Cancer Antigen 125
advertisement

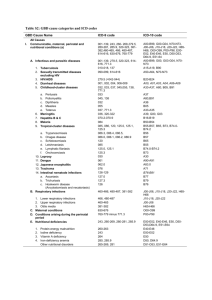
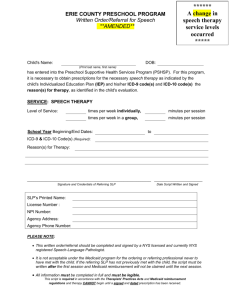
Cancer Antigen 125 (CA-125) Testing Corporate Medical Policy File name: Cancer Antigen 125 (CA-125A) Testing File Code: UM.DIAG.05 Origination: 02/2011 Last Review: 02/2014 (ICD-10 remediation only) Next Review: 02/2014 Effective Date: 07/01/2011 Document Precedence Blue Cross and Blue Shield of Vermont (BCBSVT) Medical Policies are developed to provide clinical guidance and are based on research of current medical literature and review of common medical practices in the treatment and diagnosis of disease. The applicable group/individual contract and member certificate language determines benefits that are in effect at the time of service. Since medical practices and knowledge are constantly evolving, BCBSVT reserves the right to review and revise its medical policies periodically. To the extent that there may be any conflict between medical policy and contract language, the member’s contract language takes precedence. Description Ovarian cancer is a malignancy of the ovaries that tends to elude early diagnosis. Most women with this malignancy seek medical attention late in the disease course, at which point the five year survival is only 15% to 20%. However, if diagnosed early, the five-year survival rate can be as high as 90%. Therefore, researchers have tried to develop various means of screening the general population for ovarian cancer to improve long-term survival. CA-125 is a high molecular-weight protein antigen that is commonly elevated in patients with known ovarian cancer. CA-125 may also be elevated in other gynecologic malignancies, such as endometrial cancer, although the association is not as consistent as that with ovarian cancer. CA-125 has been widely used as a technique to monitor patients with known ovarian cancer or other gynecologic malignancies that are associated with elevated levels of CA-125 in individual patients. Frequently, a rising CA-125 will be the initial sign of recurrent disease. Policy Medically Necessary: CA-125 testing may be medically necessary under the following circumstances: 1 • • • • Patients with symptoms suggestive of ovarian cancer Patients with known ovarian cancer. Individual patients with other malignancies, such as endometrial cancer, in whom baseline levels of CA-125 have been shown to be elevated. As a screening test for ovarian cancer when there is a history of hereditary cancer syndrome (a pattern of clusters of ovarian cancer within two or more generations) Investigational and Not Medically Necessary: Measurement of CA-125 is considered experimental/investigational in asymptomatic patients as a screening technique for ovarian cancer. When service or procedure is covered Women known to be at high risk for ovarian cancer are often screened regularly using a combination of the CA-125 test, transvaginal ultrasound and a rectal/pelvic examination. It should never be used as an isolated test. These include: • • • • • As a preoperative diagnostic aid in women with ovarian masses that are suspected to be malignant, such that arrangements can be made for intraoperative availability of a gynecological oncologist if the CA 125 is increased; or As a screening test for ovarian cancer when there is a history of hereditary cancer syndrome (a pattern of clusters of ovarian cancer within two or more generations); or Diagnosis of ovarian cancer in women with new symptoms (bloating, pelvic or abdominal pain, difficulty eating or feeling full quickly, or urinary frequency and urgency) that have persisted for three or more weeks, where the clinician has performed a pelvic and rectal examination and suspects ovarian cancer; or In members with adenocarcinoma of unknown primary, to