Reproductive System - Parkland Secondary School
advertisement

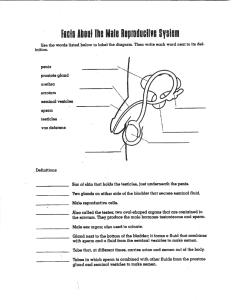
Reproductive System PLO P1 (414-417) Male Reproductive System Anatomy Organ testes seminiferous tubules interstitial cells epididymis ductus (vas) deferens prostate gland Structure male gonads suspended within the scrotum outside the abdominal cavity consists of lobules of seminiferous tubules & interstitial cells one to three tightly coiled tubules within each lobule of the testes collectively they measure about 250 m in length typical cell structure found between the seminiferous tubules (in the lobules of the testes) coiled tube lying on the dorsal and anterior surface of the testes within the scrotum muscular duct that curves around the bladder & connects the epididymis to the ejaculatory duct single doughnut-shaped gland that surrounds the upper portion of the urethra just below the bladder has a duct that connects to the urethra Function produce sperm (note: this is done exterior to abdominal cavity to allow lower temperature for better sperm production) site of spermatid production (spermatogenesis) secrete androgens (ex. testosterone) site of maturation of the spermatids into sperm receives spermatids from the seminiferous tubules stores sperm stores sperm receives sperm from the epididymis and carries it to the ejaculatory duct adds a basic fluid to semen through a duct to neutralize any acidic urine left in the urethra the prostate fluid helps somewhat to nourish sperm Cowper's glands (bulbourethral glands) pea-sized glands that lie posterior to the prostate on either side of the urethra. seminal vesicles penis urethra two glands at base of the bladder, each with a duct that joins with the vas deferens to make the ejaculatory duct long shaft with an enlarged tip (glans penis) covered by the foreskin (prepuce) layer of connective tissue under the skin rich blood supply to spongy erectile tissue smooth muscle control of blood flow duct from the bladder through the penis to the urethral opening. The urethra is joined by a duct from the prostate, the ejaculatory duct, and a duct from Cowper’s glands adds mucus-like fluid to the urethra during sexual intercourse to assist in the lubrication of coitus also neutralizes any acidic urine left in the urethra adds nutrients and fluid to semen to nourish sperm organ of sexual intercourse erectile tissue fills with blood when smooth muscle (under autonomic control) prevents blood from draining from the penis. This allows conduction of sperm to vagina through urethra peristaltic contractions move sperm and seminal fluid through urethra conducts sperm and seminal fluid from the ejaculatory duct conducts seminal fluid from the prostate conducts seminal fluid from Cowper’s glands All go through the penis to the urethral opening Reproductive System PLO P2 (414) The path of sperm (= ) Seminal Fluid Additions (= ) (sperm does not pass through these accessory glands) urethral opening Reproductive System PLO P3 (414) The seminal fluid makes up most of the 3.5 mL released during ejaculation. There can be up to 400 million sperm in a single ejaculation. Functions of Seminal Fluid seminal vesicle secretions provide a nutrient rich environment (fructose) for sperm. Sperm have high energy demands because of their motility. prostate gland and Cowper’s glands secretions’ create a basic environment (pH = 7.5) to neutralize any acidic urine left in the urethra. Sperm prefer a basic environment. Cowper’s glands secretions’ and seminal vesicle secretions’ help lubricate during coitus with the mucus-like fluids. Seminal fluid contains prostaglandins which cause the uterus to contract (some believe to help move sperm towards the egg, others believe it is to move sperm away from the egg so only strongest sperm will reach the egg) Reproductive System PLO P4 (416-417) Sperm Structure Part tail Structure protein fibres – resembles the structure of a typical flagellum midpiece an extension of the cytoplasm which has numerous mitochondria head the main part of the cytoplasm of the cell acrosome a cap covering the head of the sperm Function rhythmic contraction of the protein filaments in the tail causes a spirallike movement that propels the sperm past the surrounding fluids. The mitochondria respire sugars in the seminal fluid to generate ATP in order to provide the energy for movement of the tail. contains the nucleus with it’s 23 chromosomes including one X or Y chromosome The acrosome contains lytic enzymes which are released when the sperm reaches an ovum. These enzymes digest the outer membrane of the egg, allowing penetration of the sperm. Reproductive System PLO P5 (417) PLO P6 (417) Male sex hormones The interstitial cells of the testes produce androgens (male sex hormones) including testosterone and androsterone. Testosterone is the main male sex hormone. Hormone control The