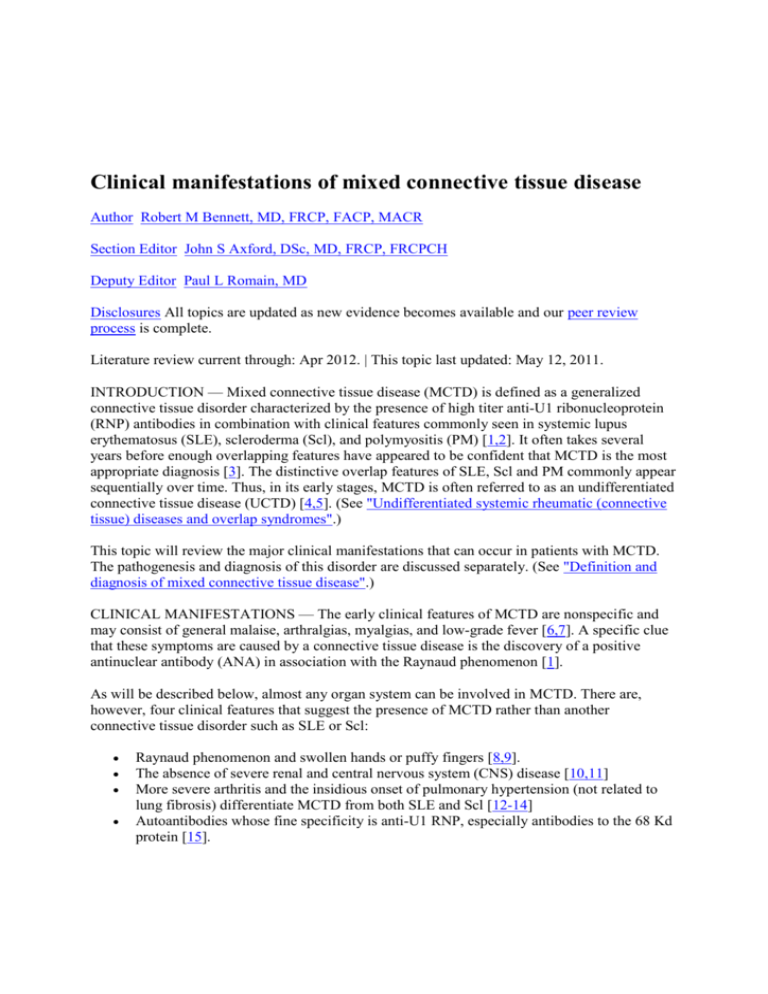
Clinical manifestations of mixed connective tissue disease
Author Robert M Bennett, MD, FRCP, FACP, MACR
Section Editor John S Axford, DSc, MD, FRCP, FRCPCH
Deputy Editor Paul L Romain, MD
Disclosures All topics are updated as new evidence becomes available and our peer review
process is complete.
Literature review current through: Apr 2012. | This topic last updated: May 12, 2011.
INTRODUCTION — Mixed connective tissue disease (MCTD) is defined as a generalized
connective tissue disorder characterized by the presence of high titer anti-U1 ribonucleoprotein
(RNP) antibodies in combination with clinical features commonly seen in systemic lupus
erythematosus (SLE), scleroderma (Scl), and polymyositis (PM) [1,2]. It often takes several
years before enough overlapping features have appeared to be confident that MCTD is the most
appropriate diagnosis [3]. The distinctive overlap features of SLE, Scl and PM commonly appear
sequentially over time. Thus, in its early stages, MCTD is often referred to as an undifferentiated
connective tissue disease (UCTD) [4,5]. (See "Undifferentiated systemic rheumatic (connective
tissue) diseases and overlap syndromes".)
This topic will review the major clinical manifestations that can occur in patients with MCTD.
The pathogenesis and diagnosis of this disorder are discussed separately. (See "Definition and
diagnosis of mixed connective tissue disease".)
CLINICAL MANIFESTATIONS — The early clinical features of MCTD are nonspecific and
may consist of general malaise, arthralgias, myalgias, and low-grade fever [6,7]. A specific clue
that these symptoms are caused by a connective tissue disease is the discovery of a positive
antinuclear antibody (ANA) in association with the Raynaud phenomenon [1].
As will be described below, almost any organ system can be involved in MCTD. There are,
however, four clinical features that suggest the presence of MCTD rather than another
connective tissue disorder such as SLE or Scl:
Raynaud phenomenon and swollen hands or puffy fingers [8,9].
The absence of severe renal and central nervous system (CNS) disease [10,11]
More severe arthritis and the insidious onset of pulmonary hypertension (not related to
lung fibrosis) differentiate MCTD from both SLE and Scl [12-14]
Autoantibodies whose fine specificity is anti-U1 RNP, especially antibodies to the 68 Kd
protein [15].
General features — MCTD is much more common in women than in men (ratio of 16 to 1) [16].
Most patients present in the second or third decades of life. Unlike SLE, however, sun exposure
is not a precipitating factor. Drug-induced MCTD is a rare occurrence, but may be an occasional
feature of anti-TNF therapy [17,18]. Vinyl chloride [19] and silica [20] are the only
environmental agents that have so far associated with MCTD.
