ch 5 - material
advertisement

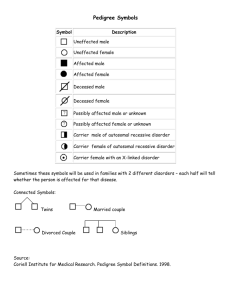
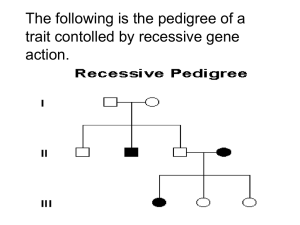
Human Inheritance Patterns Remember…the autosomes are all of the chromosomes except for the sex chromosomes. You have 22 pairs of autosomes – 44 total. Your two sex chromosomes (XX or XY) bring the final total to 46. • AUTOSOMAL RECESSIVE DISORDERS: Examples include cystic fibrosis (CF), phenylketonuria (PKU), sickle cell disease (SCD), xeroderma pigmentosum (XP), Tay-Sachs disease, hereditary hemochromatosis (HH), galactosemia, congenital fructose intolerance, lactose intolerance, etc. genotype: phenotype: AA unaffected Aa unaffected carrier aa affected In autosomal recessive inheritance, a person must receive 2 copies (aa) of the mutant defective gene in order to be affected. People who receive only 1 copy (Aa) of the defective allele are unaffected, but carry the defective gene and can pass it on to their children – they are called unaffected carriers (or simply carriers.) They are unaffected because the normal allele (A) codes for enough “good” protein to allow survival. People who have 2 normal alleles (AA) are unaffected, of course. Autosomal recessive disorders often, but not always, involve enzymes. Enzymes are special proteins that catalyze specific chemical reactions in your body. If a person has two defective genes (aa) that code for a specific enzyme, then he/she cannot produce that particular enzyme. As a result, some specific chemical reaction in the body will not take place – that person is then affected with a certain disorder. • AUTOSOMAL DOMINANT DISORDERS: Examples include Marfan syndrome, neurofibromatosis (NF), Huntington disease (HD), achondroplasia, tuberous sclerosis, familial hypercholesterolemia (FH), Osler-Weber-Rendu syndrome, etc. genotype: phenotype: AA affected Aa affected aa unaffected In autosomal dominant inheritance, a person only has to receive 1 copy (Aa) of the mutant defective gene in order to be affected. Of course, people who receive 2 copies (AA) of the defective allele also affected – sometimes more severely than those who are heterozygous (Aa). [For example, all achondroplastic dwarfs who survive through infancy are Aa … but AA babies typically die before birth, or shortly after birth.] People who are unaffected are aa. They have two “normal” alleles that code for some specific protein. Autosomal dominant disorders often, but not always, code for proteins other than enzymes – such as structural proteins, protein receptors, regulatory proteins, etc. Having just one defective gene (A) causes the production of enough “bad” protein to cause damage to cells/tissues/organs. So even a heterozygous person (Aa) is affected with a certain disorder. Constructing Pedigrees Directions ~ Draw pedigrees and list all possible genotypes for the following problems. Answer any questions that may follow. 1. You are a genetic counselor. The proposita has an autosomal recessive disorder and seeks your advice before starting a family. Based on the following information, construct a 3-generation pedigree for your client: (1) (2) (3) (4) The maternal grandfather of the proposita has the disorder; his wife does not. The mother of the proposita is unaffected and is the youngest of five children, the three oldest of which are males and the youngest of which are females. The father of the proposita is unaffected. The proposita has an affected older sister, but her youngest siblings are unaffected twins – a boy and a girl born in that order. All individuals who have the disorder have been identified in the statements above. 2. A propositus has an autosomal recessive disorder and seeks your advice. Based upon the data below, construct a 3-generation pedigree for your client: (1) (2) (3) (4) (5) The propositus is the only child of a consanguineous (brother/sister) mating. The mother of the propositus is the older sister of a girl who is affected with the disorder. The mother of the propositus is younger than her brother. The affected sister of the mother of the propositus is married to an unaffected man. They have had one affected daughter, one unaffected child of unknown sex, and a stillborn son, in that order. The phenotype of the stillborn baby is unknown. The grandparents of the propositus are unaffected. All individuals who have the disorder have been identified in the statements above. Cleft Lip Inheritance Sue and Tim were referred for genetic counseling after they inquired about the risk of having a child with a cleft lip. Tim was born with a mild cleft lip that was surgically repaired. He expressed concern that his future children could be at risk for a more