Breath Sounds & Lung Assessment Guide
advertisement
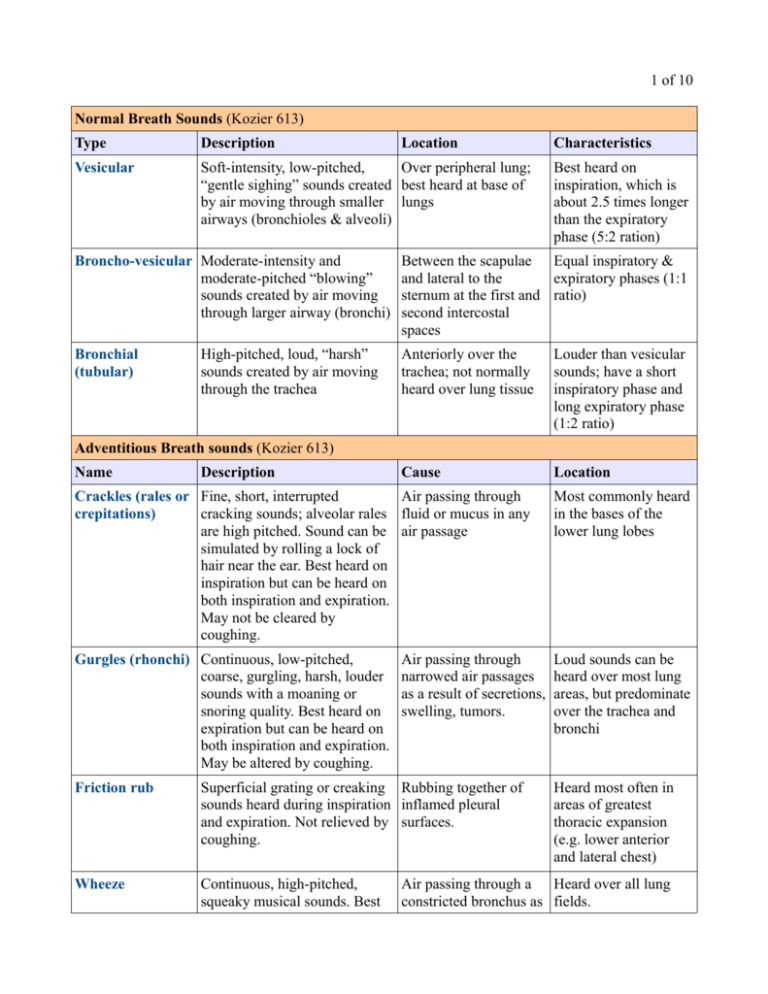
1 of 10 Normal Breath Sounds (Kozier 613) Type Description Location Vesicular Soft-intensity, low-pitched, Over peripheral lung; “gentle sighing” sounds created best heard at base of by air moving through smaller lungs airways (bronchioles & alveoli) Characteristics Best heard on inspiration, which is about 2.5 times longer than the expiratory phase (5:2 ration) Broncho-vesicular Moderate-intensity and moderate-pitched “blowing” sounds created by air moving through larger airway (bronchi) Between the scapulae Equal inspiratory & and lateral to the expiratory phases (1:1 sternum at the first and ratio) second intercostal spaces Bronchial (tubular) Anteriorly over the trachea; not normally heard over lung tissue Louder than vesicular sounds; have a short inspiratory phase and long expiratory phase (1:2 ratio) Cause Location High-pitched, loud, “harsh” sounds created by air moving through the trachea Adventitious Breath sounds (Kozier 613) Name Description Crackles (rales or Fine, short, interrupted Air passing through crepitations) cracking sounds; alveolar rales fluid or mucus in any are high pitched. Sound can be air passage simulated by rolling a lock of hair near the ear. Best heard on inspiration but can be heard on both inspiration and expiration. May not be cleared by coughing. Most commonly heard in the bases of the lower lung lobes Gurgles (rhonchi) Continuous, low-pitched, coarse, gurgling, harsh, louder sounds with a moaning or snoring quality. Best heard on expiration but can be heard on both inspiration and expiration. May be altered by coughing. Loud sounds can be heard over most lung areas, but predominate over the trachea and bronchi Air passing through narrowed air passages as a result of secretions, swelling, tumors. Friction rub Superficial grating or creaking Rubbing together of sounds heard during inspiration inflamed pleural and expiration. Not relieved by surfaces. coughing. Wheeze Continuous, high-pitched, squeaky musical sounds. Best Heard most often in areas of greatest thoracic expansion (e.g. lower anterior and lateral chest) Air passing through a Heard over all lung constricted bronchus as fields. 2 of 10 heard on expiration. Not usually altered by coughing. Absence of breath n/a sounds a result of secretions, swelling, tumors Associated with Can be “heard” collapsed and surgically wherever airflow is removed lobes or lacking. severe pneumonia Assessing the Thorax & Lungs (Kozier 614) Planning Equipment For efficiency, the nurse usually examines the posterior chest first, then the anterior chest. For posterior and lateral chest examinations, the client is uncovered to the waist and in a sitting position. A sitting or lying position may b e used for anterior chest examination. The sitting position is preferred because it maximizes chest expansion. Good lighting is essential, especially for chest inspection. • • • Stethoscope Skin marker/pencil Centimeter rule Delegation Assessment of the thorax and lungs is not delegated to a UAP. However, many aspects of breathing are observed during usual care and may be recorded by persons other than the nurse. Abnormal findings must be validated and interpreted by the nurse Implementation Performance 1. Prior to performing the procedure, introduce self and verify the client's identity using agency protocol. Explain to the client what you are going to do, why it is necessary, and how he or she can cooperate. Discuss how the results will be used in planning further care or treatments. 2. Perform hand hygiene and observe appropriate infection control procedures. 3. Provide for client privacy. In women, drape the anterior chest when it is not being examined. 