In the early phases of the MCTD many patients complain of easy fatigability, poorly defined
myalgias, arthralgias, and the Raynaud phenomenon; and diagnostic considerations include the
early stages of RA, SLE or undifferentiated connective tissue disease (UCTD) [21]. Most, if not
all, of the major organ systems may be involved at some time during the course of MCTD,
including the skin, joints, muscles, heart, lungs, gastrointestinal tract, kidneys, central nervous
system, and hematologic system [3,4]. A high titer of anti-RNP antibodies in a patient with
UCTD is a powerful predictor for a later evolution into MCTD [22].
Skin — Skin involvement occurs in most patients with MCTD. The most common skin change is
the Raynaud phenomenon, which usually presents early in the course of the disease [8,23].
Swollen digits and occasionally total hand edema are also distinctive features (picture
1) [13,24,25]; sclerodactyly and calcinosis cutis have been observed [26,27].
Other skin manifestations, such as discoid plaques and malar rash, are indistinguishable from
SLE (picture 2A-C). (See "Mucocutaneous manifestations of systemic lupus erythematosus".)
Mucous membrane involvement can include orogenital and buccal ulcerations, nasal septal
perforation, and the sicca complex [13,28,29].
Fever — Fever of unknown origin may be the presenting feature of MCTD [24]. In this setting, it
can usually be traced to a coexistent myositis, aseptic meningitis, serositis, lymphadenopathy, or
intercurrent infection.
Arthritis — It is now apparent that joint involvement in MCTD is more common and frequently
more severe than in classic SLE. Approximately 60 percent of patients with MCTD develop an
obvious arthritis, often with deformities characteristic of rheumatoid disease, such as boutonniere
deformities and swan neck changes (picture 3) [12,25]. The radiographic appearance often
resembles Jaccoud's arthropathy [30].
Other changes that can occur include small marginal erosions [31-33] (picture 4) and, in a few
patients, destructive arthritis, including arthritis mutilans (picture 5 and picture 6) [12,34].
A positive rheumatoid factor is found in about 70 percent of patients with MCTD [35]. Anticyclic citrullinated peptide (CCP) antibodies are found in about 50 percent, especially in those
MCTD patients who also fulfill the American College of Rheumatology diagnostic criteria for
rheumatoid arthritis (RA) [36].
Myositis — One of the three overlap features required for the diagnosis of MCTD is an
inflammatory myopathy clinically and histologically identical to PM [24,37,38]. (See "Clinical
manifestations and diagnosis of adult dermatomyositis and polymyositis".) Myalgia is a common
symptom in patients with the MCTD syndrome [39]. In most patients there is no demonstrable
weakness, EMG abnormalities or elevation of muscle enzymes. It is often unclear whether the
symptom represents a low-grade myositis, physical deconditioning or an associated fibromyalgia
syndrome. Sometimes myositis occurs as an acute flare against a background of general disease
activity [24]. Cases of a low grade, insidious, and persistent inflammatory myopathy have also
been described. The histology of muscle involvement in MCTD is the same as idiopathic
inflammatory myopathy [40,41] with features both of the vascular involvement of
dermatomyositis and the cell-mediated changes of PM [42]. It is increasingly apparent that a
diagnosis of "pure" PM is relatively rare, and most patients with an inflammatory myopathy turn
out to have an overlap syndrome [43].
Cardiac disease — All three layers of the heart may be involved in MCTD [44]. An abnormal
electrocardiogram is noted in about 20 percent of patients. The most common EKG changes are:
right ventricular hypertrophy, right atrial enlargement, and inter-ventricular conduction defects.
Pericarditis is the commonest clinical manifestation of cardiac involvement being reported in 10
to 30 percent of patients; pericardial tamponade is rare. Involvement of the myocardium is
increasingly recognized [45,46]. In some patients myocardial involvement is secondary to
pulmonary hypertension (PAH); this is often asymptomatic in its early stages [47]. (See
'Pulmonary hypertension' below.)
Pulmonary involvement — The lungs are commonly affected in MCTD with involvement in
about 75 percent of patients [48,49]. There is a wide spectrum of pulmonary problems that can
occur in MCTD [50]:
Pleural effusions
Pleuritic pain
Pulmonary hypertension
Interstitial lung disease
Thromboembolic disease
Alveolar hemorrhage
Diaphragmatic dysfunction
Aspiration pneumonitis/pneumonia
Obstructive airways disease
Pulmonary infections
Pulmonary vasculitis
Early symptoms that should alert one to pulmonary involvement are dry cough, dyspnea and
pleuritic chest pain [50].
Interstitial lung disease — Interstitial lung disease (ILD) occurs in 30 to 50 percent of subjects
[51]. A reduction in the single breath-diffusing capacity for carbon dioxide (DLCO) is
commonly found on lung function testing in the early stages of ILD [50].
High resolution computed tomography (HRCT) is a sensitive test to determine the presence of
ILD. The commonest HRCT findings are septal thickening, ground-glass opacities, nonseptal
linear opacities and peripheral/lower lobe predominance [52,53], which are similar to the
findings in Scl [54]. Rapid clearance of technetium labeled diethylenetriamine pentaacetate
(DTPA lung scan) is closely correlated with CT evidence of interstitial lung disease and with a
decreased DLCO [55].
