Clinical Psychology Review 32 (2012) 618–629
Contents lists available at SciVerse ScienceDirect
Clinical Psychology Review
How related are hair pulling disorder (trichotillomania) and skin picking disorder?
A review of evidence for comorbidity, similarities and shared etiology
Ivar Snorrason ⁎, Emily L. Belleau, Douglas W. Woods
Department of Psychology, University of Wisconsin-Milwaukee, Garland Hall, 2441 Harford Avenue, Milwaukee, WI, USA
H I G H L I G H T S
► Hair pulling disorder (HPD) and Skin picking disorder (SPD) co-occur more often than chance would predict.
► HPD and SPD have substantial similarities in clinical characteristics and have overlapping risk factors.
► The two disorders likely share etiology and should be categorized together in the DSM-5.
a r t i c l e
i n f o
Article history:
Received 8 July 2011
Revised 15 May 2012
Accepted 16 May 2012
Available online 20 July 2012
Keywords:
Pathological skin picking
Trichotillomania
Hair pulling disorder
Body focused repetitive behaviors
Grooming disorders
Comorbidity
a b s t r a c t
Hair pulling disorder (HPD; trichotillomania) and skin picking disorder (SPD) are relatively common and
potentially severe psychiatric conditions that have received limited empirical attention. Researchers are increasingly recognizing the similarities and co-occurrence of HPD and SPD, and several authors have
suggested that the two disorders should be categorized together in the DSM-5. In the present article, we
critically examined the evidence for comorbidity of HPD and SPD, and reviewed a diverse literature
pertaining to shared risk factors and similarities in clinical characteristics. Evidence suggests that the two
disorders co-occur more often than can be expected by chance, have substantial similarities in a variety
of clinical characteristics (e.g., symptom presentation and course of illness) and may have some distal
risk factors in common (e.g., genetic vulnerabilities). Implications for classification in the DSM-5, clinical
management and research on etiology were discussed.
© 2012 Elsevier Ltd. All rights reserved.
Contents
1.
2.
3.
4.
Introduction . . . . . . . . . . . . . . . . . . .
Definitions . . . . . . . . . . . . . . . . . . .
2.1.
Hair pulling disorder (trichotillomania) . . .
2.2.
Skin picking disorder . . . . . . . . . . .
Comorbidity . . . . . . . . . . . . . . . . . . .
Similarities and differences in clinical characteristics
4.1.
Symptom presentation . . . . . . . . . .
4.2.
Phenomenology . . . . . . . . . . . . . .
4.2.1.
Affective experiences . . . . . . .
4.2.2.
Dissociation . . . . . . . . . . .
4.2.3.
Automaticity . . . . . . . . . . .
4.3.
General demographics . . . . . . . . . . .
4.4.
Age at onset . . . . . . . . . . . . . . .
4.5.
Course of illness . . . . . . . . . . . . . .
4.6.
Response to treatment . . . . . . . . . . .
4.7.
Relation with other psychopathology . . . .
4.7.1.
Common axis I disorders . . . . .
4.7.2.
Axis II disorders . . . . . . . . .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
619
619
619
619
620
620
620
621
621
621
621
621
622
622
622
622
622
622
⁎ Corresponding author at: University of Wisconsin-Milwaukee, Department of Psychology, 2441 East Hartford Avenue, Milwaukee, WI 53201, USA. Tel.: +1 414 335 5919.
E-mail address: ivarsnorrason@gmail.com (I. Snorrason).
0272-7358/$ – see front matter © 2012 Elsevier Ltd. All rights reserved.
doi:10.1016/j.cpr.2012.05.008
I. Snorrason et al. / Clinical Psychology Review 32 (2012) 618–629
4.7.3.
Obsessive compulsive disorder (OCD) . . . . . . .
4.7.4.
Body dysmorphic disorder (BDD) . . . . . . . . .
4.7.5.
Body focused repetitive behaviors (BFRB) . . . . .
5.
Shared risk factors . . . . . . . . . . . . . . . . . . . . . . . .
5.1.
Familiality . . . . . . . . . . . . . . . . . . . . . . . .
5.2.
Genetic risk factors . . . . . . . . . . . . . . . . . . . .
5.3.
Neural substrates . . . . . . . . . . . . . . . . . . . . .
5.4.
Neurocognitive deficits . . . . . . . . . . . . . . . . . .
5.5.
Temperamental antecedents . . . . . . . . . . . . . . . .
5.6.
Environmental risk factors . . . . . . . . . . . . . . . .
5.6.1.
Under-stimulated environment . . . . . . . . . .
5.6.2.
Trauma . . . . . . . . . . . . . . . . . . . . .
6.
Discussion . . . . . . . . . . . . . . . . . . . . . . . . . . .
6.1.
What is the nature of the relationship between HPD and SPD?
6.2.
Future directions . . . . . . . . . . . . . . . . . . . . .
6.3.
Implications for research and practice . . . . . . . . . . .
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1. Introduction
Hair pulling disorder (HPD; trichotillomania) and skin picking disorder (SPD; also known as neurotic/psychogenic excoriation and pathological skin picking) are characterized by recurrent and excessive hair
pulling and skin picking, respectively. Both conditions have been described in the medical literature for more than a century (Hallopeau,
1989; Wilson, 1875) but have received limited empirical attention.
Mounting evidence shows significant morbidity associated with HPD
and SPD; including functional impairment, severe emotional distress,
disfigurement and medical complications (Arnold et al., 1998;
Diefenbach, Tolin, Hannan, Crocetto, & Worhunsky, 2005; Flessner &
Woods, 2006; Franklin et al., 2008; Lewin et al., 2009; Morales-Fuentes,
Camacho-Maya, Coll-Clemente, & Vázquez-Minero, 2010; O'Sullivan,
Phillips, Keuthen, & Wilhelm, 1999; Odlaug & Grant, 2008a; Odlaug,
Kim, & Grant, 2010; Soriano et al., 1996; Tucker, Woods, Flessner, Franklin, & Franklin, 2011; Wetterneck, Woods, Norberg, & Begotka, 2006;
Wilhelm et al., 1999; Woods, Flessner, et al., 2006). Nonetheless, little
is known about the etiology of these disorders, and there is a lack of consensus about how to conceptualize or categorize them.
Currently, HPD (trichotillomania) is classified as an impulse control
disorder in the fourth edition of the Diagnostic and Statistical Manual for
Mental Disorders (DSM-IV), but SPD lacks its own diagnostic category. In
the last two decades, researchers and clinicians increasingly have recognized the similarities and co-occurrence of HPD and SPD (Penzel, 2003),
and several authors have suggested that the two disorders should be
classified in the same class of disorders in the next edition of the DSM
(Bohne, Keuthen, & Wilhelm, 2005; Hoppe, Ipser, Lochner, Thomas, &
Stein, 2010; Stein, Chamberlain, & Fineberg, 2006; Stein et al., 2010;
Teng, Woods, Twohig, & Marcks, 2002). Moreover, an APA work group
(Stein et al., 2010) has provided a preliminary recommendation that
SPD should have its own diagnostic category in the DSM-5, and that
the two disorders should optimally be classified under the overall category of body focused repetitive behavior disorders (BFRBD). It is thus
timely to review the existing literature with respect to the nature and
the extent of the relationship between HPD and SPD. Greater understanding of the relationship not only informs nosological decisions, it
can also have implications for clinical management and guide research
on the etiology of both disorders.
The aim of the present review was to investigate the relationship between HPD and SPD through three lines of inquiry. First, we reviewed
studies examining whether co-occurrence of the disorders exceeds
chance levels (i.e., whether the two disorders are comorbid). Because
co-occurrence of psychiatric conditions can result from various methodological reasons (e.g., Klein & Riso, 1993; Neale & Kendler, 1995), we
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
619
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
622
623
623
623
623
624
624
625
625
625
625
625
626
626
626
626
627
critically examined existing studies with the aim of ruling out methodological artifacts. Second, we reviewed a diverse literature pertaining to
similarities and differences in clinical characteristics. The current conceptualization of psychiatric disorders (APA, 2000) is based on the assumption that a group of individuals demonstrating similar clinical
characteristics (e.g., similar symptom presentation and course of illness)
represent a distinct diagnostic entity that reflects common etiology
(Robins & Guze, 1970). Likewise, if two syndromes present a highly similar clinical picture, they could share etiological mechanisms. Thus, our
second aim was to compare HPD and SPD on a variety of clinical characteristics including symptom presentation, phenomenology, general demographics, age of onset, course of illness, response to treatment and
relation with other psychopathology. In our third line of inquiry we examined evidence for shared underlying risk factors including familiality,
genetic vulnerabilities, neural abnormalities, neurocognitive deficits,
temperamental traits and environmental stressors. Throughout the review we tried to identify methodological limitations and gaps in the
literature.
2. Definitions
2.1. Hair pulling disorder (trichotillomania)
HPD involves excessive and recurrent pulling out hairs from the
scalp, eyebrows, eyelids, pubic area, legs or other parts of the body. In
DSM-IV (APA, 2000), HPD is defined as recurrent hair pulling that is
not better accounted for by another mental disorder (e.g., delusions)
or medical condition (e.g., dermatological problem), and results in noticeable hair loss and significant distress or functional impairment. Additional criteria include increased arousal before pulling or when the
behavior is resisted, and pleasure, gratification or relief when hair is
pulled out. Recently, a work group formed by the APA recommended
these additional criteria be deleted because many sufferers of clinically
significant hair pulling fail to report these experiences (Stein et al.,
2010).
2.2. Skin picking disorder
SPD is characterized by excessive and recurrent picking or
scratching of the skin on the face, extremities or other parts of the
body. People with SPD tend to pick at scabs, acne or other irregularities on the skin. The APA work group (Stein et al., 2010) suggested the
following definition of SPD for DSM-5: recurrent skin picking that results in skin lesion(s) and clinically significant distress or functional
impairment, but is not restricted to the symptoms of another mental
620
I. Snorrason et al. / Clinical Psychology Review 32 (2012) 618–629
disorder (e.g., body dysmorphic disorder or delusional disorder) or
due to a medical condition or the effects of drugs. Other similar
criteria have been offered (e.g., Keuthen et al., 2010; Odlaug &
Grant, 2012), some of which also included a requirement of mounting
tension, urge or intrusive preoccupation before picking and gratification or relief during the act (Arnold, Auchenbach, & McElroy, 2001).
3. Comorbidity
Comorbidity can be defined as a co-occurrence of two disorders in a
population that exceeds chance levels. The likelihood of an individual
having two disorders by chance can be calculated by multiplying the
prevalence of each disorder. Thus, co-occurrence exceeding this number indicates comorbidity between the disorders (Klein & Riso, 1993).
Unfortunately, there are no data available on the co-occurrence of
HPD and SPD in the general population. However, several studies have
assessed prevalence of HPD in SPD samples, and prevalence of SPD in
HPD samples. It is therefore possible to compare the frequency of
co-occurrence in these samples with base-rates in clinical populations.
The estimated lifetime prevalence of HPD in inpatient psychiatric samples ranges from 1.3 to 4.4% (Grant, Levine, Kim, & Potenza, 2005;
Müller et al., 2011; Tamam, Zengin, Karakus, & Ozturk, 2008) and the
lifetime prevalence of SPD in inpatient samples ranges from 7.3 to
11.8% (Grant, Williams, & Potenza, 2007; Müller et al., 2011). According
to these base-rates (i.e., average of 9.6% for SPD and 2.7% for HPD), the
prevalence of co-occurrence by chance in inpatient settings should be
around 0.26% (i.e., 9.6 × 2.7 = 0.26), and presumably somewhat lower
in outpatient settings (data on base-rates in outpatient samples are
not available for both HPD and SPD). Our review of the literature
showed that the prevalence of SPD in HPD outpatient samples ranged
from 10 to 34% (average of 20.8% across studies, see Table 1) and the
prevalence of HPD in SPD outpatient samples ranged from 5 to 29.2%
(average of 15.5% across studies, see Table 2). Thus, the co-occurrence
of SPD and HPD appears to be much higher than expected by chance.
