. Kumar, B.A., Parker, M.J. (2000) Are hip protectors cost effective? Injury, International Journal of the Care of the Injured,31,693-695. - 41 - Tools for living well: hip protectors 42. Laurintzen, J.B. (1997). Hip fractures: epidemiology, risk factors, falls, enery absorption, hip protectors and prevention. Danish Medical Bulletin,44,155-168. 43. Lauritzen & Askegaard. (1992). Protection against hip fractures by energy absorption. Danish Medical Bulletin,39,91-3. 44. Lauritzen,J.B.. (1996). Hip fractures: incidence, risk factors, energy absorption, and prevention. Bone, 18,65S-75S. 45. Lauritzen, J.B. & Lund, B. Padding of the hip and protection against hip fractures. Chapter 8 Osteroporotic fracture: epidemiology and risk factors. 46. Lauritzen, J.B., McNair, P.A., Lund, B. (1993). Risk factors for hip fractures. Danish Medical Bulletin,40,479-485. 47. Lauritzen, J.B., Pertersen, M.M., Lund, B. (1993), Effect of external hip protectors on hip fractures. The Lancet,341,11-13. 48. Law, M.R., Walk, N.J., Meade, T.W. (1991). Strategies for prevention of osteoporosis and hip fracture British Medical Journal,303,453-459. 49. Lawrence, R.H., Tennstedt,S.L., Kasten,L.E., Shih,J., Howland,J., and Jette,A.M. (1998).Intensity and correlates of fear of falling and hurting oneself in the next year. Journal of Aging and Health,10(3),267-286. 50. Lips, P., & Ooms,M.E. (2000) Non pharmacological interventions. Bulliere’s Clinical Endocrinology & Metabolism,14,265-277. 51. Luukinen,H., Koski,K., Laippala,P., and Kivela,S. (1997). Factors predicting fractures during falling impacts among home-dwelling older adults. Journal of American Geriatrics Society,45,1302-1309. 52. Magaziner, J., Simonsick, E.M., Kashner, M., et al.(1989). Survival experience of aged hip fracture patients. American Journal of Public Health,79,274-278. 53. McAughey, J.M.(2002). Acceptability of hip protectors. Available at: http://bmj.com/eletters/324/7334/375. 54. McAughey,M., and McAdoo,M. (2002). Acceptability of hip protectors. British Medical Journal, 324,375. 55. McLaren, M.I., Cooper, C.(1989). Bone mass in women with hip fractures. Annals of the Royal College of Surgeons of England,71(2),77-8. - 42 - Tools for living well: hip protectors 56. Melton, L.J., Wahner, H.W., Richelson, L.S., O'Fallon, W.M., Riggs, B.L. (1986). Osteoporosis and the risk of hip fracture. American Journal of Epidemiology, 124,25461. 57. Meltzer, M., Lessig, H.J., Siegel, J.A.(1989). Bone mineral density and fracture in postmenopausal women. Calcified Tissue International, 45(3),142-5. 58. Merilainen, S., Nevalainen, T., Luukinen, H., Jalovaara, P. (2002). Risk factors for cervical and trochanteric hip fracture during a fall on the hip. Scandinavian Journal of Primary Health Care,20,188-192. 59. Meyer, H.E., Tverdal,A., Falch,J.A. (1993). Risk factors for hip fracture in middle-aged Norwegian women and men. American Journal of Epidemiology,137,1203-11. 60. Mills, N.J. (1996). The biomechanics of hip protectors. Journal of Engineering in Medicine,210,259-266. 61. Myers,A.H., Michelson,J.D.,Van Natta,M., et al. (1995). Prevention of hip fractures in the elderly: receptivity to protective garments. Archives Gerontological Geriatrics,21,179-89. 62. National Osteoporosis foundation.(2001). Disease Statistics. http://www.nof.org/osteoporosis/stats.htm 63. Nelson,H.D., Nevitt,M.C., Scott,J.C., Stone,K.L., Cummings,S.R. (1994). Smoking, alcohol, and neuromuscular and physical function of older women. Journal of American Medical Association,272,1825-31. 