Based upon a combination of high resolution CT (HRCT) and DTPA scans, the prevalence of
interstitial lung disease in MCTD was found to be 66.6 percent [55]. Untreated ILD is usually
progressive with the development of severe pulmonary fibrosis in 25 percent of subjects after
four years of follow-up [51]. Esophageal dilatation has been associated with a tendency to
develop interstitial lung disease in MCTD [56].
Pulmonary hypertension — A major cause of death in MCTD is pulmonary hypertension [57].
This complication is caused by a bland intimal proliferation and medial hypertrophy of
pulmonary arterioles (picture 7).
The presence of pulmonary hypertension may be suspected from the history, physical findings,
and laboratory tests, particularly if the patient has four or more of the following [58]:
Exertional dyspnea
Systolic pulsation at the left sternal border
An accentuated second pulmonary sound
Dilation of the pulmonary artery on x-ray (picture 8)
Right ventricular hypertrophy on electrocardiogram
Right ventricular enlargement on echocardiogram
The early detection of pulmonary hypertension is increasingly important, as there are now more
effective therapeutic options. PAH is probably under-diagnosed, its prevalence in a community
rheumatology practice was 13 percent, based on echocardiography to estimate right ventricular
systolic pressure [59].
Two-dimensional echocardiography with Doppler flow studies is the most useful screening test
[60], with a definitive diagnosis requiring cardiac catheterization showing a mean resting
pulmonary artery pressure greater than 25mm Hg at rest [61]. The development of pulmonary
hypertension has been correlated with a nail-fold capillary pattern similar to that seen in Scl,
anti-endothelial cell antibodies and anticardiolipin antibodies [62-64]. (See "Overview of
pulmonary hypertension".)
Renal disease — The absence of severe renal disease is a hallmark of MCTD [1]. It is possible
that high titers of anti-U1 RNP antibodies, which are characteristic of MCTD, may protect
against the development of diffuse proliferative glomerulonephritis, independent of whether
these antibodies occur in MCTD or classic SLE [10,65].
However, some degree of renal involvement occurs in about 25 percent of patients [10,13,66].
Membranous nephropathy is the most common finding (picture 9A-E) [10,13,67] and nephrotic
range proteinuria may occur [65]. Hypertensive crises similar to Scl kidney have also been
reported [68,69]. (See "Scleroderma renal crisis".)
Gastrointestinal disease — Gastrointestinal involvement is the commonest clinical overlap
feature with Scl, occurring in about 60 to 80 percent of patients [11,48]. Disordered motility in
the upper gastrointestinal tract is the commonest problem [56,70,71]. There have been case
reports of hemoperitoneum, hematobilia, duodenal bleeding, megacolon, pancreatitis, ascites,
and protein loosing enteropathy, primary biliary cirrhosis, portal hypertension, pneumatosis
intestinalis and autoimmune hepatitis [13,72-74]. Malabsorption syndrome can occur secondarily
to small bowel dilation with bacterial overgrowth. Liver involvement in the form of chronic
active hepatitis and Budd-Chiari syndrome has been described. Pseudodiverticulae, identical to
those seen in Scl, may be seen along the anti-mesenteric border of the colon. Abdominal pain in
MCTD may result from bowel hypomotility, serositis, mesenteric vasculitis, colonic perforation
and pancreatitis.
Central nervous system disease — The original description of MCTD emphasized the lack of
CNS involvement [1]. This observation remains largely correct since patients with MCTD do not
develop severe complications such as cerebritis, psychosis, or seizures [75]. However,
approximately 25 percent of patients have some, typically mild form of CNS disease [57,75].
The most frequent CNS manifestation is a trigeminal (fifth cranial) nerve neuropathy,
which may be the presenting feature of the disease [76,77]. Trigeminal neuropathy is also
the most common CNS problem in patients with Scl.
Headaches are also common. They are most often vascular in origin [78], but can be
caused by aseptic meningitis [79,80], due to the disease itself or to a reaction to
nonsteroidal anti-inflammatory drugs [81,82] and by muscle tension and myofascial
trigger points.
Sensorineural hearing loss is often not recognized, but is reported to occur in about 50
percent of MCTD patients [83].
Isolated cases of cerebral hemorrhage [84], transverse myelitis [85], cauda equina syndrome
[86], retinal vasculitis [87], progressive multifocal encephalopathy [88,89], and demyelinating
neuropathy [90] have also been reported.
Hematologic and laboratory abnormalities — Nonspecific hematologic and laboratory
abnormalities are common in MCTD:
Approximately 75 percent of patients have a low-grade anemia [13].
As in classic SLE, leukopenia, mainly affecting the lymphocyte series, is a common
finding that tends to correlate with disease activity [13,91]. (See "Hematologic
manifestations of systemic lupus erythematosus in adults".)
The majority of patients have hypergammaglobulinemia [24,92].
The rheumatoid factor is positive in 50 to 70 percent of patients [35].
Anti-cyclic citrullinated peptide (CCP) antibodies are found in about 50 percent of
patients [36].
