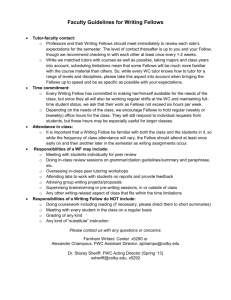
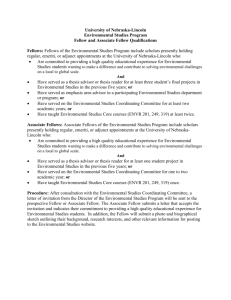
Educational Goals and Objectives
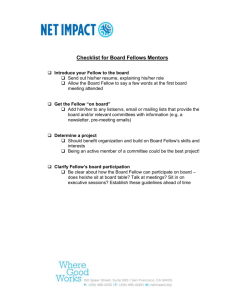
advertisement

University of Minnesota Division of Plastic & Reconstructive Surgery 2007-2008 FELLOWSHIP INFORMATION: PROGRAM MANUAL Policies, Guidelines, & Reference Listings Department of Surgery Division of Plastic & Reconstructive Surgery Introduction/Explanation of Manual The information contained in this Program Manual (formerly known as the Part B Manual) pertains to fellows in the Division of Plastic and Reconstructive Surgery. For information that applies to all fellows at the University of Minnesota, please review the Institution Policy Manual (formerly known as the Part A Manual), available online at http://www.med.umn.edu/gme/residents/parta.html. Information in the Institution Policy Manual takes precedence over that in the Program Manual. Department of Surgery Mission Statement The academic charge of the Department of Surgery at the University of Minnesota is to provide a superb environment to facilitate the training of individuals at all levels-medical student, resident, and fellow-in the discipline of clinical surgery and surgical sciences. Program Mission Statement The academic charge of the Department of Surgery at the University of Minnesota is to provide a superb environment to facilitate the training of individuals at all levels-medical student, resident, and fellow-in the discipline of clinical surgery and surgical sciences. Page 2 of 43 Table of Contents Introduction/Explanation of Manual ................................................................................................................................... 2 Department of Surgery Mission Statement ...................................................................................................................... 2 Program Mission Statement ................................................................................................................................................. 2 SECTION I: STUDENT SERVICES .......................................................................................... 6 Universal University Pagers ................................................................................................................................................. 7 E-Mail and Internet Access................................................................................................................................................... 7 HIPPA Training ........................................................................................................................................................................ 8 UMMC Photo ID Badge ........................................................................................................................................................ 10 Doctor Number and UMMC Computer Access .............................................................................................................. 10 Regions Hospital Introduction Information ................................................................................................................... 10 SECTION II: BENEFITS .......................................................................................................... 11 Stipends .................................................................................................................................................................................. 12 Vacation Policy, Non-Regions Rotations ....................................................................................................................... 12 Vacation Policy, Regions Rotations................................................................................................................................. 12 Sick Leave Policy .................................................................................................................................................................. 13 Health and Dental Insurance Coverage........................................................................................................................... 13 Professional and Academic Leave ................................................................................................................................... 13 Parental Leave: Family Medical Leave Policy/Childbirth or Adoption .................................................................... 13 Policy on Effect of Leave for Satisfying Completion of Program ............................................................................ 14 Long Term Disability Insurance ........................................................................................................................................ 14 Short Term Disability Insurance ....................................................................................................................................... 14 Professional Liability Insurance ....................................................................................................................................... 14 Life Insurance ........................................................................................................................................................................ 14 Meal Tickets ........................................................................................................................................................................... 14 Laundry Service .................................................................................................................................................................... 14 Parking..................................................................................................................................................................................... 15 Travel Policy........................................................................................................................................................................... 15 Page 3 of 43 SECTION III: DISCIPLINARY AND GRIEVANCE PROCEDURES ........................................ 17 Fellow Grievance Policy ...................................................................................................................................................... 18 SECTION IV: GENERAL POLICIES AND PROCEDURES .................................................... 19 Program Curriculum............................................................................................................................................................. 20 Division Conferences .......................................................................................................................................................... 20 Program Goals and Objectives ......................................................................................................................................... 23 YEAR 1A .............................................................................................................................................................................. 23 YEAR 1B .............................................................................................................................................................................. 24 YEAR 2 ................................................................................................................................................................................. 26 Training / Graduation Requirements ............................................................................................................................... 28 Operative Records ................................................................................................................................................................ 28 ACGME Competencies ........................................................................................................................................................ 28 Duty Hours .............................................................................................................................................................................. 29 Evaluation ............................................................................................................................................................................... 30 Mock Oral Examinations ..................................................................................................................................................... 32 On Call Schedules ................................................................................................................................................................ 33 Overnight Call Rooms/Call Rooms .................................................................................................................................. 34 Resident Exercise Room ..................................................................................................................................................... 34 Resident Lounges ................................................................................................................................................................. 35 Support Services .................................................................................................................................................................. 35 Laboratory/Pathology/Radiology Services .................................................................................................................... 35 Medical Records.................................................................................................................................................................... 35 Security/Safety ...................................................................................................................................................................... 35 Moonlighting Policy ............................................................................................................................................................. 36 Supervision Policy ................................................................................................................................................................ 36 Graded Responsibility ......................................................................................................................................................... 37 Monitoring of Resident Well-Being .................................................................................................................................. 38 Photocopying ......................................................................................................................................................................... 38 Office Support Services ...................................................................................................................................................... 39 Guidelines of Professional Dress ..................................................................................................................................... 39 Page 4 of 43 SECTION V: ADMINISTRATION ............................................................................................ 40 Main Hospital Contact Information .................................................................................................................................. 41 S.O.U.P. Administrative Phone List & 11th Floor PWB Offices ................................................................................ 42 Telephone/Pager Hints And Instructions ....................................................................................................................... 43 Paging ................................................................................................................................................................................... 43 Page 5 of 43 SECTION I: Student Services (Please refer to Institution Policy Manual for Medical School Policy on the following: Child Care, Computer Discount, Credit Union, Legal Services, Library Services, Medical School Campus Map, Residency Assistance Program, Tuition Reciprocity, U Card, University Recreation Sports Center, University Tickets, and Use of Phone Numbers.) Page 6 of 43 Universal University Pagers Plastic surgery fellows receive alpha pagers at the beginning of the year and are provided to you by the residency program coordinator. The number you are assigned remains the same for the duration of your training. For malfunctioning beepers, please contact Lana in the Communications Office (952-924-1452). If your beeper is not turned in at the end of your training you will be assessed a fine for $170.00 to cover the costs of a new one. New batteries can be obtained from the Department of Surgery Front Desk, 11th floor PhillipsWangensteen Building. Paging Instructions USER: University Campus: U of M phone with a 624/625/626 Prefix Dial Access Code 19393 Fairview phone with a 273 Prefix Dial Access Code 893 Riverside Campus: Fairview phone with a 672 or 273 Prefix Dial Access Code 893 Off Campus: Dial Access Code 899 SYSTEM: Please enter the four digit I.D. to page USER: Enter the FOUR digit I.D. number SYSTEM: displayed. States the status and if the person is available, directs you to enter the number you wish to be USER: Enter your SEVEN digit call back phone number, then hang up. Alpha Pagers All plastic surgery staff and resident pagers from the University are alpha-numeric. The URL for alpha, or text, messaging is: http://www.americanmessaging.net/index.asp Pages sent numerically should be considered urgent and a call-back is expected. Alpha text does not usually require a response, unless indicated (e.g., Call me). Abbreviated text is used liberally. If in doubt, call the sender. E-Mail and Internet Access To set up E-mail account: Check to make sure you are registered as a student (all surgical fellows are registered students at the University of Minnesota). You can do this by going to the UMN search page at http://search.umn.edu/. Under search for people, type in your name and click on search. If you are not registered, you won’t be in the system. If you are not registered, please contact Teri Wolner, at (612) 625-3926, to make sure all of your paperwork is complete. Call the E-Mail help line at 612-626-4276, or go to the Computer Information Services Office in Room 152 Shepherd Laboratories, 100 Union Street, to set up your account and password. To access your E-mail account: Any computer with Internet access can be used to access your University of Minnesota E-mail account. Page 7 of 43 Go to http://www.mail.umn.edu/ (if you forget this address, there is a link to this page on the Department of Surgery home page at http://www.surg.umn.edu ). Click on "GopherMail" or "WebMail 3.0" Enter your Internet ID and Password To set up Internet access from home: The University of Minnesota provides an Internet account to all faculty, staff, and enrolled students. The University also provides 50 hours of free modem pool access per month. Additional blocks of 30 hours are available at a rate of $4 per 30 hours. The Internet kit contains software and instructions for connecting your computer to the Internet, as well as many popular Internet programs and utilities. More information about the Internet kits can be found at http://www1.umn.edu/adcs/software/internetkit/. E-mail merge instructions: If you use another e-mail (e.g., Hotmail, Yahoo) other than your university e-mail, please make sure that you have your university e-mail forwarded to your other account. E-mail notification is the primary communication tool used by the division, department, the Dean’s Office, AHC, and the University to notify faculty, staff, and students for all required information and deadlines. The steps to do this are: 1. 