(1) and -acetoxyelatadihydrochalcone (2)
advertisement

ANTIPLASMODIAL AND LARVICIDAL
FLAVONOIDS FROM THE SEEDPODS OF
TEPHROSIA ELATA AND TEPHROSIA AEQUILATA
LOIS MWIKALI MUTISYA
MASTER OF SCIENCE
Medicinal Chemistry
JOMO KENYATTA UNIVERSITY OF
AGRICULTURE AND TECHNOLOGY
2009
Antiplasmodial and Larvicidal Flavonoids from the Seedpods of
Tephrosia elata and Tephrosia aequilata
Lois Mwikali Mutisya
A Thesis submitted in Partial Fulfilment for the Degree of Master of
Science in Medicinal Chemistry in the Jomo Kenyatta University of
Agriculture and Technology
2009
i
DECLARATION
This is my original work and has not been presented for a degree in any other university.
Sign....................................................
Date...............................................
Lois Mwikali Mutisya
This thesis has been submitted for examination with our approval as University
supervisors
Sign.....................................................
Date..................................................
Prof. Abiy Yenesew
UON, Kenya
Sign.......................................................
Date..................................................
Prof. Joseph M. Keriko
JKUAT, Kenya
Sign.......................................................
Date..................................................
Dr. Solomon Derese
UON, Kenya
Sign......................................................
Date...................................................
Dr. Charles Mutai
KEMRI, Kenya
ii
DEDICATION
This thesis is dedicated to my beloved husband Charles and my lovely children: Fred,
Immanuel and Maryann. Their support and encouragement enabled me to undertake this
piece of work. My love for them is immeasurable.
iii
ACKNOWLEDGEMENT
I would like to express my sincere gratitude to my supervisors Prof. Abiy Yenesew,
Prof. Joseph M. Keriko, Dr. Solomon Derese and Dr. Charles Mutai for their prompt
guidance, support and inspiration throughout my MSc work.
I am deeply indebted to Prof. Martin G. Peter and Dr. Matthias Heydenreich for
organizing and analyzing the samples on high resolution NMR, MS, and CD. Mr. Akala,
H., Dr. Waters, N. C and Ms. Liyala, P. of Kenya Medical Research Institute and United
States Army Medical Research Unit - Kenya are greatly acknowledged for their
collaboration in carrying out the antiplasmodial tests described in this work.
I wish to sincerely acknowledge the financial support of Africa Institute for Capacity
Development (AICAD), the Deutsche Forschungsgemeinschaft (DFG), Germany, Grant
No. Pe 264/14-5 and by the Bundesministerium fuer Zusammenarbeit (BMZ), Grant No.
Pe-264/14-6.
Special acknowledgement goes to Dr. S. Mpoke – Co-ordinator ITROMID Programme
for his constant encouragement and support during my study period.
I owe much gratitude to the technicians of the Zoology Department, University of
Nairobi, for the supply and hatching of the mosquito larvae of the Aedes aegypti used in
the larvicidal tests. Sincere acknowledgement goes to Mr. Patrick C. Mutiso of the
University of Nairobi Herbarium for identification of the plants investigated in this study
and the academic and technical staff of the Department of Chemistry, University of
Nairobi. My parents, brothers, sisters, friends and colleagues are sincerely thanked for
their endless support and encouragement. Finally, I am very grateful to my dear husband
Charles whose constant love, understanding, encouragement and moral support shone
light to my ego and provided humble space during the hard times of my research. Lastly,
I wish to thank the almighty God for giving me life, strength and protection during the
entire study period. To Him, I give all the Honour and Glory, Amen.
iv
TABLE OF CONTENTS
DECLARATION ............................................................................................................... ii
DEDICATION .................................................................................................................. iii
ACKNOWLEDGEMENT ............................................................................................... iv
TABLE OF CONTENTS .................................................................................................. v
LIST OF TABLES ............................................................................................................ x
LIST OF FIGURES ........................................................................................................ xii
LIST OF SCHEMES ..................................................................................................... xiii
APPENDICES ................................................................................................................ xiv
LIST OF ABBREVIATIONS ........................................................................................ xv
ABSTRACT ................................................................................................................... xvii
CHAPTER ONE ............................................................................................................... 1
1.0 INTRODUCTION ....................................................................................................... 1
1.1 Background information ............................................................................................... 1
1.2 Biodegradable larvicides ............................................................................................... 5
1.3 Statement of Problem .................................................................................................... 6
1.4 Rationale and Significance of the study ........................................................................ 7
1.5 Hypothesis ..................................................................................................................... 9
1.5.1 Alternative hypothesis................................................................................................ 9
1.6. Objectives ................................................................................................................... 10
1.6.1 General objective ..................................................................................................... 10
1.6.2 Specific objective ..................................................................................................... 10
CHAPTER TWO ............................................................................................................ 11
v
2.0 LITERATURE REVIEW......................................................................................... 11
2.1 Malaria ........................................................................................................................ 11
2.1.1 Epidemiology ........................................................................................................... 11
2.2 Malaria control strategies ............................................................................................ 12
2. 2.1 Vector control.......................................................................................................... 13
2.2.2 Larval control ........................................................................................................... 13
2.2.3 Insecticides ............................................................................................................... 15
2.2.4 Bed nets and repellents............................................................................................. 15
2.2.5 Vaccine development ............................................................................................... 16
2.2.6 Chemotherapy for malaria........................................................................................ 17
2.2.7 Medicinal plants and herbal medicines .................................................................... 19
2.3 Botanical Information ................................................................................................. 20
2.3.1 The family Leguminosae ......................................................................................... 20
2.3.1.1 The sub-family Papilionoideae ............................................................................. 20
2.3.1.2 The genus Tephrosia ............................................................................................. 20
2.1.3 Tephrosia elata ........................................................................................................ 22
2.3.1.4 Tephrosia aequilata .............................................................................................. 23
2.3.2 Ethno-medical information of Leguminosae ........................................................... 23
2.3.3 Biological activities of the genus Tephrosia ............................................................ 26
2.3.3.1 Flavonoids as antimalarial agents ......................................................................... 28
2.4 Phytochemical Information on the genus Tephrosia .................................................. 30
2.4.1 Flavonoids ................................................................................................................ 30
2.4.1.1 Biosynthesis of Flavonoids ................................................................................... 32
vi
2.4.2 Compounds Reported from Tephrosia ..................................................................... 36
2.4.2.1 Flavanones of Tephrosia ....................................................................................... 36
2.4.2.2 Flavones of Tephrosia ........................................................................................... 41
2.4.2.3 Isoflavones of Tephrosia ....................................................................................... 43
2.4.2.4 Chalconoids of Tephrosia ..................................................................................... 47
2.4.2.5 Rotenoids of Tephrosia ......................................................................................... 51
2.4.2.6 Pterocarpanoids of the genus Tephrosia ............................................................... 55
2.4.2.7 Other compounds from the genus Tephrosia ........................................................ 57
CHAPTER THREE ........................................................................................................ 61
3.0 MATERIALS AND METHODS ............................................................................. 61
3.1 General ........................................................................................................................ 61
3.2 Reagents ...................................................................................................................... 62
3.2.1 Apparatus ................................................................................................................. 62
3.2.2 Test organisms ......................................................................................................... 62
3.3 Plant Materials ............................................................................................................ 63
3.3.1 Collection of plants materials .................................................................................. 63
3.3.2 Preliminary processing of the samples ..................................................................... 63
3.3.3 Preliminary phytochemical profile evaluation ......................................................... 64
3.4 Extraction and Isolation of Compounds ...................................................................... 64
3.4.1 Extraction and isolation of compounds from the seedpods of T. elata .................... 64
3.4.2 Extraction and isolation of compounds from the seedpods of T. aequilata ............. 65
3.4.3 Acetylation of compound 1 ...................................................................................... 66
3.5 Physical and Spectroscopic Data of the Isolated Compounds .................................... 66
vii
3.5.1 Compound 1 ............................................................................................................. 66
3.5.2 Compound 2 ............................................................................................................. 67
3.5.3 Compound 3 ............................................................................................................. 67
3.5.4 Compound 4 ............................................................................................................. 68
3.5.5 Compound 5 ............................................................................................................. 68
3.5.6 Compound 6 ............................................................................................................. 69
3.5.7 Compound 7 ............................................................................................................. 69
3.5.8 Compound 8 ............................................................................................................. 70
3.5.9 Compound 9 ............................................................................................................. 70
3.6 Biological Activity Assays .......................................................................................... 71
3.6.1 In-vitro antiplasmodial activity assay ...................................................................... 71
3.6.2 Larvicidal activity assay........................................................................................... 72
CHAPTER FOUR ........................................................................................................... 74
4.0 RESULTS AND DISCUSSION ............................................................................... 74
4.1 Preliminary Test Results ............................................................................................. 74
4.1.1 Phytochemical profile evaluation results ................................................................. 74
4.1.2 In-vitro antiplasmodial activity evaluation results ................................................... 74
4.2 Characterization of Isolated Compounds .................................................................... 75
4.2.1 Compounds from Tephrosia elata ........................................................................... 75
4.2.1.1 Chalcones .............................................................................................................. 75
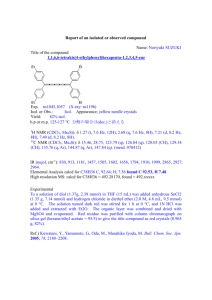
4.2.1.1.1 Elatadihydrochalcone (1) and -acetoxyelatadihydrochalcone (2).................... 75
4.2.1.1.2 Obovatachalcone (3) .......................................................................................... 83
4.2.1.2 Flavanones ............................................................................................................ 85
viii
4.2.1.2.1 Obovatin (4) ....................................................................................................... 85
4.2.1.2.2 Obovatin methyl ether (5) .................................................................................. 86
4.2.1.3 Rotenoids .............................................................................................................. 88
4.2.1.3.1 Deguelin (6) ....................................................................................................... 88
4.2.1.3.2 Rotenone (7) ....................................................................................................... 89
4.2.2 Compound Isolated from Tephrosia aequilata ........................................................ 91
4.2.2.1 Chalcones .............................................................................................................. 91
4.2.2.1.1 Praecansone A (8) .............................................................................................. 91
4.2.2.1.2 Demethylpraecansone B (9) ............................................................................... 93
4.3 Biological Activities of the Isolated Compounds ....................................................... 95
4.3.1 Antiplasmodial activities of compounds from the seedpods of T. elata .................. 95
4. 3.2 Antiplasmodial Activities of compounds from the seedpods of T. aequilata ......... 96
4.3.3 Results and Discussion of Larvicidal tests ............................................................... 96
CHAPTER FIVE ............................................................................................................. 98
5.0 CONCLUSIONS AND RECOMMENDATIONS .................................................. 98
5.1 Conclusions ................................................................................................................. 98
5.2 Recommendations ....................................................................................................... 99
REFERENCES .............................................................................................................. 102
APPENDICES ............................................................................................................... 119
ix
LIST OF TABLES
Table. 2.1:
Regional Distribution of Malaria ..................................................... 12
Table. 2.3:
Flavanones of Tephrosia .................................................................. 37
Table. 2.4:
Flavones of Tephrosia ...................................................................... 41
Table. 2.5:
Isoflavones of Tephrosia .................................................................. 44
Table. 2.6:
Chalconoids of the genus Tephrosia ................................................ 48
Table. 2.7:
Rotenoids of the genus Tephrosia .................................................... 52
Table. 2.8:
Pterocarpanoids of the genus Tephrosia .......................................... 55
Table. 2.9:
Other compounds isolated from Tephrosia ...................................... 57
Table. 4.1:
In vitro IC50 values of the crude seedpods extracts from T. elata
and T. aequilata against D6 and W2 strains of P. falciparum ........ 75
1
Table . 4.2:
H NMR (300 MHz) and 13C NMR (75 MHz) along with HMBC
Correlations for elatadihydrochalcone (1) and
Acetoxyelatadihydrochalcone (2)………………………..………79
Comparison of the 1H NMR (a) and 13C NMR (b) data of the an
Table. 4.3a:
atoms of elatadihydrochalcone (1) with literature for
Hydroxydihydrochalcone derivatives (152-8) and flavanones
(4and 5). ........................................................................................... 80
13
Table. 4.3b:
Table. 4.4:
1
Table. 4.5:
1
C NMR data .................................................................................. 80
H (200 MHz) and 13C NMR (50 MHz) data for obovatachalcone (3)84
H (300 MHz) and 13C NMR (75 MHz) data along with HMBC
x
Correlationsfor obovatin (4) and obovatin methyl ether (5) in CDCl3.87
Table. 4.6:
1
H NMR (300 MHz) and 13C NMR (75 MHz) data along with
HMBC Correlations for deguelin (6) and rotenone (7) in CDCl3. .. 90
Table. 4.7:
1
H NMR (200 MHz) and 13 C (50 MHz) NMR data for (E)-
praecansone A .................................................................................. 92
Table. 4.8:
1
H (200 MHz) and 13 C (50 MHz) NMR data for
demethylpraecansone B .................................................................... 94
Table. 4.9:
In vitro antiplasmodial activities of flavonoids isolated from T. elata
T. aequilata against D6 and W2 strains of P. falciparum ................. 96
Table. 4.10:
Larvicidal test results for crude extract and isolated compounds
from the seedpods of T. elata. .......................................................... 97
xi
LIST OF FIGURES
Figure. 2.2:
Tephrosia elata at different stages of growth ................................ 22
Figure. 2.3:
Tephrosia aequilata at different stages of growth ......................... 23
Figure. 2.4:
Basic skeletons of flavonoids and isoflavonoids .......................... 32
Figure. 2.7:
Summary of sub-classes of compounds from genus Tephrosia ... 60
Figure. 4.2:
nOe interactions observed for obovatin methyl ether (5) ............. 88
Figure. 4.3:
nOe interactions observed for (E)-praecansone A (8) .................. 92
Figure. 4.4:
nOe interactions observed for demethylpraecansone B (9) .......... 94
xii
LIST OF SCHEMES
Scheme 2.1.
Biosynthesis of chalcones and isoflavonoids. .................................. 34
Scheme 2.2.
Biosynthetic interrelationships among different flavonoids ............ 35
xiii
APPENDICES
APPENDIX A:
Spectra for compound 1 .......................................................... 120
APPENDIX B:
Spectra for compound 2 .......................................................... 137
APPENDIX C:
Spectra for compound 3 .......................................................... 150
APPENDIX D:
Spectra for compound 4 .......................................................... 155
APPENDIX E:
Spectra for compound 5 .......................................................... 162
APPENDIX F:
Spectra for compound 6 &7.................................................... 170
APPENDIX G:
Spectra for compound 8 .......................................................... 174
APPENDIX H:
Spectra for compound 9 .......................................................... 177
APPENDIX I:
Publication ............................................................................... 180
xiv
LIST OF ABBREVIATIONS
Brs
Broad singlet
13C
Carbon-13 isotope
CHI
Chalcone isomerase
CHS
Chalcone synthase
Chemical shift in delta values
CD
Circular dichroism
IC50
Concentration causing 50% inhibition
LC50
Concentration causing 50% lethality
COSY
Correlated spectroscopy
J
Coupling constant
DDT
Dichlorodiphenyltrichloroethane
DMSO
Dimethyl sulfoxide
d
Doublet
dd
Doublet of a doublet
ddd
Doublet of a double doublet
EI-MS
Electron ionization mass spectroscopy
Hz
Hertz
HMBC
Heteronuclear multiple bind correlation
HMQC
Heteronuclear multiple quantum coherence
HR-MS
High Resolution Mass spectroscopy
xv
IFS
Isoflavonoid synthase
m/z
Mass to charge ratio
MS
Mass spectroscopy
max
Maximum wavelength
of absorption
MHz
Mega hertz
m
Multiplet
NMR
Nuclear magnetic resonance
NOESY
Nuclear overhauser and exchange spectroscopy
NOE
Nuclear overhauser effect
PTLC
Preparative thin layer chromatography
1H
Proton
.8
[]28
D
Specific rotation measured with sodium D-line light
(589 nm) at 28.80 C
TLC
Thin layer chromatography
UV
Ultra violet
xvi
ABSTRACT
The genus Tephrosia is rich in flavonoids and isoflavonoids including rotenoids. In the
search for compounds with antiplasmodial and larvicidal activities from medicinal
plants, the seedpods of Tephrosia elata and Tephrosia aequilata were analysed. The
dried and ground seedpods of T. elata and T. aequilata were extracted separately with
CH2Cl2/MeOH (1:1) by cold percolation for 24 hours at room temperature. The crude
extracts showed significant antiplasmodial activities with IC50 values of 8.4 + 0.3 and
8.6 + 1.0 g/ml for T. elata, and 1.5 + 0.2 g/ml and 22.4 + 5.2 g/ml for T. aequilata,
against chloroquine-sensitive (D6) and chloroquine-resistant (W2) strains of
Plasmodium falciparum, respectively. The crude seedpods extract of T. elata also
showed larvicidal activity against the mosquito larvae of Aedes aegypti with LC50 of
68.9 ± 0.3 g/ml at 24 hours and 40.2 ± 0.2 g/ml at 48 hours. Chromatographic
separation of the CH2Cl2/MeOH (1:1) extract of the seedpods of T. elata led to the
isolation of seven compounds. These were identified as the β-hydroxydihydrochalcone
(S)-(-)-3',4'-(2'',2''-dimethylpyrano)-2',-dihydroxy-6'-methoxydihydrochalcone,
trivial
name elatadihydrochalcone (1); the chalcone obovatachalcone (3); the flavanones,
obovatin (4) and obovatin methyl ether (5); the rotenoids deguelin (6) and rotenone (7).
The CH2Cl2/MeOH (1:1) crude seedpods extract of T. aequilata yielded three known
compounds, obovatin methyl ether (5), (E)-praecansone A (8) and demethylpraecansone
B (9). Elatadihydrochalcone (1) is a novel compound and is the first of its kind in the
genus Tephrosia. The presence of β-hydroxy group was confirmed by the preparation of
xvii
the mono acetate, -acetoxyelatadihtydrochalcone (2). Obovatachalcone (3), obovatin
(4), deguelin (6) and rotenone (7) are reported here for the first time from T. elata. The
identification of these compounds was based on spectroscopic techniques (1H NMR, 13C
NMR, HMBC, HMQC, COSY, DEPT, nOe, UV and MS). The stereochemistry in
elatadihydrochalcone (1) was determined from CD spectrum. The isolated compounds
from T. elata were tested for antiplasmodial activities. The novel compound,
elatadihydrochalcone (1) showed antiplasmodial activity with IC50 = 2.8 + 0.3 g/ml and
5.5 + 0.3 g/ml against (D6) and (W2), respectively. Obovatin methyl ether (5) showed
activity against (D6) and (W2) strains of P. falciparum with IC50 value of 3.8 + 0.3 and
4.4 + 0.6 g/ml, respectively. Praecansone A (8) showed antiplasmodial activity with
IC50 value of 6.6 + 1.1 g/ml and 6.4 + 1.0 g/ml against D6 and W2 respectively.
Deguelin (6) and rotenone (7) together showed larvicidal activity against 3rd instar
mosquito larvae of Aedes aegypti with LC50 value of 7.6 ± 0.4 g/ml at 24 hours.
xviii
CHAPTER ONE
1.0 INTRODUCTION
1.1 Background information
Malaria is one of the most severe public health problems worldwide. It is a disease that
has overwhelmed mankind for many years, with far reaching medical, social and
economic consequences. It is the leading cause of the rising morbidity and mortality
rates in most countries in Sub-Saharan Africa [Taylor and Triggle, 2007]. Malaria
accounts for 350 to 500 million clinical cases and up to 2.7 million deaths each year
[Johnson et al., 2007; Taylor and Triggle, 2007]. About 90% of these casualties occur in
tropical Africa, the great majority being children under the age of 5 years [Frankish,
2002; Taylor and Triggle, 2007]. It is predicted that clinical infections and death will
increase due to rapid global spread of multi-drug resistant malaria parasites [Johnson et
al., 2007].
In Kenya, malaria is the greatest contributor to the rising rate of morbidity and mortality
of all infectious diseases. The high-risk groups of people are: those in whom immunity
has not yet developed (children under five years of age, travellers and immigrants) and
those in whom immunity has diminished (pregnant women, immuno-compromised
subjects and people from endemic areas who have ceased to be routinely exposed to reinfection) [Kigondu, 2007; Kirira et al., 2006]. It is important to continually prepare for
the possibility that some of the drugs that are available now may not be effective
indefinitely [Frankish, 2002].
1
It is predicted that clinical infections and death will increase due to rapid spread of
multi-drug resistant malaria parasites [Johnson et al., 2007]. Of the four strains of
malarial parasites: P. falciparum, P. vivax, P. ovale and P. malariae, P. falciparum is the
most deadly while P. vivax is the leading cause of morbidity due to the dominant phases
of the parasite that reside in the liver hepatocytes. Both P. falciparum and P. vivax have
developed resistance to numerous anti-malarial drugs which has undermined the
available options of prophylaxis and treatment [Johnson et al., 2007]. For instance,
resistance to anti-malarial drug chloroquine is common throughout Africa and resistance
to sulfadoxine-pyrimethamine is also increasing [Frankish, 2002].