Many patients also make antibodies directed against hnRNP-A2, fibrillin-1, and
nucleosomes, but not to RNA polymerases [93] or proteasome [94].
Antiphospholipid antibodies occur less frequently than in SLE [95,96]. If present, they
tend to correlate with thrombocytopenia and pulmonary hypertension, but not with
thrombosis and/or abortions. Anti-beta(2)-glycoprotein I antibodies are fairly uncommon
in MCTD, occurring in about 10 percent of patients. Their presence is often associated
with the development of pulmonary hypertension [64].
Anti-endothelial cell antibodies occur in some 50 percent of MCTD patients [97], and
appear to be reactive with a voltage-dependent anion-selective channel 1 (VDAC-1) [98].
Their occurrence tends to be associated with microvascular injury in the lung and kidneys
[99].
Less common problems include thrombocytopenia, thrombotic thrombocytopenic purpura
[100,101], Coombs positive hemolytic anemia [102], and red cell aplasia [103].
The one specific serological finding is that, by definition, all patients with MCTD have a positive
ANA whose fine specificity is anti-U1 RNP, especially antibodies to the 68 Kd protein [104].
(See "Definition and diagnosis of mixed connective tissue disease".)
Vasculopathy — The Raynaud phenomenon is a typical early feature of MCTD [23]; thus, an
absence of Raynaud argues against this diagnosis. The characteristic vascular lesion of MCTD is
bland intimal proliferation and medial hypertrophy affecting medium and small size vessels
[105]; this is also the characteristic pathology in pulmonary hypertension and renovascular crises
(picture 2A-C) [57]. This pathologic changes differs from that usually noted in SLE, in which
perivascular inflammatory infiltrates and necrosis are more characteristic.
Similar to Scl, abnormal fingernail capillaroscopy is a common feature of MCTD [106,107]. The
capillary pattern is characterized by dilation and drop-out (picture 10). Nailfold capillaroscopy
can be performed at the bedside, a test that is useful for the prognostic stratification of those with
early Raynaud phenomenon [108]. (See "Clinical manifestations and diagnosis of the Raynaud
phenomenon", section on 'Nailfold capillary microscopy'.)
Angiographic studies reveal a high prevalence of medium-sized arterial occlusions (picture
11) [109].
Pregnancy — Conflicting reports describe the effects of pregnancy on the course of MCTD and
the effects of MCTD on the fetus [110,111]. One study described increased fetal wastage and a
40 percent prevalence of flares during pregnancy [112]. Another report, however, did not
confirm disease exacerbations associated with pregnancy or the postpartum period [24,113].
Small for gestational age infants occurred in 50 percent and 63 percent of pregnancies in one
series of 20 patients [111]. The mechanism for pregnancy complications is probably an
autoimmune reaction against placental tissues, as immunostaining studies show deposits of
fibrinogen, IgG, IgM, IgA, and complement 3 (C3) localized to the trophoblast basement
membrane [114]. Furthermore, there is an association of anti-endothelial antibodies with
spontaneous abortion in MCTD [115].
Patients with severe Raynaud phenomenon in general often have low birth weight infants [116],
presumably due to placental ischemia. This relationship has also been described in patients with
MCTD [117].
Use of UpToDate is subject to the Subscription and License Agreement.
REFERENCES
1. Sharp GC, Irvin WS, Tan EM, et al. Mixed connective tissue disease--an apparently
distinct rheumatic disease syndrome associated with a specific antibody to an extractable
nuclear antigen (ENA). Am J Med 1972; 52:148.
2. Aringer M, Smolen JS. Mixed connective tissue disease: what is behind the curtain? Best
Pract Res Clin Rheumatol 2007; 21:1037.
3. Bennett, RM. Overlap Syndromes. In: Textbook of Rheumatology, 8th Ed, Harris, ED
(Ed), W. B. Saunders Co, Philadelphia 2009. pp. 1381-99.
4. Bodolay E, Csiki Z, Szekanecz Z, et al. Five-year follow-up of 665 Hungarian patients
with undifferentiated connective tissue disease (UCTD). Clin Exp Rheumatol 2003;
21:313.
5. Mosca M, Tani C, Neri C, et al. Undifferentiated connective tissue diseases (UCTD).
Autoimmun Rev 2006; 6:1.
6. Farhey Y, Hess EV. Mixed connective tissue disease. Arthritis Care Res 1997; 10:333.
7. Rasmussen EK, Ullman S, Høier-Madsen M, et al. Clinical implications of
ribonucleoprotein antibody. Arch Dermatol 1987; 123:601.
8. Lambova SN, Kuzmanova SI. Raynaud's phenomenon in common rheumatic diseases.
Folia Med (Plovdiv) 2006; 48:22.
9. Maldonado ME, Perez M, Pignac-Kobinger J, et al. Clinical and immunologic
manifestations of mixed connective tissue disease in a Miami population compared to a
Midwestern US Caucasian population. J Rheumatol 2008; 35:429.
10. Kitridou RC, Akmal M, Turkel SB, et al. Renal involvement in mixed connective tissue
disease: a longitudinal clinicopathologic study. Semin Arthritis Rheum 1986; 16:135.
