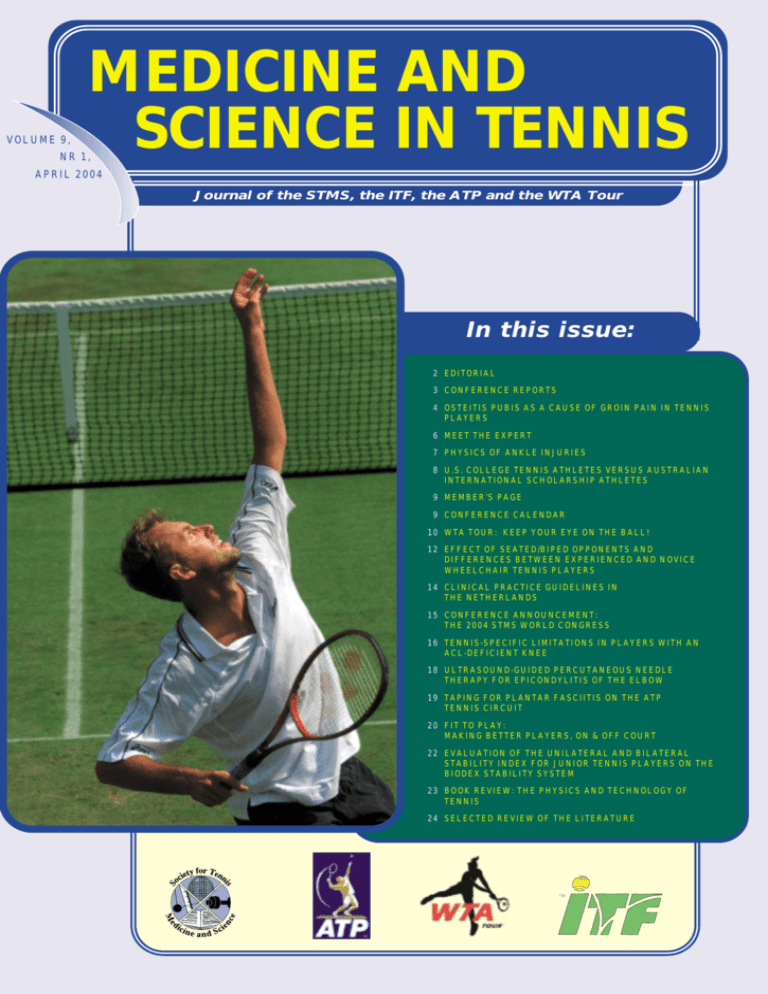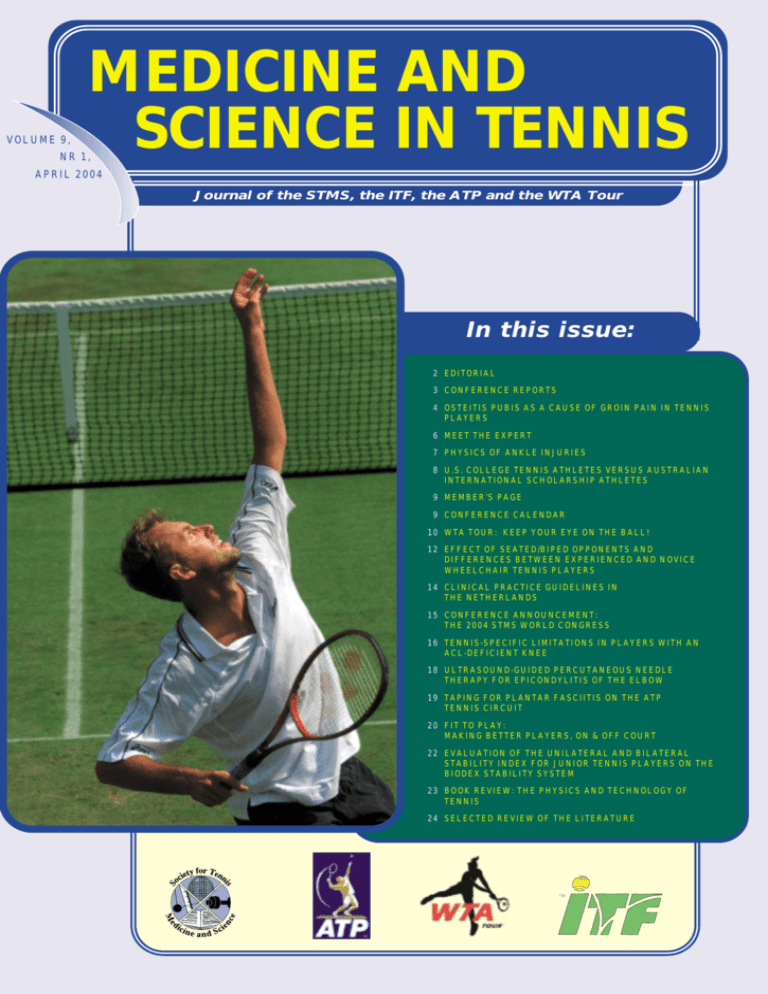
VOLUME 9,
MEDICINE AND
SCIENCE IN TENNIS
NR 1,
APRIL 2004
Journal of the STMS, the ITF, the ATP and the WTA Tour
In this issue:
2 EDITORIAL
3 CONFERENCE REPORTS
4 OSTEITIS PUBIS AS A CAUSE OF GROIN PAIN IN TENNIS
PLAYERS
6 MEET THE EXPERT
7 PHYSICS OF ANKLE INJURIES
8 U.S. COLLEGE TENNIS ATHLETES VERSUS AUSTRALIAN
INTERNATIONAL SCHOLARSHIP ATHLETES
9 MEMBER’S PAGE
9 CONFERENCE CALENDAR
10 WTA TOUR: KEEP YOUR EYE ON THE BALL!
12 EFFECT OF SEATED/BIPED OPPONENTS AND
DIFFERENCES BETWEEN EXPERIENCED AND NOVICE
WHEELCHAIR TENNIS PLAYERS
14 CLINICAL PRACTICE GUIDELINES IN
THE NETHERLANDS
15 CONFERENCE ANNOUNCEMENT:
THE 2004 STMS WORLD CONGRESS
16 TENNIS-SPECIFIC LIMITATIONS IN PLAYERS WITH AN
ACL-DEFICIENT KNEE
18 ULTRASOUND-GUIDED PERCUTANEOUS NEEDLE
THERAPY FOR EPICONDYLITIS OF THE ELBOW
19 TAPING FOR PLANTAR FASCIITIS ON THE ATP
TENNIS CIRCUIT
20 FIT TO PLAY:
MAKING BETTER PLAYERS, ON & OFF COURT
22 EVALUATION OF THE UNILATERAL AND BILATERAL
STABILITY INDEX FOR JUNIOR TENNIS PLAYERS ON THE
BIODEX STABILITY SYSTEM
23 BOOK REVIEW: THE PHYSICS AND TECHNOLOGY OF
TENNIS
24 SELECTED REVIEW OF THE LITERATURE
ISSN: 1567-2352
EDITORIAL
Medicine and Science in Tennis is a Journal produced by the Society
for Tennis Medicine (STMS) in co-operation with the ITF, the ATP, and
the WTA Tour, and is issued three times a year (April, August, and
December). The STMS is an international organization of sports
medicine and science experts aiming to serve as an international forum
for the generation and dissemination of knowledge of tennis medicine
and science.
Dear tennis friends,
I would like to welcome you all to the April issue of
Medicine and Science in Tennis. In this issue you will
find our first Members’ News page (page 9).
Members’ news is designed for members to let them
keep up-to-date on issues and events of interest to
STMS members. Members’ News is also the first step
towards increasing the benefits of being an STMS
member.
You can learn more about the medical ins and outs of the Wimbledon
Championships on page 6, where we introduce to you our medical
Wimbledon expert, Dr. Peter Tudor Miles. Peter has been the Medical
Director of the Wimbledon Championships for more than 25 years, and is
as familiar to Wimbledon Watchers as Strawberries and Cream. If reading
this interview has aroused your interest and you would like to visit
Wimbledon in person, do not hesitate! You can now sign up for our 2004
STMS World Congress, to be held in conjunction with the Wimbledon
Championships. You will be able to interact with world-renowned medical
experts in the field of tennis, and attend one of the first two days of the
Wimbledon Championships. Don’t miss it!
The spate of injuries at the Australian Open prompted two experts to look
into these matters more closely. Rod Cross focused his research on ankle
injuries in relation to the court surface and came up with both the cause
and the solution to these injuries (page 7). Dr. Tim Wood, Chief Medical
Officer of the Australian Open, discusses osteitis pubis as a cause of groin
pain in tennis players, and presents a very well-designed rehabilitation
programme (pages 4 and 5). More original research included in this issue
are: Dr. Marks’ study on physical performance profiling; the visual response
of wheelchair tennis players; limitations of tennis players with an
ACL-deficient knee and percutaneous needle therapy as a treatment modality for tennis elbow. The medical staff of the ATP and the WTA both contributed with very practical articles on eye protection and taping for plantar
fasciitis, respectively.
Currently, the WTA is conducting a 10-Year Review of the Age Eligibility
Rule. This 10-year Age Eligibility process is being spearheaded by the Age
Eligibility Advisory Panel, a panel of independent international experts in
the field of sports sciences and medicine. The panel has been advisory to
the WTA Tour regarding appropriateness of the current rule and the development of the programs with the ultimate goals being to promote career
longevity, fulfilment and the overall well being of players on the WTA
Tour. The four major components that comprise the 10-Year AER Review
include: a tennis wide survey, conducted by questionnaires and open forum;
data collection; medical literature review; and development of an evidencebased consensus statement that will be advisory to the WTA. The open
forum was held from 26th-28th March in Miami. In the next issue of
Medicine and Science in Tennis we hope to be able to present you the outcome of the Review.
THE INTERNATIONAL BOARD OF THE STMS
President:
Babette M. Pluim, Arnhem,The Netherlands.
Vice President:
Marc R. Safran, San Francisco,CA,USA;
Secretary:
Javier Maquirriain, Buenos Aires, Argentina;
E-mail: info@stms.nl
Membership Officer:
Alan Pearce, Melbourne, Australia;
E-mail: membership@stms.nl
Treasurer:
George C.Branche III, Arlington, VA, USA;
Past-president:
Per A.F.H. Renström, Stockholm, Sweden;
Other members:
Peter Jokl, New Haven, CT, USA;
W. Ben Kibler, Lexington, KY, USA.
Savio L-Y Woo, Pittsburgh, PA, USA
Associates to the Board:
Miguel Crespo, Representative of the ITF;
Kathy Martin, Representative of the WTA Tour;
Gary Windler, Representative of the ATP.
North American Regional Committee:
Chairman: Marc R. Safran, San Francisco, CA, USA;
Peter Jokl, New Haven, CT, USA;
W. Ben Kibler, Lexington, KY, USA;
Michael F. Bergeron, Augusta, GA;
William Micheo, San Juan, Puerto Rico;
Carol L. Otis, Los Angeles, CA, USA;
E. Paul Roetert, Key Biscayne, FL, USA;
Savio L-Y. Woo, Pittsburgh, PA, USA.
EUROPEAN REGIONAL COMMITTEE
Chairman: Giovanni di Giacomo, Rome, Italy, Chairman;
Gilles Daubinet, Paris, France;
Hartmut Krahl, München, Germany;
Hans-Gerd Pieper, Essen, Germany;
Babette Pluim, Arnhem, the Netherlands;
Angel Ruiz-Cotorro, Barcelona, Spain;
Michael Turner, London, United Kingdom;
Reinhard Weinstabl, Vienna, Austria.
SOUTH AMERICAN REGIONAL COMMITTEE
Chairman: Rogério Teixeira Silva, São Paulo,Brazil;
Javier Maquirriain, Buenos Aires, Argentina.
SCIENTIFIC COMMITTEE
Chairman: W. Ben Kibler, Lexington, KY, USA;
Michael F. Bergeron, Augusta, GA, USA;
Bruce Elliott, Perth, Australia;
Karl Weber, Cologne, Germany;
Savio L-Y. Woo, Pittsburgh, PA, USA.
EDUCATIONAL COMMITTEE
Chairman: Marc. R. Safran, San Francisco, CA, Chairman;
George C.Branche III, Arlington, VA, USA;
Henrik Ekersund, Gothenburgh, Sweden;
Stacie Grossfeld, Louisville, KY,USA;
Peter Jokl, New Haven, CT, USA;
W. Ben Kibler, Lexington, KY, USA;
Kathy Martin, Melbourne, Australia;
Fernando Segal, Buenos Aires, Argentina;
Piotr Unierzyski, Poznan, Poland;
Gary Windler, Summerville, SC, USA.
Editorial Board:
Editor-in-Chief: Babette M. Pluim;
Todd Ellenbecker, Scottsdale, AZ, USA;
Javier Maquirriain, Buenos Aires, Argentina;
Rogério Teixeira Silva, São Paulo, Brazil
Alan Pearce, Melbourne, Australia;
Gary Windler, Summerville, SC, USA;
EDITORIAL OFFICE:
PO Box 302, 6800 AH Arnhem,
The Netherlands.
Phone +31-26-4834440
Fax +31-26-4834439
E-mail: editor@stms.nl
MEMBERSHIP OFFICE:
Alan Pearce, Ph.D.
C/o Tennis Australia
Private Bag 6060
Richmond South
Victoria 3121
Australia
T + 61 3 9286 1177
F + 61 3 9650 2743
E-mail: membership@stms.nl
Full membership: $100.00
Associate membership $ 50.00
Student membership $ 35.00
MEMBERSHIP PAYMENTS:
Commonwealth Bank of Australia
Richmond 242 Bridge Road
Richmond, Victoria, 3165
Australia
Routing # (BSB #) 063-165
Account # 10287882
PHOTOGRAPHERS:
Michael Kooren, Arjan Verbruggen
FRONT COVER:
LeAnn Silva, ATP, Ponte Vedra Beach, Fl, USA
CIRCULATION: 2,400
Babette Pluim, MD, PhD
President STMS
PUBLISHING OFFICE:
Modern BV, Bennekom, The Netherlands
WEBMASTER:
Ivo Wildeman, Hilversum, The Netherlands
E-mail: webmaster@stms.nl
Website: http://www.stms.nl
The newsletter ‘Medicine & Science in Tennis’ is supported by:
Disclaimer:
This journal is published by the Society of Tennis Medicine and
Science for general information only. Publication of information in the
journal does not constitute a representation or warranty that the
information has been approved or tested by the STMS or that it is
suitable for general or particular use. Readers should not relay on any
information in the journal and competent advice should be obtained
about its suitability for any particular application.
© 2003 Society of Tennis Medicine and Science. All rights reserved.
No part of this publication may be reproduced in any form without
prior written permission of the copyright holder. Opinions and research
expressed in this journal are not necessarily those of the STMS.
MEDICINE
& SCIENCE
IN
TENNIS 2
CONFERENCE REPORT:
12th Argentine Sports Medicine Conference
Tennis Science Symposium
T
Javier Maquirriain and Fernando Segal
he 12th Argentine Sports Medicine
Conference was held in Buenos Aires on
September15th. The scientific meeting was
organised by the Argentine Society of Sports
Medicine and the Gatorade Sports Science
Institute.
Dr. Juan Carlos Mazza, a renowned sports
scientist and chairman of the scientific
committee organised an interesting program including different sports-specific
sessions.
The Tennis Science Symposium was
co-ordinated by Javier Maquirriain (MD),
Argentine Tennis Association Medical
Director.