rule out ovarian cancer; or In members with known ovarian cancer, as an aid in the monitoring of disease, response to treatment, detection of recurrent disease, or assessing value of performing second-look surgery. When service or procedure may not be covered CA-125 as a Screening Tool for Ovarian Cancer Currently, there is no definitive evidence that ovarian cancer screening of the general public using serum CA-125 measurements decreases mortality of the screened group. To date, the published reports utilizing CA-125 with or without other modalities do not demonstrate a high enough sensitivity to justify its use in low-risk, asymptomatic women. 2 Administrative and Contractual Guidance Benefit Determination Guidance Benefits are subject to all terms, limitations and conditions of the subscriber contract. For New England Health Plan (NEHP) members an approved referral authorization is required. Benefits for FEP members may vary. Please consult the FEP Service Plan Brochure. Coverage varies according to the member’s group or individual contract. Not all groups are required to follow the Vermont legislative mandates. Member Contract language takes precedence over medical policy when there is a conflict. If the member receives benefits through a self-funded (ASO) group, benefits may vary or not apply. To verify benefit information, please refer to the member’s plan documents or contact the customer service department. Audit Information BCBSVT reserves the right to conduct audits on any provider and/or facility to ensure compliance with the guidelines stated in the medical policy. If an audit identifies instances of non-compliance with this medical policy, BCBSVT reserves the right to recoup all non-compliant payments. Billing and Coding/Physician Documentation Information See Attachments below for coding tables & instructions as applicable. Eligible Providers Allopathic Physicians (M.D.) Osteopathic Physicians (D.O.) Policy Implementation/Update information 02/2011-New Policy 02/2014- ICD-10 Remediation. Updated standard policy language added. RLJ. Scientific Background and Reference Resources Buys, Saundra S., MD, et al., “Ovarian cancer screening in the Prostate, Lung, Colorectal and Ovarian (PLCO) cancer screening trial: Findings from the initial screen of a randomized trial.” American Journal of Obstetrics and Gynecology,” Volume 193, pp. 1630-9, 2005). 3 · Centers for Medicare & Medicaid Services (CMS), Medicare Coverage Database, “NCD for Tumor Antigen by Immunoassay-CA-125,” Manual Section Number 190.28, Original effective date 11/25/02, current effective date 1/1/06, < http://www.cms.hhs.gov/pf/printpage.asp?ref=http://www.cms.hhs.gov/mcd/viewnc d.asp?nc d_id=190.28&ncd_version=2&basket=ncd%3A190%2E28%3A2%3ATumor+Antigen+by+Im munoassay+%2D+CA+125 >, (accessed 3/4/09). · Goonewardene, Tyronne, MRCP, et al., “Management of asymptomatic patients on follow up for ovarian cancer with rising CA-125 concentrations,” The Lancet Oncology,” Volume 8, Issue 9, September 2007, pp. 813-821. · Graham, Lisa, “ACOG Releases Guidelines on Management of Adnexal Masses,” American Family Physician,” Volume 77, Number 9, May 1, 2008, pp. 1320-1323. · HAYES Medical Technology Directory, “CA-125 for Ovarian Cancer Screening in AverageRisk Women," Lansdale, PA: HAYES, Inc., February 22, 2005. · Hayes Update Search, “Ca 125 for Ovarian Cancer Screening in Average-Risk Women, Lansdale, PA: Hayes, Inc. February 21, 2008. · Kurman, Robert J., MD, et al., “Early detection and treatment of ovarian cancer: shifting from early stage to minimal volume of disease based on a new model of carcinogenesis,” American Journal of Obstetrics and Gynecology (Reviews), April 2008, pp. 351-356. · Mironov, Svetlana, MD, et al., “Ovarian Cancer,” Radiologic Clinics