MAYO CLINIC HEALTH LETTER
Reliable Information for a Healthier Life
VOLUME 30
NUMBER 7
JULY 2012
Inside this issue
HEALTH TIPS . . . . . . . . . . . . . . . . . . 3
Freshen bad breath.
NEWS AND OUR VIEWS . . . . . . 4
Increased emphasis on exercise
for osteoarthritis. New drug shows
promise for advanced colorectal
cancer.
HAND TREMORS . . . . . . . . . . . . . . 4
Not always Parkinson’s disease.
TINNITUS . . . . . . . . . . . . . . . . . . . . . . 6
Notice the noise less.
PREOPERATIVE
EVALUATION . . . . . . . . . . . . . . . . . . 7
Avoiding surprises.
Chronic
lung disease
Pay attention
to your breath
Persistent shortness of breath and a
chronic cough lasting more than three
to six weeks may signal a potentially
serious or chronic lung condition such
as chronic obstructive pulmonary disease (COPD).
COPD refers to a group of lung
­diseases that limit airflow as you exhale
and make it increasingly difficult to
breathe out. COPD affects millions of
Americans and is usually attributed to
exposure to tobacco smoke and airborne irritants over a period of time.
Most often, it occurs in long-term or
former smokers. Left untreated and allowed to progress, COPD literally takes
your breath away, making it a leading
cause of death in the United States.
Damage done to the lungs by COPD
isn’t fully reversible. That’s why early
diagnosis, treatment and prevention —
particularly physical activity and smoking cessation — are critically important.
When COPD is detected early, management improves symptoms and survival.
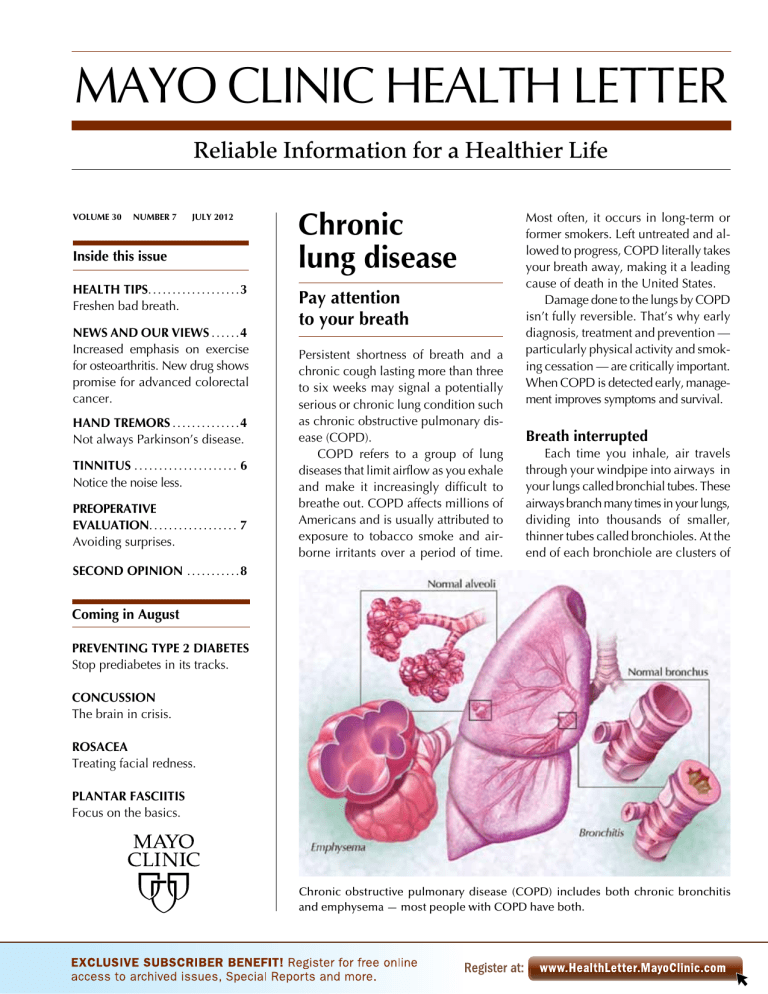
Breath interrupted
Each time you inhale, air travels
through your windpipe into airways in
your lungs called bronchial tubes. These
airways branch many times in your lungs,
dividing into thousands of smaller,
­thinner tubes called bronchioles. At the
end of each bronchiole are clusters of
SECOND OPINION . . . . . . . . . . . 8
Coming in August
PREVENTING TYPE 2 DIABETES
Stop prediabetes in its tracks.
CONCUSSION
The brain in crisis.
ROSACEA
Treating facial redness.