Professor Javier Capitaine opened with
“Physical conditioning for the elite tennis
player”. Capitaine is recognised for his
strength and co-ordination training
expertise. Professor Luis Erdociain then
presented an interesting lecture on
“Perception, attention and visual training
for tennis player” and psychologist
Fernando Vazquez lectured on
“Psychological profile of successful tennis
coaches”. The second part of the symposium began with the presentation
“Nutritional demands of the tennis player”
by Dr. Juan Carlos Mazza. Fernando Segal
(International tennis coach) presented the
final talk on “Developmental basis for
junior tennis players”.
High level of lecturers, interesting discussions and a one-hundred attendance
helped to constitute a successful scientific
meeting which also shows the growing
interest in Tennis medicine and science.
Sponsorship: Gatorade Sports Science
Institute, Temis Lostalo Laboratories,
Sevier Laboratories.
Australian Tennis Conference Report – 2004
he 9th Australian Tennis Conference
held just prior to the Australian Open
was a great success with about 300 coaches
and other industry professionals in attendance from around the globe. The theme of
this year’s conference was “Achieve More in
2004.” Several topics focussed on the competitive challenges our sport faces in the
21st Century. After a welcoming address
from the President of Tennis Australia,
Geoff Pollard, participants were treated to
an outstanding presentation from Jim
Stynes, one of Australia’s best Aussie Rules
players who focussed on the importance of a
coach’s role as a character mentor for young
people. Dan Santorum from the PTR then
followed and inspired us all with his talk
about The Coach - the key to tennis development. Another topic – The Coach – the
key to club success, was delivered by a panel
of selected successful coaches from around
Australia. A common theme that developed
from these sessions was the pivotal role
coaches play in developing grassroots tennis
and ensuring the future delivery of tennis to
all participants so it remains a major participation sport.
T
Canberra helped coaches themselves plan
recovery strategies to prevent burnout.
There were also a host of other tennis
coaching specialists.
During the traditional Conference Dinner
held at Royal South Yarra Tennis Club,
attendees heard from one of the legends of
Australian Tennis – Peter McNamara, who
kept everyone thoroughly entertained with
his recollections with life on the Tour
playing and coaching.
As in previous years, the calibre of presenters was world class. With a mixture of on
court sessions, workshops and indoor
forums, attendees saw presentations from
internationally renowned names such as
Professor Bruce Elliott who presented the
latest research in biomechanics, Miguel
Crespo from the ITF who provided an
entertaining session on court of psychological drills, Dr Ann Quinn helped us to
Prepare to Win, and Dr Paul Roetert from
the USTA taught us how to recognise and
develop potential and be dynamically flexible. Angie Calder from the University of
Feedback has been very positive and
thanks have been extended to the
Australian Tennis Conference Committee
who worked tirelessly to ensure another
success. Hope we can see you down under
in 2006 when our conference will be held
in conjunction with the Australian Open
and the STMS World Congress. Mark your
calendars now and come and enjoy some
great tennis and Aussie hospitality whilst
learning the latest research and coaching
methods from around the world.
Professor Bruce Elliott
MEDICINE
& SCIENCE
IN
TENNIS 3
ORIGI
RESE NAL
ARCH
Osteitis Pubis as a Cause of Groin Pain
in Tennis Players
DR TIMOTHY WOOD, CHIEF MEDICAL OFFICER OF THE AUSTRALIAN OPEN, E-MAIL GEORGEWOOD@BIGPOND.COM
uring this year’s Australian Open, two
tennis players (male) were diagnosed
with osteitis pubis. In both cases they had
had symptoms for more than six months
and one had had surgery to repair an
inguinal hernia, the presumed cause of his
pain. His symptoms had recurred as soon
as he resumed high intensity court work.
D
Groin pain is a relatively common complaint amongst tennis players and recently
the hip joint, and more specifically labral
tears, have been in the spotlight.3
Previously most groin pain has been attributed to pathology in the adductor tendons,
either acute or chronic or ‘occult’ inguinal
hernia.1 Whilst it is important to systemat-
ically check for all potential causes of groin
pain,2 it is important to include osteitis
pubis in that list. Whilst probably more
prevalent in sports which involve kicking,
e.g. soccer, where repetitive rotational
stresses are placed on the symphysis pubis,
tennis nevertheless does place significant
stress through this and surrounding structures.
The primary pathology in osteitis pubis
appears to be in the bone (GVerrall –
personal communication) which progresses
to involve the joint, including the cartilaginous disc, and may involve the multitude of
entheses in the region. These changes are
initially best appreciated on MRI, although
later CT scanning gives a better picture of
Figure 1 The squeeze test
the specific bony pathology.
Clinically the ‘squeeze’ test seems to give
the best reliability in diagnosing the condition. A clenched fist is held between the
knees at varying degrees of hip flexion and
the patient is asked to perform an isometric contraction of their adductors
(Figure 1). Two observations should be
noted. Firstly, the patient should state that
the manoeuvre reproduces their pain.
Secondly the examiner should note the
strength of the contraction. Many patients
will have very weak adductors if they have
had osteitis pubis for a significant period
of time. Alternatively a blood pressure cuff
inflated to 20 mmHg can replace the fist
and the maximal pressure reached by the
patient is measured. Normal pressures
achieved by asymptomatic individuals
would be expected to be above 120-140
mmHg. Chronic osteitis pubis sufferers
often can only achieve 60-80 mmHg
(DYoung – personal communication).
Local tenderness over the pubic bones is
thought to be too unreliable to use as a
test of osteitis pubis and is not recommended as a valid diagnostic finding.
Restricted hip internal rotation is thought
to be a risk factor for osteitis pubis in susceptible athletes (Figure 2).4
Once a diagnosis of osteitis pubis has been
made then a comprehensive rehabilitation
programme needs to be carried out. Such
a programme has arisen in Australia due to
the common prevalence of osteitis pubis in
Australian rules footballers (Table 1).
Strict adherence to it has yielded encouraging results but there are still players who
will struggle and some come to surgery to
debride the symphysis pubis. Newer treatments including intravenous bisphosphonates are currently being trialed.
In summary, in assessing a player with
groin pain, it is important not to forget
ostatis polio in the list of differential diagnoses. Early diagnosis allows the institution of an appropriate programme and
hopefully minimise time away from competition.
References
1. Gilmore J. Clin Sports Med 1998;17:
787-93
2. Lovell G. Aust J Sci Med Sport 1995;
27(3):76-9
3. Narvani A et al. Br J Sports Med 2003;
37:207-211
4. Williams J. Br J Sports Med 1978;12:
129-133.
Figure 2 Internal rotation of the hip
SPORTS MEDICINE
ABOUT THE AUTHOR
Tim Wood is Chief medical officer of the
Australian Open since October 2001 and a
medical consultant to Tennis Australia since
2002. He is a member of Tennis Australia
anti-doping review board and member of
the ITF Sports Science and Medical
Commission. Dr. Wood is a sports physician
in fulltime private practice in Melbourne.
& SCIENCE
IN
TENNIS 4
SPORTS MEDICINE
& SCIENCE
IN
TENNIS 5
Isolation Trans
Abd & Pelvic Floor
Local Tissue
therapy
Core Stability
Knees apart in
(all planes)
Standing in
bilateral stance
Upper body
(sit, lying)
Not indicated
Sport specific
Challenge via
‘sliding’
Swiss Ball, Pilates
‘challenging’
The same, if
required
consider nsaids
Run alternate days
Stage 5
Controlled
Change of
Direction
Off Court - Gym
Single leg stance
Ease back as start
running drills
Glut max-squat
Adductors-pulley
On Court - Hit up
Short duration
Fitness testing
Set new goals
Increase effort
strengthendurance
Off Court - Gym
Start hitting up
Single leg squat
Lateral lunge
Self Massage
Sustained stretch
Practice warm up
Challenge via
balance
Fatigue resistance
Conditioning ++
Standard Recovery
(cold water etc)
Non-weight
bearing rest after
Session
Stage 6
Uncontrolled
Change of
Direction
Split lunge
Adductor Magnus
Massage adductor Massage adductors
before+/- after run
+/- TFL/Hip F/QL
Stretch the same
Stretch the same
Sideways shuttles
Walk, 1/2 squat
+ lateral movt.
Swiss Ball ‘easy’
Ice massage
adductor after run
100 m run thru
10 m accel/decel
Stage 4
Straight-line
Running
QL = quadratus lumborum
PNF = proprioceptive neuromuscular fascilitation
Cross train
Cycle/Versa etc
Swim
(pool buoy)
Not indicated
‘pain’
Cardio-vascular
fitness
TFL = tensor fascia lata
Hip F = hip flexors
Theraband
Adductors
Isometric
Adductors
Pain inhibited!
Muscle strength
PS = pubic symphysis
MVC = minimal voluntary contraction
Cont Massage
Stretch Hip F,
hams,quads, calf
Add Massage of
TFL, Gluts
Single leg stance
Inner unit + single
leg stance
Ice, PNF
Massage
Adductors
Squeeze the ball
Inner unit
(sit, stand, lie)
Muscle length
(don’t stretch
adductors)
Low MVC
Co-contraction
Nsaids,
ice massage
electrotherapy
Unload
Abd-Add
Synergy
Keep knees
together
Pelvic sacro iliac
belt
Reduce adductor
tone
Modules
Stage 3
Exercise out
of PS neutral
If delayed,
If settle slowly,
consider prolotherconsider infiltration
apy
Stage 2
Exercise in
PS Neutral
Stage 1
Unload & Local
Tissue Therapy
Table 1 Example of Conservative Rehabilitation for Osteitis Pubis for Tennis – Adapted from Hogan (personal communication)
Be aware of
fatigue/pain
Limit running to on
court ie don’t run
to get fit
Taper off
Massage before
and after training
Include in
warm-up
Maintain inner
unit awareness
No nsaid masking
Plan recovery days
Stage 7
Resume
Training
MEET THE EXPERT
Dr Peter Tudor Miles
MEDICAL DIRECTOR, THE CHAMPIONSHIPS, WIMBLEDON
CHIEF MEDICAL ADVISOR, THE ALL ENGLAND LAWN TENNIS CLUB (AELTC)
and ultrasound scans. They bring a
color enhanced, state of the art ultrasound scanner on site and take the
images and interpret them in front of
the players and doctors. The MRIs,
radiographs, and isotope scans are done
off site.
My role is to provide general medical
services ( non-injury) care to players,
and for key tournament staff. There are
around 6000 temporary staff. I also run
the whole medical team administration.
There are two nurses who act as nurse/
receptionists. There are also two remedial gymnasts. They supervise the gym
and provide some educational input to
players/coaches and managers (who
often need some guidance on best
practice in using the gym/equipment) .
Dr. Peter Tudor Miles
last of a series of four interviews
doctors who work for the grand
Islamnwiththetournaments,
Medicine and
Science in Tennis talks to Peter Tudor
Miles. Dr. Tudor Miles has recently
announced his retirement from General
Practice and from his role as the
Medical Director for the Wimbledon
Championships. He has co-ordinated
and managed the medical cover for
Wimbledon for over 25 years and is as
familiar to regular Wimbledon
Watchers as Strawberries and Cream.
1. What is your specialty?
Family medicine. I have been a
Principal in a family medicine practice
since 1972 in Wimbledon Village and
Senior partner since 1986. This is a
group practice with five partners. It is
also a training practice and I was the
accredited trainer.
I was first Secretary and then Chairman
of the South London Faculty of the
Royal College of General Practitioners (
350 members).
2. For how long have you worked as a
tournament doctor?
Twenty eight years. I was the only doctor at the Grand Slam Wimbledon for
players from 1975 -1999 inclusive. In
1999-2000 I had the opportunity with
the Tournament Diector to build a
team as the All England built the players and Members a new £ 20,000,000
pound facility with a new medical
centre.
We appointed two full time Sports
Medicine specialists (Mark Batt and
Philip Bell) and two radiologists who
report all the plain radiographs, MRIs
3. What is your regular job?
I retired as a Family Physician in March
2003.
4. Which tournaments do you cover?
The All England Championships only.
In the 1970s and early 1980s I did provide medical cover for the English
Davis cup team when playing at home
on a number of occasions and the
Wightman Cup
(USA versus UK, ladies ) for home
events but not in the USA. I covered
no other tennis events.
5. How did you first become involved
in providing medical cover for
tennis tournaments?
I stood in for a sick colleague at
Wimbledon and I suppose the All
England decided they could put up
with me!
6. Are you responsible for the general
public as well?
No, I am not responsible for the public.
The public are cared for by a separate
team of volunteers from St John’s
Ambulance organisation. Each day,
there are two doctors and around 15
nurses.
7. What changes have you made over
the years that have had the greatest
positive impact on care for players at
tournaments?
The appointment of a comprehensive
team in 2000, in new premises. Now
we have two full time sports physicians,
two radiologists, two nurse/receptionists, and a chiropodist/podiatrist, two
remedial gymnasts, in addition to the
pre-existing complement of physiotherapists.
MEDICINE
& SCIENCE
IN
TENNIS 6
8. Do you foresee any significant
changes in the future in terms of
care for professional tennis players
at tournaments?
Yes, If possible for faster rehabilitation
through the agency of enhanced physical therapy. The possibility to provide
individual players with some educational input on injury prevention in collaboration with coaches/managers. Time
would be a problem!
9. Is there a difference in the medical
care of male and female athletes?
Difficult question. The factor that
mainly springs to mind is the relative
immaturity of some very young female
athletes who need great sensitivity in
approaching their problems and often
acting as an advocate for them.
Coaches, managers and families may
load unreal expectations and pressures
onto the athlete.
10. What is the most interesting
medical problem you have
encountered?
The one that caused the most tension
pre-event was gender assignation. A
male karyotype who put in an entry for
the ladies singles. It was decided on the
karyotype that this applicant was male
and could not compete as a female
despite his/her gender re-assignation/
surgery etc.
On court, a suspected re-entrant tachycardia re-occurence was in a men’s
semi-final on court when the players
felt faint and had to come off court for
evaluation. He had had a cardiac ablation procedure for a previous event and
we and the ATP medical teams were
quite unaware of this! The ATP medical
data protocols at the time allowed for
no prior notification of any pre-existing,
potentially serious/fatal illnesses to be
communicated to tournament physicians. This was felt then to be a possible
breach of confidential medical information if provided.
I argued with the ATP medical committee that this information should be
made known to the doctors responsible
for player medical care (in confidence)
for safe medical care .
Only information on serious illness
which might require emergency medical action, so called “ Red Flag events “
The ATP have actioned this. Players are
now sent an annual questionnaire
specifically asking them to give the ATP
medical teams any new/changing information re: “ Red Flag events”.
ORIGI
N
RESE AL
ARCH
Physics of Ankle Injuries
ROD CROSS, PHYSICS DEPARTMENT, SYDNEY UNIVERSITY, SYDNEY, AUSTRALIA
ABOUT THE AUTHOR
Rod Cross is an Associate Professor in
physics at Sydney University and co-author
of the book The Physics and Technology of
Tennis with Howard Brody and Crawford
Lindsey (see photo). His main research
interest is the physics of tennis equipment.
A more recent interest is the physics of
falling off cliffs and high buildings.
shows that a vehicle is more likely to roll
over as it rounds a bend if it has a high
centre of gravity and a narrow wheel base.