The future of antimalarial chemotherapy appears bleak due to the increasing crossresistance to drugs, because the available drugs used clinically are structurally similar
and pharmacologically related [Vishnu et al., 2000]. Thus the need for structurally
different efficacious anti-malarial drugs is self-evident. The problem of drug resistance
can be circumvented either by identifying new targets which are critical to the disease
progress or essential for the survival of the parasites [Vishnu et al., 2000]. The other
possible way could be to design and synthesize a new efficacious clinical entity with
least side effects. Natural products are known as the chief source of identification of lead
structures. Structural modification of such compounds is expected to result in highly
efficacious chemotherapeutic agents with reduced toxicity and side effects [Vishnu et
al., 2000].
2
Most of the available anti-malarial drugs that are in use today were developed through
screening of natural products and subsequent synthesis. Herbal medicines are considered
as a potential source of new drugs or templates for developing new drugs [Mark, 2004;
Rates, 2001]. Pharmaceutical research in natural products represents a major strategy for
discovering and developing new drugs. The discovery of quinine (10) from Cinchona
succiruba Vahl. (Rubiaceae) [Rang et al., 2003; Trease and Evans, 2002] and
artemisinin (11) from Artemisia annua L. (Asteraceae) followed by their subsequent
development as antimalarial drugs provided impetus to the management of malaria
[Taylor and Triggle, 2007; Rang et al., 2003].
The resurgence of malaria vector resistance to insecticides and resistance of Plasmodium
species to the most valuable chemotherapeutic agents such as chloroquine (12) has
magnified the problem. The success of artemisinin (11) in the management of
uncomplicated malaria with little signs of resistance development, has opened a new
horizon in anti-malarial drug research and increased interest in plants with medicinal
properties [Abosi et al., 2006]. Plants concoctions still continue to be used in this
3
millennium for the treatment of various diseases. The medicinal properties of plants are
usually dependent upon the presence of certain active phytochemicals, which are very
significant to modern medicine, since they are important sources of several useful
modern clinical drugs [Trease and Evans, 2002]. Approximately one hundred and twenty
distinct chemical substances isolated from plants are considered to be important
therapeutic agents [Rates, 2001].
However, there is still a great potential for plants in the development of new drugs
especially from medicinal plants. Thus, there is hope that phytochemicals with specific
action against malaria might be isolated from medicinal plants. Several plants are being
investigated around the world with the objective of identifying lead structures for the
next generation of anti-malarial drugs. Flavonoids are among different classes of natural
products currently being investigated for anti-plasmodial activity. For instance
Licochalcone A (13) a chalcone isolated from Chinese licorice roots has been reported to
be highly effective in an in vitro screen against chloroquine sensitive (3D7) and
chloroquine resistant (Dd2) isolate of P. falciparum [Taylor and Triggle, 2007; Vishnu
4
et al., 2000]. The efficacy of this product has also been confirmed in vivo against P.
yoelii in mice [Vishnu et al., 2000]. Thus, licochalcone A (13) provided a lead to design
and synthesize chalcones as new antimalarials [Rafi et al., 2002; Vishnu et al., 2000].
The flavanone abyssinone-IV (14) is a flavonoid isolated from the roots of E. abyssinica
which showed good activity against both strains of P. falciparum [Yenesew et al., 2003;
Derese, 2004].
Tephrosia species are known to elaborate flavonoids and isoflavonoids which include:
chalcones, flavanones, isoflavones and pterocarpans. These subclasses of flavonoids
have been reported as antiplasmodial agents among plant metabolites [Yenesew et al.,
2003; Vishnu et al., 2000].
1.2 Biodegradable larvicides
The emergence of insect resistance to convectional insecticides together with the
growing environmental concern on the use of many synthetic insecticides for instance
DDT, has resulted in high prevalence of mosquito transmitted diseases such as malaria
5
in sub-Saharan Africa [Derese, 2004]. In the search for biodegradable and cost effective
alternatives for the control of disease vector insects, plant extracts and pure compounds
have been tested for larvicidal activities [Yenesew et al., 2006; Omena et al., 2007].
Tephrosia, Derris and Lonchocarpus genera are well known sources of the insecticidal
and pesticidal rotenoids with Tephrosia containing the largest number of rotenoids
producing species [James et al., 1958]. Deguelin (6), rotenone (7) and tephrosin (15) and
have showed potent larvicidal activity against 2nd instar larvae of Aedes aegypti
[Yenesew et al., 2006] and are also known to occur in the genus Tephrosia [Ahmad et
al., 1999].
1.3 Statement of Problem
Malaria is a major contributor to the global burden of disease and a significant
impediment to socio-economic development in poor countries. Malaria remains one of
the deadliest diseases on this planet, which accounts for 350 – 500 million clinical cases
and up to 2.7 million deaths each year [Taylor and Triggle, 2007]. It is the leading cause
of the rising morbidity and mortality rates in most countries in Sub-Saharan Africa. At
6
least one child dies of malaria every 40 seconds in the world and this shows the
devastating effect of this disease [Geissbϋhler et al., 2007; Taylor and Triggle, 2007].
Efforts to combat the disease are hampered by growing resistance of malaria parasites to
the readily available drugs. The cost of drugs is a sizable proportion of the total health
expenditure in most developing countries. Drug related expenses in these countries
account for up to 30-50% of the total cost of healthcare [Taylor and Triggle, 2007;
WHO, 2007]. Toxicity of the available antimalarial drugs to many of the patients is an
important issue yet to be addressed conclusively because it prompts many of them to
turn to herbal medicines which may result to be more detrimental to their health, since
little or no scientific research has been done on those herbal remedies to prove their
safety and efficacy. Due to the increasing prominence of herbal remedies, additional
contributions describing scientific investigations of a rigorous nature are most
welcomed. In addition, continuous research is desperately needed in order to come up
with compounds which can be developed into new, cheap, less toxic and more
efficacious antimalarial drugs for combating the disease.
1.4 Rationale and Significance of the study
In sub-Saharan Africa, malaria remains the main cause of the high mortality rate with
the poor who have little or no access to modern medicine being the most affected
[Taylor and Triggle, 2007; Peter, 2007]. This group represents about 75% of the world’s
population that relies on herbal remedies [Anthonia and Benjamin, 2003].
7
Malaria is becoming more resistant to a number of current drugs and is on the increase
because of the global warming process, thus, many communities who live in endemic
areas have tirelessly been involved in the search for malaria remedies in plants found in
their local environment. Therefore, scientific investigation of the plants used in
traditional herbal remedies for the disease will contribute to both knowledge and health
[Anthonia and Benjamin, 2003].
Various attempts have been made in the control of malaria including, selective
application of vector control, early diagnosis and effective and prompt treatment of
malarial disease and early detection or forecasting of epidemics and rapid application of
control measures. Since malaria is transmitted by the female anopheles mosquito, a
major strategy of control is to attack the vector with insecticides and/or larvicides.
Extended use, however, has led and continues to lead to the emergence of insecticideresistant mosquitoes [Campbell, 1997]. The use of Tephrosia species of Kenyan origin
for the control of mosquitoes at the larval stage may provide a useful deterrent against
proliferations of these disease vectors. Previous investigations of the phytochemical
profile of the genus Tephrosia have resulted in the isolation and identification of
compounds such as flavavones, isoflavonoids, chalcones and rotenoids. Rotenone (7)
and tephrosin (15) have showed potent larvicidal activity against 2nd instar larvae of
Aedes aegypti [Yenesew et al., 2006]. The study of T. elata and T. aequilata may lead to
the isolation, identification and characterization of cheap, less toxic and more efficacious
8
natural antiplasmodial compounds for use as lead compounds in the process of discovery
of new antimalarial drugs.
The identification of antiplasmodial compounds and larvicides which are biodegradable
and environmentally friendly as an alternative to synthetic antimalarial drugs and
larvicides will contribute significantly to the health of the people especially those living
in malaria endemic rural areas. It is worth to note that the medicinal plant industry plays
a critical role in empowering large numbers of rural folk in many African countries
[Anthonia and Benjamin, 2003].
Thus, in this study the antiplasmodial activities of the crude extracts and isolated
compounds from the seedpods of Tephrosia elata and Tephrosia aequilata were tested
against chloroquine-sensitive (D6) and chloroquine-resistant (W2) strains of P.
falciparum. Furthermore the larvicidal activities of the crude seedpods extract and the
isolated compounds of Tephrosia elata were tested against the larvae of Aedes aegypti,
in order to establish the potential use of the two plants in the treatment and control of
malaria.
1.5 Hypothesis
1.5.1 Alternative hypothesis
The phytochemicals from the seedpods of Tephrosia elata and Tephrosia aequilata
possess inhibitory activity on the growth of Plasmodium falciparum in vitro and
larvicidal activity against the larvae of Aedes aegypti.
9
1.6. Objectives
1.6.1 General objective
To isolate, identify and characterize the compounds of the seedpods of Tephrosia elata
and Tephrosia aequilata and determine their antiplasmodial and larvicidal activities.
1.6.2 Specific objective
i.
To investigate the antiplasmodial activity of the crude seedpods extracts of
Tephrosia elata and Tephrosia aequilata.
ii.
To determine the larvicidal activity of the crude seedpods extract of Tephrosia
elata.
iii.
To isolate and characterize the constituents of the seedpods of Tephrosia elata
and Tephrosia aequilata.
iv.
To test the antiplasmodial and larvicidal activity of the isolated compounds.
10
CHAPTER TWO
2.0 LITERATURE REVIEW
2.1 Malaria
Malaria is an acute and chronic illness characterized by paroxysms of fever, chills,
sweats, fatigue, anaemia and splenomegaly [Peter, 2007]. It is caused by intracellular
Plasmodium protozoa transmitted to human by female Anopheles mosquitoes. Four
species of Plasmodium cause malaria in humans: P. falciparum, P. malariae, P. ovale
and P. vivax. Malaria can also be transmitted through blood transfusion and from a
pregnant woman to her foetus [Peter, 2007; Taylor and Triggle, 2007].
2.1.1 Epidemiology
Malaria is a major worldwide problem occurring in more than one hundred countries
with a combined population of greater than 1.6 billion people [Peter, 2007]. The threat
from this disease has increased in recent years due to changing global climate, resistance
developed by the parasite to antimalarial drugs currently available in the market, and
increasing international travel which exposes non-immune populations to malaria
parasites [Kigondu, 2007]. The principal areas of transmission are Africa, Asia and
South America. P. falciparum and P. malariae are found in most malarious areas. P.
falciparum is the predominant species in Africa, Haiti, and New Guinea. P. vivax
predominates in Bangadesh, Central America, India, Pakistan, and Sri Lanka [Peter,
2007; Taylor and Triggle, 2007]. Table 2.1 below summarizes the regional distribution
11
of malaria and the contribution to global malaria mortality burden [Taylor and Triggle,
2007].
Table. 2.1: Regional Distribution of Malaria
Plasmodium
species
Principal vectors
AFRICA
P. falciparum (93%)
P. vivax or its mixed
infections with P.
falciparum (7%)
A. gambiae
A. funestus
Population at risk 66%
59%
Contribution to
the global burden
of clinical malaria
cases
ASIA
P. falciparum
(35%)
P. vivax
THE AMERICAS
P. falciparum
(18%)
P. vivax (72%)
P. malriae
A. culicifacies,
A. minimus
A. annularis,
A. maculipennis
A. sacharovi
A. superpictus,
A. farauti
49%
38%
A. albimanus
(Central America)
A. darlingi
(Amazon Basin)
14%
14%
2.2 Malaria control strategies
Malaria is a focal disease, which differs in its characteristics from country to country and
from one geographical location to the other even within the same country [WHO, 1995].
This variation mainly depends on climatic conditions such as rainfall, humidity and
temperature. Hence no single strategy for malarial control is applicable for all situations.
There has to be a regular assessment of each country's malarial epidemic situation. There
are a variety of factors to take into account, such as the biological, anthropological,
cultural and social characteristics of the population; the intensity and periodicity of
12
malaria transmission; the species of malaria parasites and their sensitivity to antimalarial
drugs among other factors [WHO, 1995]. The three essential elements of malaria control
are: (i) Vector control, (ii) Early diagnosis, and effective and prompt treatment of
malarial disease (chemotherapy) and (iii) Detection or forecasting of epidemics and rapid
application of control measures [WHO, 1995].
2. 2.1 Vector control
The most efficient malaria vector is the African Anopheles gambiae. Environmental
management strategies (EMS) such as filling ditches, covering water containers,
flushing irrigation channels and clearing of ponds of weed growth reduces breeding sites
which contribute significantly to malaria reduction [Bruce-Chwart, 1993]. Use of
chemicals is the mainstay of mosquito control. It includes spraying petroleum oils and
derivatives onto the water surface to form a thin film that prevent larvae and pupae from
breathing through the surface of the water [Bruce-Chwart., 1993]. There is also use of
mosquito repellents as in the case of treated bed nets and mosquito coils [Phillipe and
Miller, 2002].
2.2.2 Larval control
The use of larvicides to control mosquito populations at the larval stages of development
is referred to as larval control. For most malaria vectors, reduction in mosquito
population densities by means of larvae eradication is an efficient way of controlling
malaria transmissions [Bruce –Chwart, 1993; WHO, 1995]. The most common larval
habitats include; stagnant waters, pods, small pools and dams which can be identified
13
and targeted for treatment, although their numbers are numerous and hence require a lot
of resources. In general, organophosphates, larvicidal oils, arsecal compounds, and
development inhibitors have been used with varying degrees of success [Gratz and Pal,
1988]. Continued application of organophosphates such as methoprene and insect
growth regulators like diflubenzuron are generally practiced for the control of mosquito
larvae [Yang et al., 2002]. Natural constituents of Azadirachta indica (limonoinds),
Derris trifoliata (rotenoids), tobacco (alkaloids) and pyrethrum (pyrethrins) form a
group of larvicides used to control the populations of the mosquitoes [Bruce-Chwart,
1993; WHO, 1995].
The repeated use of these insecticides results to effective larval control but can lead to
disruption of natural biological control systems. This consequently, result in the
widespread development of resistance leading to an outbreak of large population of
mosquitoes and undesirable effects on non-target organisms, creating environmental and
human health concerns [Yang et al., 2002]. These problems have highlighted the need
for the development of new strategies for selective, affordable and biodegradable
mosquito larvicides.
In search of more effective, affordable and biodegradable alternatives for the control of
disease vector insects, plant extracts and isolated pure compounds have been tested for
larvicidal activity [Mwangi and Rembold, 1998]. Rotenone (7), which is one of the most
extensively used natural insecticide, has been reported to be highly active against fourth
- instar larvae of Aedes aegypti [Kiplagat, 2006]. The insecticidal activities of rotenone
14
(7) and some other rotenoids including dequelin (6) and tephrosin (15) against a variety
of insect species are well known [James et al. 1970; Dewick, 2002]. These and other
rotenoids are known to occur in the related genera including Tephrosia. [Dewick, 2002].
2.2.3 Insecticides
The use of insecticides involves eradicating the adult mosquitoes directly by spraying
insecticides at the sites in which they hide, for instance the dark corners in the house,
bushes,
and
flower
beds
around
residential
areas.
Organochlorines,
like
dichlorodiphenyltrichloroethane (DDT) and dieldrin, organophosphates such as
malathion and temephos constitute groups of insecticides [Phillipe and Miller, 2002].
The environmental concerns which arise from the use of insecticides are well
documented especially organochlorines, like dichlorodiphenyltrichloroethane (DDT) and
it has worsened with time and use. Vector-insecticide resistance and environmental
concerns over the use of such insecticides has increased tremendously [Yenesew et al.,
2003; Malcom, 1988].
2.2.4 Bed nets and repellents
The prevention of vector contact with human hosts can be achieved by the use of
personal repellents or by physical barrier such as insecticide treated bed nets. Synthetic
repellents are mainly very useful to visitors to endemic regions [Gratz and Pal, 1998].
The use of plants as natural repellents or insecticides has been documented, but most of
the products from plants have not been carefully analysed [Curtis et al., 1990; Kiplagat,
2007].
15
2.2.5 Vaccine development
Nearly all stages of the plasmodium life cycle can be viewed as targets for vaccine
development. The development of clinical immunity after continuous exposure to
parasites in the case of individuals living in endemic areas, gives hope for vaccine (s)
against malaria [Taylor and Triggle, 2007]. The main challenge comes from the complex
life cycle of the parasites, having a number of stages expressing a wide variety of
surface antigens. Plasmodia’s ability to adapt to the human immune system and
misdirect or suppress it, further hiders the process of finding a successful vaccine
[Taylor and Triggle, 2007; Wakelin, 1996]. Lack of proper in vitro and in vivo surrogate
assays, slows down the entire process. One of the most promising results pertaining to
vaccines against sporozoite-stage parasites have been reported from studies using
irradiated sporozoites which conferred protection against infection in mice, nonhuman
primates and humans [Taylor and Triggle, 2007]. Great limitation with this approach
was the difficulty in having a large number of parasites for vaccine development. Liver
stage antigens, LSA-1 and LSA-3 have received special attention in recent years and are
undergoing clinical evaluation [Taylor and Triggle, 2007]. Even though there are
encouraging results, considering the complex nature of the parasites, their interactions
with each other and with hosts, it may take several more decades to develop an effective
and widely applicable malaria vaccine.
16
2.2.6 Chemotherapy for malaria
The fight
against
malaria relies
heavily on chemotherapy after infection.
Chemoprophylaxis is one method used to prevent infection with the disease, but if an
individual is already suffering from the disease or if the parasites evade the prophylactic
drug then treatment is absolutely necessary in order to save lives [Kigondu, 2007]. The
main concern remains that P. falciparum, especially in Africa, has developed resistance
to the commonly prescribed drugs such as quinine (10), chloroquine (12) mefloquine
(16), amodiaquine (17), primaquine (18), halofantrine (Halfan®) (19), atovaquone (20),
proguanil (21), sulphadoxine (22) and dapson (23) [Madrid et al., 2005; Gareth, 2004;
Rang et al., 2003; Polrat et al., 2002].
17
Few effective new drugs are available in combination therapy and are too expensive, for
example artemisinin (11) derivatives such as Artemether (24) and artesunate (25)
[Taylor and Triggle, 2007; Polrat et al., 2002]. The potential value of drug
combinations, notably those an artemisinin derivative, to improve efficacy, delay
18
development, and selection drug-resistance parasites thus prolonging the useful
therapeutic life of existing antimalarial drugs, is widely adopted [Polrat et al., 2002].
2.2.7 Medicinal plants and herbal medicines
Plants produce over a million diverse secondary metabolites. Most of these compounds
are derived from the isoprenoid, phenylpropanoid or through the fatty-acid/polyketide
pathways. They act as defense agents for plants against microbial or insect/animal
predatory. Related plant families generally make use of related chemical structures for
defense, for example, isoflavonoids in Leguminosae and sesquiterpenes in Solanaceae
[Dewick, 2002]. However, because of the vastness of the plant kingdom most of the
species of plants have not been surveyed for phytochemicals or for biological activity.
Herbal medicines are considered as a potential source of new drugs or templates for
development of synthetic analogues [Mark, 2004; Rates, 2001]. Studies have also
revealed a diverse range of plant secondary metabolites (phytochemicals) with varied
levels of antimalarial activities [Nkunya, 1992]. Thus, there is need to continue
19
investigating medicinal plants used in traditional malaria therapy for activity and
identification of the bioactive components in these plants.
2.3 Botanical Information
2.3.1 The family Leguminosae
The genus Tephrosia belongs to the family Leguminosae, also known as Fabaceae,
comprising of 657 genera and 18,000 species of trees, shrubs and herbs, which are
widely distributed in the temperate as well as tropical regions of the world. This family
is the second largest of the dicotyledons after the Compositae, and plants in the family
are known for their ability to support nitrogen fixation through symbiosis [Heywood,
1971]. The family is subdivided into three sub-families: Mimosoidaea, Papilionoideae
and Caesalpinioideae. The genus Tephrosia belongs to the Papilionoidae sub-family
[Polhill et al., 1981a].
2.3.1.1 The sub-family Papilionoideae
Papilionoideae is the largest of the three sub-families with some 440 genera and 12,000
species of trees, shrubs, lianas or herbs. It is sub-divided into 32 tribes [Polhill et al.,
1981b]. This subfamily is distinguished from the other two subfamilies by the presence
of Papilionoid flowers.
2.3.1.2 The genus Tephrosia
Tephrosia is a large tropic and sub-tropic genus of perennial woody shrubs. It is
estimated to contain between 300 and 400 species, distributed all over the world as
follows; 35 species occur in India, 30 are native of South America, 70 are found in
20
South Africa, 50 in equatorial Africa of which 30 are found in Kenya [Tarus et al., 2002;
Beentje, 1994]. It is a highly branched, sub-erect, herbaceous perenial herb. The leaves
are usually imparipinnate, without stipels. Corola (petal) usually reddish-purple, flowers
white and pod flattened and fruit 10 to 15 by 1.6 cm [Beentje, 1994]. Examples of some
Kenyan Tephrosia species include; T. aequilata, T. elata, T. hildebrandtii, T. holstii, T.
interrupta, T. linearis, T. noctiflora, T. paucijuga, T. pentaphylla, T. pumila, T.
purpurea, T. villosa among others [Aqnew and Shirley, 1994]. Fig. 2.1 below shows
three different species of Tephrosia found in Kenya.
