Osteopathic Approach To Headaches
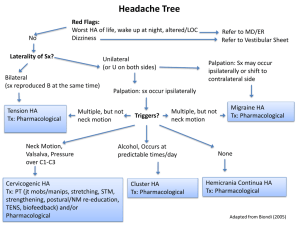
advertisement

Osteopathic Approach to Headache Gautam J. Desai, DO, FACOFP Lauren J. Branham, OMSIV, OMM Fellow KCU Homecoming CME Disclaimers Neither of the presenters nor the table trainers have any true or perceived conflict of interest nor financial conflicts. This presentation is for educational purposes only and we are not able to offer individual OMT to attendees. HEADACHE PRIMARY • • • • • Migraines Cluster Analgesic Tension Cervicogenic SECONDARY • • • • • • • • • • • SAH Meningitis Abscess Tumor Temporal arteritis Pseudotumor cerebri Vertebral artery dissection AV malformation Chiari malformation Cerebral aneurysm Trigeminal Neuralgia Assessment of Headache PRIMARY • History and Physical NO RED FLAGS • • • • • Fever Focal neurological deficit Progressive + N/V New onset >50 yo Sudden onset YES SECONDARY • CT • LP • Biopsy Analgesic Rebound Tension/ Cervicogenic Cluster Migraines Analgesic Rebound • Path: Withdrawal • Pt: on pain meds • Tx: Meds/NSAIDS/ Acetaminophen Tension/ Cervicogenic Cluster Migraines Analgesic Rebound • Path: Withdrawal • Pt: on pain meds • Tx: Meds/NSAIDS/ Acetaminophen - Withdrawal; so avoid • Dx: Clinical Tension/ Cervicogenic Cluster Migraines Analgesic Rebound • Path: Withdrawal • Pt: on pain meds • Tx: Meds/NSAIDS/ Acetominophen - Withdrawal; so avoid • Dx: Clinical Tension/ Cervicogenic • Path: Muscular/ Structural • Pt: B/L Viselike; radiates to neck or from neck to head • Dx: Clinical • Tx: NSAIDs/OMT/ Acetaminophen Cluster Migraines Analgesic Rebound • Path: Withdrawal • Pt: on pain meds • Tx: Meds/NSAIDS/ Acetominophen - Withdrawal; so avoid • Dx: Clinical Tension/ Cervicogenic • Path: Muscular/ Structural • Pt: B/L Viselike; radiates to neck or from neck to head • Dx: Clinical • Tx: NSAIDs/OMT/ Acetaminophen Cluster • • • • • Path: Vascular Pt: Asx for months 30+ attacks in 1-3 days; Horner’s Syndrome; ipsilateral lacrimation, conjunctival inflammation, rhinorrhea, periorbital pain Dx: Clinical Tx: 100% HIGH FLOW O2; Ergots; PPx w/ CCBs F/U with Brain Imaging Migraines Analgesic Rebound • Path: Withdrawal • Pt: on pain meds • Tx: Meds/NSAIDS/ Acetominophen - Withdrawal; so avoid • Dx: Clinical Tension/ Cervicogenic • Path: Muscular/ Structural • Pt: B/L Viselike; radiates to neck or from neck to head • Dx: Clinical • Tx: NSAIDs/OMT/ Acetaminophen Cluster • • • • • Path: Vascular • Pt: Asx for months 30+ attacks in 1-3 days; • Horner’s Syndrome; ipsilateral lacrimation, conjunctival inflammation, • rhinorrhea, periorbital • pain Dx: Clinical Tx: 100% HIGH FLOW O2; Ergots; PPx w/ CCBs • F/U with Brain Imaging? • Migraines Path: Vascular (vasodilation) Pt: Photo/phonophobia; TRIGGER, +/- Aura; 3648hrs; aborts with sleep but have “hangover” Dx: Clinical Tx: Avoid Triggers; mild + early = NSAIDs; Modsevere = Ergots/triptans (caution in CAD) PPX: CCBs; BBs F/U with Brain Imaging? Typical Patient Presentation: Cervicogenic Headache (CHA) • Unilateral head pain • Moderate to severe, deep, non-throbbing and non-lancinating • Does not shift from side to side • Fluctuates in intensity – increased by certain movements of the head or sustained positions • Radiates from occipital to frontal regions • +/- history of whiplash/head/neck injury prior to symptom onset • May have restricted neck range of motion, ipsilateral neck, shoulder or arm pain • Varying duration with lack of response to medications usually helpful in alleviating other types of headaches Osteopathic Structural Exam • C-Spine shows decreased AROM and PROM in all planes, somewhat worse with right sidebending and rotation • Cervical paravertebral and upper trapezius musculature demonstrate increased tone with mild tenderness to palpation • Tenderness, muscular tension, and fullness in the suboccipital region (R > L) • OA F RrSl, AA Rr, C2-3 E RlSl, deep palpation radiates pain to area of right orbit • T1-3 N RrSl, T4-5 E RlSl In the neutral position (seated or prone), place thumbs over the TP’s of vertebrae being evaluated Left thumb posterior Right thumb posterior = Left Posterior TP (PTP) = Right Posterior TP (PTP) = Left rotation = Right rotation Check in flexion & extension Symmetry restored in flexion Symmetry restored in extension F RL S L E RL S L Check in flexion & extension Symmetry NOT restored in flexion or extension N RL S R Symmetry restored in flexion Symmetry restored in extension F RR S R E RR SR Symmetry NOT restored in flexion or extension N RR S L Adapted from OMT Review, 3rd Edition, Savarese, 2002. Practice Time Check your partner’s T spine for dysfunction Anatomy Review Cervical