interstitial cells of the testes are ultimately under the control of the hypothalamus. Recall: The hypothalamus is linked to the anterior pituitary gland by a portal system (two capillary beds) where the hypothalamus releases a releasing hormone or a inhibitory hormone for each of several hormones released from the anterior pituitary. In this case, the hypothalamus releases gonadotropin-releasing hormone (GnRH) that stimulates the anterior pituitary to secrete the gonadotropic hormones: follicle-stimulating hormone (FSH) and luteinizing hormone (LH) In males: - FSH promotes the production of sperm in the seminiferous tubules and a hormone called inhibin. - LH (aka: interstitial cell-stimulating hormone (ICSH)) controls the production of testosterone by the interstitial cells. - These hormones work on a negative feedback system to regulate the production of sperm and testosterone (ie. testosterone and inhibin inhibit the release of LH and FSH from the anterior pituitary AND release of GnRH from the hypothalamus) Functions of testosterone: responsible for the development of the male sex organs brings about and maintains the secondary sexual characteristics that appear during puberty. - height (growth spurt) - broad shoulders - longer legs - deeper voices (longer vocal cords) - hair on the face, chest, back male pattern baldness greater muscular development building up and maintaining bone mass in men NOT part of a PLO - Other functions: Androgens influence fat distribution and deposition Cognition – testosterone and other androgens are important in maintaining the wellbeing of the mind Men with high testosterone levels are likely to be depressed or anxious provides cardiovascular protection (lowers cholesterol) improves energy level and mental alertness enhances sex drive and sexual performance increases red blood cell mass promotes adequate sperm count causes growth of penis during puberty - Low testosterone results in: decrease in sex drive fatigue and at times anxiety and depression. decreases in bone mass and may lead to osteoporosis which places these men at high risk for fracture of bones, especially of the hip and spine. enlargement of the breast area, known as gynecomastia. - Causes of low testosterone in adults includes: Aging (testosterone level starts decreasing after the age of 40-45) Pituitary tumor Pituitary surgery / Radiation to the head area Excessive alcohol drinking Certain drugs, such as chemotherapy agents Mumps Testicular trauma Testicular surgery ( rarely even after vasectomy) Varicocele (a testicular condition) Undescended or retractile testes Chronic illnesses - Reproductive System PLO P7 (418, 419) Female Reproductive System Anatomy Organ Structure ovaries (female gonads) follicles corpus luteum oviducts (fallopian tubes) small oval shaped structure on each side of upper pelvic cavity connective tissue layer that surrounds many follicles and corpus luteum This is a structure within the ovary. There are 3 stages a follicle can be in primary: immature diploid sex cells stuck in prophaseI surrounded with a simple squamous epithelium secondary: immature diploid sex cell surrounded by stratified cuboidal epithelium and some follicular fluid vesicular: built like a secondary follicle except the cavities of follicular fluid have begun to balloon out and the diploid sex cell divides in two and stops in metaphase II (one big cell: secondary oocyte, one small cell: polar body) Temporary gland-like structure made of the epithelial cells of a follicle after it has released it’s oocyte from the ovary. muscular tubes lined with cilia that receive egg from the ovary (not attached to ovary – egg must cross gap) oviducts have fimbriae that help sweep egg into the oviduct after ovulation Function produces eggs produces sex hormones estrogen and progesterone site of egg maturation within the ovary produce estrogen and some progesterone produces the hormones estrogen and progesterone move egg towards the uterus location of fertilization uterus cervix vagina thick-walled muscular organ about the size of a pear (upside down) joined to the oviducts at it’s anterior end At it’s posterior end (the cervix) it is joined to the vagina lining is the endometrium which forms part of the placenta during pregnancy endometrium has varying thickness at different stages of the uterine cycle Most posterior portion of the uterus opening of uterus to the vagina dips down into the vagina makes a 90 degree angle between the uterus and the vagina single, elastic, muscular tube that extends from the uterus to the exterior of the body. clitoris found in the cleft between the labia minora an erectile structure comparable to the penis that becomes engorged with blood during sexual arousal rich in nerve endings houses developing foetus site of implantation lining becomes part of the placenta which exchanges nutrients/gases with