11. Bennett, RM. Mixed Connective Tissue Disease and Overlap Syndromes. In: Textbook of
Rheumatology, 7th Edition, Harris, ED, et al. (Eds), W.B. Saunders, Philadelphia 2004.
pp. 1241-529.
12. Bennett RM, O'Connell DJ. The arthritis of mixed connective tissue disease. Ann Rheum
Dis 1978; 37:397.
13. Pope JE. Other manifestations of mixed connective tissue disease. Rheum Dis Clin North
Am 2005; 31:519.
14. Hassoun PM. Pulmonary arterial hypertension complicating connective tissue diseases.
Semin Respir Crit Care Med 2009; 30:429.
15. Hoffman RW, Maldonado ME. Immune pathogenesis of Mixed Connective Tissue
Disease: a short analytical review. Clin Immunol 2008; 128:8.
16. Nakae, K, Furusawa, F, Kasukawa, R, et al. A nationwide epidemiological survey on
diffuse collagen diseases: Estimation of prevalence rate in Japan. In: Mixed Connective
Tissue Disease and Anti-nuclear Antibodies, Kasukawa, R, Sharp, G (Eds), Excerpta
Medica, Amsterdam, 1987. p.9.
17. Christopher-Stine L, Wigley F. Tumor necrosis factor-alpha antagonists induce lupus-like
syndrome in patients with scleroderma overlap/mixed connective tissue disease. J
Rheumatol 2003; 30:2725.
18. Costa MF, Said NR, Zimmermann B. Drug-induced lupus due to anti-tumor necrosis
factor alpha agents. Semin Arthritis Rheum 2008; 37:381.
19. Kuipers EJ, van Leeuwen MA, Nikkels PG, et al. Hemobilia due to vasculitis of the gall
bladder in a patient with mixed connective tissue disease. J Rheumatol 1991; 18:617.
20. Silver TM, Farber SJ, Bole GG, Martel W. Radiological features of mixed connective
tissue disease and scleroderma--systemic lupus erythematosus overlap. Radiology 1976;
120:269.
21. Bodolay E, Szegedi G. [Undifferentiated connective tissue disease]. Orv Hetil 2009;
150:867.
22. Greidinger EL, Hoffman RW. Autoantibodies in the pathogenesis of mixed connective
tissue disease. Rheum Dis Clin North Am 2005; 31:437.
23. Grader-Beck T, Wigley FM. Raynaud's phenomenon in mixed connective tissue disease.
Rheum Dis Clin North Am 2005; 31:465.
24. Bennett RM, O'Connell DJ. Mixed connective tisssue disease: a clinicopathologic study
of 20 cases. Semin Arthritis Rheum 1980; 10:25.
25. Venables PJ. Mixed connective tissue disease. Lupus 2006; 15:132.
26. Goolamali SI, Gordon P, Salisbury J, Creamer D. Subcutaneous calcification presenting
in a patient with mixed connective tissue disease and cutaneous polyarteritis nodosa. Clin
Exp Dermatol 2009; 34:e141.
27. Setty YN, Pittman CB, Mahale AS, et al. Sicca symptoms and anti-SSA/Ro antibodies
are common in mixed connective tissue disease. J Rheumatol 2002; 29:487.
28. Hamza M. Orogenital ulcerations in mixed connective tissue disease. J Rheumatol 1985;
12:643.
29. Willkens RF, Roth GJ, Novak A, Walike JW. Perforation of nasal septum in rheumatic
diseases. Arthritis Rheum 1976; 19:119.
30. Paredes JG, Lazaro MA, Citera G, et al. Jaccoud's arthropathy of the hands in overlap
syndrome. Clin Rheumatol 1997; 16:65.
31. O'Connell DJ, Bennett RM. Mixed connective tissue disease--clinical and radiological
aspects of 20 cases. Br J Radiol 1977; 50:620.
32. Ramos-Niembro F, Alarcón-Segovia D, Hernández-Ortíz J. Articular manifestations of
mixed connective tissue disease. Arthritis Rheum 1979; 22:43.
33. Martínez-Cordero E, López-Zepeda J. Resorptive arthropathy and rib erosions in mixed
connective tissue disease. J Rheumatol 1990; 17:719.
34. Halla JT, Hardin JG. Clinical features of the arthritis of mixed connective tissue disease.
Arthritis Rheum 1978; 21:497.
35. Mimura Y, Ihn H, Jinnin M, et al. Rheumatoid factor isotypes in mixed connective tissue
disease. Clin Rheumatol 2006; 25:572.
36. Takasaki Y, Yamanaka K, Takasaki C, et al. Anticyclic citrullinated peptide antibodies in
patients with mixed connective tissue disease. Mod Rheumatol 2004; 14:367.
37. Alarcón-Segovia D, Cardiel MH. Comparison between 3 diagnostic criteria for mixed
connective tissue disease. Study of 593 patients. J Rheumatol 1989; 16:328.
38. Amigues JM, Cantagrel A, Abbal M, Mazieres B. Comparative study of 4 diagnosis
criteria sets for mixed connective tissue disease in patients with anti-RNP antibodies.
Autoimmunity Group of the Hospitals of Toulouse. J Rheumatol 1996; 23:2055.
