Clinical Evaluation of Coma and Brain Death
advertisement

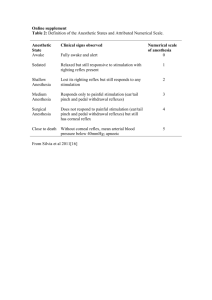
© 2013 Neurocritical Care Society Practice Update Clinical Evaluation of Coma and Brain Death David M. Greer MD, MA, FCCM, FAHA Yale University School of Medicine New Haven, CT CLINICAL CASE A 62-year-old man with hypertension, diabetes, hyperlipidemia and a prior TIA suffers a cardiac arrest. His initial rhythm is ventricular tachycardia, and he is resuscitated with return of spontaneous circulation (ROSC) after 25 minutes. He remains comatose, and undergoes therapeutic hypothermia (TH) with a temperature maintained between 32-34°C for 24 hours. He is subsequently rewarmed to normothermia over a 12-hour period. His neurological examination off all sedation after complete rewarming is notable for coma, with no eye opening to noxious stimulation. He has reactive pupillary, corneal and oculocephalic reflexes. He has extensor posturing to noxious stimuli. He has intermittent myoclonic jerking of the face, eyes and upper extremities. You are asked to evaluate the patient and guide the team through the clinical evaluation, and to consider brain death testing. OVERVIEW Coma and brain death are conditions neurointensivists are commonly called upon to evaluate, and the examination can be intimidating and challenging. Proper evaluation requires an understanding of the etiology and pathogenesis of the condition, and examination of the patient under optimal circumstances. Numerous pitfalls exist in the clinical examination, of which the examiner needs to be aware. The brain death examination can be viewed as the coma examination extended: not only must the patient be comatose, but also all brainstem functions must be absent, including respiratory drive as measured through apnea testing. Herein we will review the specifics of coma and brain death clinical evaluations. DEFINITION Coma is strictly defined as a state of complete unresponsiveness, from which a patient cannot be aroused. (1) Eyes are typically closed, with a notable exception being rare patients postcardiac arrest with “eyes open coma” but who are otherwise completely unresponsive, and who do not close their eyes in response to external stimulation. Cranial nerves and brainstem reflexes may be partially or fully intact, but there can be no purposeful responses to stimulation on the cranium or body. There can be no eye opening to vigorous auditory or tactile stimulation, no grimacing, no blink to visual threat, and no movement of the extremities or trunk reflective of purposeful responsiveness; reflexive or posturing movements are permissible in coma, as they are represent brainstem or spinally-mediated responses and not a conscious or purposeful response. © 2013 Neurocritical Care Society Practice Update EPIDEMIOLOGY/PATHOPHYSIOLOGY Coma can occur due to traumatic or non-traumatic causes. The true incidence of coma is difficult to estimate, as many studies do not stay true to the standard definition above. The most common causes of traumatic coma are motor vehicle accidents, physical abuse and falls. Non-traumatic causes include toxic-metabolic insults, global hypoxia/ischemia, ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage, brain tumors, CNS infections (meningitis, encephalitis, abscess), inflammatory conditions and psychogenic coma. Comatose patients are at high risk for morbidity and mortality; a rapid and systematic diagnostic work up to evaluate and potentially treat the underlying etiology is paramount. The ascending reticular activating system (ARAS) begins in the lower brainstem as an ill-defined group of nuclei and neurons that extends through the rostral brainstem, projecting into both cerebral hemispheres. Thus, in order to cause coma, a process must either affect the brainstem primarily or both cerebral hemispheres concomitantly. Processes that affect both cerebral hemispheres and cause coma are typically diffuse metabolic or toxic processes, such as drug intoxication or severe electrolyte/metabolite abnormalities; other causes of diffuse hemispheric dysfunction include meningoencephalitis, hydrocephalus, multifocal cerebral insults (e.g. multiple large concomitant cerebral emboli) or cardiac or respiratory arrest. A unilateral hemispheric process does not commonly cause coma in the acute setting, unless it is associated with mass effect and compression of the brainstem; coma due to brainstem compression from an ischemic stroke typically occurs during the time of peak edema, around 35 days after the ictus. Processes that primarily affect the brainstem are most commonly structural, such as infarction or hemorrhage. Findings on the coma