2. 3. 4. 5. Go to http://www.umn.edu/dirtools Enter your Internet ID and Password Click on “Set eIn the “send e-mail to” field, click "other" and type in your alternate eSubmit Important Web Pages: The Department of Surgery’s web page is: http://www.surg.umn.edu/ The Division of Plastic & Reconstructive Surgery’s web page is: http://www.surg.umn.edu/surgery/General/Plastic.html The UMN Graduate Medical Education office’s web page is: http://www.med.umn.edu/gme/ The Medical School’s web page is: http://www.meded.umn.edu/ Campus Mail Your mail is delivered to the general Plastic & Reconstructive Surgery box, and will be sorted by the residency coordinator. The coordinator will notify you when you have mail, and have it available for pick up in Mayo, C261. Your campus mail address is; 420 Delaware Street SE, MMC 195, Minneapolis, MN 55455. Please have any magazines or journals, etc. sent to your home address, in order to insure you receive your materials in a timely manner. HIPPA Training All Plastic Surgery fellows must complete the University of Minnesota’s HIPAA training. You will be assigned your sections to complete through your AHC Portal. Please contact Sara Gort, at (612) 624-7149, for any questions. University Privacy & Data Security Training: Compliance Requirements for Individuals There are security courses that are required of all individuals, and privacy and security training courses that are appropriate only for some individuals. The particular training that each individual must complete depends in large part on job duties and responsibilities. The privacy and security training courses offered at the University of Minnesota are listed in the table on the next page. HIPAA Privacy training requirements: All employees, student workers, and health science students and volunteers in the AHC (with the exception of those in College of Veterinary Medicine programs) and other University health care Page 8 of 43 components are required to complete the primary Introduction to HIPAA Privacy and Security videotape course. All employees, students, and volunteers with research-related duties are required to complete the Privacy and Confidentiality in Research core course. All employees, students, and volunteers with clinical responsibilities are required to complete the Privacy and Confidentiality in Clinical Settings core course. Security training requirements: All employees, students, and volunteers are required to complete the three primary security courses: Data Security in Your Job, Securing Your Computer Workstation, and Using University Data. All employees, students, and volunteers in the AHC (with the exception of those in College of Veterinary Medicine programs) are required to complete the Managing Health Data Securely topical course. Course Name Course Length (approximate) Privacy Training Introduction to HIPAA Privacy and Security videotape (primary) Privacy and Confidentiality in Research (core) Privacy and Confidentiality in Clinical Settings (core) 7 minutes 35 minutes 55 minutes Security Training Data Security in Your Job1 (primary) Securing Your Computer Workstation (primary) Using University Data2,3 (primary) Managing Financial Data Securely (topical) Managing Personnel Data Securely (topical) Managing Health Data Securely (topical) Managing Student Data Securely (topical) Data Security Information for Faculty, Managers, and Supervisors (topical) 20 minutes 20 minutes 20 minutes 20 minutes 20 minutes 20 minutes 20 minutes 20 minutes Privacy and Security Training Courses Offered by the University of Minnesota 1Only the first security course, Data Security in Your Job, is initially assigned by either the Tracking system automatically or by a privacy coordinator. Two weeks later, the second security course, Securing Your Computer Workstation, is automatically assigned (with the person that training was assigned to receiving an e-mail notification about training), whether or not the first course has been completed. Two weeks after the second security primary course is assigned, the third course, Using University Data, is assigned (whether or not the first or second course has been completed), with an e-mail sent to the person assigned training. 2The third security course, Using University Data, contains an assessment module at the end. The assessment is a required component of security training. If a person who finishes the third security course does not complete the assessment, he or she will still receive a completion e-mail notification. However, the course will be treated as incomplete until the assessment is completed. A person who completes the course but not the assessment receives one reminder e-mail with a link to the assessment. 3The assessment that follows the Using University Data course is listed as a separate course in the Tracking system that privacy coordinators use. It is also listed in the myU portal as a separate course to highlight its importance as a tool for determining and delivering additional curricula. About security training topical courses Depending on roles/duties and type of data used in his or her position, an individual may need to take additional topical courses beyond the required primary security courses. An assessment that an individual completes at the end of the third primary security course determines the additional topical courses that he or she needs. Based on the responses to the assessment, the Tracking system automatically assigns the appropriate courses and sends an e-mail to the individual with information about how to take the necessary topical courses. Page 9 of 43 How to Access the On-Line Courses All required training can be accessed in the University-wide “myU” portal at www.myu.umn.edu Once authenticated (“signed in”), Employees will need to go to their “my WORK LIFE” tab and Students will need to go to their “my ACADEMICS & CAREER” tab. Additional information Questions regarding training requirements, University policies, HIPAA, or privacy and security issues in general can be directed to the Privacy & Security Office at 612.624.7447 or at privacy@umn.edu. UMMC Photo ID Badge There are two locations to obtain a UMMC photo ID badge. The first one is in the Main Hospital, 2-112 Security Office. Hours are from noon to 5 PM on Thursdays and 7 AM to noon Fridays. For more information, call (612) 273-4948. Otherwise, you may go to the Main Security Office, M141 East Building, Riverside Campus. For more information call, (612) 273-4544. They are open 24 hours a day, 7 days a week. To get to the Riverside campus from the University campus, board the shuttle to the Riverside campus at the entrance of the Hospital—you may obtain the schedule from the Hospital Information Desk. The shuttle drops you off at the East Building. Go in the entrance and follow the signs to the Main Security Office. The office will have a list of Department of Surgery fellows. You will be required to fill out a form giving your name, address, Social Security Number, etc. Doctor Number and UMMC Computer Access Teri Wolner, in the Surgical Education Office, will provide you the forms to complete and return in order to be assigned your doctor number and computer access number. You can reach Teri at, (612) 626-2590. Regions Hospital Introduction Information Prior to beginning the Regions plastic surgery rotation, please contact the Regions Plastic Surgery Office at (651) 254-0883. They will instruct you where and at what time to report to the hospital and meet with the Plastics staff. (Usually 6:30 a.m.) On first day of rotation, register with Willie Braziel (3rd Floor, North Bldg). Where applicable, he will assist you with the following: Parking ID Badge Computer Codes (Epic Web, Rampis) Dictation Codes Access to secured areas (O.R., E.R.) Call Room Access If you have any problems with computer or door access, codes, parking, etc. or any questions about Regions Hospital or its policies, please contact Willie Braziel at (651) 254-1530. Page 10 of 43 SECTION II: BENEFITS (Please refer to Institution Policy Manual for Medical School Policy on the following: Boynton Health Services, Dental Insurance, Health Insurance, Life Insurance, Long-Term Disability Insurance, Short-Term Disability Insurance, Insurance Coverage Changes, Loan Deferment, Optional Retirement Contributions, Pre-Tax Reimbursement Program, Overview of Pre-Tax Accounts, Professional Liability Insurance, Resident Leave Policy, Stipends, Workers’ Compensation Benefits.) Page 11 of 43 Stipends Fellow stipends are determined each year. Your annual stipend amount will be sent to you each year with your Graduate Medical Education Program Residency Agreement. Fellows must be hired at the appropriate stipend level paid by their PGY year level by their department/program. Years away in non-accredited program (clinical service, research, government service etc.) cannot be counted when determining the appropriate stipend level. The 2007/2008 base stipends were approved by the UM GMEC at their November 28, 2006 meeting. Please note that we will continue to withhold FICA as appropriate. Level G6 G7 G8 Stipend $52,204 $53,873 $55,597 The 2007/2008 rates are posted on the GME web-site at: http://www.med.umn.edu/gme/directors/finance.html, along with an update of the stipend history spreadsheet. Fellows will receive a paycheck every other week. Payroll dates are stated in the Institution Policy Manual. The Department of Surgery receives the paychecks from Payroll on every other Wednesday and mails them to the fellows’ home. As paychecks have the potential of being lost or delayed in the mail, fellows are encouraged to use the direct deposit system. Paychecks are credited to the bank accounts of those using the direct deposit system on the morning the paychecks are delivered to the Department Office. If you have any questions, please contact Kirk Skogen, payroll personnel, at (612) 625-3954 or k-skog@umn.edu. Vacation Policy, Non-Regions Rotations A maximum of 7 days may be taken during each four-month rotation and the fellows are encouraged to utilize all vacation days available during that time. Vacation requests must be submitted at least 30 days in advance on the division form. The site director will be responsible for its distribution to the rest of the faculty. Fellows are responsible for arranging call coverage and must indicate the coverage on the vacation request form. Request forms must be approved by the site director who will notify the other sites. It is undesirable that two fellows should be on vacation at the same time. Holiday schedules are as below, but residents may negotiate between themselves: First year resident has Thanksgiving weekend free; works on Christmas. Third year resident has Christmas free; works on Thanksgiving. Vacation Policy, Regions Rotations Fellows may take 21 days of vacation each year (July to June). Vacation not taken during the year may not be applied toward vacation in subsequent years. Vacation must be taken up to a maximum of 7 days during each 4-month period as follows: BLOCK 1: 1 week during July – October BLOCK 2: 1 week during November – February BLOCK 3: 1 week during March – June Page 12 of 43 Vacation requests must be submitted in writing to the Residency Program Coordinator during the block prior to the block you are requesting vacation time. Once vacations are approved they may not be changed and vacation days not taken during a 4-month period may not be carried forward. Vacation may not be taken during the following time periods: December 24-January 1 January 16–25 June 13–30 The site director will arrange for every fellow to have three days off during the period of December 24 th through January 1st, allowing all fellows time off during these dates. Estimated dates for maternity or paternity leave should be submitted in writing to the Program Coordinator three months in advance. Greater than 7 days of vacation may be taken only under special circumstances (e.g., marriage, overseas travel, etc.) with a maximum of 11 days, and must be split at the end of one rotation and the beginning of another. Sick Leave Policy In the event of illness, the affected fellow is personally responsible for notifying the faculty member of the affected clinic(s)/service(s) or Program Director’s office as soon as the fellow knows that the illness will cause an absence from clinical responsibilities. Sick leave will be approved only for legitimate illness. A physician’s note may be requested to support the fellow’s request for sick leave. If the above policy is not followed, the absence will be counted as vacation time. It is the responsibility of the fellow and the program director to ensure that Board eligibility requirements are met within the original residency period or alternative arrangements are made. Health and Dental Insurance Coverage See the Institution Policy Manual. Please contact Teri Wolner, at (612) 625-3926, for any questions. Professional and Academic Leave You must submit in writing to the Residency Program Coordinator, a vacation request form for any time off of service for fellowship interviews, meetings, teaching ATLS, etc., although you will not be charged vacation time. Time away from the hospital for academic leave, continuing medical education, and conferences is available in addition to the regular vacation time. This is under the jurisdiction of the residency content of their fellowship. If the fellow is assigned to an off-service rotation, the residency program needs to make mutually agreeable arrangements with any department that may be affected. If requested, the fellow must provide of a replacement, either with another fellow or a qualified substitute. See the Institution Policy Manual for the Institutional Fellow/Resident Leave Policy. Parental Leave: Family Medical Leave Policy/Childbirth or Adoption A leave of absence for serious illness of the fellow; serious health condition of a spouse, parent, or child; or birth or adoption of a child shall be granted through formal request to the program director. The length of the leave will be determined by the program director based upon an individual’s particular circumstances and the need of the department, not to exceed 12 weeks in any 12-month period. The fellow shall be granted, upon request, up to six weeks paid maternity leave for birth or two weeks paid leave for adoption. After using paid maternity leave and all unused vacation, any additional leave will be without pay. Two weeks paid paternity leave will be granted upon request to the program director. The fellow should exercise consideration in informing the program director as early as possible to allow scheduling of curriculum plans to accommodate the leave. It is the responsibility