Similarly, a tennis player (or a soccer player or a basketball player) is more likely to
roll the ankle if the shoe is narrow or has a
thick sole (raising the centre of gravity) or
if there is a high COF between the shoe
and the court surface. The vertical reaction force from the court acts up through
the middle of the shoe when a player is
standing upright, but it shifts towards the
outside edge of the shoe if the player
pushes down and sideways. If the player
pushes hard enough the reaction force
shifts to the extreme outside edge. Any
harder and the foot will roll.
Rod Cross, Crawford Lindsey and Howard Brody
he spate of ankle injuries leading up to
the Australian Open this year prompted a lot of comment concerning the fact
that Rebound Ace becomes sticky in hot
weather. The physics of this is quite interesting and is illustrated in Figure 1. If a
player pushes down and sideways on a
shoe then there are several possible outcomes, including the fact that the foot can
roll or tip over as illustrated. The vertical
component of the force is opposed by a
vertical reaction force from the court, and
the horizontal component is opposed by
the friction force acting between the shoe
and the court. If these forces are in balance
then the shoe can’t move vertically and it
can’t move horizontally. The shoe might
still be able to rotate, but under normal
conditions the total torque (due to the
various forces on the shoe) will also add
up to zero. However, if the force on the
shoe is big enough then the shoe will
either slide along the court or it will roll
over, depending on the coefficient of
friction (COF) between the shoe and the
court.
T
over depending on where you push it. The
packet will slide if you push it near the
bottom but it will probably tip over if you
push it near the top (as in Figure 2). It will
certainly tip over if there is a large COF
between the packet and the table. The
mathematics and the physics of this shows
that the packet tips over more easily if the
COF is large, or if the packet has a high
centre of gravity, or if the packet is relatively narrow. The same mathematics
Figure 1
On a clay court the COF is small since
small particles under the shoe act a bit like
ball bearings, and the shoe will slide. The
COF between a tennis ball and a clay
court is actually very large, which is why
clay courts are so slow, but the COF is
small between the court and a shoe. On a
rough-textured hard court the COF is
large and there is a much greater chance
that the shoe will rotate about the outside
edge, with unpleasant consequences.
The difference between sliding and rolling
is easily demonstrated with a packet of
cornflakes on a table. If you push sideways
on the packet, it will either slide or tip
Figure 2
MEDICINE
& SCIENCE
IN
TENNIS 7
Conclusion
Inventing better shoes based on these principles is unlikely to be very profitable.
Such shoes would suit mainly top players
competing on hard courts. Average players
and many professionals make the mistake
of wearing the same type of shoe on all
surfaces. Top players don’t ask how much
shoes cost. They ask how
much they will be paid to wear them.
ABST
Physical Performance Profiling:
RACT
U.S. College Tennis Athletes versus Australian
International Scholarship Athletes
BONITA L. MARKS, PH.D., FACSM, ELIZABETH W. GALLEHER, B.S., MIKIKO SENGA, B.S, LAURENCE M. KATZ, M.D., FACEP
UNIVERSITY OF NORTH CAROLINA AT CHAPEL HILL, DEPTS. OF EXERCISE AND SPORT SCIENCE AND EMERGENCY MEDICINE,
CHAPEL HILL, NC 27599-8700, E-MAIL MARKS@EMAIL.UNC.EDU
he physiological demands of competitive tennis necessitate the training of both the anaerobic and aerobic energy systems for optimal
tennis performance. Despite this knowledge, there is a surprising paucity of published information about the physical fitness and skill
attributes of competitive tennis players at the U.S. college level. Therefore the purpose of this study was to determine how U.S. college
tennis athletes compared to an international group of competitors. Twenty U.S. college tennis players (11 M, 9 F, 18-23 years old,
average age = 19.5) were invited to participate in a series of evaluations. The U.S. athletes completed university-approved research
participation consent forms. Published performance results from the AIS Tennis Program were used as the comparison group (n = 19;
7 males, 12 females; age: 16-19 years old). Two-tailed Student T-Tests were used to determine significant differences between the
published AIS Tennis Program scores vs. the U.S. scores:
T
Variable
Height (cm)
Body Mass (kg)
Body Fat (%)
Hamstring Flex.(cm)
VO2max (ml•kg-1•min-1)
Vertical Jump (cm)
5 m Sprint (s)
10 m Sprint (s)
Spider Test (s)
Overhead Throw (m)
Lf. Sidearm Throw (m)
Rt. Sidearm Throw (m)
Flat Serve (mph)
U.S. Men
AI.S. Men
180.6 ± 4.6
76.9 ± 7.6
8.2 ± 3.5
45.2 ± 7.3
61.0 ± 4.5*
53.0 ± 9.9**
1.3 ± 0.2**
1.9 ± 0.1
17.1 ± 0.9
12.2 ± 1.3
13.2 ± 0.7**
14.7 ± 1.4*
107.1 ± 3.4**
184.6 ± 6.8
79.2 ± 6.9
7.8 ± 3.0
n/a
56.9 ± 4.8
66.4 ± 9.2
1.1 ± 0.1
1.8 ± 0.1
16.8 ± 1.1
11.9 ± 1.2
16.3 ± 1.7
16.7 ± 1.4
96.7 ± 3.7
U.S. Women
166.1 ± 5.2 [n=3]
58.0 ± 6.4 [n=3]
19.1 ± 5.1 [n=3]
49.8 ± 4.9
n/a
41.8 ± 5.9**
1.3 ± 0.2
2.1 ± 0.2
19.5 ± 1.1**
6.7 ± 0.8**
8.0 ± 0.7**
8.6 ± 0.8**
91.7 ± 5.1*
A.I.S. Women
170.0 ± 5.5
64.9 ± 6.1
18.9 ± 3.5
n/a
55.8 ± 3.3
50.1 ± 5.2
1.2 ± 0.1
2.0 ± 0.1
17.4 ± 0.5
9.5 ± 1.4
12.1 ± 1.3
12.3 ± 1.2
85.7 ± 3.8
* Statistically significant difference, p < 0.05; ** Statistically significant difference, p < 0.001
In conclusion, even though the teams of these particular U.S. college tennis players were ranked among the top 25 NCAA Division I
Tennis Teams, with the exception of the flat serve, this data suggests that the U.S. players could benefit from more specific anaerobic
training. Conversely, the U.S. males were more aerobically trained. A larger, more diverse collegiate sample would be needed to determine how widespread these performance outcomes were nationwide.
Figure 1 Subject performs the sit
and reach test to determine lower
back/hamstring flexibility
Figure 2 Subject demonstrates
a side-arm throw with a 2-kg
medicine ball
Figure 3 Subject prepares for one
of 12 service attempts
Figure 4 Subject having his
quadriceps fatfold measured for
body fat estimation
FROM
LITER THE
ATUR
E
Effect of Type 3 (Oversize) Tennis Ball
on Serve Performance and Upper Extremity Muscle Activity
BLACKWELL J, KNUDSON D
UNIVERSITY OF SAN FRANCISCO, CALIFORNIA, USA
Sports Biomech 2002;1(2):187-92
his study investigated the effect of the
larger diameter (Type 3) tennis ball on
performance and muscle activation in the
serve.
T
Sixteen male advanced tennis players performed serves using regular size and Type
3 tennis balls. Ball speed, surface elec-
tromyography, and serve accuracy were
measured. There were no significant differences in mean initial serve speeds
between balls, but accuracy was significantly greater (19.3%) with the Type 3
ball than with the regular ball. A consistent temporal sequence of muscle activation and significant differences in mean
MEDICINE
& SCIENCE
IN
TENNIS 8
activation of different muscles were
observed. However, ball type had no effect
on mean arm muscle activation. These
data, combined with a previous study, suggest that play with the larger ball is not
likely to increase the risk of overuse injury,
but serving accuracy may increase compared to play with the regular ball.
MEMBER’S NEWS
Society for Tennis
Medicine and Science
From the Membership Office
I would like to welcome you all to
the first Member’s News page.
Member’s News is designed for
members to keep communicated on
issues and events of interest to
STMS members. Member’s News is
also the first step in creating
greater benefits of being an STMS
member.
We are aiming to have Member’s
News included in each issue of the
Journal of Medicine and Science in
Tennis. However, if demand for
more updates increase, we will
certainly look at having Member’s
News as an email service for
members
Member’s News will be light and
informal in content, however, it will
not be limited to one page.
We encourage members to send
contributions of related events they
wish to publicise, and the more
news and information we have to
distribute, the better I say!
Welcome
New
Members
Mr Richard Bricknell
Mr David Lovejoy
Dr Sharat Kumar Paripati
Please send your contribution of
news and/or information to the
Membership Officer on
membership@stms.nl
I look forward to you contributions!
Mr Carl Petersen
Ms Kristel Schuffelers
Dr Timothy Wood
Dr Atushi Akaike
Dr Shuzo Okudaira
Alan Pearce, PhD
Dr Bonita Marks
Dr Iwasaki Takaaki
THE BENEFITS OF BEING AN STMS MEMBER
STMS was founded as an international
organisation of sports medicine and
science experts aiming to serve as a
forum for the generation and dissemination of knowledge of tennis
medicine and science.
• Opportunity to acquire fellowship
status for services to the STMS
Full Membership benefits include:
• Subscription to three issues per year
of the Journal Medicine and Science
in Tennis
• Subscription to three issues per year
of the Journal Medicine and Science
in Tennis
• Dedicated member area
CONFERENCE CALENDAR
Please feel free to let other members know of
conferences, seminars, workshops in your
country
19-20 J UNE 2004
6th International Conference on Medicine
and Science in Tennis. Held in conjunction
with LTA Sports Science and Sports
Medicine Conference, London, UK
Information: Dr Michael Turner
Michael.Turner@LTA.org.uk
14-16 A PRIL 2004
Australian Association of Exercise and
Sports Science 2004: From research to practice inaugural conference will be held at
Queensland University Technology,
Australia
Information: www.aaess2004.qut.edu.au
13-16 S EPTEMBER 2004
5th International Conference on the
Engineering of Sport. University of
California, Davis, USA
Information: isea2004@cislunar.com
Associate and Student benefits
include:
• Discounts to STMS meetings
JSMS Tennis Edition
After contact with Sports Medicine
Australia, STMS have some good news
regarding the Journal of Science and
Medicine in Sport (Tennis Edition).
A number of members have enquired
receiving a copy. However with
Dr Alan Pearce changing employment,
records of those who enquired
purchasing a copy were lost in the
move. This is regrettable and STMS
apologises for any inconvenience
caused. If you still wish to have a copy
we are continuing the offer of US$10
per copy (plus postage). Stocks are
limited and this will be the last of the
stock.
Enquires to Dr Alan Pearce on
alpearce@bigpond.net.au
MEDICINE
& SCIENCE
IN
Mr Fernando Segal
Ms Nell Mead
Congratulations . . .
• STMS voting rights
• Discounts to STMS meetings
• Entitlement to use the STMS nomenclature (MSTMS)
Dr Masahiro Horiuchi
TENNIS 9
Congratulations on STMS member
Prof Bruce Elliott who along with Dr
Miguel Crespo and Macher Reid
recently published the ITF Advanced
Biomechanics of Tennis. From all
accounts the text has been well
received internationally.
WTA
WTA Tour: Keep your Eye on the Ball!
KATHY MARTIN, SPORTS PT, AND LAURA EBY, PT, ATC, WTA TOUR, ONE PROGRESS PLAZA, SUITE 1500,
ST. PETERSBURG, FL 33701, USA
eeing the ball clear and sharp is a necessity for top tennis performance.
Educating players about the benefits of,
and encouraging players to adopt the practice of wearing protective eyewear is part
of the preventative, performance enhancing health care process in which the
Primary Health Care Providers of the
WTA Tour engage.
S
The first step in any education process
with tennis players is to provide the facts
in an easy to understand format. With that
aim in mind, the WTA Tour produces a
monthly education topic, ‘Physically
Speaking’ that targets key issues for young
women professional tennis players. The
topics are available at every WTA Tour
event, are posted on the WTA Tour player
extranet, as well as being emailed to players and other key members in the players’
support group, e.g. coaches. The topic of
eyewear for tennis was covered in 2003.
The challenge in this instance is presenting
the material in a way that will influence
and impact upon the prevailing culture.
Within that culture, it is a firmly
entrenched idea that sunglasses are fashion
items only. Tennis players are notorious
for wearing UV protective eyewear everywhere except on the court during matches
and practice!
There is an enormous amount written
about the dangers of exposure to UV
radiation. Most tennis players are aware of
the need for sun protection for the skin in
terms of wearing a hat and application of
sun block. Information collected during
the annual WTA Tour physicals would
indicate that players are increasingly wearing a hat to play and applying sun block to
their face routinely. Less frequently, they
apply sun block to other areas of exposed
skin on the body. It is rare, however that
players are aware of the potential eye
damage related to UV radiation and of the
protective effects of wearing sunglasses;
even rarer is a player who plays tennis in
protective sunglasses.
The sun gives off different types of radiation, including: visible light/sunlight and
invisible radiation known as ultraviolet
radiation, or ‘UV’. It is well documented
that UVA and UVB rays are harmful to
the skin but UV can also have disastrous
effect on the eyes. Eye damage from UV
exposure can include: cataracts, a gradual
clouding of the lens of the eye that leads
to loss of vision; various cancers of the
eyelid and skin around the eye; macular
degeneration, an eye disease that causes
damage to the central retina and is the
leading cause of blindness; and photokeratitis, a painful sunburn of the cornea or
surface of the eye. Reflected sunlight is a
common causative factor in development
of photokeratitis. Reflection from concrete
(e.g. tennis stadiums) is particularly dangerous. Staring directly at the sun can also
permanently scar the retina, and lead to
vision loss. Players must be cautioned
about these risks.
Eye disorders in tennis players are caused
by UV exposure and chronic eye irritation
from dry, dusty conditions. Two of the
most frequently seen are:
1. Pinguecula, which is a yellowish patch
on the white of the eye, usually on the
side nearest the nose, that generally
does not affect vision.
2. Pterygium, which is a fleshy tissue
growth that grows over the cornea of
the eye that can decrease vision.
Pterygia are common in tennis and can
progress from being merely unattractive to occluding vision. The only way
to correct the problem once it is in situ
is to have the tissue surgically removed.
The chances of a pterygium returning
with increased damage are high. Players
post surgery need at least two months
rest; no sun exposure and they must
wear sunglasses for the surgery to have
any chance of success. The only way for
pterygia not to get worse (with or without surgery) is to wear 100% UVA and
UVB protective sunglasses. There is
definitely a case for player education
and to encourage players to wear UV
protective sunglasses.
Eye damage caused by the sun is cumulative and there is evidence to suggest that
children are particularly at risk, due to the
clarity of their lens structure that permits
greater UV and low wavelength (violetblue) visible light penetration than an
adult lens. It is estimated that up to 80%
of the lifetime cumulative UV exposure
occurs before a person reaches 20 years of
age.5 For this reason it is critical that
player education begins early, ideally at
the junior and ITF circuit level.
MEDICINE
& SCIENCE
IN
TENNIS 10
ABOUT THE AUTHORS
Kathy Martin was the Australian Olympic
Team Physiotherapist in 2000, the
Australian Fed Cup Team Physiotherapist
from 1994 to 2000, and Sports Medicine
Consultant to Tennis Australia from 1998 to
2003. She joined the Tour as a Primary
Health Care Provider in 1991. Her current
positions with the WTA Tour include the
Professional Development Department,
Coordinator of the Athlete Assistance
Program, the ‘Partners for Success’ Mentor
Program, the Career Development Program,
and the Player Education Program.
