Physical Therapy and Headaches
advertisement
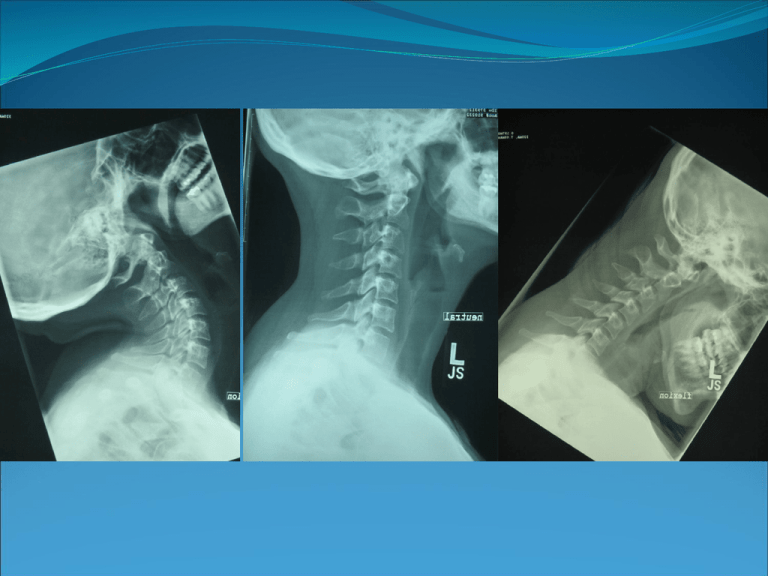
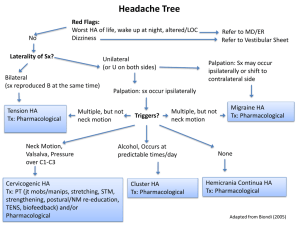
Kristin Stockham, SPT Regis University Objectives The learner will be able… To state the criteria necessary for a diagnosis of cerviogenic headache; To provide information assessed in the examination and evaluation for cervicogenic headache; To apply current evidence in development of an intervention for cervicogenic headache. This 17 year old female was referred with the following information: Dx: Neck pain & HA Rx: Evaluate & Treat S: 2 year hx of R sided headaches that can be brought on by too much reading. What We Know Diagnostic Criteria International Headache Society1 1. 2. 3. 4. Pain localized in the neck and occiput, which can spread to other areas in the head, such as forehead, orbital region, temples, or ears, usually unilateral. Pain is precipitated or aggravated by specific neck movements or sustained posture. At least one of the following: i. Resistance to or limitation of passive neck movements. ii. Changes in neck muscle contour, texture, tone, or response to active and passive stretching and contraction. iii. Abnormal tenderness of neck musculature. Radiological examination reveals at least one of the following: i. Movement abnormalities in flexion/extension. ii. Abnormal posture. iii. Fractures, congenital abnormalities, bone tumors, RA, or other distinct pathology (not spondylosis or osteochondrosis). Cervicogenic Headache Facts Incidence (up to 20% of all headaches)2 Structural Causes3 Gross cervical ROM vs. C0-1 & C1-2 ROM 4,5,6 Anatomy Kinesiology & Biomechanics C0-1-Convex-concave articulations Atlas moves in direction of skull motion7 C1-2: Convex-convex articulations History “Heather” is a 17 year old female about to begin her senior year of high school. She started experiencing intermittent neck pain and headaches about 2 years ago. She reports no known MOI, but notes the pain has steadily increased. She inconsistently tried chiropractic treatments about 6-7 months ago, but found no relief. She said her headaches are usually right-sided and can be brought on with extended periods of reading. She also notes that sometimes she experiences “numbness” in her R arm with certain arm movements. She reports taking 2 extra strength Tylenol 4x/d. Initial Examination Posture FHP, increased upper thoracic spine kyphosis, rounded shoulders UE: Dermatomes Myotomes Reflexes Normal: C4-T1 Normal: C4-T1 2+: biceps brachii, triceps & brachioradialis Cervical AROM RR/LR=60º; FB/BB=60º; RSB/LSB=45º Supine OA Nodding6 Unable to achieve neutral Sitting C1-2 Rotation6 RR=2º; LR=5º Supine C2-3 PIVM8 R=1/6; L=2/6 Supine C3-6 PIVM8 R/L=4/6 Thoracic Spine Mobility Limited bilateral C7-T4 extension NDI: NPRS 27: 6/10 Spurlings ULTT (Median Nerve bias) Cervical distraction test Negative = R/L Negative = R/L Negative Muscle Palpation Pain to the suboccipital mm. specifically superior oblique, rectus capitis posterior major, semispinalis capitis; muscles of mastication including bilateral superficial masseters, anterior and middle temporalis and medial pterygoids. DNF painful B with decreased strength/endurance (5 seconds) Radiograph Evaluation PIP: “I am unable to complete all my homework on time, because too much reading makes my headaches and neck pain worse.” Pt presents with signs and symptoms consistent with cervicogenic headache as is seen by: movement abnormalities of the upper cervical spine (C0-3) in flexion on radiographic imaging, decreased cervical lordosis in neutral on radiographic imaging, limitation of passive neck movements at C0-3, abnormal tenderness of neck musculature, and unilateral headaches and neck pain is aggravated by prolonged flexion. Diagnosis/Prognosis Preferred Practice Pattern B- Impaired Posture ICD-9 Codes: 723.1- Cervicalgia 784.0- Headache Prognosis: Based on the following prognostic factors, this patient has a good prognosis for restoration of upper cervical spine ROM and decreased HA frequency with physical therapy interventions. Positive Factors: young age, active, unremarkable PMH, family support, motivated. Negative Factors: chronic headache duration. Goals Within 2 weeks patient will: Achieve at least 10º of R/L C1-2 rotation. Be able to read for 15 continuous minutes without increasing neck pain and exacerbating headaches. Within 4-6 weeks patient will: Achieve 20º of R/L C1-2 rotation. Be able to read for 30 continuous minutes without experiencing neck pain (0/10) or headaches. Decrease headache frequency to no more than 2x/wk. Plan of Care Physical therapy 2x/wk for 4-6 weeks including: Manual therapy treatment utilizing the following: joint mobilization/manipulation techniques to limited joints and soft tissue techniques including soft tissue mobilization to restore muscle motion and normal tone. Exercise program for neck specific ROM and nodding of the upper