foetus constricts to close the uterus during foetal development dilates for birth is beginning of birth canal (vagina) receptacle for sperm during intercourse part of birth canal after feotal development is complete centre of sexual sensation in females Reproductive System PLO P9 (421-423) PLO P10 (421-424) PLO P12 (424, 449, 450) The Ovarian and Uterine cycles The ovarian cycle drives the uterine cycle. The Ovarian Cycle A female is born with as many as 2 million follicles. There are only 300 000 to 400 000 left at puberty. Only 400 will ever mature and be released from the ovary (ovulation). The primary follicles all have a sex precursor cell that is halted in metaphase I of meiosis. The follicular phase The FSH from the anterior pituitary circulates in the blood and promotes the development of a follicle. The follicle secretes estrogen and some progesterone during it’s development. The circulating estrogen feeds back to the anterior pituitary and slows the release of FSH (follicular phase will end) At the same time, the circulating estrogen feeds back to the hypothalamus where it causes further release of GnRH in a spike at the end of follicular development. Net result is that LH is still secreted from the anterior pituitary; FSH is too but to a lesser degree (neg. feedback from estrogen) Ovulation The high LH in the blood causes the fully developed follicle (vesicular follicle) to release it’s egg on the 14th day of the 28 day cycle. The follicle matures to a secondary follicle and then to a vesicular follicle when it ruptures and releases the egg within to the outside of the ovary. This process is called ovulation. The follicle that remains on the inside of the ovary is then referred to as the corpeus luteum. Luteal phase LH continues to circulate and promotes development of the corpus luteum that maintains estrogen and progesterone secretions. Progesterone causes the endometrium (lining of uterus) to build up As progesterone builds up, it has negative feedback over the anterior pituitary secretion of LH. The result is the corpus luteum degenerates and the endometrium can no longer build up and sloughs off (menstruation) The Uterine Cycle Driven by the events of the ovarian cycle. A 28 day cycle that breaks down as follows: Days 1-5 Corpus luteum has just degenerated, so there’s low levels of estrogen & progesterone. The endometrium disintegrates (blood vessels rupture) Menstruation occurs; day 1 is particularly heavy flow of blood and tissues out of vagina. Days 6-13 (proliferative phase) FSH builds in blood stream causing follicular development Developing follicle causes increase in blood estrogen concentration Endometrium thickens Day 14 Ovulation occurs Days 15-28 (secretory phase) Increased production of progesterone by corpus luteum causes endometrium to further increase thickness of endometrium Development and maturation of uterine glands (secrete thick mucuslike fluid) Endmetrium awaits implantation. If implantation does not occur, then the corpus luteum degenerates and endometrium begins breaking down. If implantation occurs, then the forming placenta produces human chorionic gonadotropin (HCG) which maintains the corpus luteum until the placenta can make it’s own estrogen and progesterone which will prevent the endometrium from disintegrating. (ie. No menstruation during pregnancy) Reproductive System PLO P8 (423, 424) PLO P11 (208, 394, 455, 458) The main female sex hormone is estrogen. The functions of estrogen Estrogen promotes the release of GnRH from the hypothalamus during follicular phase of ovarian cycle Estrogen inhibits release of FSH from the anterior pituitary during follicular phase of the ovarian cycle. Estrogen is responsible for development of the secondary sexual characteristics in females including: fat distribution body hair. breast development widening and deepening of the pelvic girdle. The functions of Oxytocin Oxytocin is an example of a hormone that has a positive feedback mechanism During birth, sensory receptors in the cervix detect the baby’s head pushing against it. When these nerve impulses reach the brain, the brain causes the posterior pituitary to release oxytocin. Oxytocin causes the uterus to contract pushing further against the cervix and stimulating more receptors and thereby causing more oxytocin release. Oxytocin also causes milk let-down during nursing. The more a baby suckles, the more oxytocin is released (neural pathway) from the posterior pituitary Menopause The cessation of ovulation due to the lack of responsiveness of the ovaries to LH and FSH If menstruation is still occurring then it is still possible to conceive. Usually, the uterine cycle becomes irregular and a woman is not said to be menopausal until she has not menstruated for a full year. Symptoms of menopause are: – hot flashes – dizziness – headaches – insomnia – sleepiness – depression