of the fellow and the program Page 13 of 43 director to ensure that Board eligibility requirements are met within the original fellowship period or that alternative arrangements are made. Policy on Effect of Leave for Satisfying Completion of Program The Board considers a residency in plastic surgery to be a full-time endeavor and looks with disfavor upon any other arrangement. The minimum acceptable training year is 48 weeks. Should absence exceed four weeks per annum for any reason, the circumstances and possible make-up time of this irregular training arrangement must be approved by the program director and the additional months required in the program must be approved by the Residency Review Committee (RRC-PS) for Plastic Surgery and documentation of this approval must be provided to the Board by the program director. No credit but no penalty is given for military, maternity/paternity or other leaves during training. Residents or candidates in the examination process called to active military duty do not need to submit a reapplication if five years expire during the active duty period. Long Term Disability Insurance See the Institution Policy Manual. Please contact Teri Wolner, at (612) 625-3926, for any questions. Short Term Disability Insurance Short-Term disability insurance is offered as an optional coverage. The cost is based on the amount of coverage elected. Coverage may be applied to in increments of $100 from a minimum of $300 to a maximum of $5000, but not to exceed 2/3 of the fellow’s monthly gross salary. Benefits are effective the first day of a disability due to an accident or the eighth day of disability due to sickness or pregnancy and, if certified, can continue for up to 26 weeks. Professional Liability Insurance See the Institution Policy Manual. Please contact Teri Wolner, at (612) 625-3926, for any questions. Life Insurance See the Institution Policy Manual. Please contact Teri Wolner, at (612) 625-3926, for any questions. Meal Tickets Meal Tickets will be provided for you on all clinical rotations as fellows on duty must have access to adequate and appropriate food services 24 hours a day at all institutions. For UMMC, the Residency Coordinator will provide on call fellows with preprogrammed meal cards. When the card has been used up, leave the card with the cafeteria staff. If the meal card is lost or stolen, contact the Residency Coordinator. At the VA, the kitchen has a list of who is on call, and at Regions, Willie Braziel, in the Surgical Education Office will provide you with preprogrammed meal cards. There is no food service available for any other institutions (e.g., North Memorial, West Health, Centennial Lakes). Laundry Service The Division of Plastic and Reconstructive Surgery will provide each incoming fellow with two long white lab coats. You will receive an order form to purchase the coats through the University of Minnesota Health Sciences Bookstore. The division provides laundry service for the lab coats through AmeriPride laundry. All coats need to be tagged in order for this service to be had so please notify the residency coordinator once the coats are ready to be cleaned. Page 14 of 43 Parking The Division of Plastic and Reconstructive Surgery provides a parking contract for Ramp C on Oak Street and Delaware Street SE for fellows when on service at the University. Parking at Regions is available through Willie Braziel, in the Surgical Education Office; at the VA no parking card is required, the surface lot is open to all. At all other sites, the on-site Education Office will provide you with the details of how and where to park. Travel Policy Annual Travel The division of Plastic and Reconstructive Surgery at the University of Minnesota enthusiastically supports the fellows’ educational experience by committing funds for each fellow to attend one academic meeting per year. Travel dollars do not carry over. For years one or two of the plastic surgery fellowship, fellows are free to choose any academic meeting; provided they attend either a board review course of their choice or the Core Curriculum course in Plastic Surgery. Fellows are strongly encouraged to attend the Core Curriculum course at least once during the fellowship. The flexibility allows fellows who wish to achieve board certification in their primary residency to attend a board review course. It also allows fellows who plan to take an additional fellowship to attend a meeting that would allow them to make the necessary contacts for their intended fellowship. In year three, the fellow is strongly encouraged to attend the senior residents course as a participant in the program. Travel to Present at Meetings Fellows in the Plastic and Reconstructive Surgery fellowship program at the University of Minnesota are provided resources and strongly encouraged to perform clinical and/or basic science research during the course of their three years of training. The division supports the fellow research experience by committing funds to each fellow to attend the major national meeting to which they have abstracts accepted. Acceptance of an abstract for presentation in poster or oral format at a meeting will entail travel expenses that must be reimbursed by the senior investigator on the abstract or by a sponsoring organization. Travel outside of the 48 continental states in the U.S. will be approved on an individual basis. Overseas Travel Third world trips are determined on an individual case-by-case basis and will not negatively impact on the amount of meeting time available per year as described above. Pre-travel Instructions Prior to any travel a Travel Authorization form must be filled out, signed by the division director, and if applicable, the research mentor. Forms are to be completed by the fellow and returned to the Department of Surgery Budget Office. Forms are available in the Department of Surgery office (11-100 PWB). Estimated expenses should be reflective of actual expenses that will be incurred. If travel is for abstract presentation, please enclose a copy of the letter indicating acceptance of your abstract and a copy of the abstract itself. If a concurrent submission of a manuscript is required, a copy of the cover letter to the editor of the journal to which the manuscript has been submitted and a copy of the manuscript itself should also be enclosed. For all fellow travel, support will be reimbursed according to the Travel Reimbursement Schedule in compliance with the Department of Surgery guidelines, as noted below: Page 15 of 43 Travel Reimbursement Schedule (minimum levels) Per diem (hotel plus meals) $120.00 per day and subject to actual expenses and allowable limits as per University of Minnesota guidelines (see http://travel.umn.edu/polandpro.php); We suggest that you share a room with one of your colleagues whenever possible. Airfare (must be lowest rate possible [14-21 day advance] and include a Saturday night stay if the meeting ends on Saturday or begins on Sunday). The reimbursement for a Saturday night stay will always be allowable, if the difference between airline ticket cost for non-Saturday and a Saturday stay exceeds $130.00. Full reimbursement for the hotel room (not to exceed $130.00) will occur for Saturday night. Reasonable ground transportation at city of destination, i.e. taxi to and from airport to hotel or rental car if cost benefit shows savings for staying at another hotel for a reduced rate. The maximum reimbursement per trip will not exceed $1,000.00, unless there is a concurrent submission of a manuscript at the time of the meeting. This will increase the maximal reimbursement up to $1,150.00. Applying for Travel Expense Reimbursement Obtain proper approval for reimbursing the traveler. The Travel Voucher requires two signatures, the traveler and the Program Director. Submit the Travel Voucher for data entry within 15 days from the return date of the trip. If an advance was obtained and the required voucher is not submitted within 30 days of the anticipated return date, collection of the advance through payroll deduction will commence. Original receipts are required for all expenses of $25 or more, except for meals. Receipts should be detailed vendor receipts rather than general charge card transaction slips. Receipts for meals are not required (even if meal is over $25) unless your department requires them for their own internal audit procedures. Foreign expenses must be submitted in U.S. dollars using the exchange rate in effect during the dates of travel or the exchange rate used by the University Corporate Charge Card at time of billing. If conversions are necessary, please indicate what exchange rate was used. For assistance in itemizing foreign expenses, call Disbursement Services at 612-624-7819. Page 16 of 43 SECTION III: Disciplinary and Grievance Procedures (Please refer to Institution Policy Manual for Medical School Policy on the following: Discipline/Dismissal of Residents/Fellows, Regents’ Student Academic Grievance Policy, University Senate Policy on Sexual Harassment, Resident Procedure for Reporting Sexual Harassment and Discrimination, and Sexual Assault Victim’s Rights Policy.) Page 17 of 43 Fellow Grievance Policy The Division of Plastic and Reconstructive Surgery encourages fellows at any time to communicate directly with any of the staff or faculty members regarding issues, problems, concerns or stresses that they may be experiencing. In particular, if there are logistical problems in their current rotations, conflicts with staff, or issues regarding fellow evaluations, the site director for that rotation should be contacted to discuss possible solutions. The Program Director, Dr. Bruce Cunningham, will address general concerns affecting more than one rotation. Fellows may log grievances either at their quarterly rotation review or they may contact the residency coordinator in order to obtain a grievance form, to be completed and returned the University offices for the Program Director’s review. When fellows are reluctant to voice minor concerns to the Program Director and staff, they may contact the program’s Ombudsman. The ombudsman position was created in an attempt to facilitate communication regarding fellows’ complaints and concerns at an informal level before they reach a point where official action is required by the Program Director. To address minor irritants before they become serious problems, fellows are encouraged to contact the ombudsman to air their concerns and solicit advice on an informal basis. The ombudsman is a recent graduate of the program, who is aware of many of the specific elements of the individual rotations, and serves as an accessible link between the supervising staff, and the fellows. The current ombudsman is Dr. Marie-Claire Buckley, contact information listed below; Marie-Claire Buckley, MD Phone: 612-625-5470 Fax: 612-624-4441 Pager: 612-899-5143 Cell: 612-201-2751 Email: buckl012@umn.edu Office: Mayo Building, room C260 Address: 420 Delaware Street SE, MMC 195 Minneapolis, MN 55455 Page 18 of 43 SECTION IV: General Policies and Procedures (Please refer to Institution Policy Manual for Medical School Policy on the following: Academic Health Center Policy on Student Background Checks, Classification Policy, Duty Hours, Dress Code Policy, On-Call Room Policy, Eligibility and Selection of Residents/Fellows, Evaluation of Residents/Fellows, RMS Instructions, GME Core Curriculum Seminars, Immunizations and Vaccinations, Impaired Resident/Fellow Policy, Impaired Resident/Fellow Procedure, Institutional and Program Requirements, International Medical Graduates, Jury Duty Policy, Licensure, Moonlighting Policy, New Training Program Policy, Observer Policy, Program Evaluation, Promotion of Residents/Fellows Policy, Policy Blood Borne Diseases, Restrictive Covenants, Supervision Policy, and Without Salary Appointments.) Page 19 of 43 Program Curriculum The goal of training is to assist the fellow in preparing a broad-based foundation for his/her future clinical and research endeavors. The philosophy of the Department is to train academically oriented surgeons by fostering and facilitating independent discovery and research. The faculty serves as a resource, a clinical and intellectual database to which the trainee can refer for assistance in answering questions stimulated by reading or clinical exposure. Fellows will acquire the necessary technical skills in several ways. In addition to didactic lectures and conferences, dissection on cadaver specimens will provide anatomical experience in flap anatomy and aesthetic surgery. The basic fundamentals of microsurgery are taught and practiced in the micro surgical research laboratory. As the fellow demonstrates a mastery of the basic skills in a laboratory setting, he or she will be provided progressively increasing operative responsibility in the clinical area. The rotation schedule is designed to allow maximum exposure to the requirements outlined by the RRC. Plastic and Reconstructive surgery experience will take place at three core facilities (University of Minnesota Medical Center, Fairview, Regions Hospital, North Memorial Medical Center) and a number of affiliated private hospitals. This experience will expose fellows to the full range of surgical care environments, from busy community hospitals to the clinical private practice setting. Division Conferences The following Plastic Surgery conferences are mandatory. Attendance of both fellows and faculty is taken and recorded, and is a criterion for advancement. Faculty are in attendance at each conference. Complete conference schedules are e-mailed to all residents and faculty members on a monthly basis. Also invited to participate are medical students and community surgeons. Fellows have the opportunity to evaluate the conferences in writing, and the input is used to improve the conferences bi-annually. Conferences are organized by the faculty and held to allow discussion of topics selected to broaden knowledge in the wide field of plastic surgery and to evaluate current information. Teaching conferences augment the didactic Core Curriculum Conference, and cover the scope of plastic surgery. Teaching conferences are designed to include basic science subjects, such as anatomy, physiology, pathology, embryology, radiation biology, genetics, microbiology, and pharmacology. Presentations are primarily given in Power Point or other electronic formats. Grand Rounds: This mandatory conference is conducted monthly, and may have one of two formats as determined by Dr. Bruce Cunningham. The most common format is conducted as a lecture by a member of the faculty, or a visiting plastic surgeon or other professional. Invited presenters have included University and regional experts from other specialties such as Dentistry, Orthopedics and Otolaryngology, Biomedical Ethics, Hospital General Council, UMMC Billing Office, ASPS President, and ASPS Executive Director. Invited speakers are used three to four months of the year for the conference. Staff, residents and guest speakers discuss the clinical or General Competency material as indicated. At other times one or more of the fellows present recent clinical cases illustrative of basic plastic surgery problems, topics or techniques. Fellows are required to emphasize the basic science aspects of the topic, including