cervical spine. NO STRETCHES. This patient has increased midcervical spine joint motion. Intervention and Evidence Van Duijn J, Van Duijn AJ, Nitsch W. Orthopaedic manual physical therapy including thrust manipulation and exercise in the management of a patient with cervicogenic headache: A case report. J Manual Manipulative Ther. 2007;15(1):10-24.9 Case Study: the use of manual therapy, including mobilization and manipulation to the upper neck, and exercise to treat a patient with cervicogenic headaches. Favorable response. ROM improved as well as subjective findings (I.e. NDI, pain). Hoving JA, Koes BW, de Vet HCW, et al. Manual therapy, physical therapy or continued care by a general practitioner for patients with neck pain. Ann Intern Med. 2002;136:713:722.10 “Manual therapy is a favorable treatment option for patients with neck pain when compared with physical therapy or continued care by a general practitioner” Interventions 97140: Manual therapy Soft tissue mobilization (STM) to posterior neck and upper thoracic spine (lamina release) Supine bilateral OA nodding Supine unilateral R/L OA nodding Supine unilateral R/L C1-2 rotation Sitting C1-2 rotation stretch Supine unilateral R/L C3-6 facet upglides/downglides Standing thoracic manipulation Prone thoracic PA mobilizations/manipulations. 97112: Neuro Re-Education Postural re-education Supine DNF exercises Re-Evaluation at visit 10 Initial Evaluation @ Visit 10 Posture FHP, increased thoracic spine kyphosis, rounded shoulders. Decreased FHP, decreased upper thoracic spine kyphosis, decreased rounded shoulders. Supine OA Nodding Unable to achieve neutral FB = 10º Sitting C1-2 Rotation RR = 2º; LR = 5º RR = 15º; LR = 20º C2-3 PIVM R = 1/6; L = 2/6 R = 2/6; L = 3/6 C3-6 PIVM R/L = 4/6 R/L = 3/6 Thoracic Spine Mobility Limited B C7-T4 extension Limited R extension C7-T2 NDI: NPRS 27: 6/10 18: 2/10 Muscle Palpation Pain to the suboccipital mm. specifically superior oblique, rectus capitis posterior major, semispinalis capitis; muscles of mastication including bilateral superficial masseters, anterior and middle temporalis and medial pterygoids. DNF painful B with decreased strength/endurance (5 seconds) Minimal, intermittent pain to suboccipital mm specifically superior oblique, rectus capitis posterior major; muscles of mastication including superficial masseter and R medial pterygoids. DNF strength/endurance (25 seconds) Review Diagnostic Criteria for Cervicogenic Headache- IHS Clinical Tests – Sitting C1-2 Rotation Test, Cervical Radiographs Flexion/Extension views, upper cervical joint mobility. Treatment – Manual therapy to restore upper neck ROM, STM to decrease increased muscle tension, DNF training to increase muscle endurance. Check for Understanding T/F: According to the International Headache Society an individual must present with bilateral pain in the neck and occiput to meet the diagnostic criteria for cervicogenic headache. Which test does the literature show is the most useful for the measurement of C1-2 rotation? 1. Sitting C1-2 rotation 2. Cervical flexion rotation 3. General cervical AROM Which of the following is NOT an appropriate intervention strategy for a person with cervicogenic headaches presenting with mid-cervical spine hypermobility? 1. 2. 3. Manual therapy to the cervical spine Cervical spine stretching DNF training References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Headache classification subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephaligia. 2004;24 Suppl 1:9-160. Hall T, Robinson K. The flexion-rotation test and active cervical mobility: A comparative measurement study in cervicogenic headache. Manual Ther. 2004;9:197-202. Zito G, Jull G, Story I. Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Manual Ther. 2006;11:118-129. Smedmark V, Wallin M, Arvidsson I. Inter-examiner reliability in assessing passive intervertebral motion of the cervical spine. Manual Ther. 2000;5(2):97-101. Hoppenfeld S, Murthy VL. Treatment and rehabilitation of fractures. 1st ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1999:515. Aprill C, Axinn MJ, Bogduk N. Occipital headaches stemming from the lateral atlanto-axial (C1-2) joint. Cephaligia. 2002;22:15-22. University of St. Augustine for Health Sciences. S3: Advanced evaluation & manipulation of cranio facial, cervical & upper thoracic spine. St. Augustine, FL. Gonnella C, Paris SV, Kutner. Reliability in evaluating passive intervertebral motion. Phys Ther. 1982;62(4):436-444. Van Duijn J, Van Duijn AJ, Nitsch W. Orthopaedic manual physical therapy including thrust manipulation and exercise in the management of a patient with cervicogenic headache: A case report. J Manual Manipulative Ther. 2007;15(1):1024. Hoving JA, Koes BW, de Vet HCW, et al. Manual therapy, physical therapy or continued care by a general practitioner for patients with neck pain. Ann Intern Med. 2002;136:713:722.