Evaluation of ROM
advertisement
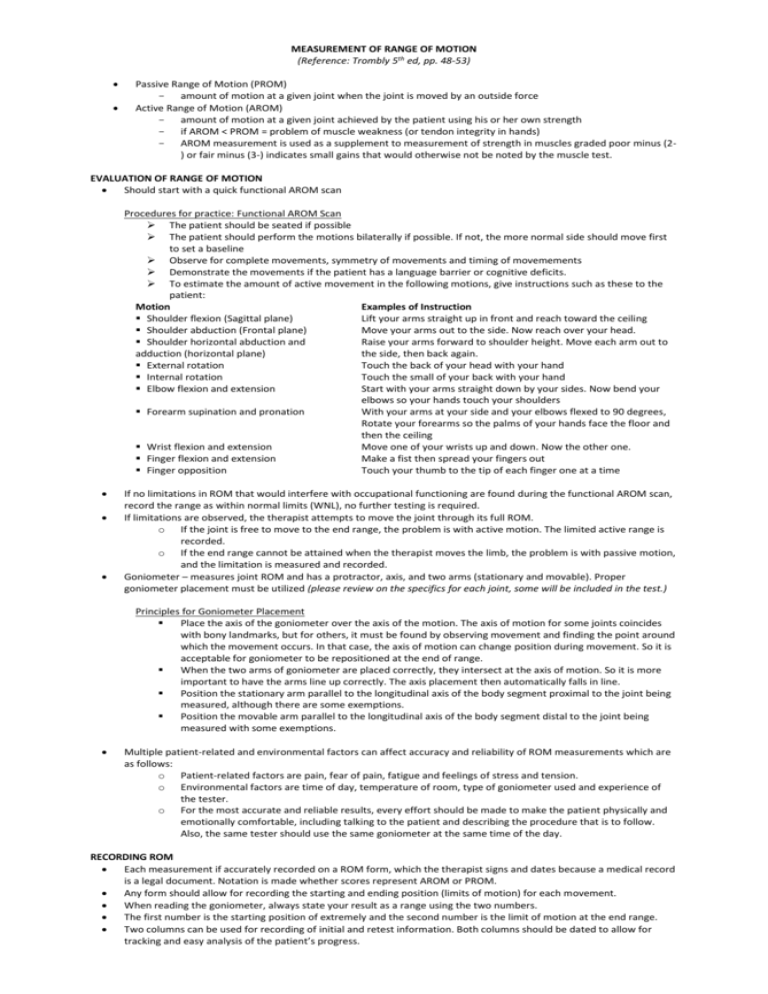
MEASUREMENT OF RANGE OF MOTION (Reference: Trombly 5th ed, pp. 48-53) Passive Range of Motion (PROM) - amount of motion at a given joint when the joint is moved by an outside force Active Range of Motion (AROM) - amount of motion at a given joint achieved by the patient using his or her own strength - if AROM < PROM = problem of muscle weakness (or tendon integrity in hands) - AROM measurement is used as a supplement to measurement of strength in muscles graded poor minus (2) or fair minus (3-) indicates small gains that would otherwise not be noted by the muscle test. EVALUATION OF RANGE OF MOTION Should start with a quick functional AROM scan Procedures for practice: Functional AROM Scan The patient should be seated if possible The patient should perform the motions bilaterally if possible. If not, the more normal side should move first to set a baseline Observe for complete movements, symmetry of movements and timing of movemements Demonstrate the movements if the patient has a language barrier or cognitive deficits. To estimate the amount of active movement in the following motions, give instructions such as these to the patient: Motion Examples of Instruction Shoulder flexion (Sagittal plane) Lift your arms straight up in front and reach toward the ceiling Shoulder abduction (Frontal plane) Move your arms out to the side. Now reach over your head. Shoulder horizontal abduction and Raise your arms forward to shoulder height. Move each arm out to adduction (horizontal plane) the side, then back again. External rotation Touch the back of your head with your hand Internal rotation Touch the small of your back with your hand Elbow flexion and extension Start with your arms straight down by your sides. Now bend your elbows so your hands touch your shoulders Forearm supination and pronation With your arms at your side and your elbows flexed to 90 degrees, Rotate your forearms so the palms of your hands face the floor and then the ceiling Wrist flexion and extension Move one of your wrists up and down. Now the other one. Finger flexion and extension Make a fist then spread your fingers out Finger opposition Touch your thumb to the tip of each finger one at a time If no limitations in ROM that would interfere with occupational functioning are found during the functional AROM scan, record the range as within normal limits (WNL), no further testing is required. If limitations are observed, the therapist attempts to move the joint through its full ROM. o If the joint is free to move to the end range, the problem is with active motion. The limited active range is recorded. o If the end range cannot be attained when the therapist moves the limb, the problem is with passive motion, and the limitation is measured and recorded. Goniometer – measures joint ROM and has a protractor, axis, and two arms (stationary and movable). Proper goniometer placement must be utilized (please review on the specifics for each joint, some will be included in the test.) Principles for Goniometer Placement Place the axis of the goniometer over the axis of the motion. The axis of motion for some joints coincides with bony landmarks, but for others, it must be found by observing movement and finding the point around which the movement occurs. In that case, the axis of motion can change position during movement. So it is acceptable for goniometer to be repositioned at the end of range. When the two arms of goniometer are placed correctly, they intersect at the axis of motion. So it is more important to have the arms line up correctly. The axis placement then automatically falls in line. Position the stationary arm parallel to the longitudinal axis of the body segment proximal to the joint being measured, although there are some exemptions. Position the movable arm parallel to the longitudinal axis of the body segment distal to the joint being measured with some exemptions. Multiple patient-related and environmental factors can affect accuracy and reliability of ROM measurements which are as follows: o Patient-related factors are pain, fear of pain, fatigue and feelings of stress and tension. o Environmental factors are time of day, temperature of room, type of goniometer used and experience of the tester. o For the most accurate and reliable results, every effort should be made to make the patient physically and emotionally comfortable, including talking to the patient and describing the procedure that is to follow. Also, the same tester should use the same goniometer at