anatomy, physiology, pathology, embryology, epidemiology and pharmacology in their discussion as they relate to the topics. The conference may alternate between the Regions and University Campus from time to time. Mortality and Morbidity & Quality Assurance Conference: Each month there is a compulsory review of the morbidity and mortality experiences of the service that is conducted by the Program Director at the University and includes data from all rotations for the collecting period. Complications are pulled from each participating institution; cases with learning potential are selected by the Senior Fellow, and presented by the appropriate fellow on service using illustrative patient documentation. In the course of the discussion the fellow is expected to refer to an appropriate literature survey that documents the frequency, cause, basic science foundation, and treatment of the particular complication. This mandatory conference is combined with a Quality Assurance Conference, where fellows and staff present particularly challenging pre-operative clinical problems for review, comment, and suggestions by Page 20 of 43 the other participants in the conference. Patient images are used, and the clinical problem delineated to the group. The fellows then suggest appropriate solutions to the problem, starting from junior and progressing to the senior fellow. Journal Club: For this mandatory monthly conference in which the Senior Fellow selects articles from the recent literature to be read by the fellows and faculty attending the conference. The conference is held at the home of the Program Director and directed by him. Topics include basic science, clinical innovations, ethics, and medico-legal articles. The conference format consists of exposition of the articles by individual fellows, with a scholarly evaluation of the article, including a discussion of the hypothesis, study design, analytical methods, statistics, and a critical evaluation of the conclusions expected of the presenter. A discussion between staff and fellows helps place the article into perspective. Core Curriculum in Plastic Surgery: As noted above, this required monthly conference is the didactic backbone of the residency and is hosted and led by Dr. Marie Claire Buckley. The conference represents a cyclic repetition of the core curriculum topics in Plastic Surgery as defined by AACPS CoreQuest (http://www.aacplasticsurgery.org/), and supplemented by Selected Readings in Plastic Surgery. This conference deals with the resection, repair, replacement, and reconstruction of defects of form and function of the integument and its underlying anatomic systems, including the craniofacial structures, the oropharynx, the trunk, the extremities, the breast, and the perineum. It includes aesthetic surgery of structures with undesirable form, special knowledge and skill in the design and transfer of flaps, in the transplantation of tissues, and in the replantation of structures are vital to these ends, as is skill in excisional surgery, in management of complex wounds, and in the use of alloplastic materials. Each section of the Selected Readings contains CME credit questions that the fellows must answer prior to the conference and discuss during it. Fellows are required to read the subject matter in its entirety before each session. During conference one fellow will give a 15 minute overview of the subject, another fellow shall lead a quiz/discussion using past In-Service examination questions, and the final fellow shall choose to present to the group recent journal articles related to the subject matter. While this exposure is not a substitute for didactic training during residency rotations, it does familiarize them with most of the core scientific content, and makes subsequent exposure a reinforcement rather than a discovery. CoreQuest 1. Local Anesthetics 2. Breast Reduction 3. Breast Aug, Mastopexy 4. Breast Reconstruction 5. Burns 6. Cleft Lip and Palate 7. Coding 8. Liposuction/Abdominoplasty 9. Facelifts 10. Blepharoplasty 11. Chemical Peel 12. Hair Transplant 13. Rhinoplasty 14. Craniofacial 15. Ear Reconstruction 16. Eye/Eyelid 17. Flaps 18. Chest Wall / Abdominal Wall 19. Congenital Hand 20. Hand Fractures / Dislocations 21. Wrist 22. Hand Nerves 23. Rheumatoid Hand 24. Hand Tumors 25. Hand/Fingertip Amputations, Dupuytren's, Vascular 26. Hemangiomas 27. Head and Neck Anatomy 28. Head and Neck Tumors / Parotid 29. Laser 30. Facial Palsy 31. Lower Extremity 32. Lymphedema 33. Mandible 34. Orthognathic, TMJ, Chin 35. Melanoma 36. Microsurgery 37. Nasal Reconstruction 38. Pressure Sore 39. Skin Lesions 40. Soft Tissue Infection 41. Skin, Fat and Cartilage Grafts 42. Tissue Expansion 43. Wound Healing / Keloids 44. Lip/Cheek Reconstruction Cleft Lip/Palate, Craniofacial Interdisciplinary Conferences: There are two optional University of Minnesota referral clinics held in the School of Dentistry-the Craniofacial Anomalies Clinic and Cleft Lip & Palate Clinic. The conferences serve as interdisciplinary referral evaluations by faculty of the University community. Typically, five to seven patients are evaluated and reviewed at each clinic by a team Page 21 of 43 composed of the appropriate medical, surgical, dental specialties as well as speech-language pathology, neuropsychology and genetics. After the multiple clinical examinations are performed by each specialist, a face-to-face conference is held and a consensus treatment plan is derived by the team and communicated to the referring physician, as well as all specialists currently involved in the management of the patient. The emphasis of the conference is clinical, and consists of examinations and review of the laboratory and radiology findings prior to making treatment recommendations. The fellows attend this elective conference when one of the teaching staff is involved. Multidisciplinary Maxillofacial Trauma Conference: This mandatory monthly conference is organized by Dr. Schubert, and held at Regions Hospital on a Thursday evening. This conference includes participants from all of the major teaching institutions in the Minneapolis/St. Paul, is multi-disciplinary, and is coordinated with Plastic Surgery, Otolaryngology and Oral and Maxillofacial Surgery at the University of Minnesota. The conference format can vary, consisting usually of lectures given by local or invited experts from the participating disciplines speaking on their area of interest. Often the speakers are nationally and internationally recognized in their areas of expertise. Frequently the lecture is followed by presentation of clinical cases for analysis by the visiting expert, and is used as a springboard for open discussion. At other times there is more emphasis on fellows presenting challenging or problem cases to the group in an attempt to draw out the different interdisciplinary approaches to the problem. This is also the research forum for residents and papers accepted for presentation and publication are reviewed at this conference. Plastic surgery residents are expected to attend and present when appropriate. This conference is approved by the office of GME for 1.0 Cat I credit. Hand & Wrist Conference: This is a required bi-monthly conference during the Regions rotation. It is a combined Plastics/Orthopedic Hand clinical presentation and patient rounds, which consists of all of the attendings from the Division of Plastic Surgery and the Department of Orthopedics. Clinical cases are presented by orthopedic hand fellows/Plastic surgery residents/ interns or attendings for discussion of the scientific and clinical aspects of the case. The conference is directed by Dr. James Fletcher and an broad overview of common hand problems is covered in an annual basis. Emphasis on evidence-based approach for best practice in Hand Surgery is a priority. This conference is approved by the office of GME for 1.0 Cat I credit. Maxillofacial Trauma Radiology Conference: This is a weekly conference organized by Dr. Warren Schubert, at Regions, to discuss all of the Maxillofacial trauma cases that have been admitted or treated during the previous week by Plastic Surgery and ENT. For the five busiest months of the year, Oral and Maxillofacial Surgery participates. It is mandatory for the Interns and Plastics fellow on the Regions rotation. Pre-operative x-rays, operative management and post-operative x-rays are presented. A correlation with anatomy and pathology is discussed, as well as use of synthetic and alloplastic materials. Research Meeting: Monthly (as needed), Dr. Lacy directs a review of current research proposals with the residents in the program. Updates of IRB status and current projects are reviewed. Attendance is mandatory. Lecture by On-Call Staff: This is a weekly conference given by all regions staff on a rotating basis. On call staff meets weekly with an assigned lecture in basic anatomy and management for maxillofacial trauma and hand trauma. Other topics covered are infectious disease/flap technique and post-op care/breast health and other core topics in plastic surgery. These are also attended by the interns and are designed to provide basic management skills for the ER, wards, and OR. Guest lecture is often given by staff of Infectious disease regarding management of common patients on the service. Attendance is mandatory. Regions Morbidity and Mortality and Grand Rounds: This is a Wednesday morning monthly conference run by the resident rotating at regions. This conference is a review of morbidity on the regions plastic surgery service with review of literature and didactic presentation by the resident regarding current best practice regarding these complications. Further discussion by staff centers around clinical problems and experience with similar clinical cases. Didactic sessions are also given by rotating interns in general surgery, ortho, ER, OMF on topics of special interest for the entire department. Attendance is mandatory. This conference is approved by the office of GME for 1.0 Cat I credit. Page 22 of 43 Operative Preparation Conference: This is the major teaching conference held monthly at the Centennial Lakes Medical Center and is organized by Dr. Allen Van Beek. The conference format is Socratic, and consists of a series of unknown clinical situations which are presented to the fellows to solve. The fellows are asked to be consultants solving the problem, and are expected to use the provided x-rays and other clinical data to derive a treatment plan. This conference has a format similar to, and is designed to prepare the fellows for, the examiner’s cases in the ABPS certifying oral exam, where the fellow is expected to define the clinical problem, and to plan and articulate the appropriate treatment program. Typically the case is initially presented to the junior fellow who takes the problem as far as possible, before calling for assistance from his more senior fellows who manage the problem in turn. Attendance is mandatory. Program Goals and Objectives The following is an outline of the specific goals and objectives at each level of training, year-by-year, rotation by rotation. Goals and Objectives are formulated by the Curriculum Committee, with a resident member, approved by the faculty annually, and reviewed in a combined faculty meeting with the fellows annually. Achieving the program’s goals and objectives in a timely fashion, evaluated at the end of each rotation, will serve as objective evidence of personal and professional growth. We consider achieving these goals and objectives, as reflected in faculty and 360 degree reviews of the fellows, to represent satisfactory levels of progress. Achieving beyond them is encouraged and expected. Both faculty and fellows are encouraged refer to these goals and objectives frequently throughout the years of training, and during appropriate rotations. They are also reviewed quarterly between each fellow with the Program Director during the evaluation interviews at the end of each rotation. YEAR 1A July 1 through October 31 General Plastic Surgery I at the University of Minnesota Medical Center, Fairview and Veteran’s Administrative Medical Center At completion of the fellow’s first year of residency at the University of Minnesota, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Clinical evaluation of wounds and discussion of treatment plan Methods of clinical evaluation for basic aesthetic surgical patients including fellow’s aesthetic clinic Evaluation and preparation treatment plan options for breast reconstruction Management of a consultation service for CV, pressure ulcer and peripheral vascular problems at VAMC Basic preparation and presentation of computer generated graphics and data at conferences Use of internet and medical literature search techniques Methods for self-evaluation of practice by presenting complications and surgical outcomes November 1 through November 30 Oral Surgery Rotation at University of Minnesota Medical Center, Fairview At completion of the OMS rotation in the first year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Evaluation and treatment of patients with orthognathic deformities Manufacturing special splints and dental models Serving as a member of a multi-disciplinary oral trauma and tumor treatment team Evaluation and treatment of TMJ disorders Treatment of common oral pathological conditions Page 23 of 43 December 1 through February 28 Cosmetic Rotation I at University of Minnesota Medical Center, Fairview and West Health At completion of the cosmetic rotation in the first year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: The financial differences of private physician’s office practice The role of ancillary aesthetic office services Patient assessment and evaluation techniques of aesthetic surgical patients Management of the Fellow Aesthetic Clinic at UMMC Planning an aesthetic clinical research project How to ensure patient safety in out patient office surgery Assist and perform primary aesthetic procedures March 1 through June 30 General Plastic Surgery Rotation I at Regions Hospital At completion of the fellow’s first year of residency at Regions Hospital, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: How to evaluate and manage ambulatory hand injuries and maxillofacial injuries How to manage and direct the rehabilitation program for simple hand & maxillofacial injuries The basic techniques and modalities for evaluating complex trauma injuries Planning and assisting in harvesting free flap donor sites, and in micro anastomoses How to interact with families and other professionals, and present patients at multi-specialty conferences YEAR 1B July 1 through August 31 Hand Rotation I at Regions Hospital At completion of the hand rotation in the first year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: How to perform as the assisting surgeon on micro-surgical procedures Initial management of wrists and distal forearm fractures Methods for tendon transfers to – congenital and post traumatic injuries Evaluate, repair, and rehabilitation of major - peripheral nerve injuries The ability to identify, diagnose and manage common brachial plexopathies How to independently repair flexor tendons and peripheral nerves, propose and manage rehabilitation program. How to manage syndactyle, thumb hypoplasia and other common deformities September 1 through