64. Nevitt, M.C., Cummings, S.R. (1993).Type of fall and risk of hip and wrist fractures: the study of osteoporotic fractures. The Study of Osteorporotic Fractures Research Group. Journal of American Geriatrics Society,41,1226-1234. 65. Nilsson,B.E..and Westlin, N.E.(1977).Bone mineral content and fragility fractures. Clinical Orthopaedics & Related Research, 125,196-9. 66. Office of Technology assessment (1993).Hip fracture outcomes in people age 50 and over: mortality, service use, expenditures, and long-term functional impairment. Washington, DC: Office of Technology assessment, Congress of the United states. US Dept of Commerce Publication NTIS PB94107653. 67. Pakkari, Kannus, Poutala. (1994). Vouri Force attenuation properties of various trochanteric padding materials under typical falling conditions of the elderly. Journal of Bone & Mineral Research,9,1391-1396. 68. Parker,M., Gillespie,L., & Gillespie,W. (2003). Hip protectors for preventing hip fractures in the elderly. The Cochrane Database of Systematic Reviews, 1-28. - 43 - Tools for living well: hip protectors 69. Poor, G., Atkinson, E.J., O’Fallon, W.M., Melton, L.J. III. (1995). Determinants of reduced survival following hip fractures in men. Clinical Orthop,319,260-265. 70. Riggs, B.L., Wahner, H.W., Seeman, E., Offord, K.P., Dunn, W.L., Mazess, R.B., Johnson, K.A., Melton, L.J. (1982). Changes in bone mineral density of the proximal femur and spine with aging. Differences between the postmenopausal and senile osteoporosis syndromes. Journal of Clinical Investigation,70,716-23. 71. Robinovitch, Hayes & McMahon. (1991). Prediction of femoral impact forces in falls on the hip. Journal of Biochemical Engineering,113,366-74. 72. Robinovitch, S.N., Hayes, W.C., McMahon, T.A. (1995). Energy-shunting hip padding system attenuates femoral impact force in a simulated fall. Journal of Biomechanical Engineering,117,409-413. 73. Robinovitch, S.N., Hsiao, E.T., Sandler, R., Cortex, J., Liu, Q., Paiement, G.D. (2000). Prevention of falls and fall-related fractures through biomechanics. Exercise and Sport Sciences Reviews,28,74-79. 74. Ross,J., Woodworth,G.W., Wallace, R.B. (1996). Compliance by elderly in wearing hip joint protectors. Paper presented at the Third International Conference on Injury Prevention and Control, Melbourne, Australia. 75. Salkeld, G., Cameron, I.D., Cummings, R.G., Easter, et al.(2000). Quality of life related to fear of falling and hip fracture in older women: A time trade off study/Commentary. British Medical Journal, 320,341-346. 76. Segui-Gomez, M., Keuffel, E., Frick, K.D. (2002). Cost and effectiveness of hip protectors among the elderly. International Journal of Technology Assessment in Health Care,18,55-66. 77. Slemenda,C. (1997). Prevention of hip fractures: risk factor modification. The American Journal of Medicine,103(2A),65S-71S. 78. Suzuki,T., Yoshida,H., Ishizaki,T., et al. (1999). Compliance in use of external protectors for hip fractures among the community elderly in Japan [in Japanes]. Nippon Ronen Igakkai Zasshi,36,40-4. 79. Telser, H. & Zweifel, P. (2000). Pravention von schenkelhalsfracturen durch huftprotektoren: Eine okonomische analyse bfu-Report 46. 80. Thompson,P.W., Jones,C. (2000). Adherence to hip protector use in elderly people requiring domiciliary care is greater in fallers than non-fallers. Age and Ageing, 29,459. - 44 - Tools for living well: hip protectors 81. Tinetti, M.E., Richman, D., Powell, L. (1990). Falls efficacy as a measure of fear of falling. Journal of Gerontology,45,P239-243. 