examination are crucial in determining prognosis. For example, a unilateral dilating pupil, with or without outward/downward deviation of the eye, is indicative of compression of the IIIrd nerve due to an expanding hemispheric mass lesion, and portends a poor prognosis if not promptly treated. Classically, comatose patients following a cardiac arrest will have a poor prognosis if they have absent pupillary and corneal reflexes, as well as a motor response of extensor posturing or worse. (2,3) However, more recent studies have drawn into question the validity of the motor response, especially in the setting of therapeutic hypothermia. (4-5) CLINICAL FEATURES/DIAGNOSIS The coma exam is straightforward and systematic, and can be separated into broad assessment steps: 1) consciousness, 2) cranial nerves, and 3) brainstem function. Although the examination can be intimidating to inexperienced clinicians, remember these primary principles: ensure a comfortable examination position for yourself, provide strong enough stimuli, and repeat aspects of the testing in which you are uncertain of the response. Minimize potential negative © 2013 Neurocritical Care Society Practice Update influences to the examination, most notably including sedation or metabolic abnormalities, whenever possible. When uncertain how to describe a movement or response, rather than trying to force terms like “extensor” or “flexor” or “dyskinetic,” simply describe the response using plain language and as many words as are necessary to convey your thoughts. Taking video of abnormal movements can often be helpful, taking care not to include any identifiable information, or gaining written permission from the family/surrogate decision-maker. The examination begins upon entry to the room, with direct observation of the patient the resting state. Most patients are ventilated, and careful attention to the respiratory pattern can give clues to brainstem function. Respiratory Patterns: non-volitional respiratory function is mediated primarily through the caudal brainstem and upper cervical spinal cord. Thus, dysfunction at different anatomical levels can cause specific respiratory patterns. However, there are often multiple forces at play, including not just anatomic but also metabolic influences, commonly clouding the picture. Figure 1 provides a visual depiction of the descriptions below. Cheyne-Stokes Respiration (CSR) – this pattern manifests as oscillation between periods of hyperventilation and relative apnea. Although common, it is a relatively nonspecific pattern, and can be seen in both cerebral and systemic (e.g. CHF, hypoxia) conditions. If patients cannot voluntarily breathe during the apneic phase or slow down the breathing during the tachypneic phase, the cause of CSR is most likely of cerebral origin. Centrallymediated CSR is most commonly secondary to bilateral hemispheric dysfunction, sometimes extending to the diencephalon. Central Hyperventilation – this manifests as regular, rapid and deep breaths, often resulting in significant hypocapnea and alkalosis. Lesions are typically in the rostral brainstem in the upper pons/lower midbrain region. Central hyperventilation can rarely be seen in noncomatose patients with infiltrative tumors of this region. Apneustic Respiration – clinically this appears as pauses of up to 2-3 seconds at endinspiration and sometimes end-expiration. It localizes to the mid- to caudal pontine region, most commonly caused by basilar artery occlusion. Ataxic Respiration - this is an irregular and unpredictable pattern of respiration, with both deep and shallow breaths. It is a most ominous sign, commonly seen with medullary lesions as a late manifestation of herniation, and precedes complete apnea. Assessment of Coma: The most common mistakes made by clinicians attempting to assess a comatose patient are 1) not adequately observing, and 2) not providing enough of a stimulus. Some general principles: Uncover the patient’s extremities (maintaining decency at all times). Failure to uncover the arms and legs during the examination may preclude the ability to see some responsiveness to stimulation. Observations also should be made for spontaneous movements, including rhythmic movements that may be reflective of seizures, jerking movements that may reflect myoclonus, or dyskinetic movements. © 2013 Neurocritical Care Society Practice Update Use sufficient stimulation to try to assess consciousness. Start with auditory stimulation, yelling the patients name and telling them to open their eyes. Assume that the patient is deaf (especially if they are older or have previously received ototoxic drugs) until proven