Laura Eby graduated from the University of
Connecticut and became a licensed and certified Physical Therapist / Athletic Trainer in
1989. She has worked for the WTA since
January 1998 as a Primary Health Care
Provider, including two years as Manager of
the Sport Sciences and Medicine Department (2000-2002). Laura’s continuing education in physical therapy has included the
areas of manual therapy, muscle energy,
myofascial release, craniosacral and osteopathic techniques.
To minimise solar radiation exposure of
the eye, ophthalmologists recommend that
sports participants wear an appropriate
sunscreen of Sun Protection Factor 15 or
higher; a hat with a brim to shade the face
and eyes; and appropriate sunglasses. To
protect the eyes and reduce damage
caused by dry atmospheric conditions,
eye-wetting solutions may also help.
The two components of sunglasses, the
frames and lenses, come in an array of
choices.
Frames:
Advise players to select frames that incorporate high performance technology, are
lightweight, and impact resistant. For the
best fit, frames should cover the entire eye
socket, fit close to the face, and come with
padding and non-slip components at the
temple/bridge of the nose. Elasticised
bands work best to hold the frames in
place. The frames should allow the player
to have clear peripheral vision. Wraparound frames offer almost complete UV
protection, whereas regular frames still
allow 5% UV to reach the eyes. Nylon and
plastic are lightweight and are the most
common sport frames. Metal can also
work well. For prescription sunglasses, a
player may be more limited on frame
selection, as some wrap-around frames do
not work well with prescription lenses.
Lenses:
If a player requires prescription glasses,
make sure that they are also wearing prescription sunglasses. Many players’ eye
exams during the annual WTA Tour physicals indicate that they have less than
20/20 vision. Although all these players
are recommended to consult with a qualified optometrist, sports vision optometrist
or ophthalmologist for further testing and
prescription of corrective lenses, many do
not. There is still a culture within professional tennis that discourages the wearing
of any types of lasses. The reasons given by
players relate to: perceived discomfort,
especially in relation to movement of the
glasses with sweating; unfamiliar with
wearing glasses; and the potential for
decreased peripheral vision. This remains
one of the challenges the Primary Health
Care Providers try to overcome when educating the players. Players are reminded
that optimal visual ability directly relates
to on court performance.
All sunglass lenses should be ‘optically
ground lenses’ to provide the clearest
vision. Polycarbonate lenses are super
strong and the only true impact resistant
material for sport; important factors that
will assist in protecting the eye from traumatic injury if direct impact were to
occur. A tennis ball may impact the eye at
immense speeds, up to 200 km/h
(120 m/h) on a serve. That ball is like a
missile if it hits the eye and can cause
debilitating damage that may end a promising career.
There are many varieties of lens available
on the market, some of which are considered below. It is critical that a knowledgeable practitioner directs players to an
appropriate product for tennis.
Ultraviolet Ray (UV) Protection: This is a
must for all tennis players. The American
Academy of Ophthalmology recommends
that sunglasses should block out 99-100%
of UVA and UVB rays for proper eye
protection. Players must be instructed to
check the UV protection information on
the label before buying sunglasses. Players
who wear contact lenses with inherent UV
protection are still recommended to wear
UV protective sunglasses.4 The American
Academy of Ophthalmology advises that
the protective benefits of UV absorbing
contact lenses against UV exposure has
not been established. More research needs
to be done.
Polarisation:
This reduces or eliminates the reflective
glare of surfaces such as a tennis court and
the stands. Polarisation changes the colour
of the lens but it does not protect the
wearer from UV radiation. Players need to
be aware to check the lens is polarised and
provides sufficient UV protection.
Tint:
Tinting is frequently applied to lenses for
the purpose of filtering certain wavelengths of light through the lens, to
improve visual acuity and enhance the
clarity of other colours in the spectrum.
Manufacturers of sunglasses market a blue
tinted lens for tennis, claiming this provides an increase in colour contrast
between the yellow of the tennis ball and
the background of the court. However,
players must be educated that there will
be no benefit when playing on any court
with a greenish or blue green surface, e.g.
most of the hard courts, most of the
indoor courts, the green clay of the USA
and grass courts, where the colour contrast
is questionable how beneficial they are for
tennis players, and most practitioners view
them as a cosmetic option.1
Photo chromatic lenses:
These will lighten or darken depending on
the amount of light present. They may
provide sufficient UV absorption, but as it
takes time for them to adjust to changing
light conditions, they are unlikely to be
effective for tennis players outdoors where
the light conditions can change dramatically in a matter of moments.
may actually be reduced with this kind of
lens. At best, these lenses will provide
improved colour contrast on a red clay surface.3
Additionally, there are concerns about
what effect a blue lens tint has on UV
exposure. Recommendations form the
American Academy of Ophthalmology
indicate that additional retinal protection
is provided by lenses that reduce the transmission of violet-blue visible light. There is
concern that both near-UV and visible
blue light may contribute to macular ageing and degeneration. Blue lenses do exactly the opposite: they admit the violet-blue
end of the light spectrum, and potentially
may be creating more eye damage. With a
blue lens, much of the bright long wavelengths (yellow) end of the light spectrum
is blocked, and the player perceives the
world to be darker. This can result in a relatively dilated pupil, which will increase
the exposure to short (blue) wavelength
light than without any sunglasses. There
may be added risks of blue lenses with
children, due to the higher transmission of
short wavelength light permitted in to the
lens of a young eye.3 It is recommended
that advise about lens tinting for tennis
only be given by a qualified optometrist,
sports vision optometrist or ophthalmologist who is fully conversant with the
impact of tint.
Anti-Reflective Coatings:
These can be another useful choice for
tennis players. In prescription eyewear,
these are used for cosmetic purposes; the
coating makes the lens look thinner, and
reduces the reflection caused by a thick
lens. In sports sunglasses, an anti-reflective
coating helps to reduce glare by decreasing
the reflected light that enters from behind
the sunglasses wearer and bounces off the
lens into the eyes. It is best applied to the
surface of the sunglasses that is nearest the
eye.1
Mirror Coating:
These can provide some additional reduction in intense glare and may be useful in
bright sun situations, like snow skiing.2 It
MEDICINE
& SCIENCE
IN
TENNIS 11
Educating players on the potential risks of
eye damage from exposure to UV radiation and of the potential protective benefits of sunglasses is critical to the players’
eye care, visual acuity and ultimately
impacts upon their on-court performance.
The inclusion of advice and guidance by
qualified optometrists, sports vision
optometrists or ophthalmologists who are
fully conversant with the needs of professional players is part of the education
process. A significant paradigm shift needs
to occur among professional players before
routine wearing of protective eyewear during training and competition is adopted.
The Primary Health Care Providers of the
WTA Tour have begun the process to help
the professional women players make this
change and to adopt better preventative
eye care habits.
References
1. DeFranco L. Do you need lens
coatings? In
www.allaboutvision.com/lenses/
coatings.htm, 2003.
2. Dunleavy BP. Lens choices. Sport
Specs 2003;20:88-89.
3. Marmor MF. Double Fault! Ocular
hazards of tennis sunglasses. Arch
Ophthalmol 2001;119(7):1064-1066.
4. Vinger PF. A practical guide for sports
eyewear protection. Phys Sports Med
2000;28(6).
5. Young S and Sands J. Sun and the eye:
Prevention and detection of lightinduced disease. Clin Dermatol
1998;16:477-485.
Effect of Seated/Biped Opponents and Differences between
Experienced and Novice Wheelchair Tennis Players
RAÚL REINA VAÍLLO,1 FRANCISCO JAVIER MORENO HERNÁNDEZ,1
DAVID SANZ RIVAS2 AND VICENTE LUIS DEL CAMPO1
1 University
of Extremadura, Faculty of Sport Sciences. Laboratory of Motor Control and Learning, Spain
Tennis Federation, Avenida Diagonal 618 2º 2ª, Barcelona 08021, Spain
2 Spanish
O
ne of the objects in studying the visual
behaviour in sport situations is to find
and to establish relationships between the
level of the athlete’s visual skills and his sport
performance.4 Nevertheless, this research
topic has not been extensively explored in the
area of players with disabilities.12 Some studies suggest that a successful performance
requires as much ability in perception as it
does in precise execution of the movement.1,16,20,21 The ability to perceive events
quickly in complex sports situations is an
essential requirement for a skilled performance.
In sports like wheelchair tennis, the player’s
motor response is determined by a temporally
limited situation.13 For instance, we consider
it as effective perceptive behaviour when the
sources of information are reduced to more
important ones. The player needs to perceive
the space-temporary information structure
from the environment to improve his actions.19
Therefore, it is not the quantity of information that will determine the success of the
action, but rather the quality and the speed
with which it is obtained.
An important aim of visual behaviour studies
in sport environments is to increase the spatial validity of these studies, while avoiding
the loss of experimental control. Also, the
perception and the action processes should be
understood as interdependent,7,8 since the
actions are determined by the previous perception process. The separated study of these
processes could create an artificial situation
which does not constitute a reliable measure
of the players´ experience in their sport environment.5 Therefore, the experiments of this
study were carried out in situations that
duplicate the real game environment, where
the players had not only to code and recover
information accurately, but also had to
respond under a pressured game situation.
In order to evaluate the visual search process,
the location of the visual fixations is assumed
to reflect the important cues used in decision-
making, whereas the number and duration of
the fixations are presumed to reflect the
information-processing demands placed on
the performer.19 That is, fixation characteristics are taken as representing the approach
used by the observer to extract specific information from the opponent.
The aims of our study were: a) to study the
visual and motor responses of tennis and
wheelchair tennis players in the return to
serve against biped and wheeler opponents;
b) to study the differences between experienced and novice wheelchair tennis players
Methods
An automated system is applied to study the
perceptive and motor behaviours of tennis
and wheelchair tennis players in a simulation
of return to serve situation, in real situation of
game (three-dimensional) as well as in videobased situation (two-dimensional), through
several technological subsystems.11
a) Visual behaviour. The ASL Eye Tracking
System SE5000 (Applied Sciences
LaboratoriesTM) allows us to obtain an
image with the point of gaze as seen by
the player.
b) Motor response and its precision. This system has been developed from a simulation
system for the training of open sport abilities, also applied in tennis.12 The players
must hit two surfaces located to their right
(forehand stroke) and to their left (backhand stroke) (Figure 1). We obtain values
for reaction time (RT), movement time
(MT) and reaction response (RR).
c) To measure and control the temporal
(speed) and spatial (precision) variability
of the serves.
d) To simulate the return to serve action by
means of video-based apparatus (twodimensional).
Three groups were studied: a) novices wheelchair tennis players (n=7 and less than 2 years
of experience); b) expert wheelchair tennis
players (n=5, included in top 10 Spanish
ranking and with international experience);
Figure 1 Parameters of the reaction response
(RT = reaction time, TM = movement time, RR = reaction response)
MEDICINE
& SCIENCE
IN
TENNIS 12
and c) young tennis players (n=6).
All participants were shown two series of 24
top-spin serves (one series in real game situation and the other one by video-projection),
performed by four right-handed players, two
in biped position and two seated in wheelchairs. The serves were performed to the
“cross” and to the “corner” of the serve square
in a pre-established random order.
Results
We analysed the number of visual fixations
(NF) and the duration of the fixations (TF)
on different body areas of the opponent, racket and ball for the following phases of the
serve: Phase A, as the player separates the
arms until the ball toss; Phase B, until the
head of the racket reaches the lowest point
before the hit; Phase C, until the hit of the
ball; and Phase D, until the ball hits the net
or it bounces on the court.
A repeated measures analysis of variance was
carried out (within-groups). Table 1 shows
the mean scores and the variables with significant differences among biped and wheeler
opponents, both in video-based and in court
situation. In the video-based situation, the
groups perform higher NF and TF on freearm, with higher values among the biped
opponents. On this location there were also
differences in phases A (NFA and TFA) and
B (NFB). In the court situation, only differences in NF and NFB are noted. About the
upper body, there are differences in the number of fixations and in the fixation time on
the racket-arm in the phase C. Finally, there
are many differences in fixation on the ball,
with higher mean values when the serve is
performed by a seated opponent, except in
the values of the phase A (when the hand of
the free-arm holds the ball). There are also
significant differences in the area where the
racket hits the ball (phase D), where the
players point their visual fixation before following the ball’s trajectory. The differences in
this area were obtained both in video-based
(F1,14 = 17.7; p<0.01) and in court situation
(F1,11 = 8.03; p<0.05).
With regard to motor response, another
repeated measures ANOVA analysis revealed
that players in both situations show better
reaction times and reaction responses with
serves directed toward a “forehand” movement (Table 2). For the serves directed
toward a “backhand” movement, there are
only significant differences in the reaction
time in the video-based situation (F1,15 = 5.97;
p<0.05). Another analysis of variance was
carried out between the experienced and
novice wheelchair tennis players. In the
video-based situation, against biped opponents, the experienced group showed higher
fixation time (5.89%) on the racket in phase
C (F1,9 = 5.8; p<0.05) than the novice ones
(1.22%). There are also differences in the fixation time on the upper body in phase A,
both in video-based (F1,9 = 14.31; p<0.01)
and in court situation (F1,9 = 6.6; p<0.05).
Finally, a Pearson correlation analysis between
visual behaviour and motor response data
Table 1 Repeated measures analysis of variance among seated and biped opponents in video-based and court situations for the visual behaviour (NF=number of visual fixation -n-; TF = time of visual fixation -%-)
Location
Measure
Phase
F
Sig.
M Seated
M Biped
Video-Based Situation (2D)
Free Arm
Racket Arm
Upper Body
Ball
NF
TF
NF
TF
NF
NF
TF
TF
NF
TF
NF
TF
NF
TF
NF
TF
–
–
A
A
B
C
C
–
B
B
C
–
A
C
D
D
14.81 (1,14)
8.66 (1,14)
15.18 (1,14)
5.92 (1,14)
8.9 (1,14)
6.88 (1,14)
4.67 (1,14)
5.21 (1,14)
14.02 (1,14)
6.68 (1,14)
7.04 (1,14)
7.12 (1,14)
5.69 (1,14)
6.6 (1,14)
13.63 (1,14)
15.21 (1,14)
0.002
0.011
0.002
0.029
0.010
0.020
0.048
0.039
0.002
0.022
0.019
0.018
0.032
0.022
0.002
0.002
1.27
15.99
1.22
39.27
0.27
0.38
22.48
27.02
0.57
17.55
0.12
44.51
0.11
75.71
3.38
58.36
1.89
23.37
1.80
51.03
0.47
0.57
33.7
32.03
0.88
27.56
0.26
39.99
0.22
63.08
2.66
50.24
–
B
–
–
A
A
D
4.903 (2,11)
10.229 (2,11)
8.895 (2,11)
5.004 (2,11)
27.110 (2,11)
5.359 (2,11)
8.963 (2,11)
0.049
0.008
0.012
0.047
0.000
0.041
0.012
1.41
0.18
22.25
52.34
0.12
1.58
67.61
1.86
0.39
26.02
48.28
0.25
2.83
55.25
Court Situation (3D)
Free Arm
Upper Body
Ball
NF
NF
TF
TF
NF
TF
TF
revealed a significant correlation between the
visual fixation on racket in phase C and the
movement time (cor.=-.971*) against seated
opponents. On the other hand, playing
against biped opponents, another correlation
was obtained between the fixation time on
the arm-racket and the reaction response
(cor.=-.977*).