Figure 2.1: Some Tephrosia species found in Kenya
21
2.1.3 Tephrosia elata
It is a short-lived bushy perennial shrub. Leaflets grey-green, 15 - 21, 70 X 10 mm, often
deeply notched at apex, lateral veins beneath visible, flowers pink or purple, numerous
in rather dense terminal racemes which are usually longer than their stalks; standard
golden hairly, 14 - 16 mm long; pods 55 x 5 mm, ascending or erect, with dense light
brown hairs [Aqnew and Shirley, 1994]. The main habitat is grassland, former cultivated
land and thicket margins up to 2000 m. In Kenya, it is found in Makueni, Kitui, Mumias,
Kisii, Magadi, Nairobi, Machakos, Embu and Kajiado districts [Aqnew and Shirley,
1994; Beentje, 1994]. Fig. 2.2 below shows T. elata at different stages of growth.
Figure 2.2: Tephrosia elata at different stages of growth
22
2.3.1.4 Tephrosia aequilata
It is a shrub 1-3 m high. Flowers are purple in dense terminal almost sessile, almost
rounded, inflorescences; petals 13 – 17 cm long. Fruit above 3 – 4 x 0.5 – 0.6 cm,
densely tomentose, beaked. Leaf lets 13 - 21 per leaf, eliptic, base cuneate to
subcordinate, apex rounded or apiculate, 1.5 – 5 by 0.6 – 1.5 cm, dark green and almost
glabrous above, densely whitish - puberscent beneath (Fig. 2.3). It inhabits rocky hills,
usually in grasslands or heathzone near summit. It is found at the summit of Nzaui hills
in Makueni district, Kenya [Beentje, 1994; Aqnew and Shirley, 1994].
Figure 2.3: Tephrosia aequilata at different stages of growth
2.3.2 Ethno-medical information of Leguminosae
Plants belonging to this family have been used traditionally by various communities for
the treatment of various ailments. For instance, Licorice root, one of the most commonly
used medicinal plants in Traditional Chinese medicine, has been used for the treatment
23
of gastric and duodenal ulcers, bronchial asthma, inflammation among other disorders
[Friis- Moller et al., 2002]. The root of Sophora flavescens Aiton, another well-known
Chinese herbal medicine is used as a diuretic and for the treatment of diarrhoea,
gastrointestinal haemorrhage and eczema [Woo et al., 1998]. The roots of Taverniera
abyssinica, is widely used in Ethiopia as an effective remedy for sudden pain
particularly of stomach [Duddeck et al., 1987]. Plants belonging to the genera Derris,
Lonchocarpus, Millettia, Mundulea and Tephrosia of the family Leguminosae have long
been used in Africa, Asia and South America as insecticides and fish poison because
they synthesize rotenoids [Derese, 2004; James et al., 1958]. In Kenya, several plants of
this family are used for the treatment of various ailments. Table 2.2 below gives ethnomedicinal
uses
of
some
representative
24
Kenyan
Tephrosia
species.
Table 2.2: Ethno-medicinal use of some Tephrosia species of Kenya
Species
T. aequilata
T. elata
T. interrupta
T. holstii
T. linearis
T. noctiflora
T. paucijuga
T. pentaphylla
T. pumila
T. purpurea
T. villosa
Plant part and Ethno-medical use
Roots dug out, boiled and mixed
with milk and drunk for pain in
liver and spleen. Roots chewed with
salt as a cure for venereal diseases.
Roots chewed as a cure for stomach
pains, fever and general weakness.
Locality/Community
Makueni (Kamba),
Kajiado (Maasai),
Coast (Pare, Digo)
References
Agnew et al., 1994;
Kokwaro, 1993
Machakos,
(Kamba), Kajiado
(Maasai)
Agnew et al., 1994;
Lwande, 1985
The roots are roasted and ground,
mixed with a little salt and used as a
cough cure. Roots may also be
pounded, mixed with porridge and
eaten by women after childbirth to
give them strength.
Roots used as a medicine for
stomach
pains
and
general
weakness.
Juice of boiled leaves used as
medicine for babies.
The roots are chewed as a cough
remedy and water is drunk at the
same time. The roots have a strong
taste, and are also used as an
emetic.
Roots and leaves dried, pounded or
ground into powder form and
applied on wounds.
The roots are chewed as a remedy
for sore throat and cold in the chest.
The roots are chewed as a remedy
for cold in the chest. Roots are also
boiled and the infusion taken in
broth as a cure for venereal
diseases.
Roots used as a medicine for
stomach pains. Leaves used for
snake bite treatment, and for
headache. Aerial parts are used as
laxative, deobstruent and diuretic,
useful in treating cough, biliary
febrile attacks, obstructions of the
liver,
spleen
and
kidneys.
Anthelmintic for children and
chronic diarrhoea.
Roots dug out, boiled, mixed with
milk and drunk for pain in the liver
and spleen.
Ngong hills (Kikuyu,
Maasai)
Kyulu hills (Kamba)
Kokwaro, 1993;
Beentje, 1994;
Agnew et al., 1994.
Kitui (Kamba), Kisumu
(Luo), Machakos
Agnew et al., 1994
Beentje, 1994
Western Kenya
(Luhya)
Makueni (Kamba),
Magadi (Maasai)
Kokwaro, 1993
Coastal region
(Nyika)
Kokwaro, 1993;
Coastal region
(Digo)
Coastal region
(Digo),Kibwezi
Kamba) Kajiando
(Maasai)
Agnew et al., 1994;
Kokwaro, 1993
Agnew et al., 1994
Kokwaro, 1993
Kilifi
(Giriama),
Machakos,
(Kamba)
Kokwaro, 1993;
Agnew et al., 1994;
Almad et al.,1999.
Coastal region (Digo),
Kibwezi,
(Kamba)
Kokwaro, 1993;
Agnew et al., 1994
25
Kokwaro, 1993;
Agnew et al., 1994.
2.3.3 Biological activities of the genus Tephrosia
Based on the wide ethno-medical uses of Tephrosia, chemical investigations have
resulted to the isolation of active compounds from these plants. Examples of such
bioactive compounds are flavonoids including the isoflavonoids and rotenoids.
Rotenoids show activity against insects, and exhibit strong cytotoxic activity [Andrei et
al., 1997]. Rotenone (7), was found to have insecticidal properties [Ramen et al., 1992].
Tephrosin (15) hsa been shown to be active against tumours including skin cancer
[Andrei et al., 1997]. T. purpurea has quite a number of traditional medicinal uses as
shown in Table 2.2. and T. purpurea is a well-known herb for its hepatoprotective,
anticancer, antiulcer, antibacterial and in healing bleeding piles and wounds [Santram et
al., 2006]. These observed biological activities could be due to the presence of the
compounds such as lipophilic flavonoid aglycones (flavanones, flavonols, flavones and
chalcones) in the plant extracts [Santram et al., 2006]. The roots of T. emoroides yielded
emoroidenone (26) which showed insect anti-feedant activity against the larvae of stalk
borer, Chillo partellus (Machocho et al., 1995). The roots of T. hildebrandtii yielded
hildecarpin (27) which exhibited insect anti-feedant activity against the legume podborer, Maruca testulalis as well as anti-fungal properties [Lwande et al., 1986].
26
Pongamol (28) which was isolated from T. lanceolata and T. purpurea is used in
insecticides and pesticides manufacture [Parmar et al., 1989]. Rotenone (7) is widely
distributed in the Leguminosae including many Tephrosia species is used as antineoplastic agent, contact insecticide and pesticide, potent mitochondrial poison and toxic
against Artemia salina [Dagne et al., 1989]. Pseudosemiglabrin (29), isolated from T.
apollinea is used as platelet aggregation inhibitor [Waterman et al., 1980]. 4Methoxymaackiain (30) which is a constituent of T. aequilata (root) showed antifungal
activity [Tarus et al., 2002]. -Toxicarol (31) which is obtained from the stem of T.
odorata and T. toxicaria is used as fish poison closely related in properties to rotenone
(7) [Jang et al., 2003].
27
2.3.3.1 Flavonoids as antimalarial agents
The naturally occurring dihydrochalcone glycoside, phlorizidin (32) from Micromelum
tephrocarpum (Rutaceae), a plant used ethnomedically for the treatment of malaria, was
one of the first chalcones shown to posses anti-parasitic activity. Phlorizidin (32) is said
to inhibit the induced permeability in Plasmodium-infected erythrocytes to various
substrates including glucose [Induli, 2006]. Ever since anti-plasmodial flavonoids were
detected from Artemisia annua (Asteracae), flavonoids have attracted renewed interest
28
(Yenesew et al., 2003; Trease and Evans, 2002). Other Artemisia species have been
tested, and exiguaflavanone A (33) and B (34) isolated from Artemisia indica exhibited
in vitro activity against P. falciparum with IC50 values of 4.6 and 7.1 g/ml respectively
[Induli, 2006]. Among the flavonoids belonging to the genus Erythrina, the flavanone
abyssinone-IV (14) isolated from the roots of E. abyssinica showed high activity against
both strains of P. falciparum [Yenesew et al., 2003]. Licochalcone A (13) first isolated
from Glycrrhiza glabra (Fabaceae) is another example of a naturally occurring chalcone
which exhibited activity in vitro and in vivo against chloroquine-sensitive and
chloroquine-resistant strains of P. falciparum. Thus, it has provided a lead structure to
design and synthesise chalcones and bischalcones as new anti-malarial drugs [Taylor
and Triggle, 2007]. Different classes of flavonoids including; chalcones, flavanones and
isoflavones have been reported as antiplasmodial agents among plant metabolites.
Recently pterocarpans, pterocarpenes and isoflavenes have also been identified to
represent new sub-classes of isoflavonoids with antiplasmodial activities [Yenesew et
al., 2003].
29
2.4 Phytochemical Information on the genus Tephrosia
Phytochemical investigation of the genus Tephrosia has resulted in the isolation of
different classes of flavonoids among them flavanones, flavones, flavans, flavens,
isoflavones, flavanol, chalcones, rotenoids and pterocarpans.
2.4.1 Flavonoids
The term “flavonoid” is generally used to describe a broad collection of natural products
that include a C6-C3-C6 carbon frame work or more specifically a phenylbenzopyran
functionality. They constitute one of the largest groups of naturally occurring phenols
[Markham, 1982]. They are virtually found in all species of terrestrial plants and the
relatively advanced Algae family [Induli, 2006]. It has been estimated that about 2% of
all carbon photosynthesized by plants is converted into flavonoids or closely related
compounds [Markham, 1982]. Flavonoids are widely distributed in higher plants.
However, the interest on biological activities of these compounds has been very limited.
30
However, there is growing interest on plant flavonoids as human dietary compounds and
as pharmacological agents [Harborne et al., 1986].
In plants, flavonoid aglycones occur in a variety of structural forms. They contain fifteen
carbon atoms in their basic nucleus and these are arranged in a C6-C3-C6 configuration.
Each C6 represents an aromatic ring. These aromatic rings are linked by a three carbon
unit which form a third heterocyclic ring via cyclization with one of the aromatic ring
via an oxygen atom. The aromatic rings are labelled as ring A and B and heterocyclic
ring as ring C. Depending on the position of the linkage of the aromatic ring to the
benzopyrano moiety, this group of natural products may be divided into three classes:
the
flavonoids
(2-phenylbenzopyrans),
isoflavonoids
(3-benzopyrans)
and
the
neoflavonoids (4-benzopyrans). These groups usually share a common chalcone
precursor, and thus are biogenetically and structurally related [Agrawal, 1989].
The flavonoids sensu lato are classified into flavonoids and isoflavonoids based on the
basis of the attachment of the B-ring on the phenyl propane system. In addition to this,
different degrees of oxidation result into different sub-classes of flavonoids and
isoflavanoids [Markham, 1982]. For instance, those flavonoids which possesses ‘2phenylchromone skeleton as such is designated as ‘flavones’. The 3-hydroxy derivative
of flavone is termed as ‘flavonol’. Flavonoids having 3-phenylchromanone skeleton are
designated as ‘flavanone’ or ‘dihydroflavones’. Similarly, 3-hydroxy substituted
flavanones are termed as ‘flavanonol’ or ‘dihydroflavonol’ [Agrawal, 1989]. Fig. 2.4
31
below shows the basic skeleton of flavonoids and isoflavonoids and the numbering
system.
Figure 2.4: Basic skeletons of flavonoids and isoflavonoids
Natural flavonoids and isoflavonoids are usually oxygenated and bear hydroxyl or
methoxyl substituents. A large number of flavonoids occur as O-glycosides in which one
or more of the hydroxyl groups of the flavonoid are bound to a sugar or sugars via an
acid labile hemiacetal bond [Agrawal, 1989].
2.4.1.1 Biosynthesis of Flavonoids
All flavonoids sensu lato are biosynthesized from common precursors which incorporate
both shikimate and acetate malonate pathways. The flavonoids initially formed in the
biosynthesis are chalcones and all other forms are derived from these by a variety of
routes.
The Scheme 2.1 below summarizes the biosynthesis of isoflavonoids. They are
synthesized by extension of p-hydroxycoumaroyl CoA with three molecules of malonyl
32
CoA in a head-to-tail manner in order to form a tetraketide intermediate. The process is
catalyzed by the enzyme chalcone synthase (CHS). The intermediate then folds and
condenses further to give a chalcone. This reaction is the first committed step in
isoflavonoid biosynthesis and is also catalyzed by chalcone synthetase (CHS). Fabaceae
species
biosynthesize
two
types
of
isoflavonoids,
the
first
type
are
5-
hydroxyisoflavonoids such as genistein (35) and the second type are 5deoxyisoflavonoids such as daidzein (36). In order to synthesize 5-deoxyisoflavonoids
NADPH reductase and CHS should act as catalysts together [Derese, 2004].
Chalcone isomerase (CHI) is the second enzyme involved in the biosynthesis of
isoflavonoids and it catalyzes the stereospecific intramolecular cyclization of
isoliquiritigenin (37) and naringeninchalcone (38) into a (2S)-liquiritigenin (7, 4’dihydroxyflavanone) (39) and (2S)-naringenin (5, 7, 4’-trihydroxyflavanone) (40),
respectively [Derese, 2004; Dewick, 2002]. These flavanones (39) and (40) are the
precursors for the construction of 5- deoxyisoflavonoids and 5-hydroxyisoflavonoids
skeletons and flavonoids in general.
The enzyme isoflavone synthetase (IFS) converts the flavanone substrates to
liquiritigenin and naringenin to the isoflavones daidzein (36) and genistein (35),
respectively. This reaction is proposed to involve two steps: the 2-hydroxylation and aryl
migration of flavanone substrates to yield a 2-hydroxyisoflavanone, followed by a
dehydration step to the corresponding isoflavone derivative. Daidzein (36) and genistein
33
(35) are then further metabolised to give the various classes of isoflavonoids [Derese,
2004; Dewick, 2002].
Scheme 2.1: Biosynthesis of chalcones and isoflavonoids [Derese, 2004; Dewick,
2002].
34
Scheme 2.2: Biosynthetic interrelationships among different flavonoids [Induli,
2006; Dewick, 2002]
35
The biosynthetic interrelationships among different flavonoid types are summarized in
Scheme 2.2 above [Induli, 2006; Markham, 1982]. The variation in structure among the
various flavonoid and isoflavonoid classes has been achieved by the loss of hydroxyl
groups, by the introduction of an additional hydroxyl groups, by methylation or
formation of methylene-dioxy groups, by attachment of C-prenyl, and structural
modifications of these such as dimethylpyrano and furano rings [Induli, 2006; Dewick,
2002].
2.4.2 Compounds Reported from Tephrosia
2.4.2.1 Flavanones of Tephrosia
Flavanones possess 2-phenylchromanone as the parent skeleton. Since carbon-2 of the
flavanones molecule is an asymmetric centre, two isomeric forms of each structure are
possible but most of the naturally occurring flavanones acquire phenyl substituent at C-2
position in pseudoequatorial orientation [Agrawal, 1989]. Fig. 2.5 shows the basic
skeleton of flavanones and the numbering system.
Figure 2.5: Flavanone (dihydroflavone)
36
To date, quite a number of flavanones have been characterised from various species of
the genus Tephrosia. Nearly 50% of these flavanones are prenylated at C-8 on ring A
and in all except lupinifolin (46), ring B is unsubstituted. Most of these flavanones are
found in the aerial parts, stem and in the roots of the Tephrosia plants [Rao et al., 1994;
Jang et al., 2003; Chang et al., 2000]. Flavanones are known to have antimicrobial
activities and probably are synthesized by these plants for defensive purpose [Maillard et
al., 1987]. Table 2.3 gives a summary of these flavanones.
Table 2.3:
Flavanones of Tephrosia
Flavanones
Biological source
Candidone (41)
T. elata (RT)
Fulvinervin A (42)
T. fulvinervis (SD)
Epoxycandidone (43)
T. hamiltonii (WP)
Tephroleocarpin A (44)
T. leiocarpa (RT)
Tephroleocarpin B (45)
T. leiocarpa (RT)
Lupinifolin (46)
T. lupinifolia (RT)
Maximaflavanone A (47)
7-Methoxy-8-(3-methoxy-3-methyl-1butenyl)flavanones (48)
Isolonchocarpin (49)
T. maxima (RT)
T. purpurea (RT)
Dehydroisoderricin (50)
Purpurin (51)
Purpurin, 7a, 10, 10a-Triepimer (52)
Tephroglabrin (53)
T. purpurea (RT)
T. purpurea (AP)
T. purpurea (RT)
T. purpurea (RT)
Tephrorin A (54)
Tephrorin B (55)
Quercetol C (56)
T. purpurea (AP)
T. purpurea (AP)
T. quercetorum (ST)
T. purpurea (RT)
References
Lwande, 1985
Rao et al., 1985
Hussaini et al., 1987
Gomez-Garibay et
al., 1988
Gomez-Garibay et
al., 1991
Smalberger et al.,
1974
Rao et al., 1994
Waterman et al.,
1985
Waterman et al.,
1980
Rao et al., 1984
Chang et al., 2000
Rao et al., 1984
Waterman et al.,
1980
Chang et al., 2000
Chang et al., 2000
Gomez-Garibay et
al., 1988
Rao et al., 1992
Rao et al., 1992
Jang et al., 2003
Spinoflavanone B (57)
T. spinosa (RT)
Spinoflavanone A (58)
T. spinosa (RT)
5-Hydroxy-7-methoxy-8-(3-oxo-1T. toxicaria (ST)
butenyl)flavanones (59)
Tephrinone (60)
T. villosa (SD)
Kishore et al., 2003
Tephrowatsin C (61)
T. watsoniana (ST)
Gomez et al., 1985a
Key: RT – roots, SD – seeds, WP – whole plant, AP – aerial parts, ST – stem
37
38
39
40
2.4.2.2 Flavones of Tephrosia
Flavones are 2,3-dehydroderivative of the flavanones which have 2,3-olefinic bond
[Agrawal, 1989]. Flavones have been reported from the genus Tephrosia. Table 2.4
below shows a list of the flavones of this genus.
Table 2.4: Flavones of Tephrosia
Flavones
Biological source
Reference
5-Hydroxy-7-methoxy- T. abbottiae (ST)
Gomez-Garibay et al., 1986
8-prenylflavone (62)
Apollinine (63)
T. apollinea (SD)
Waterman et al., 1980
Glabratephrin (64)
T. apollinea (SD)
Waterman et al., 1980
Glabratephrinol (65)
T. apollinea (SD)
Waterman et al., 1980
Lanceolatin A (66)
T. apollinea (SD)
Waterman et al., 1980
Pseudosemiglabrin (67) T. apollinea (SD)
Waterman et al., 1980
Pseudosemiglabrinol
T. apollinea (SD)
Waterman et al., 1980
(68)
Semiglabrin (69)
T. apollinea (SD)
Waterman et al., 1980
Emoroidone (70)
T. emoroides (RT)
Machocho et al., 1995
Fulvinervin B (71)
T. fulvinervis (SD)
Rao et al., 1985
Fulvinervin C (72)
T. fulvinervis (SD)
Venkataratnam et al., 1986
Hookerianin (73)
T. hookeriana (SD)
Prabhakar et al., 1996
Tachrosin (74)
T. polystachyoides (ST) Smalberger et al., 1972
5-Methoxy-6,6T. praecans (SD)
Camele et al., 1980
dimethylpyrano[2,3:7,6]
flavones (75)
Pongaglabol (76)
T. purpurea (AP)
Ahmad et al., 1999
Key: RT – roots, SD – seeds, AP – aerial parts, ST – stem
41
42
2.4.2.3 Isoflavones of Tephrosia
Isoflavones have been reported from the genus Tephrosia. Calopogoniumisoflavone B
(78) has a pyrano-ring on ring A at 7,8- position while Pumilaisoflavone C (90) is
prenylated at C-7. Biosynthetically, these isoflavones (C-5 oxygenated) are derived from
(2S)- liquiritigenin (49) which lead to 7,4'-oxygenation. Table 2.5 below gives a list of
the isoflavones isolated from Tephrosia.