otherwise. Note that the command “open your eyes” may not be followed if the patient has an eye opening apraxia, and thus other commands should also be used, such as “stick out your tongue” and “wiggle your thumb” and “wiggle your toes.” If the patient does not respond to maximal auditory stimulation, tactile stimulation should be used. In a patient without a question of C-spine integrity, a vigorous shake from side-to-side can be a very potent stimulus to awaken patients (a technique passed down by Dr. C. Miller Fisher). Pressure should be applied to the supra-orbital ridge and temporo-mandibular joint, as quadriplegic patients may not respond to noxious stimulation below the cranium. A vigorous sternal rub can also be used, as well as deep nail bed pressure in the extremities. More proximal noxious stimulation may be used, and may be helpful when the nail bed pressure response is ambiguous. However, care must be taken to use this sparingly, as it can cause bruising and/or skin tears. Upper Cranial Nerves The eye examination is most informative, and can be broken down into several parts. With the eyes held open (or, if already open in situations of “eyes open coma”), a blink to visual threat should be tested. Starting in the peripheral visual fields, a flat hand should be used to slowly approach the patient’s eye, one at a time, taking care not to create a wind current (and thus unintentionally stimulate a corneal reflex). If there is no response to an approach from the periphery, a central approach should then be used. Each eye should be tested separately. The blink to visual threat should be tested prior to testing pupillary responses. Also with they eyes held open, the position of the eyes, spontaneous eye movements, and the presence of conjugance or dysconjugance should be noted. A flashlight shined directly 1-2 feet from the face should shine approximately equally in both pupils and allow better observation of spontaneous movements or dysconjugance. Horizontal dysconjugance is not uncommon in the setting of a depressed level of consciousness, and does not always reflect cranial nerve and/or brainstem dysfunction. Care should be taken to note the presence of a internuclear ophthalmoplegia, reflective of injury to the medial longitudinal fasciculus. Vertical dysconjugance, or a “skew” deviation, is nearly always pathological, however, and reflects dysfunction of the upper brainstem and/or IIIrd or IVth cranial nerves. With a IIIrd nerve palsy due to a compressive lesion (e.g. herniation syndrome), the affected eye is deviated laterally and inferiorly, and the pupil is dilated and unreactive. A nuclear IIIrd nerve palsy will not occur in isolation, and when due to a midline structural lesion will cause bilateral ptosis and upgaze pareses. Spontaneous eye movements toward one side may reflect damage to the frontal eye fields or paramedian pontine reticular formation (PPRF), or can be reflective of seizure activity. Upward or downward beating eye movements is often reflective of lower brainstem dysfunction. Retraction nystagmus involves spontaneous contraction of all extraocular muscles, and is seen with midbrain tegmental lesions. Roving eye © 2013 Neurocritical Care Society Practice Update movements are reflective of an intact brainstem to some extent, and cannot be produced voluntarily, thus ruling out psychogenic coma. “Ping-Pong” eye movements are repetitive horizontal movements of the eyes, with pauses of several seconds in the lateral positions, and is a variant of roving eye movements, sometimes seen with structural lesions of the cerebellar vermis. Ocular bobbing is a brief, rapid downward jerk of the eyes with a slower return to the midposition, classically localizing to the ponto-medullary junction. Eye movements may be tested with the oculocephalic reflex (“Dolls Eyes”, OCR) maneuver and oculovestibular reflex (“cold caloric”, OVR) testing. The OCR should only be tested when there is no question of C-spine integrity. The head is rapidly rotated horizontally, with a pause at the farthest most point. In an intact brainstem, they eyes should move conjugately in the opposite direction from which the head is turned, with a slow compensatory response toward the midline. Vertical eye movements should also be tested, with the same principle (eyes moving in the opposite direction of head movement). Extreme care must be taken in intubated patients to avoid accidentally extubating the patient or disconnecting the ventilator tubing. The OVR is tested with the following steps. First, the external auditory canal is examined and cleared of any cerumen/debris, and the integrity of the tympanic membrane is