However, several methodological limitations need to be considered
before confidence in this conclusion can be expressed. For instance,
many of the studies (e.g., Christenson, 1995; Simeon, Cohen, et al.,
1997; Tay, Levy, & Metry, 2004) defined SPD quite loosely (e.g., failed
to exclude SPD due to dermatologic problems), and most of the studies
did not include a comparison group (e.g., psychiatric controls). Nonetheless, the few studies that did use strict diagnostic criteria showed
high co-occurrence rates (e.g., Grant, Odlaug, & Kim, 2007; Lochner,
Seedat, & Stein, 2010; Snorrason, Smari, & Olafsson, 2011) and one
study found higher rates of HPD in a SPD sample than in an OCD sample
(Grant, Odlaug, & Kim, 2010). Another limitation is the use of treatment
seeking samples that are known to artificially inflate co-occurrence
rates (e.g., because of a Berkson's bias or a clinical selection bias). Reassuringly, non-treatment seeking samples have produced similar findings as those conducted in treatment seeking samples (see Tables 1
and 2). Additionally, Hajcak et al. (2006) found a moderate correlation
(r = 0.30) between severity of hair pulling and skin picking in a large
sample of non-selected college students. Thus, even though population
based epidemiological studies are warranted, we tentatively conclude
that the co-occurrence of HPD and SPD is higher than expected by
chance.
4. Similarities and differences in clinical characteristics
4.1. Symptom presentation
HPD and SPD have strikingly similar symptom presentations (Bohne
et al., 2005; Lochner, Simeon, Niehaus, & Stein, 2002; Odlaug & Grant,
2008b; Teng et al., 2002). At a general level, both disorders involve recurrent behavior aimed at removing parts of the body (i.e., hair or
skin). People with HPD often seek to pull hairs that are different from
other hairs (e.g., coarse or gray hairs) and people with SPD target certain kinds of imperfections on the skin. In both groups, the sight or
feel of these preferred features often triggers episodes (Arnold et al.,
1998; Odlaug & Grant, 2008b). Individuals with HPD usually pluck out
hair one by one, often targeting specific areas on the body
(Christenson, Mackenzie, & Mitchell, 1991), and individuals with SPD
typically pick methodically at specific areas (Arnold et al., 1998). Patients in both groups ordinarily use the fingers to pick or pull but
some may also use implements (e.g., tweezers) (Arnold et al., 1998;
Christenson et al., 1991; Snorrason et al., 2011; Wilhelm et al., 1999).
Rituals before and after pulling or picking are common and frequently involve tactile stimulation (e.g., stroking hair against the lips
or rolling the skin between the fingers). Studies show that 48 to 72%
of HPD patients report at least one oral habit associated with hair
pulling (Christenson et al., 1991; Lochner et al., 2010) and 10 to 30%
sometimes eat the hair afterwards (Christenson et al., 1991; Odlaug &
Grant, 2008b; Schlosser, Black, Blum, & Goldstein, 1994). Likewise,
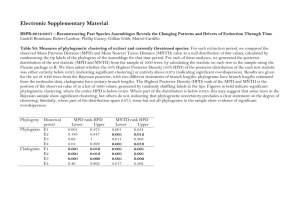
Table 1
Prevalence of skin picking disorder (SPD) in hair pulling disorder (HPD) samples.
Reference
Settings
Assessment
Results
Treatment seeking samples
Reeve, Bernstein, and Ten children/adolescents with HPD
Christenson (1992)
Sample
Outpatient child psychiatric clinic
One participant (10%) had a
current “face picking habit”.
Christenson, 1995a
164 adults with HPD
Outpatient psychiatric clinic
Tay et al.
(2004)
Ten consecutive children/adolescents
with HPD
Outpatient dermatology clinic in
children's hospital
Interview with patients and their
parent. Definition of SPD
not reported
Interview. Definition of SPD
not reported
Retrospective chart review.
Definition of SPD not reported
Lochner et al.
(2010)
58 adults with HPD
Outpatient psychiatric clinic
20 participants (28%) reported
lifetime history of at least some
“skin picking” and ten (14%)
lifetime history of at least some
“skin scratching”.
51% of participants with hair
pulling problem and 53% of
participants with HPD reported
problematic skin picking habit.
34% reported “scab picking” and
34% “acne picking”.
One patient (10%) had SPD in the
chart. (The authors did not report
whether SPD was systematically
screened for)
Interview. SPD defined according 17 participants (29.3%) had SPD
to proposed DSM-5 criteria
Non-treatment seeking samples
Simeon, Cohen, et al.
71 adolescents and adults with HPD
(1997)
Participants were responders to a
national magazine article
Mail self-report survey.
Definition of SPD not reported
Stein et al.
(2008)
Survey posted on a website of a
patient advocacy organization
Self-report Internet survey.
Definition of SPD not reported
a
1697 adults with hair pulling problem.
Thereof, 990 met strict DSM-IV
criteria for HPD
Unpublished data cited in Christenson and Mansueto (1999).
I. Snorrason et al. / Clinical Psychology Review 32 (2012) 618–629
621
Table 2
Prevalence of hair pulling disorder (HPD) in skin picking disorder (SPD) samples.
Reference
Sample
Settings
Assessment
Results
Treatment seeking samples
Simeon, Stein, et al. (1997)
21 adult with SPD
Outpatient psychiatric clinic
Two (9.5%) had HPD.
Arnold et al. (1998)
34 adults with SPD
Outpatient dermatology clinic
Wilhelm et al. (1999)
31 adult with SPD
Outpatient psychiatric clinic
Grant, Odlaug, and Kim (2007)
24 adults with SPD
Outpatient psychiatric clinic
Neziroglu et al. (2008)
40 adults with SPD
Outpatient psychiatric clinic
Grant, Odlaug, & Kim (2010)
Adults with SPD
(n = 53) and OCD
(n = 51)
Outpatient psychiatric clinic
Interview. HPD defined
according to DSM-III-R
Interview. HPD defined
according to DSM-IV
Interview. HPD defined
according to DSM-IV
Interview. HPD defined
according to DSM-IV
Interview. HPD defined
according to DSM-IV
Interview. HPD defined
according to DSM-IV
University students
with (n = 55) and
without SPD (n = 55)
University settings
Interview. HPD defined
according to DSM-IV
92 adults with SPD
Survey posted on a website of a
patient advocacy organization
Self-report Internet survey
Six (10.9%) SPD participants had HPD,
and additional two (3.6%) had problematic
hair pulling. No participant in the
control group had HPD.
25% had HPD.
Non-treatment seeking samples
Snorrason et al. (2011)
Walther et al. (2009)
people with SPD often engage in post picking behaviors, and studies
show that 32 to 35% eat the skin afterward (Snorrason et al., 2011;
Wilhelm et al., 1999). Pulling the hair or picking the skin on other people is reported in a minority of both groups (Snorrason et al., 2011;
Wilhelm et al., 1999; Woods, Flessner, et al., 2006) but may be more
common among SPD patients (Odlaug & Grant, 2008b).
Both hair pulling and skin picking tend to be highly habitual behaviors and sufferers usually pick or pull every day. People in both groups
commonly pick or pull in intermittent episodes throughout the day,
and some individuals spend hours each day engrossed in the activity.
Odlaug and Grant (2008b) found that individuals with SPD spent significantly more time per day engaged in the behavior than individuals
with HPD (105 vs. 56 min on average per day). Many patients in both
groups report general worsening of the behavior in the evening
(Lochner, Simeon, et al., 2002; Wilhelm et al., 1999), and it is interesting
that both hair pulling (Murphy, Redenius, O'Neill, & Zallek, 2007) and
skin picking (Singareddy, Moin, Spurlock, Merritt-Davis, & Uhde,
2003) have been found to occur during sleep.
4.2. Phenomenology
4.2.1. Affective experiences
Individuals with HPD and SPD commonly report affective experiences in relation to pulling/picking episodes. It has been proposed that
these behaviors function to produce stimulation (i.e., pleasure, gratification or relief) or regulate states of high or low arousal, such as anxiety or
boredom (Mansueto, Townsley-Stemberger, Thomas, & Golomb, 1997;
Penzel, 2003; Stein et al., 2006). Existing evidence supports these hypotheses. Several studies in clinical samples, as well as large Internet
surveys, indicate that a similar proportion of adults in both diagnostic
groups (around 80%) report increased tension before picking/pulling
and relief or gratification during the act (Arnold et al., 1998;
Christenson et al.,1991; Cohen et al., 1995; Odlaug & Grant, 2008a;
Tucker et al., 2011; Wilhelm et al., 1999; Woods, Flessner, et al., 2006).
Also, a series of studies have asked people with HPD and SPD to retrospectively rate the intensity of various affective states before, during and
after skin picking or hair pulling episodes (Diefenbach, Mouton-Odum, &
Stanley, 2002; Diefenbach, Tolin, Meunier, & Worhunsky, 2008; Duke,
Bodzin, Tavares, Geffken, & Storch, 2009; Duke, Kelley, Ricketts, Geffken,
& Storch, 2010; Meunier, Tolin, & Franklin, 2009; Neal-Barnett & Stadulis,
2006; Neziroglu, Rabinowitz, Breytman, & Jacofsky, 2008; Shusterman,
Feld, Baer, & Keuthen, 2009; Snorrason, Smari, & Olafsson, 2010; Wilhelm
Five (14.7%) had HPD.
Seven (23%) had HPD.
Seven (29.2%) had HPD.
Two (5%) had HPD.
Nine (17.3%) SPD and two (3.9%) OCD
participants had current HPD.
et al., 1999). Results show that the majority of patients in both groups report a rise in gratification or relief during pulling/picking. The results also
show that many patients report negative affect (e.g., boredom, tension or
anxiety) just before pulling/picking and a marked reduction in these
states after the behavior. Taken together, the evidence show that affective
experiences associated with hair pulling and skin picking are remarkably
similar and consistent with the notion that these behaviors serve to regulate arousal/affect and produce pleasurable feelings.
4.2.2. Dissociation
Approximately one-third of people with SPD report being in a
trance or feeling mesmerized while picking (Snorrason et al., 2010;
Wilhelm et al., 1999) and one study showed that 21.3% of individuals
with HPD sometimes experience depersonalization during hair
pulling episodes (du Toit, van Kradenburg, Niehaus, & Stein, 2001).
4.2.3. Automaticity
An interesting feature of both hair pulling and skin picking is that
many sufferers report little or no reflective awareness of the act as it occurs. A substantial proportion of patients in both groups reports being unaware of the act at least some of the time, although very few exclusively
pick or pull without awareness (Christenson, Ristvedt, & Mackenzie,
1993; Flessner, Conelea, et al., 2008; Tucker et al., 2011; Walther,
Flessner, Conelea, & Woods, 2009; Woods, Flessner, et al., 2006). Some
authors have suggested that both HPD and SPD may be meaningfully divided into two subtypes or styles of engaging in the behavior. One style
involves “automatic pulling/picking” that occurs out of reflective awareness in sedentary situations and the other, called “focused pulling/picking”, happens in full awareness in response to urges or negative
affective states. Factor analytic studies have identified distinct factors
representing both automatic and focused styles in HPD (Flessner,
Conelea, et al., 2008) and SPD (Walther et al., 2009) samples, however,
further research is needed to establish the predictive validity and clinical
utility of these subtypes (Lochner et al., 2010).
4.3. General demographics
Three studies directly compared HPD and SPD samples and found
very similar educational level, marital status, work status, mean age
and racial/ethnic distribution (Lochner, Simeon, et al., 2002; Odlaug
& Grant, 2008b; Odlaug, Kim, & Grant, 2010). McCarley, Spirrison,
and Ceminsky (2002) surveyed African American and non-African
622
I. Snorrason et al. / Clinical Psychology Review 32 (2012) 618–629
American college students and did not find differences in HPD frequency. Skin picking was not assessed.
Existing data also suggest that the gender ratio in HPD and SPD is
very similar, with high female preponderance in both groups. Findings
from adult clinical samples and surveys in patient advocacy organizations show that 88 to 94% of HPD patients are female (Cohen et al.,
1995; Christenson et al., 1991; Diefenbach et al., 2008; Gershuny et
al., 2006; Odlaug et al., 2010; Woods, Flessner, et al., 2006) and 75 and
94% of SPD patients are female (Arnold et al., 1998; Flessner & Woods,
2006; Neziroglu et al., 2008; Odlaug & Grant, 2008a; Snorrason et al.,
2010; Schuck, Keijsers, & Rinck, 2011; Wilhelm et al., 1999; Tucker et
al., 2011). The reason for this large gender bias is not clear. It could be
that more women than men suffer from SPD and HPD, or perhaps
women are more likely than men to seek help or support when dealing
with these problems and are thus overrepresented in clinical
populations.