of North America, Volume 45, Number 1, January 2007. · Nossov, Vladimir, MD, et al., “The early detection of ovarian cancer: from traditional methods to proteomics. Can we really do better than serum CA-125?” American Journal of Obstetrics and Gynecology, Volume 199, Issue 3, September 2008, pp, 215-223. · Pavelka, James C., MD, et al., “Hereditary Ovarian Cancer-Assessing Risk and Prevention Strategies,” Obstet Gynecol Clin N Am, Volume 34, 2007, pp. 651–665. · Sevinc, Alper, et al., “Benign causes of increased serum CA-125 concentration,” The Lancet Oncology, Volume 8, Issue 12, December 2007, pp. 1054-1055. · U.S. Preventive Services Task Force, “Screening for Ovarian Cancer: Recommendation Statement,” American Family Physician, Volume 71, Number 4, February 15, 2005. · van Nagell, Jr., J. R., MD, and P. D. DePriest, MD, “Management of adnexal masses in postmenopausal women,” American Journal of Obstetrics and Gynecology, Volume 193, 2005, pp.30–5. 4 Approved by BCBSVT Medical Director Date Approved Spencer Borden MD Chair, Medical Policy Committee Robert Wheeler MD Chief Medical Officer Attachment I CPT code list Code Type Number Brief Description Policy Instructions The following codes will be considered as medically necessary when applicable criteria have been met. CPT Immunoassay for Tumor Antigen, 86304 quantitative; CA 125 Attachment II ICD-9 Code List Code Type Number Description The following diagnoses apply to this medical policy. ICD-9 158.0 Malignant neoplasm of retroperitoneum ICD-9 158.8 Malignant neoplasm of specified parts of peritoneum ICD-9 158.9 Malignant neoplasm of peritoneum, unspecified ICD-9 180.0 Malignant neoplasm of endocervix ICD-9 182.0 Malignant neoplasm of corpus uteri, except isthmus ICD-9 182.1 Malignant neoplasm of isthmus 5 ICD-9 182.8 Malignant neoplasm of other specified sites of body of uterus ICD-9 183.0 Malignant neoplasm of ovary ICD-9 183.2 ICD-9 183.3 Malignant neoplasm of fallopian tube Malignant neoplasm of broad ligament of uterus ICD-9 183.4 Malignant neoplasm of parametrium ICD-9 183.5 Malignant neoplasm of round ligament of uterus ICD-9 183.8 Malignant neoplasm of other specified sites of uterine adnexa ICD-9 183.9 Malignant neoplasm of uterine adnexa, unspecified Malignant neoplasm of other specified sites of female genital organs ICD-9 184.8 ICD-9 198.6 Secondary malignant neoplasm of ovary ICD-9 198.82 Secondary malignant neoplasm of genital organs ICD-9 199.0 Disseminated malignant neoplasm ICD-9 236.0 Neoplasm of uncertain behavior of uterus ICD-9 236.1 Neoplasm of uncertain behavior of placenta ICD-9 236.2 Neoplasm of uncertain behavior of ovary Neoplasm of uncertain behavior of other and unspecified female genital organs ICD-9 236.3 ICD-9 338.3 Neoplasm related pain (acute) (chronic) ICD-9 789.30 Abdominal or pelvic swelling, mass, or lump, unspecified site ICD-9 789.31 Abdominal or pelvic swelling, mass, or lump, right upper quadrant 6 ICD-9 789.32 Abdominal or pelvic swelling, mass, or lump, left upper quadrant ICD-9 789.33 Abdominal or pelvic swelling, mass, or lump, right lower quadrant ICD-9 789.34 Abdominal or pelvic swelling, mass, or lump, left lower quadrant ICD-9 789.35 Abdominal or pelvic swelling, mass, or lump, periumbilic ICD-9 789.36 Abdominal or pelvic swelling, mass, or lump, epigastric ICD-9 789.37 Abdominal or pelvic swelling, mass, or lump, generalized Abdominal or pelvic swelling, mass, or lump, other specified site; multiple sites ICD-9 789.39 ICD-9 795.82 Elevated cancer antigen 125 [CA 125] ICD-9 795.89 Other abnormal tumor markers ICD-9 V10.43 Personal history of malignant neoplasm of ovary Personal history of malignant neoplasm of other female genital organs ICD-9 V10.44 ICD-9 V16.41 Family history of malignant neoplasm of ovary ICD-9 V71.1 