ensured. Second, the head is positioned at 30° ensure the proper orientation of the semicircular canals. Ice water is then instilled into one ear at a time for 60 seconds, and the eyes observed for movement. With an intact brainstem, the eyes will tonically deviate toward the coldirrigated ear, sometimes accompanied by nystagmus with a fast component in the opposite direction. Vertical eye movements can be tested with instillation into both ears at the same time (causing conjugate downward eye movement), but this is rarely performed. The pupillary light reflex is tested with a bright light shown into one eye at a time. Note should be made of the direct and consensual response. A magnifying glass should be used if the pupils are small, or if there is a question of any response, such as in brain death testing (see below). Automated “pupillometers” are commercially available, but have not been rigorously compared with the bedside magnifying glass examination, and are quite expensive. An important clinical pearl is that toxic-metabolic disorders should not cause pupillary abnormalities (notable exceptions are hypothermia and high-dose barbiturates); thus, when pupillary dysfunction is present it is most likely due to a structural cause. A funduscopic examination should be performed in all patients – it is the one opportunity to look directly at nerves and vessels, and gives evidence of intracranial pressure phenomena. The presence of spontaneous venous pulsations essentially rules out the possibility of raised ICP. A unilateral miotic pupil is often reflective of loss of sympathetic innervation, such as with a Horner syndrome. Horner syndrome is often seen as a constellation also involving ipsilateral ptosis and sometimes anhydrosis, depending on the location of the lesion. Horner syndrome can be seen with lesions in the hypothalamus or lateral medulla. Damage to the midbrain may affect the IIIrd nerve and cause pupillary abnormalities. Lesions in this location often cause midposition pupils that are 4-6 mm, nonreactive to light. However, hippus may be present, and the ciliospinal reflex may be preserved. The © 2013 Neurocritical Care Society Practice Update ciliospinal reflex is ipsilateral pupillary dilation in with neck, face or upper trunk noxious stimulation, only present with an intact sympathetic pathway. Pontine pupils are small (often described as “pinpoint”), and reflect loss of sympathetic input. Lower Cranial Nerves Facial movement and sensation are tested via various techniques. Painful stimuli should be applied to the cranium to look for responsiveness, either as a facial grimace or with movement elsewhere in the body. A “nasal tickle” is performed by inserting a Q-tip into one nares at a time and shaking/twisting lightly. A corneal reflex is typically tested with brief instillation of sterile saline or water, but this may be an insufficient stimulus in some patients, and thus a more vigorous stimulus may be necessary. A cotton wisp may be applied to the cornea, or for even more vigorous stimulation, a Q-tip may be pressed to the cornea adjacent to the iris (usually reserved for brain death testing, see below). Hearing and vestibular testing is performed as above (auditory stimulation, OCR and OVR testing). Palatal movement is tested with stimulation to the posterior pharynx and looking for a gag reflex or palatal movement. This may be challenging in intubated patients, and light tugging on the endotracheal tube may be sufficient stimulation (taking care not to extubate the patient or push the tube into a main stem bronchus). If able, a tongue depressor, suction catheter or Q-tip can be pressed against the soft palate as well to try to elicit a response. A cough reflex is tested by deep bronchial suctioning. Motor and Sensory Examination Comatose patients require noxious stimulation to assess both sensory and motor responses. Tone should be checked first, performed as passive and unpredictable movement at multiple joints in the same limb simultaneously. Note should be made of increased or decreased tone, or of dyskinetic movements. Muscle bulk should also be noted, and any fasciculations or jerking movements. Pain is typically applied first to the nail beds, as this is least likely to cause injury. However, based on the response, further stimulation in other places may be necessary. Monitoring for facial (grimace) and head movements is necessary to ensure that there is not a corticospinal tract lesion that prevents a motor response but with a clear signal that the patient feels the stimulus. In general, one of three motor responses can be expected: purposeful, pathological, or none. Purposeful responses