43
Table 2.5: Isoflavones of Tephrosia
Isoflavones
Biological source
References
Scandenone (77)
T. elata (RT)
Lwande, 1985
Calopogoniumisoflavone B (78)
T. maxima (RT)
Murthy et al., 1985
Maximaisoflavone J (79)
T. maxima (RT)
Murthy et al., 1985
Maximaisoflavone B (80)
T. maxima (RT)
Murthy et al., 1985
2',4',5',7,8T. maxima (PD & RT) Rao et al., 1984
Pentahydroxyisoflavone (81)
2',7,8-Trimethoxy-4',5'T. maxima (PD & RT) Rao et al., 1984
methylenedioxyisoflavone (82)
Maximaisoflavone G (83)
T. maxima (PD & RT) Rao et al., 1984
Maximmaisoflavone C (84)
T. maxima (PD & RT) Rao et al., 1984
Maximaisoflavone E (85)
T. maxima (PD & RT) Rao et al., 1984
Maximaisoflavone D (86)
T. maxima (PD & RT) Rao et al., 1984
Maximaisoflavone A (87)
T. maxima (PD & RT) Rao et al., 1984
Maximaisoflavone H (88)
T. maxima (PD & RT) Rao et al., 1985
4'-OT. polyphylla (RT)
Dagne et al., 1992
Demethyltoxicarolisoflavone (89)
Pumilaisoflavone C (90)
T. pumila (SD & PD ) Yenesew et al., 1989
Pumilaisoflavone B (91)
T. pumila (PD)
Dagne et al., 1988
Pumilaisoflavone D (92)
T. pumila (SP)
Yenesew et al., 1989
Pumilaisoflavone A (93)
T. pumila (SP)
Yenesew et al., 1989
Purpuranin A (94)
T. purpurea (PD)
Rao et al., 1984
4',7-Dihydroxy-3',5'T. purpurea (AP)
Chang et al., 2000
dimethoxyisoflavone (95)
Elongatin (96)
T. viridiflora (ST)
Gomez et al., 1985b
Viridiflorin (97)
T. viridiflora (ST)
Gomez et al., 1985b
Key: RT – roots, SD – seeds, PD - pods, AP – aerial parts, ST – stem
44
45
46
2.4.2.4 Chalconoids of Tephrosia
Chalconoids being the initial products in biosynthesis of flavonoids occur in a variety of
structural forms. The term chalconoids include all compounds which possesses 1,3diarylprop-2-en-1-one carbon frame work as the parent skeleton. The characteristic
feature of these compounds is the presence of olefinic bond and a keto group. In few
cases,
hydroxyl
group
was
found
to
be
substituted
at
C-resulting
to
hydroxychalcones [Gomez-Garibay et al., 2002; Dewick, 2002]. The chalcones are
the most common and wide-spread group of chalconoids possessing 1,3-diarylprop-2en-1-one
as the basic skeleton [Agrawal, 1989]. Compounds belonging to the
chalcanoids class are derived from 1, 3-diarylpropane as the parent carbon skeleton
which may or may not possess a hydroxyl or an olefinic bond. The most important
feature of these compounds is the absence of the keto group [Agrawal, 1989]. The Fig
2.6 shows the basic skeletons of chalconoids and chalcanoids with their numbering
system.
Figure 2.6: Basic skeleton of chalcones and chalcanes
47
In chalcones the A ring, normally written to the left, is given primed numbers, while the
B ring carbons are given unprimed numbers. The exocyclic carbons are designated
and relative to the carbonyl function. In the genus Tephrosia, chalconoids have been
reported and they include; chalcones, chalcan-1,3-dione and a chalcene. Majority of the
chalcones of this genus are oxygenated at C-2'. Praecansone B (98) and purpurenone
(105) have a pyrano-ring attached to ring A. Table 2.6 below lists the chalconoids of the
genus Tephrosia.
Table 2.6: Chalconoids of the genus Tephrosia
Chalconoids
Biological source
References
Praecansone B (98)
T. aequilata (RT)
Tarus et al., 2002
Tephrone (99)
T. candida (SD)
Tanaka et al., 1992
Ovalichacone (100)
T. candida (SD)
Roy et al., 1986
Epoxyobovatachalcone (101)
T. carrollii (RT)
Gomez-Garibay et al., 2001
Crassichalcone (102)
T. crassifolia (RT & AP)
Gomez-garibay et al., 1999
2',6'-Trihydroxy-4'-methoxy-
T. major (RT & AP)
Gomez-Garibay et al., 2002
Praecansone A (104)
T. praecans (RT)
Tarus et al., 2002
Purpurenone (105)
T. purpurea (AP)
Rao et al., 1984
Tepropurpurin (106)
T. purpurea (AP)
Chang et al., 1997
Teprosone (107)
T. purpurea (FT & FL)
Chang et al., 2000
Spinochalcone B (108)
T. spinosa (RT)
Rao et al., 1992
Spinochalcone C (109)
T. spinosa (RT)
Rao et al., 1992
Spinochalcone A (110)
T. spinosa (RT)
Rao et al., 1992
Tunicatachalcone (111)
T. tunicata (RT)
Andrei et al., 2000
3'-prenylchalcone (103)
Key: RT – roots, SD – seeds, FT - fruit, FL – flowers, AP – aerial parts
48
49
50
2.4.2.5 Rotenoids of Tephrosia
Rotenoids is a general name for a class of isoflavonoid compounds containing an extra
carbon in an additional heterocyclic ring. The C-2 of the isoflavanone skeleton bears an
extra methylene carbon (C-11), which get cyclised with C-2' of ring B via an epoxy
bridge and thus forming a tetracyclic ring system. Rotenoids possess 2-methlene, 2'epoxy isoflavanone skeleton [Agrawal, 1989].
The genus Tephrosia is known for the presence of rotenoids normaly: rotenone (7)
(James et al., 1958), deguelin (6) [Yenesew, 1997] and tephrosin (15) [Kiplagat, 2006].
Other common rotenoids isolated from this genus are listed in Table 2.7 below.
51
Table 2.7: Rotenoids of the genus Tephrosia
Rotenoids
Dehydrodeguelin (112)
Dehydrodihydrorotenone (113)
Dehydrorotenone (114)
Dihydrostemonal (115)
6-O-Acetyldihydrostemonal (116)
9-Demethyldihydrostemonal (117)
6-Hydroxyrotenone (118)
4',5'-Dihydo-5', 11-dihydroxy-4'methoxytephrosin (119)
Biological source
T. candida (RT)
T. candida (RT)
T. falciformis (PD)
T. pentaphylla (RT)
T. pentaphylla (RT)
T. pentaphylla (RT)
T. pentaphylla (RT)
T. toxicaria (ST)
Reference
Crombie et al., 1998
Roy et al., 1987
Roy et al., 1987
Dagne et al., 1989
Dagne et al., 1989
Dagne et al., 1989
Dagne et al., 1989
Jang et al., 2003
Sumatrol (120)
T. toxicaria (ST)
Prashant et al., 1993
Toxicarol (121)
T. toxicaria (ST)
Andrei et al., 1997
9-O-Demethyl-6-O-methyl-8prenylstemonal (122)
6-Hydroxysumatrol (123)
T. villosa (SD)
Prashant et al., 1993
T. villosa (PD)
Prashant et al., 1993
Villosol (124)
T. villosa (PD)
Prashant et al., 1993
Didehydrovillosin (125)
T. villosa (PD)
Prashant et al., 1993
Villinol (126)
T. villosa (PD)
Prashant et al., 1993
Villosone (127)
T. villosa (PD)
Prashant et al., 1993
Key: Key: RT – roots, SD – seeds, FT - fruit, FL – flowers, AP – aerial parts
52
53
54
2.4.2.6 Pterocarpanoids of the genus Tephrosia
Pterocarpanoids are the second largest group of isoflavonoids [Dewick, 1994].
Pterocarpanoids tend to be phytoalexins, which are toxic compounds produced by plants
following microbial infections, constituting a natural defence mechanism against
microorganisms [Ingham, 1980]. Pterocarpanoids occur mostly in the root and stem bark
presumably for defence purpose against microbial attacks.
Among the 12 pterocarpanoids that have been characterised from this genus, 3 are
pterocarpans, 5 are 6a-hydroxypterocarpans, 3 are coumestan and one pterocarpene. The
division into the four above-mentioned groups depends on the level of oxidation in ring
B and at the B - C ring junction. Table 2.8 below lists some of the pterocarpanoids of
Tephrosia.
Table 2.8: Pterocarpanoids of the genus Tephrosia
Pterocarpanoids
Biological source
Acanthocarpan (128)
T. bidwilli (LV)
Tephrocarpin (129)
T. bidwilli (LV)
Tephcalostan (130)
T. calophylla (WP)
Emoroidocarpan (131)
T. emoroides (RT)
2-O-Methyllucernol (132)
T. hamiltonii (RT)
Hildecarpidin (133)
T. hildebrandtii (RT)
Key: RT – roots, LV – leaves, WP – whole plant
55
Reference
Ingham et al., 1980
Ingham et al., 1980
Kishore et al., 2003
Machocho et al., 1995
Rajani et al., 1988
Lwande et al., 1987
56
2.4.2.7 Other compounds from the genus Tephrosia
Thus far, three flavans, flavan-4-ols, flavan-3,4-diol and a flavanonol are reported from
the genus Tephrosia among others. Some like crassifolin (134) and tepicanol A (143)
exist as dimmers hence referred to as biflavanoids. Abbottin (137) and tephrowatsin B
(147) possess a double bond between C-3 and C-4, hence referred to as flavenes. Table
2.9 below shows a summary of the flavanoids and isoflavanoids of the genus Tephrosia.
Flavonols and 3-methoxyflavones have also been reported from Tephrosia. Examples
include; candinol (148), candirone (149) isolated from the roots and seeds of T. candida
[Dutt et al., 1983; Parmar et al., 1987] and 7-Ethoxy-3,3',4'-trihydroxyflavone (150)
from the roots of T. procumbens [Tarus et al., 2002; Venkataratnam et al., 1987].
Table 2.9: Other compounds isolated from Tephrosia
Compound
Biological Source
Reference
Crassifolin (134)
T. crassifolia (RT)
Gomez-garibay et al., 1999
Hildgardtol A (135)
T. crassifolia (RT)
Gomez-garibay et al., 1999
Methylhidgardtol A (136) T. crassifolia (RT)
Gomez-garibay et al., 1999
Abbottin (137)
T. emoroides (RT)
Machocho , A.K., 1995
Methylhidgardtol B (138) T. hildebrandtii (RT)
Gomez-garibay et al., 1986
Hildgardtol B (139)
T. quercetorum (RT/AP)
Gomez-garibay et al., 1988
Quercetol A (140)
T. quercetorum (AP)
Gomez-garibay et al., 1988
Quercetol B (141)
T. quercetorum (AP)
Gomez-garibay et al., 1988
Astraciceran (142)
Tephrosia strigosa (LV)
Ingham et al., 1980
Tepicanol A (143)
T. tepicana (RT &AP)
Gomez-garibay et al., 1997
Tephrowatsin A (144)
T. watsoniana (ST)
Gomez et al., 1985a
Tephrowatsin E (145)
T. watsoniana (ST)
Gomez et al., 1985a
5,7-Dimethoxy-8T. watsoniana (ST)
Gomez et al., 1985a
prenylflavan (146)
Tephrowatsin B (147)
T. watsoniana (ST)
Gomez et al., 1985a
Key: RT – roots, ST – stem, LV – leaves, AP – aerial parts
57
58
59
Fig .2.7 below shows a summary of some of the sub-classes of compounds reported
from the genus Tephrosia.
Figure 2.7: Summary of sub-classes of compounds from genus Tephrosia
60
CHAPTER THREE
3.0 MATERIALS AND METHODS
3.1 General
The 1H-NMR (300 or 200 MHz) and
13
C-NMR (75 MHz or 50 MHz) spectra were
recorded on Bruker or Varian-Mercury spectrometers using TMS as internal standard.
Chemical shifts were measured in ppm in values relative to TMS. HMQC and HMBC
spectra were acquired using the standard Bruker software. EIMS spectra were recorded
on a direct inlet, 70 eV, on SSq 710, Finnigan MAT mass spectrometer. UV spectra
were recorded using SP8 150 UV/VIS spectrophotometer. CD was run using JASCO J170 spectropolarimeter. Melting points were recorded using a Gallenkamp melting point
apparatus with capillary tubes.
Column chromatography was carried out using silica gel 60 (70-230 mesh) and
Sephadex LH 20. Analytical TLC was done using Merck pre-coated silica gel 60 F254
plates. Preparative thin layer chromatography (PTLC) was done on silica gel (Merck).
PTLC plates were prepared by adding 200 ml of water to 80 g of silica gel. Slurry was
formed and allowed to stand for 30 minutes. The slurry was then poured and spread
evenly on clean 20 cm2 glass plates and was left to dry at room temperature. Activation
of the silica gel was done in the oven for 30 minutes at a 383 k temperature, removed
and allowed to cool at room temperature ready for use. Chromatographic zones were
detected under UV (254, 366 nm) light and/or exposing in some cases to iodine vapour.
61
3.2 Reagents
Organic solvents; n-hexane, dichrolomethane, ethyl acetate, methanol, acetone, acetic
acid, acetic anhydride and Iodine crystals were sourced from Kobian, Nairobi, Kenya
and Sigma chemical company, St. Louis, USA. All the solvents were distilled prior to
use.
3.2.1 Apparatus
All reusable glassware (test tubes, conical flasks, round bottomed flasks, measuring
cylinders, vials, beakers, volumetric flasks, teat pipettes) were soaked in hot water with
liquid detergent before washing thoroughly and rinsing with distilled water. They were
then dried in an electric oven at about 105 0C for about 1 hour and allowed to cool
slowly to room temperature. Just before use, the apparatus were rinsed with a mixture of
distilled solvents to remove any organic impurities.
3.2.2 Test organisms
The standard test organisms (D6 and W2 strains of Plasmodium falciparum) were
obtained from the United States Army Medical Research Unit-Kenya, Walter Reed
Project, Kisumu (courtesy of Mr Hoseah M. Akala), all preserved at -20 0C.
The eggs of Aedes aegypti L. (Diptera: Culicidae) were obtained from the Department of
Zoology, University of Nairobi.
62
3.3 Plant Materials
3.3.1 Collection of plants materials
The roots, stems, leaves and seedpods of Tephrosia elata and Tephrosia aequilata were
collected from their natural habitats; T. elata was obtained from Kilungu hills in
Makueni district in August, 2007, and T. aequilata obtained from Nzaui hills in Makueni
district in November, 2007. The plant species were identified by Mr. Patrick C. Mutiso
of the University Herbarium, School of Biological Sciences, at the University of
Nairobi, where a voucher specimen (Mutiso- 027 / August 2007 for T. elata and (Mutiso
- 028/November 2007) for T. aequilata are deposited.
3.3.2 Preliminary processing of the samples
After collection, each of the plant samples was separated into different parts, seedpods,
stem and leaves. They were then air dried for about two weeks at room temperature by
spreading evenly in the open drying area. The samples were ground separately into fine
powder using a Willy mill. About 30 g of the ground seedpods and stem of each plant
were exhaustively extracted with CH2Cl2/MeOH (1:1) to obtain the organic extracts for
preliminarily investigation of phytochemical profile and antiplasmodial and larvicidal
activities. The extracts were filtered through Whatman No.1 filter paper and solvent
removed using a rotary evaporator. The extracts were divided into two portions, one for
phytochemical evaluation and the other for biological evaluation. The later was stored in
sterile air-tight vials at 4 0C in readiness for bioassay tests (Harborne, 1998).
63
3.3.3 Preliminary phytochemical profile evaluation
Thin layer chromatography was carried out on each extract using CH2Cl2/EtOAc (4:1)
and 100% dichloromethane as solvent systems. The spots after development were
viewed under a UV light and the number of spots observed for each sample recorded.
3.4 Extraction and Isolation of Compounds
3.4.1 Extraction and isolation of compounds from the seedpods of T.
elata
The air dried and ground seedpods (1.7 Kg) of T. elata were extracted with
dichloromethane- methanol (1:1) solvent system by cold percolation at room
temperature (3 X 1.5 L). The solvent was removed under vacuum by use of a rotary
evaporator at 35 0C afforded a brown oily extract (53 g). A portion of the extract (50 g)
was subjected to CC on silica (500 g) eluting with hexane containing increasing
percentage of ethyl acetate (3%, 5%, 7%, 10%, 13%, 15%, 20% and 30% ethyl acetate
in hexane each of ca 1 L). The fraction eluted with 3% EtOAc in n-hexane was further
separated on Sephadex LH-20 column (eluent CH2Cl2/MeOH, 1:1) and purified by
PTLC on silica gel (hexane/CH2Cl2, 3:2) to yield compound 3 (3.5 mg) and compound 4
(24.8 mg) [Andrei et al., 2000]. The fraction which was eluted with 10% EtOAc in
hexane was purified by PTLC (hexane/acetone, 9:1) and yielded compound 1 (89.4 mg).
The fraction eluted with 13% EtOAc in hexane was also purified by PTLC
(hexane/CH2Cl2/EtOAc, 5:9:1) to give crystals of compound 5 (78.5 mg) [Andrei et al.,
64
2000] and a mixture of compound 6 and compound 7 (40.6 mg) [Andrei et al., 1997;
Yenesew, 1997; Dagne et al., 1991].
3.4.2 Extraction and isolation of compounds from the seedpods of T.
aequilata
1.8 Kg of the air dried seedpods were ground and extracted with dichloromethanemethanol (1:1) solvent system by cold percolation at room temperature (3 X 1.5 L). The
extract was filtered and the solvent removed under vacuum using a rotary evaporator at
35 0C to yield 64 g of a dark brownish oily paste. A portion of the extract (50 g) was
subjected to CC on silica (500 g) eluting with hexane containing increasing percentage
of ethyl acetate (3%, 5%, 7%, 10%, 13%, 15%, 20% and 30% ethyl acetate in hexane
each of ca 1 L). The fraction that was eluted with 7% ethyl acetate in hexane was further
subjected to column chromatography on Sephadex LH-20 {CH2Cl2/MeOH (1:1)} and
the major fraction was further purified by PTLC (5 % EtOAc in hexane) to yield
compound 8 (82 mg) and 9 (20 mg) [Tarus et al., 2002; Machocho et al., 1995; Dagne et
al., 1990; Yenesew at al., 1989]. The fractions that were eluted with 10 – 20 % ethyl
acetate in hexane were combined and subjected to Sephadex LH-20 column {
CH2Cl2/MeOH (1:1)} and the major fraction was further purified by PTLC (25 % EtOAc
in hexane) to give additional compound 5 (26 mg) [Andrei et al., 2000; Machocho et al.,
1995].
65
3.4.3 Acetylation of compound 1
In a round bottomed flask containing compound 1 (35 mg), acetic anhydride (excess)
and pyridine (1 drop) was added and the mixture was allowed to stand for 12 hours. The
reaction mixture was poured over ice-water and stirred in ice-bath. The product
precipitated was filtered and washed with water. The precipitate was taken up with
CH2Cl2 and dried with Na2SO4 and filtered. The filtrate was then transferred into a round
bottomed flask and the solvent removed using a rotary evaporator under vacuum.
Purification of the product by PTLC yielded monoacetate compound 2 (26 mg).
3.5 Physical and Spectroscopic Data of the Isolated Compounds
3.5.1 Compound 1
.8
Light yellowish oil. Rf = 0.2 (hexane/EtOAc, 9:1). [ ] 28
= + 34.50 (c 0.71, CHCl3). UV
D
max (MeOH, Log nm: 274.5 (0.83), 295.5 (0.32), 308 (0.30), 349 (0.07) nm. CD
(MeOH, 0.01): [Ө]350 +3187, [Ө]290 -8346. HRMS found: 355.1535, calculated for
C21H23O5 (Appendix A). 1H NMR (CDCl3, 300 MHz): H 7.26 -7.44 (m, H-2, -3, -4, -5, 6), 5.87 (s, H-5'), 3.45 (dd, J = 3.0, 18.0 Hz, H-), 3.34 (dd, J = 9.0, 18.0 Hz, H-), 5.28
(dd, J = 3.0, 9.0 Hz, H-), 5.46 (d, J = 10.1 Hz, H-3''), 6.66 (d, J = 10.1 Hz, H-4''), 1.44
(s, Me2-2''), 3.78 (s, MeO-6'), 13.98 (s, 2'-OH).
C NMR (CDCl3, 75 MHz), C 143.4
13
(C-1) 125.9 (C-2/6), 128.4 (C-3/5), 127.4 (C-4), 105.6 (C-1'), 161.9 (C-2'), 102.9 (C-3'),
160.7 (C-4'), 91.4 (C-5'), 163.0 (C-6'), 52.7 (C-), 70.2 (C-), 78.3 (C-2''), 125.5 (C-3''),
115.8 (C-4''), 28.4 (Me2), 55.7 (MeO-6'), 204.2 (C=O). EIMS (m/z, rel int): 354 (52,
66
[M]+), 339 (15, [M-Me]+), 336 (15, [M-H20]+), 321 (55, [M-Me-H20]+), 233 (98,
C13H13O4), (217 (100, C12H9O4)), 107 (9, C7H7O), (Appendix A).