Spine has 7 vertebral segments: Atlas (C1) and Axis (C2) are atypical Atlas has no vertebral body (rotates around dens) Vertebral body of C2 extends superiorly to form dens (odontoid process) Articulation between C2 and C3 and rest of cervical joints is considered typical Facets are in a plane that points towards the eye in the uppers, and opposite ASIS for the lower segments Important for manipulative force vectors Biomechanics Occipitoatlantal (OA) Joint: Major motions: flexion & extension *Minor motions: SB & rotation The occiput rotates and SB to opposite sides Biomechanics Atlantoaxial (AA) joint: Primary motion: rotation *atlas rotates about the dens Almost no SB or flexion/extension Biomechanics Typical Cervical Segments (C2 thru C7): Rotation and SB: same side *but some find clinically, SB and rotation to opposite sides Modified Type II Mechanics Structural Evaluation Base off of patient’s H&P: Problem with: jaw cervical, thoracic or lumbar spine/innominates patient’s spirit (depression, anxiety, stress) work-related (hairdresser, manual labor) Try to elucidate how structure is affecting function Remember to check the first rib Often a culprit as a trigger for headaches Especially in pts who use hands/upper back at work Students carrying backpacks, etc. Cervical Spine Treatment OA Suboccipital Release Cup occiput and give gentle axial traction and some lateral traction Wait for musculature to relax Teach pts to do at home with pillow AT Still did to himself Cervical Spine Treatment AA Muscle Energy Fully flex head and neck then rotate into the barrier Ask the pt to gently move head and neck to neutral while dr resists motion Relax, move to next new barrier and then repeat process until no new barriers reached Muscle Energy Treatment Typical Cervicals (i.e. C3ERRSBR) Muscle Energy Pt seated/supine with dr standing behind pt Dr’s R index finger on PTP (C3 in this case), and rest of hand on side of neck, dr’s L hand atop pt’s head Take to barrier: in this case flex, SB and rotate L Pt to gently straighten head vs. dr’s resistance for 3-5 seconds During period of relaxation, take further into barrier (more flexion, SB left, and rotation left) Repeat 3 times Cervical Spine Treatment Scalene muscles Myofascial release Pt seated Dr stands behind pt Grasp scalene muscle with thumb and index finger and pull towards dr Perpendicular stretch Now SB head away from side you are stretching Longitudinal stretch Practice Time On your partner: Check C spine Do suboccipital release AA and typical C spine ME Cervical Spine Treatment Typical Cervicals Still’s Technique (i.e. C3ERRSBR) Pt supine with dr at head of table Dr’s R index finger on PTP (C3 in this case), and rest of hand wrapped around side of neck to support (and also to use as a fulcrum) Dr’s L hand on top of pt’s head Take where dysfunction already is and exaggerate: in this case extend, and SB and rotate R. as pt supine, extension and SB are minimal, but rotate until you feel relaxation of tissues. this removes strain from affected segment Cervical Spine Treatment Typical Cervicals Still’s Technique (i.e. C3ERRSBR) Push down on head with L hand (axial compression) Move head away from area of dysfunction. Rotate head to L, while simultaneously SB L, and flexing cspine. Take to barrier, and as you are moving, may feel release with monitoring hand at PTP. Release compression, and take pt back to neutral Retest Upper Extremity Treatment Rhomboid Stretch Pt seated (or supine), with dr standing facing pt Place finger pads on medial and inferior aspect of scapula Drape pt’s arm over your forearm Attempt to roll your fingers under medial edge of scapula to apply traction to rhomboids Continue traction while exerting a lateral force against medial aspect of scapula Relax and reapply traction force 3-5 times Thoracic Treatment Still’s Technique Pt seated (or supine) , dr standing on side of tx With one hand, contact tissues between rib angle and transverse process and spring anteriorly to feel for hard endfeel With other hand, grab olecranon and induce motion in UE, so olecranon moves toward contact point of posterior hand, until motion felt at contact point Thoracic Treatment Still’s Technique (continued) Now ADduct UE at shoulder until motion felt at contact point. Determine if internal or external rotation at shoulder is freer motion Depending on which motion is freer, continue arc of motion in upper extremity 360 degrees. If internal rotation freer: arc of motion is as if using an overhand throwing motion If external rotation freer: arc of motion is as if using an underhand throwing motion Thoracic Treatment Still’s Technique (continued) Usually articulation or palpable motion felt at contact point of posterior hand. Recheck segment by springing anteriorly. Repeat for each thoracic level Best to start at T-12 and work superiorly After 1 side of cage complete, repeat on other side Practice Time Cervical Still’s Rhomboid Stretch Thoracic Still’s Lumbar Spine Always important to check from below in pts with cephalgia May find adult onset scoliosis Asymmetrical lumbar spine may cause muscle tension above due to desire to keep eyes level S/P MVA Check innominate lengths Usually asymmetrical in cephalgia pts Especially if hx hip fx, ankle injury Check ASIS and medial malleoli b/l The Best Treatment is Prevention! Search for triggers, and have your pts avoid them Do stretching exercises Reduce stress Need multifaceted approach for treatment success Can OMT save money? One study reviewed EMRs from 631 pts seen at 2 Florida residency clinics One osteopathic and had OMT available, and the other allopathic and did not offer OMT 1427 office visits for migraine related reasons Costs tallied Average cost per pt visit was approximately 50% less at osteopathic clinic than at allopathic clinic ($195.63 vs $363.84, respectively; P<.001). Entirely attributable to difference in average # of meds rx’d per visit at the two clinics 0.696 prescriptions at the osteopathic clinic and 1.285 prescriptions at allopathic clinic (P<.001) Lower average med cost per visit at osteopathic clinic than at allopathic clinic ($106.94 vs $284.93, respectively; P<.001). Pts at the osteopathic clinic 5 years younger on average than allopathic clinic (P<.001) No statistically significant difference observed btw two practices in pts' ratings of pain severity Authors’ Conclusion: The inclusion of OMT in a treatment regimen for patients with migraine headache may lower the cost of the treatment regimen. However, further study is needed to confirm these results. Schabert, Crow, Impact of OMT on Cost of Care for Patients With Migraine Headache: A Retrospective Review of Patient Records , JAOA August 1, 2009 vol. 109 no. 8 403-407 Bibliography 1. Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. Headache. 1990;30(11):725. 2. Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, Emberson J, Marschner I, Richardson C. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine (Phila Pa 1976). 2002;27(17):1835. 3. Hall T, Chan HT, Christensen L, Odenthal B, Wells C, Robinson K. J Orthop Sports Phys Ther. Efficacy of a C1-C2 self-sustained natural apophyseal glide (SNAG) in the management of cervicogenic headache. 2007 Mar;37(3):100-7. 4. Haldeman S, Dagenais S. Cervicogenic headaches: a critical review. Spine J 2001;1(1):3146 5. Pollmann W, Keidel M. Headache and the cervical spine: a critical review. Cephalgia 1997;17:801-816 6. Schwartz BS, Stewart WF. Lost workdays and decreased work effectiveness associated with headache in the workplace. J Occup Environ Med 1997;39(4):320-327 7. Bogduk N. The anatomical basis for cervicogenic headache. J Manipulative Physiol Ther. 1992;15(1):6 8. Hruby, Raymond J. Ch. 60 Cervicogenic Headache. Foundations of Osteopathic Medicine, 3rd ed. 9. Lord SM, Barnsley L, Wallis BJ, Bogduk N. Third occipital nerve headache: a prevalence study. J Neurol Neurosurg Psychiatry. 1994;57(10):1187 10. Biondi DM. Cervicogenic headache: mechanisms, evaluation, and treatment strategies. J Am Osteopath Assoc. 2000;100(9) Bibliography (continued) 11. Bogduk N, Govind J. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol. 2009;8(10):959. 12. Cooper G, Bailey B, Bogduk N. Cervical zygapophysial joint pain maps. Pain Med. 2007;8(4):344. 13. Foreman RD. Integration of viscerosomatic sensory input at the spinal level. Prog Brain Res 2000;122:209-221 14. Bogduk, N. Distinguishing primary headache disorders from cervicogenic headache: clinical and therapeutic implications. Headache Currents. 2005; 2:27. 15. The International Classification of Headache Disorders, 3rd edition (beta version). Headache Classification Committee of the International Headache Society (IHS). Cephalalgia. 2013 Jul;33(9):629-808. 16. Bogduk N. The neck and headaches. Neurol Clin. 2004;22(1):151. 17. Joshua D. Brooks, PhD on AMA Wire 12/8/2014 18. COILS – Patient with a headache, AACOM’s Education Council on Osteopathic Principles. 2015. 19. Cervicogenic headache after whiplash injury. Drottning M, Staff PH. Cephalalgia 2002;22(3):165-171. 20. Stovner L, Hagen K, Jensen R, et al. The global burden of headache: A documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27:193–210. 21. Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003,290(18):2443-2454.