October 31 Craniomaxillofacial Rotation at Regions Hospital At completion of the craniomaxillofacial rotation in the first year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Have an understanding of the comprehensive multidisciplinary management of the acutely traumatized facial injury patient. Understand the diagnosis, investigation and management of the patient with a post-traumatic facial deformity. Design surgical treatment plan and social service program and rehabilitation of secondary facial reconstruction patients. Identify and manage common craniosynostosis syndromes, including pediatric skull moulding techniques Page 24 of 43 November 1 through December 31 Breast Rotation at University of Minnesota Medical Center, Fairview At completion of the breast rotation in the first year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: How to participate in multi-disciplinary breast treatment team Evaluation and management of congenital breast disease including psychological and social issues Diagnostic tests and modalities to evaluate and stage breast cancer and to evaluate breast implant for integrity Evaluation of patients and selection of methods for breast reconstruction after mastectomy Evaluation and treatment of patient needing revisions of reconstructions and aesthetic procedures January 1 through February 28 Pediatric Plastic Surgery Rotation I (Craniofacial) at University of Minnesota Medical Center, Fairview and Children’s Hospitals At completion of the pediatrics rotation in the first year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Presenting patients and participating in the comprehensive multidisciplinary management of the craniofacial patient. Diagnosis and treatment of the craniosynostoses both syndromic and non-syndromic and their surgical management. Diagnosis and treatment of craniofacial anomalies, both syndromic and non-syndromic and their surgical management. March 1 through April 31 Microneurosurgery Rotation at North Memorial Medical Center At completion of the Micro-neuro rotation in the first year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Evaluate and surgically manage patients with amputation injuries Evaluate and mange patients for reconstruction after nerve injury or degenerative disease Evaluation and management of brachial plexus injuries Successful peripheral nerve, grafting and rehabilitation May 1 through June 30 General Plastic Surgery I at the University of Minnesota Medical Center, Fairview and Veteran’s Administrative Medical Center At completion of the fellow’s first year of residency at the University of Minnesota, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Management of patients in the context of a multi-disciplinary breast clinic setting Demonstrate the ability to plan and perform free TRAM and secondary breast reconstructions Performing as Principle surgeon with independent responsibility for complex aesthetic and reconstructive procedures Evaluation and independent selection of management plan of complicated secondary reconstructions Independent coordination and management of recurrent pressure ulcers, and chronic or recurrent wounds The ability to plan and perform free tissue and other complicated forms of secondary reconstruction Mentoring and teaching medical students and general surgery fellows The technique to present research work at national meeting(s) Finally, at completion of the fellow’s first year of residency at Regions Hospital, in addition to the subspecialty rotations, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Page 25 of 43 Perform capably to manage the team caring for complex maxillofacial trauma How to perform as fellow managing adult craniofacial cases and problems The capability to be primary surgeon on complicated eyelid and facial burn reconstruction cases Demonstrate ability to mentor and direct Oral Surgery fellow, interns, medical students, and manage the resources of a multi disciplinary team including a physician assistant In addition to the above, all fellows are required to meet the following goals and objectives for each year of training: Satisfactory attendance and participation in academic teaching conferences Submission of operative log data after each rotation In-Service scores above 25th percentile Adequate clinical performance YEAR 2 July 1 through August 31 Pediatric Plastic Surgery Rotation I (Clefts) at University of Minnesota Medical Center, Fairview and Children’s Hospitals At completion of the pediatrics rotation in the second year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Presenting patients and participation in the comprehensive multidisciplinary management of the cleft lip and palate patient and be able to surgically manage this patient. Understand the embryology of normal facial development and common congenital anomalies of the head and neck and extremities. Working knowledge of the diagnosis, investigation and management of hemangiomas, vascular malformations and congenital nevi. Coordinate post-op care with Pediatric service. September 1 through October 31 Cosmetic Rotation II at the University of Minnesota Medical Center, Fairview and West Health At completion of the cosmetic rotation in the second year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Independent evaluation and management of aesthetic patients Completion of an aesthetic clinical research project How to manage complications independently How to evaluate and manage complicated aesthetic patients and secondary patients Planning and establishing ancillary services in a private office Financial & safety management of office surgery facility Ethical marketing of personal practice on internet and in print November 1 through December 31 General Reconstruction II at Regions Hospital At completion of the fellow’s second year of residency at Regions Hospital, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: The ability to choose and independently harvest free flap donor sites How to evaluate free tissue/replantation patients and manage post operatively The ability to perform micro-surgical procedures as assistant How to plan & perform the surgical repair of maxillofacial injuries and congenital defects Evaluate & manage complex referral patients as part of multi-disciplinary team & articulate the specific care plan for patients with complex trauma Page 26 of 43 January 1 through February 28 Hand Rotation I at Regions Hospital At completion of the hand rotation in the second year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: The ability to evaluate, plan, and perform the primary surgical repair of common hand injuries Evaluate and propose treatment plan options for complex multi-level upper extremity injuries Coordinate evaluation of the injury at the remote site and preparation for transfer of patient and amputated parts Assist in the repair flexor and extensor tendons and manage rehabilitation program Design and fabrication of common hand splints Evaluate effectiveness of treatment outcomes by presenting cases at Hand Clinic conferences Complete didactic reading schedule assigned by Chief of Hand Surgery related to the Hand/Lower extremity/Microsurgery March 1 through April 30 Post-Bariatric Surgery Rotation at the University of Minnesota Medical Center, Fairview At completion of the post-bariatric surgery rotation in the second year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Evaluating post bariatric patients and participation in post-bariatric clinic Propose and execute treatment plans for management of post-bariatric patient Coordinate treatment team management of pre and post bariatric wounds Evaluate and manage large and recurrent ventral incisional hernias, and abdominal wall reconstruction May 1 through May 31 Burn Rotation at Regions Hospital At completion of the burn rotation in the second year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Medical management of patients with burns Burn wound reconstruction Wound care including local and acute Goals of physical rehabilitation Reconstruction of the burn patient Operative intervention for burn wounds Plan & assist at secondary revisions of complex facial & extremity burn wounds The ability to identify and institute resuscitation of burn patient. The ability to identify deep, perform excise and close including autograft and synthetic material The ability to identify and plan acute treatment of severe face and hand burns The ability to identify and treat electrical injuries and long-term sequelae June 1 through June 30 Head and Neck Rotation at University of Minnesota Medical Center, Fairview At completion of the Head and Neck rotation in the second year of residency, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: Evaluating and stage the extent of disease Making a differential diagnosis of head and neck disorders Obtaining appropriate laboratory and radiologic tests to evaluate patients Formulating, and justifying the recommendations of a treatment plan Recognition and detection of recurrence of malignancy Page 27 of 43 Finally, at completion of the fellow’s second year of residency at University of Minnesota Medical Center, Fairview, in addition to the subspecialty rotations, the fellow will have gained knowledge, skills, understanding and demonstrate competence regarding: How to evaluate and manage post-bariatric patients with body contouring procedures Designing treatment plan and operative management of common & basic aesthetic procedures Indications and technique of soft tissue expander and pedicle tissue breast reconstruction How to manage clinical and operative complications independently Proposing plans for operative and non-operative management of common wound problems The operative evaluation and management of primary pressure ulcers The primary evaluation and management of open chest wounds, head and neck cancer and skin lesions Planning independent research project with faculty mentor Coordinating health care team for inpatient, extended care, and post discharge patients Learn coding and billing terminology Training / Graduation Requirements The fellow must perform satisfactorily on clinical rotations, and demonstrate an adequate knowledge of the specialty to meet the graduation requirements for the Program, and be approved to sit for the ABPS qualifying and certifying examinations. The Board considers a fellowship in plastic surgery to be a full-time endeavor and looks with disfavor upon any other arrangement. The minimum acceptable training year is forty-eight weeks. Should absence exceed four weeks per annum for any reason, the circumstances and possible make-up time of this irregular training arrangement must be approved by the RRC for Plastic Surgery and documentation of this approval must be provided to the Board by the program director. Training in plastic surgery must cover the entire spectrum of plastic surgery. It should include experience in both the functional and aesthetic management of congenital and acquired defects of the head and neck, trunk, and extremities. Sufficient material of a diversified nature should be available to prepare the fellow to pass the examinations of the Board after the prescribed period of training. This period of specialized training should emphasize the relationship of basic science – anatomy, pathology, physiology, biochemistry, and microbiology – to surgical principles fundamental to all branches of surgery and especially to plastic surgery. In addition, the training program must provide in-depth exposure to the following subjects: the care of emergencies, shock, wound healing, blood replacement, fluid and electrolyte balance, pharmacology, anesthetics, and chemotherapy. Operative Records The Residency Review Committee for Plastic Surgery requires that each fellow keep a detailed record of operative experience. The maintenance and accuracy of this record are the responsibility of the individual fellow. In addition, copies of operative notes must be kept for all cases in which the fellow is listed as responsible surgeon. Your Log In user name and password will be given to you by the Residency Program Coordinator. Further instructions are to be downloaded from the ACGME web site at: http://www.acgme.org/. Click on Resident Case Log System then User Manuals to begin. The program is authorized for PDA usage. Case logs are reviewed by the Program Director three times a year during the fellows’ evaluation periods. ACGME Competencies All University of Minnesota Medical School Residency/Fellowship training programs define the specific knowledge, skills, attitudes, and educational experiences required by the RRC to ensure its residents/fellows demonstrate the following: Page 28 of 43 Patient Care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. Medical Knowledge about established and evolving biomedical, clinical, and cognate (e.g. epidemiological and social-behavioral) sciences and the application of this knowledge to patient care. Practice-Based Learning and Improvement that involves investigation and evaluation of their own patient care, appraisal and assimilation of scientific evidence, and improvements in patient care. Interpersonal and Communication Skills that result in effective information exchange and teaming with patients, their families, and other health professionals. Professionalism, as manifested through a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population. Systems-Based Practice, as manifested by actions that demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value. Duty Hours It is essential for patient care and medical education purposes that undue stress and fatigue among the fellows is avoided. Thus the following policy has been developed regarding fellow duty hours, and reflects the current ACGME and Department of Surgery mandates. Duty hours are defined as all clinical and academic activities related to the residency program, i.e., patient care (both inpatient and outpatient), administrative duties related to patient care, the provision for transfer of patient care, time spent in-house during call activities, and scheduled academic activities such as conferences. Duty hours DO NOT include reading and preparation time spent away from the duty site. Specific provisions include: Duty hours must be limited to 80 hours per week, averaged over a four-week period, inclusive of all in-house call activities. Residents called back to the hospital while on call at home must count these in-house hours towards their weekly limit. Residents/Fellows must be provided with 1 day in 7 free from all educational and clinical responsibilities, averaged over a 4-week period, inclusive of call. One day is defined as one continuous 24-hour period free from all clinical, educational, and administrative activities. The training program provides adequate time for rest and personal activities, which consists of a 10 hour time period provided between all daily duty periods and after in-house call. Tracking Duty Hours In order to better assess the program’s compliance with ACGME working condition stipulations, the Division of Plastic and Reconstructive Surgery at the University of Minnesota has implemented a duty hour tracking system within Residency Management Suite (RMS). RMS is a web-based system, which the user accesses at: https://www.new-innov.com/. Fellows should log their duty hours into the