the same time of the day. RECORDING ROM Each measurement if accurately recorded on a ROM form, which the therapist signs and dates because a medical record is a legal document. Notation is made whether scores represent AROM or PROM. Any form should allow for recording the starting and ending position (limits of motion) for each movement. When reading the goniometer, always state your result as a range using the two numbers. The first number is the starting position of extremely and the second number is the limit of motion at the end range. Two columns can be used for recording of initial and retest information. Both columns should be dated to allow for tracking and easy analysis of the patient’s progress. The most common method of determining ROM is the neutral zero method recommended by the Committee of Joint Motion of the American Academy of Orthopaedic Surgeons. In this method, the anatomical position is considered is considered to be 0 degrees, or if a given starting position is different from the anatomical position. It is defined as zero measurement is taken from the stated starting position to the stated end position. If the patient cannot achieve the stated starting and end position, the actual starting and end position are recorded to indicate limitations of movement. An example of this using elbow flexion is as follows: o 0-150 degrees : No Limitation o 20-150 degrees : A limitation in extension (problem with the start position) o 0-120 degrees : A limitation in flexion (problem with the end position) o 20-120 degrees : A limitation in flexion and extension (problem with the start and end positions) To record hyperextension of a joint, which may be occasionally seen in metacarpophalengeal or elbow joints, the American Academy of Orthopaedic Surgeons recommends a separate measurement to describe the available ROM without confusion. For example, if 20 degrees of elbow hyperextension (an unnatural movement) is noted, it should be recorded as follows: o 0-150 degrees of flexion o 150 to 0 degrees of extension o 0-20 degrees of hyperextension If a joint is fused, the starting and end positions are the same, with no ROM. This is recorded as fused at x0. If move in one direction, the ROM limited motion is recorded as none. For example, if wrist flexion is 15 to 80 degrees with a 15 degrees flexion contracture, the wrist cannot be positioned at 0 or moved into extension therefore wrist extension is recorded as none. Because there are various systems of notation, each having its own meaning, it is important to clarify the intended meaning to ensure consistency among therapists and physicians within the same facility. INTERPRETING THE RESULTS Significant Limitation – one that decreases functional performance or may lead to deformity. The therapist noted whether the limitation is the result of tissue changes (PROM < NROM) or muscle weakness (AROM < PROM) The therapist can compare the scores of the involved and the other extremities but must be mindful that there are studies that found significant difference in ROM between dominant and nondominant sides. The nondominant side had greater range in many upper extremity joints tested. This info must be kept in mind when comparing the two sides. The patient’s scores can be compared with the average limits (norms) expected for each motion. The average limits stated by the Committee of Joint Motion of the American Academy of Orthopaedic Surgeons are commonly used. However, patients may be functional with less ROM than is noted in the norms for particular joints. The emphasis of OT is functional movement. With the probable cause in mind, treatment goals vary for the identified problems cited: o If it be as a result of skin and/or muscle tissue shortening due to immobilization, the goal is to increase range by stretching these tissues. o If as a result of edema, pain, spasticity, or muscle weakness, the primary goal is to reduce or correct the underlying problem and the secondary goal is to prevent the loss of ROM caused by immobility imposed by the primary condition. o If the cause is bony ankylosis or longstanding contractures, the goal is to teach the patient methods of compensation, since these conditions do not respond to nonsurgical treatments. It is important to compare initial evaluation scores to mid and post treatment scores to assess the outcome and redirect treatment if necessary. For a difference in measurements of Rom to be considered to reflect actual change, the amount of change must exceed measurement error which was found to be 50 for UE and 60 for LE.