severe form of clefting. Sue was in her twelfth week of pregnancy, and both were anxious about this pregnancy because Sue had a difficult time conceiving. The couple stated that they would not consider terminating the pregnancy for any reason but wanted to be prepared for the possibility of having a child with a birth defect. The genetic counselor took a three-generation family history from both Sue and Tim and found that Tim was the only person to have had a cleft lip. Sue’s family history showed no cases of cleft lip. Tim and Sue had several misconceptions about how clefting occurs, and the genetic counselor spent time explaining how cleft lips occur and some of the known causes of this birth defect. The following list summarizes the counselor’s discussion with this couple. • Fathers, as well as mothers, can pass on genes that cause clefting. • Some clefts are caused by environmental factors, meaning the condition didn’t come from the father or the mother. • One child in 33 is born with some sort of birth defect. One in 700 is born with a cleft-related birth defect. • Most clefts occur in boys; however, a girl can be born with a cleft. • If a person (male or female) is born with a cleft, the chances of that person having a child with a cleft, given no other obvious factor, is 7 in 100. • Some clefts are related to identifiable syndromes. Of those, some are autosomal dominant. A person with an autosomal dominant gene has a 50% probability of passing the gene to an offspring. • Clefting seems to be related to ethnicity, occurring most often among Asians, Latinos, and Native Americans (1:500); next most often among persons of European ethnicity (1:700); and least often among persons of African origin (1:1,000). • A cleft condition develops during the fourth to the eighth week of pregnancy. After that critical period, nothing the mother does can cause a cleft. Sometimes a cleft develops even before the mother is aware that she is pregnant. • Women who smoke are twice as likely to give birth to a child with a cleft. • Women who ingest large quantities of vitamin A or low quantities of folic acid are more likely to have children with a cleft. • In about 70% of cases, the fetal face is clearly visible using ultrasound. Facial disorders have been detected at the fifteenth gestational week of pregnancy. Ultrasound can be precise and reliable when diagnosing fetal craniofacial conditions. Question 1: After hearing this information, should Sue and Tim feel that their chances of having a child with a cleft lip are increased over that of the general population? Question 2: Can cleft lip be surgically corrected? Question 3: If the child showed a cleft lip through ultrasound analysis, and the parents then started blaming each other (because Sue is a smoker, and Tim was born with the defect), how would you counsel them? More Autosomal Recessive Pedigrees Directions ~ Draw pedigrees and list all possible genotypes for the following problems. Answer any questions that may follow. 1. You are a genetic counselor. Derek and Tami are parents of the proposita who has Tay Sachs disease, a fatal autosomal recessive disorder. Tami is pregnant with her 4th child. They seek your advice. Draw a pedigree based upon the following: (1) (2) (3) (4) (5) (6) (7) • • Derek and Tami, the parents of the proposita, are unaffected. The proposita had an older brother who died from Tay Sachs, and has a younger brother who is unaffected. Tami is pregnant for the 4th time. The sex of the fetus is unknown as of this time. Tami is the older sister of a boy who died from Tay Sachs. Her parents are unaffected. Derek is the youngest of three children. His oldest sibling, Amanda, is unaffected. Amanda’s husband is unaffected. Derek’s other sister, Jana, died from the disease at age two. Derek’s parents are both unaffected. Amanda and her husband currently have three children. Their oldest, Mark, is unaffected; their next child, Susan, has Tay Sachs. Amanda next had twins – a boy, Kevin, who is unaffected, and a girl, Kimi, who died from the disease. All individuals suffering from the disease have been revealed in the statements above. Draw the pedigree and place all possible genotypes under each individual. Draw a Punnett square for Derek and Tami to determine the odds that their next child will have Tay Sachs disease. Use 5-step format, please. 