4.4. Age at onset
Both HPD and SPD can occur in any age range, from infancy to old
age. However, studies in adult clinical psychiatric samples, as well as
surveys in a patient advocacy organization, have consistently shown
that adolescence is the most common age at onset for both SPD and
HPD. The average age at onset for SPD reported in these samples has
ranged from 12.3 to 16.1 years, with an average of 13.5 years across
studies (Flessner & Woods, 2006; Grant, Odlaug, et al., 2007; Grant,
Odlaug, & Kim, 2010; Lochner, Simeon, et al., 2002; Odlaug et al.,
2010; Odlaug & Grant, 2008a, 2008b; Snorrason et al., 2010; Wilhelm
et al., 1999). The average age at onset for HPD has ranged from 11.8 to
14.2 years, with an average of 12.9 years across studies (Cohen et al.,
1995; Christenson et al., 1991; Christenson, Mackenzie, Mitchell, &
Callies, 1991; Christenson, Chernoff-Clementz, & Clementz, 1992;
Grant, Odlaug, & Kim, 2010; Lochner et al., 2010; Norberg, Wetterneck,
Woods, & Conelea, 2007; Odlaug & Grant, 2008b; Odlaug et al., 2010). It
is worth noting, however, that some studies in dermatology samples
have found that the most common age at SPD onset is later in adulthood
(Arnold et al., 1998; Fruensgaard, 1984; Gupta, Gupta, & Haberman,
1986). The reason for the discrepancy between dermatology samples
and other samples is not clear. It is possible that individuals with later
age at onset are for some reason more likely to seek help from a dermatologist compared to individuals with earlier onset.
4.5. Course of illness
There are no data available on the long-term natural course of either
disorder. However, cross-sectional studies, mostly conducted in adult
clinical samples, suggest that the typical course of illness in both disorders is chronic with waxing and waning symptom severity (Christenson
et al., 1991; Gershuny et al., 2006; Snorrason et al., 2011; Swedo,
Leonard, Lenane, & Rettwe, 1992; Wilhelm et al., 1999). It has been
suggested that HPD occurring at a preschool age is often a benign
form of the disorder that has a more episodic course and may resolve
without intervention (Santhanam, Fairley, & Rogers, 2008; Swedo et
al., 1992; Swedo & Leonard, 1992; Tay et al., 2004). However, this notion
has not been subject to empirical scrutiny with longitudinal data. Even
though childhood SPD onset is commonly reported in adult SPD samples, a parallel benign childhood subtype of SPD has not been discussed
in the literature, to the best of our knowledge. It is conceivable that skin
picking in childhood is less likely than hair pulling to come to clinical attention, as the behavior (e.g., picking at scabs) may be considered less
abnormal and more socially acceptable than recurrent hair pulling.
4.6. Response to treatment
Empirical evidence has consistently shown that habit reversal is effective in eliminating or reducing both hair pulling (Bloch et al., 2007;
Keuthen et al., 2010; van Minnen et al., 2003; Woods, Wetterneck, et
al., 2006) and skin picking (Schuck et al., 2011; Teng, Woods, &
Twohig, 2006), at least in the short term (for review see Woods,
Snorrason, & Espil, 2012). Preliminary evidence also shows that acceptance and commitment therapy may be effective for both conditions
(Flessner, Busch, et al., 2008; Twohig, Hayes, & Masuda, 2006; Woods,
Wetterneck, et al., 2006).
Several drugs have been shown to benefit individuals with HPD,
including clomipramine (Bloch et al., 2007) and olanzapine (van
Ameringen, Mancini, Patterson, Bennett, & Oakman, 2010), but no
study has examined these drugs in SPD samples. A large randomized
controlled trial showed that N-Acetylcysteine, a glutamate modulator,
was superior to placebo in reducing hair pulling (Grant, Odlaug, &
Kim, 2009), and case reports indicate that individuals with SPD might
benefit from this drug (Odlaug & Grant, 2007). Similarly, a randomized
controlled trial (Grant, Odlaug, Chamberlain, & Kim, 2010) showed that
lamotrigine, a drug that also acts on glutamate, reduced skin picking in a
subgroup of SPD patients that performed poorly on a cognitive
set-shifting task (the efficacy of lamotrigine for SPD was also demonstrated in an uncontrolled trial, see Grant, Odlaug, et al., 2007). Taken
together, these studies suggest a possible glutaminergic dysfunction in
a subgroup of both SPD and HPD patients.
SSRIs are the only medications that have been tested in randomized trials in both HPD and SPD samples. Case studies and uncontrolled trials have
shown some efficacy of SSRIs in treating HPD (e.g., Iancu, Weizman, Kindler,
Sasson, & Zohar, 1996). However, a meta-analysis of the four randomized
controlled trials conducted so far indicated that SSRIs are no more effective
than a placebo in reducing hair pulling (Bloch et al., 2007). Uncontrolled trials have demonstrated some post treatment reduction in skin picking (e.g.,
Keuthen et al., 2007), but the three controlled trials published so far have
produced mixed findings (Arbabi et al., 2008; Bloch, Elliot, Thompson, &
Koran, 2001; Simeon, Stein, et al., 1997).
4.7. Relation with other psychopathology
4.7.1. Common axis I disorders
Studies in clinical samples show that people with SPD (Arnold
et al., 1998; Calikusu et al., 2003; Odlaug & Grant, 2008a; Neziroglu
et al., 2008; Snorrason et al., 2011; Wilhelm et al., 1999) and HPD
(Cohen et al., 1995; Schlosser et al., 1994) are frequently afflicted
with other psychiatric conditions, in particular anxiety- and depressive disorders. Lochner, Simeon, et al. (2002) directly compared the
frequency of common Axis I disorders in SPD and HPD samples and
found very similar comorbidity patterns. People in both samples
reported a high incidence of lifetime major depression and anxiety
disorders. The only significant difference between the groups was
higher prevalence of dysthymia in the SPD sample (the authors
noted that this difference might be due to the different cultures the
samples came from). In another study, no differences in Axis I comorbidity patterns were found between SPD and HPD patients (Odlaug &
Grant, 2008b).
4.7.2. Axis II disorders
Studies show that personality disorders are common among individuals who seek treatment for HPD and SPD (Christenson et al.,
1992; Cohen et al., 1995; Schlosser et al., 1994; Swedo & Leonard,
1992; Wilhelm et al., 1999). Lochner, Simeon, et al. (2002) compared
HPD and SPD samples and found no difference in the prevalence of
the personality disorders that were assessed (i.e., obsessive–compulsive
personality disorder, avoidant personality disorder, schizotypal personality disorder and borderline personality disorder).
4.7.3. Obsessive compulsive disorder (OCD)
It has been suggested that both HPD and SPD are related to OCD or
belong to the putative OCD spectrum (Stanley & Cohen, 1999; Stein,
Hutt, Spitz, & Hollander, 1993). Given the substantial phenomenological
I. Snorrason et al. / Clinical Psychology Review 32 (2012) 618–629
similarities between SPD and HPD, it is not surprising that differences
and similarities between these disorders and OCD are alike. Both HPD
and SPD are similar to OCD in that they involve repetitive motor behavior, but are dissimilar in that the behavior is typically not preceded by
harm-avoidant cognitions (Arnold et al., 1998; Woods, Flessner, et al.,
2006) and is ego-syntonic rather than ego-dystonic (Grant, Odlaug, &
Kim, 2010; Stanley & Cohen, 1999).
Studies in OCD samples show that prevalence of HPD (4 to 36%) and
SPD (10 to 26%) is similar (Bienvenu et al., 2000; Cullen et al., 2001;
Grant, Odlaug, & Kim, 2010; Grant, Mancebo, Eisen, & Rasmussen,
2010; Hasler et al., 2007; LaSalle et al., 2004; Lovato et al., 2012;
Miguel et al., 2008), although one might expect somewhat higher prevalence of SPD given that it has higher base-rate in clinical samples. Prevalence of OCD is similar across HPD (8.3 to 30.4%) and SPD (6 to 45%)
samples (Arnold et al., 1998; Calikusu, Yucel, Polat, & Baykal, 2003;
Christenson et al., 1991; Lochner, Simeon, et al., 2002; Odlaug & Grant,
2008b; Schlosser et al., 1994), however, two studies conducted in OCD
clinics have obtained even higher rates of OCD in SPD samples
(Neziroglu et al., 2008; Wilhelm et al., 1999). Finally, mixed findings
have been reported in studies investigating the familial relation between HPD/SPD and OCD (Bienvenu et al., 2000; Cullen et al., 2001;
Grant, Odlaug, & Kim, 2010; Lenane et al., 1992), making it difficult to
determine whether HPD and SPD have different familial associations
with OCD.
4.7.4. Body dysmorphic disorder (BDD)
Studies show that individuals with BDD often pick their skin in order
to correct minor or imagined flaws or imperfections on the skin
(Phillips & McElroy, 1992; Phillips & Taub, 1995; Tanquary, Lynch &
Masand, 1992). Few case studies have also described BDD patients
that pull hair in order to correct appearance (Fontenelle, Mendlowicz,
Mussi, Marques & Versiani, 2002; Tanquary, 1994). Typically, definitions of HPD and SPD exclude hair pulling and skin picking that is solely
due to BDD. Nonetheless, BDD patients who pick skin in response to appearance concerns have similar affective experiences related to skin
picking (i.e., gratification, tension reduction etc.) as pure SPD cases
(Phillips & Taub, 1995), and it is not clear whether or in what way
SPD (or HPD) secondary to BDD is different from primary forms of the
disorders.
It may be that BDD is more related to SPD than HPD. Grant, Menard,
and Phillips (2006) interviewed 176 BDD patients and found that 45%
had a lifetime history of SPD secondary to BDD. Only 2.3% had primary
HPD, but the authors did not examine primary SPD, possibly because
all the skin pickers in the sample were defined as secondary SPD. Nonetheless, these findings indicate that BDD is possibly more related to SPD
than HPD. Studies in SPD samples have found prevalence of BDD
unrelated to the SPD ranging from 5 to 32% (Arnold et al., 1998;
Neziroglu et al., 2008; Snorrason et al., 2011; Wilhelm et al., 1999).
Only two studies have documented BDD in HPD samples. One study
found a 22% prevalence of BDD in a HPD sample (Soriano et al., 1996),
however BDD was assessed with a self-report questionnaire which
may have resulted in overestimation. In contrast, Christenson and
Mackinzie (1995) reported that only 5 out of 169 HPD patients (3%)
had comorbid BDD. However, the authors noted that BDD was not systematically assessed in the sample, so this might be an underestimation.
Interestingly, all the comorbid BDD/HPD cases in the Grant et al. sample
and most of the comorbid BDD/HPD cases in the Christenson and
Mackinzie sample suffered from SPD as well. Thus, it may be that HPD
is only associated with BDD through its comorbidity with SPD. Taken together, the overall data suggest that SPD may be more strongly related
to BDD than is HPD.
4.7.5. Body focused repetitive behaviors (BFRB)
Several authors have noted associations between HPD/SPD and other
repetitive behaviors aimed at the body, such as nail biting and cheek/lip
biting (Sarkhel, Praharaj, & Akhtar, 2011; Stein et al., 2008; Stein et al.,
623
2010; Teng et al., 2002). Collectively these behaviors have been called
BFRBs, and it has been argued that all of these problems should be categorized together in the DSM-5 (Stein et al., 2010). In support of this notion, evidence suggests comorbidity between HPD/SPD and other BFRBs
(Christenson et al., 1991; du Toit et al., 2001; Odlaug & Grant, 2008b;
Grant, Odlaug, & Kim, 2010; Reeve, Bernstein & Christenson, 1992;
Stein et al., 2008; Teng et al., 2002). Studies also show a high incidence
of nail biting in family members of HPD and SPD patients (Grant,
Odlaug, & Kim, 2010; Odlaug & Grant, 2008b), and a genetic association
between pathological hair pulling, skin picking and nail biting
(Bienvenu et al., 2009). Finally, studies show that nail biting serves to
regulate arousal/affect just like HPD and SPD (Teng, Woods, Marcks, &
Twohig, 2004; Wells, Haines, Williams, & Brain, 1999).