Discussion and Conclusions
The study has been undertaken from a perception-action perspective, where action is
continuously being coupled to the perceptual
information presented.14,15
The higher visual fixation scores on the ball in
the serves performed by seated opponents
could be due to the fact that the player grabs
the rim of the wheelchair with the free arm,
in order to obtain stability during the serve.
The results obtained for the free-arm and the
ball in the phase A, with higher mean values
among biped servers, could support this
explanation. Nevertheless, it could also be
due to the lesser mobility experienced by the
players seated in the wheelchair, and the
need to acquire information from different
locations of the biped server. Therefore,
against seated opponents, the players perform
a longer pursuit of the ball’s trajectory and
they show lower fixations on the area where
the racket hits the ball. Furthermore, they
employ less time in starting the pursuit of the
ball’s trajectory because the serves of those
opponents was slower than those of biped
servers. This explanation is supported by
higher fixations on advanced areas of the
Table 2 Repeated measures analysis of variance
among seated and biped opponents in videobased and court situations for the motor
response (RT= reaction time; MT= movement
time; RR= reaction response -ms-)
Measure F
Sig.
M
Seated
M
Biped
0.005
0.721
0.077
261.52
156.49
408.93
210.48
151.95
366.51
0.019
0.125
0.008
316.75
147.91
464.41
276.61
139.15
412.93
Video-Based Situation (2D)
RT
MT
RR
10.70 (1,15)
0.13 (1,15)
3.60 (1,15)
Court Situation (3D)
RT
MT
RR
7.32 (1,12)
2.71 (1,12)
9.97 (1,12)
flight ball’s position for the serves performed
by seated players. On the other hand, higher
fixations were obtained in the posterior area
of the flight ball’s position for the serves performed by biped opponents. The higher values in the reaction response against biped
opponents could be due to a greater movement´ width, and it would offer important
cues to help in predicting trajectory before
the serve than it would be the case with
seated servers.13 Therefore, we should avoid
coaching situations where wheelchair tennis
players play against biped coaches/instructors,
since the information that they offer differs
from that which the player would obtain in
real game situation. Regarding the analysis of
the experience of the wheelchair tennis players, the higher fixations on the upper body
performed by the experienced players could
be due to their superior experience in the
sport, and that they are able to collect the
information they need to predict the ball’s
trajectory straightaway. Some authors consider that the motion of the racket before the
contact with the ball is one of the most reliable cues to predict the ball’s trajectory.6,12
The negative correlation between values of
the motor response and the fixation on the
arm-racket indicates that the experienced
players extract information that allows them
to obtain better values of motor response.
It seems that experienced players make better
use of the arm-racket information in order to
respond more quickly during play.17,18 The
implications of these results for learning
processes are important, since we they indicate that we should not only teach players to
guide the point of gaze to those important
cues, but also how they should interpret that
information.1,2 (90 minutes)
References
1. Abernethy B. The effects of age and
expertise upon perceptual skill development in a racquet sport. Res Q Exerc
Sport 1988;59(3):210-221.
2. Abernethy B. Visual search strategies and
decision–making in sport. Int J Sport
Psychol 1991;22:189-216.
3. Abernethy B, Wollstein J. Improving
anticipation in racquet sports. Sports
Coach 1989;12:15-18.
4. Arteaga M. Influencia del esfuerzo físico
MEDICINE
& SCIENCE
IN
TENNIS 13
anaeróbico en la percepción visual. Tesis
Doctoral. Universidad de Granada, 1999.
5. Chamberlain CJ, Coelho AJ. The perceptual side of action: Decision-making in
sport. In: JL Starkes and F.Allard (Eds.).
Cognitive issues in motor expertise.
Amsterdam: Elsevier Science, 1993.
6. Farrow D, Abernethy B. Can anticipatory
skills be learned through implicit videobased perceptual training? J Sport Sci
2002;20:471-485.
7. McMorris T, Beazeley A. Performance of
experienced and inexperienced soccer
players on soccer specific tests of recall,
visual search and decision-making. J
Human Mov Stud 1997;33:1-13.
8. Mestre DR, Pailhous J. (1991). Expertise
in sports as a perceptivo-motor skills. Int J
Sport Psychol 1991;22:211-216.
9. Moreno FJ, Oña A. Analysis of a professional tennis player to determine anticipatory pre-cues in service. J Human Mov
Stud 1998;35:219-231.
10. Moreno FJ, Oña A, Martínez M.
Computerized simulation as a means of
improving anticipation strategies and
training in the use of the return in tennis.
J Human Mov Stud 2002;42:31-41.
11. Moreno FJ, Reina R, Luis V, Damas JS,
Sabido R. Desarrollo de un sistema tecnológico para el registro del comportamiento de jugadores de tenis y tenis en
silla de ruedas en situaciones de respuesta
de reacción. Motricidad. Eur J Human
Mov 2003;10:165-190.
12. Moreno FJ, Reina R, Sanz D, Ávila F. Las
estrategias de búsqueda visual de
jugadores expertos de tenis en silla de
ruedas. Revista de Psicología del
Deporte, 2002;11(2):197-208.
13. Reina R. Estudio de la influencia de la
lateralidad y la posición del oponente en
el servicio de tenis sobre el proceso perceptivo de tenistas en silla de ruedas.
Tesis de Máster (European Master
Degree in Adapted Physical Activity).
Katholieke Universiteit Leuven e Institut
Nacional d´Educació Física Lleida, 2002.
14. Savelsbergh GJP, Van der Kamp J.
(2000). Information in learning to coordinate and control movements: Is there a
need for specificity of practice? Int J
Sport Psychol 2000;31:476-484.
15. Savelsbergh GJP, Williams AM, Van der
Kamp J, Ward P. Visual search, anticipation and expertise in soccer goalkeepers.
J Sport Sci 2002;20:279-287.
16. Singer RN, Williams AM, Frehlich SG,
Janelle CM, Radlo SJ, Barba DA,
Bouchard LJ. New frontiers in visual
search: An exploratory study in live
tennis situations. Res Q Exerc Sport
1998;69(3):290-296.
17. Starkes JL, Allard F. Cognitive issues in
motor control. Amsterdam: North
Holland, 1993.
18. Tenenbaum G. The development of
expertise in sport: Nature and nurture.
Int J Sport Psychol 1999;30:113-304.
19. Williams AM, Davids K, Williams JG.
Visual perception and action in sport.
London: E & FN Spon, 1999.
20. Williams AM, Davids K, Burwitz L,
Williams JG. Perception and action in
sport. J Human Mov Stud 1992;22:
147-205.
21. Williams AM, Davids K, Burwitz L,
Williams JG. Visual search strategies in
experienced and inexperienced soccer
players. Res Q Exerc Sport 1994;65(2):
127-135.
Clinical Practice Guidelines in The Netherlands
THE ROYAL DUTCH SOCIETY FOR PHYSICAL THERAPY (KNGF)
A prospect for continuous quality improvement in physical therapy
ROELOF BOEKEMA PT, HANZEHOGESCHOOL GRONINGEN, DEPT. OF PHYSIOTHERAPY,
VAN SWIETENLAAN 1, 9728 NX GRONINGEN, THE NETHERLANDS. TEL +31 50 595 3763. E-MAIL: R.D.BOEKEMA@PL.HANZE.NL
s a result of international collaboration
in guideline development, The Royal
Dutch Society for Physical Therapy has
translated nine evidence-based clinical
practice guidelines into English to make
the guidelines accessible at an international level. The clinical practice guidelines in
Physical Therapy make it possible for
Physical Therapists to use the guidelines as
a reference for treating their patients.
A
In evidence based clinical practise guidelines, best practise in Physical Therapy
diagnosis and treatment is described, based
on available scientific evidence and experience from clinical practice. Clinical practice guidelines are ‘systematically developed statements to assist both practitioner
and patient when making decisions about
appropriate health care for specific clinical
circumstances’1.
Their purpose is ‘to make explicit recommendations with a definite intent to influence what clinicians do’2. There is some
proof that evidence based guidelines are
instruments to provide insight, both in
quantity as in quality, in the health care
provided. It has been suggested that guidelines are adequate management instru-
ments for continuous quality improvement, quality assurance and continuing
education3.
Currently nine evidence-based guidelines
have been developed and can be downloaded
from our website at:
www.fysionet.nl/index.hmtl?menuIO=62
• Acute ankle sprain
• Chronic ankle sprain
• Stress Urine Incontinence
• Chronic Obstructive Pulmonary Disease
(COPD)
• Osteoporosis
• Low back pain
• Osteoarthritis of hip and knee
• Cardiac Rehabilitation
• Whiplash
Each guideline consists of three parts:
1. a summary in flow-chart or in written
text;
2. the guideline itself, focusing on
Physical Therapy diagnosis and treatment;
3. review of the evidence.
MEDICINE
& SCIENCE
IN
TENNIS 14
For further information, please contact
KNGF, PO Box 248, 3800 AE Amersfoort
The Netherlands. Tel +31 33 467 2900,
fax +31 33 467 2999
E-mail: hoofdkantoor@kngf.nl
Website: www.kngf.nl
References
1. Lohr KN, Field MJ. A provisional
instrument for assessing clinical practice guidelines. In: Field MJ, Lohr KN
(eds). Guidelines for clinical practice.
From development to use. Washington
D.C. National Academy Press, 1992.
2. Hayward RSA, Wilson MC, Tunis SR,
Bass EB, Guyatt G, for the evidencebased Medicine Working Group. Users
guides to the Medical Literature. VII.
How to use clinical practise guidelines?
A. Are recommendations valid? JAMA,
1995;274:570-574.
3. Hendriks HJM, Bekkering GE,
Van Ettekhoven H, Brandsma JW,
Van der Wees PJ, De Bie RA.
Development and implementation of
national practice guidelines: a prospect
for continuous quality improvement in
physiotherapy. Physiotherapy
2000,86,10: 535-547.
CONFERENCE ANNOUNCEMENT
The Lawn Tennis Association (LTA) and Society for Tennis Medicine and Science (STMS)
in collaboration with
The Association of Chartered Physiotherapists in Sports Medicine (ACPSM)
The 2004 STMS World Congress in Tennis
The LTA 2004 Sports Medicine Conference
The LTA 2004 Grand Slam Coaching Conference
The ACPSM 2004 Annual Conference
Saturday 19th and Sunday 20th June 2004
The Millennium Gloucester Hotel
Harrington Gardens
London SW7 4LH
This multi-disciplined Conference will feature parallel sessions for physicians, physical therapists and coaches.
The physicians program will include – internal impingement of the shoulder (Dr Ben Kibler USA, Mr Roger Emery GB,
Dr Marc Safran USA, Dr David Connell AUS), Gilmore’s Groin (Mr Jerry Gilmore GB), Supplements and hydration
(Dr Tim Noakes RSA), Biomechanics and tennis (Prof Bruce Elliott AUS), Juniors (Dr Rogerio Teixera de Silva BRA),
Stress and recovery (Dr Peter Jokl USA), Age eligibility (WTA Age Eligibility Panel), Ice vests in wheelchair tennis
(Dr Paul Castle GB), respiratory disability in tennis (Dr Mark Harries GB), Core Stability (speakers drawn from all those
in attendance)
The physic therapy program will include – the shoulder (Mr Andrew Wallace GB), the tennis player’s elbow and wrist
(Mr Nicholas Goddard GB) as well as seminars and practical sessions from Mark Comerford, Mark Bender,
Pete Emerson, Joanne Elphinston, Roger Kerry, Alan Taylor, Seonaid Airth and Stephen Mutch.
The coaching programme includes on court sessions with input from – Anne Pankhurst, Prof Bruce Elliott, Craig Tiley,
Todd Ellenbecker, Piotr Unierzyski, Dr Babette Pluim and Dr Ann Quinn.
Venue and Accommodation
All accommodation MUST be booked directly with your chosen hotel. Special conference rates are available at the
Gloucester Millennium Hotel (4 Star De Luxe – 822 rooms)
Tel. No.
+44-207-373-6030
Fax. No.
+44-207-373-0409
E-mail
sales.Gloucester@mill-cop.com
Webpage www.millenniumhotels.com
Registration Fee
The delegate fee will be £350 (500 Euros) with a reduced rate for STMS members and ACPSM members of £280
(400 Euros).
This fee includes attendance at the Conference for 2 days, the Conference Pack, all tea and coffee at the venue and
lunch each day. It does not include accommodation (see above) or the Conference dinner on Saturday 19th June
(which is an additional £50 (75 Euros)).
Registration
Please complete the Registration Form and return it to:
Dr. Michael Turner
The Lawn Tennis Association
Palliser Road,
London W14 9EG,
United Kingdom
Fax. No. +44-207-381-3001
E-mail sarah.hall@LTA.org.uk
Delegates who attend both days of the Conference may request a pass to attend the one of the first 2 days of the
Championships, Wimbledon on Monday 21st or Tuesday 22nd June 2004. The tickets will be allocated on a strictly first
come, first served basis. Passes for the Championships, Wimbledon are issued at the sole discretion of the LTA.
MEDICINE
& SCIENCE
IN
TENNIS 15
Tennis-specific Limitations in Players with
an ACL-deficient Knee
JAVIER MAQUIRRIAIN, MD, PHD., ORTHOPEDIC DEPT, CENTRO NACIONAL DE ALTO RENDIMIENTO DEPORTIVO, BUENOS AIRES,
ARGENTINA. JMAQUIRRIAIN@YAHOO.COM
ABOUT THE AUTHOR
Javier Maquirriain MD, PhD, is an
Orthopaedic Surgeon and Sports Medicine
Specialist working at the Centro National de
Alto Rendimiento Deportivo (Buenos Aires,
Argentina). He is Associate Professor of
Sports Mdicine at Buenos Aires University
and Medical Director of the Argentine
Tennis Association.
he anterior cruciate ligament (ACL) is
the most frequent completely disrupted ligament of the knee. Without treatment, this injury can lead to potentially
debilitating consequences such as meniscus tears, anterior and rotational instability
and early onset of osteoarthritis.6,10
Consequently, most orthopedic surgeons
advocate surgical reconstruction of the
ACL in patients who seek to return to athletic endeavors that depend on high functional demands on this ligament. However,
demands of tennis movements on the ACL
remain unknown and ACL insufficiency
specific related to tennis players has
received limited research interest with
only few mentions in the sports medical
literature.
The aim of this prospective study was to
identify tennis specific subjective limitations in players with an unilateral ACLdeficient knee.
T
Materials and Methods
Sixteen players (mean age 39.93 ± 2.33
years; 2 women, 14 men) with an
unilateral ACL-deficient knee and 16
healthy control tennis players (mean age
38.25 ± 8.47 years; 2 women, 14 men)
were included in this prospective study.
Inclusion criteria for patients were: age
older than 18 years; unilateral isolated
ACL-deficient knee confirmed by clinical
and magnetic resonance imaging (MRI)
evaluation; tennis practice on a regular
basis at any level; and no previous surgery
of either knee. Inclusion criteria for control subjects were: age older than 18 years;
tennis practicing in regular basis at any
level; no previous knee surgery in both
knees. Clinical diagnosis of ACL deficient
knee was supported by history and physical examination through commonly
accepted knee anterior instability tests
(Lachman test, Pivot-shift tests, Anterior
drawer test, etc). Physical exam revealed
no evidence of additional knee joint instability. Diagnosis of acute or chronic ACL
rupture on MRI was based on primary and
secondary signs according to the guidelines
of Valley et al.15
Knee function was evaluated by the modified Lysholm score,14 which generates a
number from 0-100 (highest) and is based
on a series of questions pertaining knee
function. Furthermore, all 16 patients
were asked to evaluate subjectively their
injured knee in relation to their tennis preinjury level in a 0-100% visual scale.