PLANTAR FASCIITIS
Focus on the basics.
Chronic obstructive pulmonary disease (COPD) includes both chronic bronchitis
and emphysema — most people with COPD have both.
air sacs (alveoli). Inside the walls of the
alveoli, tiny blood vessels (capillaries)
absorb inhaled oxygen and release carbon dioxide so it can be exhaled.
Healthy bronchioles and alveoli are
stretchy, so when you breathe in, each
little air sac fills up like a balloon, and
when you exhale, each one deflates.
Although a slight decline in lung function is part of normal aging, it’s a different scenario for lungs damaged by
COPD. The tubes can be thickened or
plugged with mucus, and the air sacs
can be destroyed and very floppy. As a
result, the lungs can’t expel air as well,
so they become less efficient. This process
becomes gradually worse over time —
more slowly if you stop smoking and
faster if you continue.
Elements of risk
Risk of developing COPD is mainly
related to your lungs’ exposure to irritants. Tobacco smoke tops the list, but
there are others — dust, secondhand
smoke, air pollution, and industrial gases,
vapors and fumes. Indoor fires for heating and cooking are a major cause in
developing countries.
Some COPD risk factors are inherited. One is a rare genetic disorder
known as alpha-1-antitrypsin deficiency, which is the cause of about 1 percent of cases of COPD. People with
asthma or sensitive airways (bronchial
hyperresponsiveness) also have increased risk.
Signs and symptoms of COPD are
usually slowly progressive. They may
include shortness of breath, wheezing,
chest tightness, chronic cough, and
sputum or phlegm production.
COPD includes both chronic bronchitis and emphysema — most people
with COPD have both. Chronic bronchitis is defined by the presence of a
cough and sputum production. Other
characteristics include chronic inflammation and thickening of airways.
Emphysema is defined by chronic
damage to the alveoli. This chronic
­injury — usually from smoking — destroys the inner walls of alveolar clus-
2
www.HealthLetter.MayoClinic.com
ters, reducing the surface area available
to exchange oxygen for carbon dioxide
and allowing them to overexpand. Normally, the alveolar walls are stretchy.
Emphysema causes them to lose elasticity, so they fail to contract during
exhalation, trapping air in the lungs.
The result is shortness of breath because the chest muscles have to work
harder to breathe in and out.
Pulmonary function tests are key in
diagnosing COPD and its stage. Spirometry uses a machine (spirometer) to
measure how much air you can blow
out of your lungs, and how quickly you
can blow air out. Spirometry is an important test for current or former smokers who have COPD symptoms. Spirometry also is used to track how well
treatment is working.
Your doctor may recommend getting
a chest X-ray or a computerized tomography (CT) scan to look for other problems. CT may be helpful to screen for
early lung cancer, which is a risk for
smokers, especially those with COPD.
A blood test may be done to see how
capable your lungs are of supplying
oxygen to your blood and removing
carbon dioxide. Sputum (phlegm) can
be examined under a microscope for
cancer cells, but that’s not recommended as a screening tool.
Treatment options
Treatment focuses on minimizing
further damage, controlling symptoms
and preventing sudden worsening of
COPD, called an exacerbation. Foremost is eliminating exposure to the irritant that’s damaged your lungs. If you
smoke, it’s very important to stop in
order to keep your COPD from getting
worse. After smoking cessation, you’ll
likely have fewer symptoms and your
lung function may improve slightly.
Vaccination against pneumonia
and an annual influenza vaccine are
strongly recommended for anyone who
has COPD. Flu shots reduce risk of res­
piratory hospitalization by up to half.
Adopting a physically active lifestyle
is of critical importance — research
July 2012
demonstrates that people with COPD
who exercise do better overall. Studies
show that people who have COPD and
walk more than two hours a day have a
much easier time managing their COPD.
Several groups of medications are
used to treat the symptoms and complications of COPD. Some may be taken
on a regular basis and others as needed.
These include:
n Bronchodilators — Drugs such as
albuterol, ipratropium (Atrovent) and a
number of others are used as bronchodilators to help relax muscles around
your airways. The various bronchodilators work by different mechanisms and
usually come in an inhaler. They can
help relieve coughing and make breathing easier. Depending on how severe
your COPD is, you may need a short-
MAYO CLINIC HEALTH LETTER
Managing Editor
Aleta Capelle
Medical Editor
Robert Sheeler, M.D.
Associate Editors
Carol Gunderson
Joey Keillor
Associate Medical Editor
Amindra Arora, M.D.