Observation for suspected malignant neoplasm ICD-9 V76.46 Screening for malignant neoplasms of the ovary Attachment III ICD-10 Code List (Effective 10/1/2014) Code Type Number Description 7 The following diagnoses apply to this medical policy. ICD-10 C45.1 Mesothelioma of peritoneum ICD-10 C48.0 Malignant neoplasm of retroperitoneum ICD-10 C48.1 Malignant neoplasm of specified parts of peritoneum ICD-10 C48.2 Malignant neoplasm of peritoneum, unspecified Malignant neoplasm of overlapping sites of retroperitoneum and peritoneum ICD-10 C48.8 ICD-10 C51.8 Malignant neoplasm of overlapping sites of vulva ICD-10 C53.0 Malignant neoplasm of endocervix ICD-10 C54.0 Malignant neoplasm of isthmus uteri ICD-10 C54.1 Malignant neoplasm of endometrium ICD-10 C54.2 Malignant neoplasm of myometrium ICD-10 C54.3 Malignant neoplasm of fundus uteri ICD-10 C54.8 Malignant neoplasm of overlapping sites of corpus uteri ICD-10 C54.9 Malignant neoplasm of corpus uteri, unspecified ICD-10 C56.1 Malignant neoplasm of right ovary ICD-10 C56.2 Malignant neoplasm of left ovary ICD-10 C56.9 Malignant neoplasm of unspecified ovary ICD-10 C57.00 Malignant neoplasm of unspecified fallopian tube ICD-10 C57.01 Malignant neoplasm of right fallopian tube ICD-10 C57.02 Malignant neoplasm of left fallopian tube ICD-10 C57.10 Malignant neoplasm of unspecified broad ligament 8 ICD-10 C57.11 Malignant neoplasm of right broad ligament ICD-10 C57.12 Malignant neoplasm of left broad ligament ICD-10 C57.20 Malignant neoplasm of unspecified round ligament ICD-10 C57.21 Malignant neoplasm of right round ligament ICD-10 C57.22 Malignant neoplasm of left round ligament ICD-10 C57.3 Malignant neoplasm of parametrium ICD-10 C57.4 Malignant neoplasm of uterine adnexa, unspecified ICD-10 C57.7 Malignant neoplasm of other specified female genital organs ICD-10 C57.8 Malignant neoplasm of overlapping sites of female genital organs ICD-10 C79.60 Secondary malignant neoplasm of unspecified ovary ICD-10 C79.61 Secondary malignant neoplasm of right ovary ICD-10 C79.62 Secondary malignant neoplasm of left ovary ICD-10 C79.82 Secondary malignant neoplasm of genital organs ICD-10 C80.0 Disseminated malignant neoplasm, unspecified ICD-10 D39.0 Neoplasm of uncertain behavior of uterus ICD-10 D39.10 Neoplasm of uncertain behavior of unspecified ovary ICD-10 D39.11 Neoplasm of uncertain behavior of right ovary ICD-10 D39.12 Neoplasm of uncertain behavior of left ovary ICD-10 D39.2 Neoplasm of uncertain behavior of placenta 9 Neoplasm of uncertain behavior of other specified female genital organs ICD-10 D39.8 ICD-10 D39.9 Neoplasm of uncertain behavior of female genital organ, unspecified ICD-10 G89.3 Neoplasm related pain (acute) (chronic) ICD-10 R19.00 Intra-abdominal and pelvic swelling, mass and lump, unspecified site ICD-10 R19.01 Right upper quadrant abdominal swelling, mass and lump ICD-10 R19.02 Left upper quadrant abdominal swelling, mass and lump ICD-10 R19.03 Right lower quadrant abdominal swelling, mass and lump ICD-10 R19.04 Left lower quadrant abdominal swelling, mass and lump ICD-10 R19.05 Periumbilic swelling, mass or lump ICD-10 R19.06 Epigastric swelling, mass or lump ICD-10 R19.07 Generalized intra-abdominal and pelvic swelling, mass and lump ICD-10 R19.09 Other intra-abdominal and pelvic swelling, mass and lump ICD-10 R97.1 Elevated cancer antigen 125 [CA 125] ICD-10 R97.8 Other abnormal tumor markers Encounter for observation for other suspected diseases and conditions ruled out ICD-10 Z03.89 ICD-10 Z12.73 Encounter for screening for malignant neoplasm of ovary ICD-10 Z80.41 Family history of malignant neoplasm of ovary ICD-10 Z85.43 Personal history of malignant neoplasm of ovary 10 ICD-10 Z85.44 Personal history of malignant neoplasm of other female genital organs 11