Both groups responded to a questionnaire
regarding tennis specific abilities, adapted
from Mont et al.,8 in the presence of the
author. Each ability was evaluated by a
five-graded scale: 1, “cannot do it”; 2,
“extremely difficult” (pain and instability);
3, “difficult” (instability only and slight
pain); 4, “able to do it with some instability and no pain”; 5, “able to do it with no
pain and no instability”. Any preventing
motion of the previous playing technique
due to mistrust, fear of giving-way or other
knee complaints was graded as 1.
In order to simplify terminology, we
named as dominant knee the homolateral
joint of the serve arm. Statistical significance was stated as follows: alpha
error=0.05, beta error=0.20; power analysis was calculated by appropriate
software.5 Kolmogorov-Smirnov test for
non-parametric variables of small independent samples was used for tennis abilities analysis. Standard statistical package
(Statistics for Windows, StatSoft Inc,
Tulsa, Okla) was used to generate all statistics.
Results
The right knee was affected in 5 (31.25%)
players and the left knee in 11 (68.75%);
5 (31.25%) knees were “dominant” and
MEDICINE
& SCIENCE
IN
TENNIS 16
11 (68.75%) were “non-dominant”.
Players´ injury mechanism of the ACL was
related to soccer (62.5%), skiing (12.5%),
tennis (6.25%), paddle-tennis (6.25%),
rugby (6.25%) and other (6.25%).
The Lysholm score was 85.68±10.37
points in the study group and 100±0.00
points in the control group (p=0.000005,
t-test for independent samples).
Injured tennis players evaluated their functional sport level as 66.87 ± 15.26% compared with their 100% pre-injury level
(p=0.0014, t-test for dependent samples).
Capacities significantly affected in the
ACL-deficient group were: 1) landing
after a smash stroke (p<0.001); 2) stopping abruptly and changing directions
(p<0.001); 3) playing a 3-set singles match
(p<0.05); 4) playing on hard courts
(p<0.001).
No other requested abilities showed statistical significant differences.
Complete tennis ability analysis is shown
in Table 1.
We failed to find any significant relationship between limitations in baseline side
movements (right, left) and ACL-deficient
knee in this group of tennis players.
Only one patient used a rigid knee-brace
for tennis playing. All players played at
arecreational level.
Discussion
The results of this study identified subjective limitations of ACL deficient knee subjects during tennis movements. Tennis
players did not refer significant restrictions
performing the majority of tennis strokes
like forehand, backhand, volleys and serve.
The major limitation was referred to landing after hitting a smash. This task has
been often perceived by ACL deficient
subjects as difficult to perform with confidence.7 Many players from the study
group referred avoidance of this motion.
Interesting correlations may be obtained
regarding tennis player displacement tasks.
Injured players did not have significant
limitations in straightforward run like
“serving and volleying” or “reaching a
drop-shot” movements. In contrast, the
ACL deficient knee tennis player showed
significant limitation with “stop suddenly
and change direction”. This type of stressful deceleration task creates high anterior
loading on the tibiofemoral joint.13 The
external varus-valgus and internal-external
rotations loads placed on the knee joint
increase dramatically during cutting tasks
compared with normal running.2 These
varus-valgus and internal-external rotational moments are believed to be responsible for placing the knee joint ligaments at
a higher risk of injury. Compared with
straight running, the external loads of
flexion, valgus and internal rotation during
sidestepping have the potential to substantially increase the load experienced by the
ACL and medial collateral ligament.2
The ability of normal subjects to perform
deceleration tasks without ACL rupture or
giving way of the knee is attributed to the
coordinated interactions among the ligamentous and other soft-tissue passive
restraints, joint geometry and congruency,
friction between the cartilage surfaces,
active muscular control and the tibiofemoral joint compressive forces.13
As the ACL is considered to restrain
approximately 86% of the shear forces,4
those loads in the ACL deficient knee
must be restrained by the articulating surfaces and surrounding soft tissues.13
Most ACL injuries are indirect in nature
yet occur in contact sports. Tennis
involves tremendous forces during cutting,
pivoting and sudden deceleration maneuvers but ACL injuries are less common in
this sport than in contact sports.11,12 In our
series, most injuries were suffered during
contact sports, like soccer or rugby, but
the exact mechanism (direct vs. indirect)
was not determined. Sallay et al.11 hypothesized that a tennis player is not as likely
to sustain an injury of the ACL because of
the ability of the neuromuscular system to
coordinate muscular function in anticipation of each movement with little surprise
effect. Many authors have indicated that
anticipating a movement can change reflex
response and postural adjustments to minimize forthcoming perturbation and maintain an appropriate posture. Besier et al.1,3
were able to confirm previous hypotheses
that knee joint moments increase under
unanticipated conditions compared with
pre-planned maneuvers, primarily due to a
large increase in varus-valgus and internalexternal rotational moments during the
unanticipated conditions. It is believed
that the unanticipated condition alters the
external moments applied to the knee by
reducing the time to implement appropriate postural adjustment strategies. Tennis
game may have low incidence of indirect
ACL injuries due to absence of frequent
complete twisting maneuvers and high
jumping, and also by giving the player
enough time to anticipate strokes, especially from baseline.
ACL deficient knee tennis players showed
clear incapacity to play on hard courts
where demanding eccentric deceleration
motions are required. It is supposed that
frontal and rotational knee moments are
increased on hard surfaces owing to higher
friction between the foot and the
ground.2,9 Clay courts seem to be a better
option for the ACL deficient-knee tennis
player.
In summary, complete rupture of the ACL
Table 1 Tennis Mobility Subjective Evaluation (adapted from reference 8)
Ability
Bending to hit a shot at knee level
Shifting weight in forehand
Shifting weight in backhand
Shifting weight in first serve
Shifting weight in second serve
Shifting weight in volleys
Shifting weight in smash
Move to right side on the baseline
Move to left side on the baseline
Move forward to reach a drop-shot
Move forward after serve to volley
Stop abruptly and turn direction
Hit a ground-stroke on the run
Play a 3-set match of singles
Play a 3-set match of doubles
Play on hard-court
Play on clay-court
ACL-def. knee
Control
p-value
4.81±0.75
4.43±1.03
4.43±0.89
4.62±0.71
4.75±0.68
4.68±0.79
2.68±1.66
4.43±0.81
4.37±0.88
4.50±1.09
4.75±0.44
3.50±1.15
4.68±0.70
3.93±1.38
4.68±1.01
3.62±1.54
4.81±0.5)
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
5.00±0
p>0.10
p>0.10
p>0.10
p>0.10
p>0.10
p>0.10
p<0.001
p>0.10
p>0.10
p>0.10
p>0.10
p<0.001
p>0.10
p<0.05
p>0.10
p<0.005
p>0.10
Graded scale 1: cannot do it; 2: extremely difficult (pain and instability);
3: difficult (instability only and slight pain); 4:a ble to do it with some instability
and no pain; 5: able to do it with no pain and no instability.
P values obtained by Kolmogorov-Smirnov test for non-parametric variables of small
independent samples
is a debilitating injury that causes significant alterations in knee joint kinematics.
Untreated patients have been associated
with joint instability, chronic articular
degeneration and knee dysfunction.
Despite the problems associated with
questionnaire studies, we clearly identified
specific limitations related to complete
isolated ACL rupture. The ACL deficient
knee tennis player showed significant
impairment of subjective overall sport performance, inability to land after smashing,
inability to stop and turn direction, inability to play a 3-set singles match and inability to participate on hard courts, compared
to healthy controls.
Further studies are needed to determine
the true incidence of ACL injuries in tennis, to analyze knee biomechanics of tennis
motions and to determine improvements
of tennis abilities after ACL reconstruction.
References
1. Besier TF, Lloyd DG, Ackland TR, et
al. Anticipatory effects on knee joint
loading during running and cutting
maneuvers. Med Sci Sports Exerc
2001;33(7):1176-1181.
2. Besier TF, Lloyd DG, Cochrane JL et
al. External loading of the knee joint
during running and cutting maneuvers.
Med Sci Sports Exerc 2001;33(7):
1168-1175.
3. Besier TF, Lloyd DG, Ackland TR.
Muscle activation strategies at the knee
during running and cutting maneuvers.
Med Sci Sports Exerc 2003;35(1):119127.
4. Butler DL, Noyes FR, Grood ES.
Ligamentous restraints to anterior-posterior drawer in the human knee: a biomechanical study. J Bone Joint Surg
1980;62-A:259-270.
5. Castiglia VC. Programa experimental
de cálculos estadísticos VCC 001.
Módulo para estimación de N muestrales.
www.institutodemetodologia.com.
MEDICINE
& SCIENCE
IN
TENNIS 17
6. Hawkins RJ, Misamore GW, Merrit
TR. Followup of the acute nonoperative isolated anterior cruciate ligament
tear. Am J Sports Med1986; 14:
205-210,1986.
7. McNair PJ, Marshall RN. Landing
characteristics in subjects with normal
and anterior cruciate ligament deficient knee joints. Arch Phys Med
Rehabil 1994;75(5):584-9.
8. Mont MA, LaPorte DM, Mullick T, et
al. Tennis after total hip arthroplasty.
Am J Sports Med 1999;27(1):1-5.
9. Nigg BM, Segesser B. The influence of
playing surface on the load on the
locomotor system and on football and
tennis injuries. Sports Med 1988;5(6):
375-385.
10. Noyes FR, Mooar PA, Mathews DS,
et al. The symptomatic anterior cruciate-deficient knee. Part 1. The longterm functional disability in athletically active individuals. J Bone Joint Surg
1983;65A:154-162.
11. Sallay PI, Feagin JA. Basic science of
the crucial ligaments. In: Operative
Arthroscopy, 2nd Ed. McGinty JB,
Caspari RB, Jackson RW, Phoeling
GG. Philadelphia: Lippincott-Raven
Publishers, 1996.
12. Schabus R. Reconstructed anterior
cruciate ligaments in tennis players. In
Tennis: Sports Medicine and Science,
Krahl H, Pieper HG, Kibler WB,
Renström PA (editors). Düsseldorf:
Walter Rau Verlag, 1995.
13. Steele JR, Brown JM. Effects of
chronic anterior cruciate ligament
deficiency on muscle activation patterns during an abrupt deceleration
task. Clin Biomech 1999;14:247-257.
14. Tegner Y, Lysholm J. Rating systems
in the evaluation of knee ligament
injuries. Clin Orthop 1985;198:
43-49.
15. Vahey TN, Meyer SF, Shelbourne
KD, et al. MR imaging of anterior cruciate ligament injuries. MRI Clin
North Am 1994;2(3):365-380.
ORIGI
N
RESE AL
ARCH
Ultrasound-Guided Percutaneous Needle Therapy
for Epicondylitis of the Elbow
MARINA OBRADOV, MD, PHD,1 MONIQUE REIJNIERSE, MD2, PHD,1 MIRJAM JACOBS,PT, AND DENISE EYGENDAAL, MD, PHD3
1Department
of Radiology, 2Department of Physiotherapy, 3Department of Orthopaedics,
Sint Maartenkliniek, 6522 JV Nijmegen, The Netherlands. E-mail: m.obradov@maartenskliniek.nl
ABOUT THE AUTHORS
The Sint Maartenskliniek is a specialized
hospital for orthopaedics in Nijmegen, the
Netherlands. Dr. Obradov, PhD, and Dr.
Reijnierse, PhD, are both senior consultants
at the Department of Radiology and specialises in intervention radiology of the locomotor system. Mrs. Jacobs is a manual therapist of the Department of Physiotherapy
and specialises in sports related injuries. Dr.
Eygendaal, PhD, is orthopaedic surgeon and
specialises in upper limb surgery in athletes.
he evolution of current treatment of
epicondylitis of the elbow is directly
dependent on the understanding of the
true patho-anatomy of tendon failure.
Nirschl defined the histo-pathology of
this entity in precise detail for both
medial and lateral epicondylitis. At the
lateral side the primary patho-anatomic
areas of epicondylitis are located at the
extensor carpi radialis brevis tendon and
in a lesser degree at the anteromedial
edge of the extensor digitorum communis tendon. At the medial side the tendons involved are often the pronator
teres and flexor carpi radialis. If conservative treatment is not successful, surgical treatment is an option. Surgical treatment has evolved from extensive releases
to arthroscopic debridement of the above
mentioned tendons. However, rehabilitation is long and intensive after conventional surgery which is a great disadvantage, especially in athletes. Minimal invasive procedures focused at the local
histo-pathology can possibly overcome
this problem.
T
The aim of this pilot study was to assess
the effect of ultrasound-guided needling
of the chronic lateral of the medial elbow
epicondylitis combined with corticosteroid injection in a group of patients
that had not responded to a previous
conservative or surgical management.
Twenty-five patients (10 males, 15
females, mean age 41.7 years) visiting the
orthopaedic outpatient clinic consecutively from May through October 2003
with chronic medial (10) or lateral (15)
epicondylitis were included in this study.
The mean duration of complaints was
24 months. All of them had had previous
corticosteroid injections and physiotherapy. Seven out of 25 had used a brace,
and eight had had surgery. An ultrasound
investigation with a phased array linear
transducer (5 MHZ to 12 MHz) showed
erosive cortex on the lateral side of the
elbow in seven of fifteen patients
(46.7%), and at the medial side in four of
ten patients (40%). Hypoechoic tendons
were visualised in seven of the fifteen
patients (46.7 %) with lateral epicondylitis, and in five of the ten patients (50%)
with medial epicondylitis. Tendon calcifications were found in eleven of the fifteen patients (73.4%) with lateral epicondylitis and in nine of the ten (90%)
with medial epicondylitis. A primary tear
was demonstrated in four of the fifteen
patients (26.7%) with lateral epicondylitis and in five of the ten (50%) with
medial epicondylitis. The hypoechoic
areas, calcifications or tendons with concordant pain were identified by ultrasound and perforated 5-10 times with a
18 gauge needle. At the end, 1 ml of corticosteroid was injected. After treatment
consisted of a standardized protocol
under supervision of a physiotherapist.
MEDICINE
& SCIENCE
IN
TENNIS 18
The clinical effect of needling was considered a success if patients had an excellent Andrews test (elbow functional
assessment), decrease of the VAS score
of at least three points, improvement of
“grip strength” and complete restoration
of the work and sport activities.
Twelve-week follow-up showed a statistically significant reduction (p=0.001) of
the VAS score in lateral epicondylitis
during provocation (a mean VAS score
before/after: 7.53/3.43).
Eight of the 25 patients (all with lateral
epicondylitis) completed all criteria of
clinically successful needling. All of them
subjectively reported a complete restoration of the elbow function and expressed
satisfaction with the procedure. In the
whole group there was no significant difference in the incidence of tendinosis,
tendon calcifications, positions and
aspect of dimensions of the calcifications.
The group had predominantly involvement of only m. extensor carpi radialis
brevis (five of the eight) and seven of the
eight had had no previous surgery. Of
the eight patients with previous surgery,
five showed no change in “grip strength”,
seven no changes in the Andrews test en
6 no change in the VAS score. The “failure” group (i.e. patients without previous
surgery) of ten patients consisted of eight
patients with medial epicondylitis and
two patients with lateral epicondylitis.
Six of the ten had had a primary tendon
tear and both cases of lateral epicondylitis showed simultaneous involvement of
the m.extensor carpi radialis longus en
brevis.