Medical Illustration
Michael King
Editorial Research
Deirdre Herman
Proofreading
Customer Service Manager Miranda Attlesey
Ann Allen
Donna Hanson
Julie Maas
Administrative Assistant
Beverly Steele
EDITORIAL BOARD
Shreyasee Amin, M.D., Rheumatology; Amindra
Arora, M.B., B.Chir., Gastroenterology and Hepatology;
Brent Bauer, M.D., Internal Medicine; Julie Bjoraker,
M.D., Internal Medicine; Lisa Buss Preszler, Pharm.D.,
Pharmacy; Bart Clarke, M.D., Endocrinology and
Metabolism; William Cliby, M.D., Gynecologic
Surgery; Clayton Cowl, M.D., Pulmonary and Critical
Care; Mark Davis, M.D., Derma­tology; Michael
Halasy, P.A.-C., Emergency Medicine; Timothy
Moynihan, M.D., Oncology;Suzanne Norby, M.D.,
Nephrology; Norman Rasmussen, Ed.D., Psychology;
Daniel Roberts, M.D., Hospital Internal Medicine;
Robert Sheeler, M.D., Family Medicine; Phillip
Sheridan, D.D.S., Perio­don­tics; Peter Southorn, M.D.,
Anes­thesiology; Ronald Swee, M.D., Radiology;
Farris Timimi, M.D., Cardiology; Matthew Tollefson,
M.D., Urology; Debra Zillmer, M.D., Orthopedics;
Aleta Capelle, Health Information. Ex officio: Carol
Gunderson, Joey Keillor.
Mayo Clinic Health Letter (ISSN 0741-6245) is
published monthly by Mayo Foundation for Medical
Education and Research, a subsidiary of Mayo
Foundation, 200 First St. SW, Rochester, MN 55905.
Subscription price is $29.55 a year, which includes a
cumulative index published in December. Periodicals
postage paid at Rochester, Minn., and at additional
mailing offices. POSTMASTER: Send address changes
to Mayo Clinic Health Letter, Subscription Services,
P.O. Box 9302, Big Sandy, TX 75755-9302.
acting bronchodilator just before activities, a long-acting one for everyday
use, or both. Long-acting bronchodilators are typically prescribed if you have
moderate to severe COPD.
n Inhaled corticosteroids — These
drugs don’t slow decline in lung function, but when used selectively they
do reduce airway inflammation. Their
use is fundamental in treating all but
the mildest cases of asthma. For people whose symptoms indicate both
asthma and COPD, inhaled corticosteroids are probably appropriate in
most cases.
Importantly, inhaled corticosteroids
may be prescribed to prevent sudden
exacerbations. They can be beneficial
for people who have more than one
exacerbation in a year. Exacerbations
are often due to chest colds.
In the wake of a severe exacerbation
that requires hospitalization, inhaled
corticosteroids are usually prescribed
for six months or even longer. The most
common side effects of corticosteroids
include increased risk of skin bruising,
hoarseness and a yeast infection in the
mouth, which can be prevented by gargling after using the inhaler.
n Antibiotics — These are used when
necessary to fight respiratory infections
— such as acute bronchitis and pneumonia and influenza — and to prevent
flare-ups of COPD in certain situations.
They’re mainly recommended for acute
exacerbations.
Supplemental oxygen also may be
needed. Some people require constant
oxygen, others may need it only during
activity or sleep.
A pulmonary rehabilitation program can be your opportunity to better
understand COPD and to adopt a lifestyle that may improve your quality of
life and also slow the progression of
COPD. Typically, these programs are
provided by a team of health care professionals who combine education
with the introduction of a more active
lifestyle. Regular exercise improves
endurance and the efficiency of your
cardiovascular system. Pulmonary re-
habilitation is customized to your
needs no matter what roadblocks you
may have or how severe your disability. It’s effective even for people with
such severe lung disease that they are
eligible for lung transplantation.
Surgery may be considered if you
have severe emphysema that isn’t
helped enough with medications alone.
Lung volume reduction involves removal of damaged lung tissue. This
creates extra space for the remaining
lung tissue and diaphragm to work
more efficiently. Single- or double-lung
transplants may be an option for people
with severe emphysema who meet specific criteria. Both of these surgeries are
specialized options for some with very
severe COPD. New therapies, such as
endobronchial valves, are in development but are experimental.
When things get worse
Even with optimal COPD treatment,
you may encounter sudden exacerbations. About half of exacerbations are
due to either viral or bacterial infections, though some are due to irritants.
Exacerbations are serious threats.
Without prompt treatment, one may
lead to lung failure and the need for
hospitalization. People with only mild
or moderate COPD can develop severe
exacerbations. People with previous
exacerbations are the most likely to
develop recurrent exacerbations.