RMS system daily. The program director monitors the work activity of the fellows on a monthly basis, to ensure that duty hours do not exceed the standard, and that the fellows are not required to perform excessively difficult or prolonged duties regularly. If necessary, fellows may contact the Ombudsman if they feel the workload is negatively affecting the quality of their education or not adhering to required guidelines. Training and account set-up for RMS is provided by Stephanie Schaffer, RMS Coordinator. Please contact her for new user instructions at (612) 626-4959 or sriedel@umn.edu. Page 29 of 43 Evaluation The Plastic Surgery Training Program is committed to comprehensive, regular and timely evaluation of the educational and professional achievement of surgical fellows. This section presents the purpose, components and methodology of the fellow evaluation system. Purpose of the Evaluation System To provide information on the quality of the fellows for the following reasons: To make informed decisions on fellow promotion To provide data to specialty boards for certification To write letters of recommendation Identify performance deficits to improve the quality of the fellow Identify program strengths and weaknesses and target areas for modification in the curriculum To properly evaluate a fellow’s performance the assumptions must be clearly stated. By doing so, the foundation is laid for the evaluation of the progress of the fellow and for determining the effectiveness of the program to educate fellows. The fellow must demonstrate efforts to develop themselves to the high level of performance expected of a specialist in plastic surgery while functioning in an environment where they are an integral part in providing service to the patient. To do so they are expected to: Develop a personal program of self-study and professional growth with guidance from the teaching staff. Participate in safe, effective and compassionate patient care under supervision, commensurate with their level of responsibility. Participate fully in the education activities of the program and, as required, assume responsibility for teaching and supervision other fellows and students. Participate in institutional programs, activities involving the medial staff and adhere to established practices, procedures, and policies of the institutions. Apply cost containment measures in the provision of patient care. Our goal is to prepare the trainee to function as a qualified practitioner of surgery at the high level of performance expected of a specialist. The surgical fellow must be committed to provide an exemplary quality of service to patients, performed in concert with educational activities in order to graduate as a well rounded, knowledgeable and highly qualified surgeon. In order to accomplish these goals the following objectives have been established. The fellow must: Acquire a solid foundation of fundamental surgical knowledge. This is done through self-study, an organized Core Curriculum, Conferences, both departmentally and institutional and service specific, and close association with faculty. An understanding of biology as it relates particularly to disorders of a surgical nature and an understanding of the etiology, pathogenesis, diagnosis and management of surgical disorders is absolutely necessary for completion of the program. Use sound surgical judgment, think rationally and use the literature to solve problems. Achieve a satisfactory level of critical skill prior to completion of program. The fellow should have superb history and physical skills, should do an appropriate diagnostic work-up with an understanding of the tests to be ordered, and be able to develop a management plan. All this should be done efficiently and in an organized manner. Exhibit good technical skills commensurate with residency level. The fellow should be prepared, show initiative and be willing to accept direction in the operating room. The fellow must maintain the highest moral and ethical values and demonstrates a mature attitude. The fellow should be trustworthy, conscientious and maintain a professional attitude both in demeanor and attitude. Being sensitive to the needs and feelings of others be it faculty, patients, family members or fellow fellows is also necessary. Acquire good teaching skills. The fellow should be willing to question and answer questions of students and junior fellows. The fellow should consistently create a supportive learning environment for all learners. Page 30 of 43 These goals are attained by a progressively graded clinical and operative experience. Within the limits of variability found in clinical practice an equivalent opportunity will be afforded each fellow, under the guidance and supervision of a qualified teaching staff, to develop the degree of mature surgical judgment and operative skill to render him or her prepared to provide surgical care to patients with a wide range of disorders. The teaching staff supervising the fellow will make the assessment of achieving this goal. Methodology of Evaluation The methodology used to achieve a broad, reliable and valid evaluation on the competency of each fellow includes: PSEF In-Service training examination scores Mock Oral examination scores Rotation evaluation forms by faculty Quality of presentations at Grand Rounds and other conferences Nursing and physician assistants’ evaluations Medical Student evaluations Performance teaching students and junior residents Patient evaluations of fellow care The quality and timeliness of record keeping Conference attendance The Plastic Surgery Educational Foundation In-Service training examination is an objective method used to evaluate the cognitive knowledge of the fellow. To progress fellows must score above the 40th percentile nationally at his/her level of training. Academic probation may be imposed for performance less than the 30th percentile, and fellows have been informed in the past, when their scores fell below this level in the first or second year, that unless their score exceeds this required percentile score, that they will not be advanced or graduated. The mock oral examination is a method of evaluating the clinical thinking of the resident. The examiners grade the residents’ answers on a pass/fail basis. Residents are expected to pass at least one of the mock oral examinations during their residency training. Failure to do so requires the resident to retake the test until they have successfully passed. Fellows are evaluated on conference presentations and attendance. Fellows should be well prepared for their presentation, able to discuss alternative treatments, present basic science background for the topic, and include a bibliography in all talks given. Records of attendance are maintained for monitoring conference attendance. These records are reviewed each year at the fellow evaluation sessions. Faculty complete evaluation forms on fellows at the end of each rotation, using the RRC evaluation template. These evaluations are designed to effectively assess the performance of the fellow in categories of patient care, medical knowledge, interpersonal and communication skills, practice-based learning and improvement, professionalism, and systems-based practice. The evaluator is also asked whether the evaluation is based on extensive, moderate or occasional observation. The service director is encouraged to meet with the fellow at the end of the rotation to review the evaluations with the fellow and provide immediate feedback on his/her performance. This meeting is documented on the appropriate form. Nursing staff and physician assistants at University of Minnesota Medical Center, Fairview (UMMC) and Regions Hospital complete similar evaluations of the fellows. The support staff evaluations are a shorter version of the faculty evaluation of the fellows, and are reviewed at the end of each rotation or every four months. Competencies evaluated include patient care, interpersonal and communication skills, practice-based learning and improvement, professionalism, and systems-based practice. Medical Students who rotate on the plastic surgery service at both UMMC and Region’s Hospital also complete evaluations on the fellows. This is a one page evaluation form concentrates on evaluating the fellows competencies in interpersonal and communication skills, practice-based learning and improvement, and professionalism. They work to assess the teaching effectiveness of surgical fellows. In addition to receiving ongoing feedback as to his or her teaching performance, this data will be summarized for each fellow for review at the annual fellow evaluation session. Page 31 of 43 Patients from University of Minnesota Medical Center, Fairview and Regions Hospital also complete evaluations on the fellows. At the University of Minnesota Medical Center, Fairview approximately 20 evaluations are mailed 15 days prior to the end of the rotation to patients who had been on the plastic surgery service. At Regions Hospital evaluations are handed to patients in clinic with the instruction to return the evaluation via mail to the Residency Program Coordinator at the University. These evaluations are then included in the evaluation review at the end of each rotation or every four months. Competencies evaluated include professionalism and interpersonal and communication skills. Important in fellow performance is his/her attention to record keeping. This includes accuracy, timeliness, and readability. In addition to the program directors random review of records, a compliance report is run on average two times a year on fellows rotating at University of Minnesota Medical Center, Fairview and Regions Hospital. The Plastic Surgery faculty holds evaluation sessions, three times a year, to review each fellow’s clinical evaluations, conference attendance, In-Service score, teaching performance, academic development, and record keeping habits. Suggestions for counseling of a particular fellow may result from this meeting. This discussion on each fellow is brought to conclusion with one of the following recommendations: Advancement with statement of exemplary performance and areas that need development. Advancement with statement of deficiencies to be improved. Advancement with notification of academic probation and statement of deficiencies to be improved. Unsatisfactory performance and dismissal from the program. Each fellow meets with the program director after each rotation. The fellow’s PSOL must be available to the residency coordinator for review prior to the meeting with the Program Director. The Program Director will review faculty, support staff, medical student, and patient fellow evaluations and the PSOL data with the fellow, who will have an opportunity to comment on the evaluations and sign a written performance summary. Based upon the PSOL data review, plans will be made to provide the appropriate clinical case emphasis for the upcoming months. The resident has an opportunity to submit a response to the evaluation in writing if they desire. Appeal Process A fellow may exercise the right to appeal any decision regarding plans for non-renewal of contract or dismissal from the program. This process is outlined in the fellow contract as well as the Institution Policy Manual. The Division of Plastic and Reconstructive Surgery Fellowship Training Program in such case will carefully follow the University of Minnesota School of Medicine appeal guidelines. Mock Oral Examinations The purpose of a mock oral examination is to prepare the residents on the process for taking the ABPS oral exam rather than on the content or the answers. It is also a method of evaluating the clinical thinking of the resident. The mock exam is scheduled to take place in either May or June of each year and is arranged by the Residency Program Coordinator. All residents are required to attend; local graduates are also invited. All ABPS Oral Examination Guest or Senior Examiners on the faculty are specifically interdicted from participating in the Mock Oral Exam process as a stipulation of their ABPS activity. One month prior to the mock exams, faculty are asked to e-mail Dr. Migliori one case each for the oral examination. Case examples include: facial fracture, cleft, breast, head and neck, and spaghetti wrist. A total of 9 cases minimum is required. On the day of the exam each resident is interviewed separately in front of at least two faculty members. Three cases or more are presented for approximately six to eight minutes apiece for a total of no more than 30 minutes a resident. Residents are interviewed separately at different times over the course of a day. The examiners grade the residents’ answers on a pass/fail basis. The resident must pass 5 out of the 6 cases in order to pass the examination. Residents are expected to pass at least one of the mock oral examinations during their residency training. Failure to do so requires the resident to retake the test until they have successfully passed. Page 32 of 43 On Call Schedules The objective of on-call activities is to provide fellows with continuity of patient care experiences throughout a 24hour period. In-house call is defined as those duty hours beyond the normal work day when fellows are required to be immediately available in the assigned institution. In-house call must occur no more frequently than every third night, averaged over a four-week period. Continuous on-site duty, including in-house call, must not exceed 24 consecutive hours. Residents may remain on duty for up to six additional hours to participate in didactic activities, transfer care of patients, conduct outpatient clinics, and maintain continuity of medical and surgical care. No new patients, as defined in Specialty and Subspecialty Program Requirements, may be accepted after 24 hours of continuous duty At-home call (pager call) is defined as call taken from outside the assigned institution. The frequency of at-home call is not subject to the every third night limitation. However, at-home call must not be so frequent as to preclude rest and reasonable personal time for each resident. Residents taking at-home call must be provided with 1 day in 7 completely free from all educational and clinical responsibilities, averaged over a 4-week period. When residents are called into the hospital from home, the hours residents spend in-house are counted toward the 80-hour limit. The program director and the faculty must monitor the demands of at-home call in their programs and make scheduling adjustments as necessary to mitigate excessive service demands and/or fatigue. At Regions Hospital, Dr. Warren Schubert designs the fellows' work schedules so that on average, fellows have at least 1 day out of 7 free of routine responsibilities and are on call from home no more often than every third night and are often on every fourth night. In order to accomplish this, general and emergency medical interns, oral surgery fellows, a hand fellow, and physician assistants assist in call coverage. At University of Minnesota Medical Center, Fairview, Dr. Bruce Cunningham is in charge of creating the monthly call schedule. While on this rotation the plastic surgery fellow has responsibility to first triage the patient and then call the plastic surgery staff when direction is required. In some cases the General Surgery