In conclusion we can say that the short
term results are promising for lateral epicondylitis without previous surgery. On
the basis of the pilot study results we
decided to start prospective crossover
investigation on patients with chronic
lateral epicondylitis and without previous
surgery.
ATP
Taping for Plantar Fasciitis on the ATP Tennis Circuit
BY MICHAEL NOVOTNY, ATP SPORTS MEDICINE TRAINER
lantar fasciitis is a common cause of
hindfoot pain in tennis players. The
plantar fascia is the strong band of tissue
under the foot that connects the toes to
the heel. In conjunction with the muscles
and bones, it helps to maintain the arch
of the foot. Repetitive stress on the
plantar fascia may result in inflammation,
micro-rupture and chronic pathological
changes at its attachment to the front of
the heel.
P
Heel spurs identified on X-ray may form
in the region of the plantar fascia attachment. It should be noted that these spurs
are not the source of pain. In fact, many
people with radiographically confirmed
heel spurs have never had symptoms of
plantar fasciits. Furthermore, in cases in
which a heel spur is present, successful
treatment of the symptoms of plantar
fasciitis does not require removal of the
spur.
Treatment for plantar fasciitis generally
includes rest, orthotics, stretching exercises, icing and other physical therapy modalities, non-steroidal antiinflammatoy medications and local corticosteroid injections.
Although most patients with plantar fasciitis do well with conservative treatment,
cases of plantar fasciitis unresponsive to
the above measures may require surgical
release of the damaged tissue. Shock wave
therapy has also been used to treat resistant cases, with varying degrees of success
reported.
Taping can be used as an important
adjunct in the treatment regimen for plantar fasciitis in the tennis athlete. When
properly applied, taping can reduce the
stretching of the plantar fascia, resulting in
significant pain relief. As with all taping
techniques, care must be exercised to
avoid skin problems, such as blisters.
ABOUT THE AUTHOR
Michal Novotny graduated from the
University of Oviedo and became a licensed
and certified Physical Therapist in 1999. He
has worked for different footballs teams as
physical therapist and for the ATP since
2002 as sports medicine trainer. He is also
the official physical therapist for the Czech
Davis Cup Team. He has been trained in the
areas of manual therapy and osteopathic
techniques.
Figure 1 Plantar fasciitis and heel spur
Drawing by Frans Bosch
1. Apply a fixation stroke in a circular
fashion over the metatarsals (forefoot).
2. Starting at the medial side of the foot,
at the base of the first toe, run the tape
over the sole of the foot, towards the
lateral side of the heel, around the heel,
and return over the medial side of the
foot to the toe.
3. Apply a second tape, starting at the lateral side of the foot at the base of the
fifth metatarsal, over the sole of the
foot towards the medial side of the
heel, around the heel, and return to the
lateral side of the foot.
4. Below the starting point on the medial
side of the foot, apply a second tape,
exactly the same way.
5. Repeat the same from the lateral side.
6. Close the tape on the bottom of the
foot with semi-circular straps of tape
running from the tape on the medial to
the tape on the lateral side of the foot.
7. Finally, a layer of elastic adhesive bandage is applied to cover the loose ends of
the tape.
Figure 5 Second medial and lateral sole
tapes in place
Figure 6 Elastic adhesive bandage
being applied
Material:
2.5 cm wide athletic tape
Elastic adhesive bandage
Figure 2 Circular fixation tape on forefoot
in place
Figure 4 Lateral sole tape in place
Figure 3
Medial sole tape in place
MEDICINE
& SCIENCE
IN
TENNIS 19
Figure 7
The final product
BOOK
EXCER
PT
Fit to Play:
Making Better Players, On & Off Court
CARL PETERSEN, B.SC. P.T., CITY SPORTS AND PHYSIOTHERAPY CLINICS, 420 - 890 WEST PENDER STREET,
VANCOUVER, B.C. V6C 1J9, CANADA. TEL: +1-604-606-1420, FAX: +1-604-606-1488, E-MAIL: CARL@CITYSPORTSPHYSIO.COM
NINA NITTINGER, BERLAGEWEG 16B, 30559 HANNOVER, GERMANY. TEL: +49-172-5308289, FAX: +49-511-554623,
E-MAIL: FITTOPLAYTENNIS@AOL.COM
WEBSITE WWW.FITTOPLAY.COM
Excerpt from their new book
Fit to Play Tennis
oday’s athletes have to be in great shape to
be competitive on a consistent basis. The
competition schedule, environmental factors
and associated travel can be gruelling. The
physical and mental demands of the sport all
take their toll on even the finest tuned
athletes. Developing proper training habits
early and sticking to them will pay off in the
long run. Players must strive to develop
training and playing attitudes that help them
improve not only as a player but as a person.
T
Successful tennis players require physical ability, technical skill and mental toughness.
Designing programs to ensure optimal tennis
training and performance is both an art and a
science (Figure 1). The practical training tips
in this Fit to Play article are designed by
coaches, physical therapists, sport medicine
physicians and other sport science and medicine personnel. Gone are the days of the professional tennis coach showing up on court for
the allotted hour of coaching. Successful high
performance coaches must ensure they are
well versed and educated in regards to the
many factors that influence athletic development and tennis performance.
To ensure proper training, practice progressions and optimise performance it is important to look at all of the factors that affect
physical training and on-court play.
These include:
• The athlete’s chronological age;
• Growth and development concerns;
• The athletes “training age” (how many years
they have been in formal training);
• Technical and biomechanical strengths and
weaknesses as identified by the athlete,
coach, physical therapist or strength and
conditioning coach;
• The athlete’s body type;
• The pre-existing general and specific fitness
level;
• General health status;
• The rehabilitation status of any past or current injuries;
• Physical strengths and weaknesses as identified by sport specific field testing and lab
testing where appropriate;
• Mental strengths and weaknesses as
identified by the athlete, coach, sport psychologist or mental trainer.
uses the concept of “Interconnecting Gears”
(Figure 2) to illustrate the importance of different factors in producing optimal performance.2 The on court performance gear must
turn smoothly and efficiently in to allow optimal training and performance. Players,
regardless of their skill level, must be physically and mentally prepared, be well recovered, healthy and practice proper nutritional
and hydration habits to optimally perform
and reach their full potential.
Performance is the central gear and all of the
other gears have an effect on its movement
and ultimately affect a player’s performance.
Some athletes can have success with high
abilities in certain areas like skill however to
perform optimally and consistently, all of the
gears must be working and turning smoothly
as well. Designing a well rounded physical
training, on-court practice and competition
schedule requires a good line of communication between the athlete, coach, physical
therapist, strength and conditioning (fitness
coach) and other involved sport medicine and
science personnel (Figure 3). As training age
increases and training and competition
demands become more comprehensive and
sophisticated, athletes will need to draw upon
the advice and knowledge of other professionals to ensure a safe, effective, conditioning
program.
The S’s of Smart Training
The responsibility for making a better player
falls directly on the athlete’s shoulders. To
optimise training and ultimately on-court performance they need to develop and build a
solid five point training plan that includes:
• Structured Tennis Practice;
• Structured Physical Training;
• Structured Mental Training;
• Structured Assessments;
• Survival Strategies for Staying Healthy.
Structured Practice
(On Court Training, Figure 3):
• Develop specific training and competition
plans in consultation with others athlete and
coach;
• Develop contingency plans for adverse
weather conditions (indoor courts or daily
physical training adjustment either planned
or improvised alternative training);
ABOUT THE AUTHORS
Carl Petersen is a Partner and Director of
High Performance Training at City Sports &
Physiotherapy Clinics in Vancouver, Canada.
From 1984-2003 he has travelled on the
World Cup Ski Circuit as the Physiotherapist
and Fitness Coach and he was the dedicated
Physiotherapist at the Olympic Winter
Games in Calgary, Albertville and
Lillehammer. Today he is working as the
physiotherapist and fitness coach with a
variety of tennis players from club level to
professionals on the WTA tour.
Nina Nittinger was a professional tennis
players who spent over 6 years full time on
the tour. She has a Masters Degree in
Sports Management. She is also a certified
tennis coach of the German Federation and
is a licensed mental trainer in Sport
Psychology. She recently co-authored a
German book about mental training for
tennis players.
• Ensure appropriate equipment and clothing
(shoes, clothing, sunscreen, hats etc.).
Structured Physical Training (Planning and
Periodization) – General:
• Ensure proper planning and periodization of
training includes pre-competition, in competition maintenance and post-season recovery break;
• Always include dynamic warm-ups, appropriate stretching and cool-downs in training
and playing sessions;
• Always include appropriate recovery protocols used both during and post training sessions to minimise the fatigue carried into
the next days training (Figure 4);
• Ensure sport specific training in the precompetition phase;
• Ensure general sports involvement and cross
training activities at all levels to ensure
multi-skill development and to add fun
(Figure 5);
• Regularly monitor signs of overstress. How
they feel physically and mentally including
mood and attitude to training and practice.
Have them note sleep and recovery cycles;
• Ensure they keep a daily logbook of training
to aid in monitoring volume, intensity and
density of training loads and help recognise
potential overstress or overtraining states.
For example in tennis, many factors come
into play when trying to optimise training and
performance. The Fit to Play training model
Figure 1 Science and art of training
Figure 2 Dr. Howie Wenger’s “Gears.”2
MEDICINE
& SCIENCE
IN
TENNIS 20
Figure 3 A good line of communication
should be established
• It is important to develop a network of reliable, qualified, sports medicine backup personnel that know and understand tennis and
the rigors of training;
• Physicians’ / Physiotherapists’ working
closely with the athlete and coach to determine an effective pre-habilitation or rehabilitation program;
• Utilising trusted sport science and medicine
professionals to help in planning, structuring and modifying the training schedule.
Structured Mental Training
Keeping a journal or diary and use it daily.
Ensure resources for appropriate sport
psychology or mental training are available.
Initiate contact and goal setting.
Provide opportunities for athletes to practice
techniques like imagery, distraction control,
and relaxation.
Take individual athletic requirements into
account: social climate, school, work, family
and interpersonal relations, daily stresses –
exams, deadlines, personal
conflicts.
STRUCTURED ASSESSMENTS
i) Medical / Physical:
By using the expertise and experience of
other sport medicine and science personnel
one may add several other facets towards
optimising athletic performance.
• Comprehensive pre-participation
medical screening including ligament laxity
tests, blood work and urinalysis;
• Get prompt help for any and all injuries and
illnesses. Contact particulars including telephone and fax numbers and
e-mail addresses of trusted health care professionals;
• Carry first aid supplies and have ice for
prompt attention to blisters and sore muscles.
ii) Sport Specific Assessment:
• Early identification and prevention of
injuries can be facilitated by pre-season
athlete screening (Figure 6);
• This is best done at least 6-8 weeks prior to
the start of heavy tournament period;
• A sport specific assessment by someone
who knows what to look for may save the
athlete a lot of pain and frustration later in
the season;
• Have the physiotherapist continually screen
for potential problem areas.
strokes or overheads can cause tissue breakdown and inflammation (micro-trauma).
Injury prevention is an important part of the
training plan of every athlete, parent and
coach. The best planned and periodized
training program is of little use if the athlete
is constantly injured and unable to train or
compete effectively.
Here are some simple tips to promote performance through injury prevention that all
athletes, parents and coaches can benefit
from:
iii) Field Testing and Laboratory
Assessments:
• Physiological assessments including field
tests and selected laboratory tests will
provide objective insight on:
• How the training is progressing and what
areas need to be worked on;
• Identifying strengths and weaknesses.
• Comparison to peers and self;
• Test protocols should be set and reviewed
based on current research and practice;
• Re-Assessment with the same test and conditions and preferably the same tester:
• It is encouraged that the athlete works with
a local sport scientist and develops a protocol of tests based on the facilities and equipment available.
Survival Strategies for Staying Healthy
Due to the asymmetrical nature of tennis
training and playing the most common
injuries are of the overuse variety. The cumulative effect of pounding around the courts
and repetitive actions like hitting ground
1) Develop a Team of Sports Medicine &
Science Specialists:
The multifaceted needs of today’s tennis players cannot be met by the coach or parents
alone. Optimal performance needs a combination of factors including coaching, physical
and mental preparation and proper nutrition
and medical monitoring. As the athlete progresses up the competition ladder and the
sophistication of performance increases, the
coaches and parents must act as co-ordinator
for the sport medicine and science needs of
the tennis player.
• Get to know local sports physicians and
sports physiotherapists;
• They may be able to help in locating other
specialist sport medicine and science specialists such as:
• – Sports Massage Therapist, Podiatrist,
Nutritionists and Dieticians,
• – Sport Psychologist, Exercise Physiologist,
• – Sport Vision Specialist (Optometrist),
• – Kinesiologists and Strength and
Conditioning Specialists.
Figure 4
On court training should be structured
Figure 5
Include appropriate recovery protocols
MEDICINE
& SCIENCE
IN
TENNIS 21
2) Proper Rest, Recovery and Rehabilitation
Techniques:
Training for and playing tennis are both physically and mentally demanding and recovery
sessions must be incorporated into sports specific training programs. The benefits of structured recovery sessions are well documented,
both in terms of improved performance and
decreased injury rates.1 Athletes, coaches and
parents all need to be aware of the importance of recovery following heavy workloads.
It is difficult to have a 100% injury free training program. Tennis player’s work hard, pushing themselves to the limits to achieve best
performance and injuries are an ever present
danger. However, injuries can be minimised
and controlled with a sensible injury prevention and management strategy at the heart of
the training plan.
Parents can be the frontline in injury
prevention and management strategy.
If any deficiencies are identified and prehabilitative (training for training) programs are
prescribed, the parents need to reinforce
these as part of the overall training schedule.
Successful coaches use sport specific training
and recovery programs that are scientifically
based. They make effective use of mental
training and ensure optimal health and nutrition. It is vital that all coaches keep up to date
with current research on training techniques
and constantly update their coaching practices.
References
1. Calder A. Recovery. In: Strength and conditioning for tennis. M Reid, A Quinn, M
Crespo (Eds). London: ITF. pp 227-239,
2003.
2. Wenger HA, and Bell G J. The interaction
of intensity, frequency, and duration of
exercise training in altering cardio respiratory fitness. Sports Med 1986;3:346-356.
Figure 6 Ensure general sports involvement
Figure 7
Pre-season athlete screening
MEMB
ER
ACTIV SHIP
ITIES
Evaluation of the Unilateral and Bilateral Stability
Index for Junior Tennis Players on the Biodex Stability System
MARCELO BANNWART SANTOS, PT, ROGÉRIO TEIXEIRA DA SILVA, MD, MAURICIO GARCIA, PT, MOISES COHEN, MD, PHD
Centre for Sports Medicine CETE, Federal University of São Paulo, São Paulo, Brazil
ostural stability is a complex process
Pproprioceptive
that demands visual, vestibular and
inputs, which, integrated
and processed by the central nervous system, provides motor control.7 A knee or
ankle sprain leads to deficits in postural
stability by damaging the function of the
mechanoreceptors, leading to an imbalance in motor control.5
Background
Evaluating balance is an important part
of the rehabilitation process of an athletic injury. In order to evaluate the postural stability, researches developed several methods such as the force plate3 and
stabilometry.6 Recently, new equipment
has been developed to study the postural
stability such as the Biodex Stability
System (Biodex, Inc., Shirley, New
York).10
Pincivero and Lephart have studied the
reliability of this instrument in 1995.8
The normative data for the stability
index of the equipment has been established in a study developed by Finn et al
in 1995, including 200 North American
non-athletes (males and females) aged 18
to 89 years old.2
athletes have to their arms at their side,
and have to look straight ahead to a
white wall 1 meter away. A 45-second
rest period will be allowed between tests.