For some people predisposed to
exacerbations, long-term use of an
anti-inflammatory antibiotic or a bronchodilator that also acts as an anti-inflammatory may help prevent further
exacerbations. For instance, roflumilast
(Daliresp) is in the latter group of drugs.
It’s approved to help prevent exacerbations in people whose COPD is due
primarily to chronic bronchitis.
If you develop a chest cold or notice
more coughing or a change in your mucus,
or if you have a harder time breathing,
seek medical attention. Treatment for
exacerbations usually requires antibiotics.
Oral steroids are usually required to
treat severe exacerbations. ❒
July 2012
Health tips
Freshen bad breath
Bad breath (halitosis) often stems
from food particles in your mouth
or from a health problem. To prevent or reduce bad breath:
■ Clean your teeth after you eat
— Brushing your teeth is best, but
if not convenient to do so, 30
seconds of swishing with mouthwash or chewing sugarless gum
can help rid the mouth of food
particles that contribute to halitosis.
■ Floss your teeth at least once
a day — Flossing removes decaying food from between your teeth.
■ Clean the back of your tongue
— Mucus from postnasal drip can
decay on the back of your tongue.
You can remove this by brushing
your tongue or scraping it with a
tongue scraper. Gargling with
mouthwash also can help.
■ Drink water or chew gum —
When your mouth is dry, there’s
insufficient saliva to wash away
dead cells and food debris. Water
helps keep your mouth moist,
and chewing sugarless gum can
stimulate saliva production.
■ Clean your dentures daily —
They can harbor bacteria and
food particles.
■ Limit foods or beverages that
may cause bad breath — This
includes onions and garlic, because oils from these are absorbed through the lungs and
exhaled. Coffee and alcohol can
also cause bad breath.
■ See your dentist or doctor —
Bad breath that doesn’t respond
to simple measures may be related to a health problem such as
gum disease, an abscessed tooth,
infection, sinus problems, chronic bronchitis, certain throat problems or another condition. ❒
www.HealthLetter.MayoClinic.com
3
News and our views
Increased emphasis on exercise for osteoarthritis
Revised treatment guidelines released in spring 2012 by the
American College of Rheumatology (ACR) confirm what
you may already know if you have knee or hip osteoarthritis
— exercise can be a very effective treatment tool.
In terms of nondrug treatment strategies for knee or hip
osteoarthritis, the ACR strongly supports involvement in
regular aerobic exercise or strengthening — or both. If
you’re out of condition, the ACR recommends the exercise be geared to
your abilities and preferences. That may mean taking part in a water exercise
program, which provides some resistance training and is a gentle way to
start exercising — especially if weight-bearing activity is painful. Water
exercise also helps you improve your aerobic capacity. After accomplishing
that, exercise options can move beyond the pool if you wish. The ACR suggests working with your doctor or physical therapist to put in place an
aerobic exercise conditioning plan or a strengthening program, or if you
prefer, both can be done. The key is to gear the exercise activity to your
interests and ability. In addition to exercise, the ACR recommends discussing weight loss with your doctor if you’re overweight and have knee or hip
pain related to osteoarthritis.
Mayo Clinic experts say the updated ACR recommendations substantiate
what they’ve seen in clinical practice. When properly done, exercise can
help strengthen muscles that support hip and knee joints affected by osteoarthritis. That muscle support helps stabilize the joints, which contributes
to reduced pain and the ability to remain mobile. ❒
New drug shows promise for advanced colorectal cancer
Treating advanced colon cancer can be difficult, and when treatment isn’t
effective at stopping cancer progression, medical options for prolonging life
and improving quality of life are limited.
However, a recent international study led by a Mayo Clinic oncologist
has shown that an experimental drug — regorafenib — can help stabilize
colorectal cancer in some people when all other treatment methods have
failed. Regorafenib works by inhibiting factors that contribute to cancer
advancement, and that promote multiplication of cancer cells and the
­development of new blood vessels that nourish cancer cells.
The study involved about 750 people who had advancing colorectal
cancer even after standard treatments had been tried. Those who received
regorafenib lived about six months, whereas those who received a placebo
lived about five months. In addition, the cancer stabilized in about 43 percent
of those on regorafenib and only in about 14 percent of those taking the placebo.
Side effects of regorafenib included fatigue, skin rashes, diarrhea, mouth
sores and high blood pressure. However, only about 8 percent of those
­taking regorafenib discontinued the drug due to side effects.