39. Hall S, Hanrahan P. Muscle involvement in mixed connective tissue disease. Rheum Dis
Clin North Am 2005; 31:509.
40. Oxenhandler R, Hart M, Corman L, et al. Pathology of skeletal muscle in mixed
connective tissue disease. Arthritis Rheum 1977; 20:985.
41. Greenberg SA, Amato AA. Inflammatory myopathy associated with mixed connective
tissue disease and scleroderma renal crisis. Muscle Nerve 2001; 24:1562.
42. Vianna MA, Borges CT, Borba EF, et al. Myositis in mixed connective tissue disease: a
unique syndrome characterized by immunohistopathologic elements of both polymyositis
and dermatomyositis. Arq Neuropsiquiatr 2004; 62:923.
43. Troyanov Y, Targoff IN, Tremblay JL, et al. Novel classification of idiopathic
inflammatory myopathies based on overlap syndrome features and autoantibodies:
analysis of 100 French Canadian patients. Medicine (Baltimore) 2005; 84:231.
44. Lundberg IE. Cardiac involvement in autoimmune myositis and mixed connective tissue
disease. Lupus 2005; 14:708.
45. Lash AD, Wittman AL, Quismorio FP Jr. Myocarditis in mixed connective tissue disease:
clinical and pathologic study of three cases and review of the literature. Semin Arthritis
Rheum 1986; 15:288.
46. Whitlow PL, Gilliam JN, Chubick A, Ziff M. Myocarditis in mixed connective tissue
disease. Association of myocarditis with antibody to nuclear ribonucleoprotein. Arthritis
Rheum 1980; 23:808.
47. Haroon N, Nisha RS, Chandran V, Bharadwaj A. Pulmonary hypertension not a major
feature of early mixed connective tissue disease: a prospective clinicoserological study. J
Postgrad Med 2005; 51:104.
48. Sullivan WD, Hurst DJ, Harmon CE, et al. A prospective evaluation emphasizing
pulmonary involvement in patients with mixed connective tissue disease. Medicine
(Baltimore) 1984; 63:92.
49. Prakash UB. Lungs in mixed connective tissue disease. J Thorac Imaging 1992; 7:55.
50. Bull TM, Fagan KA, Badesch DB. Pulmonary vascular manifestations of mixed
connective tissue disease. Rheum Dis Clin North Am 2005; 31:451.
51. Végh J, Szilasi M, Soós G, et al. [Interstitial lung disease in mixed connective tissue
disease]. Orv Hetil 2005; 146:2435.
52. Kozuka T, Johkoh T, Honda O, et al. Pulmonary involvement in mixed connective tissue
disease: high-resolution CT findings in 41 patients. J Thorac Imaging 2001; 16:94.
53. Devaraj A, Wells AU, Hansell DM. Computed tomographic imaging in connective tissue
diseases. Semin Respir Crit Care Med 2007; 28:389.
54. Afeltra A, Zennaro D, Garzia P, et al. Prevalence of interstitial lung involvement in
patients with connective tissue diseases assessed with high-resolution computed
tomography. Scand J Rheumatol 2006; 35:388.
55. Bodolay E, Szekanecz Z, Dévényi K, et al. Evaluation of interstitial lung disease in
mixed connective tissue disease (MCTD). Rheumatology (Oxford) 2005; 44:656.
56. Fagundes MN, Caleiro MT, Navarro-Rodriguez T, et al. Esophageal involvement and
interstitial lung disease in mixed connective tissue disease. Respir Med 2009; 103:854.
57. Burdt MA, Hoffman RW, Deutscher SL, et al. Long-term outcome in mixed connective
tissue disease: longitudinal clinical and serologic findings. Arthritis Rheum 1999; 42:899.
58. Nishimaki T. [Mixed connective tissue disease and overlap syndrome]. Nihon Rinsho
1999; 57:355.
59. Wigley FM, Lima JA, Mayes M, et al. The prevalence of undiagnosed pulmonary arterial
hypertension in subjects with connective tissue disease at the secondary health care level
of community-based rheumatologists (the UNCOVER study). Arthritis Rheum 2005;
52:2125.
60. McGoon MD. The assessment of pulmonary hypertension. Clin Chest Med 2001; 22:493.
61. Chemla D, Castelain V, Hervé P, et al. Haemodynamic evaluation of pulmonary
hypertension. Eur Respir J 2002; 20:1314.
62. Bodolay E, Csipo I, Gál I, et al. Anti-endothelial cell antibodies in mixed connective
tissue disease: frequency and association with clinical symptoms. Clin Exp Rheumatol
2004; 22:409.
63. Vegh J, Szodoray P, Kappelmayer J, et al. Clinical and immunoserological characteristics
of mixed connective tissue disease associated with pulmonary arterial hypertension.
Scand J Immunol 2006; 64:69.
64. Hasegawa EM, Caleiro MT, Fuller R, Carvalho JF. The frequency of anti-beta2glycoprotein I antibodies is low and these antibodies are associated with pulmonary
hypertension in mixed connective tissue disease. Lupus 2009; 18:618.
65. Lundberg IE. The prognosis of mixed connective tissue disease. Rheum Dis Clin North
Am 2005; 31:535.