3.5.2 Compound 2
Yellowish oil. Rf = 0.44 (hexane/EtOAc, 9:1). UV max (MeOH, Log ) nm: 276.0 (0.75),
295.5 (0.67), 342.5 (0.40), 451 (0.02). HRMS found: 399.1721, calculated for C23H27O6.
EIMS (m/z, rel int): 398.17 (30, [M]+), {397.16 (100, C23H25O6)}. 1H NMR (CDCl3, 300
MHz): 7.27 – 7.41 (m, H-2, -3, -4, -5, -6), 5.88 (s, H-5'), 3.44 (dd, J = 4.5, 17.1 Hz,
H-), 3.62 (dd, J = 8.7, 17.1 Hz, H-), 6.38 (dd, J = 4.5, 8.7 Hz, H-), 5.45 (d, J = 10.2
Hz, H-3''), 6.64 (d, J = 10.2 Hz, H-4''), 1.44 (s, Me2-2''), 3.83 (s, MeO-6'), 13.99 (s, 2'OH), 2.03 (s, OCOCH3).
13
C NMR (CDCl3, 75 MHz): C 140.4 (C-1), 126.7 (C-2/6),
128.5 (C-3/5), 128.0 (C-4), 105.5 (C-1'), 161.9 (C-2'), 102.9 (C-3'), 160.3 (C-4'), 91.2
(C-5'), 162.6 (C-6'), 50.3 (C-), 71.9 (C-78.2 (C-2''), 125.4 (C-3''), 115.9 (C-4''),
28.4 (Me2), 55.7 (MeO-6'), 200.7 (C=O), 21.2 (OCOCH3), 170.0 (OCOCH3). OCOCH3,
(Appendix B).
3.5.3 Compound 3
Yellowish oily substance. Rf = 0.4 (CH2Cl2/hexane, 2:3). 1H NMR (CDCl3, 200 MHz):
- (m, H-2, -6); m, H-3, -4, -5); s, H-5'), 8.02 (d, J =
15.6 Hz, H- (d, J = 15.6 Hz, H-), 5.59 (d, J = 10 Hz, H-3''), 6.63 (d, J = 10 Hz,
H-4''), 1.46 (s, (Me2-2''), 1.39 (s, (Me2-2''), 3.86 (s, OCH3-6'), 14.45 (s, OH-2'). 13C NMR
(CDCl3, 50 MHz): C 135.7 (C-1), 128.7 (C-2/6), 129.3 (C-3/5), 129.0 (C-4), 105.9 (C67
1'), 160.9 (C-2'), 102.7 (C-3'), 162.6 (C-4'), 91.9 (C-5'), 163.3 (C-6'), 127.5 (C-), 142.5
(C-), 78.4 (C-2''), 125.9 (C-3''), 115.7 (C-4''), 29.2 (Me2), 56.0 (MeO-6'), 192.9 (C=O),
(Appendix C).
3.5.4 Compound 4
Whitish solid. Rf = 0.3 (CH2Cl2/Hexane, 2:3), UV max (MeOH, Log ) nm: 271.5 (0.9),
476.0 (0.003). 1H NMR (CDCl3, 300 MHz): H 5.44 (dd, J = 12.6, 3.3 Hz, H-2), 2.83
(dd, J = 3.3, -17.1 Hz, H-2eq), 3.06 (dd, J = 12.6, -17.1 Hz, H-2ax), 6.00 (s, H-6), 7.40 –
7.54 (m, H-2' ,-3', -4', -5', -6'), 5.44 (d, J = 10.8 Hz, H-3''), 6.55 (d, J = 10.8 Hz, H-4''),
1.40 (s, Me2-2''), 1.5 (s, Me2-2''), 12.09 (s, 5-OH). 13C NMR (CDCl3, 75 MHz): C 79.1
(C-2), 43.3 (C-3), 195.6 (C=O), 156.8 (C-5), 97.7 (C-6), 162.4 (C-7), 102.0 (C-8), 163.8
(C-9), 103.0 (C-10), 138.5 (C-1'), 126.0 (C-2'/6'), 128.8 (C-3'/5'), 128.8 (C-4'), 78.2 (C2''), 126.5 (C-3''), 115.6 (C-4''), 28.2 (Me2), 28.5 (Me2), (Appendix D).
3.5.5 Compound 5
Needle-like white crystals. Rf = 0.54 (Hexane/CH2Cl2/EtOAc, 5:9:1). Melting point =
134.90C. UV max (MeOH, Log ) nm: 271.5 (0.66). 1H NMR (CDCl3, 300 MHz): H
5.42 (dd, J = 12.9 Hz, H-2), 2.82 (dd, J = -16.5, 3.3 Hz, H-3eq), 3.0 (dd, J = -16.5, 12.9
Hz, H-3ax), 6.06 (s, H-6), 7.34 – 7.44 (m, H-2', -3', -4', -5', -6'), 5.47 (d, J = 9.9 Hz, H3''), 6.60 (d, J = 9.9 Hz, H-4''), 1.45 (s, Me2-2''), 1.46 (s, Me2-2''), 3.87 (s, MeO-5). 13C
NMR (CDCl3, 75 MHz): C 78.9 (C-2), 45.6 (C-3), 189.2 (C=O), 162.1 (C-5), 93.9 (C6), 159.9 (C-7), 102.9 (C-8), 158.7 (C-9), 105.7 (C-10), 139.0 (C-1'), 125.9 (C-2'/6'),
68
128.7 (C-3'/5'), 128.5 (C-4'), 78.0 (C-2''), 126.3 (C-3''), 116.0 (C-4''), 28.2 (Me2), 28.5
(Me2), 55.6 (MeO-5), (Appendix E).
3.5.6 Compound 6
Yellowish oil. Rf = 0.3 (Hex/CH2Cl2/EtOAc, 5:9:1). UV max (MeOH, Log ) nm: 271.5
(0.48), 360.5 (0.04). 1H NMR (CDCl3, 300 MHz): H 6.79 (s, H-1), 6.45 (s, H-4), 4.46
(dd, J = 12.0, 3.0 Hz, H-6ax), 4.19 (d, J = 12.0 Hz, H-6eq), 4.92 (m, H-6a), 6.48 (d, J =
8.7 Hz, H-10), 7.75 (d, J = 8.7 Hz, H-11), 3.84 (d, J = 4.2 Hz, H- 12a), 6.65 (d, J = 10.2
Hz, H-4'), 5.56 (d, J = 10.2 Hz, H-5'), 1.39 (s, Me2-2'), 1.45 (s, Me2-2'), 3.77 (s, MeO-2),
3.81 (s, MeO-3). 13C NMR (CDCl3, 75 MHz): C 110.5 (C-1), 104.8 (C-1a), 143.9 (C-2),
149.5 (C-3), 100.9 (C-4), 147.4 (C-4a), 66.3 (C-6), 72.4 (C-6a), 156.9 (C-7a), 109.1 (C8), 160.9 (C-9), 111.4 (C- 10), 128.5 (C-11), 112.7 (11a), 189.2 (C=O), 44.4 (C-12a),
115.7 (C-4'), 128.6 (C-5'), 28.1 (Me2 - 6'), 28.5 (Me2 - 6'), 56.3 (MeO-2), 55.8 (MeO-3),
(Appendix F).
3.5.7 Compound 7
Yellowish oil. Rf = 0.3 (Hex/CH2Cl2/EtOAc, 5:9:1). UV max (MeOH, Log ) nm: 271.5
(0.48), 360.5 (0.04). 1H NMR (CDCl3, 300 MHz): H 6.79 (s, H-1), 6.45 (s, H-4), 4.46
(dd, J = 12.0, 3.0 Hz, H-6ax), 4.19 (dd, J = 0.8, 3.0 Hz, H-6eq), 4.59 (dd, J = 0.8, 3.0 Hz,
H-6a), 6.48 (d, J = 8.7 Hz, H-10), 7.75 (d, J = 8.7 Hz, H-11), 5.35 (dd, J = 7.6, 9.5 Hz,
H-2'), 3.06 (dd, J = 9.5, 15.1 Hz, H-3'), 3.42 (dd, J = 9.5, 15.1 Hz, H-3'), 4.96 (brs, H-5'),
5.11 (brs, H-5'), 1.78 (s, Me-4'), 3.77 (s, MeO-2), 3.81 (s, MeO-3). 13C NMR (CDCl3, 75
MHz): C 110.5 (C-1), 104.8 (C-1a), 143.9 (C-2), 149.5 (C-3), 100.9 (C-4), 147.4 (C69
4a), 66.3 (C-6), 72.4 (C-6a), 156.9 (C-7a), 109.1 (C-8), 160.1 (C-9), 111.4 (C-10), 128.5
(C-11), 112.7 (C-11a), 189.2 (C=O), 44.4 (C-12a), 87.9 (C-2'), 30.8 (C-3'), 143.0 (C-4'),
112.9 (C-5'), 16.9 (C-6'), 16.9 (Me - 4'), 56.3 (MeO-2), 55.8 (MeO-3), (Appendix F).
3.5.8 Compound 8
Yellowish oil. 1H NMR (CDCl3, 200 MHz): H 7.45 - 7.89 (m, H-2, -3, -4, -5, -6), 6.03
(s, H-), 6.51 (s, H-5'), 5.56 (d, J = 10.4 Hz, H-3''), 6.49 (d, J = 10.4 Hz, H-4''), 1.42 (s,
Me2-2''), 1.40 (s, Me2-2''), 3.89 (s, MeO-6'), 3.69 (s, MeO-), 3.65 (MeO-2'). 13C NMR
(CDCl3, 50 MHz): C 140.4 (C-1), 128.4 (C-2/6), 127.9 (C-3/5), 127.3 (C-4), 188.7
(C=O), 96.6 (C-), 166.1 (C-), 107.7 (C-1'), 155.1 (C-2'), 11.6 (C-3'), 158.5 (C-4'),
100.9 (C-5'), 155.7 (C-6'), 76.4 (C-2''), 131.7 (C-3''), 117.0 (C-4''), 27.5 (Me2), 55.6
(MeO-6'), 61.7 (MeO-), 55.9 (MeO-2'), (Appendix G).
3.5.9 Compound 9
Yellowish needle-like crystals were obtained from n-hexane/EtOAc (9:1), melting point
= 126 - 129 oC. 1H NMR spectral data (acetone-d6, 200 MHz): H 7.86 - 7.91 (2H, m, H-2,
H-6), 7.41 – 7.50 (3H, m, H-3,-4, -5), 6.18 (1H, s, H-), 6.48 (1H, d, J = 10.0 Hz, H-4''),
5.57 (1H, d, J = 10 Hz, H-3''), 6.55 (1H, s, H-5'), 3.89 (3H, s, 2'-OMe), 1.41 (3H, s, Me22''), 1.40 (3H, s, Me2-2''). 13C NMR spectral data (acetone-d6, 50 MHz): C 188.7 (C=O),
166.1 (C-7), 158.5 (C-4'), 155.7 (C-2'), 155.1 (C-6'), 140.4 (C-1), 131.7 (C-4), 128.4 (C2, C-6), 127.9 (C-3, C-5), 127.2 (C-4''),117.0 (C-3''), 112.2 (C-3'), 107.7 (C-1'), 100.9
70
(C-8), 96.0 (C-5'), 76.4 (C-2''), 55.9 (2'-OMe), 28.8 (2''-Me2), 28.4 (2''-Me2), (Appendix
H).
3.6 Biological Activity Assays
3.6.1 In-vitro antiplasmodial activity assay
The crude extract and pure compounds were assayed using a non radioactive assay
technique [Smilkstein et al., 2004] with modifications to determine 50% growth
inhibition of cultured parasites. This is an accepted method for assaying in vitro drug
susceptibility using the fluorochrome called “SYBR Green I”, a non-radioactive
intercalating DNA marker that accurately depicts in vitro parasite replication. This test
replaces the older, 3H-hypoxanthine uptake assay, is fully endorsed by the WHO.
Briefly, two different strains, chloroquine-sensitive Sierra Leone I (D6) and
chloroquine-resistant Indochina I (W2), of Plasmodium falciparum were grown as
described in the literature [Johnson et al., 2007]. Concurrently, twofold serial dilutions
of the drugs chloroquine (1.953 to 1,000 ng/ml), mefloquine (0.488 to 250 ng/ml) and
test sample (97.7 – 50,000 ngml-1) were prepared on a 96 well plate. The culture-adapted
P. falciparum were added on to the plate containing dose range of drugs and incubated
in gas mixture (5% CO2, 5% O2, and 90% N2) at 37°C. The assay was terminated 72 hrs
later by freezing at -80°C.
After thawing, lysis buffer containing SYBR Green I (1x final concentration) were
added directly to the plates and gently mixed by using the Beckman Coulter Biomek
71
2000 automated laboratory workstation (Beckman Coulter, Inc., Fullerton, CA). The
plates were incubated for 5 - 15 minutes at room temperature in the dark. Parasite
growth inhibition was quantified by measuring the per-well relative fluorescence units
(RFU) of SYBR green 1 dye using the Tecan Genios Plus (Tecan US, Inc., Durham,
NC) with excitation and emission wavelengths of 485 nm and 535 nm, respectively, and
with the gain set at 60. Differential counts of relative fluorescence units (RFUs) were
used in calculating IC50’s for each drug using Prism 4.0 software for Windows
(Graphpad Software, San Diego, CA). A minimum of three separate determinations was
carried out for each sample. Replicates had narrow data ranges hence presented as mean
+ SD. The antiplasmodial tests were done in collaboration with Mr. Akala, H., Dr.
Waters, N and Ms. Layala, P of Kenya Medical Research Institute and United States
Medical Research Unit - Kenya.
3.6.2 Larvicidal activity assay
The eggs of Aedes aegypti L. (Diptera: Culicidae) were obtained from the Department of
Zoology, University of Nairobi. The eggs were flooded with 0.08% NaCl solution and
left to hatch at 28 0C. Twenty third instar larvae were transferred into a Petri-dish
containing 500 ml of 0.08% NaCl solution. The larvae were treated with the test extracts
and pure compounds according to Mwangi and Rembold [1998]. Twenty milligrams of
test samples were dissolved in 2 ml of DMSO. From the stock solution different
concentrations were prepared by serial dilution and the larvae were tested for mortality
at 20, 10, 5, 2.5, 1.25 and 0.65 gml-1 of sample solutions. Control larvae in all cases
72
received 50 l of DMSO as in test larvae. Mortality was checked after 24 hours. LC50
values were calculated from the average of three observations for each concentration
using Finney’s probit analysis for quantal data [McLaughlin et al., 1991; Finney, 1971].
73
CHAPTER FOUR
4.0 RESULTS AND DISCUSSION
4.1 Preliminary Test Results
4.1.1 Phytochemical profile evaluation results
The dried and ground seedpods and stem of T. elata and T. aequilata were extracted
separately with CH2Cl2/MeOH (1:1) by cold percolation. The crude extracts were then
subjected to thin layer chromatography (TLC) to establish their phytochemical profile.
The presence of several UV-active spots on TLC of the seedpod extracts of both plants
were detected under UV light (254 nm).
4.1.2 In-vitro antiplasmodial activity evaluation results
The crude extracts (CH2Cl2/MeOH, 1:1) of the seedpods of T. elata and T. aequilata
were screened for antiplasmodial activities against two different strains of the malaria
parasite. The results obtained indicated moderate antiplasmodial activities against both
D6 and W2 strains of P. falciparum. The crude extract of the seedpods of T. elata
showed an average activity against both strains of P. falciparum whereas that of T.
aequilata was more active against the sensitive strain D6 than the resistant strain W2.
Table 4.1 below summarizes the in vitro antiplasmodial activity tests for the crude
extracts.
74
Table 4.1: In vitro IC50 values of the crude seedpods extracts from T. elata and T.
aequilata against D6 and W2 strains of P. falciparum
Plant (plant part)
T. elata (seedpods)
T. aequilata (seedpods)
Chloroquine
Mefloquine
IC50 (g/ml+ SD)
D6
W2
8.4 + 0.3
8.6 + 1.0
1.45 + 0.21
22.4 + 5.2
0.008 + 0.004
0.051 + 0.010
0.042 + 0.008
0.015 + 0.002
4.2 Characterization of Isolated Compounds
4.2.1 Compounds from Tephrosia elata
The crude extract from the seedpods of T. elata afforded seven compounds. The
characterization of these compounds is discussed below.
4.2.1.1 Chalcones
4.2.1.1.1 Elatadihydrochalcone (1) and -acetoxyelatadihydrochalcone
(2)
HRMS analysis of compound 1 showed a [M+1]+ peak at m/z 355.1535 corresponding to
the molecular formula of C21H23O5 (Appendix A). The UV (max = 275, 296 and 308
nm), the 1H NMR ( 3.45, dd, J = 3.0, 18.0 Hz and 3.34, dd, J = 9.0, 18.0 Hz for CH2; 5.28 dd, J = 3.0, 9.0 Hz for H-) and 13C NMR (C 204.2 for C=O; 52.7 for C-,
70.2 for C-) spectra (Table 4.2) showed that this compound is a hydroxydihydrochalcone derivative [Nel et al., 1999; Chen et al., 2005]. The presence of
hydroxyl group at the -carbon was confirmed from 1H NMR spectrum of the mono
acetate (2) which showed down-field shift for H- (Table 4.2). In agreement with this,
75
the HMBC spectrum of 1 showed correlations between H- and C-2/6, H-2/6 and C-,
CH2- and C=O, CH2-and C-1 (Table 4.2). Furthermore the presence of a chelated
hydroxyl ( 13.98), a methoxyl (H = 3.78, C = 55.7) and a 2,2-dimethylpyran
substituent were established from NMR (Table 4.2) and MS fragmentation (Fig 4.1),
(Appendix A).
The 1H NMR and 13C NMR spectra (H 7.26 - 7.44, 5H for H-2, H-3, H-4, H-5, H-6; C
143.4 for C-1; 125.9 for C-2/6, 128.4 for C-3/5) showed that ring-A in compound 1 is
not substituted. All the substituents are then located in ring-B, with the chelated
hydroxyl and the methoxyl at C-2' and C-6'. The 2,2-dimethylpyran group could either
be adjacent to the hydroxyl group (1) or adjacent to the methoxy group (1a). The
13
C
NMR chemical shift value of the methoxy group (C 55.7) was found to be within the
normal range [Yenesew et al., 1998a] and is consistent with structure 1 rather than 1a
where the methoxy group being di-ortho-substituted resonates above 59 ppm [Yenesew
et al., 1998a]. In agreement with this, irradiation of the methoxy protons resulted in a
nOe enhancement of H-5'. Hence this compound 1 was characterized as 3',4'-(2'',2''dimethylpyrano)-2',β-dihydroxy-6'-methoxydihydrochalcone, for which the trivial name
elatadihydrochalcone was suggested. The CD spectrum showed a positive Cotton effect
at 350 nm and a negative one at 290 nm which suggested S-configuration at the -carbon
[Nel et al., 1999], (Appendix A).
76
This is the first report on the occurrence of a -hydroxydihydrochalcone in the genus
Tephrosia. -hydroxydihydrochalcones constitute a small subclass of flavonoids with
only few reported in nature [Dictionary of Organic Compounds, 2008].
The literature data on the assignments of the 1H NMR and 13C NMR data (Table 4.3) for
the characteristic -hydroxydihydrochalcone atoms were found to be inconsistent. This
prompted a comprehensive NMR analysis (Table 4.2) of elatadihydrochalcone (1) and
its acetate derivative (2). The 1H NMR and
13
C NMR data of elatadihydrochalcone (1)
are in close agreement for what have been reported for the -hydroxydihydrochalcones
(152) [Nel et al., 1999] and (153) [Chen et al., 2005], and for the methoxydihydrochalcones (like 154) [Tanaka et al., 1992] (Table 4.3). In contrast, the
data reported for 155 [Thuy et al., 1998], 156 [Rafi et al., 2002], 157 [Adinarayana et
al., 1982] and 158 [Manners and Jurd, 1979] are significantly different (Table 4.3),
(Appendix B).
Such difference could suggest different skeletal structures for the two sets of
compounds, compounds 1, 2, 152-4 as one set and compounds 155-158 as a second set.
Interestingly the NMR data for and atoms as reported for compounds 155-158 are
similar to ring-C atoms (CH2-3 and CH-2 groups) of the flavanones obovatin (4) and
obovatin methyl ether (5) [Andrei et al., 2000], and other flavanones in literature
[Tanaka et al., 1992; Andrei et al., 2000; Yenesew et al., 1998a] (Table 4.3). In fact the
similarity of NMR data of compounds 157 [Adinarayana et al., 1982] and 158 [Manners
77
and Jurd, 1979] with flavanones have been used as supporting evidence in assigning hydroxydihydrochalcone skeleton for these compounds (Appendix A).
However, the NMR data for compounds 1, 2, 152-4 is distinct from those of the
flavanones 4 and 5 (Table 4.3). Such difference is expected considering that hydroxydihydrochalcones have an open chain for and C=O atoms, while flavanones
have cyclic system (ring C). It follows then that compounds 155-158 (and other related
compounds as suggested by the authors, (Table 4.3) could be flavanones rather than hydroxydihydrochalcone derivatives. Therefore, the structure of these compounds be reexamined of these compounds by a combination of modern spectroscopic techniques to
resolve this issue (Appendix A and B).