4. Inquire if the client has any history of the following: family history of illness, including cancer, allergies, tuberculosis; lifestyle habits such as smoking & occupational hazards (e.g. inhaling fumes); medications being taken; current problems (e.g. swellings, coughs, wheezing, pain) Assessment [Posterior thorax] 5. Inspect the shape and symmetry of the thorax from posterior and lateral views. Compare the anteroposterior diameter to the transverse diameter Normal Findings • • Anteroposterior to transverse diameter in ratio of 1: 2 Chest symmetric Deviations from Normal • • Barrel chest; increased anteroposterior to transverse diameter Chest asymmetric 3 of 10 6. Inspect the spinal alignment for deformities. Have the client stand. From a lateral position, observe the three normal curvatures: cervical, thoracic, and lumbar ◦ To assess for lateral deviation of spine (scoliosis), observe the standing client from the rear. Have the client bend forward at the waist and observe from behind. • • 7. Palpate the posterior thorax. ◦ For clients who have no respiratory complaints, rapidly assess the temperature and integrity of all chest skin. ◦ For clients who do have respiratory complaints, palpate all chest areas for bulges, tenderness, or abnormal movements. Avoid deep palpation for painful areas, especially if a fractured rib is suspected. In such a case, deep palpation could lead to displacement of the bone fragment against the lungs • 8. Palpate the posterior chest for respiratory excursion (thoracic expansion). Place the palms of both your hands over the lower thorax with your thumbs adjacent to the spine and • Spine vertically aligned Spinal column is straight, right and left shoulders and hips are at the same height • • Exaggerated spinal curvatures (kyphosis, lordosis) spinal column deviates to one side, often accentuated when bending over. Shoulders or hips not even. ☼ See chart on page 7 for abnormal chest configurations • Skin intact; uniform temperatures Chest wall intact; no tenderness; no masses • Full and symmetric chest expansion. For example, when the client takes a deep breath, your thumbs should move apart an equal distance and at • • Skin lesions; areas of hyperthermia lumps, bulges; depressions; areas of tenderness; movable structures (e.g. rib) Asymmetric and/or decreased chest expansion. 4 of 10 your fingers stretched laterally.(a) Ask the client to take a deep breath while you observe the movement o your hands and any lag in movement. the same time; normally the thumbs separate 3 to 5 cm (1.5 to 2 inches) during inspiration. • (a) Position of the nurse's hands when assessing respiratory excursion on the posterior thorax. 9. Palpate the chest for vocal (tactile) fremitus, the faintly perceptible vibration felt through the chest wall when the client speaks ◦ Place the palmar surfaces of your fingertips or the ulnar aspect of your hand or closed fist on the posterio chest, starting • • • Bilateral symmetry of vocal fremitus Fremitus is heard most clearly at the apex of the lungs Low-pitched voices of males are more readily palpated that higher pitched voices of females • • Decreased or absent fremitus (associated with pneumothorax) Increased fremitus (associated with consolidated lung tissue, as in pneumonia). 5 of 10 near the apex of the lungs [(b) spot 1] ◦ Ask the client to repeat such words as “blue moon” or “one, two, three” ◦ Repeat the two steps, moving your hands sequentially to the base of the lungs, through positions 2-5 in (b). ◦ Compare the fremitus on both lungs and between the apex and the base of each lung, using either one hand and moving it from one side of the client to the corresponding area on the other side or using two hand that are placed simultaneously on the corresponding areas of each side of the chest. • (b) Areas and sequence for palpating tactile fremitus on the posterior chest ☼ See pg 10 for chart on Voice Sounds 10. Percuss the thorax Percussion of the thorax is performed to determine whether underlying lung tissue is filled with air, liquid, or solid material and to determine the positions and boundaries of certain organs. Because percussion penetrates to a dept of 5 to 7 cm (2 to 3 inches) it detects superficial rather than deep • (c) Normal percussion lesions. Percussion sounds sounds on the posterior and tones are described in chest Kozier on page 583 and Brunner on 504.