include localization or movement away from the stimulus and nonstereotyped withdrawal of the limb. Discerning whether a withdrawal response is pathological or not often requires stimulation in multiple places on the limb; a pathological response is stereotyped, nearly identical with noxious stimulation in multiple locations. Pathological responses include extensor and flexor posturing. The terms “decerebrate” and “decorticate” posturing, respectively, have been used synonymously with these © 2013 Neurocritical Care Society Practice Update movements, but these are often inaccurate and misleading. Although animal models have suggested that extensor posturing in the upper extremities reflects lesions at the level of the red nucleus in the midbrain, an anatomical correlation has not been demonstrated in humans. Nonetheless, these signs are often seen as part of a continuum, with extensor movements considered more ominous (and reflective of more extensive brainstem dysfunction) than flexor. Extensor posturing in the upper extremities manifests as extension at the elbow and hyperpronation, with internal rotation at the shoulders. In the legs, extension occurs at the knee, with internal rotation at the hip and plantar flexion at the foot. Flexor posturing in the upper extremities appears as flexion of the elbow, wrist and fingers with adduction at the shoulders. The lower extremities may display “triple flexion” as a pathological response, with flexion at the hip, knee and ankle. Distinguishing triple flexion from purposeful withdrawal can be challenging, and mandates providing noxious stimulation at multiple locations in the lower extremity. A good rule of thumb is that a purposeful response will manifest as movement away from a noxious stimulation; thus, in a patient with triple flexion vs. purposeful withdrawal with nail bed pressure at the toe, painful stimulation at the medial thigh should produce abduction of the leg at the hip. It should be kept in mind that movements are not always easily categorized as flexion or extension; when in doubt simply provide a detailed description of the movement, so that others can see how the movements appear in comparison. Flaccid/absent motor responses may be reflective of injury anywhere along the neuroaxis, and may even reflect severe peripheral nervous system dysfunction (e.g. fulminant Guillian Barré Syndrome). Reflexes Deep tendon reflexes may always be checked, and are graded on a 0-4 scale: 0=absent, 1=hypoactive, 2=normal, 3=hyperactive without clonus, and 4=hyperactive with clonus. Deep tendon reflexes rating 3 or 4 are consistent with an upper motor neuron process. Note that a jaw jerk reflex can be tested as well, and may be helpful in distinguishing cervical spine lesions from processes causing generalized hyporeflexia. Pathological reflexes include the Babinski sign: the lateral aspect of the plantar aspect of the foot is slowly and steadily stroked in one long motion from the heel to the ball of the foot, and then medially across the ball of the foot. A pathological reflex (or “present” Babinski sign) involves two components: the great toe extends as the smaller toes fan out in abduction. A nonpathological response consists of plantar flexion of the great toe and a curling in adduction of the smaller toes. A Hoffman sign is produced by flicking the distal end of the middle or ring finger and observing ipsilateral flexion of the thumb. It is not necessarily a pathological sign, as it is often seen in patients who are normal and nonpathologically hyperreflexic. © 2013 Neurocritical Care Society Practice Update BRAIN DEATH Brain death is defined as the complete and irreversible loss of all brain function, including the brain stem. The American Academy of Neurology Practice Parameters for brain death determination were updated in 2010. (6) There are 3 cardinal components: coma, brain stem areflexia and apnea. The physical examination includes the techniques described above for the coma examination, but with specific mandatory findings, which will be described below. The evaluation can be broken down into 4 discrete steps: satisfying prerequisites, the clinical examination (including apnea testing), ancillary testing (if necessary) and documentation. A discussion of ancillary testing is beyond the focus of this chapter, and what ensues is a detailed explanation of the clinical evaluation. Prerequisites The cause of the neurological state must be known, and must be known to be irreversible. This is the “do not pass go” point of the evaluation – if there is any doubt about the diagnosis or reversibility, specific brain death testing should not be undertaken. The