Increasing survival with colorectal cancer by 1 1/2 months may not seem like
much. Still, regorafenib may give people with late-stage colorectal cancer an
additional option to that which existed previously. It’s possible that regorafenib
could prove to be more effective if used at an earlier phase. ❒
4
www.HealthLetter.MayoClinic.com
July 2012
Hand tremors
Not always
Parkinson’s disease
Try holding a piece of paper with your
hand extended out in front of your body
for a short time and you’ll likely see a
slight tremble of the hand. This is totally
normal and goes largely unnoticed. It’s
caused by the motions of your body
processes — your heart beating and
your chest moving as you breathe —
which have a kind of ripple effect on
muscles all over your body.
However, with age, tremors of the
hands and other areas of the body can
become more noticeable, and can even
begin to affect normal actions such as
handwriting, holding a cup, eating with
utensils or even speaking.
This may be annoying or embarrassing — or lead to fear that you may have
a disease such as Parkinson’s. For some,
tremors worsen, making it increasingly
difficult to perform day-to-day tasks.
Tremors can take many forms and
have many causes. Most tremors can’t
be cured, but treatment strategies can
help most who have tremors regain a
measure of control and confidence,
thus making it easier to enjoy life and
maintain independence.
Different tremors
Tremor is indeed one sign of Parkinson’s disease, but most tremors occur for
other reasons. The diagnosis relating
to the various types of tremor can be
difficult without a thorough medical
exam.
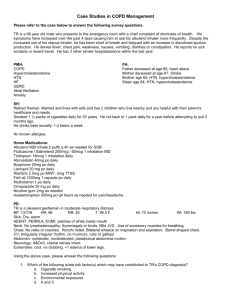
The chart on the next page can help
you understand the common avenues
of therapy for and the typical characteristics of tremor types including:
n Essential tremor
n Parkinsonian tremor
n Physiologic tremor
n Tremor related to brain injury
or disease
n Dystonic tremor
n Orthostatic tremor
Tremor type
Tremor characteristics
First line treatments
Advanced treatments
Essential
tremor
Most common tremor type. Often inherited, caused by unclear mechanisms. Most often affects the hands,
but can affect the head, voice, and
legs. The tremor occurs when you
hold a posture — such as holding your
arms outstretched — or when you
move or perform a task. But usually
doesn’t occur at rest.
Beta blockers such as
propranolol (Inderal) or
nadolol; the anticonvulsant drug primidone (Mysoline). Second line choices
include gabapentin (Neurontin) or topiramate (Topamax).
Parkinsonian
tremor
Often an early sign of Parkinson’s.
Often affects the hand first and looks
as if you’re rolling a pill between
thumb and forefinger. Can affect the
chin, lips or legs, but not the head or
voice. Tremors occur at rest and diminish or go away with movement.
Occurs with other signs of parkinsonism,
such as rigid joints, slow movements
or difficulty walking.
Drugs to control Parkinson’s, such as levodopa
combined with carbidopa (Sinemet), pramipexole (Mirapex) or ropinirole (Requip).
Surgical interventions such
as deep brain stimulation.
This involves implanting a
wire electrode into a specific area of the brain. This
delivers electrical impulses
to stop tremor. The wire
electrode is connected to a
small battery implanted into
the body.
Physiologic
tremor
Occurs when certain short-lived metabolic factors or drugs provoke tremor in otherwise normal people. An
underlying cause leads to an exaggeration of normal tremor. Causes
include stress, anxiety, low blood
sugar, thyroid problems, stimulants
such as caffeine, certain asthma drugs,
corticosteroids or alcohol withdrawal.
Addressing the cause,
whether adjusting a medication dose, switching
medication, reducing caffeine or nicotine intake,
or treating an underlying
disease.
Single doses of propranolol
in anticipation of social
situations that are likely to
cause tremor may be useful
for some.
Tremor
related to
brain injury
or disease
Commonly caused by brain damage
in certain regions, such as provoked
by multiple sclerosis, tumors, trauma
or stroke. The tremor can be very severe and disabling.
For severe tremor of this
type, medications typically fail.
Deep brain stimulation, as
discussed above, may be
necessary in severe cases.
Dystonic
tremor
Associated with dystonia, an involuntary muscle contraction that some
experience as writer’s cramp. Occurs
in the same area as the dystonia.
Usually treatment is directed at the associated
dystonia, which is the primary source of disability.
Medications are usually
ineffective.
Botulinum toxin (Botox)
injections to the affected
muscle group can provide
several months of relief, but
need to be repeated.
Orthostatic
tremor
Limited to the legs and trunk and occurs
with standing. The tremor often isn’t
visible. It results in troubling unsteadiness. Goes away with sitting and usually
improves with walking.
Clonazepam (Klonopin)
proves helpful for some.
Deep brain stimulation has
been studied when other
treatments aren’t effective.