(c) ☼ See chart on page 9 for ◦ Ask the client to bend characteristics of Percussion the head and fold the Sounds. arms forward across the chest. Rationale: • (d) sequence for posterior chest percussion 6 of 10 This separates the scapula and exposes more lung tissue to percussion. ◦ Percuss in the intercostal spaces at about 5 cm (2in) intervals in a systematic sequence (d) ◦ Compare one side of the lung with the other ◦ Percuss the lateral thorax every few inches, starting at the axilla and working down to the eighth rib 11. Percuss for diaphragmatic excursion (movement of the diaphragm during maximal inspiration and expiration) ◦ Ask the client to take a deep breath and hold it while you percuss downward along the scapular line until dullness is produced at the level of the diaphragm. Mark this point with a marking pencil, and repeat the procedure on the other side of the chest. ◦ Ask the client to take a few normal breaths and then expel the last breath completely and hold it while you percuss upward from the marked point to assess and mark the diaphragmatic excursion during deep expiration on each side • • Excursion is 3 to 5 cm (1.5 to 2 in) bilaterally in women and 5-6 cm (2 to 3 in) in men. Diaphragm is usually slightly higher on the right side. • Restricted excursion (associated with lung disorder). 7 of 10 ◦ Measure the distance between the two marks 12. Auscultate the chest using the flat disc diaphragm of the stethoscope (best for transmitting the high pitched breath sounds). ◦ Use the systematic zigzag procedure used in percussion ◦ Ask the client to take slow, deep breaths through the mouth. Listen at each point to the breath sound during a complete inspiration and expiration ◦ Compare findings at each point with the corresponding point on the opposite side of the chest. • Vesicular and bronchovesicular breath sounds • • Adventitious breath sounds (e.g. crackles, gurgles, wheeze, friction rub) Absence of breath sounds 8 of 10 Abnormal Chest Configurations Barrel Chest • • • Funnel Chest (Pectus Excavatum) • • • Pigeon Chest (Pectus Carinaturm) • • • Occurs as a result of overinflation of the lungs increase in an anteroposterior diameter of the thorax ribs are more widely spaced & intercostal spaces tend to bulge on expiration Occurs when there is a depression in the lower portion of the sternum can compress the heart & great vessels, resulting in murmurs can occur with rickets or Marfan's syndrome Occurs as a result of displacement of the sternum increases the anteroposterior diameter can occur with rickets, Marfan's syndrom, or severe kyphoscoliosis 9 of 10 Kyphoscoliosis (Kyphosis) • • • Lordosis • • • Characterized by elevation of the scapula & corresponding sshaped spine limits lung expansion within the thorax can occur with osteoporosis & other skeletal disorders affecting the thorax Characterized by an exaggerated lumbar curve can occur with osteoporosis, any skeletal disorders affecting the thorax, weak lower back muscles and poor posture depending on severity, may not affect chest configuration Characteristics of Percussion Sounds (Brunner 504) Sound Relative Intensity Relative Pitch Relative Duration Location Example Examples Flatness Soft High Short Thigh Large pleural effusion Dullness Medium Medium Medium Liver Lobar pneumonia Resonance Loud Low Long Normal Lung Simple chronic bronchitis Hyperresonance Very Loud Lower Longer None normally Emphysema, pneumothorax High – – Gastric air bubble, puffed-out cheek Large pneumothorax Tympany Loud distinguished by a musical timbre 10 of 10 Voice Sounds • sound heard through stethoscope as pt speaks is known as vocal resonance Sound Description Indicative Bronchophony Vocal resonance that is more intense and clearer than normal Indicative of consolidation, as it occurs in pneumonia or pleural effusion. Egophony Voice sounds that are distorted. Indicative of consolidation, as it Best appreciated by having the pt occurs in pneumonia or pleural repeat the letter E. The distortion effusion. produced by the consolidation transforms the sound into a clearly heard “A” rather than “E”. Whispered pectoriloquy Distinctly hearing words that seem to come from a spot being auscultated. Heard in the presence of rather dense consolidations of the lungs. This is not part of normal physiology, but is difficult to identify.