2. John and Hannah are the paternal grandparents of the proposita who has galactosemia, an autosomal recessive disorder. You offered genetic counseling to the family. Construct a pedigree based upon this information: (1) John and Hannah are unaffected and had five children. (2) Hannah’s firstborn was an unaffected daughter, Elizabeth. Her second child, a affected boy died at an early age. Her next child, a female with galactosemia, died at the age of ten. Hannah’s next baby, a boy whose phenotype was undetermined, was stillborn. Her youngest child, Eric, is unaffected. (3) Elizabeth’s husband is unaffected. The couple produced two children: a girl who died young and was affected with galactosemia, and a boy who is unaffected. (4) The father of the proposita is married to an unaffected woman. They have three children: the proposita, who is the eldest child and is affected, and MZ (monozygotic) twin boys, both of whom are unaffected. (5) All individuals suffering from the disorder are revealed in the statements above. • Draw the pedigree and place all possible genotypes under each individual. Mitochondrial Genes – Fact sheet Mitochondria in humans contain several copies of mini-chromosomes that carry about 37 genes. There is a high mutation rate in these 37 genes, because they lack DNA repair enzymes and the mitochondrion is the site of energy reactions that produce free radicals that cause damage to DNA. Mitochondria are maternally inherited, but cause sperm do not contain mitochondria. Human cells have many mitochondria that can contain different alleles for the same gene. Mitochondrial genes encode proteins that participate in protein synthesis and energy production. (24 of the genes encode RNA molecules that help assemble proteins and 13 genes encode proteins that function in cellular respiration) Heteroplasmy – because a cell has many mitochondria a mutation may be present in some mitochondria chromosomes and not others. This causes a wide variety of expressivity. Mitochondrial DNA is used as a forensic tool to link suspects to crimes and identify war dead. Kearns-Sayre Syndrome and Mitochondrial Disorders Florence is an active 44-year-old elementary school teacher who began experiencing severe headaches and nausea. She told her physician that her energy level had been dramatically reduced the last few months, and her arms and legs felt like they “weighed 100 pounds each,” particularly after she worked out in the gym. Her doctor performed a complete physical and noticed that she did have reduced strength in her arms and legs and that her left eyelid was droopier than her right eyelid. He referred her to an ophthalmologist who discovered that she had an unusual pigment accumulation on her retina, which had not yet affected her vision. She then visited a clinical geneticist who examined the mitochondria in her muscles. She was diagnosed with a mitochondrial genetic disorder known as Kearns-Sayre syndrome. Mitochondria are responsible for the conversion of food molecules into energy to meet the cell’s energy needs. In mitochondrial disorders, these biochemical processes are abnormal, and energy production is reduced. Muscle tends to be particularly affected because it requires a lot of energy, but other tissues such as the brain may also be involved. Under the microscope, the mitochondria in muscle from people with mitochondrial disorders look abnormal, and they often accumulate around the edges of muscle fibers. This gives a particular staining pattern, known as a “ragged red” appearance, and this is usually how mitochondrial disorders are diagnosed. Mitochondrial disorders affect people in many ways. The most common problem is a combination of mild muscle weakness in the arms and legs together with droopy eyelids and difficulty in moving the eyes. Some people do not have problems with their eye muscles, but have arm and leg weakness that gets worse after exertion. This weakness may be associated with nausea and headaches. Sometimes muscle weakness is obvious in small babies if the illness is severe, and they may have difficulties in feeding and swallowing. Other parts of the body may be involved, including the electrical conduction system of the heart. Most mitochondrial disorders are mildly disabling, particularly in people who have eye muscle weakness and limb weakness. The age at which the first symptoms develop is variable, ranging from early childhood to late adult life. About 20% of those with mitochondrial disorders have similarly affected relatives. Because only mothers transmit this disorder, it was suspected that some of these conditions are caused by a mutation in the genetic information carried by mitochondria. Mitochondria have their own genes, separate from the genes in the chromosomes of the nucleus. Only mothers pass mitochondria and their genes on to children, whereas the nuclear genes come from both parents. In about one-third of people with mitochondrial