July 2012
www.HealthLetter.MayoClinic.com
5
Tinnitus
Notice the noise less
Whether it’s a ringing, buzzing, roaring, whistling or a hissing noise, tinnitus (TIN-i-tus) is the label for those
sounds you hear in your ear or head. It
can range in severity from being only
mildly annoying or temporary to being
so loud and constant that it interferes
with your ability to concentrate or get
a good night’s sleep.
Occasionally tinnitus may be a sign
of something serious, but usually it’s
not. Still, the more irritating tinnitus
becomes, the more it may result in fatigue and sleep problems, unwanted
Underlying cause
Tinnitus or a worsening of tinnitus
can have an underlying cause.
Sometimes, when the cause can
be addressed, tinnitus may diminish or go away. Tinnitus can
be a side effect of numerous drugs.
If tinnitus occurs or worsens after
starting a new drug, talk to your
doctor about adjusting the dose
or finding another option.
Additional underlying causes
may include excessive earwax,
problems with the neck vertebrae, the joint connecting your
jaw to your skull — called the
temporomandibular joint (TMJ)
— allergies, Meniere’s disease,
middle ear fluid or thyroid problems. Tinnitus that your doctor
can hear with a stethoscope (objective tinnitus) may have an underlying cause such as cardiovascular disease or other blood
vessel problems, high blood pressure, or tumors of the head and
neck. If you have bothersome
tinnitus, talk with an ear, nose
and throat doctor or an audiologist for assistance.
6
www.HealthLetter.MayoClinic.com
stress, memory problems, anxiety, depression, and irritability.
For most people with tinnitus, there’s
no cure. However, various management strategies may help reduce the
amount of noise you hear, distract your
attention from the tinnitus, or help you
find ways to mask the noise.
Hearing loss and damage
Tinnitus isn’t a disease. Rather, it’s
a symptom of something wrong with
the hearing mechanism, hearing nerves,
or part of the brain that processes
sound. Most of the time, tinnitus is believed to be the result of damage to
cells of the inner ear. Tiny delicate hairs
in your inner ear move in relation to
sound waves. This movement sends
signals to your brain. Your brain interprets these signals as sound.
If the tiny hairs become bent or broken — usually as a result of exposure
to loud noises or age-related hearing
loss — they may send random signals
to the brain, resulting in the sensation
of sound when there is none.
When tinnitus develops due to hearing loss or damage — with no correctable
underlying cause — management generally focuses on finding ways to reduce
the amount of irritation that tinnitus
causes. More than one method may need
to be tried — or a combination of strategies may be necessary. Sound therapy is
one technique, which may include:
■ Hearing aids — If you have hearing
loss and tinnitus, hearing aids may
help. Hearing aids help you hear the
sounds around you better, which may
reduce your awareness of tinnitus.
■ Using a masking noise — This may
include a small device you wear in
your ear that emits pleasant sounds —
such as soft, steady noise, tones or music — that cover your tinnitus. These
can be combined with hearing aids in
a single device. Tabletop sound machines can be used in your bedroom
so that you don’t notice your tinnitus
as you sleep. A fan or soft noise from
an FM radio tuned between stations
may achieve a similar result.
July 2012
■ Tinnitus retraining therapy — This
involves listening to a low-level steady
noise, which over time may desensitize
you to the tinnitus so that you no longer
notice it unless you pay attention to it.
This is usually reserved for more severe
tinnitus, and is done as part of a more
comprehensive long-term tinnitus management program that includes counseling. There are numerous tinnitus
retraining clinics throughout the U.S.
Other management methods:
■ Counseling — Cognitive behavioral therapy with a trained professional can help you reframe your view
of tinnitus so that it causes less distress.
■ Managing sleep problems, anxiety,
stress and depression — These often go
hand in hand with severe tinnitus.
Learning how to manage them may
help improve your ability to tolerate
tinnitus. Medications commonly used
for depression or anxiety may help reduce tinnitus severity — and may also
help by improving your mood.
■ Preventing it from getting worse —
Turn music volume down or use earplugs or hearing protectors whenever
you’re around loud noises. ❒
When the tiny, delicate hairs in your inner ear become bent or broken, they
send random signals to the brain, resulting in the sensation of sound when
there is none.
Preoperative
evaluation
Avoiding surprises
It’s time to have surgery to replace your
hip joint. You’re ready to get on with it
— how about tomorrow? Not so fast.
You’ll need a preoperative evaluation before surgery. This is done to determine how you’ll likely do under
anesthesia and during surgery. It also
helps your doctors take steps to improve your ability to go through surgery
and have the best possible outcome.