5. Shared risk factors
5.1. Familiality
Several studies have investigated the prevalence of HPD and SPD in
first-degree relatives of patients with either or both disorders. Unfortunately, most of the studies relied on the family history method
(i.e., asked patients about problems in their relatives without
interviewing relatives directly). Also, most of the studies failed to report
how many relatives were inquired about. Therefore, we reviewed the
findings in terms of how many patients reported at least one relative
with the disorders (rather than examining percentage of afflicted individuals in samples of first-degree relatives). Findings show that 5.3 to
17.8% of HPD patients report having a first-degree relative with HPD,
and one study (Cohen et al., 1995) found that 3% of HPD patients
reported having a relative with a formal diagnosis of HPD (Table 3).
Arnold et al. (1998) interviewed 34 individuals with SPD and only one
participant (2.9%) reported having a first-degree relative with SPD. In
contrast, other studies in SPD samples have shown that 19 to 45% of participants report having first-degree relatives with SPD (see Table 3).
Familiality across the two disorders has also been examined in a few
studies. No participant in the Arnold et al. (1998) SPD sample reported a
family history of HPD, but other studies have shown that 3.8 to 9.5% of
SPD patients report a family history of HPD (see Table 4). Likewise,
two studies have shown a 6.6 to 8.3% prevalence rate of SPD in
first-degree relatives of individuals with HPD (see Table 4).
Most of the studies examining familiality of SPD or HPD have methodological limitations that need to be considered. First, given that only a
few studies reported how many relatives were inquired about, it is impossible to compare disorder prevalence in first-degree relative samples with prevalence in the general population. Moreover, most of the
studies failed to include comparison groups, making it difficult to compare prevalence of HPD/SPD patients reporting afflicted relatives with
prevalence in general (or clinical) populations reporting afflicted relatives. However, one study (Grant, Odlaug, & Kim, 2010) included a clinical comparison group and found a significantly higher percentage of
SPD patients reporting relatives with SPD compared to a percentage of
OCD patients reporting relatives with SPD (36.5% vs. 0). The results
also showed a non-significant trend toward higher rates of family history of HPD in the SPD group compared to the OCD group (3.8% vs. 0).
Second, all the studies with the exception of one (Swedo & Leonard,
1992) asked the patients about their relatives rather than interviewing
relatives directly. This method can be inaccurate and lead to either
under-reporting or over-reporting. However, it is interesting that the
only study that did interview relatives of HPD clients directly reported
high rates of afflicted relatives (Swedo & Leonard, 1992). Perhaps this
is because HPD and SPD are very secretive disorders and many sufferers
keep their problem hidden even from family members (Penzel, 2003;
Wilhelm et al., 1999).
A third limitation involves not taking into account comorbidity in
the patients themselves when asking about their relatives. For example,
a high incidence of relatives with HPD in a SPD sample might simply be
624
I. Snorrason et al. / Clinical Psychology Review 32 (2012) 618–629
Table 3
Familiality of hair pulling disorder (HPD) and skin picking disorder (SPD).
Reference
Sample
HPD in relatives of individuals with HPD
Swedo and Leonard (1992) 28 consecutive HPD patients
(children, adolescents and
adults) and 18 healthy
controls
Schlosser et al. (1994)
22 adults with HPD
King et al. (1995)
Cohen et al. (1995)
du Toit et al. (2001)
Malhorta, Grover, Baweja,
and Bhateja (2008)
Santhanam et al. (2008)
Odlaug and Grant (2008b)
Settings
Assessment
Results
Outpatient child/
adolescent
psychiatric clinic
Relatives of HPD cases (n = 106) and
relatives of healthy controls (n = 65)
were interviewed by raters blinded for
diagnostic status.
Participants interviewed about their
relatives
Parents interviewed (n = 30)
Five (17.8%) relatives of the HPD participants
and no relative of the controls had HPD.
Outpatient
psychiatric clinic
15 children/adolescents
Outpatient child/
with HPD
adolescent
psychiatric clinic
123 children, adolescents and Participants were
adults with HPD
responders to a
national magazine
article.
47 adults with HPD
Outpatient
psychiatric clinic
20 consecutive children/
Child/adolescent
adolescents with HPD
psychiatric
outpatient clinic
38 consecutive children/
Outpatient
adolescents with HPD
psychodermatology
clinic
Outpatient
Adults with HPD (n = 24),
psychiatric clinic
SPD (n = 33) and comorbid
HPD/SPD (n = 20)
SPD in relatives of individuals with SPD
Simeon, Stein, et al. (1997)
21 adult with SPD
Arnold et al. (1998)
Wilhelm et al. (1999)
Neziroglu et al. (2008)
Odlaug and Grant (2008b)
Outpatient
psychiatric clinic
34 adults with SPD
Outpatient
dermatology clinic
31 adult with SPD
Outpatient
psychiatric clinic
37 adults with SPD
Outpatient
psychiatric clinic
Adults with SPD (n = 33) and Outpatient
comorbid HPD/SPD (n = 20) psychiatric clinic
Grant, Odlaug, & Kim (2010) Adults with SPD (n = 53) and Outpatient
OCD (n = 51)
psychiatric clinic
Five participants (22.7%) had relatives
with HPD.
One participant (6.7%) had a parent
with HPD.
Mail self-report survey. Respondents asked Four (3%) reported having at least one
family member formally diagnosed
about formal diagnosis of HPD in their
with HPD.
family members
Participants interviewed about
their relatives
Retrospective chart review of HPD cases
(it is not clear whether family history was
systematically screened for)
Participants and their parents interviewed
Twelve (25.5%) had a family history
of HPD.
Charts of two (10%) cases indicated a
family history of HPD.
Participants interviewed about their
relatives
12.5% of the HPD individuals and 20% of
comorbid HPD/SPD individuals reported
having first degree relative with HPD.
Participants
relatives
Participants
relatives
Participants
relatives
Participants
relatives
Participants
relatives
Four (19%) had first degree relative
with SPD.
One (2.9%) reported family history
of SPD.
Fourteen (45%) reported having first
degree relative with SPD.
Sixteen (43%) reported having
first-degree relative with SPD.
30.3% of the SPD and 35% of the comorbid
HPD/SPD participants had first
degree relative with SPD.
19 SPD (36.5%) and no OCD participant
had first degree relative with SPD.
interviewed about their
interviewed about their
interviewed about their
interviewed about their
interviewed about their
Participants interviewed about their
relatives
because many of the patients themselves have HPD. Only one study
reported findings from pure HPD and SPD samples (Odlaug & Grant,
2008b). The results showed high prevalence of HPD familiality in SPD
patients without HPD (6.1%) as well as high prevalence of SPD
familiality in HPD patients without SPD (8.3%) (see Table 4). Finally,
no study reported how many relatives had both SPD and HPD, and
many studies failed to use specific diagnostic criteria when asking patients about HPD or SPD in their relatives (i.e., only asking a single question about whether any relative had either disorder). In conclusion,
preliminary evidence suggests that both HPD and SPD run in families,
however, given the underdeveloped literature it is difficult to determine
whether the two disorder share familiality.
5.2. Genetic risk factors
A few studies have investigated the genetic underpinnings of HPD and
SPD. Novak et al. (2009) examined concordance rates for HPD in a group
of monozygotic (MZ) (n=24) and dizygotic (DZ) twins (n=10). Results
showed that concordance rates for MZ twins (38.1%) were greater
than the concordance rates of DZ twins (0%), suggesting that HPD
has a significant genetic component (heritability estimate of 76%).
The authors also assessed concordance rates for SPD in the sample,
and found a trend toward a significant difference between MZ and
DZ twins (p = 0.06). The failure to find statistical difference was possibly due to lack of power.
In addition to twin study methodology, other researchers have
begun to examine specific genes associated with HPD and SPD. On the
Two (5.3%) children had relatives
with HPD.
bases of leads from animal models (Welch et al., 2007) demonstrating
that a deletion of the gene encoding SAP90/PSD95-associated protein
3 (Sapap3) resulted in pathological hair and skin removal, researchers
have attempted to link the Sapap3 gene to HPD and SPD in humans.
Zuchner et al. (2009) found an association between Sapap3 and HPD,
but Boardman et al. (2011) failed to find an association after correction
for multiple testing. Bienvenu et al. (2009) examined the link in a large
OCD family study and discovered that both SPD and HPD were associated with single nucleotide polymorphism (SNP) 3, rs6662980 in the
Sapap3 region of chromosome 1p35. Each disorder also had unique associations with other SNPs, where HPD was associated with SNP6
(rs4652869) and SPD with SNP4 (rs4652867). This suggests that HPD
and SPD may have both common and unique genetic associations. Interestingly, neuroimaging studies (Chamberlain et al., 2008; Lee et al.,
2010) have shown that individuals with HPD have abnormalities in
the striatum, a brain region where Sapap3 is highly expressed.
5.3. Neural substrates
To date, there has been no neuroimaging study conducted in an SPD
sample, and the few studies conducted in HPD samples have produced
somewhat mixed findings. Several studies have found evidence for abnormalities in multiple brain areas, including regions that are involved
in habit learning (e.g., striatum), emotion regulation (e.g., amygdalo–
hippocampal complex) and the ability to generate and suppress motor
responses (e.g., several cortical areas) (Chamberlain et al., 2008;
Chamberlain et al., 2010; Grachev, 1997; Keuthen et al., 2007; Lee et
I. Snorrason et al. / Clinical Psychology Review 32 (2012) 618–629
al., 2010; Swedo et al., 1991; O'Sullivan et al., 1997). In contrast, other researchers have failed to find brain abnormalities in individuals with HPD
(Rauch et al., 2007; Stein, Coetzer, Lee, Davids, & Bouwer, 1997). Thus,
further studies are needed to examine brain abnormalities in these disorders, and complete lack of data for SPD is especially noteworthy.
5.4. Neurocognitive deficits
Only a handful of studies have investigated neurocognitive deficits
in SPD and HPD. Chamberlain, Blackwell, Fineberg, Robbins, and
Sahakia (2005) theorized that deficits in inhibitory control underlie
both HPD and SPD. However, mixed findings have been reported from
studies comparing individuals with HPD or SPD to healthy controls on
neurocognitive tests designed to assess motor inhibition (i.e., the Stop
Signal Task and the Go/No-go task; Bohne, Savage, Deckersbach,
Keuthen, & Wilhelm, 2008; Chamberlain, Fineberg, Blackwell, Robbins,
& Sahakian, 2006; Martin et al., 1993; Grant, Odlaug, & Chamberlain,
2011; Odlaug, Chamberlain, & Grant, 2010; Snorrason et al., 2011). A
range of other neurocognitive deficits have been found in HPD samples
including problems in spatial working memory (Chamberlain et al.,
2007), divided attention (Stanley, Hannay, & Breckenridge, 1997), and
visuo spatial learning (Chamberlain, Odlaug, Boulougouris, Fineberg, &
Grant, 2009). However, no data are available on these deficits in SPD
samples. Studies using the Intra-dimensional/Extra-dimensional set
shifting task have consistently shown intact cognitive flexibility in
both HPD and SPD participants (Chamberlain et al., 2006; Grant et al.,
2011; Odlaug, et al., 2010).
5.5. Temperamental antecedents
There have been no longitudinal studies conducted on temperamental antecedents of SPD or HPD. However, preliminary cross sectional data indicate that both disorders deviate in similar ways from
normal populations with respect to some temperamental traits.