resident assigned to cross-cover the service may be asked to provide first triage for Plastic Surgery in-patients or ER calls. At the Veteran’s Administrative Medical Center, the plastic surgery fellow serves as a sub-specialty back up to a general surgery fellow who has responsibility to first triage the patient and then call the plastic surgery fellow. With this arrangement, the plastic surgery fellows do not spend an inordinate amount of time in non-educational activities that can be discharged properly by other personnel. If the Plastic Surgery fellow is not available the VAMC general surgery fellow will contact faculty directly for patient care issues. On the North Memorial Medical Center rotation, the faculty member with whom the plastic surgery fellow is rotating is usually called first and then contacts the plastic surgery fellow if it is a case that has educational merit. The call schedule at North Memorial Medical Center is published for the eight rotating faculty every two months. Fellows are welcome to participate with any of the program faculty members. The fellow call schedule is also published every two months. The fellow will take call by pager from home and is expected to be available for night call twice a week and two weekends a month. The fellow will most often be called by the responsible staff person to either evaluate the patient initially or after the patient has already been seen. The fellow call schedule is provided to all plastic surgeons who take call at North Memorial. The fellow will also be available Monday through Friday from 7:00 AM to 5:00 PM. The fellow not assigned to the University or Regions will be expected to work with the UMMC fellow to coordinate weekend call so that each fellow has at least one day in seven free of responsibilities. Page 33 of 43 Patient care, however, is the ultimate responsibility of the faculty and there will be no instance when that care is the sole responsibility of the fellow. Overnight Call Rooms/Call Rooms Medical students, residents and fellows that must remain on call at the University of Minnesota Medical Center, Fairview and University of Minnesota Children's Hospital, Fairview overnight are guaranteed a room. Rooms closest to in-patient areas are assigned by your department, with additional rooms available to be signed out on an individual basis on the 4th floor of the Mayo Building (University Campus). Details are listed below. Understanding that space is a premium for call room availability; UMMC, Fairview, along with the University of Minnesota Medical School's Graduate Medical Education office developed the following principles for assigning rooms to each department. Rooms are prioritized for: 1. 2. 3. 4. 5. 6. Residents and fellows required to take overnight, in-house call. Year 3 and 4 medical students required to take overnight, in-house call. 1st and 2nd year medical students not required to take in-house call. Faculty and hospitalists required to take in-house call. All other residents, fellows, staff physicians or medical students needing a call room. Non-medical staff, excluding CRNAs. Room Availability Call rooms on the 4th floor of the Mayo Building are available for checkout as needed. These daily rooms have punch code security access changed everyday, and a security monitor on duty daily from 2 p.m. to 7 a.m. Call 612-626-6330 to reserve a room. Checking In Check-in can only occur during designated check-in hours: 2 p.m. to 7 a.m. Go to the check-in desk located in the Resident Lounge (Mayo C-496). The check-in desk is staffed by a security monitor (after 2:30 p.m.) during set hours seven days a week and will require you to present your ID badge. The security monitor will assign you a room, the room access code and the locker room and lounge access codes. Checking Out All individuals must be out of their room by 8 a.m. Housekeeping will begin cleaning by 9 a.m. If you wish to sleep past 9 a.m., make sure your "do not disturb" sign is indicated on your door. Do not leave personal belongings in the room. Resident Exercise Room An exercise room is available for resident, fellow or medical student use only, 24 hours, seven days a week. Located in Mayo C-496, it's equipped with treadmill, elliptical, weights and mats. Contact Mira Jurich, Coordinator, GME UMMC, at (phone) 612-273-7482, (pager) 612-899-7958 or mjurich1@fairview.org for the most recent access code. Mayo Locker Rooms One men's and one women's locker room with toilets, sinks and showers is available 24 hours, seven days a week. There are also lockers available for daily use. The access code is the same as the exercise room (see above for contact information). Important Things to Note: If you are assigned to carry a code pager for your department, please talk with your chief resident or resident coordinator about dedicated on-call for your department in or near the hospital. No room is checked out to the same service two consecutive days. You must have a valid hospital ID to checkout a room. Page 34 of 43 Belongings left in a room past noon will be removed and kept in a security locker. Belongings can be picked up anytime after 2:30 p.m. from the security monitor. Padlocks can be checked out for use in the locker rooms on a daily basis only. Resident Lounges The UMMC Resident Lounge is located in Room 6-501 in Unit J and is available 24 hours a day for residents from all specialties. The room is accessible by punch code access, which is changed weekly, or by open door when security monitor is on duty. TV/VCR, computers, and phones with access to the main hospital are available. There is also a partially stocked kitchen with refrigerator, coffee/tea makers, microwave, and toaster. Contact Mira Jurich, Coordinator, GME UMMC, at (phone) 612-273-7482, (pager) 612-899-7958 or mjurich1@fairview.org for the most recent access code. The Department of Surgery Resident Workroom is located in C278 Mayo. The room has punch code security access, which can be obtained from the Surgical Education Office, and is accessible to surgery residents 24 hours a day. Plastic Surgery residents may access their e-mail, connect to the Internet and catch up on duties requiring a telephone. The above room also houses the bulk of the division’s library. Selected Readings and the Journal of Plastic and Reconstructive Surgery can be found here. Suggestions as to additional materials are welcome. Additional materials can be found in the faculty's offices. Support Services A full range of patient support services are provided in a manner appropriate to and consistent with education objectives and patient care. These include but are not limited to Care Management Services, Employee Health Service, Health Information Management, Infection Control, Laboratory Medicine and Pathology, Nursing Administration, Nutrition Services, Patient Relations, Patient Transport, Pharmacy Services, Radiology Film File Services, Rehabilitation Services, Security Services, Social Services, Spiritual Health Services, and Shuttle Service between the Riverside and University campuses. Similar patient support services are provided by all major participating hospitals. Laboratory/Pathology/Radiology Services Federal and state regulation and regulatory agencies mandate competency validation for testing personnel (including physicians), documentation, quality assurance, quality control, etc. The regulations cover hospitals, clinics, physicians’ offices, nursing homes, and any site where testing is performed. Testing performed by physicians, practitioners, nursing staff, and laboratorians must meet regularly guidelines. Failure to comply with the mandates can lead to suspension, revocation, or limitation of certification and denial of reimbursement. Laboratory, pathology, and radiology services are readily available through all the major participating hospitals. Medical Records All University of Minnesota Medical Center and Fairview Riverside patient records can be accessed either via Allscripts, the Electronic Medical Records (EMR) system, or by calling the Health Information Management (HIM) offices at 612-626-3535. For instructions on medical record retrieval at additional sites, please direct inquiries to the appropriate site. Security/Safety The Security Monitor Program (SMP) is a branch of the University of Minnesota Police Department. SMP offers a walking/biking escort service to and from campus locations and nearby adjacent neighborhoods. This service is available completely free to students, staff, faculty, and visitors to the University of Minnesota - Twin Cities campus. To request an escort from a trained student security monitor, please call 612-624-WALK shortly before your desired departure time and walk safe. Page 35 of 43 University of Minnesota Medical Center, Fairview also employes security officers are on duty 24 hours a day to respond to emergencies and to escort persons to and from the parking facilities. Call 612-273-4544 if you wish to have an escort, and a security officer will meet you at your location. Moonlighting Policy Moonlighting requires a prospective, written statement of permission from the program director that will be made part the fellows’ file. No fellow will be required to engage in moonlighting activities, and such activities are strongly discouraged as they represent an unavoidable dilution of the time and energy available for Medical Education. Moonlighting activities are not included as part of the educational program in the fellowship programs. Moonlighting activities will not be allowed to conflict with the scheduled and unscheduled time demands of the educational program and its faculty. Fellows must disclose time spent in moonlighting activities. Failure to provide this information is grounds for discipline under Section VI of the Residency/Fellowship Agreement. The Fellow’s performance will be monitored for the effect of these activities upon performance and that adverse effects may lead to withdrawal of permission. Internal Moonlighting must be counted toward the 80-hour weekly limit on duty hours. The professional liability policy for fellows does not cover any activities that are not part of the formal education program. A fellow on a J-1 visa wishing to moonlight must obtain a separate J-1 visa for each facility where the fellow works outside the training program. Fellows engaging in moonlighting activities must be properly licensed and credentialed as determined by the organization where they moonlight. Supervision Policy It is the program director’s responsibility to ensure, direct, and document adequate supervision of residents and fellows at all times. Fellows are not to operate without faculty present, or conducted clinics without faculty present. No fellow activities are performed without the clear understanding and direction of one of the faculty members, except under extreme emergency conditions. The faculty attends the patient personally, and bears the ultimate responsibility for their care. This policy is applied uniformly at each of the teaching institutions. All patient care is supervised by qualified faculty in such a way that the fellows assume progressively increasing responsibility according to their level of education, ability, and experience. The teaching staff determines the level of responsibility given to each fellow. Fellows are provided with rapid, reliable systems for communication with supervising faculty, while the on–call schedules for teaching staff are structured to ensure that direct supervision is readily available to fellows on duty at all times. Faculty and fellows are educated to recognize the signs of fatigue and will adopt and apply policies to present and counteract the potential negative effects on an annual basis. At the University of Minnesota Medical Center, Fairview and Veteran’s Administrative Medical Center, if the patient undergoes surgery in either a major operating room or the ambulatory surgery suite, the nursing staff will Page 36 of 43 not call for the patient unless the attending surgeon is present in the surgical suite. Faculty is available by pager, and telephone 24/7, and a call schedule for faculty and fellows is published monthly. Inpatient hospital care is provided by the fellows with direct supervision of the attending staff on a daily basis. Rounds are made with the fellows by each attending on assigned patients in the hospital daily. Similarly, all patients seen in the clinic area are seen by attending and fellow alike and their management is discussed fully. When patients are seen in the emergency department at night or on the weekends, they are evaluated first by the fellow on call, consistent with duty hour limitations. That Plastic Surgery fellow ultimately conveys the information to the attending by telephone, and, if it is a minor problem, the fellow, based on his/her experience level, manages it, directed by the attending. If the patient problem requires admission, intra-operative treatment, or has any problems, the attending comes to the hospital, evaluates the patient, and supervises his care from there. This policy extends to all clinics and satellite surgery centers at all times. When a fellow rotates at North Memorial, they are involved with primarily one surgeon assisting or managing the patient in a directly supervised manner. Patient care in these rotations occurs with direct communication and supervision by the private attending. At North, fellows are assigned periodically to trauma call. It is required that they communicate with the attending by telephone to formulate a treatment plan, prior to initiating treatment. In most cases the attending comes to the hospital to provide direct supervision, and frequently only involves the fellow in cases with strong educational potential. The faculty rounds with fellows on assigned inpatients daily. At Regions Hospital the fellow always has on-site staff supervision. Ninety-seven percent of all patients seen in clinic, and all patients scheduled for the operating room are seen personally by the faculty who coordinates care with the fellow. Often the fellows will see the patient and then present the patient to the faculty member. Patients with minor injuries seen in the emergency room may be treated by the fellow but must be discussed with the faculty to confirm the treatment plan, prior to treatment. All cases performed in the operating room are under the direct supervision of the faculty. The fellow may be involved with managing some outpatient problems in the emergency room without direct visual supervision by the staff, but the staff is always available by pager or by phone. Graded Responsibility Fellow responsibilities increase at the beginning of each year of training (July 1). Whether to advance a fellow is decided by the faculty and is based on review of each fellow’s clinical evaluations, conference attendance, InService score, teaching performance, and record keeping habits. Below is a general description of graded clinical responsibility for plastic surgical fellows years one through three. During the three years of plastic surgery fellowship the fellow is gradually exposed to higher levels of responsibility for patient care, teaching, and scholarship. In the first year there is emphasis on general plastic surgery in the core rotations. The fellow is expected to be able to evaluate a patient, clearly