Why we did not adopt PBL? - Joint Master of Health Professions
advertisement

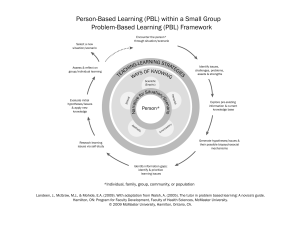
Proceedings: 7th Asian- Pacific Conference on PBL, 2008 PBL in Health Professions Education, Why and why not: FAIMER Fellows' Perspective Wagdy Talaat, MD, Ph.D.; Stewart Mennin, Ph.D.; Si Mui Sim, Ph.D.; Yucel Gursel MD, Ph.D.; Naranchimeg Sodovsuren MD, Ph.D.; Kofo Soyebi, MD, FWA,CS,FMCI; & Elena Barragnan, MD, Ph.D. Abstract A group of 2006 and 2007 International FAIMER (Foundation for Advancement of Medical Education and Research) Fellows explored online issues related to the adoption of PBL in their institutions. The theme of web discussion was focused on two questions: 1) If you are using PBL at your school, what are the challenges and issues you and your colleagues faced as you implemented and continued to use PBL? (2) If you are not using PBL at your school, or are contemplating using it and have not yet implemented it, what are the issues and concerns of teachers about PBL that made it not possible at this time to be used? About thirty percent of the fellows (n=43) responded to the first question and 69.7% responded to the second question. Analysis of the responses revealed issues of cost, faculty development and resources are major impediments to adoption of PBL. The attraction of more students-centered, self-directed learning was common. Different strategies for implementing PBL among the respondents were also common. Key words: Education, medical, Problem-Based Learning, curriculum strategy, FAIMER. Correspondence: Wagdy Talaat, MD, PhD. Department of Medical Education, Faculty of Medicine, University of Suez Canal, Ismailia 41111, Egypt. E-mail: watalaat@gmail.com Introduction The Foundation for Advancement of International Medical Education and Research (FAIMER) is a non-profit foundation committed to improving world health through education. It was established in 2000 by the Educational Commission for Foreign Medical Graduates (ECFMG®). In partnership with ECFMG, FAIMER promotes excellence in international health professions education through programmatic and research activities. FAIMER's fellowship programs are targeted to international health professions education faculty who have the potential to play key roles in improving education in their schools. These programs develop skills that allow participants to serve as resources for their colleagues, institutions, local communities, and global regions. The programs emphasize education methods, education leadership and management, and development of a community of educators. Participants focus on education innovation projects of their choosing that are supported by their home institutions1. An integral part of distance learning program at FAIMER is to be involved in Mentoring and Learning Web discussions (ML Web) on monthly basis. On January 2008, the theme of the ML 1 Web discussion was Problem-Based Learning (PBL) in Health Professions Education: what, why, and how. Two questions formed the basis of the discussion. (1) If you are using PBL at your school, what are the challenges and issues you and your colleagues faced as you implemented and continued to use PBL? (2) If you are not using PBL at your school, or are contemplating using it and have not yet implemented it, what are the issues and concerns of teachers about PBL that made it not possible at this time to be used? Methods This study was carried out on 43 International FAIMER fellows from classes of 2007 and 2006 that represent 15 countries in Africa, Asia, and Latin America and FAIMER international faculty. Data were collected from the fellows through ML Web discussions over one month that started December 25th, 2007 and ended January 25th, 2008. To prepare for the discussion and extraction of results, a couple of relevant articles were posted at the beginning for awareness and terminology definition. Upon slowing down of discussion more provocative questions were asked to keep the heat up and extraction of more in depth information. All participants were encouraged to participate either by inquiring or answering peer inquires. The discussion leaders were following the online discussion on daily basis and were commenting on each point then provided a final summary by the end of the whole discussion. Results During this PBL ML Web discussion, 138 responses were received from 43 FAIMER fellows and faculty with an average of 3.2/participant. Most of the participants reported that they enjoyed the discussions and benefited from the depth of information provided. Some fellows indicated that they were more encouraged to try PBL. Out of the ML Web discussion, the list of topics, in the order of interest was: Costs of PBL and its required resources. Concepts and rationale of PBL. Pre-requisites for adopting PBL. Background of students before admission to PBL schools. Different ways of implementing PBL. Advantages and disadvantages of PBL. Evaluation of students and faculty in PBL. Comparison between graduates of PBL versus graduates of traditional curricula. Most of these topics will be discussed in relevance to the main research questions that have been addressed at the beginning of this article. Why we did not adopt PBL? Thirty fellows who constituted the majority of respondents (69.7%) reported different reasons for not adopting PBL as an educational strategy in their institutions. The following points were frequently addressed during the web discussion and listed below according to the order of frequency: PBL is costly and resource demanding in terms of finance, large number of classrooms for small group tutorials, human resources working as curriculum designers, block planners, problem/case designers, coordinators, class tutors, and seminars moderators (80%). Large number of students compared to number of faculty (66.6%). Lack of competent trainers both at the local and national levels (66.6%). Lack of sufficiently persuasive evidence regarding difference in educational outcomes studied (60.0%). 