78
Table 4.2: 1H NMR (300 MHz) and
Correlations
for
13C
NMR (75 MHz) along with HMBC
elatadihydrochalcone
(1)
and
-
acetoxyelatadihydrochalcone (2)
Position
C
1
2/6
143.4
125.9
3/5
128.4
4
127.4
1'
2'
3'
4'
5'
105.6
161.9
102.9
160.7
91.4
6'
163.0
52.7
70.2
2''
3''
78.3
125.5
4''
115.8
2''(CH3)2
6'-OCH3
2'-OH
28.4
55.7
C=O
OCOCH3
OCOCH3
204.2
CDCl3)
m
(J in Hz)
HMBC
7.26-7.44 m C-1, ,
3/5, 4
7.26-7.44 m C-1,
2/6, 4
7.26-7.44 m C-2/6,
3/5
5.87 s
3.45 dd
(3.0,18.0)
3.34 dd
(9.0,18.0)
5.28 dd
(3.0, 9.0)
5.46 d
(10.1
6.66 d
(10.1)
1.44 s
3.78 s
13.98 s
C-1', 3',
4', 6'
acetone-d6)
CDCl3)
C
m
C
m
(J in Hz)
(J in Hz)
145.6
140.4
126.1
7.23-7.48 m 126.7
7.27-7.41 m
128.3
7.23-7.48 m 128.5
7.27-7.41 m
127.2
7.23-7.48 m 128.0
7.27-7.41 m
105.7
161.9
102.6
160.6
91.7
105.5
161.9
102.9
160.3
91.2
163.0
C=O, 54.0
-1
C-2/6
70.0
C-3'
78.2
125.9
C-2'', 4'
115.7
C-2'', 3''
C-6'
C-1', 2',
3'
27.9
55.8
203.9
79
6.00 s
3.44 dd
(4.6,16.2)
3.37 dd
(7.8,16.2)
5.29 dd
(4.6,7.8)
5.56 d
(10.2)
6.66 d
(10.2)
1.43 s
3.91 s
14.21 s
162.6
50.3
71.9
78.2
125.4
115.9
28.4
55.7
200.7
21.2
170.0
5.88 s
3.44 dd
(4.5,17.1)
3.62 dd
(8.7,17.1)
6.38 dd
(4.5,8.7)
5.45 d
(10.2)
6.64 d
(10.2)
1.44 s
3.83 s
13.99 s
2.03 s
Table 4.3a: Comparison of the 1H NMR (a) and 13C NMR (b) data of the and atoms of elatadihydrochalcone (1)
with literature for -hydroxydihydrochalcone derivatives (152-8) and flavanones (4 and 5).
H
1
(CDCl3)
3.45 dd
(2.9, 18.3)
3.34 dd
(9.0, 18.3)
5.28 dd
(3.0, 9.0)
1
(acetoned6)
3.44 dd
(4.6, 16.2)
3.37 dd
(7.8, 16.2)
5.29 dd
(4.6, 7.8)
152
(CDCl3)
153
(CDCl3)
154
(CDCl3)
3.40 dd
(3.3, 18.1)
3.30 dd
(9.1, 18.1)
5.21 m
(3.6, 8.7)
3.37 dd
(8.8, 17.4)
3.29 dd
(3.2, 17.4)
5.34 dd
(3.2, 8.8)
3.55 dd
(9, 17)
3.15 dd
(5, 17)
4.74 dd
(5, 9)
155
(pyridined5)
2.93 dd
(2.9, 16.3)
3.27 dd
(12.8,16.3)
5.52 dd
(2.9, 12.8)
156
(CDCl3)
157
(acetone
-d6)
2.69 dd
2.77
(3.1, 16.3) (8, 15)
3.06 dd
3.01
13.0, 16.3) (5, 15)
5.38 dd
5.21 m
(3.0, 13.0)
158
(DMSO
-d6)
2.76 dd
(8, 15)
3.00 dd
(5, 15)
5.07 m
4*
(CDCl3)
5*
(CDCl3)
2.81 dd
(3.3, 16.7)
3.10 dd
(12.5, 16.7)
5.45 dd
(3.3, 12.5)
2.75 dd
(3.4, 16.7)
2.95 dd
(12.5, 16.5)
5.39 dd
(3.4, 12.6)
Table 4.3b: 13C NMR data
C
1
1
152
155
156
158
4*
5*
(CDCl3) (acetone-d6) (CDCl3) (pyridine-d5) (CDCl3) (DMSO-d6) (CDCl3) (CDCl3)
52.7
54.0
52.45
46.1
45.24
40.1
43.19
45.52
70.2
70.0
70.41
79.5
81.33
73.3
78.97
78.84
*For flavanones 4 and 5, = C-3 and = C-2
152 = -Hydroxy-4,4'dimethoxy-2'-O-methoxymethyldihydrochalcone [Nel et al., 1999].
153 = 3'-Methoxy-2',4',-trihydroxydihydrochalcone [Chen et al., 2005].
154 = Ponganone VIII (2',5', -Trimethoxy-3,4-methylenedioxy-6'',6''-dimethylpyrano[2'',3'':4',3']dihydrochalcone [Tanaka et
al., 1992].
155 = 4,2',4',-Tetrahydroxy-6'-methoxy-,-dihydrochalcone [Thuy et al., 1998].
156 = 2',4,4',-Tetrahydroxydihydrochalcone [Rafi et al., 2002].
157 = Pterosupin (3'--D-glucopyranosyl-2',4,4',-tetrahydroxydihydrochalcone [Adinarayana et al., 1982].
158 = Gliricidol (4-metoxy-,2',3,4',5-pentahydroxydihydrochalcone [Manners and Jurd, 1979].
80
81
The fig 4.1 below shows the fragmentation pattern inferred from the EIMS spectrum
peaks for compound 1.
Figure 4.1: EIMS fragmentation in elatadihydrochalcone (1) (Appendix A).
82
4.2.1.1.2 Obovatachalcone (3)
Compound 3 was isolated as a yellow oily substance. On TLC plate the yellow spot
turned brown upon exposure to iodine vapour. Evidence that this compound is a
chalcone was available from the 1H-NMR spectrum which shows signals for H-H
8.02, d, J = 15.6 Hz) and H-H 8.01, d, J = 15.6 Hz). The corresponding
13
C NMR
signals for C-and C-wereatCandrespectively, while the carbonyl
group resonated at 192.9 ppm [Andrei et al., 2000]. The NMR (Table 4.4) further
showed the presence of a chelated hydroxyl group (H 14.60, s), methoxyl group (C
56.03, H 4.02 s) and a 2,2-dimethylchromene at H 5.59 (d, J = 10 Hz) for H-3''; 6.63 (d,
J = 10 Hz) for H-4'' and 1.46 (s), 1.3 (s) for 2''-(CH3)2 groups.
The 1H and 13C NMR spectra (H 7.73 - 7.82, m, 2H for H-2/H-6; H 7.44 – 7.48, m, 3H
for H-3/H-4/H-5; C 135.7 for C-1; 128.8 for C-2/6, 129.3 for C-3/5 and 129.0 for C-4)
further showed that A ring in compound 3 is unsubstituted. All the substituents are
therefore located in ring-B, with the chelated hydroxyl and the methoxyl at C-2' and C6', respectively. The 2,2-dimethylpyrano group could either be adjacent to the hydroxyl
group 3 or adjacent to the methoxy group as in 3a. The 13C NMR chemical shift value of
the methoxyl (C = 56.0) is within the normal range and is consistent with structure 3
rather than 3a where the methoxyl group being di-ortho-substituted is resonates above
59 ppm (Yenesew et al., 1998a). In agreement with this, irradiation of the methoxy
protons resulted in a nOe enhancement of H-5'. Hence this compound was characterized
as
3',4'-(2'',2''-dimethlylpyrano)-2'-hydroxy-6'-methoxychalcone
83
(trivial
name
obovatachalcone) [Andrei et al., 2000]. This is the first report on the occurence of
obovatachalcone in T. elata. Obovatachalcone (3) has previous been isolated from
several members of this genus such as the roots of T. tunicata [Andrei et al., 2000] and
T. obovata [Garcez et al., 1988], (Appendix C).
Table 4.4: 1H (200 MHz) and 13C NMR (50 MHz) data for obovatachalcone (3)
3 (acetone-d6)
Position
C
(ppm)
3 (acetone-d6)
Position
(ppm) m,J in Hz)
C
(ppm)
(ppm) m,J in Hz)
127.5
8.02 d, (15.6)
8.01 d, (15.6)
1
135.7
2/6
128.7
7.73 – 7.82 m
142.5
3/5
129.3
7.44 – 7.48 m
''
78.4
4
129.0
7.44 – 7.48 m
''
125.9
5.59 d, (10)
1'
105.9
''
115.7
6.63 d (10)
2'
160.9
2''(CH3)2
29.2
1.46 s
3'
102.7
4'
162.6
5'
91.9
6'
163.3
1.39 s
'-OCH3
56.0
'-OH
6.06 s
C=O
84
3.86 s
14.45 s
192.9
4.2.1.2 Flavanones
4.2.1.2.1 Obovatin (4)
Compound 4 was isolated as an amorphous solid. The 1H NMR ( 5.44, dd, J = 12.6, 3.3
Hz for H-2; 2.84, dd, J = 17.1, 3.3 Hz for H-3eq; 3.06, dd, J = 17.1, 12.6 Hz for H-3ax)
and
13
C (C 79.1 for C-2; 43.3 for C-3 and 195.6 for C=O) NMR spectra (Table 4.7)
were consistent with a flavanone skeleton. The 1H NMR indicated the presence of a
chelated hydroxyl at H 12.9 (s) and a 2,2-dimethylchromene at H 5.44 (d, J = 10.8 Hz)
for H-3''; 6.55 (d, J = 10.8 Hz) for H-4'' and 1.50 (s), 1.40, (s) for 2''-(CH3)2 groups.
The 1H and 13C NMR spectra (H = 7.40 - 7.45, m, 5H for H-2', H-3', H-4', H-5', H-6'; C
= 138.5 for C-1', 126.0 for C-2'/6', 128.8 for C-3'/5' and 128.8 for C-4') showed that ringB in compound 4 is unsubstituted. All the substituents are therefore located in ring-A,
with the chelated hydroxyl (H 12.09, s, for OH-5) group at C-5 and the 2,2dimethylchromene attached at either C-7/8 (4) or C-6/7 (4a). HMBC correlation
between OH-5 and C-6 (97.7) allowed the placement of the 2,2-dimethylchromene
group at C-7/8 (Table 4.5). Hence this compound was characterized as 7,8-(2'',2''dimethylchromene)-5-hydroxyflavanone (trivial name as obovatin). This is the first
report of the isolation of obovatin (4) from T. elata. It has, however, been previously
isolated from T. emoroides [Machocho et al., 1995], T. obovata [Lwande, 1985] and T.
tunicata (Andrei et al., 2000], (Appendix D).
85
4.2.1.2.2 Obovatin methyl ether (5)
Compound 5 was isolated as an amorphous solid. The 1H NMR (H 5.42, dd, J = 12.9,
3.3 Hz for H-2; 2.82, dd, J = -16.5, 3.3 Hz for H-3eq; 3.0, dd, J = -16.5, 12.9 Hz for H3ax) and 13C (C 78.9 for C-2; 45.6 for C-3 and 189.2 for C=O) NMR spectra (Table 4.5)
were consistent with a flavanone skeleton. The 1H and
13
C NMR spectrum further
indicated the presence of a methoxyl group (H 3.87, C 56.5) and a 2,2dimethylchromene ring (Table 4.5). The 1H NMR further showed a multiplet between
(H 7.34 and 7.44 (5H) assigned to an unsubstituted ring-B. In ring-A, a singlet aromatic
proton at 6.06 (1H, s) was assigned to H-6 with a methoxy being at C-5 and 2,2dimethylpyrano group at C-7/8. The nOe interactions between H- ( 6.06) and the
methoxyl ( 3.87), confirms the placement of the aromatic proton at C-6 and the 2,2dimethylchromene group at C-7/8. Therefore, compound 5 was characterized as 7,8(2'',2''-dimethylchromene)-5-methoxyflavanone, trivial name obovatin methyl ether.
This is the first report of obovatin methyl ether (5) from the seedpods of T. elata.
However, it has previously been isolated from the roots of this plant [Lwande, 1985], T.
86
emoroides [Machocho et al., 1995], T. obovata [Lwande, 1985], T. aequilata, [Tarus et
al., 2002] and T. tunicata [Andrei et al., 2000], (Appendix E).
Table 4.5: 1H (300 MHz) and 13C NMR (75 MHz) data along with HMBC
Correlations for obovatin (4) and obovatin methyl ether (5) in CDCl3.
Position
2
4
C (ppm) (ppm), (m, J in
Hz)
79.1
5.44 (dd, 12.6,
3.3)
43.3
2.83 (dd, 17.1,
3.3, Heq)
3.06 (dd, 17.1,
12.6, Hax)
HMBC
C-2'/6', 9,
C=O
C-2, C=O
C-2, C=O
C=O
5
6
7
195.6
156.8
97.7
162.4
8
9
10
1'
2'/6'
102.0
163.8
103.0
138.5
126.0
3'/5'
4'
2''
3''
128.8
128.8
78.2
126.5
7.40 – 7.45 (m)
7.40 – 7.45 (m)
4''
2''-Me2
115.6
28.2
28.5
6.55 (d, 10.8)
1.4 (s)
1.5 (s)
C-8, 5'',
6''
C-2'', 7, 9
C-2'', 3''
C-2'', 3''
12.09 (s)
C-6
5-OMe
5-OH
6.00 (s)
7.40 – 7.45 (m)
5.44 ( d, 10.8)
5
C (ppm) (ppm), (m, J in
Hz)
78.9
5.42 (dd, 12.9,
3.3)
45.6
2.82 (dd, 16.5,
3.3, Heq)
C-8, 10
C-1', 3'/5',
C-4'
C-1', 4'
2'/6'
87
189.2
162.1
93.9
159.9
102.9
158.7
105.7
139.0
125.9
HMBC
C-2'/6',
9, C=O
C-1', 2,
C=O,
3.0 (dd, 16.5,
12.9, Hax)
C-1', 2,
C=O,
6.06 (s)
C-8, 10
7.34 – 7.44 (m)
128.7
128.5
78.0
126.3
7.34 – 7.44 (m)
7.34 – 7.44 (m)
C-2, 1',
3'/5', 4'
C-1', 4'
C-2'/6'
5.47 (d, 9.9)
C-8
116.0
28.2
28.5
55.6
6.60 (d, 9.9)
1.45 (s),
1.46 (s)
3.87 (s)
C-2'', 7
C-2'', 3''
C-2'', 3''
C-5
Figure 4.2: nOe interactions observed for obovatin methyl ether (5)
4.2.1.3 Rotenoids
4.2.1.3.1 Deguelin (6)
The 1H NMR and 13C NMR spectra showed compound 6 to be a rotenoid derivative with
a 2,2-dimethylpyran and two methoxyl substituents (Table 4.6). The presence of two
para-oriented aromatic protons at 6.79 (s) for H-1 and 6.45 (s) for H-4 in ring-A
places the methoxyl groups at C-2 and C-3. Furthermore, the appearance of an AX spin
system of aromatic protons ( 6.48 (d, J = 8.7 Hz) for H-10 and 7.75 (d, J = 8.7 Hz)
for H-11 with C 111.4forC-10 and C-128.5 for C-11, respectivelyin ring-D would
place the 2,2-dimethylchromene substituent at C-8/C-9 (Table 4.6). Thus, this compound
was identified as deguelin (6). It was isolated as a major component in a mixture of two
rotenoids. This compound has earlier been isolated from several plants of this family
including T. candida [Andrei et al., 1997] and M. Dura [Yenesew, 1997], (Appendix F).
88
4.2.1.3.2 Rotenone (7)
The 1H NMR and 13C NMR spectra showed compound 7 to be a rotenoid derivative with
a prenylated furano and two methoxyl substituents (Table 4.6). The presence of two
para-oriented aromatic protons in ring-A ( 6.79 (s) for H-1, 6.45 (s) for H-4 and C
110.5 for C-1, 100.9 for C-4, respectively) places the methoxyl groups at position C2/C-3. Furthermore, the appearance of an AX spin system of aromatic protons ( 6.48
(d, J = 8.7 Hz) for H-10 and 7.75 (d, J = 8.7 Hz) for H-11 with C 111.4forC-10 and
C-128.5 for C-11, respectivelyin ring-D would place the prenylated furano substituent
at C-8/C-9 (Table 4.6). Hence, this compound was identified as rotenone. It was
obtained as a minor component in the sample from which deguelin (6) was identified
(section4.2.1.3.1). Rotenone (7) has previously been isolated from several plants of this
family including T. candida [Kole et al., 1992], T. vogelii [Hagemann et al., 1972] and
Derris trifoliata [Kiplagat, 2007], (Appendix F).
89
Table 4.6: 1H NMR (300 MHz) and 13C NMR (75 MHz) data along with HMBC
Correlations for deguelin (6) and rotenone (7) in CDCl3.
6
Position
7
C (ppm)
110.5
104.8
143.9
149.5
100.9
147.4
66.3
66.3
(ppm), m,J in Hz)
6.79 s
6a
7a
8
9
10
11
11a
C=O
12a
2'
3'
72.4
156.9
109.1
160.1
111.4
128.5
112.7
189.2
44.4
4.92 m
4'
5'
115.7
128.6
6.65 d (10.2)
5.56 d (10.2)
6'
6'-Me2
77.7
28.1
28.5
1.39 s
1.45 s
1
1a
2
3
4
4a
6 ax
6 eq
4'-Me
2-OMe
3-OMe
56.3
55.8
6.45 s
4.64 dd (12.0, 3.0)
4.19 d (12.0)
6.48 d (8.7)
7.75 d (8.7)
3.84 d (4.2)
C (ppm)
110.5
104.8
143.9
149.5
100.9
147.4
66.3
66.3
(ppm), m,J in Hz)
6.79 s
72.4
156.9
109.1
160.1
111.4
128.5
112.7
189.2
44.4
87.9
30.8
4.59 dd (0.8, 3.0)
143.0
112.9
16.9
56.3
55.8
3.77 s
3.81 s
90
6.45 s
4.46 dd (12.0, 3.0)
4.19 dd (0.8, 3.0)
6.48 d (8.7)
7.75 d (8.7)
3.84 d (4.2)
5.35 dd (7.6, 9.5)
3.06 dd (9.5,15.1)
3.42 dd (9.5, 15.1)
4.96 (br s)
5.11 (br s)
1.78 s
3.77 s
3.81 s
4.2.2 Compound Isolated from Tephrosia aequilata
4.2.2.1 Chalcones
4.2.2.1.1 Praecansone A (8)
Compound 8 was isolated as a yellow oily substance. The 1H NMR (6.40, s, for H)
and
C (C 101.4 for C; C 165.7 for C; C 189.9 for C=O) NMR spectra suggested
13
that this compound is a retro-chalcone (Table 4.7) [Tarus et al., 2002, Dagne et al.,
1990]. The 1H and
13
C NMR indicated the presence of three methoxyl and a 2,2-
dimethylpyrano groups (Table 4.7). The 1H NMR further displayed a singlet at 6.19
for H-5' and a set of mutually coupled five aromatic protons at 7.45 – 7.5 (m, 3H, for
H-3/H-4/H-5) and 7.89 – 7.92 (m, 2H for H-2/H-6 belong to a monosubstituted ringA. In ring-B, a singlet aromatic proton ( could be assigned to H-2' or H-5'. The
nOe interactions between this singlet and the methoxyl at 6'-OMe (showed this
singlet is for H-5' (Fig 4.3).
The geometry across the and -carbons was established to be (E) configured due to
nOe interactions between H ( 6.56, s) and the methoxyl at C- ( 3.88). Based on
these observations and comparison with literature [Dagne et al, 1990; Tarus et al., 2002]
compound
8
was
characterized
as
(E)-3',4'-(2'',2''-dimethylpyrano)-,2',6'-
trimethoxyretrochalcone (8) whose trivial name is (E)-praecansone A. This is the first
report on the isolation (E)-praecanson A (8) from the seedpods of T. aequilata. This
91
compound has been previously isolated from the roots of T. aequilata [Tarus et al.,
2002] and pods of T. pumila [Dagne et al., 1990], (Appendix G).