cause is typically gleaned through the history and neuroimaging. Occasionally, laboratory testing (such as CSF examination in fulminant bacterial endocarditis) may be used. Drug effect must be excluded. If it is unknown whether the patient has received potential CNS-acting drugs, a toxicology screen must be performed. If medications have been used to treat the patient (e.g. narcotics, benzodiazepines or barbiturates), clearance must be determined by calculating 5 times the drug’s half-life, assuming normal hepatic and renal function. It should be kept in mind that hypothermia (including therapeutic hypothermia as used in ICP crisis and cardiac arrest) will delay drug metabolism and neuronal recovery. If a patient has received neuromuscular blocking agents, their continued presence must be excluded by implementation of electrical nerve stimulation. Severe electrolyte, acid-base, or endocrine abnormalities and hyperammonemia must be excluded. Normothermia must be achieved, defined as a core temperature > 36°C. Sufficient blood pressure must be established, with a lowest systolic limit of 100 mm Hg. Clinical Examination Coma – as defined above, with no purposeful response to any and all noxious stimulation. Only spinally-mediated responses are permissible. Pupillary reflexes must be absent. A bright light (and optimally a magnifying glass) should be used. Pupils should be 4-9 mm and are typically midposition. Smaller pupils should suggest the possibility of a medication effect (e.g. narcotics). © 2013 Neurocritical Care Society Practice Update Ocular movements should be completely absent with OCR and OVR testing. With coldcaloric testing, both ears must be tested separately, with an interval of at least 5 minutes between ears. Absent corneal reflex (with maximal stimulation, as above). Absent facial movement to noxious stimulation in the body and cranium. Facial myokymias may be observed, but should be spontaneous and not in response to stimulation. Cough and gag reflexes must be absent with palatal stimulation and deep bronchial suctioning, respectively. Movement in the trunk and extremities must be absent, other than spinally-mediated; these include deep tendon reflexes, Babinski sign, triple flexion and a constellation of features called “Lazarus signs.” Distinguishing these movements as spinally-mediated requires expertise, and sometimes ancillary testing when in doubt. Extensor or flexor posturing in the upper extremities is reflective of a brain stem mediated response, and is not permissible in brain death. Apnea Testing Establish euvolemia – patients with brain death often have diabetes insipidus, and a negative fluid balance will make the patient more prone to hypotension during apnea testing, which may require that the test be aborted. Establish eucapnea – the goal pCO2 should be 35-45 mm Hg. In known CO2 retainers, establish the patient’s baseline pCO2, if known. Pre-oxygenate the patient for at least 10 minutes with 100% FiO2 to achieve a PO2 > 200 mm Hg. At no point during apnea testing should the patient become hypoxic, as this may lead to hemodynamic compromise and even cardiac arrest. Reduce the PEEP to 5 cm H20. If this results in significant oxygen desaturation, it is an indication that the patient may be unlikely to complete apnea testing. Disconnect the patient from the ventilator, providing a constant source of oxygen via a catheter to the level of the carina. Closely observe the patient for respiratory movements of the chest and abdomen, which should be uncovered. An optimal place for the clinician to stand is at the foot of the bed, where they can observe both the chest and abdomen of the patient as well as the monitor, watching for hypotension, arrhythmias or desaturation. Abort the test if the patient becomes hypotensive, defined as an SBP <90 mm Hg, despite the use of vasopressors and or fluids. The clinician is also obliged to abort the apnea test if the patient becomes hypoxic, defined as an O2 saturation <85% for > 30 seconds. An ABG should be drawn after 8-10 minutes, if the patient has been stable, and the ventilator reconnected. If the patient became hypotensive or hypoxic during testing, a brief period of hyperventilation can be used to rapidly correct the underlying respiratory acidosis which is likely the cause. If the pCO2 is >60 mm Hg, or >20 mm Hg above the baseline value, and the patient displayed no respiratory effort, the apnea test is positive and the patient is brain dead. © 2013 Neurocritical Care Society Practice Update If the pCO2 is <60 mm Hg or <20 mm Hg above the baseline value, but the patient displayed no visible respiratory effort during testing, the apnea test is indeterminate and should be repeated for a longer period of time (10-15 minutes), but only after again establishing hyperoxygenation, eucapnea and adequate blood pressure. If the testing cannot be performed adequately, an ancillary test may be necessary. Documentation The time of death is the time the arterial blood gas is officially reported, with the requisite pCO2 value. If an ancillary test is performed, the time of death is the time the test has been officially reported by the attending physician. Table 1 provides a template for brain death determination. REFERENCES 1. Plum F, Posner JB. The diagnosis of stupor and coma. Contemp Neurol Ser 1972;10:1286. 