disorders, substantial chunks of the mitochondrial genes are deleted. Most of these individuals do not have affected relatives, and it seems likely that the deletions arise either during development of the egg or during very early development of the embryo. Deletions are particularly common in people with eye muscle weakness and the Kearns-Sayre syndrome. Question 1: Why would mitochondria have their own genomes? Question 2: How would mitochondria be passed from mother to offspring during egg formation? Why doesn’t the father pass on mitochondria to offspring? Pearson Syndrome A 34-year-old woman and her 1-month-old newborn were seen by a genetic counselor in the neonatal intensive care unit in a major medical center. The neonatologist was suspicious that the newborn boy had a genetic condition and requested a genetic evaluation. The newborn was very pale, was failing to thrive, had diarrhea, and had markedly increased serum cerebrospinal fluid lactate levels. In addition, he had severe muscle weakness with chart notes describing him as “floppy,” and he had already had two seizures since birth. The neonatologist reported that the infant was currently suffering from liver failure, which would probably result in his death in the next few days. The panel of tests performed on the infant led the neonatologist and genetic counselor to the diagnosis of Pearson syndrome. The combination of marked metabolic acidosis and abnormalities in bone marrow cells is highly suggestive of Pearson syndrome. Pearson syndrome is associated with a large deletion of the mitochondrial (mt) genome. The way the deletion containing mtDNA molecules are distributed during mitosis is not known. However, it is assumed that during cell division daughter cells randomly receive mitochondria carrying wild type (WT) or mutant mtDNA. Mitochondrial DNA is, theoretically, transmitted only to offspring through the mother via the large cytoplasmic component of the oocyte. Nearly all cases of Pearson syndrome arise from new mutational events. Mitochondria have extremely poor DNA repair mechanisms, and mutations accumulate very rapidly. Most infants with Pearson syndrome die before age 3, often due to infection or liver failure. A diagnosis of Pearson syndrome results in an extremely grave prognosis for the patient. Unfortunately, at this point, treatment can be directed only toward symptomatic relief. Question 1: Why doesn’t the mother have the disease if she has mutant mitochondrial DNA? Question 2: How would you react to hearing this diagnosis? How would you counsel a couple through this kind of situation? Question 3: How would a large deletion in the mitochondrial genome cause a disease? CF and Genetic Testing Todd and Shelly Z. were referred for genetic counseling because of advanced maternal age (Shelley was over 40 years old) in their current pregnancy. While obtaining the family history, the counselor learned that during their first pregnancy, the couple had elected to have an amniocentesis for prenatal diagnosis of cytogenetic abnormalities because Shelly was 36 years old at the time. During that pregnancy, Shelly and Todd reported that they were also concerned that Todd’s family history of cystic fibrosis (CF) increased their risk for having an affected child. Todd’s only sister had CF, and she had severe respiratory complications. The genetic counseling and testing was performed at an outside institution, and the couple had not brought copies of the report with them. They did state that they had completed studies to determine their CF carrier status and that Todd was found to be a CF carrier, but Shelly’s results were negative. The couple was no longer concerned about their risk of having a child with CF based on these results. To support their belief, they had a healthy 5-year-old son who had a negative sweat test at the age of 4 months. The counselor explained the need to review the records and scheduled a followup appointment. The test report from their first pregnancy only tested for the delta F508 mutation, the most common mutation in CF. The report confirmed that Shelly is not a carrier of this mutation and that Todd is. This report reduced Shelly’s risk status from 1 in 25 to about 1 in 300. More information has been learned about the different mutations in the CF gene since the last time they received genetic counseling. The counselor conveyed the information about recent advances in CF testing to the couple, and Shelly decided to have her blood drawn for CF mutational analysis with an expanded panel of mutations. Her results showed that she is a carrier for the W1282X CF mutation. The family was given a 25% risk for CF for