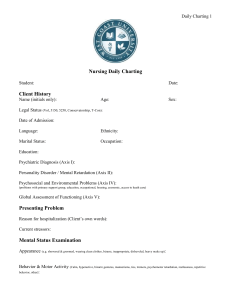
patient care manual policy
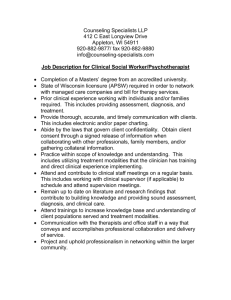
advertisement
PATIENT CARE MANUAL POLICY NUMBER #V-20 DATE PAGE July 5, 2010 1 APPROVED BY: Senior Vice President of Medicine & Chief of Staff, and Vice President & Senior Operating Officer; Rural Health Services & Professional Practice Lead CATEGORY: Documentation TITLE: Patient Chart Documentation Purpose Policy Statement Applicability OF 2 To provide guidelines to ensure that health care providers record information in a manner that is consistent with organizational and unit/department charting standards. Covenant Health staff and physicians shall maintain an accurate and complete health care record of each patient and will adhere to organizational and unit/department charting standards. This policy applies to Covenant Health – Edmonton Acute care facilities. Responsibility Covenant Health staff and physicians who provide care shall document on the patient care record and will demonstrate compliance with organizational and unit/department charting standards. Principles Documentation in the health care record provides a: 1. 2. 3. 4. 5. 6. 7. legal record of the patient’s assessment and treatment communication tool for health care providers method to identify problems and organize the treatment plan tool for evaluating the efficacy of treatment basis for peer review or quality assurance review basis to ensure continuity of care record for research projects that a patient may be part of. NUMBER #V-20 DATE PAGE TITLE: Related Documents July 5, 2010 2 OF Patient Chart Documentation Patient Care Manual P/P #V-35. Preprinted Patient Care Orders Patient Care Manual P/P #III-115, Medication Orders Patient Care Manual P/P #V-5, Completion of Health Records by Medical Staff Patient Care Manual P/P #V-15, Patient Care Record Accompanying the In-patient for Tests/Treatments Instructions for Use of the Nursing Assessment and Care Record 2 APPENDIX A NUMBER V-20 DATE July 5, 2010 PAGE TITLE: 1 OF 2 Patient Chart Documentation GUIDELINES FOR ‘CHARTING’ 1. 2. 3. Record only what you saw, heard or did. • Only document your own actions or observations. If circumstances arise that you must document the care given by others, the record should clearly identify both the caregiver and the individual who is documenting the information. • Do not include opinions or judgements. Record in a concise, factual and clear manner. • Use objective descriptors (do not use words like ‘good’ or ‘fine’). • Ensure your notes are legible and that your signature is immediately identifiable (and/or identifiable using the signature log as appropriate for the specific unit/department). • The use of abbreviations is discouraged and staff shall not use abbreviations listed in the “Prohibited Abbreviations” or “Dangerous Abbreviations” lists per Patient Care Policy/Procedure #III-115, Medication Orders. • Record in black ink on forms approved by the department. • Ensure the correct patient and hospital identification is on the upper right hand corner of each page of the patient’s record. Record consistently with unit/department guidelines and charting methodology. APPENDIX A NUMBER V-20 DATE July 5, 2010 PAGE TITLE: 2 OF 2 Guidelines for Charting GUIDELINES FOR ‘CHARTING’ - continued 4. Record contemporaneously* and in chronological order. (*definition: the ability to chart as soon as able) The ability to chart as soon as able and the amount of charting detail are dictated by a number of factors, including: a) b) c) d) • 5. organizational/unit policies and procedures, guidelines, practice NOTE: depending on the nature of the work, individual departments or areas may have specific charting requirements. When a department-specific charting standard varies from this policy/procedure, the standard of greater expectation will prevail. the complexity of the health problems the degree to which the patient’s condition puts him/her at risk; and the degree of risk involved in the treatment or care. It is imperative to record an event at the time it occurred (or as close as is prudently possible). The rationale for this is the notation is more likely to be viewed as accurate if it is made close to the time of the event. And, when an entry must be added out of order (late entries are better than no entries), the entry should be dated and signed, indicating both the time of entry and the time the event itself occurred. Record corrections clearly. • Correct errors but don’t obliterate them. Never erase or apply correction fluid. Make a straight line through the mistake so that it remains legible and write your initials beside it. • The new entry should include the date, time at which the correction was made, and the writer’s signature. APPENDIX B NUMBER V-20 DATE July 5, 2010 PAGE TITLE: 1 OF Patient Chart Documentation GUIDELINES FOR ‘CHARTING BY EXCEPTION’ DEFINITIONS Charting by Exception ¾ A method of documenting patient assessment parameters/critical indicators based on clearly defined guidelines for practice; i.e. predetermined criteria for nursing assessments, a plan of care, and expected patient outcomes. Relevant Care ¾ Pertinent information that is documented regarding the patient. This should include a change in patient condition or treatment/interventions, patient outcomes or description of concerns. 1. Covenant Health utilizes Charting by Exception in defined practice areas. Practice areas using Charting by Exception must adhere to the aforementioned “Guidelines for Charting”. 2. When combined with predetermined guidelines of practice, symbol charting for routine care and documentation of relevant care (eg. narrative charting and flow charting), exception charting: • • • • fosters analytical/critical thinking by the caregiver facilitates conciseness, continuity of care, and tracking of information promotes easy access to patient information, and decreases duplication. 3. The major activities reflected in any documentation process (eg. admission data base, care plans, protocols, flow sheets, progress notes) are included in exception charting. Documentation is by reference to predetermined guidelines for practice and relevant care; however, some aspects of narrative charting and flow charting will still be found in the patient record. 4. Patient care areas that utilize the exception charting method (eg. CareMaps or assessment tools) shall have guidelines describing how to document on the patient care record1 which must be adhered to. 5. Narrative notes could include assessment, intervention, and patient response. Record when there is a significant change in the patient’s status or treatment. NOTE: In some practice areas the charting guidelines indicate progress and narrative notes are not necessarily done if the significant change is toward the norms. 1 Burke & Murphy. Nursing ’90. May 1990. 1