106 - Medical Home Oncology
advertisement
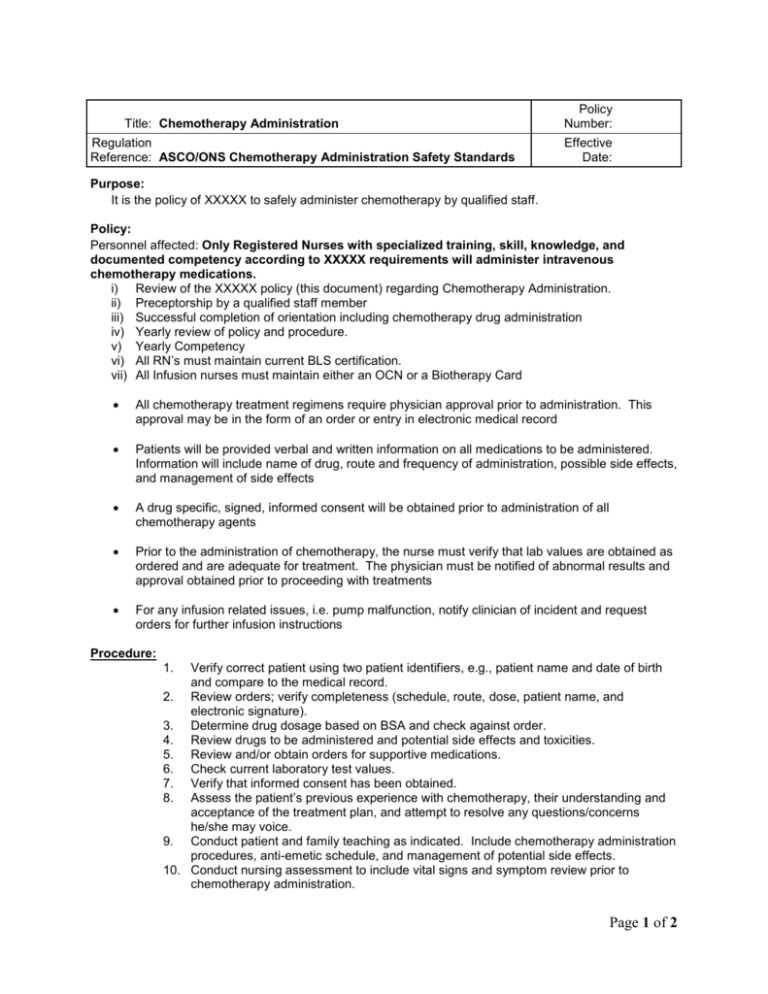
Title: Chemotherapy Administration Regulation Reference: ASCO/ONS Chemotherapy Administration Safety Standards Policy Number: Effective Date: Purpose: It is the policy of XXXXX to safely administer chemotherapy by qualified staff. Policy: Personnel affected: Only Registered Nurses with specialized training, skill, knowledge, and documented competency according to XXXXX requirements will administer intravenous chemotherapy medications. i) Review of the XXXXX policy (this document) regarding Chemotherapy Administration. ii) Preceptorship by a qualified staff member iii) Successful completion of orientation including chemotherapy drug administration iv) Yearly review of policy and procedure. v) Yearly Competency vi) All RN’s must maintain current BLS certification. vii) All Infusion nurses must maintain either an OCN or a Biotherapy Card All chemotherapy treatment regimens require physician approval prior to administration. This approval may be in the form of an order or entry in electronic medical record Patients will be provided verbal and written information on all medications to be administered. Information will include name of drug, route and frequency of administration, possible side effects, and management of side effects A drug specific, signed, informed consent will be obtained prior to administration of all chemotherapy agents Prior to the administration of chemotherapy, the nurse must verify that lab values are obtained as ordered and are adequate for treatment. The physician must be notified of abnormal results and approval obtained prior to proceeding with treatments For any infusion related issues, i.e. pump malfunction, notify clinician of incident and request orders for further infusion instructions Procedure: 1. Verify correct patient using two patient identifiers, e.g., patient name and date of birth and compare to the medical record. 2. Review orders; verify completeness (schedule, route, dose, patient name, and electronic signature). 3. Determine drug dosage based on BSA and check against order. 4. Review drugs to be administered and potential side effects and toxicities. 5. Review and/or obtain orders for supportive medications. 6. Check current laboratory test values. 7. Verify that informed consent has been obtained. 8. Assess the patient’s previous experience with chemotherapy, their understanding and acceptance of the treatment plan, and attempt to resolve any questions/concerns he/she may voice. 9. Conduct patient and family teaching as indicated. Include chemotherapy administration procedures, anti-emetic schedule, and management of potential side effects. 10. Conduct nursing assessment to include vital signs and symptom review prior to chemotherapy administration. Page 1 of 2 11. Obtain IV access and connect to primary baseline fluids at least at KVO rate, unless otherwise specified by physician order. a) Venipuncture Select distal sites before proximal sites Evaluate general condition of veins Note type of medication to be infused Sites where damage to underlying tendons or nerves is more likely to occur – antecubital region, wrist, distal surface of the hand, areas with recent venipuncture, should be avoided when possible sites, sclerosed veins, or areas of previous surgery such as skin grafts, side of mastectomy, lumpectomy, node dissection, or partial amputation b) Portacath or vascular access device Refer to Policy XXXXX (Implanted VAD: Access, Lab Draw, Maintenance, Troubleshooting) Assess for patency by flushing the line with normal saline Observe for signs and symptoms of infiltration and for blood return 12. Prepare drugs as ordered. Note: If mixing on site, Chemotherapy drugs should not be mixed until IV access has been obtained. 13. Two (2) clinical personnel, RN must be one of them, check the drug label, for correct patient, correct dosage, and consistency with orders. 14. Locate and secure appropriate emergency equipment as indicated 15. Administer pre-chemotherapy hydration, anti-emetics, and other premedications, if ordered 16. Administer chemotherapy drugs according to XXXXX Dilution and Stability Chart, or as specified by physician orders, with attention to the five patient rights. Right medication Right time. Right route. Right dose. Right patient. 17. Frequently assess the patient for signs of infiltration (burning, pain, swelling, redness) and extravasation 18. Allow 3-30 ml’s of normal saline to infuse between drugs and at completion of the infusion 19. Observe patient for at least 15 minutes after medication completed with IV needle or catheter in place and NS at rate to maintain patency. 20. Remove the needle or IV catheter, or inject heparin into the central line or device indicated 21. Apply dressing to site and gentle pressure to reduce local bleeding Responsibility and Approval Authority: This policy shall be reviewed by the appropriate committees, managers and staff to whom it is relevant, approved by the Executive Committee of the Board, with final signatory authority of the Medical Director. Version Number: Original Approval Date: Reviewed Date: Revision Prepared by: Approved by: Page 2 of 2