Figure 4.3: nOe interactions observed for (E)-praecansone A (8)
Table 4.7: 1H NMR (200 MHz) and 13 C (50 MHz) NMR data for (E)-praecansone
A
Position
1
2/6
8 (acetone-d6)
C (ppm) (ppm), m,J in Hz)
140.4
128.4
7.86 - 7.92 m
127.9
7.45 - 7.50 m
4
(C=O)
131.7
205.6
100.9
166.1
7.45 - 7.50 m
1'
2'
3'
107.7
158.5
112.8
-
6.56 s
-
Position
4'
5'
6’
2''
3''
4''
2''-Me2
OMe (C-2')
OMe (C-6')
OMe (C-)
92
8 (acetone-d6)
C (ppm)
(ppm), m,J in Hz)
155.1
96.0
6.19 s
155.7
76.4
117.0
127.3
27.6
27.5
61.7
55.9
55.6
5.57 d, (9.8)
6.49 d, (9.8)
1.42 s
1.40 s
3.70 s
3.64 s
3.88 s
4.2.2.1.2 Demethylpraecansone B (9)
Compound 9 was isolated as yellow needle-like crystals. On TLC plate the yellow spot
turned brown upon exposure to iodine vapour. Evidence that this compound is a
chalcone was available from the 1H NMR spectrum which showed a singlet for an
aromatic proton H-H 6.18) and corresponding 13C NMR signal for C-C100.9a
-oxygenated chalcones [Tarus et al., 2002]. The NMR (Table 4.8) further showed the
presence of a methoxyl (C 55.9, H 3.89 s), a 2,2-dimethylchromene (H 5.57, d, J = 10.0
Hz), for H-3''; 6.48, d, J = 10.0 Hz), for H-4'' and 1.41, s, 1.40, s, for 2''-(CH3)2 groups.
The 1H and 13C NMR spectra (H 7.86 - 7.91, m, 2H for H-2, -6; H 7.41 -7.50, m, 3H for
H-3, -4, -5; C 131.7 for C-1; 128.4 for C-2/6, 127.9 for C-3/5 and 131.7 for C-4) showed
that ring-A in compound 9 is unsubstituted. All the substituents are therefore located in
ring-B, with the hydroxyl and methoxyl being at C-2' and C-6', respectively. The 2,2dimethylpyrano group could either be attached at C-3'/4' (9) or adjacent to the methoxy
group as in (9a).
The
13
C NMR chemical shift value of the methoxyl (C = 55.9) is within the normal
range and is consistent with structure (9) rather than (9a) where the methoxyl group
being di-ortho-substituted resonates above 59 ppm [Yenesew et al., 1998]. The nOe
interactions between H-5' (6.55 s) and the methoxyl at 6'-OMe (3.89 sconfirms
the assignment of the aromatic proton to H-5' (Fig 4.4), (Appendix H).
93
Hence, this compound was identified as 3',4'-(2'',2''-dimethlylpyrano)-2'-hydroxy-6'methoxy--hydroxychalcone which is commonly known by its trivial name
demethylpraecansone B. This is the first report on the isolation of demethylpraecansone
B (9) from the seedpods of T. aequilata. However, it has previously been isolated from
some members of the Leguminosae family including the roots of T. aequilata [Tarus et
al., 2002] and seeds of Lonchocarpus constaricensis [Waterman and Mahmoud, 1985].
Figure 4.4: nOe interactions observed for demethylpraecansone B (9)
Table 4.8: 1H (200 MHz) and 13 C (50 MHz) NMR data for demethylpraecansone B
Position
1
2/6
3/5
4
C=O
1'
2'
9 (acetone-d6)
C (ppm) (ppm), m,J in Hz)
131.7
128.4
7.86 - 7.91 m
127.9
7.41 -7.50 m
131.7
7.41 - 7.50 m
100.9
6.18 s
166.1
188.7
107.7
155.7
Position
3'
4'
5'
6'
2''
3''
4''
6'-OMe
2''-Me2
94
9 (acetone-d6)
C (ppm) (ppm), m,J in Hz)
112.2
158.5
96.0
6.55 s
155.1
76.4
117.0
5.57 (d, J = 10.0 Hz)
127.2
6.48 (d, J = 10.0 Hz)
55.9
3.89 s
28.8
1.41 s
28.4
1.40 s
4.3 Biological Activities of the Isolated Compounds
4.3.1 Antiplasmodial activities of compounds from the seedpods of T.
elata
Some of the compounds isolated from the seedpods of T. elata were tested for
antiplasmodial activities against chloroquine-sensitive Sierra Leone I (D6) and
chloroquine-resistant Indochina I (W2) strains of P. falciparum (Table 4.9). The new
compound elatadihydrochalcone (1) exhibited good antiplasmodial activity with IC50
values of 2.8 + 0.3 and 5.5 + 0.3 g/ml against D6 and W2 strains of P. falciparum,
respectively. This compound along with the other flavonoids appears to be responsible
for the antiplasmodial activities observed in the crude extract.
It is worth noting that elatadihydrochalcone (1) is more active against the chloroquinesensitive
strain
(D6)
than
the
chloroquine-resistant
strain
(W2).
The
-
acetoxyelatadihydrochalcone (2) exhibited less activity against both strains of P.
falciparum with IC50 values of 9.6 + 2.1 g/ml and 12.6 + 0.5 g/ml against D6 and W2,
respectively, compared to that of elatadihydrochalcone (1). Obovatin (4) and obovatin
methyl ether (5) showed good activities (IC50 values of 4.9 + 1.7 and 6.4 + 1.1 g/ml)
and (IC50 values of 3.8 + 0.3 and 4.4 + 0.6 g/ml), respectively. The antiplasmodial
activities of some flavonoids [Andayi et al., 2006; Yenesew et al., 2003] especially of
chalcones [Taylor and Triggle, 2007; Liu et al., 2001 and Li et al., 1995], have been
reported. However, this is the first report on the antiplasmodial activity of a hydroxydihydrochalcone.
95
4. 3.2 Antiplasmodial Activities of compounds from the seedpods of T.
aequilata
The MeOH/CH2Cl2 (1:1) extract the seedpods of T. aequilata, yielded three compounds
which
include;
obovatin
methyl
ether
(5),
(E)-praecansone
A
(8)
and
demethylpraecansone B (9). (E)-Praecansone A (8) was tested against the D6 and W2
strains of P. falciparum, and showed good antiplasmodial activity with IC50 values of
6.6 + 1.1 g/ml and 6.4 + 1.0 g/ml, respectively.
Table 4.9: In vitro antiplasmodial activities of flavonoids isolated from T. elata and
T. aequilata against D6 and W2 strains of P. falciparum
IC50 in g/ml + SD
Tested compound
Elatadihydrochalcone (1)
D6
2.8 + 0.3
W2
5.5 + 0.3
-acetoxyelatadihydrochalcone (2)
9.6 + 2.1
12.6 + 0.5
Obovatin (4)
4.9 + 1.7
6.4 + 1.1
Obovatin methyl ether (5)
3.8 + 0.3
4.4 + 0.6
Deguelin/Rotenone (6/7) mixture
6.3 + 1.8
8.9 + 2.0
(E)-Praecansone A (8)
6.6 + 1.1
6.4 + 1.0
Chloroquine
0.008 + 0.004
0.051 + 0.010
Mefloquine
0.042 + 0.008
0.015 + 0.002
4.3.3 Results and Discussion of Larvicidal tests
The MeOH/CH2Cl2 (1:1) extract of the seedpods of T. elata was tested for larvicidal
activity against the third instar mosquito larvae of Aedes aegypti, and showed dose
dependent but lowlarvicidal activity (LC50 = 68.9 g/ml at 24 hours and 40.2 g/ml at 48
96
hours). Among the isolated compounds from the seedpods of T. elata, deguelin (6) was
tested for larvicidal activity against the third instar mosquito larvae of Aedes aegypti,
and showed dose dependent larvicidal activity (LC50 = 7.6 g/ml and at 24 hours and 4.0
gml-1 at 48 hours). The LC50 (7.6 g/ml) of the mixture of deguelin (6) and rotenone
(7) was comparable with the LC50 (8.54 g/ml) of the extract from the roots of Derris
trifoliata in the family (Leguminoseae) [Omena et al., 2007] and that of the ethanolic
extract of root wood of Annona crassiflora (LC50 = 8.94 g/ml) in the family of
Annonaceae [Omena et al., 2007]. However, the larvicidal activity observed in this
study is lower compared to that of the MeOH extract of the seeds of D. trifoliata which
showed good larvicidal activity against the 2nd instar larvae of Aedes aegypti with LC50
of 0.74 + 0.3 g/ml and that of rotenone, LC50 of 0.47 + 0.2 g/ml [Yenesew et al.,
2006; Fukami et al., 1971].
Table 4.10: Larvicidal test results for crude extract and isolated compounds from
the seedpods of T. elata.
LC50 in g/ml ± SD
Plant extract/compound
At 24 hours
At 48 hours
Crude extract
68.9 ± 0.3
40.2 ± 0.2
Deguelin (6) and rotenone (7)
7.6 ± 0.4
4.0 ± 0.2
Rotenone standard
4.4 ± 0.4
2.7 ± 0.3
97
CHAPTER FIVE
5.0 CONCLUSIONS AND RECOMMENDATIONS
5.1 Conclusions
In this study two plants (T. elata and T. aequilata) were investigated and a total of nine
compounds were isolated and characterized. The conclusions drawn from this study are
outlined below:
1. The phytochemical study on the seedpods of T. elata led to the isolation and
characterization of a total of seven compounds. These include; one hydroxydihydrochalcone,
{elatadihydrochalcone
(1)}
one
chalcone,
{obovatachalcone (3)}, two flavanones, {obovatin (4) and obovatin methyl ether
5)}, two rotenoids, {deguelin (6) and rotenone (7)}. Elatadihydrochalcone (1) is
a new compound belonging to the rare subclass of flavonoids, hydroxydihydrochalcone. This is the first report on the occurrence of a hydroxydihydrochalcone in the genus Tephrosia.
2. The literature NMR data on -hydroxydihydrochalcones were found to be
inconsistent and the identity of some of the compounds questioned.
3. The study on the seedpods of T. aequilata led to the isolation of three known
compounds which include a flavanones, obovatin methyl ether (5), a retrochalcone (E)-praecansone A (8) and demethylpraecansone B (9).
98
4. The antiplasmodial activities of the crude extracts and the flavonoids of these
medicinal plants were tested against chloroquine-sensitive strain (D6) and the
Chloroquine-resistant strain (W2) of P. falciparum parasite for malaria. The
results showed that among the flavonoids tested, the -hydroxydihydrochalcone
(1) had the highest activity followed by the flavanones, {obovatin methyl ether
(5) and obovatin (4)} and the retro-chalcone (8) in that order whereas the
rotenoids {deguelin (6) and rotenone (7)} had the least activity.
5. The results presented in this document indicate the possibilities of the use of hydroxydihydrochalcones and flavanones as lead structures in the future
development of antimalarial drugs.
6. In this study the crude extract of the seedpods of T. elata and its rotenoids were
tested for larvicidal activity against the larvae of Aedes aegypti. The results
indicate that the seedpods of this plant have potential use for small-scale control
of mosquitoes in rural communities where mosquito transmitted diseases such as
malaria is endemic.
5.2 Recommendations
Although the results of the study demonstrated moderate antiplasmodial and larvicidal
activities of the extracts and compounds isolated from the seedpods T. elata and T.
aequilata, more information on toxicity and efficacy is required as a means of
99
developing them into therapies for human use and for the control of mosquitoes. In order
to fulfil some of these requirements, I put forward the following recommendations:
1. Further phytochemical investigation of the seedpods of T. elata and T.
aequilata should be carried out in order to determine fully all the major and
isolable compounds that are synthesized by these medicinal plants.
2. In vivo antiplasmodial activity tests should be carried out on the extracts and
isolated compounds from these medicinal plants in order to establish their
potency and efficacy.
3. Toxicity study of the extracts and compounds from these medicinal plants is
necessary in order to establish their safety and efficacy.
4. The mechanism of action of the compounds needs to be fully examined so
that targeted proteins by these compounds can be clearly demonstrated for
differentiation with those of already established drugs. This information is
necessary as a platform for developing the compounds as therapies for
management of infections arising from resistant strains of P. falciparum
malaria parasite.
5. Comprehensive structure-activity relationship studies should be carried out
on the -hydroxydihydrochalcones and flavanones isolated in this study to
100
determine the functional groups responsible for the good antiplasmodial
activities observed.
6. The literature NMR data on -hydroxydihydrochalcones were found to be
inconsisitent and thus the need for thorough revision of the reported
structures.
101
REFERENCES
Abosi, A.O., Mbukwa, E., Majinda, R.R.T., Raseroka, B.H., Yenesew, A., Midiwo, J.O.,
Akala, H., Liyala, P and Waters, N.C. (2006). Vangueria infausta root bark: in
vivo and in vitro antiplasmodial activity. British Journal of Biomedical Science
63: 129-133.
Adinarayana, D., Syamasundar, K.V., Seligmann, O and Wagner, H. (1982). Structure
Elucidation of Pterosupin from Pterocarpus marsupium, the First Naturally
occurring C-Glycosyl--hydroxy-dihydrochalcone, Z. Naturforsch 37C: 145147.
Agnew, A.D.Q and Shirley A. (1994). Upland Kenya Wild Flowers, 2nd Edition. East
Africa National History Society: 118-121.
Agrawal, P.K. (1989). Studies in Organic Chemistry 39 “Carbon-13 NMR of
Flavonoids”. Published by Elsevier, Amsterdam, Nethalands.
Ahmad,V.U., Ali, Z.,Hussaini, S.R, Iqbal, F., Zahid, Abbas,M., Saba,N. (1999).
Flavonoids of Tephrosia purpurea. Fitoterapia 70: 443 – 445.
Andayi, A.W., Yenesew, A., Derese, S., Midiwo, J.O., Gitu, P.M., Jondiko, O.I., Waters,
N., Liyala, P., Akala, H., Heydenreich, M and Peter, M.G. (2006). Antiplasmodial activities of flavonoids from Erythrina sacleuxii. Planta Medica 72:
187-189.
102
Andrei C.C., Ferreira D.T., Faccione M., de Moraes L.A.B., de Carvalho M.G and BrazFilho R (2000). C-prenylflavonoids from roots of Tephrosia tunicata.
Phytochemistry 55: 799- 804.
Andrei, C.C., Vieira, P.C., Fernandes J.B., Da Silva M.F and Fo, E.R. (1997).
Dimethylchromene Rotenoids from Tephrosia candida. Phytochemistry 46:
1081-1085.
Anthonia, O.A and Benjamin H. R. (2003). In vivo antimalarial activity of Vernonia
amygdalina. British Journal of Biomedical Science 60: 89-91.
Beentje, H. (1994). Kenya trees, shrubs and lianas. National Museums of Kenya,
Nairobi: 269-320.
Bruce- Chwatt, L. (1993). In: Essential Malariology, 3rd Edn. H.M. Gllies, and D.A.
Warrall. Edward Arnold, London.
Camele, G., Monache, F.D., Monache, G.D and Marini-Betolo, G.B. (1980). Three new
flavonoids from Tephrosia praecans. Phytochemistry 19: 707–709.
Campbell, C.C. (1997). Malaria: an emerging and re-emerging global plague. FEMS
Immunology. Medical Microbiology 18: 325-331.
Chang, L.C., Chavez, D., Song, L.L., Farnsworth, N.R., Pezzuto, J.M and Kinghorn,
D.A. (2000). Absolute configuration of Novel Bioactive Flavonoids from
Tephrosia purpurea. Organic Letters 2: 515-518.
103
Chen, J. J., Lee, H. H., Duh, C. Y and Chen, I. S (2005). Cytotoxic Chalcones and
Flavonoids from the Leaves of Muntingia calabura. Planta Medica 71: 970-973.
Crombie, L and Whiting, D.A. (1998). Review article number 135 biosynthesis in the
rotenoid group of natural products: applications of isotope methodology.
Phytochemistry 49: 1479-1507.
Curtis, C.F., Lines, J.D., Baolin, L and Renz, A., (1990). Natural and synthetic
repellents. Appropriate technology in vector control 5.
Dagne, E., Bekele, A., and Waterman, P. G. (1989). The Flavonoids of Millettia
ferruginea subsp. Darassana in Ethiopia. Phytochemistry 28: 3207-9.
Dagne, E., Dinku, B., Gray, C.D., Waterman, P.G. (1988). Pumilaisoflavones A, B from
the seedpods of Tephrosia pumila. Phytochemistry 27: 1503–1505.
Dagne, E., Mammo, W., Bekele, A., Odyek, O and Byaruhanga, M.A (1991). OGeranylated and O-Prenylated flavonoids from Millettia ferruginea. Bull
Chemical Society of Ethiopia 5: 81-3.
Dagne, E., Mammo, W and Sterner, O. (1992). Flavonoids of Tephrosia polyphylla.
Phytochemistry 31: 3662-3663.
Dagne, E., Yenesew, A., Gray, A.I and Waterman, P.G. (1990). Praecanson A: Evidence
for the existence of 8,9-(E) and 8,9-(Z) Isomers in extracts from Tephrosia
pumila. Bull Chemical Society of Ethiopia 4: 141-145.
104
Derese S.W. (2004). Phtochemical investigation of some Kenyan Papilinoideae species
(Erythrina and Millettia species). Ph.D. Thesis, Department of Chemistry.
University of Nairobi.
Dewick, P.M (2002). Medicinal Natural Products: A Biosynthetic Approach. John Wiley
& Sons, 2nd edition, New.York.
Dewick, P.M. (1994). Isoflavonoids: In The Flavonoids: Advances in research since
1986. Chapman and Hall, London.
Dictionary of Organic Compounds on CD Rom. (2008), CRC Press
Duddeck, H., Yenesew, A., and Dagne, E. (1987). Isoflavonoids from Taverniera
abyssinica. Bull Chemical Society of Ethiopia 1: 32-35.
Dutt, S.K and Chibber, S.S. (1983). Candidol, a flavonol from Tephrosia candida.
Phytochemistry 22: 325-326.
Finney, D.J. (1971). Probit Analysis.3rd Edition. Cambridge University press.
Frankish, H., (2002). Scientists reach milestone in malaria research. Science and
Medicine, The Lancet Publishing Group 360: 1075.
Friis-Moller, A., Chen, M., Fuursted, K., Christensen, S.B., and Kharazmi. (2002): In
vitro anti-mycobacterial and anti-legionella activity of Licochalcone A from
Chinese Licorise roots. Planta Medica 68: 415-7.
105
Fukami, H., Nakajima, M., Jacobson, M and Crosby, D.G. (1971). Rotenone and
rotenoids. Ed, Naturally Occurring insecticides, Marce Dekker INC., New York:
71-75.
Garcez, F.R., Scramin, S., do Nascimento, M.C and Mors, W.B. (1988). Prenilated
flavonoids as evolutionary indicators in the genus Dahl-stedtia. Phytochemistry,
27 1079-1083.
Gareth T. (2004). Medicinal Chemistry. An introduction. John Wiley & Sons Ltd: 37406.
Geissbϋhler, Y., Chaki, P., Emidi, B., Govella, N.j., Shirima, R., Mayagaya,V., Mtasiwa,
D., Mshida, H., Filliger, U., Lindsay, S.W., Kannady, K.., de Castro, M. C.,
Tanner, M., and Gerry, F. (2007). Interdependence of domestic malaria
prevention measures and mosquito- human interactions in urban Dar es Salaam,
Tanzania. Malaria Journal 6:126-129.
Gomez-Garibay, F., Calderon, J.S., Arciniega, M. De La O., Cespedes, L.C and
Oswaldo T.V.T. (1999). An unusual isopropenyldihyfuran biflavanol from
Tephrosia crassifolia. Phytochemistry 52: 1159-1163.
Gomez-Garibay, F., Calderon, J.S., Quijano, L., Aguirre, G and Rios T. (1986). Abbottin
and tephrobotin two new flavonoids from Tephrosia abbottiae. . Chemistry and
industry 23: 827.
106
Gomez-Garibay, F., Calderon, J.S., Quijano, L., Dominguez, M and Rios T. (1985b).
Viridiflorin, an isoflavone from Tephrosia viridiflora. Phytochemistry 24: 1126-1128.
Gomez-Garibay, F., Calderon, J.S., Quijano, L., Morales, S and Rios T. (1988).
Prenylflavonoids from Tephrosia quercetorum. Phytochemistry 27: 2971-2973.
Gomez-Garibay, F., Calderon, J.S., Quijano, L., Rodriguez, J,S., Rodriguez and Rios T
(1985a). Prenylflavans from Tephrosia watsoniana. Phytochemistry 24: 1057-9.
Gomez-Garibay F., Calderon J.S., Quijano L, Tellez V., O, Olivares S.M and Rios T.
(1997). Unusual prenylbiflavonol from Tephrosia tepicana. Phytochemistry 46:
1285-1287.
Gomez-Garibay, F., De la O Arcienega, M., Cespedes, C. L., Taboada, J and Calderon,
J.S. (2001). Chromene chalcones from Tephrosia carrollii and the revised
structure of oaxacacin. Z. Naturforsch 56c: 969-972.
Gomez-Garibay, F., Quijano, L and Rios T (1991). Flavonones from Tephrosia
leiocarpa. Phytochemistry 30: 3832-4.
Gomez-Garibay, F., Tellez-Valdez, O., Moreno-Torres and Calderon, J. S. (2002).
Flavonoids from Tephrosia major. A New Prenyl--hydroxychalcone. Z.
Naturforsch 57c: 579-583.
Gratz, N.G and Pal, R. (1988). Malaria vector control: larviciding. Principles and
Practices of Malarialogy: 1213-5.