First, people with SPD and HPD both score higher than normal controls on questionnaires assessing emotionality or emotion regulation
difficulties (Shusterman et al., 2009; Snorrason et al., 2010). Second,
Lochner, Simeon et al. (2002) found that HPD and SPD patients differed in similar ways from population norms on subscales of the Temperament and Character Inventory. Both groups scored high on harm
625
avoidance (worry, fearfulness, pessimism), very high on reward dependence (sociality, warmth, dependence) but in the average range
on novelty seeking. Another study using a different version of this
scale in a community sample found that hair pulling was associated
with harm avoidance, but not reward dependence, and skin picking
was related to neither dimension (Favaro, Ferrara, & Santonastaso,
2007). However, this study is limited due to inadequate diagnosis of
HPD and SPD and few diagnosed individuals. In sum, preliminary
data suggest that both HPD and SPD are characterized by emotional
temperament, and possibly harm avoidance and reward dependence.
The extent to which these traits represent causal agents in the development of these problems (as opposed to e.g., being a result of the behavior itself or comorbid conditions) remains to be investigated.
5.6. Environmental risk factors
5.6.1. Under-stimulated environment
Lack of stimulation is a well documented risk factor for compulsive behaviors, including over-grooming, in animals (Moon-Fanelli,
Dodman, & O'Sullivan, 1999), but this issue has received scant research attention in the human literature. Nonetheless, there are
some clues suggesting that this type of environmental stressor may
have a role in HPD and SPD. First, experimental studies (Teng et al.,
2004) and self-report surveys (Shusterman et al., 2009; Snorrason
et al., 2010) show that boredom (i.e., lack of stimulation) often triggers skin picking and hair pulling episodes. Secondly, case reports
(Evans, 1976; Gupta et al., 1986) suggest that a period of severe activity restriction sometimes precedes the development of HPD and SPD.
Further studies are warranted to investigate this interesting
hypothesis.
5.6.2. Trauma
A number of case studies have reported an association between HPD
and history of trauma (Bordnick, Thyer, & Ritchie, 1994) and a few
uncontrolled studies suggest high incidence of trauma in clinical samples
of HPD (Boughn & Holdom, 2003; Gershuny et al., 2006) and SPD
(Neziroglu et al., 2008) patients. However, it is unclear whether history
of trauma is more prevalent in these samples compared to other psychiatric samples (Lochner, du Toit et al., 2002). Favaro et al. (2007)
interviewed a large community sample (n=934) of young females
Table 4
Shared familality of hair pulling disorder (HPD) and skin picking disorder (SPD).
Reference
Sample
HPD in relatives of individuals with SPD
Simeon, Stein, et al. (1997) 21 adult with SPD
Arnold et al. (1998)
34 adults with SPD
Odlaug and Grant (2008b)
Adults with HPD (n = 24), SPD
(n = 33)
and comorbid HPD/SPD (n = 20)
Settings
Assessment
Results
Outpatients psychiatric
clinic
Participants interviewed about their
relatives
Outpatient
dermatology
clinic
Outpatients psychiatric
clinic
Participants interviewed about their
relatives
(n = 279)
Participants interviewed about their
relatives
Two participants (9.5%) had
relative
with HPD
No participant had relative
with HPD
Grant, Odlaug, & Kim (2010) Adults with SPD (n = 53) and OCD Outpatient psychiatric
(n = 51)
clinic
SPD in relatives of individuals with HPD
King et al. (1995)
15 children/adolescents with HPD Outpatient child/
adolescent psychiatric
clinic
Outpatient psychiatric
Odlaug and Grant (2008b)
Adults with HPD (n=24), SPD
clinic
(n=33) and comorbid HPD/SPD
(n=20)
Participants interviewed about their
relatives
Two (6.1%) of the pure SPD
participants and four (20%) of
the participants with comorbid
HPD/SPD reported having
first-degree relative with HPD.
Two (3.8%) of the SPD participants
and no OCD participant had
first-degree relative with HPD.
Parents interviewed
(n = 30)
One participant (6.6%) had a
parent with SPD.
Participants interviewed about their
relatives
Two (8.3%) of the pure HPD
individuals and 7 (35%) of the
comorbid HPD/SPD individuals
had first-degree relative
with SPD.
626
I. Snorrason et al. / Clinical Psychology Review 32 (2012) 618–629
(age 18–25 years) and found that childhood sexual molestation and
childhood rape predicted skin picking/biting, but not hair pulling. However, the diagnostic criteria of HPD and SPD used in this study were limited, and few cases were identified. Taken together, empirical evidence
suggest that trauma or stress may be associated with both HPD and
SPD in some cases, but longitudinal data are needed to determine whether a causal relation exists between traumatic events and these disorders.
6. Discussion
6.1. What is the nature of the relationship between HPD and SPD?
Overall, our review revealed strong evidence for relatedness between HPD and SPD. Existing data suggest that the disorders have substantial similarities in a variety of clinical features and have significant
comorbidity that is likely not due to methodological artifacts. Nonetheless, there are many possible explanations for the relationship between
HPD and SPD. For instance, it is conceivable that the two disorders do
not share etiology and that one disorder for some reason simply enhances the risk for the other, thus explaining the high co-occurrence
rates. However, empirical data showing a consistent pattern of one disorder preceding the other are lacking. Also, the substantial similarities
in clinical characteristics and shared risk factors suggest that the relationship is more inherent than that. Another possibility is that comorbid
cases represent a distinct entity with independent etiology from pure
cases. Again, this explanation is unsatisfactory because it does not account for the similarities in clinical features. Moreover, Odlaug and
Grant (2008b) did not find meaningful differences between comorbid
cases and pure forms of the disorders.
The most parsimonious explanation for the overall literature is that
the two disorders share etiology. Given evidence for both unique and
shared genetic underpinning, and some unique risk factors across HPD
and SPD (see below), it is perhaps inaccurate to conclude that the two
disorders are simply different expressions of the same underlying condition. They likely have both shared and unique etiological mechanisms.
The state of the literature does not allow strong statements regarding
the nature or the extent of the shared etiology, but some broad conclusions can be made. First, evidence suggests that the two disorders have a
common genetic underpinning possibly explaining, at least in part, the
comorbidity and similarities in clinical features. Second, it seems plausible that the two disorders share some proximal etiological mechanisms.
The similarities in phenomenology may provide clues as to what these
mechanisms might be. Both hair pulling and skin picking modulate affective states as well as providing pleasurable stimulation, and it appears
that affective experiences play an important role in maintaining and possibly causing these problems (Shusterman et al., 2009; Snorrason et al.,
2010). Interestingly, healthy individuals report similar affective experiences associated with normal body grooming behaviors (e.g., picking at
acne or plucking eyebrows for cosmetic reasons), although the intensity
is much less than reported by patients (Bohne, Wilhelm, Keuthen, Baer,
& Jenike, 2002; Keuthen et al., 2000; Snorrason et al., 2010). It may
thus be hypothesized that some of the underlying etiological mechanisms shared by HPD and SPD have to do with a propensity for intense
affective experiences in relation to body-grooming behaviors.
It should be noted that both SPD and HPD may be heterogeneous
conditions (Arnold et al., 2001; Grant, Odlaug, et al., 2010; Lochner et
al., 2010), and it is possible that only subgroups of each disorder share
etiological mechanism. For instance, Stein et al. (2008) found that HPD
patients with a comorbid BFRB, including skin picking, were more likely
to be “focused pullers” (i.e., pull with full awareness in response to an
urge or negative affect) than HPD patients without such comorbidity.
6.2. Future directions
Even though significant progress has been made in describing symptom presentation of HPD and SPD, further research is warranted. For
example, clinical lore suggests that perfectionistic experiences are common in SPD and HPD (Arnold et al., 1998; Fruensgaard, 1984; Gupta,
Gupta, & Schork, 1996; Swedo et al., 1992), but empirical data are lacking (although some data concerning picking/pulling to obtain symmetry
have been collected, Tucker et al., 2011; Woods, Flessner, et al., 2006). In
addition to investigating the commonality in symptoms, a potentially
fruitful approach is to identify shared underlying psychological,
neurocognitive or psychobiological processes. For example, investigating psychophysiological or psychocutaneous processes involved in affective experience surrounding body grooming may prove fruitful. Other
researchers have suggested that HPD and SPD may have overlapping deficits in affective regulation, inhibitory control and processes involving reward/addiction (Stein et al., 2006). Given preliminary evidence for a
shared genetic risk between SPD and HPD, it may be useful to investigate
whether deficits in some underlying processes represent a shared
endophenotype (Chamberlain et al., 2005).
Another useful approach to shed light on the relationship between
SPD and HPD is to investigate different explanatory models of comorbidity (e.g., partly or fully shared etiology, one disorder causes the other,
etc.). By quantifying data from epidemiological studies, longitudinal family studies or twin studies, researchers are increasingly able to test hypotheses concerning causes of comorbidity (Klein & Riso, 1993; Neale &
Kendler, 1995). These methods typically require large sample sizes but
can be helpful in understanding the relationship between SPD and HPD.
Finally, understanding the differences between HPD and SPD may
provide unique insights into the etiology of either or both conditions.
There are at least four lines of research suggested by the current literature. First, one study found that dermatological problems often preceded
the development of SPD (Wilhelm et al., 1999), and it is possible that
these types of problems serve as a higher risk for SPD than HPD. Second,
in a preliminary study involving few participants, it was found that SPD
patients, but not HPD patients, showed enhanced response to an opiate
sensitivity test, suggesting a difference between the disorders with regard
to the role of endogenous opiates (Frecska & Arato, 2002). Third, given
data showing a higher prevalence of SPD secondary to BDD, than HPD
secondary to BDD (Grant et al., 2006), it may be that appearance concerns
are more of a risk for SPD than HPD. Fourth, Bienvenu et al. (2009) discovered independent as well as shared genetic underpinning associated with
HPD and SPD. Likewise, the family history studies showed that relatives
of HPD patients were more likely to have HPD than SPD, and relatives
of SPD patients were more likely to have SPD than HPD. Thus, future studies may want to investigate familial environment or a genetic underpinning that differently affects the risk for the two disorders.
6.3. Implications for research and practice
The findings from the current review have nosological implications.
Given the evidence for co-occurrence of HPD and SPD in clinical samples
along with data showing relatedness in clinical characteristics and response to the same treatment (e.g., habit reversal), it seems appropriate
to categorize the two disorders in the same overall category in DSM and
ICD. The possibility that HPD and SPD share etiological mechanisms provides further support for these nosological arrangements. As to the
question of what general category the two disorders fit best, our review
concurs with the preliminary recommendation of the APA work group
(Stein et al., 2010) that the two disorders should optimally be classified
in an overall category of BFRB. Consistent with this view are data showing high comorbidity between different BFRBs, similarities in phenomenology (e.g., arousal regulation) and genetic associations.
Other classification schemes may also have validity. Some authors
have argued that SPD and HPD are heterogeneous conditions that can
be conceptualized as part of the putative obsessive–compulsive spectrum (Ferrão, Miguel, & Stein, 2009; Stein et al., 1995), and others have
suggested classifying SPD patients according how much their symptoms
involve impulsive and compulsive features (Arnold et al., 2001). Our review showed that the majority of patients in both groups endorse
I. Snorrason et al. / Clinical Psychology Review 32 (2012) 618–629
impulsive symptoms (i.e., preceding arousal and subsequent gratification), but data concerning compulsivity is less clear (Ferrão, Almeida,
Bedin, Rosa, & Busnello, 2006). Nonetheless, there appears to be some affinity between HPD/SPD and compulsive disorders (OCD and BDD) that
warrants further research attention (Ferrão et al., 2009). Similarly, despite evidence for impulsive features, further studies are needed to investigate the relationship between SPD/HPD and other disorders
involving impulsivity (Grant, Odlaug, & Potenza, 2007; Odlaug & Grant,
2010; Snorrason et al., 2011).
Our review also has implications for research. Shared etiology would
suggest that researchers investigating the etiology of either disorder
might benefit from considering the other one too. Comparing and contrasting findings from studies on SPD and HPD may provide unique insights into the etiology of either or both disorders, and information
concerning one disorder could guide research on the other. Moreover,
a failure to consider the other disorder when studying etiological factors
in either one may result in loss of power. For example, if the disorders
share etiology, then failure to screen for both disorders when selecting
healthy controls may obscure group differences. Finally, given that HPD
and SPD serve similar functions (e.g., affect/arousal regulation), clinicians and researchers investigating treatment may want to consider
the possibility of symptom substitution and monitor changes in both
behaviors when treating comorbid cases.