82. Van Schoor, N.M., Deville, W.L., Bouter, L.M., Lips, P. (2002). Acceptance and compliance with external hip protectors: A systematic Review of the Literature. Osteoporosis International,13,917-924. 83. Van Schoor, N.M., Smit, J.H., Twisk, J.W.R., Bouter, L.M., Lips, P. (2003). Prevention of hip fractures by external hip protectors: a randomized controlled trial. Journal of American Medical Association,289,1957-1962. 84. Villar, M.T.A., Hill, P., Inskip, H., Thompson, P., Cooper, C. (1998).Will elderly rest home residents wear hip protectors? Age and Aging,27,195-8 85. Weaver,J. (2000). Unsafe home environment is not leading cause of falls among elderly, study finds. Yale Bulletin & Calendar, 29(13). http://www.yale.edu/opa/v29.n13/story14.html. 86. Weiner, S.L., Andersson, G.B.J., Nyhus, L.M., Czech, J. (2002). Force reduction by an external hip protector on the human hip after falls. Clinical Orthopaedics and Related Research,398,157-168. 87. Wicks, et al. (1982). Absence of metabiolic disease in the proximal femur in patients with fracture of the femoral neck. Journal of Bone Joint Surg BR,64,319-22. 88. Wiktorowicz, M.E., Goeree,R., Papaioannou,A., Adachi,J.D., and Papadimitropoulos,E. (2001). Economic implications of hip fracture: health service use, institutional care and cost in Canada. Osteoporosis International,12,271-278. 89. Wilkins, K. (1999). Health care consequences of falls for seniors. Health Reports,10(4). Statistics Canada, Catalogue 82-003. 90. Wolinsky, F.D., Fitzgerald, J.F., Stump, T.E. (1997).The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. American Journal of Public Health,87(3),398–403. 91. Zimmer,Z., Myers,A. (1997). Receptivity to protective garments among the elderly. Journal of Aging Health,9,355-72. - 45 - Tools for living well: hip protectors APPENDIX A: List and description of hip protectors - 46 - Tools for Living Well: Hip Protectors Hip Protector Hip Belt Brief Guard Safe Hip underwear Safe Hip underwear Belt HARD Shell SOFT Shell Approx. Purchase Price Suggested Retail Price $105 Hip Guard Anne Kovin, President Phone: 1-800-299-8892 www.hipguard.net info@hipguard.net $75 $115 Hip Guard Anne Kovin, President Phone: 1-800-299-8892 www.hipguard.net info@hipguard.net $110 Not Available $59.99 N/A $59 Energy Shunting SEWN IN Energy Shunting SEWN IN Contact Information Energy Shunting Regency Medical Supplies (Burnaby, BC) Allaster Campbell 1-604-434-1383 www.regencymed.com SEWN IN Hip Saver underwear Energy Shunting & Energy Absorbing - 47 - (Does not sell to retailers) Help Mates Karen Brown, President Phone: 1-888-771-0977 www.hipsaver.ca kbrown@helpmates.on.ca Tools for Living Well: Hip Protectors Hip Protector Brief Belt HARD Shell SOFT Shell Approx. Purchase Price Suggested Retail Price $65 $95 Contact Information REMOVABLE Hip Shield HIPS Hip System Protection REMOVABLE Energy Shunting HIPS Hip System Energy Shunting & Energy Absorbing Protection $110 (Discount may apply) Not Available $110 Not Available Energy Shunting REMOVABLE Pro-Hips Energy Shunting & Energy Absorbing - 48 - $55.65 ERP Group Maria Di Pasquo Phone: 1-800-361-3537 www.erp.ca Ladies Item# ERP6672-12 (size small) -13/14/15 (other sizes) Men’s Item# ERP6672-02 (size small) -03/04/05 (other sizes) REMOVABLE Professional Orthopedic Products Martin Paul Onrot Phone: 514-484-4441 martinonrot@sympatico.ca $79.50 Regency Medical Supplies