Key elements
The type of evaluation you undergo
before a scheduled surgery is customized to your situation. Results can vary
considerably based on age, health and
the risks of the procedure. Driving the
evaluation is information from your
medical history and a physical exam:
■ Medical history — A thorough review
includes a list of medications and supplements you take, if you have allergies to
any medications, your experience with
any previous anesthesia, and whether
you smoke or use alcohol.
Among other questions, you’ll be
asked about any symptoms you’re experiencing. Cough, chest pain, shortness of breath during exertion or ankle
swelling might indicate a disorder affecting your heart or lungs. Fever or
pain while urinating may indicate infection. Any known medical problems
— particularly high blood pressure
(hypertension), chronic lung disorders,
diabetes, bleeding disorders, and heart,
kidney or liver disease — may increase
risk of complications and are factored
into whether other tests are needed.
■ Physical examination — Along with
height and weight, your vital signs are
taken, including blood pressure, pulse
and breathing rate. Particular attention
is given to your heart and lungs.
Based on these exams, some modifications may be recommended before
a scheduled surgery. For example, stopping smoking is associated with improved surgical outcomes, improved
wound healing and reduced complications. If you normally take medications,
your doctor may discuss which ones to
continue before surgery and which you
can safely discontinue. If you have
asthma or chronic obstructive pulmonary disease (COPD), steroids and
bronchodilators may be given before
and after surgery to help with lung function. If you’ve taken oral or injected
steroids within the last year, it’s important to tell your care team during your
preoperative evaluation.
Sometimes, elective surgery is put
on hold. For example, if a productive
cough and fever are present, scheduled
surgery is typically delayed. If you’ve
had a recent heart attack, it may be best
to delay surgery to reduce your risk of
having another. If you have poorly controlled diabetes, surgery may be delayed until it’s properly treated.
a­ nemia or if anemia is suspected. The test
is generally recommended if you are 65
or older or scheduled for major surgery.
■ Serum electrolytes — A balanced
blood potassium level is of particular
interest. Potassium plays an important
role in normal heart rhythm. Measuring
your potassium level may be of extra
significance if you take digoxin, diuretics, angiotensin-converting enzyme
(ACE) inhibitors or angiotensin receptor
blockers (ARBs).
■ Chest X-ray — This is no longer routinely done before surgery, but may be
recommended depending on the type
of surgery you’re having, or if you have
a cough or signs or symptoms of new
or unstable heart or lung disease. ❒
Further evaluation
Specific laboratory or other tests
also may be recommended before surgery. Tests that may be done include:
■ Electrocardiogram (ECG) — This
noninvasive test monitors your heart for
irregularities in its rhythm and structure. If you’ve not had a recent ECG, it
may be recommended if you have a
history of diabetes, hypertension, chest
pain, congestive heart failure, smoking,
peripheral vascular disease, extreme
obesity or if you’re unable to exercise.
An ECG may also be done if you’re
older than 65 or if your preoperative
evaluation turns up new cardiovascular
symptoms or evidence of new or unstable heart disease.
■ Blood-clotting (coagulation) studies
— These studies may be done if you
take an anti-clotting medication or have
a known history of bleeding susceptibility or a recent history that suggests
clotting problems may be present.
■ Hemoglobin — This blood test looks
at your oxygen-carrying red blood cells
and may be ordered if you’ve had
July 2012
About beta blockers
Beta blocker drugs are commonly used to help manage heart
health. They help reduce blood
pressure by lowering the rate at
which your heart beats, relaxing
blood vessels and reducing the
heart’s demand for oxygen. Beta
blockers are thought to stabilize
atherosclerotic plaques in artery
linings, making rupture of plaques
and clot formation less likely.
Because of these properties,
beta blockers may also help prevent cardiovascular complications
during surgery.
If you normally take a beta
blocker, guidelines support continuing its use before, during and
after surgery. Beta blockers are
also suggested if you are having
vascular surgery and have had a
stress test that indicates heart
function problems. Outside of
these situations, first-time use of
beta blockers for noncardiac surgery is less certain. That type of
decision depends on your cardiovascular health and can be determined by your doctor.
www.HealthLetter.MayoClinic.com
7
Second opinion
Q
What’s the difference between
a regular bunion and a tailor’s
bunion?
A
A tailor’s bunion — or bunionette
— affects the little toe and is very
much like a regular bunion, which occurs on the big toe. Both types appear
as a protrusion at
the joint where the
longer foot bones
(metatarsals) meet
the toe bones (phalanges). The protrusion is caused by
bone or tissue at the
joint that moves out
of place, forcing the
toe to bend toward the three middle toes
of the foot. Both may occur on the same
foot, or just one of them may be present.