2. Levy DE, Caronna JJ, Singer BH, et al. Predicting outcome from hypoxic-ischemic coma. JAMA 1985;253:1420-1426. 3. Wijdicks EF, Hijdra A, Young GB, et al. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2006;67:203-210. 4. Greer DM, Yang J, Scripko PD, et al. Clinical examination for outcome prediction in nontraumatic coma. Crit Care Med. 2012;40:1150-1156. 5. Rossetti AO, Oddo M, Logroscino G, Kaplan PW. Prognostication after cardiac arrest and hypothermia: a prospective study. Ann Neurol. 2010;67:301-307. 6. Wijdicks EF, Varelas PN, Gronseth GS, Greer DM, American Academy of N. Evidencebased guideline update: determining brain death in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2010;74:1911-1198. © 2013 Neurocritical Care Society Practice Update Figure 1. Abnormal respiratory patterns associated with lesions in particular location in the brain (from Plum F and Posner JB. The Diagnosis of Stupor and Coma. 3rd Ed. Oxford, UK. Oxford University Press, 1982. With permission) © 2013 Neurocritical Care Society Practice Update Figure 2. Oculocephalic and Oculovestibular Reflexes (from Plum F and Posner JB. The Diagnosis of Stupor and Coma. 3rd Ed. Oxford, UK. Oxford University Press, 1982. With permission) The top panel illustrates the movements with the brainstem intact. With the oculocephalic (OCR) reflex, the eyes move in the opposite direction from which the head is turned. With the oculovestibular reflex (OVR), the eyes will deviate toward the cold-irrigated ear. Please note that hot water is never used, and simultaneous stimulation of both ears, either with cold or warm water, is rarely performed. In brain death (lowest panel), there are no eye movements with any stimuli. © 2013 Neurocritical Care Society Practice Update Table 1. Sample checklist for brain death determination I. PREREQUISITES A. Clinical/neuroimaging evidence of CNS catastrophe compatible with total and irreversible loss of brain function B. Absence of complicating medical conditions 1. Absence of severe electrolyte, acid-base or endocrine disturbance or severe hyperammonemia 2. Absence of drug intoxication or poisoning 3. Core temperature ≥36°C II. COMA or UNRESPONSIVENESS Absence of any cerebrally-mediated response to auditory and tactile noxious stimulation, peripherally and in the cranium III. ABSENCE of BRAINSTEM REFLEXES A. Absent pupillary responses 1. Pupillary size midposition or dilated 2. Pupils unresponsive to bright light B. Absent eye movements 1. Absent oculocephalic reflex (only tested with C-spine cleared) 2. Absent oculovestibular reflex (caloric responses) C. Absent corneal reflexes D. Absent pharyngeal and tracheal reflexes 1. Absent gag to posterior pharyngeal stimulation 2. Absent cough to bronchial suctioning 3. Absent spontaneous respirations IV. APNEA A. Prerequisites 1. Core temperature ≥36° C 2. Systolic BP ≥100 mmHg (with or without vasopressor agents) 3. Arterial pCO2 35-45 mm Hg (in known non-CO2 retainer) 4. Arterial pO2 greater than 200 mm Hg B. Apnea testing checklist 1. Preoxygenate to a PaO2 >200 mm Hg 2. Disconnect the ventilator; monitor with pulse oximeter 3. Deliver 100% FIO2 into the trachea via a cannula at the level of the carina, maintaining oxygen saturation above 85% 4. Check arterial blood gas at 8-10 minutes and reconnect the ventilator. The test is positive when either a) pCO2 is ≥60, or b) pCO2 is > 20 mmHg above the patient’s known baseline (in known CO2 retainers) 5. Abort the apnea test and immediately reconnect the ventilator for any of the following: a. SBP < 90 mm Hg or cardiovascular collapse b. Oxygen desaturation (<85% for >30 seconds) c. Significant cardiac arrhythmia d. Respiratory movements are observed C. Results of Apnea Testing 1. Apnea confirmed 2. Apnea testing contraindicated 3. Apnea test aborted 4. Apnea test indeterminate (may repeat) A. Yes No 1. Yes 2. Yes 3. Yes No No No Yes No 1. Yes No Untestable 2. Yes No Untestable 1. Yes No Untestable 2. Yes No Untestable C. Yes No Untestable 1. Yes No Untestable 2. Yes No Untestable 3. Yes No Yes Yes Yes Yes No No No No 1. Yes 2. Yes 3. Yes No No No 4. Yes No a. b. c. d. Yes Yes Yes Yes No No No No 1. 