2 Power struggle between change advocates and resistant faculty who deny the need for change and are reluctant to move out of their comfort zone (60.0%). Lack of maturity of entry students with diverse backgrounds to be able to handle their own learning (40.0%). Lack of political will to depart from the traditional discipline-based form of teaching/learning (33.3%). Lack of motivation of the staff to develop the intellectual materials required (cases, etc.) (26.6%). "We followed the British Curriculum, when there was no PBL" (a comment by Indian and Pakistani fellows) (10.0%). Why we adopted and implemented PBL? Those fellows whose institutions adopted PBL, either partially or fully constituted a minority among the respondents (30.3%). The reasons given why PBL was adopted were: It promotes active and self-directed learning (100%). It emphasizes peer learning (100%). Students learn to articulate their knowledge well and are confident and professionally fluent (100%). It focuses on acquiring competencies rather than the mere recall of knowledge (100%). It gives students direct responsibility for their own learning (76.9%). It reverts medical education to the natural whole by integrating the medical sciences away from the artificial separation (76.9%). It encourages students to practice critical thinking and clinical reasoning (76.9%). It makes the learning process more fun (53.8%). It brings relevance to medical education (53.8%). Students are better able to engage in a clinical conversation by the time they get to the clinical clerkship years (30.7%). It produces competent doctors with a holistic approach to the practice of medicine (30.7%). In response to the current fashion in innovation (one response). How we implemented PBL? As an educational strategy, PBL was implemented by the FAIMER fellows in their own institutes as in the following formats: - PBL concepts were implemented in the pre-clinical phase and considered clinical training to be problem-based by its very nature (15.3%). - A Hybrid PBL strategy was adopted in the pre-clinical years (30.7%). - A pure PBL strategy was adopted in the pre-clinical phase (15.3%). - A pure and full PBL strategy was implemented across the whole curriculum (23.0%). - A pure and full PBL strategy was implemented in conjunction with another innovative strategy: Community-Based Education across the whole curriculum (15.3%). Discussion Issues of cost and resources dominated the discussion of why PBL was not adopted at fellows’ institutions. Issues of cost often focus around the absolute amount of resources available and it is rare to find discussions or literature examining the question of how existing resources could be redistributed to support innovations such as PBL. There remain some questions about this in the literature2, 3 although there are only three studies with data that show that up to a class size of 100 students, the human, physical, technical, and financial resources are different but not necessarily more costly4, 5, 6. Reasons for the different perspectives in the literature remain to be clarified. The discussion about sufficiently prepared teachers to support a PBL curriculum addresses a critical issue. Faculty development in most medical schools in the 3 world is not well supported or attended. What is required in PBL are teachers with skills and knowledge in facilitating smallgroup, self-directed learning. This requires an initial investment of time and energy and many institutions are either unprepared to make such an investment or lack the skilled personnel to undertake it. The principal reasons given for adopting PBL center are the increase in relevance, activation and stimulation of student learning. The limitations with this study include the fact that we did not collect data on when the PBL programs were implemented or considered and what was going on at the institutions and in the regions that might have influenced their decisions. This would be of interest to follow up. It seems that the implementation of pure PBL programs and parallel tracks that marked the early years of PBL is not being sustained in the institutions represented by the Fellows in this study. Many assume this approach to learning is extensively time consuming and too expensive compared to the traditional forms of medical education4. An interesting result that was driven from the discussion about the adopted strategies for implementing PBL was the prevalence of hybrid curricula among PBL medical schools. On depth discussions about this point revealed different styles of implementing hybrid PBL. It seems that the term "hybrid" in PBL means different things to different people. As long as it seems to become more popular compared to "pure" PBL, it is about time to work on some definitions and processes that limit the vagueness of such strategy and possible misconceptions. Another interesting argument about why PBL was not adopted that says "We followed the British Curriculum, when there was no PBL". During the discussion, the point was made that the British themselves have reformed their curriculum introducing innovation, integration, and problem-oriented learning. Many reasons had been given to explain why PBL was addressed. Most of these reasons were acknowledged by researchers except a few like the one that says “Produces more competent doctors with a holistic approach to the practice of medicine”. This point, like many others, is disputed in the literature7, 8, 9, 10 . Areas for future research The literature on the cost of PBL compared to that of traditional approaches is derived from studies at North American, European and Australian institutions. To what extent is this true in other regions of the world? What are the pros and cons and feasibility of implementation of PBL, in the preclinical compared to the clinical phase? What are the most suitable student assessment methods for PBL and how can they be best integrated with other assessment methods? To what extent is it possible to link curriculum innovations and outcome studies on physician competence and capability? Such areas and many others still raise a lot unanswered questions that need further investigations. Acknowledgement The authors acknowledge the support of the FAIMER Institute for the Fellows and ML Web. References 1. Available at: www.faimer.org 2. Johnson, S & Finucane, P. The Emergence of problem-based learning in medical education. Journal of Evaluation in Clinical Practice, 2000; 6, 3: 281-291. 3. Kilroy D. Problem based learning. Downloaded from Emj.bmj.com, 2006. 4. Mennin S & Martinez-Burrola N. The cost of problem-based vs traditional medical education. Medical Education, 1986; 20: 187-194. 5. Donner RS & Bickley H. Problem-based learning: An assessment of its feasibility 4 6. 7. 8. 9. 10. and costs. Human Pathology, 1990; 21: 881-885. Nieuwenhuijzen-Kruseman AC, Kolle LFJTh, Scherpbier AJJA. Problem-based learning at Maastricht - An assessment of cost and outcome. Education for Health, 1997; 10: 179-187. Berkson L. Problem-based learning: have the expectations been met? Acad Med, 1993;68:S79-88. Albanese M. Problem-based learning: why curricula are likely to show little effect on knowledge and clinical skills. Med Edu 2000; 34:729-38. Colliver JA. Effectiveness of problembased learning curricula: research and theory. Acad Med 2000; 75:259-66. Soveri I. Does PBL make better doctors? Miniproject, pedagogisk kurs for universitetslarare I, vt, 2006. 5