References
American Psychiatric Association (2000). Diagnostic and statistical manual of mental
disorders (4th ed., text revision). Washington, DC: American Psychiatric Association.
Arbabi, M., Farnia, V., Balighi, K., Mohammadi, M. R., Nejati-Safa, A. A., Yazdchi, K., et al.
(2008). Efficacy of citalopram in treatment of pathological skin picking, a randomized double blind placebo controlled trial. Acta Medica Iranica, 46, 367–372.
Arnold, L. M., Auchenbach, M. B., & McElroy, S. L. (2001). Psychogenic excoriation:
Clinical features, proposed diagnostic criteria, epidemiology and approaches to
treatment. CNS Drugs, 15, 351–359.
Arnold, L. M., McElroy, S. L., Mutasim, D. F., Dwight, M. M., Lamerson, C. L., & Morris, E. M.
(1998). Characteristics of 34 adults with psychogenic excoriation. The Journal of Clinical Psychiatry, 59, 509–514.
Bienvenu, O. J., Samuels, J. F., Riddle, M. A., Hoehn-Saric, R., Liang, K. Y., Cullen, B. A.,
et al. (2000). The relationship of obsessive–compulsive disorder to possible spectrum disorders: Results from a family study. Biological Psychiatry, 48, 287–293.
Bienvenu, O. J., Wang, Y., Shugart, Y. Y., Welch, J. M., Grados, M. A., Fyer, A. J., et al. (2009).
Sapap3 and pathological grooming in humans: Results from the OCD collaborative
genetics study. American Journal of Medical Genetics. Part B, Neuropsychiatric Genetics,
150B, 710–720.
Bloch, M. R., Elliot, M., Thompson, H., & Koran, L. M. (2001). Fluoxetine in pathological
skin picking: Open-label and double-blind results. Psychosomatics, 42, 314–319.
Bloch, M. H., Landeros-Weisenberger, A., Dombrowski, P., Kelmendi, B., Wegner, R.,
Nudel, J., et al. (2007). Systematic review: Pharmacological and behavioral treatment for trichotillomania. Biological Psychiatry, 62, 839–846.
Boardman, L., van der Mewre, L., Lochner, C., Kinnear, C. J., Seedat, S., Stein, D. J., et al.
(2011). Investigating SAPAP3 variants in the etiology of obsessive–compulsive disorder and trichotillomania in the South African white population. Comprehensive
Psychiatry, 52, 181–187.
Bohne, A., Keuthen, N., & Wilhelm, S. (2005). Pathological hair pulling, skin picking,
and nail biting. Annals of Clinical Psychiatry, 17, 227–232.
Bohne, A., Savage, C. R., Deckersbach, T., Keuthen, N. J., & Wilhelm, S. (2008). Motor inhibition in trichotillomania and obsessive–compulsive disorder. Journal of Psychiatric
Research, 42, 141–150.
Bohne, A., Wilhelm, S., Keuthen, N. J., Baer, L., & Jenike, M. A. (2002). Skin picking in
German students: Prevalence, phenomenology, and associated characteristics. Behavior Modification, 26, 320–339.
Bordnick, P. S., Thyer, B. A., & Ritchie, B. W. (1994). Feather picking disorder and trichotillomania: An avian model of human psychopathology. Journal of Behavior Therapy
and Experimental Psychiatry, 25, 189–196.
Boughn, S., & Holdom, J. J. (2003). The relationship of violence and trichotillomania.
Journal of Nursing Scholarship, 35, 165–170.
Calikusu, C., Yucel, B., Polat, A., & Baykal, C. (2003). The relation of psychogenic excoriation
with psychiatric disorders: A comparative study. Comprehensive Psychiatry, 44, 256–261.
Chamberlain, S. R., Blackwell, A. D., Fineberg, N. A., Robbins, T. W., & Sahakia, B. J.
(2005). The neuropsychology of obsessive compulsive disorder: The importance
of failures in cognitive and behavioural inhibition as candidate endophenotypic
markers. Neuroscience and Biobehavioral Reviews, 29, 399–419.
Chamberlain, S. R., Fineberg, N. A., Blackwell, A. D., Clark, L., Robbins, T. W., & Sahakian,
B. J. (2007). A neuropsychological comparison of obsessive–compulsive disorder
and trichotillomania. Neuropsychologia, 45, 654–662.
Chamberlain, S. R., Fineberg, N. A., Blackwell, A. D., Robbins, T. W., & Sahakian, B. J.
(2006). Motor inhibition and cognitive flexibility in obsessive–compulsive disorder and trichotillomania. The American Journal of Psychiatry, 163, 1282–1284.
627
Chamberlain, S. R., Hampshire, A., Menzies, L. A., Garryfalladis, E., Grant, J. E., Odlaug, B. L.,
et al. (2010). Reduced brain white matter integrity in trichotillomania: A diffusion
tensor imaging study. Archives of General Psychiatry, 67, 965–971.
Chamberlain, S. R., Menzies, L. A., Fineberg, N. A., Del Campo, N., Suckling, J., Craig, K.,
et al. (2008). Grey matter abnormalities in trichotillomania: Morphometric magnetic resonance imaging study. The British Journal of Psychiatry, 193, 216–221.
Chamberlain, S. R., Odlaug, B. L., Boulougouris, V., Fineberg, N. A., & Grant, J. E. (2009).
Trichotillomania: Neurobiology and treatment. Neuroscience and Biobehavioral
Reviews, 33, 831–842.
Christenson, G. A. (1995). Medical complications of trichotillomania. In syllabus and
proceedings summary of the 148th annual meeting of the American Psychiatric Association, USA, 158.
Christenson, G. A., Chernoff-Clementz, E., & Clementz, B. A. (1992). Personality and clinical
characteristics in patients with trichotillomania. The Journal of Clinical Psychiatry, 53,
407–413.
Christenson, G. A., Mackenzie, T. B., & Mitchell, J. E. (1991). Characteristics of 60 adult
chronic hair pullers. The American Journal of Psychiatry, 148, 365–370.
Christenson, G. A., Mackenzie, T. B., Mitchell, J. E., & Callies, A. L. (1991). A
placebo-controlled, double-blind crossover study of fluoxetine in trichotillomania.
The American Journal of Psychiatry, 148, 1566–1571.
Christenson, G. A., & Mackinzie, T. B. (1995). Trichotillomania, body dysmorphic disorder,
and obsessive–compulsive disorder. The Journal of Clinical Psychiatry, 56, 211–212.
Christenson, G. A., & Mansueto, C. S. (1999). Trichotillomania: Descriptive characteristics and phenomenology. In D. J. Stein, G. Christenson, & E. Hollander (Eds.),
Trichotillomania (pp. 1–41). Washington, DC: American Psychiatric Press.
Christenson, G. A., Ristvedt, S. L., & Mackenzie, T. B. (1993). Identification of trichotillomania cue profiles. Behaviour Research and Therapy, 31, 315–320.
Cohen, L. J., Stein, D. J., Simeon, D., Spadaccini, E., Rosen, J., Aronowitz, B., et al. (1995).
Clinical profile, comorbidity, and treatment history in 123 hair pullers: A survey
study. The Journal of Clinical Psychiatry, 56, 319–326.
Cullen, B. A., Samuels, J. F., Bienvenu, O. J., Grados, M., Hoehn-Saric, R., Hahn, J., et al.
(2001). The relationship of pathologic skin picking to obsessive–compulsive disorder. The Journal of Nervous and Mental Disease, 189, 193–195.
Diefenbach, G. J., Mouton-Odum, S., & Stanley, M. A. (2002). Affective correlates of
trichotillomania. Behavior Research and Therapy, 40, 1305–1315.
Diefenbach, G. J., Tolin, D. F., Hannan, S., Crocetto, J., & Worhunsky, P. (2005). Trichotillomania: Impact on psychosocial functioning and quality of life. Behavior Research
and Therapy, 43, 869–884.
Diefenbach, G. J., Tolin, D. F., Meunier, S., & Worhunsky, P. (2008). Emotion regulation
and trichotillomania: A comparison of clinical and nonclinical hair pulling. Journal
of Behavior Therapy and Experimental Psychiatry, 39, 32–41.
du Toit, P. L., van Kradenburg, J., Niehaus, D. J. H., & Stein, D. J. (2001). Characteristics
and phenomenology of hair-pulling: An exploration of subtypes. Comprehensive
Psychiatry, 42, 247–256.
Duke, D. C., Bodzin, D. K., Tavares, P., Geffken, G. R., & Storch, E. A. (2009). The phenomenology of hairpulling in a community sample. Journal of Anxiety Disorders, 23, 1118–1125.
Duke, D. C., Kelley, M. L., Ricketts, E. J., Geffken, G. R., & Storch, E. A. (2010). The phenomenology of hairpulling in college students. Journal of Psychopathology and
Behavioral Assessment, 32, 281–292.
Evans, B. (1976). A case of trichotillomania in a child treated in a home token program.
Journal of Behavior Therapy and Experimental Psychiatry, 7, 197–198.
Favaro, A., Ferrara, S., & Santonastaso, P. (2007). Self-injurious behavior in a community sample of young women: Relationship with childhood abuse and other types of
self-damaging behaviors. The Journal of Clinical Psychiatry, 68, 122–131.
Ferrão, Y. A., Almeida, V. P., Bedin, N. R., Rosa, R., & Busnello, E. D. (2006). Impulsivity and
compulsivity in patients with trichotillomania or skin picking compared with patients
with obsessive–compulsive disorder. Comprehensive Psychiatry, 47, 282–288.
Ferrão, Y. A., Miguel, E., & Stein, D. J. (2009). Tourette's syndrome, trichotillomania, and
obsessive–compulsive disorder: How closely are they related? Psychiatry Research,
170, 32–42.
Flessner, C. A., Busch, A. M., Heideman, P. W., & Woods, D. W. (2008). Acceptanceenhanced behavior therapy (AEBT) for trichotillomania and chronic skin picking: Exploring the effects of component sequencing. Behavior Modification, 32, 579–594.
Flessner, C. A., Conelea, C. A., Woods, D. W., Franklin, M. E., Keuthen, N. J., & Cashin, S. E.
(2008). Styles of pulling in trichotillomania: Exploring differences in symptom severity,
phenomenology, and functional impact. Behaviour Research and Therapy, 46, 345–357.
Flessner, C. A., & Woods, D. W. (2006). Phenomenological characteristics, social problems,
and the economic impact associated with chronic skin picking. Behavior Modification,
30, 944–963.
Fontenelle, L. F., Mendlowicz, M. V., Mussi, T. C., Marques, C., & Versiani, M. (2002). The
man with the purple nostrils: a case of rhinotrichotillomania secondary to body
dysmorphic disorder. Acta Psychiatrica Scandinavica, 106, 464–466.
Franklin, M. E., Flessner, C. A., Woods, D. W., Keuthen, N. J., Piacentini, J. C., Moore, P.,
et al. (2008). The child and adolescent trichotillomania impact project: Descriptive
psychopathology, comorbidity, functional impairment, and treatment utilization.
Journal of Developmental Behavior Pediatrics, 29, 1–8.
Frecska, E., & Arato, M. (2002). Opiate sensitivity test in patients with stereotypic
movement disorder and trichotillomania. Progress in Neuro-Psychopharmacology
& Biological Psychiatry, 26, 909–912.
Fruensgaard, K. (1984). Neurotic excoriations: A controlled psychiatric examination.
Acta Psychiatrica Scandinavica, 69(Suppl. 312), 1–52.
Gershuny, B. S., Keuthen, N. J., Gentes, E. L., Russo, A. R., Emmott, E. C., & Jameson, M.
(2006). Current posttraumatic stress disorder and history of trauma in trichotillomania. Journal of Clinical Psychology, 62, 1521–1529.
Grachev, I. D. (1997). MRI-based morphometric topographic parcellation of human
neocortex in trichotillomania. Psychiatry and Clinical Neurosciences, 51, 315–321.
628
I. Snorrason et al. / Clinical Psychology Review 32 (2012) 618–629
Grant, J. E., Levine, L., Kim, D., & Potenza, M. N. (2005). Impulse control disorders in
adult psychiatric inpatients. The American Journal of Psychiatry, 162, 2184–2188.