each of their pregnancies based on their combined molecular test results. They proceeded with the amniocentesis because of the risks associated with advanced maternal age and requested fetal DNA analysis for CF mutations. The fetal analysis was positive for both parental mutations, indicating that the fetus had a greater than 99% chance of being affected with CF. Question 1: How is it that the fetus has a greater than 99% chance of being affected with CF if each parent carries a different mutation? Is the fetus homozygous or heterozygous for these mutations? Question 2: If this child has CF, what are the chances that any future child will have this disease? Does the fact they have a healthy 5-year-old son affect the chances of having future children with CF? Cystic Fibrosis Gene It is May1989 and the scene is a crowded research laboratory with beakers, flasks, and pipettes covering the lab bench. People and equipment take up every possible space. One researcher, Joe, passes a friend staring into a microscope. Another student wears gloves while she puts precisely measured portions of various liquids into tiny test tubes. Joe glances at the DNA sequence results he is carrying. Something is wrong. There it is, a unique type of genetic mutation in a DNA sequence. The genetic information required to make a complete protein is missing, as if one bead had fallen from a precious necklace. Instead of returning to his station, Joe rushes to tell his supervisor, Dr. Tsui (pronounced “Choy”), that he has found a specific mutation in a person with cystic fibrosis (CF), but he does not see this same mutation in a normal person’s genes. CF is a fatal disease that kills about 1 out of every 2,000 Caucasians (mostly children). Dr. Tsui examines the findings and is impressed but wants more evidence to prove that the result is real. He has had false hopes before, so he is not going to celebrate until they check this out carefully. Maybe the difference between the two gene sequences is just a normal variation among individuals. Five months later, Dr. Tsui and his team identify a “signature” pattern of DNA on either side of the mutation, and using that as a marker, they compare the genes of 100 normal people with the DNA sequence from 100 CF patients. By September1989, they are sure they have identified the CF gene. After several more years, Tsui and his team discover that the DNA sequence with the mutation encodes the information for a protein called CFTR (cystic fibrosis transmembrane conductance regulator), a part of the plasma membrane in cells that make mucus. This protein regulates a channel for chloride ions. Proteins are made of long chains of amino acids. The CFTR protein has 1,480 amino acids. Most children with CF are missing one single amino acid in their CFTR. Because of this, their mucus becomes too thick, causing all the other symptoms of CF. Thanks to Tsui’s research, scientists now have a much better idea of how the disease works. We can now easily predict when a couple is at risk for having a child with CF. With increasing understanding, scientists may also be able to devise improved treatments for children born with this disease. CF is the most common genetic disease among those of European ancestry. Children who have CF are born with it. Half of them will die before they are 25 and few make it past 30. It affects all parts of the body that secrete mucus: the lungs, stomach, nose, and mouth. The mucus of children with CF is so thick sometimes they cannot breathe. Why do 1 in 25 Caucasians carry the mutation for CF? Tsui and others think that people who carry it may also have resistance to diarrhea-like diseases. Question 1: Dr. Tsui’s research team discovered the gene for cystic fibrosis. What medical advances can be made after a gene is cloned? Question 2: Why do you think a change in one amino acid in the CF gene can cause such severe effects in CF patients? Relate your answer to the CFTR protein function and the cell membrane. Hardy-Weinberg and CF Jane, a healthy woman, was referred for genetic counseling because she had two siblings, a brother Matt and a sister Edna, with cystic fibrosis who died at the ages of 32 and 16, respectively. Jane’s husband, John, has no family history of cystic fibrosis. Jane wants to know the probability that she and John will have a child with cystic fibrosis. The genetic counselor used the Hardy-Weinberg model to calculate the probability that this couple will have an affected child. The counselor explained that there is a two-in-three chance that Jane is a carrier for the mutant CFTR allele. She used a Punnett square to illustrate this. The probability that