The unilateral stance evaluation will consist of three 30-second assessments of
each lower limb (beginning with the
dominant limb). The athlete will keep
the opposite knee flexed in a comfortable
position (10º to 15º), with arms at the
side, keeping the eyes opened and looking straight to a white wall 1 meter away.
In both evaluations (bilateral and unilateral stance) the stability level will start
on 8 (most stable) and every 3,75 second
it will be decreased one level until it
reaches level 1 (least stable).
After the three tests the software will
perform the stability index that will than
be recorded. The results will be sent to
statistical analysis to detect a normative
stability index for junior tennis players.
Goal
Establish a normative bilateral and unilateral stability index for junior tennis
players on the Biodex Stability System.
This normative data was developed on
bilateral stance with the highest stability
level (eight). Since this normative data is
not representative for athletes, who are
much better trained, the goal of the present study is to establish normative data
(stability index) from bilateral and unilateral stance for junior tennis players.7
Inclusion Criteria
• At least two years of tennis practice of
at least hours/week)
• No previous injuries of the knee or
ankle
• No injuries of the hips or lower back
during the laast six months
• No cerebellar dysfunctions
• No injuries of the central nervous system
Material and Methods
Junior tennis players with no history of
knee or ankle injuries will be evaluated
through a questionnaire and by a physician. The study will be conducted at the
Sports Traumatology Center Research
Laboratory. After the athletes have
signed an informed consent form according to the standards of the Human
Research Ethical Committee, they will
be assessed on the Biodex Stability
System.
This equipment consists of a movable
platform that allows a 20º oscillation,
related to the ground, in all directions.
This platform is linked to software
(Biodex, version 3.1, Biodex, Inc.) that
allows an objective evaluation of postural
stability.1,3,4,9 The test protocol will consist of two trial tests, and three evaluations, of 30 seconds each, on bilateral
and unilateral stance.
The evaluations will start with three 30
seconds bilateral stance assessments. The
References
1. Cachupe JC, Shifflett B, Leamor K,
Wughalter E H: Reliability of Biodex
balance system measures. Measur
Phys Educ Exerc Sci 2001;5(2):
97-108.
2. Finn JA, Alvarex MM, Jett RE, Axtell
RS, Kemler DS. Biodex balance
assessment among subjects of disparate balancing abilities. Presented at
the American College of Sports
Medicine Annual Meeting, 1999
3. Goldie PA, Bach TM, Evans OM.
Force platform measures for evaluating postural control: reliability and
validity. Arch Phys Med Rehabil
1989;70:510-517.
4. Hinman MR. Factors affecting reliability of the Biodex balance system:
a summary of four studies. J Sport
Rehabil 2000;9:240-252.
5. Laskowski ER, Sheth P, Yu B. Ankle
disk training influences reaction times
of selected muscles in a simulated
MEDICINE
& SCIENCE
IN
TENNIS 22
ABOUT THE AUTHORS
Marcelo Bannwart Santos, PT, is physical
Therapist and a certified athletic trainer.
Marcelo Bannwart works in the Research
Laboratory of the Sports Traumatology
Center as sports physical therapy specialist.
He is assistant physical therapist at the
Sports Physical Therapy post-graduation
program at the Federal University of Sao
Paulo – UNIFESP.
Rogerio Teixeira Silva, MD is an orthopaedic
surgeon with a special interest in sports
medicine. Dr. Silva is the Medical Director of
the Brazil Open Tennis Tournament since
2001. He is takes care of elite tennis players
in Brazil, and is the founder of the Medical
Department of the Brazilian Tennis Confederation. He is a Board Member of the
Brazilian Orthopaedic Sports Medicine
Society and is Chairman of the South
American Committee of the STMS.
Mauricio Garcia, PT, works as the co-ordinator of the Physical Therapy scientific program at the Centre for Sports Medicine
(CETE - Federal University of Sao Paulo).
Dr. Moises Cohen, MD, PhD, is the
Chairman of the Sports Medicine Centre
(CETE) at the Federal University of Sao
Paulo, and Professor of the Orthopaedic
Department at this university. Dr. Cohen is a
member of the International Board at the
ISAKOS, and has been elected to be the
president of the SLARD, the Latin American
Society of Arthroscopy, Knee Surgery and
Sports Medicine. Dr. Cohen is a worldwide
known expert in knee surgery and
arthroscopy, and takes care of many professional athletes in Brazil.
12. ankle sprain. Am J Sports Med
1997; 25(4):538-543.
6. Leanderson J, Eriksson E, Wykman
A. Ankle sprain and postural sway in
basketball players. Knee Surg Sports
Traumatol Arthr 1993;1:203-205.
7. Perrin P, Schneider D, Deviterne D,
Perrot C, Constantinescu L. Training
improves the adaptation to changing
visual conditions in maintaining
human posture control in a test of
sinusoidal oscillation of the support.
Neurosci Lett 1998;245:155-158.
8. Pincivero DM, Lephart SM, Henry
TJ. Learning effects and reliability of
the Biodex Stability System. J
Athletic Training 1995;S30:S35.
9. Schmitz R, Arnold B: Intertester and
intratester reliability of a dynamic
balance protocol using the Biodex
stability system. J Sport Rehabil
1998;7:95-101.
10. Testerman C, Griend R V:
Evaluation of ankle instability using
the Biodex stability system. Foot
Ankle Int 1999;20(5):317-321.
BOOK REVIEW
The Physics and Technology of Tennis
rare to find a book that combines
knowledge of three experts in their
Ifieldttheis into
one eminently readable and
third section demonstrates his immense
knowledge of the subject from the range
and construction of strings available to a
detailed explanation of string tension.
There is now no reason for any player to
use the wrong string or the wrong tension!
well-structured volume. It is even more
unusual for these three experts to write
so that their material appeals and informs
such a wide variety of tennis experts, be
they sports scientists, sports medics or
tennis coaches. Throughout this book
each of the authors has achieved so
much. The wealth of information they all
give is backed up with photographs,
graphs and charts, to give visual back up
to the written information.
The book is divided into four main
sections, beginning with racket composition, moving to the strokes of the game
and then racket strings, concluding with
court surfaces and tennis balls.
All three authors have impeccable
credentials, knowledge and experience.
Howard Brody is an eminent physicist
who has combined his scientific work
with being a tennis coach and player.
He is well known to tennis coaches as a
scientist who makes sense to them. In
this book he appeals to the wider tennis
fraternity. He writes especially well on
the effects of physics on rackets, strings
and tennis balls.
The section on the strokes of the game
re-iterates Howard’s work on the serve
and receiving serve, together with the
effects of spin.
As ever, he gives the facts and in so doing
FROM
LITER THE
ATUR
E
The book is written with great detail and
explanation, but also with clarity.
Depending on the level of interest and
knowledge, the different chapters within
each section can only help the reader
understand the scientific principles of
rackets, strings, balls and courts. For perhaps the first time it brings all the aspects
of tennis together in one book. It is a
book that does what it says in the title.
Furthermore and very importantly, it
dispels the myths and explains the facts
about the different components of tennis. It leaves only one thing out and that
is the indeterminate one – the player!
removes the doubt!
Rod Cross, too, is a physicist working on
the physics of tennis, but from the perspective of rackets and strings. Rod gives
relevant and important information in
the first section on racket technology and
concludes the book with a chapter on the
links between the racket’s effect on the
ball, both of the strings and the court.
Any coach or player ignores the information at their peril!
The name of Crawford Lindsey is synonymous with stringing and rackets. The
Anne Pankhurst
Coach Education Director, LTA
The Physics and Technology of Tennis
Howard Brody, Rod Cross and
Crawford Lindsey
Vista, CA: Racquet tech, USRA 2002
Number of pages: 450
Price: 29.95 US$
ISBN 0-9722759-0-8
Factors associated with Prognosis of Lateral
Epicondylitis after 8 Weeks of Physical Therapy
WAUGH EJ, JAGLAL SB, DAVIS AM, TOMLINSON G, VERRIER MC
DEPARTMENT OF PHYSICAL THERAPY, UNIVERSITY OF TORONTO, TORONTO, ON, CANADA. E.WAUGH@UTORONTO.CA
Arch Phys Med Rehabil 2004;85(2):308-318
he objective of this study was to idenT
tify key factors associated with outcomes of patients who underwent eight
weeks of physical therapy for lateral
epicondylitis.
The study had a multicenter prospective
design with inception cohort of lateral
epicondylitis patients commencing physiotherapy. Baseline clinical examinations
were conducted by one physical therapist; self-report outcome measures were
completed at baseline and eight weeks
later. The study was performed in nine
private sports medicine clinics and two
hospital outpatient departments in
Ontario, Canada.
The participants were eighty-three
patients with unilateral lateral epicondylitis identified by the treating physical therapists. The final scores of the
Disability of the Arm, Shoulder and
Hand (DASH) questionnaire and a
vertical pain visual analog scale (VAS)
were used as the dependent variables.
The final prognostic model for the eight
week DASH scores included the baseline
score (95% confidence interval, 0.340.66), sex (female) (95% confidence
interval 3.3-14.5), and self-reported
nerve symptoms (95% confidence
interval 0.8-13.8).
The model for the 8-week VAS scores
included the baseline score (95% confidence interval 0.01-0.37), sex (female)
(95% confidence interval 0.4-18.2), and
MEDICINE
& SCIENCE
IN
TENNIS 23
self-reported nerve symptoms (95% confidence interval, 4.7-25.5).
A subanalysis indicated that women were
more likely than men to have work-related onsets, repetitive keyboarding jobs,
and cervical joint signs. Among women,
these factors were associated with higher
final DASH and VAS scores.
It was concluded that women and
patients who report nerve symptoms are
more likely to experience a poorer shortterm outcome after physical therapy
management of lateral epicondylitis.
Work-related onsets, repetitive keyboarding jobs, and cervical joint signs
have a prognostic influence on women.
SELECTED REVIEW OF THE LITERATURE
Recent
Advances
on the
Management
of
Tennis Elbow
Patients
Dr. Rogério Teixeira
Silva
I selected two review articles on tennis
medicine for this issue of the newsletter.
Also, I will comment on some other papers
discussed during the last meeting of the
American Academy of the Orthopedic
Surgeons, that was held in San Francisco,
March 2004.
1. SHOCK WAVE THERAPY FOR LATERAL
ELBOW PAIN
Buchbinder R, Green S, White M, Barnsley
L, Smidt N, Assendelft WJJ (Cochrane
Review). In: The Cochrane Library, Issue 2,
2003. Oxford: Update Software
This paper systematically reviews the literature about a controversial topic of treatment
– extra corporeal shock wave therapy for the
treatment of lateral elbow pain, a common
finding among amateur tennis players. Two
independent reviewers assessed all identified
trials and original papers against pre-determined inclusion criteria. Randomised and
pseudo randomised trials in all languages were
evaluated for inclusion in the review, provided they described individuals with lateral
elbow pain and were comparing the use of
extra corporeal shock wave therapy as a
treatment strategy.
Two trials of extra corporeal shock wave therapy versus placebo were included in this
review. The relative risk for treatment failure
(defined as Roles-Maudsley score of four) of
Figure 1 MRI of an patient with lateral epicondylitis. Note the chronic fibrotic tissue at the
origin of the extensor muscles (red arrow)
extra corporeal shock wave therapy over
placebo was 0.40 (95% confidence interval,
0.08 to 1.91) at six weeks and 0.44 (95% confidence interval, 0.09 to 2.17) at one year.
After six weeks, there was no statistically
significant difference in improvement of pain
at rest, pain with resisted wrist extension or
pain with resisted middle finger extension.
Results after 12 and 24 weeks were similar.
The reviewers concluded that the two trials
included in this review yielded conflicting
results, and that further trials are needed to
clarify the value of extra corporeal shock
wave therapy for lateral elbow pain.
Comments:
This Cochrane database work is a very important contribution for the scientific guidelines
that we have to focus from now on. In my
personal experience, extra corporeal shock
wave therapy has a low rate of success in the
treatment of tennis elbow injuries, mainly
those injuries that lasts more than six months
and have some degree of tissue rupture.
Otherwise, in the office, this option continues
to be a strong therapeutic issue, mainly for
those patients that do not want to undergo a
surgical procedure.
Despite the results of the Cochrane Review,
two papers were presented at the AAOS
2004 last March, about these findings. Levitt
et al.1 presented the results of a multicenter,
prospective, randomised, double blind,
crossover, placebo controlled trial of extra
corporeal shock wave therapy for chronic
lesions of lateral epicondylitis. From the
225 patients selected, there was a significant
improvement in the symptoms in the study
group when compared to placebo. Rompe et
al.,2 in Germany, also presented at the same
meeting good results for their tennis players
(78 athletes), but they also noted that a
placebo effect is possible and is a fact with
extra corporeal shock wave therapy.
Comments:
This is an interesting topic. The orthopaedic
surgeons always have these problems when
they want to study two or more protocols for
scientific reasons. There is an ethical dilemma
when wanting to assess the efficacy of a surgical treatment. That is the creation of a control
group. In my opinion we have to work
together more in order to solve this problem,
because without a control group it will be
difficult to show whether surgery is the best
option and may be the best surgery for any
given problem. In the article above we
discussed the tennis elbow problem, but we
also have reviews on knee, ankle and shoulder
surgery that demonstrated poor scientific
evidence for justifying specific surgical
procedures.
References
1. Levitt RL, Selesnik FH, Ogden J.
Shockwave therapy for chronic lateral epicondylitis: an FDA study. Free Paper,
Specialty Day AOSSM, Annual Meeting
of the American Academy of Orthopaedic
Surgeons, San Francisco, March 2004
2. Rompe JD, Schoellner C, Nefe B, Heine J,
Decking J, Theis C. Repetitive low-energy
shockwave therapy for chronic lateral epicondylitis in tennis players. Free Paper,
Specialty Day AOSSM, Annual Meeting
of the American Academy of Orthopaedic
Surgeons, San Francisco, March 2004
If you have any interesting articles for this
section please contact me by email at
rgtsilva@uol.com.br.
Rogerio Teixeira Silva, MD
Orthopaedics and Sports Medicine
Chairman – South American Committee –
STMS
São Paulo, Brazil
2. SURGERY FOR LATERAL ELBOW PAIN
Buchbinder R, Green S, Bell S, Barnsley L,
Smidt N, Assendelft WJJ (Cochrane Review).
In: The Cochrane Library, Issue 2, 2003.
Oxford: Update Software
Randomised and pseudo randomised trials
(RCT) in all languages were to be included in
the review provided they were studying the
effects of a surgical intervention and included
a control as treatment for adults with lateral
elbow pain. The control intervention could
comprise no treatment or another intervention including an alternate surgical intervention. Outcomes of interest included pain,
function, disability and quality of life,
strength and adverse effects. The authors
search did not identify any controlled trials
investigating the effect of surgery on lateral
elbow pain.
The reviewers concluded that at this time
there are no published controlled trials of
surgery for lateral elbow pain – they pointed
out that without a control group, it is not
possible to draw any conclusions about the
value of this modality of treatment.
Figure 2 The picture shows the amount of
fibrotic tissue after partial resection of the tendon
(red arrow). This is of the same patient as in
the MRI. The yellow arrow indicates the lateral
epicondyle
The newsletter Medicine and Science in Tennis is endorsed by:
MEDICINE
& SCIENCE
IN
TENNIS 24