Grant, J. E., Mancebo, M. C., Eisen, J. L., & Rasmussen, S. A. (2010). Impulse-control disorders in children and adolescents with obsessive–compulsive disorder. Psychiatry
Research, 30, 109–113.
Grant, J. E., Menard, W., & Phillips, K. A. (2006). Pathological skin picking in individuals
with body dysmorphic disorder. General Hospital Psychiatry, 28, 487–493.
Grant, J. E., Odlaug, B. L., & Chamberlain, S. R. (2011). A cognitive comparison of pathological skin picking and trichotillomania. Journal of Psychiatric Research, 45,
1634–1638.
Grant, J. E., Odlaug, B. L., Chamberlain, S. R., & Kim, S. W. (2010). A double-blind,
placebo-controlled trial of Lamotrigine for pathological skin picking: Treatment
efficacy and neurocognitive predictors of response. Journal of Clinical Psychopharmacology, 30, 396–403.
Grant, J. E., Odlaug, B. L., & Kim, S. W. (2007). Lamotrigine treatment of pathologic skin
picking: An open-label study. Journal of Clinical Psychology, 68, 1384–1391.
Grant, J. E., Odlaug, B. L., & Kim, S. W. (2009). N-acetylcysteine, a glutamate modulator,
in the treatment of trichotillomania: A double-blind, placebo-controlled study.
Archives of General Psychiatry, 66, 756–763.
Grant, J. E., Odlaug, B. L., & Kim, S. W. (2010). A clinical comparison of pathologic skin picking and obsessive–compulsive disorder. Comprehensive Psychiatry, 51, 347–352.
Grant, J. E., Odlaug, B. L., & Potenza, M. N. (2007). Addicted to hair pulling? How an alternate model of trichotillomania may improve treatment outcome. Harvard Review of
Psychiatry, 15, 80–85.
Grant, J. E., Williams, K. W., & Potenza, M. N. (2007). Impulse-control disorders in adolescent psychiatric inpatients: Co-occurring disorders and sex differences. The
Journal of Clinical Psychiatry, 68, 1584–1594.
Gupta, M. A., Gupta, A. K., & Haberman, H. F. (1986). Neurotic excoriations: A review
and some new perspectives. Comprehensive Psychiatry, 27, 381–386.
Gupta, M. A., Gupta, A. K., & Schork, N. J. (1996). Psychological factors affecting
self-excoriative behavior in women with mild-to-moderate facial acne vulgaris.
Psychosomatics, 37, 127–130.
Hajcak, G., Franklin, M. E., Simons, R. F., & Keuthen, N. J. (2006). Hairpulling and skin
picking in relation to affective distress and obsessive–compulsive symptoms.
Journal of Psychopathology and Behavioural Assessment, 28, 179–187.
Hallopeau, H. (1989). Alopecie par grattage (trichomanie ou trichotillomanie). Annales
de Dermatologie et de Syphiligraphie, 10, 440–441.
Hasler, G., Pinto, A., Greenberg, B. D., Samuels, J., Fyer, A. J., Pauls, D., et al. (2007).
Familiality of factor analysis-derived YBOCS dimensions in OCD-affected siblings
pairs from the OCD collaborative genetics study. Biological Psychiatry, 61, 617–625.
Hoppe, L. J., Ipser, J., Lochner, C., Thomas, K. G. F., & Stein, D. J. (2010). Should there be a
category: “Grooming disorders?”. In A. V. Kalueff, J. L. LaPorte, & C. L. Bergner
(Eds.), Neurobiology of grooming behavior (pp. 226–251). Cambridge, UK:
Cambridge University Press.
Iancu, I., Weizman, A., Kindler, S., Sasson, Y., & Zohar, J. (1996). Serotonergic drugs in
trichotillomania: Treatment results in 12 patients. The Journal of Nervous and
Mental Disease, 184, 641–644.
Keuthen, N. J., Deckersbach, T., Wilhelm, S., Hale, E., Fraim, C., Baer, L., et al. (2000).
Repetitive skin-picking in a student population and comparison with a sample of
self-injurious skin-pickers. Psychosomatics, 41, 210–215.
Keuthen, N. J., Jameson, M., Loh, R., Deckersbach, T., Wilhelm, S., & Dougherty, D. D.
(2007). Open-label escitalopram treatment for pathological skin picking. International Clinical Psychopharmacology, 22, 268–274.
Keuthen, N. J., Makris, N., Schlerf, J. E., Martis, B., Savage, C. R., McMullin, K., et al.
(2007). Evidence for reduced cerebellar volumes in trichotillomania. Biological
Psychiatry, 61, 374–381.
Keuthen, N. J., Rothbaum, B. O., Welch, S. S., Taylor, C., Falkenstein, M., Heekin, M., et al.
(2010). Pilot trial of dialectical behavior therapy-enhanced habit reversal for
trichotillomania. Depression and Anxiety, 27, 953–959.
King, R. A., Scahill, L., Vitulano, L. A., Schwab-Stone, M., Tercyak, K. P., & Riddle, M. A.
(1995). Childhood trichotillomania: clinical phenomenology, comorbidity, and
family genetics. Journal of the American Academy of Child and Adolescent Psychiatry,
34, 1451–1459.
Klein, D. N., & Riso, L. P. (1993). Psychiatric disorders: Problems of boundaries and comorbidity. In C. G. Costello (Ed.), Basic issues in psychopathology (pp. 19–66). New
York: Guilford Press.
LaSalle, V. H., Cromer, K. R., Nelson, K. N., Kazuba, D., Justement, L., & Murphy, D. L. (2004).
Diagnostic interview assessed neuropsychiatric disorder comorbidity in 334 individuals with obsessive–compulsive disorder. Depression and Anxiety, 19, 163–173.
Lee, J. A., Kim, C. K., Jahng, G. H., Hwang, Y. W., Cho, Y. J., Kim, W. H., et al. (2010). A pilot
study of brain activation in children with trichotillomania during a visual–tactile
symptom provocation task: A functional magnetic resonance imaging study. Progress in Neuro-Psychopharmocology & Biological Psychiatry, 34, 1250–1258.
Lenane, M. C., Swedo, S. E., Rapoport, J. L., Leonard, H., Sceery, W., & Guroff, J. J. (1992).
Rates of obsessive compulsive disorder in first degree relatives of patients with trichotillomania: A research note. Journal of Child Psychology and Psychiatry, 33, 925–933.
Lewin, A. B., Piacentini, J., Flessner, C. A., Woods, D. W., Franklin, M. E., Keuthen, N. J.,
et al. (2009). Depression, anxiety, and functional impairment in children with
trichotillomania. Depression and Anxiety, 26, 521–527.
Lochner, C., du Toit, P. L., Zungu-Dirwayi, N., Marais, A., van Kradenburg, J., Seedat, S., et al.
(2002). Childhood trauma in obsessive–compulsive disorder, trichotillomania, and
controls. Depression and Anxiety, 15, 66–68.
Lochner, C., Simeon, D., Niehaus, D. J., & Stein, D. J. (2002). Trichotillomania and skin
picking: A phenomenological comparison. Depression and Anxiety, 15, 83–86.
Lochner, C., Seedat, S., & Stein, D. J. (2010). Chronic hair-pulling: Phenomenology-based
subtypes. Journal of Anxiety Disorders, 24, 196–202.
Lovato, L., Ferrão, Y. A., Stein, D. J., Shavitt, R. G., Fontenelle, L. F., Vivan, A., et al. (2012).
Skin picking and trichotillomania in adults with obsessive–compulsive disorder.
Comprehensive Psychiatry, 53, 562–568.
Malhorta, S., Grover, S., Baweja, R., & Bhateja, G. (2008). Trichotillomania in children.
Indian Pediatrics, 45, 403–405.
Mansueto, C. S., Townsley-Stemberger, R. M., Thomas, A., & Golomb, R. (1997). Trichotillomania: A comprehensive behavioral model. Clinical Psychology Review, 17, 567–577.
Martin, A., Pigott, T. A., Lalonde, F. M., Dalton, I., Dubbert, B., & Murphy, D. L. (1993).
Lack of evidence for Huntingtons disease-like cognitive dysfunction in obsessive–
compulsive disorder. Biological Psychiatry, 33, 345–353.
McCarley, N. G., Spirrison, C. L., & Ceminsky, J. L. (2002). Hair pulling behavior reported
by African American and non African American college students. Journal of Psychopathology and Behavioral Assessment, 24, 139–144.
Meunier, S. A., Tolin, D. F., & Franklin, M. (2009). Affective and sensory correlates of hair
pulling in pediatric trichotillomania. Behavior Modification, 33, 396–407.
Miguel, E. C., Ferrao, Y. A., Rosario, M. C., Mathis, M. A., Torres, A. R., & Fontenelle, L. F. (2008).
The Brazilian research consortium on obsessive compulsive spectrum disorders: Recruitment, assessment instruments, methods for the development of multicenter collaborative studies and preliminary results. Brazilian Journal of Psychiatry, 30, 185–196.
Moon-Fanelli, A. A., Dodman, N. H., & O'Sullivan, R. L. (1999). Veterinary models of
compulsive selfgrooming: Parallels with trichotillomania. In D. J. Stein, G. A.
Christenson, & Hollander (Eds.), Trichotillomania (pp. 63–92). Washington, D.C.:
American Psychiatric Press, Inc.
Morales-Fuentes, B., Camacho-Maya, U., Coll-Clemente, F. L., & Vázquez-Minero, J. C.
(2010). Trichotillomania, recurrent trichobezoar and rapunzel syndrome: Case report and literature review. Cirugiay Cirujanos, 78, 265–266.
Müller, A., Rein, K., Kollei, I., Jacobi, A., Rotter, A., Schütz, P., et al. (2011). Impulse control disorders in psychiatric inpatients. Psychiatry Research, 15, 434–438.
Murphy, C., Redenius, R., O'Neill, E., & Zallek, S. (2007). Sleep-isolated trichotillomania:
A survey of dermatologists. Journal of Clinical Sleep Medicine, 3, 719–721.
Neal-Barnett, A. M., & Stadulis, R. (2006). Affective states and racial identity among
African American women with trichotillomania. Journal of the National Medical
Association, 98, 753–757.
Neale, M. C., & Kendler, K. S. (1995). Models of comorbidity for multifactorial disorders.
American Journal of Human Genetics, 57, 935–953.
Neziroglu, F., Rabinowitz, D., Breytman, A., & Jacofsky, M. (2008). Skin picking phenomenology and severity comparison. The Primary Care Companion to the Journal of
Clinical Psychiatry, 10, 306–312.
Norberg, M. M., Wetterneck, C. T., Woods, D. W., & Conelea, C. A. (2007). Experiential
avoidance as a mediator of relationships between cognitions and hair-pulling severity. Behavior Modification, 31, 367–381.
Novak, C. E., Keuthen, N. J., Stewart, S. E., & Pauls, D. L. (2009). A twin concordance study of
trichotillomania. American Journal of Medical Genetics Part B, 150B, 944–949.
O'Sullivan, R. L., Phillips, K. A., Keuthen, N. J., & Wilhelm, S. (1999). Near-fatal skin picking from delusional body dysmorphic disorder responsive to fluvoxamine. Psychosomatics, 40, 79–81.
Odlaug, B. L., Chamberlain, S. R., & Grant, J. E. (2010). Motor inhibition and cognitive
flexibility in pathologic skin picking. Progress in Neuro-Psychopharmacology &
Biological Psychiatry, 34, 208–211.
Odlaug, B. L., & Grant, J. E. (2007). N-acetyl cysteine in the treatment of grooming disorders. Journal of Clinical Psychopharmacology, 27, 227–229.
Odlaug, B. L., & Grant, J. E. (2008a). Clinical characteristics and medical complications of
pathologic skin picking. General Hospital Psychiatry, 30, 61–66.
Odlaug, B. L., & Grant, J. E. (2008b). Trichotillomania and pathological skin picking: Clinical
comparison with an examination of comorbidity. Annals of Clinical Psychiatry, 20, 57–63.
Odlaug, B. L., & Grant, J. E. (2010). Pathological skin picking. The American Journal of
Drug and Alcohol Abuse, 36, 296–303.