John is a carrier is equal to the population carrier frequency (2pq). The probability that John and Jane will have a child who has cystic fibrosis equals the probability that Jane is a carrier (2/3) multiplied by the probability that John is a carrier (2pq) multiplied by the probability that they will have an affected child if they are both carriers (1/4). Question 1: Using the heterozygote frequency for cystic fibrosis among white Americans to estimate the probability that John is a carrier, what is the likelihood that their child would have the disease? Question 2: If you were their genetic counselor, would you recommend that Jane and John be genetically tested before they attempt to have any children? Question 3: It is now possible to use preimplantation testing, which involves in vitro fertilization plus genetic testing of the embryo before implantation, to ensure that a heterozygous couple has a child free of cystic fibrosis. Do you see any ethical problems or potential future dangers associated with this technology? Notes: Autosomal Dominant Inheritance Remember: The following genotypes and phenotypes apply in autosomal dominant inheritance: AA = affected Aa = affected aa = unaffected Please notice there are no carriers in this inheritance pattern. Sometimes (depending on the disorder) the AA genotype is more seriously affected than is the Aa genotype. An example is the AA genotype for achondroplasia. Called “double-dominant dwarfs,” these fetuses typically die before birth – or shortly after birth. So all achondroplastic dwarfs in the general population are Aa heterozygotes. You need to know the following additional vocabulary terms for autosomal dominance… 1. VARIABLE EXPRESSIVITY = when the symptoms of a disorder vary (differ) in intensity in different affected people. For example, some people with NF – neurofibromatosis – have very mild symptoms, while others with NF have more severe symptoms. 2. PENETRANCE = when a person inherits a disorder-causing dominant allele and displays (expresses) its symptoms. 3. LACK OF PENETRANCE (INCOMPLETE PENETRANCE) = when a person inherits a disordercausing dominant allele, yet does not display its symptoms. A person could be Aa for NF and not show a single symptom of the disorder! He may never even know he has the mutant gene and could pass it on to his offspring – and those children could express the disorder. 4. PERCENT PENETRANCE = is calculated mathematically. For example, if 85 out of 100 people who inherited a dominant gene (and are Aa) actually express symptoms, but 15 of them do not express symptoms, then the allele is said to be “85% penetrant.” You could also say the gene shows “85% penetrance.” 5. FRESH (SPONTANEOUS) MUTATION = is fairly common in many human autosomal dominant disorders. A fresh mutation can occur in an egg, a sperm cell, or in the zygote. It is estimated that 85% of all cases of achondroplasia are the result of fresh mutations. 6. DELAYED ONSET = when a person inherits a dominant allele, but does not begin to express the symptoms of the disorder until later in life. For example, in Huntington disease, symptoms do not typically arise until persons are in their 30s or 40s. 7. PLEIOTROPY = is pronounced (PLY – uh – tropee). This is when a certain mutant allele codes for a protein that affects different parts of the body. For example, in Marfan syndrome, a mutant allele codes for a defective type of protein called fibrillin, an elastic connective tissue found in many places in the body. Defective fibrillin causes multiple symptoms – it has pleiotropic effects – such as eye lens dislocation, spindly fingers, chest abnormalities, and weakened aorta. The Marfan gene is pleiotropic. An Autosomal Dominant Pedigree Directions: Read the following bits of information, and then construct a 3-generation pedigree. List all possible genotypes under each of the symbols in the pedigree. Kristi (proposita), a 15-year-old high school sophomore, has a severe case of neurofibromatosis (NF). She has two brothers, one older and the other younger than she, both of whom are unaffected. Kristi’s father has no disfiguring tumors, but he does have eight, large, brown, café-au-lait spots on his stomach, back, and right leg – this means he is mildly affected. Kristi’s mother, and Kristi’s maternal and paternal grandparents are unaffected. • Construct a 3-generation pedigree, listing all possible genotypes under each symbol, using the space below. • Using a Punnett square, with 5-step format, show how it was possible for Kristi’s parents to produce a child with NF. ♀ x ♂ genotypes: phenotypes: • Explain how it is possible that Kristi’s unaffected