Burnaby, BC Allaster Campbell 1-604-434-1383 www.regencymed.com D.R. Médical 1-888-268-0778 www.dr-medical.com Briefs come in four colours: white, black, grey & beige Tools for Living Well: Hip Protectors Hip Protector Brief Belt HARD Shell SOFT Shell Approx. Purchase Price Suggested Retail Price $55.00 Not Available REMOVABLE Gerihip brief Energy Absorbing Energy Absorbing $54.20 $93.50 Catalogue #6016 – Standard Brief Catalogue #6017 – Incontinent Brief Catalogue #6018 – Male Fly Brief SEWN IN Rite- Fit Hip Protection Garment Impactwear Hip Protectors Energy Shunting & Energy Absorbing REMOVABLE Energy Shunting - 49 - Geriatric Protection Products Jeff Elstad 1-800-234-8291 www.preventproducts.com jeffe@preventproducts.com Canadian Hospital Specialties 1-905-825-9300 www.chsltd.com SEWN IN Posey Hipsters Contact Information $48.00 Not Available Invacare Supply Group 1-800-225-4792 www.invacaresg.com (Item #00979) $86.75 $115 Impact Body Wear Ltd. Ellaine Gallagher, President 1-250-474-5535 www.impactbodywear.com impactbodywear@shaw.ca Tools for Living Well: Hip Protectors Hip Protector Briefs Belt HARD Shell SOFT Shell Approx. Purchase Price Suggested Retail Price SEWN IN OR REMOVABLE Safety Pants http://www.raunomo .fi/index.htm $79.00 $118 Energy Absorbing Contact Information Impact Body Wear Ltd. Ellaine Gallagher, President 250-474-5535 www.impactbodywear.com impactbodywear@shaw.ca Does not sell to Canada REMOVABLE KPH Protector Hip Hornsby Healthy Hips Energy Shunting SEWN IN OR REMOVABLE Energy Shunting HIProtector 1-800-930-9255 www.hipprotector.com Cannot be sold in Canada Phone: +61 2 9477 9768 Fax: +61 2 9477 9105 klockwoo@doh.health.nsw.gov.au Notes: Information presented in this list was obtained by the manufacturers. Information has not been objectively evaluated for this project. This list may not be complete and will need to be updated periodically, as new products are manufactured. Costs are suggested costs as of Autumn, 2003. Assistive Devices to Help Prevent Falls. A joint venture between the University of Ottawa and the Canadian Association of Occupational Therapists (CAOT). For more information about this project please contact the CAOT at 613-523-2268 or www.caot.ca Funding provided by Health Canada/Veterans Affairs Canada Falls Prevention Initiative. - 50 - Tools for Living Well: Hip Protectors APPENDIX B. Demographic, health, lifestyle, and psychological risk factors for hip fractures - 51 - Tools for Living Well: Hip Protectors Study Risk factor for hip fracture OR / RR reported CI (95%) Merilainen et al., 2002 Normal or excess body weight OR: .93(cervical fracture) OR: .94 (trochanteric fracture) 0.91-0.96 0.91-0.96 Being tall OR: 1.1 (cervical fracture) OR: 1.1 (trochanteric fracture) 1.1-1.2 1.1-1.1 Inability to walk alone outdoors OR: 2.8 (cervical fracture) 1.4-5.8 Presence of respiratory disease OR: 4.3 (cervical) OR: 3.4 (trochanteric fracture) 1.7-11.0 1.3-8.6 Fear of falling OR: 2.5 1.1-5.6 Reduced knee strength OR: 3.4 1.0-11.4 Poor visual acuity 3.5 1.1-10.6 Height 1.5 1.2-2.2 Tricep weakness (based on isokinetic Dynamometer) 1.7 1.2-2.5 Advanced age** RR: 1.5 1.3-1.7 Maternal family history of hip fracture** RR: 2.0 1.4-2.9 Weight increase since age 25** RR: 0.6 0.5-0.7 Tall height at age 25** RR: 1.2 1.1-1.4 Self-rated good health RR: 1.7 1.3-2.2 History of hyperthuroidism** RR: 1.8 1.2-2.6 Use of benzodiazapines** RR: 1.6 1.1-2.4 Use of anticonvulsants RR: 2.8 1.2-6.3 Use of caffeine** RR: 1.3 1.0-1.5 