Odlaug, B. L., & Grant, J. E. (2012). Pathological skin picking. In J. E. Grant, D. J. Stein,
D. W. Woods, & N. J. Keuthen (Eds.), Trichotillomania, skin picking and other bodyfocused repetitive behaviors (pp. 21–41). Washington, DC: American Psychiatric
Publishing, Inc.
Odlaug, B. L., Kim, S. W., & Grant, J. E. (2010). Quality of life and clinical severity in
pathological skin picking and trichotillomania. Journal of Anxiety Disorders, 24,
823–829.
O'Sullivan, R. L., Rauch, S. L., Breiter, H. C., Grachev, I. D., Baer, L., & Kennedy, D. N.
(1997). Reduced basal ganglia volumes in trichotillomania measured via morphometric magnetic resonance imaging. Biological Psychiatry, 42, 39–45.
Penzel, F. (2003). The hair-pulling problem: A complete guide to trichotillomania. New
York: Oxford University Press.
Phillips, K. A., & McElroy, S. L. (1992). Dr. Phillips and Dr. McElroy reply. The American
Journal of Psychiatry, 149, 1284.
Phillips, K. A., & Taub, S. L. (1995). Skin picking as a symptom of body dysmorphic disorder. Psychopharmacology Bulletin, 31, 279–288.
Rauch, S. L., Wright, C. I., Savage, C. R., Martis, B., McMullin, K. G., Wedig, M. M., et al.
(2007). Brain activation during implicit sequence learning in individuals with
trichotillomania. Psychiatry Research, 154, 233–240.
Reeve, E. A., Bernstein, G., & Christenson, G. A. (1992). Clinical characteristics and psychiatric comorbidity in children with trichotillomania. Journal of American Academic Child and Adolescent Psychiatry, 31, 132–138.
Robins, E., & Guze, S. B. (1970). Establishment of diagnostic validity in psychiatric illness:
Its application to schizophrenia. The American Journal of Psychiatry, 126, 983–987.
Santhanam, R., Fairley, M., & Rogers, M. (2008). Is it trichotillomania? Hair pulling in childhood: A developmental perspective. Clinical Child Psychology and Psychiatry, 13,
409–418.
Sarkhel, S., Praharaj, S. K., & Akhtar, S. (2011). Cheek-biting disorder: Another stereotypic movement disorder? Journal of Anxiety Disorders, 25, 1085–1086.
I. Snorrason et al. / Clinical Psychology Review 32 (2012) 618–629
Schlosser, S., Black, D. W., Blum, N., & Goldstein, R. B. (1994). The demography, phenomenology, and family history of 22 persons with compulsive hair pulling. Annals
of Clinical Psychiatry, 6, 147–152.
Schuck, K., Keijsers, G. P., & Rinck, M. (2011). The effects of brief cognitive-behaviour
therapy for pathological skin picking: A randomized comparison to wait-list control. Behaviour Research and Therapy, 49, 11–17.
Shusterman, A., Feld, L., Baer, L., & Keuthen, N. (2009). Affective regulation in trichotillomania: Evidence from a large-scale internet survey. Behaviour Research and Therapy, 47, 637–644.
Simeon, D., Cohen, L. J., Stein, D. J., Schmeidler, J., Spadaccini, E., & Hollander, E. (1997).
Comorbid self-injurious behaviors in 71 female hair-pullers: a survey study. Journal of Nervous and Mental Disease, 185, 117–119.
Simeon, D., Stein, D. J., Gross, S., Islam, N., Schmeidler, J., & Hollander, E. (1997). A
double-blind trial of fluoxetine in pathological skin picking. The Journal of Clinical
Psychiatry, 58, 341–347.
Singareddy, R., Moin, A., Spurlock, L., Merritt-Davis, O., & Uhde, T. W. (2003). Skin picking and sleep disturbances: Relationship to anxiety and need for research. Depression and Anxiety, 18, 228–232.
Snorrason, I., Smari, J., & Olafsson, R. P. (2010). Emotion regulation in pathological skin
picking: Findings from a non-treatment seeking sample. Journal of Behavior Therapy and Experimental Psychiatry, 41, 238–245.
Snorrason, I., Smari, J., & Olafsson, R. P. (2011). Motor inhibition, reflection impulsivity
and trait impulsivity in pathological skin picking. Behavior Therapy, 42, 521–532.
Soriano, J. L., O'Sullivan, R. L., Baer, L., Phillips, K. A., McNally, R. J., & Jenike, M. A. (1996).
Trichotillomania and self-esteem: A survey of 62 female hair pullers. The Journal of
Clinical Psychiatry, 57, 77–82.
Stanley, M. A., & Cohen, L. J. (1999). Trichotillomania and obsessive–compulsive disorder. In D. J. Stein, G. A. Christenson, & E. Hollander (Eds.), Trichotillomania
(pp. 225–261). Washington, DC: American Psychiatric Press.
Stanley, M. A., Hannay, H. J., & Breckenridge, J. K. (1997). The neuropsychology of
trichotillomania. Journal of Anxiety Disorders, 11, 473–488.
Stein, D. J., Chamberlain, S. R., & Fineberg, N. (2006). An A-B-C model of habit disorders:
Hair-pulling, skin-picking, and other stereotypic conditions. CNS Spectrums, 11, 824–827.
Stein, D. J., Coetzer, R., Lee, M., Davids, B., & Bouwer, C. (1997). Magnetic resonance
brain imaging in women with obsessive–compulsive disorder and trichotillomania. Psychiatry Research, 74, 177–182.
Stein, D. J., Flessner, C. A., Franklin, M., Keuthen, N. J., Lochner, C., & Woods, D. W.
(2008). Is trichotillomania a stereotypic movement disorder? An analysis of
body focused repetitive behaviors in people with hair pulling. Annals of Clinical
Psychiatry, 20, 194–198.
Stein, D. J., Grant, J. E., Franklin, M. E., Keuthen, N., Lochner, C., Singer, H. S., et al. (2010).
Trichotillomania (hair pulling disorder), skin picking disorder, and stereotypic
movement disorder: Toward DSM-V. Depression and Anxiety, 27, 611–626.
Stein, D. J., Hutt, C. S., Spitz, J. L., & Hollander, E. (1993). Compulsive picking and obsessive–compulsive disorder. Psychosomatics, 34, 177–180.
Stein, D. J., Mullen, L., Islam, M. N., Cohen, L., DeCaria, C. M., & Hollander, E. (1995). Compulsive and impulsive symptomatology in trichotillomania. Psychopathology, 28,
208–213.
Swedo, S. E., & Leonard, H. L. (1992). Trichotillomania. An obsessive compulsive spectrum disorder? Psychiatric Clinics of North America, 15, 777–790.
Swedo, S. E., Leonard, H. L., Lenane, M. C., & Rettwe, D. C. (1992). Trichotillomania a profile
of the disorder from infancy through adulthood. International Pediatrics, 7, 144–150.
Swedo, S. E., Rapoport, J. L., Leonard, H. L., Schapiro, M. B., Rapoport, S. I., & Grady, C. L.
(1991). Regional cerebral glucose metabolism of women with trichotillomania.
Archives of General Psychiatry, 48, 828–833.
Tamam, L., Zengin, M., Karakus, G., & Ozturk, Z. (2008). Impulse control disorders in an inpatient psychiatric unit of a university hospital. Klinik Psikofarmakiloji Bulteni, 18,
153–161.
629
Tanquary, J. (1994). Trichotillomania and body dysmorphic disorder. The Journal of
Clinical Psychiatry, 55, 35.
Tanquary, J., Lynch, M., & Masand, P. (1992). Obsessive–compulsive disorder in relation
to body dysmorphic disorder. The American Journal of Psychiatry, 149, 1283–1284.
Tay, Y., Levy, M. L., & Metry, D. W. (2004). Trichotillomania in childhood: Case series
and review. Pediatrics, 113, 494–498.
Teng, E. J., Woods, D. W., Marcks, B. S., & Twohig, M. P. (2004). Body-focused repetitive
behaviors: The proximal and distal effects of affective variables on behavioral expression. Journal of Psychopathology and Behavioral Assessment, 26, 55–64.
Teng, E. J., Woods, D. W., & Twohig, M. P. (2006). Habit reversal as a treatment for
chronic skin picking. Behavior Modification, 30, 422–441.
Teng, E. J., Woods, D. W., Twohig, M. P., & Marcks, B. A. (2002). Body-focused repetitive
behavior problems: Prevalence in a nonreferred population and differences in perceived somatic activity. Behavior Modification, 26, 340–360.
Tucker, B. T., Woods, D. W., Flessner, C. A., Franklin, S. A., & Franklin, M. E. (2011). The
skin picking impact project: Phenomenology, interference, and treatment utilization of pathological skin picking in a population based sample. Journal of Anxiety
Disorders, 25, 88–95.
Twohig, M. P., Hayes, S. C., & Masuda, A. (2006). A preliminary investigation of acceptance and commitment therapy as a treatment for chronic skin picking. Behaviour
Research and Therapy, 44, 1513–1522.
van Ameringen, M., Mancini, C., Patterson, B., Bennett, M., & Oakman, J. (2010). A randomized, double-blind, placebo-controlled trial of olanzapine in the treatment of
trichotillomania. The Journal of Clinical Psychiatry, 71, 1336–1343.
van Minnen, A., Hoogduin, K. A., Keijsers, G. P., Hellenbrand, I., & Hendriks, G. J. (2003).
Treatment of trichotillomania with behavioral therapy or fluoxetine: A randomized, waiting-list controlled study. Archives of General Psychiatry, 60, 517–522.
Walther, M. R., Flessner, C. A., Conelea, C. A., & Woods, D. W. (2009). The Milwaukee
inventory for the dimensions of adult skin picking (MIDAS): Initial development
and psychometric properties. Journal of Behavior Therapy and Experimental Psychiatry, 40, 127–135.
Welch, J. M., Lu, J., Rodriguiz, R. M., Trotta, N. C., Peca, J., Ding, J. D., et al. (2007).
Cortico-striatal synaptic defects and OCD-like behaviours in Sapap3-mutant
mice. Nature, 448, 894–900.
Wells, J. H., Haines, J., Williams, C. L., & Brain, K. L. (1999). The self-mutilative nature of
severe onychophagia: A comparison with self-cutting. Canadian Journal of Psychiatry, 44, 40–47.
Wetterneck, C. T., Woods, D. W., Norberg, M. M., & Begotka, A. M. (2006). The social and
economic impact of trichotillomania. Behavioral Interventions, 21, 97–109.
Wilhelm, S., Keuthen, N. J., Deckersbach, T., Engelhard, I. M., Forker, A. E., Bear, L., et al.
(1999). Self-injurious skin picking: Clinical characteristics and comorbidity. The
Journal of Clinical Psychiatry, 60, 454–459.
Wilson, E. (1875). Lectures on dermatology: Delivered in the Royal College of Surgeons of
England in 1874–1875. London, UK: Kessinger Publishing.
Woods, D. W., Flessner, C. A., Franklin, M. E., Keuthen, N. J., Goodwin, R. D., Stein, D. J.,
et al. (2006). The trichotillomania impact project (TIP): Exploring phenomenology,
functional impairment, and treatment utilization. The Journal of Clinical Psychiatry,
67, 1877–1888.
Woods, D. W., Snorrason, I., & Espil, F. M. (2012). Cognitive-behavioral therapy in
adults. In J. E. Grant, D. J. Stein, D. W. Woods, & N. J. Keuthen (Eds.), Trichotillomania, skin picking and other body-focused repetitive behaviors (pp. 175–192).
Washington, DC: American Psychiatric Publishing, Inc.
Woods, D. W., Wetterneck, C. T., & Flessner, C. A. (2006). A controlled evaluation of acceptance and commitment therapy plus habit reversal for trichotillomania. Behaviour Research and Therapy, 44, 639–656.
Zuchner, S., Wendland, J. R., shley-Koch, A. E., Collins, A. L., Tran-Viet, K. N., & Quinn, K.
(2009). Multiple rare SAPAP3 missense variants in trichotillomania and OCD. Molecular Psychiatry, 14, 6–9.