describe the patient’s problem, delineate the tests which would need to be ordered to confirm the patient’s health status, and be aware of the other members of the health care team who need to be communicated with. During these general surgery rotations the fellow is expected to contact the faculty to inform them of all patients’ conditions and the results of appropriate labs. The fellow is expected to offer several alternatives for treatment plans to the faculty after the patient has been assessed. In the second year, during general plastic surgery rotations the fellow is expected to not only be able to accurately assess with physical examination and history, laboratory and radiographic studies; but also to specifically recommend a treatment program when they contact the faculty. The fellow will have gained enough knowledge and experience to independently manage many emergency room and ward situations with back-up from the faculty. The fellow will take a major role in assisting for more complicated cases and performing in the majority of straight forward cases always under the supervision of the faculty. During the second year the fellow will also begin to obtain exposure to the various sub-specialties in plastic surgery. During the sub-specialty rotations, it is assumed that the fellow has general knowledge regarding the plastic surgical sub-specialty. The fellow will take a greater role in requesting and evaluating specialized examinations, directing other members of the health care team, in rehabilitation, and care. The fellow will become more responsible in supervising and educating medical students, general surgery, and oral surgery fellows on the service. It is expected that the fellow will be able to harvest most donor sites, elevate most pedicle flaps, and will gradually gain greater facility in each of the surgical sub-specialties. Page 37 of 43 In the third year it is expected that the fellow will be able to perform as an independent evaluator of patient care status and surgical operator. The fellow will begin to use the faculty more as a resource to confirm a fully articulated treatment plan rather than to fill in gaps in knowledge in a treatment plan. By the end of the third year it will be expected that the fellow will be able to perform most of the primary and many of the more complicated procedures in the field of plastic surgery with the staff as a supervising assistant. They will also be expected to assist and supervise general surgery and oral surgery residents, and others, in some of the more basic and primary cases in the plastic surgical sub-specialties. During the third year it is expected that the plastic surgery fellow will no longer be consulting basic text, but will be researching patient care electronically using and seeking out the most up-to-date treatment options available. It is also expected that fellows will know how to coordinate the ancillary services and other members of the care treatment team to obtain the best outcome for an individual patient. Monitoring of Resident Well-Being The program director is responsible for monitoring fellow stress, including mental or emotional conditions inhibiting performance or learning, and drug-related or alcohol-related dysfunction. Both the program director and faculty are sensitive to the need for timely provision of confidential counseling and psychological support services to fellows. The plastic surgical fellows’ well being is determined through direct observation by faculty and staff. If there is concern the issue may be brought up during the fellow’s evaluation period with the program director. If a fellow does not feel comfortable speaking to the program director with regards to what is bothering him, alternate options are available. Fellows are encouraged to address the program’s Ombudsman, Dr. Marie-Claire Buckley, when they feel uncomfortable directly discussing their worries with the program director. Please see Fellow Grievance Policy for more information regarding to this policy. Also available is the Resident Assistance Program (RAP). In order to monitor fellow stress, including mental or emotional conditions inhibiting performance or learning, and drug- or alcohol-related dysfunction, the University of Minnesota Medical School has contracted with an agency called Sand Creek to provide services for you or anyone in your family. Sand Creek's counselors have particular expertise in dealing with the unique needs of individuals in their residency training programs. In contacting them, you will receive help in determining the problem, what should be done, and how to go about it. Further information can be found at http://www.med.umn.edu/gme/residents/rap.html. Photocopying At the University of Minnesota fellows may photocopy on the Department's copy machines as long as they adhere to copyright laws. In general, the residency coordinator should not be requested to perform large volume copying tasks for the fellows. The copy room (Mayo C274) houses a copy machine which requires no code for billing. Please use this machine when copying single page documents such as articles, etc. The copy code for the department of surgery's copy machine in the Phillips Wangensteen Building is available from the residency coordinator upon request. A CUFS number is needed in order to make copies in the Biomedical Library. Please ask the residency coordinator for the CUFS number when necessary. At Regions Hospital fellows may photocopy on the Department's copy machine located in the office as long as they adhere to copyright laws. The support staff should not be requested to perform copying tasks for the fellows. Journals from the Regions library will have to be checked out and brought to the office for copying. There is no copy code for the Regions library. Page 38 of 43 Office Support Services The Division of Plastic and Reconstructive Surgery’s offices at the University of Minnesota consist of one office personnel/residency coordinator, and will aide you in all matters related to the administrative end of regular office business. With the exception of insurance authorizations, the office personnel/residency coordinator does not manage patient related matters. Please refer the office personnel/residency coordinator for all questions relating to evaluations, division policy, vacation requests, conference scheduling, meeting scheduling, and On-Call schedules. The Department of Plastic & Hand Surgery has three office support staff. LuAnn LaShomb supports the department chairman, Dr. Warren Schubert. Valery Rousseau supports Drs. Dean Mann and Martin Lacey. As the person who sits at the front desk at this office, almost any question can be directed to her and she will find the answer or point you in the right direction. Jessica Woodford supports Drs. James Fletcher and Loree Kalliainen. She also sits in the front of our office and is willing and able to help with anything you may need. At Regions Hospital, contact the Physician’s Assistants (PA) regarding any patient care issues. These include our Lead PA, Frank Benfante, JoAnne Eller and Ned Bruce. Frank Benfante is also able to answer questions regarding the call schedule. Each PA is assigned to a different physician on a two-month rotating basis. If there is a question regarding which PA to contact any of the office support staff can point you in the right direction. All three of the PAs are dedicated to teaching and are happy to answer any questions you may have. Guidelines of Professional Dress Fellows are expected to be neat, clean, and orderly at all times during the performance of training program activities. Jewelry, clothes, hairstyle and fragrances should be appropriate for the performance of duties in the hospital or clinic, and should reflect a professional and respectful attitude towards the patient and other professional staff. The Fellow's identification badge is to be worn whenever the fellow is involved in clinical or administrative duties. Fellows are expected to dress accordingly to generally accepted professional standards appropriate for their training program. Where safety is a factor, fellows should use common sense in choosing clothing and shoes for training activities. Scrub suits are appropriate for designated areas, e.g. Operating Room, Labor & Delivery. Page 39 of 43 SECTION V: Administration (Please refer to Institution Policy Manual for Medical School Policy on the following: University of Minnesota Physicians, Administrative Contact List, Medical School Organizational Chart, and GME Organizational Chart.) Page 40 of 43 Main Hospital Contact Information Regions Hospital Department of Plastic & Hand Surgery Program Director: Warren Schubert, MD University of Minnesota Medical Center, Fairview Division of Plastic & Reconstructive Surgery Program Director: Bruce L. Cunningham, MD Business Operation Specialist: LuAnn LaShomb luann.m.lashomb@healthpartners.com Phone: (651) 254-3792 Fax: (651) 254-2808 North Building, 3rd Floor, Suite 1 640 Jackson Street St. Paul MN 55101 Administrative Specialist: Mariah Ipsan ipsa0001@umn.edu Phone: (612) 625-0697 Fax: (612) 624-4441 C261 Mayo Building Office Secretary: Valery Rousseau valery.l.rousseau@healthpartners.com Phone: (651) 254-0883 Bruce Cunningham, MD: (612) 899-2927 cunni001@umn.edu Residency Programs Specialist: Kari Kriesel kari.e.kriesel@healthpartners.com Phone: (651) 254-1504 Fax: (651) 254-5044 North Building, 3rd Floor, Suite 8, GME offices 640 Jackson Street St. Paul MN 55101 Med Student/Residency Coordinator: Deb Collier Deb.K.Collier@healthpartners.com Phone: (651) 254-1504 Fax: (651) 254-5044 Pager: (651) 629-1630 Physician Pagers & Email Addresses: Warren Schubert, MD: (612) 580-9170 WarrenSchubert@aol.com Martin Lacey, MD: (651) 629-0203 martin.s.lacey@healthpartners.com Physician Pagers & Email Addresses: Marie-Claire Buckley, MD: (612) 899-5143 buckl012@umn.edu Umar Choudry, MD: (612) 899-9313 choud008@umn.edu Resident Pagers & Email Addresses: Sue Mi Tuttle, MD: (612) 899-8789 chaxx033@umn.edu Samuel Marquez, MD (612) 899-2094 marqu035@umn.edu Jonathan McCue, MD (612) 899-7286 mccue011@umn.edu Veterans Administrative Medical Center Med Student/Residency Coordinator: Lisa Loyas Lisa.Loyas@med.va.gov Phone: (612) 467-1330 Fax: (612) 725-2227 Room 2J 100, VA Surgery Office Paul Lim, M.D., F.A.C.S. paul.k.lim@healthpartners.com Loree Kalliainen, MD: 612-613-3353 Loree.k.kalliainen@healthpartners.com Dean Mann, MD: (612) 580-7123 dean.e.mann@healthpartners.com James Fletcher, MD: (612) 580-9192 james.w.fletcher@healthpartners.com Physician Assistant Pagers: JoAnne Eller, PA-C: (651) 629-0154 Ned Bruce, PA-C: (651) 580-2150 Page 41 of 43 S.O.U.P. Administrative Phone List & 11th Floor PWB Offices Surgery Chairman’s Office Dr. Selwyn Vickers Patti Shudy Debby Rosenauer Toni Leeth Fax: 6-0654 6-1999 6-1999 6-1999 5-1174 Location: 11-132 PWB Jay Phillips Professor and Chairman Executive Assistant Executive Ofc and Admin Spec Research Coordinator Deputy Chairman’s Office Dr. David Rothenberger Bobbie Randolph Fax: 5-3660 6-6122 6-6122 Location: 11-168 PWB Professor and Deputy Chairman Executive Ofc and Admin Spec Associates/Admin Dolly Schmidt Margueritte Uveges Karen Boone James DeGross 5-7480/4-0480 (f) 5-6427/4-7733 (f) 6-3539 6-1968 Administrative Center Director Senior Office Supervisor/Notary Public Senior Administrative Director/Clinical Senior Administrative Director/Budget Human Resources Mary Jane Towle Kathleen Olakunle Sara Gort Kirk Skogen Sonya Johnson Stephanie Samens Student Work Desk Fax: 5-8080 5-8636 5-5982 4-7149 5-3954 4-5640 5-8763 6-2598 Location: 11-145 PWB HR and Education Manager/Notary Public Sr. Personnel Document Analyst/Notary Public HR Personnel Assistant Senior Accountant/Payroll/Telecommunications Senior Personnel Document Analyst HR Representative SOUP Education Teri Wolner Stephanie Schaffer Fax: 5-8080 5-3926 6-4959 SOUP GME Manager Resident/Fellow RMS Coordinator Surgery Education Connie Schmitz, PhD Ozlem Ersin, MBA Cathy Larson Niea Johnson Fax: 5-4411 4-1722 6-7282 5-6483 6-2590 Location: 11-134 PWB Director of Educational Research & Development Education and Technology Coordinator General Surgery Residency Coordinator Surgical Education Assistant Communications & Development Fax: 6-0902 Erik Thurman 6-4848 David Knutson 4-7740 Angie Lillie 5-9646 Joel Bergstrom 4-0450 Lori Olsen-Kramer 6-0692 Location: 11-100 PWB Director of Development, Surgery Director of Development, O.U.P. Development Assistant Director of Development, DIIT Director, Communications and Project Management Budget Office John Ahearn Donita Baumgart Kay Daeger Sujata Das Abby Doepke Nicholas Hooks Jennifer Turnure Lynn Kaatz Stacey Morris Edie Nelson Gail Richardson Linda Xiong Photography Jerry Vincent Fax: 4-9797 5-0645 4-7145 5-4103 4-5642 5-5633 6-3540 6-3168 6-2180 6-3168 4-9402 5-5964 5-7614 Location: 11-115 PWB Administrative Director (11-154 PWB) Principal Accountant Principal Accounts Specialist/Acct. Supv. Accountant Accounts Specialist Accounts Specialist Senior Accountant Senior Accountant Fiscal Officer Principal Accountant Principal Accountant/Grants Principal Accounts Specialist 5-9463 Photographer/Slides/AV Support Page 42 of 43 UMP Billing Office Carol Moriarty Dana Bork Dawn Ditmarson Marjorie Dorsey Prefix: 612-884- 0828 - 0836 - 0841 - 0810 Fax: 884-0988 Patient Accounts/Supv Patient Accounts Patient Accounts Patient Accounts Clinical Transplantation Journal Mary Londborg 5-1487, 5-6242 Editorial Assistant Lillihei Heart Institute Darlene (Dee) McManus Cynthia DeKay Administrative Director Executive Ofc and Admin Spec Fax: 5-0404 5-8988 4-7610 Transplant Information Services Fax: 5-9467 David Radosevich 6-4701 Jackie Sterling 4-5453 Program Director Executive Secretary Telephone/Pager Hints And Instructions All calls within Minneapolis begin with the area code of (612). All calls within St. Paul begin with the area code of (651). All calls north the Twin Cities begin with the area code of (763). All calls south the Twin Cities begin with the area code of (952). Most University of Minnesota telephone numbers begin with a prefix of: 624-, 625- or 626You need only to dial the last 5 digits of a number when calling from the University to another University extension. Most Fairview telephone numbers begin with the prefix: 273Most Fairview Riverside telephone numbers begin with the prefix: 672Dial ‘8’ in order to make an outside call from the University. This includes calls to UMMC! This also includes when you use the University FAX machines. The University’s toll-free telephone is: 1-800-688-5252 (ext. 5-1188) Patients should be directed to call the UMMC Call Center at 612-624-9707 for all scheduling needs. Non-clinical needs are to be directed to: 612-625-0697. This is the administrative office direct line and should be used for residency and administrative issues only. Do not give patients this number. Paging All plastic surgery staff and resident pagers from the University are alpha-numeric. The URL for alpha, or text, messaging is: http://www.americanmessaging.net/index.asp. Pages sent numerically should be considered urgent and a call-back is expected. Alpha text does not usually require a response, unless indicated (e.g., Call me). Abbreviated text is used liberally. If in doubt, call the sender. Last updated: March 6, 2016 Page 43 of 43