Walking for exercise** RR: 0.7 0.5-0.9 On feet < 4 hrs/day** RR: 1.7 1.2-2.4 Luukinen et al., 1997 Nevitt & Cummings, 1993 Cummings et al. 1995 - 52 - Tools for Living Well: Hip Protectors Meyer et al.1993 Hindson, 1998 Inability to rise from chair** RR: 2.1 1.3-3.2 Poor depth perception** RR: 1.5 1.1-2.0 Resting pulse rate > 80** RR: 1.8 1.3-2.5 Low-frequency contrast sensitivity** RR: 1.2 1.0-1.5 Being tall * Women: RR: 1.6 Men: RR: 2.2 Women: 1.2-2.1 Men:1.5-3.3 Advanced age Women: RR: 1.9 Men: RR: 1.7 Women:1.6-2.4 Men:1.2-2.3 Normal or high body mass index Women: RR: .58 Men: RR: .30 Women: .36-.92 Men: .12-.79 Diagnosis of diabetes mellitus* Women: RR: 9.2 Men: RR: 9.4 Women: 3.4-24.5 Men: 2.9-30.5 History of cerebral stroke Men: RR: 10.2 Men: 1.4-75.8 Gender male OR: .80 N/a Advanced age OR: 1.5 N/a Diagnosis dementia OR: 2.6 N/a Diagnosed medical conditions OR: 1.8 N/a Experiencing dizziness OR: 1.4 N/a Tobacco use OR: 1.6 N/a RR: Relative Risk; OR: Odds ratio – numbers greater than one indicate degree of elevated risk, numbers lower than one indicate lower risk (that is, the opposite condition would be considered a risk factor). * Significance persisted in age-adjusted analyses ** Significance persisted after history of fracture and bone density added to the model, suggesting that their impact is not due to their impact on bone density. - 53 - Tools for Living Well: Hip Protectors APPENDIX C: Results of community-based randomized controlled clinical trials on effectiveness of and compliance with hip protectors - 54 - Tools for Living Well: Hip Protectors Author/date Cameron et al 7 Study Hip protector population used 600 women Safehip aged 74 years + with two or more falls or one fall requiring hospital admission in last year living in own homes (n=302 allocated to HP group) Effect Compliance No significant difference in number 3 subjects refused to wear HP at study onset. of falls, multiple falls, fall induced injuries requiring hospital care Initial non-adherence at early stage of study = 19%. between groups. Adherence with hip protector use at one year: 57% Significantly lower risk of hip of participants reported that they wore protector for fracture from fall while wearing at least half of every day. versus not wearing HP (Relative risk = .23: 95% CI = .08 to .67). Adherence at 18 and 24 months dropped to 50% Using intention to treat analysis and 42% of surviving participants. however there was no significant difference in incidence of hf between groups (RR 0.92: 95% CI 0.51 to 1.68). Three hf occurred while wearing HP: two during a fall backwards, one during motor vehicle accident Hip protectors were in place in 51% of falls in intervention group CONCLUSION FROM STUDY: When hip protectors are work there is a prevention effect (comparison between wearers and non-wearers). But, effectiveness is not supported between groups probably due to the lack of adherence, the inability of HP to prevent hf in a few cases and the limited numbers. - 55 - Tools for Living Well: Hip Protectors McAughey & 49 community McAdoo54 residents Hildreth et al. 33 384 men and women 70 years or older, recruited from orthopedic ward after first hf or from general study announcements, living in or to be discharged to own home Van Schoor et 561 elderly al. 83 persons from apartment houses for the elderly, homes for the elderly and nursing homes assigned to HP (n= 276) or control (n = 285) group by individual randomization. 