2. 3. 4. Yes Yes Yes Yes No No No No 1. 2. 3. 4. © 2013 Neurocritical Care Society Practice Update COMA AND BRAIN DEATH QUESTIONS 1. When testing the oculovestibular reflex, what is the proper head of bed angle? a) Flat b) 30 degrees c) 45 degrees d) 60 degrees e) The head of bed angle is irrelevant 2. When performing a coma examination, which are key prerequisites? a) Observing the patient b) Providing adequate stimulation c) Minimize distractions d) Detailed brainstem reflex examination e) All of the above 3. Pinpoint pupils reflect which of the following? a) Injury at the level of the red nucleus b) Pontine injury c) Diffuse bilateral injury d) Narcotic intoxication e) B and C 4. “Ping-Pong” eye movements reflect which of the following? a) Intact nuclei of the IIIrd and VIth nerves b) Severe brain stem dysfunction c) Unilateral hemispheric injury d) Brain death e) None of the above 5. All of the following are acceptable ways of testing a corneal reflex, EXCEPT: a) Squirts of sterile saline or water b) Cotton wisp c) Puff of air d) Pressing with a Q-tip e) None of the above are acceptable 6. The cardinal findings in brain death include all of the following, EXCEPT: a) Coma b) Extensor posturing c) Brainstem areflexia d) Apnea © 2013 Neurocritical Care Society Practice Update 7. Which of the following is/are used as the time of death for brain dead patients? a) When the pupils become unreactive b) When the apnea test is completed c) When the ABG values are consistent and officially reported d) When the ancillary test is formally interpreted by the fellow e) C and D 8. The lowest core temperature allowable for the clinical determination of brain death is: a) 32°C b) 33°C c) 34°C d) 35°C e) 36°C 9. Facial movements that do not preclude a clinical diagnosis of brain death include which of the following? a) Grimacing to nasal stimulation b) Corneal reflex c) Spontaneous facial myokymias d) Rhythmic facial twitching e) Smiling 10. All of the following are permissible signs in brain death, EXCEPT: a) Deep tendon reflexes b) Extensor posturing c) Lazarus signs d) Triple flexion e) Babinski sign © 2013 Neurocritical Care Society Practice Update COMA AND BRAIN DEATH ANSWERS 1. The correct answer is B. At 30 degrees there is proper orientation of the horizontal semicircular canals, providing maximal stimulation and the highest probability of seeing a response. 2. The correct answer is E. All of the answers listed ensure an optimal examination setting for evaluating a comatose patient. 3. The correct answer is E. Both pontine injury and narcotic intoxication can cause small or “pinpoint” pupils. Diffuse bilateral injury is more likely to cause midsize to dilated pupils. The red nucleus is at the level of the midbrain, and “midbrain pupils” are typically midposition and mid-size (3-6 mm). 4. The correct answer is A. “Ping-Pong” eye movements reflect some integrity of the brainstem, as the eyes are able to move laterally. A unilateral hemispheric injury will typically cause a gaze deviation to one side. In brain death, there are no eye movements, either spontaneously or in response to testing. 5. The correct answer is C. Acceptable methods for testing a corneal reflex include use of squirts of sterile saline or water, a cotton wisp or pressing with a Q-tip, the latter typically reserved for brain death examinations. A puff of air may be produced due to improper technique while trying to test a blink to visual threat, but is not a potent enough or valid method for testing a corneal reflex. 6. The correct answer is B. Extensor posturing is a brainstem-mediated response, and is not permissible in brain death. The cardinal findings in brain death are coma, brainstem areflexia and apnea. 7. The correct answer is C. The two times that may be used as the official time of death are when the ABG values are reported that have a pCO2 in the correct range, or when the ancillary test is official interpreted by an attending physician (not a fellow or resident). 8. The correct answer is E. 36°C. 9. The correct answer is C. Grimacing and smiling are purposeful responses. A corneal reflex signifies brainstem integrity with the reflex arc involving cranial nerves V and VII. Rhythmic facial twitching suggests possible seizure, which is cerebrally-mediated. Facial myokymias are permissible, so long as they are only spontaneous, and not in response to stimulation. 10. The correct answer is B. Extensor posturing is a brainstem-mediated response, and not permissible in brain death.