66. Bennett RM, Spargo BH. Immune complex nephropathy in mixed connective tissue
disease. Am J Med 1977; 63:534.
67. Yoshida A, Morozumi K, Takeda A, Koyama K. [Nephropathy in patients with mixed
connective tissue disease]. Ryumachi 1994; 34:976.
68. Celikbilek M, Elsurer R, Afsar B, et al. Mixed connective tissue disease: a case with
scleroderma renal crisis following abortion. Clin Rheumatol 2007; 26:1545.
69. Yamaguchi T, Ohshima S, Tanaka T, et al. Renal crisis due to intimal hyperplasia in a
patient with mixed connective tissue disease (MCTD) accompanied by pulmonary
hypertension. Intern Med 2001; 40:1250.
70. Dantas RO, Villanova MG, de Godoy RA. Esophageal dysfunction in patients with
progressive systemic sclerosis and mixed connective tissue diseases. Arq Gastroenterol
1985; 22:122.
71. Ling TC, Johnston BT. Esophageal investigations in connective tissue disease: which
tests are most appropriate? J Clin Gastroenterol 2001; 32:33.
72. Marshall JB, Kretschmar JM, Gerhardt DC, et al. Gastrointestinal manifestations of
mixed connective tissue disease. Gastroenterology 1990; 98:1232.
73. Aoki S, Tada Y, Ohta A, et al. [Autoimmune hepatitis associated with mixed connective
tissue disease: report of a case and a review of the literature]. Nihon Rinsho Meneki
Gakkai Kaishi 2001; 24:75.
74. Nishida S, Fujimoto T, Usui T, et al. [Mixed connective tissue disease (MCTD) with
severe acute pancreatitis]. Nihon Naika Gakkai Zasshi 2001; 90:1518.
75. Bennett RM, Bong DM, Spargo BH. Neuropsychiatric problems in mixed connective
tissue disease. Am J Med 1978; 65:955.
76. Hojaili B, Barland P. Trigeminal neuralgia as the first manifestation of mixed connective
tissue disorder. J Clin Rheumatol 2006; 12:145.
77. Hagen NA, Stevens JC, Michet CJ Jr. Trigeminal sensory neuropathy associated with
connective tissue diseases. Neurology 1990; 40:891.
78. Bronshvag MM, Pyrstowsky SD, Traviesa DC. Vascular headaches in mixed connective
tissue disease. Headache 1978; 18:154.
79. Okada J, Hamana T, Kondo H. Anti-U1RNP antibody and aseptic meningitis in
connective tissue diseases. Scand J Rheumatol 2003; 32:247.
80. Ahmadi-Simab K, Lamprecht P, Reuter M, Gross WL. Pachymeningitis in mixed
connective tissue disease. Ann Rheum Dis 2005; 64:1656.
81. Yasuda Y, Akiguchi I, Kameyama M. Sulindac-induced aseptic meningitis in mixed
connective tissue disease. Clin Neurol Neurosurg 1989; 91:257.
82. Hoffman M, Gray RG. Ibuprofen-induced meningitis in mixed connective tissue disease.
Clin Rheumatol 1982; 1:128.
83. Hajas A, Szodoray P, Barath S, et al. Sensorineural hearing loss in patients with mixed
connective tissue disease: immunological markers and cytokine levels. J Rheumatol
2009; 36:1930.
84. Toyoda K, Tsuji H, Sadoshima S, et al. Brain hemorrhage in mixed connective tissue
disease. A case report. Angiology 1994; 45:967.
85. Bhinder S, Harbour K, Majithia V. Transverse myelitis, a rare neurological manifestation
of mixed connective tissue disease--a case report and a review of literature. Clin
Rheumatol 2007; 26:445.
86. Kappes J, Bennett RM. Cauda equina syndrome in a patient with high titer anti-RNP
antibodies. Arthritis Rheum 1982; 25:349.
87. Mimura T, Usui T, Amano S, et al. Retinal vasculitis and vitreous hemorrhage associated
with mixed connective tissue disease: retinal vasculitis in MCTD. Int Ophthalmol 2005;
26:159.
88. Schneider F. [Progressive multifocal leukoencephalopathy as a cause of neurologic
symptoms in Sharp syndrome]. Z Rheumatol 1991; 50:222.
89. Matsui H, Udaka F, Oda M, et al. Encephalopathy and severe neuropathy due to probable
systemic vasculitis as an initial manifestation of mixed connective tissue disease. Neurol
India 2006; 54:83.
90. Luostarinen L, Himanen SL, Pirttilä T, Molnar G. Mixed connective tissue disease
associated with chronic inflammatory demyelinating polyneuropathy. Scand J Rheumatol
1999; 28:328.
91. Sharp GC, Irvin WS, May CM, et al. Association of antibodies to ribonucleoprotein and
Sm antigens with mixed connective-tissue disease, systematic lupus erythematosus and
other rheumatic diseases. N Engl J Med 1976; 295:1149.
92. Hämeenkorpi R, Ruuska P, Forsberg S, et al. More evidence of distinctive features of
mixed connective tissue disease. Scand J Rheumatol 1993; 22:63.
93. Hoffman RW, Greidinger EL. Mixed connective tissue disease. Curr Opin Rheumatol
2000; 12:386.