The result can be redness, swelling, tenderness and pain over the bony prominence. Walking — even wearing shoes
— can be painful.
A tailor’s bunion, like a regular bunion, generally comes about over years
of abnormal pressure and motion applied to the bony prominence of the
metatarsal. It gets its name from the fact
that tailors traditionally sat cross-legged
while working, leading to pressure on
the little toe joint. Some factors involved
may be the way you walk, inherited foot
types and the type of shoe you wear.
Shoes that are too small, too narrow
or have heels higher than 2 1/4 inches
are common aggravators of bunions.
When shoes are too small, there’s not
enough room for the natural spread of
the toes. Elevated heels focus pressure
onto the toes.
Both types of bunions can be managed by never forcing your foot into a
shoe that doesn’t fit. Choose shoes with
adequate width and depth in the toe
box. Applying protective, nonmedicated
bunion pads may help cushion a bunion
inside properly fitted shoes. Nonprescription anti-inflammatory medications
may help relieve pain. Short periods of
icing may also help, but may not be advisable if you have diabetes or poor
circulation in your feet.
Surgical treatment is generally a last
resort if pain makes walking difficult or
shoe accommodations don’t help. ❒
Q
A
I got swimmer’s itch last summer.
How do I avoid getting it again?
Swimmer’s itch is typically a rash
caused by an allergic reaction to
certain parasites that normally live inside freshwater snails and water animals. On warm days, these parasites
can be released into freshwater lakes
— or occasionally into salt water. During your swim, the parasites can burrow into your skin. But humans aren’t
suitable hosts, so the parasites soon die.
You may be able to avoid swimmer’s itch by:
■ Choosing swimming spots carefully
— Avoid areas where swimmer’s itch
is a known problem. Also avoid swimming or wading in marshy, mucky areas or areas of aquatic vegetation
where snails are commonly found.
■ Avoiding spending time in shallow
water as much as possible — If you’re
a strong swimmer, head to deeper
­water for your swim. The parasites are
more likely to be found in warmer water
near the shore.
■ Rinsing after swimming — Rinse
exposed skin with fresh water immediately after leaving the water, then vigorously dry your skin with a towel. This
may prevent the parasites from penetrating into the skin. Launder your
swimsuits often.
Although uncomfortable, swimmer’s itch typically clears up within a
few days to a week. In the meantime,
you can control itching with nonprescription anti-itch creams such as hydrocortisone. Nonprescription oral
antihistamines also may help. As much
as you’re tempted, don’t scratch too
much. An infection is possible if you
scratch the rash too harshly. If the itching is severe or lasts for more than three
days, see your doctor. A prescription
corticosteroid-type cream may be helpful — or you could have a rash from
another cause such as poison ivy. ❒
Have a question or comment?
We appreciate every letter sent to Second
Opinion but cannot publish an answer to each
question or respond to requests for consultation
on individual medical conditions. Editorial
comments can be directed to:
Managing Editor, Mayo Clinic Health Letter,
200 First St. SW, Rochester, MN 55905, or
send email to HealthLetter@Mayo.edu
For information about Mayo Clinic services,
you may telephone any of our three facilities:
Rochester, Minn., 507-284-2511;
Jacksonville, Fla., 904-953-2000;
Scottsdale, Ariz., 480-301-8000 or visit
www.MayoClinic.org
Check out Mayo Clinic’s consumer health
website, at www.MayoClinic.com
Copyright
Mailing lists
Customer Services
Purpose
Correspondence
© 2012 Mayo Foundation for Medical
Education and Research. All rights reserved.
We make our Mayo Clinic Health
Letter mailing list available to carefully selected companies and organizations. If you do not wish to receive
such mailings, please write us at the
address shown at right and enclose
your mailing label.
For subscription information from locations within United States and Canada,
call Customer Services at: 866-516-4974.
From other countries call: 903-636-9029.
Subscription prices in United States:
$29.55; in Canada: $45; all other countries:
$55 (U.S.). Single copies are available for
$4 plus shipping, handling and taxes.
To help our subscribers achieve healthier lives by providing useful, reliable,
easy-to-understand health information
that’s timely and of broad interest.
Send subscription inquiries to:
Mayo Clinic Health Letter
Subscription Services
P.O. Box 9302
Big Sandy, TX 75755-9302
MAYO, MAYO CLINIC, the triple-shield Mayo
logo, and TOOLS FOR HEALTHIER LIVES
are marks of Mayo Foundation for Medi­cal
Education and Research.
8
www.HealthLetter.MayoClinic.com
July 2012
Mayo Clinic Health Letter supplements
the advice of your personal physician,
whom you should consult for personal
health problems.
MC2019-0712
100712
Printed in the USA