paternal grandparents produced a son with NF? [Be as specific as possible, please.] Dominant Hereditary Ataxia Pedigree Important Information: Carly, the proposita, has a rare autosomal dominant disorder called dominant hereditary ataxia, a delayed-onset, degenerative neurological disorder. It is fatal. The gene has 100% penetrance. Here is some pertinent information concerning her family: (1) Carly is 30 years old. She has a 32-year-old, unaffected sister, and an affected 29-yearold sister. Carly’s mother, Andrea, is unaffected. Carly’s father, Adam, had no apparent symptoms of the disorder. He died when trampled in a buffalo stampede while on a hunting expedition in Montana nearly twenty years ago. Adam was only 33 years old at the time of his death. (2) Adam was the eldest son of Richard and Helen. Richard died of ataxia. Helen was unaffected. Richard and Helen had a middle child, Jacob, who died of the disorder. Jacob’s younger sister, Beth, is affected. (3) Jacob had married an unaffected woman. They produced two children, a 30-year-old, affected son and a 29-year-old, unaffected daughter. A third pregnancy resulted in a stillborn baby boy. (4) Beth married an unaffected man. She now has a 33-year-old, affected son, in addition to 32-year-old, unaffected, monozygotic (MZ or identical) twin sons, and a 27-year-old daughter who was recently diagnosed with the disorder. (5) Richard’s father was affected; his mother was not. Helen’s parents were unaffected. Helen died while running with the bulls in Pampalona, Spain. Both pairs of Carly’s paternal great-grandparents are deceased. • Construct a 4-generation pedigree, listing all possible genotypes under each symbol, using another piece of paper. • How could Adam and Andrea have affected children? Please give two possibilities. Then tell which of the two is the more probable of the two. • Imagine for a moment that you are the child of a father who has died of ataxia. Your mother is alive, well, and unaffected by the disorder. You are about to receive a phone call from a research team at UCSD. They are going to ask you whether or not you would be willing to participate in a scientific study to help determine the function of the ataxia gene. But first, they need a blood sample. They will test your white blood cells' DNA to determine if you have the dominant gene. You have been promised that the results will be kept strictly confidential - even you don't have to know the results...unless you wish. Would you take the gene test to aid the researchers? Would you want to know your test results? Why or why not? Achondroplasia A couple was referred for genetic counseling because they wanted to know the chances of having a child with dwarfism. Both the man and woman had achondroplasia, the most common form of short-limbed dwarfism. The couple knew that this condition is inherited as an autosomal dominant trait, but they were unsure what kind of physical manifestations a child would have if it inherited both genes for the condition. They were each heterozygous for the FGFR3 gene that causes achondroplasia, and they wanted information on the chances of having a child homozygous for the FGFR3 gene. The counselor briefly reviewed the phenotypic features of individuals who have achondroplasia. These include the facial features (large head with prominent forehead; small, flat nasal bridge; and prominent jaw), very short stature, and shortening of the arms and legs. Physical examination and skeletal x-ray films are used to diagnosis this condition. Final adult height is approximately 4 feet. Because achondroplasia is an autosomal dominant condition, a person with this condition has a 1 in 2, or 50%, chance of having children with this condition. However, approximately 75% of individuals with achondroplasia are born to parents of average size. In these cases, achondroplasia is due to a new mutation. This couple is at risk for having a child with two copies of the changed gene or double homozygosity. Infants with homozygous achondroplasia are either stillborn or die shortly after birth. The counselor recommended prenatal diagnosis via serial ultrasounds. In addition, a DNA test is available to detect the homozygous condition prenatally. Achondroplasia occurs in 1 in every 14,000 births. Question 1: What is the chance this couple will have a child with two copies of the dominant mutant gene? What is the chance that the child will have normal height? Question 2: Should the parents be concerned about the heterozygous condition as well as the homozygous mutant condition? Question 3: Why would the achrondroplasia gene be more susceptible to mutation than other genes?