144 individuals in intervention group lived in nursing home. Specific numbers in Safehip Not reported Initial acceptance = 59% 6-month acceptance = 35% During 18 month follow-up period, 8 Wear compliance = 63% at 6 weeks but only 40% hf with 6 occurring in HP group (one of individuals wearing HP every day. while participant wearing HP). The increase in hf in HP group was nonsignificant. Safehip (energy shunting type consisting of two shellshaped protectors sewn into underpants Adjusted analysis – no significant difference between participants from intervention and control groups found with regard to time to first hip fracture (hazard ratio, 1.05; 95% CI, 0.55 – 2.03). Per protocol analysis comparing 78 compliant participants in intervention group to 281 control participants – fracture rates were 3.9/100 personyears and 5.1/100 person-years . After adjusting for confounds, intervention group had a 23% lower probability of hf than control (not statistically significant with hazard ratio, 0.77; 95% CI, 0.25 – 2.38) All data combined across residential - 56 - Compliance with HP at unannounced visits = 61% after 1 month, 45% after 6 months, and 37% after 12 months (for a subject sample of 217, 246, 230 at 1, 6, and 12 months respectively). Fewer than 16% used HP at night. Tools for Living Well: Hip Protectors Kannus et al. 39 Hindso 34 apartment housed not specific. Participants aged 70 or older, low bone density and/or a high risk for falls (n= Living arrangements: a) Communitybased health care centers HP: n=406 C: n= 674 b) Supported home living HP: n= 247 C: n= 474 status. KPH protector (energyshunting) All subjects aged at least 70 years, ambulatory (assisted or unassisted) and had at least one identifiable risk factor for hip fracture 1684 patients Safehip admitted to two Hip 1404 falls in HP group with 1034 Initial decline to participate after hearing about occurring while participant was study wearing HP HP group= 31% C group = 9 % Rate of Hip fracture HP= 46 (per 1000 person/years) Degree of compliance (# days HP worn as % of all C=21.3 (per 1000 person/years) follow-up days) = 48 +/- 29% Relative hazard of hip fracture (HP vs C group) = .4 (95% CI = .2 to .8) (significant decrease in relative risk for HP group) 4 hip fractures in HP groups while wearing HP with 9 fractures in HP groups while not wearing HP (relative hazard of hip fracture while wearing device = .2; 95% CI = .05 to .5%)** ** not clear whether fractures occurred in community or LTC residents Intention to treat analysis of risk for Primary acceptance of HP = 57%. Acceptance was new hf in intervention and control higher in men (64%) and in individuals admitted - 57 - Tools for Living Well: Hip Protectors orthopedic group showed no effect of HF after a hip fracture (65%). At 6 and 12 months, departments (adjusted incidence ratio: 1.1; 95% 77% and 58% were still registered users of HP. (n=1006 in HP CI: 0.7 - 1.8). group). Women accounted for After adjusting for use of HP 81% and 92% (treatment received analysis) a of participants statistically non-significant reduction lived in their of hip fracture risk was related to use own homes. A of HP (RR: 0.88; 95% CI 0.5 – 1.5). fall preceded admittance in Users reported 143 falls with impact 1170 cases and on the HP. Two hf occurred while 543 individuals hip protectors were worn although in has sustained a neither case was an impact on the HP hf prior to the observed. study. Participants were over 74 years of age. Abbreviations: hf, hip fractures, HP, hip protectors - 58 -