94. Majetschak M, Perez M, Sorell LT, et al. Circulating 20S proteasome levels in patients
with mixed connective tissue disease and systemic lupus erythematosus. Clin Vaccine
Immunol 2008; 15:1489.
95. Komatireddy GR, Wang GS, Sharp GC, Hoffman RW. Antiphospholipid antibodies
among anti-U1-70 kDa autoantibody positive patients with mixed connective tissue
disease. J Rheumatol 1997; 24:319.
96. Doria A, Ruffatti A, Calligaro A, et al. Antiphospholipid antibodies in mixed connective
tissue disease. Clin Rheumatol 1992; 11:48.
97. Watanabe H, Kaise S, Takeda I, et al. Anti-endothelial cell antibodies in the sera of
patients with mixed connective tissue disease--the clinical significance. Fukushima J Med
Sci 1997; 43:13.
98. Kikuchi T, Yoshida Y, Morioka T, et al. Human voltage-dependent anion selective
channel 1 is a target antigen for antiglomerular endothelial cell antibody in mixed
connective tissue disease. Mod Rheumatol 2008; 18:570.
99. Magro CM, Ross P, Marsh CB, et al. The role of anti-endothelial cell antibody-mediated
microvascular injury in the evolution of pulmonary fibrosis in the setting of collagen
vascular disease. Am J Clin Pathol 2007; 127:237.
100.
Kajita N, Muro Y, Tomita A, et al. [Thrombotic thrombocytopenic purpura with
mixed connective tissue disease. A case report]. Arerugi 2009; 58:567.
101.
Kuroda T, Matsuyama K, Nakatsue T, et al. A case of mixed connective tissue
disease complicated with thrombotic thrombocytopenic purpura. Clin Rheumatol 2007;
26:101.
102.
Kao YS, Kirkley KC. A patient with mixed connective tissue disease and mixedtype autoimmune hemolytic anemia. Transfusion 2005; 45:1695.
103.
Julkunen H, Jäntti J, Pettersson T. Pure red cell aplasia in mixed connective tissue
disease. J Rheumatol 1989; 16:1385.
104.
Greidinger EL, Foecking MF, Ranatunga S, Hoffman RW. Apoptotic U1-70 kd is
antigenically distinct from the intact form of the U1-70-kd molecule. Arthritis Rheum
2002; 46:1264.
105.
Alpert MA, Goldberg SH, Singsen BH, et al. Cardiovascular manifestations of
mixed connective tissue disease in adults. Circulation 1983; 68:1182.
106.
Blockmans D, Vermylen J, Bobbaers H. Nailfold capillaroscopy in connective
tissue disorders and in Raynaud's phenomenon. Acta Clin Belg 1993; 48:30.
107.
Furtado RN, Pucinelli ML, Cristo VV, et al. Scleroderma-like nailfold
capillaroscopic abnormalities are associated with anti-U1-RNP antibodies and Raynaud's
phenomenon in SLE patients. Lupus 2002; 11:35.
108.
Lambova SN, Müller-Ladner U. The role of capillaroscopy in differentiation of
primary and secondary Raynaud's phenomenon in rheumatic diseases: a review of the
literature and two case reports. Rheumatol Int 2009; 29:1263.
109.
Peller JS, Gabor GT, Porter JM, Bennett RM. Angiographic findings in mixed
connective tissue disease. Correlation with fingernail capillary photomicroscopy and
digital photoplethysmography findings. Arthritis Rheum 1985; 28:768.
110.
Kitridou RC. Pregnancy in mixed connective tissue disease. Rheum Dis Clin
North Am 2005; 31:497.
111.
Chung L, Flyckt RL, Colón I, et al. Outcome of pregnancies complicated by
systemic sclerosis and mixed connective tissue disease. Lupus 2006; 15:595.
112.
Kaufman RL, Kitridou RC. Pregnancy in mixed connective tissue disease:
comparison with systemic lupus erythematosus. J Rheumatol 1982; 9:549.
113.
Kari JA. Pregnancy outcome in connective tissue diseases. Saudi Med J 2001;
22:590.
114.
Ackerman J, Gonzalez EF, Gilbert-Barness E. Immunological studies of the
placenta in maternal connective tissue disease. Pediatr Dev Pathol 1999; 2:19.
115.
Bodolay E, Bojan F, Szegedi G, et al. Cytotoxic endothelial cell antibodies in
mixed connective tissue disease. Immunol Lett 1989; 20:163.
116.
Kahl LE, Blair C, Ramsey-Goldman R, Steen VD. Pregnancy outcomes in women
with primary Raynaud's phenomenon. Arthritis Rheum 1990; 33:1249.
117.
Lundberg I, Hedfors E. Pregnancy outcome in patients with high titer anti-RNP
antibodies. A retrospective study of 40 pregnancies. J Rheumatol 1991; 18:359.
Topic 7546 Version 3.0
© 2012 UpToDate, Inc. All rights reserved. | Subscription and License Agreement |Release: 20.5
- C20.7
Licensed to: UpToDate Individual Web - Robert M . Bennett |Support Tag:
[ecapp1002p.utd.com-24.22.31.16-7EA7EECCC5-6.14-2242]