107
Hagemann, J.W., Pearl, M.B., Hggins, J.J., Delfel, N.E and Earle F.R. (1972). Rotenone
and Deguelin in Tephrosia vogelii at Several Stages of Maturity. Journal
Agricultural and Food Chemistry 20: 906-908.
Harborne, J., Toma s-Barbeba, N.F., Williams, C., Gil, M. (1986). A Chemotaxonomic
study of flavonoids from European Teucrium species. Phytochemistry 25: 2811.
Harborne, J.B. (1998). Phytochemical Methods. A guide to Modern Techniques of Plant
Analysis 3rd edition.
Heywood, V. (1971). The Leguminosae Systematic Preview. In: Chemotaxonomy of the
Leguminosae. Academic Press London: 1.
Hussaini, A.F and Shoeb, A. (1987). A New Epoxyflavanone from Tephrosia
hamiltonii. Planta Medica 53: 220-221.
Ingham, J.L., Markham, K.R. (1980). Tephrocarpin, a pterocarpan phytoalexin from
Tephrosia bidwilli and a structure proposal for acanthocarpan. Phytochemistry
21: 2969-2972.
Induli, M. (2006). Antiplasmodial Flavonoids from the Stem Bark of Erythrina
abyssinica. MSc. Thesis. Chemistry Department, University of Nairobi, Kenya.
James, E. I and Ruben H. F. (1958). Occurrence of Rotenoids in some Species of the
Genus Tephrosia. Journal of Agricultural and Food Chemistry, 7: 106-107.
108
Jang, D.S., Park, J.U., Kang, Y.H., Hawthorne, M.E., Vigo, J.S., Graham, J.S., Pezzuto,
J.M., and Kinghorn, A.D. (2003). Potential Cancer Chemopreventive Flavonoids
from the Stem of Tephrosia toxicaria. J. Nat. Prod 66: 1166-1170.
Johnson, J.D., Dennull, R.A., Gerena, L., Lopez-Sanchez, M., Roncal, N.E and Waters
N.C (2007) Assessment and Continued Validation of Malaria SYBR Green I –
Based Fluorescence Assay for use in Malaria Drug Screening, Antimicrobial
Agents and Chemotherapy 51: 1926-1933.
Kigondu, E.V.M (2007). Phytochemical and anti-parasitic activity studiesof some
selected Kenyan Medicinal Plants, MSc. Thesis, Jomo Kenyatta University of
Agriculture and Technology, Kenya.
Kiplagat, J.T. (2006). Larvicidal and Antiplasmodial Compounds from Derris trifoliata,
Lonchocarpus eriocalyx and Erythrina sacleuxii. MSc. Thesis, Department of
Chemistry. University of Nairobi, Kenya.
Kirira, P.G., Rukunga, G.M., Wanyonyi, A.W., Muregi, F.M., Gathirwa, J.W.,
Muthaura, C.N., Omar, S.A., Tolo, F., Mungai, G.M and Ndiege, I.O. (2006).
Antiplasmodial activity and toxicity of extracts of plants used in traditional
malaria therapy in Meru and Kilifi Districts of Kenyan. Journal of
Ethnopharmacology. Elsevier science publisher Ireland 30: 1-4.
109
Kishore, P.H., Mopuru V.B.R., Duvvuru, G., Madugula, M.M., Cristelle, C and Bernard,
B. (2003). A New Coumestan from Tephrosia calophylla. Chemical
Pharmacognosy Bull. 51: 194-196.
Kokwaro, J.O. (1993). Medicinal Plants of East Africa. East Africa Literature Bureau,
Nairobi: 250 -255.
Kole, R.K., Satpathi, C., Chowdhury, A., Ghosh, M.R and Adityachaudhury, N (1992).
Isolation of Amorpholone, a Potent Rotenoid Insecticide from Tephrosia
candida. Journal of Agricultural and Food Chemistry 40: 1208-1210.
Li, R., Kenyon, G.L., Cohen, F.E., Chen, X and Gong, B. (1995). In vitro antimalarial
activity of chalcones and their derivatives, Journal of Medicinal Chemistry 38:
5031-5037.
Liu, M., Wilairat, P and Go, M.L. (2001). Antimalarial alkoxylated and hydroxylated
chalcones [corrected]: structure-activity relationship analysis, Journal of
Medicinal Chemistry 44: 4443-4452.
Lwande, W. (1985). Flavonoids from the roots of Tephrosia elata. Journal of Natural
Products 48: 1004-1005.
Lwande, W., Bentley, M.D and Hassanali, A. (1986). The structure of hildecarpin, an
insect antifeedant 6a-hydroxypterocarpin from the roots of Tephrosia
hildebrandtii Vatke. Insect, Science, Application 7: 501–503.
110
Lwande, W., Bentley, M.D., Macfoy, C., Lugemwa, F.N., Hassanali, A and Nyandat, E.
(1987). A new pterocarpan from the roots of Tephrosia hildebrandtii.
Phytochemistry 26: 2425-2426
Machocho, A.K., Lwande, W., Jondiko, J.I., Moreka, L.V.C., Hassanali, A. (1995).
Three new flavonoids from the roots of Tephrosia emoroides, their antifeeding
activity against the larvae of the spotted stalk borer Chilo partellus. Journal of
Pharmacognosy 33: 222–227.
Madrid, P.B., Sherrill, J., Liou, A.P., Weisman, J.L., DeRisi, J.L and Guy, R.K. (2005).
Synthesis of ring-substituted 4-aminoquinolines and evaluation of their antimalarial activities. Bioorganic and Medicinal Chemistry Letters 15: 1015-1018.
Maillard, M., Gupta, M.P and Hostettmann, K. (1987). A New antifungal prenylated
flavanone from Erythrina berteroana. Planta medica 3: 563.
Malcom, C.A. (1988). Current status of pyrethroid resistance in anophelines.
Parasitology Today 4: 13.
Malkham, K.R. (1982). Techniques of Flavonoids identification, Academic Press,
London, New York: 1.
Manners, G.D and Jurd L (1979). Additional Flavonoids in Gliricidia sepium.
Phytochemistry 18: 1037-1042.
111
Mark, S.B. (2004). The Role of Natural Product Chemistry in Drug Discovery. Journal
of Natural Products 67: 2141- 2153.
McLaughlin, J.L., Chang, C.J and Smith, D.L., (1991). “Bench-Top” bioassays for the
discovery of natural products: An update; In: Studies In Natural Products
Chemistry, Atta-Ur-Rahman Edition 9: 383-5.
Murthy, M.S.R and Rao V.E. (1985). Maxima Isoflavone J: A New 0-prenylated
Isoflavone from Tephrosia maxima. Journal of Natural Products 48: 967-968.
Mwangi, R.W and Rembold, H. (1998). A growth inhibiting and larvicidal effect of
Melia volkensii extracts on Aedes aegypti larvae. Entomologia experimentalis
Applicata 46: 103.
Nel, R.J.J., van Rensburg, H., van Heerden, P.S., Coetzee, J and Ferreira D (1999).
Stereoselective
Synthesis
of
Flavonoids.
Part
7.
Poly-oxygenated
hydroxydihydrochalcones Derivatives, Tetrahedron 55: 9727-9736.
Nkunya, M.H.H. (1992). Progress in the Search for Anti-malarials. NAPRECA
Monograph Series No. 4, NAPRECA, Addis Ababa: 5.
Omena, M.C., Navarro D.M.A.F., de Paula J.E,Luna J.S., Ferreira de Lima M.R and
Sant’Ana A.E. G. (2007). Larvicidal activities against Aedes aegypti of some
Brazilian Medicinal plants. Bioresource Technology 98: 2549-2556.
112
Parmar, V.S., Rathore, J.S., Jain, R., Henderson, A and Malone, J.F. (1989). Occurrence
of pongamol as the enol structure in Tephrosia purpurea. Phytochemistry 28:
591-593.
Parmar, V.S., Ole Simonsen, R.J and Boll, P.M. (1987). Isolation of candirone: a novel
pentaoxygenation pattern in a naturally occurring 2-phenyl-4h-1-benzopyran-4one from. Tephrosia candida. Tetrahedron 43: 4241-7.
Peter, J. K. (2007). Nelson Text Book of Paediatrics 18th Edition, Saunders Elsevier Inc:
1477-1484.
Phillipe, P., Miller R.S. (2002). Quinine in Mordern Treatment of P. falciparum Malaria.
Lancet Infectoius Diseases 2: 206.
Polhill, R.M., Ravan, P.H and Stirton, C.H., (1981a). Evolution and Systematics of
Evolution of Leguminosae, in Advances in Legume Systematics. Part I. Royal
Botanic Gardens, Kew: 1.
Polhill, R.M., Ravan, P.H., Stirton, C.H., (1981b). Papilionodeae. In. Advances in
Legume Systematics. Part I. Royal Botanic Gardens, Kew: 191.
Polrat, W., Srivicha K., Sombat K., Kobsiri C., and Sornchai L. (2002). The Future
Outlook of Anti-malarial Drugs and Recent work on the Treatment of Malaria.
Archives of Medical Research 33: 416-421.
113
Prabhakar, P., Vanangamudi, A., Gandhidasan, R., Venkateswara, P.R. (1996).
Hookerianin: a flavone from Tephrosia hookeriana. Phytochemistry 43: 315-316
Prashant, A and David Krupadanam, G. L. (1993). Dehydro-6-hydroxyrotenoid and
lupenone from Tephrosia villosa. Phytochemistry 32: 484-486.
Rafi, M.M., Vastano, B.C., Zhu, N., Ho, C.T., Ghai, G., Rosen, R.T., Gallo, M.A and
Dipaola R.S. (2002). Novel polyphenol molecule isolated from Licroice Root
(Glyccrrhiza glabra) induces apopotosis, G2/M cell cycle arrest, and Bcl-2
Phosphorylation in Tumor cell lines. Journal of Agricultural and Food
Chemistry 50: 677-684.
Rajani, P and Sarma, N. (1988). A coumestone from the roots of Tephrosia hamiltonii.
Phytochemistry 27: 648-649.
Ramen, K.K., Chittaranjan, S., Ashim, C., Ghosh, M.R and Adityachaudhury. (1992).
Isolation of Amorpholone, a Potent Rotenoid Insecticide from Tephrosia
candida. Journal of Agricultural and Food Chemistry 40: 1208-1210.
Rang, H.P., Dale M.M., Ritter J.M and Moore P.K. (2003). Pharmacology 5th Edition.
Churchill Livingstone, Elsevier Limited, London: 672-82.
Rao, E.V., Rajendra, P.Y. (1992). Prenylated flavonoids from Tephrosia spinosa.
Phytochemistry 32: 183-185.
114
Rao, E. V., Rajendra, P. M., Sree, R.M. (1994). A prenylated flavanone from Tephrosia
maxima. Phytochemistry 37: 111-112.
Rao, E. V., Ranga, R. N. (1984). Two flavonoids from Tephrosia purpurea.
Phytochemistry 23: 2339-2342.
Rao, E.V., Venkataratnam, G. Vilain, C. (1985). Flavonoids from Tephrosia fulvinervis.
Phytochemistry 24: 2427-2430.
Rates, S.M.K. (2001). Plants as source of drugs. Toxicon , 39: 603-613.
Roy, M., Bhattacharya, P.K., Pal, S., Chowdhuri, A and Adityachaudhury, N. (1987).
Dehydrodihydrorotenone
and
flemichapparin-B
in
Tephrosia
candida.
Phytochemistry 26: 2423-2425.
Roy, M., Mitra, S.R., Bhattacharya, A., Adityachaudhury, N. (1986). Candidone, a
flavanones from Tephrosia candida. Phytochemistry 25: 961-3.
Santram, L., Rajesh, S. P., Alok, P.J., Singhai, A.K. (2006). Wounding healing potential
of Tephrosia purpurea (Linn.) Pers. in rats. Journal of Ethnopharmacology 108:
204 – 210.
Smalberger, T. M,. Vleggaar, R,. de Waal, H. L. (1972). Two new flavones from
Tephrosia polystachyoides bak.f. Tetrahedron Letters 13: 703-704.
115
Smalberger, T. M., Vleggaar, R. Weber, J. C. (1974). Flavonoids from Tephrosia-VII :
The constitution and absolute configuration of lupinifolin and lupinifolinol, two
flavanones from Tephrosia lupinifolia Burch (DC). Tetrahedron 30: 3927-3931
Smilkstein, M., Sriwilaijaroen, N., Kelly, J.X., Wilairat, P and Riscoe, M, (2004).
Simple and inexpensive fluorescence-based technique for high-throughput
antimalarial drug screening. Antimicrobial Agents & Chemotherapy 48: 1803–
1806.
Tanaka, T., Iinuma, M., Yuki, K., Fujii, Y and Mizuno, M. (1992). Flavonoids in Root
Bark of Pongamia pinnata, Phytochemistry 31: 993-998.
Tarus, P.K., Machocho, A.K., Lang’at–Thoruwa, C.C and Chhabra S.C. (2002).
Flavonoids from Tephrosia aequilata, Phytochemistry 60: 375 – 379.
Taylor, J.B and Triggle, D.J. (2007). Comprehensive Medicinal Chemistry II. 1st edition.
Elsevier Ltd , UK, 7: 752-813.
Trease and Evans. (2002). Pharmacognosy 15th Edition. Harcount Publishers Limited,
London: 3
Thuy, T.T., Porzel, A., Ripperger, H., van Sung T and Adam G (1998). Chalcones and
ecdysteroids from Vitex leptobotrys. Phytochemistry 49: 2603-2605.
116
Venkataratnam, G., Rao, E.V and Vilain, C. (1987). Flavonoids of Tephrosia
procumbens-revised structure for praecansone A conformation of Praecansone B.
Journal of the Chemical Society Perkin Transactions 1: 2723–2727.
Venkataratnam, G., Rao, E.V., Vilain, C. (1986). Fulvinervin C, a flavone from
Tephrosia fulvinervis. Phytochemistry 25: 1507-1508.
Vishnu, J.R., Abhishek, S.S., Srivastava, S and Chandra, S. (2000). Oxygenated
Chalcones and Bischalcones as Potential antimalarial Agents. Bioorganic and
Medicinal Chemistry Letters 10: 2159 – 2161.
Wakelin, D. (1996). Immunity to parasites: How parasitic infections are controlled, 2nd
edition. Cambridge: Cambridge University Press: 44 – 69.
Waterman, P.G and Khalid, A.S. (1980). The Major Flavonoids of the seeds of
Tephrosia apollinea. Phytochemistry 19: 909-915.
Waterman, P.G and Mahmoud, E.N. (1985). Flavonoids from the seeds of Lonchocarpus
costaricensis. Phytochemistry 24: 571-4.
WHO (1995). Vector Control for Malaria and other Mosquito- Borne Diseases. WHO
Tech. Rep. Ser 857:1-91.
Woo, E.K., Kwak, H.J and Park H. (1998). A new prenylated flavonol from the roots of
Sophora flavescens. Journal of Natural Products 61: 1552.
117
Yang, Y.C., Lee, S.G., Lee, H.K., Kim, M.K., Lee, S.H., (2002). A piperidine amide
extracted from Piper logum L. fruit shows activity against Aedes aegypti
mosquito larvae. Journal of Agricultural and food Chemistry 50: 3765.
Yenesew, A. (1997). Chemical Investigation of two Millettia and two Erythrina species
(Leguminosae) for Bioactive Constituents. Ph.D. Thesis, Department of
Chemistry, University of Nairobi.
Yenesew, A., Dagne, E., Waterman, P.G., (1989). Flavonoids from the
seed pods of Tephrosia pumila. Phytochemistry 28: 1291–1292.
Yenesew, A., Derese, S., Irungu, B., Midiwo, J.O., Norman, C.W., Pamela, L., Hosea,
A., Heydenreich M and Peter M.G. (2003). Flavonoids and Isoflavonoids with
Antiplasmodial activities from the root Bark of Erythrina abyssinica. Planta
Medica 69: 658-661.
Yenesew, A., Kiplagat, J.T., Derese, S., Midiwo, J.O., Kabaru, J.M., Heydenreich, M
and Peter M.G. (2006). Two unusual rotenoids derivatives, 7a-O- methyl-12a
hydroxydeguelol and spiro-13-homo-13-oxaelliptone, from the seeds of Derris
trifoliata. Phytochemistry 67: 988-991.
Yenesew, A., Midiwo, J.O., Miessner, M., Heydenreich, M and Peter, M.G. (1998a).
Two prenylated flavanones from stem bark of Erythrina burttii, Phytochemistry
48: 1439-1443.
118
APPENDICES
119
APPENDIX A: SPECTRA FOR COMPOUND 1
120
1H
NMR SPECTRUM FOR COMPOUND 1 (300 MHz, CDCl3)
121
1H
NMR SPECTRUM EXPANSION FOR COMPOUND 1
122
1H
NMR SPECTRUM EXPANSION FOR COMPOUND 1
123
13
C NMR SPECTRUM FOR COMPOUND 1 (75 MHz, CDCl3)
124
13C
NMR SPECTRUM EXPANSION FOR COMPOUND 1
125
1H-1H
COSY SPECTRUM FOR COMPOUND 1
126
HMBC SPECTRUM FOR COMPOUND 1
127
HMBC SPECTRUM EXPANSION FOR COMPOUND 1
128
HBMC SPECTRUM EXPANSION FOR COMPOUND 1
129
HMBC SPECTRUM EXPANSION FOR COMPOUND 1
130
HMQC SPECTRUM FOR COMPOUND 1
131
HMQC SPECTRUM EXPANSION FOR COMPOUND 1
132
EI-MS SPECTRUM FOR COMPOUND 1
133
HR-MS SPECTRUM FOR COMPOUND 1
m/z
134
CD SPECTRUM FOR COMPOUND 1
135
UV SPECTRUM FOR COMPOUND 1 (MeOH)
136
APPENDIX B: SPECTRA FOR COMPOUND 2
137
1H
NMR SPECTRUM FOR COMPOUND 2 (300 MHz, CDCl3)
138
1H
NMR SPECTRUM EXPANSION FOR COMPOUND 2
139
1H
NMR SPECTRUM EXPANSION FOR COMPOUND 2
140
13C
NMR SPECTRUM FOR COMPOUND 2 (75 MHz, CDCl3)
141
13C
NMR SPECTRUM EXPANSION FOR COMPOUND 2
142
13C
NMR SPECTRUM EXPANSION FOR COMPOUND 2
143
1H-1H
COSY SPECTRUM FOR COMPOUND 2
144
HMBC SPECTRUM FOR COMPOUND 2
145
HMBC SPECTRUM EXPANSION FOR COMPOUND 2
146
HMQC SPECTRUM FOR COMPOUND 2
147
HMQC SPECTRUM EXPANSION FOR COMPOUND 2
148
EI-MS SPECTRUM FOR COMPOUND 2
149
APPENDIX C: SPECTRA FOR COMPOUND 3
150
1H
NMR SPECTRUM FOR COMPOUND 3 (200 MHz, acetone-d6)
151
13C
NMR SPECTRUM FOR COMPOUND 3 (50 MHz, acetone-d6)
152
1H-1H
COSY SPECTRUM FOR COMPOUND 3
153
NOE SPECTRUM FOR COMPOUND 3
154
APPENDIX D: SPECTRA FOR COMPOUND 4
155
1H
NMR SPECTRUM FOR COMPOUND 4 (300 MHz, CDCl3)
156
1H
NMR SPECTRUM EXPANSION FOR COMPOUND 4
157
13C
NMR SPECTRUM FOR COMPOUND 4 (75 MHz, CDCl3)
158
1H-1H
COSY SPECTRUM FOR COMPOUND 4
159
HMBC SPECTRUM FOR COMPOUND 4
160
HMQC SPECTRUM FOR COMPOUND 4
161
APPENDIX E: SPECTRA FOR COMPOUND 5
162
1H
NMR SPECTRUM FOR COMPOUND 5 (300 MHz, CDCl3)
163
1H
NMR SPECTRUM EXPANSION FOR COMPOUND 5
164
13C
NMR SPECTRUM FOR COMPOUND 5
165
APT SPECTRUM FOR COMPOUND 5
166
1H-1H
COSY SPECTRUM FOR COMPOUND 5
167
HMBC SPECTRUM FOR COMPOUND 5
168
HMQC SPECTRUM FOR COMPOUND 5
169
APPENDIX F: SPECTRA FOR COMPOUND 6 &7
170
1H
NMR SPECTRUM FOR COMPOUND 6 & 7 (300 MHz, CDCl3)
171
13C
NMR SPECTRUM FOR COMPOUNDS 6 & 7 (75 MHz, CDCl3)
172
APT SPECTRUM FOR COMPOUNDS 6 & 7
173
APPENDIX G: SPECTRA FOR COMPOUND 8
174
1H
NMR SPECTRUM FOR COMPOUND 8 (200 MHz, acetone-d6)
175
13C
NMR SPECTRUM FOR COMPOUND 8 (50 MHz, acetone-d6)
176
APPENDIX H: SPECTRA FOR COMPOUND 9
177
1H
NMR SPECTRUM FOR COMPOUND 9 (200 MHz,CDCl3)
178
13
C NMR SPECTRUM FOR COMPOUND 9 (50 MHz,CDCl3)
179
APPENDIX I: PUBLICATION
180
181